Abstract
This paper introduces a conceptual framework for investigating individual ability to navigate healthcare in the contexts of the built environment, social environment, and healthcare infrastructure in which a person is embedded. Given the complexity of healthcare delivery in the United States, consumers are expected to have an increasingly sophisticated set of skills in order to effectively navigate and benefit from the healthcare resources available to them. Addressing barriers to navigation in vulnerable populations may be essential to reducing health disparities. This paper builds on previous conceptual developments in the areas of healthcare use, navigation, and ecological perspectives on health in order to present a behavioral-ecological framework for examining healthcare navigation and access. The model posits that healthcare navigation is an ecologically informed process not only because of the spatial distribution of health services, but because of the spatial distribution of individual and environmental factors that influence decision-making and behavior with respect to service use. The paper discusses areas for further research on healthcare navigation, challenges for research, and implications for reducing health disparities.
Introduction
In order for a healthcare consumer to make optimal use of the healthcare system in the United States, various enabling factors must favorably converge. These factors include several dimensions of healthcare access, including availability of services, affordability, and transportation, as well as health literacy, skills in communicating with healthcare providers, and social support to facilitate decision-making, treatment adherence, and healthy behaviors. Moreover, consumers and/or caregivers need an increasingly sophisticated set of skills in navigating the complexities of healthcare coverage, choosing providers, scheduling and follow-up, and weighing treatment options. Healthcare navigation can be defined as “the process(es) by which patients and/or their health caregivers move into and through the multiple parts of the healthcare enterprise in order to gain access to and use its services in a manner that maximizes the likelihood of gaining the positive health outcomes available” from these services (Sofaer 2009). Thus, while the concept of access encompasses the structural circumstances shaping healthcare opportunities and constraints, navigation is a set of dynamic processes through which individuals respond to healthcare needs, pursue opportunities, and manage constraints. These processes occur in the context of intersecting biomedical, psychosocial, economic, and environmental conditions that are often experienced differentially by race and ethnicity, as well as cultural norms, preferences and expectations.
Given that healthcare navigation is critical to a person’s involvement in his/her care and related health outcomes, addressing barriers to navigation in vulnerable populations may be essential to reducing health disparities and improving population health in general. However, there is a scarcity of tools for measuring navigation ability and a need for research to understand the myriad factors that support and hinder navigation (Sofaer 2009). To support this direction of research, this paper adds to previous conceptual developments in the area of navigation (Sofaer 2009) by expanding upon its environmental dimensions. First, the paper presents a brief overview of existing perspectives on environmental/spatial dimensions of health and healthcare access. Second, the paper proposes a conceptual framework that synthesizes two of these perspectives – namely, the behavioral model of health service use and the social-ecological model of aging and the life course. The framework is designed to guide research on healthcare access in an aging population, thus situating navigation in the contexts of the built environment, social environment, and healthcare infrastructure in which a person is embedded. Lastly, the paper discusses areas for further research on navigation, challenges for research, and implications for reducing health disparities.
Existing perspectives on spatial dimensions of health and healthcare access
The current work is informed by areas of prior research that address the spatial dimensions of health and/or access to healthcare, each of which has implications for the concept of navigation as an environmentally situated process. These perspectives speak to an overarching question: how are opportunities for managing one’s health spatially distributed and defined? One perspective stems from the large body of research examining geographic variation in healthcare access, utilization, costs, and outcomes. For example, studies have examined the geographic distribution of primary care supply in relation to potentially preventable hospitalizations (Bynum et al. 2011, Chang et al. 2011, Laditka et al. 2005, Laditka and Laditka 1999). Researchers have used national data to examine aggregate-level variations, comparing regions of the country, counties within regions, healthcare service areas, or metropolitan statistical areas.
Another body of research has examined spatial factors in health from a more granular perspective, focusing on the relationships between characteristics of the neighborhoods in which people live and individual health behaviors and outcomes (Diez Roux 2004, 2007, Yen et al. 2009). The need to identify factors underlying health disparities has motivated much of this work. Researchers have attempted to disentangle the health effects of neighborhood characteristics in various domains, such as socio-economic factors, social capital, safety, and the built environment. Numerous studies have examined the effects of neighborhood characteristics on health behaviors – including physical activity, fruit and vegetable consumption, and a high-fat diet – and health outcomes – including obesity and mortality (Freedman et al. 2011, Freedman et al. 2008, Grafova et al. 2008, Kawachi et al. 1997, Li et al. 2009a, Li et al. 2009b, Mobley et al. 2006, Winstanley et al. 2008, Witten et al. 2012, Lovasi et al. 2011, Mohnen et al. 2012). However, less is known about the ways in which the social and built environment characteristics of neighborhoods influence healthcare access and navigation.
In much of the published work on both geographic variation in health service use and neighborhood effects on health, the conceptual underpinnings of the analysis are implicit. This work is also challenged by the multiple approaches to defining geographic units of analysis as deemed appropriate for the environmental measures of interest. Whereas larger units of analysis such as counties or healthcare service areas may be considered too broad for some studies, more granular concepts of “neighborhood” are subject to numerous definitions based on both objective boundaries and subjective interpretations. Nevertheless, there have been important conceptual developments during the last thirty years that potentially complement one another and can be more fully integrated into ongoing work on healthcare access, navigation, and the environment.
The conceptual model proposed in this paper merges and builds on two broad models that relate to the bodies of research introduced above. The first is the behavioral model of health service use originally developed by Ronald Andersen in the 1960s (Andersen 1968). The model focuses on three domains of population characteristics as predictors of health service use and subsequent outcomes, namely: predisposing, enabling, and need factors (Andersen 1995). Predisposing factors include age, sex, and race/ethnicity, as socio-demographic factors represent a person’s social status, and in turn, the ability to command necessary resources to cope with health problems. Health beliefs, attitudes and values are also considered to be predisposing characteristics which could be informed by cultural or generational factors. Enabling factors are resources that facilitate or hinder service use, such as income level and health insurance. Need factors include both the patient’s perception and provider’s evaluation of healthcare needs, including health status and diagnoses. These three types of factors are determinants of health service use and personal health practices, comprising the larger domain of health behavior. These behaviors influence outcomes, including perceived health status, evaluated health status, and consumer satisfaction. The model also acknowledges the potential impact of the external environment on health service use, including physical, political, and economic aspects of the environment (Andersen 1995). The behavioral model has undergone several adaptations to account for the unique factors affecting service use in vulnerable populations (Gelberg et al. 2000). One particular adaptation adds the domain of “community characteristics,” including features of the safety net and public policy supports for low-income populations (Davidson et al. 2004).
The second conceptual model that informs the current discussion is the ecological model in the epidemiology of aging (Satariano 2006). The basic premise of this model is that a range of individual-level and contextual factors influences an individual’s health, physical and cognitive function over the life course, and survival. Individual variables include demographic, socio-economic, physiological, and psychosocial characteristics, and contextual variables include characteristics of the local environment (e.g. built and physical environment) and social capital. The ecological model of aging has conceptual roots in M. Powell Lawton’s model of “environmental press,” which suggests that individual competencies, the demands of the environment, and the interaction between the person and the environment shape individual behavior and well-being over the life course (Lawton 1986). The impact of environmental factors on a person’s health and well-being varies along a continuum of weak to strong, while a person’s competence in adapting to the demands or “press” of the environment ranges from low to high. In a situation of strong environmental press, an individual with greater competencies would adapt positively, whereas an individual with lower competencies would adapt more poorly, experiencing negative physical and psychological outcomes, such as falls and stress. The concept of the individual continually adapting to environmental demands throughout the life course – and the relationships between a person’s behavioral adaptations, health, and well-being – is an underlying principle in the growing body of research on the social determinants of health.
The above models underscore different and compatible factors relevant to healthcare access and navigation in environmental contexts. The behavioral model, as adapted by Davidson et al. (2004), emphasizes variations in the healthcare environment as important enabling factors in healthcare access, while the ecological model of aging emphasizes other environmental variables – such as built environment and social capital – as key factors in individual health. The conceptual model proposed in this paper combines the key features of these two frameworks while highlighting the environmental phenomena influencing healthcare navigation.
A behavioral-ecological model of healthcare access and navigation
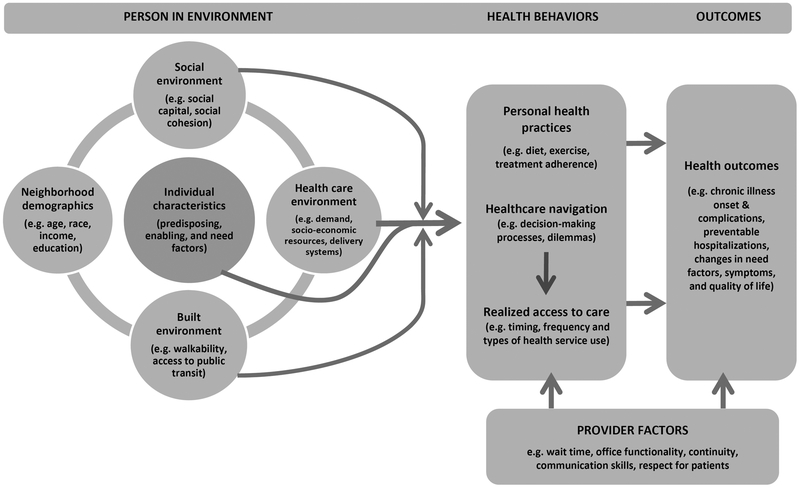
The model proposed here (Figure 1) includes the basic structure of the behavioral model of health service use while highlighting different domains of environmental phenomena. Like the behavioral model, the proposed model assumes that individual characteristics – namely, predisposing, enabling, and need factors (Andersen 1995, Davidson et al. 2004) – influence realized access to care, measured as health service use. In the behavioral model, however, the navigation processes underlying this relationship are implicit. In the proposed model, these individual characteristics are among the myriad factors that inform the processes of navigation through which individuals respond to opportunities and constraints in managing one’s health. The proposed model posits that individual-level enabling factors – and conversely, constraining factors – are important in determining the degree to which an individual is able to effectively navigate the healthcare system. Drawing on Sofaer’s model of navigation (Sofaer 2009), a person’s education level, health literacy, communication skills, degree of self-efficacy, and informal caregiver support have been identified as important factors in navigation. Someone with a higher level of education might also have a higher level of health literacy and confidence in communicating with health care providers, whereas lower education and/or health literacy might hinder communication in the absence of system-level supports for individuals with health literacy challenges (Gwynn et al. 2016, Paasche-Orlow 2011).
Figure 1.
Behavioral-Ecological Framework of Healthcare Access and Navigation
Additionally, psychosocial factors such as health-related self-efficacy and depression might enable or hinder effective navigation, respectively, as has been shown with respect to self-management of chronic conditions (Bayliss et al. 2007). Social support might enable or hinder navigation in a variety of ways that might not always be straightforward. A supportive caregiver could be an asset in dealing with health literacy issues or functional limitations, overcoming transportation barriers and other logistical problems, and facilitating adherence to a treatment plan. However, in some scenarios a cohesive social support system could be an obstacle to effective navigation in an environment where distrust of healthcare providers is common (Ganter et al. 2015, Musa et al. 2009).
Building on the behavioral model, the proposed model posits that the complex interactions among an individual’s predisposing, need, and enabling (or constraining) characteristics influence a person’s health behavior, which includes health practices (such as diet, exercise, and treatment adherence), healthcare navigation processes, and associated variations in realized access to care. Simultaneously, provider factors also inform health behaviors and the person’s navigation experiences. As previously described by Sofaer, a range of provider characteristics influence the ease or difficulty of navigation. These include but are not limited to: links between providers; the functionality of office operations; communication skills, respect for patients, and the provider’s perceptions of both patient and provider roles in a person’s care. Moreover, the quality of the patient-provider relationship affects the navigation experience; this includes issues of mutual trust and respect (Sofaer 2009). In turn, these processes influence health outcomes – such as onset of illness, complications of chronic disease, hospitalizations, and changes in functional status, symptoms and quality of life – as well as subsequent perceptions of healthcare needs in a dynamic fashion.
As in the behavioral model, the healthcare environment represents potential access to care. The proposed model builds on this premise by positing that other types of environmental factors moderate the ways in which individuals with different characteristics navigate the healthcare resources locally available to them. Building on the ecological model of aging (Satariano 2006, Lawton 1986), the proposed model focuses on three categories of environmental characteristics in which the individual is embedded: the healthcare environment, the social environment, and the built environment. Local features of the social and built environments may moderate the relationship between potential access (e.g. available healthcare resources) and realized access (e.g. actual service use) by shaping the processes of navigation.
The following discussion provides an overview of prior research within each environmental domain and how each domain potentially relates to healthcare navigation and realized access. It is important to acknowledge at the outset that most of the prior research on the health effects of the built and social environment utilizes a construct of the “neighborhood” as the unit of analysis for environmental measures. This construct is subject to a wide range of definitions based on varying physical boundaries – for example, census tracts, zip codes, or a distance-specific radius around the individual – or perceptions of relevant geographic boundaries as defined by an individual. Despite the challenges of defining neighborhood and variable definitions in the literature (Northridge et al. 2003), I adopt the term “neighborhood” here for the purpose of gleaning insight from previous research on the built and social environments. (Although the challenges of defining the neighborhood are an important area for discussion, a full treatment of these issues is outside the scope of this paper.)
In the context of this discussion, “neighborhood” refers generally to a relatively granular geographic area surrounding the individual’s place of residence and containing physical, social, and economic attributes with which the individual interacts in daily activities of travel, work, recreation, and accessing resources. These attributes are referred to here as “environmental characteristics.” Measures of neighborhood demographic composition – such as socio-economic, racial, age, and household composition – may be correlated with environmental characteristics as well as healthcare access and navigation processes. These demographic variables are shown in the proposed model but are distinguished from the three domains of environmental characteristics that function as potential explanatory mechanisms.
Healthcare environment.
For the purpose of the proposed model, the concept of the healthcare environment refers to a combination of market factors that constitute potential healthcare access within a geographic area. Andersen et al. describe four categories of variables that can be considered as main elements of the healthcare environment (Andersen et al. 2002). The first category of includes indicators of healthcare demand (Andersen et al. 2002). For example, the demand for safety-net primary care providers, such as health clinics serving low-income individuals, varies with the proportions of people in a given geographic area who are below the poverty level, are uninsured, and have Medicaid (Laditka and Laditka 1999, Billings et al. 1996, Bindman et al. 1995, Laditka and Johnston 1999). The second category within the healthcare environment is comprised of the socio-economic resources within a geographic area that influence the availability of a particular service (referred to by Andersen et al. as “support variables”). This category includes per capita income, income inequality, and unemployment (Andersen et al. 2002). The third category is delivery system characteristics, such as the supply of providers and the types of services available in a given geographic area, such as availability of safety-net providers (Andersen et al. 2002). The fourth category includes market dynamics, including payment systems variables, such as the different types of insurance coverage and the degree of managed care penetration in a geographic area (Andersen et al. 2002, Cunningham 1999, Rosenthal et al. 2005). The interactions of these supply and demand factors, along with socio-economic resources and market dynamics, are embedded within and influenced by the policy environment and the complexities of regulatory requirements.
Prior studies examining geographic variation in the healthcare environment have focused on relatively large geographic units, such as states, counties, and metropolitan statistical areas. Another approach defines geographic units based on research patterns of service utilization (Goodman et al. 2003, Skinner and Wennberg 1998, Wennberg and Gittelsohn 1973). Increasing attention has been paid to more granular variations in healthcare supply, such as at the census tract level (Brown et al. 2015). However, less is known about how granular variations in the healthcare environment, the social environment, and the built environment influence potential access, the ways that individuals navigate healthcare resources, and emergent patterns in realized access. More granular variations may be especially relevant in the context of dense urban settings, where even within a small area (e.g. such as a zip code) there may be significant variation in access to transportation and other factors that could facilitate or hinder service use. Guagliardo accounts for this in the concept of “spatial accessibility,” which posits that travel barriers must be considered along with geographic variation in measures of healthcare resources in order to fully understand spatial variations in access (Guagliardo 2004). Other researchers have also examined transportation and travel time to providers as components of access to care (Delamater et al. 2012).
The proposed conceptual model posits that the above components of the healthcare environment are central, but not sufficient, in defining the relationship between potential access (e.g. available healthcare resources) and realized access (e.g. actual utilization). Elements of the social and built environments may be important factors that moderate the ability of consumers to effectively navigate the healthcare resources available to them. Understanding the role of these environmental factors requires a more granular level of analysis than what may be appropriate for measuring variations in the healthcare environment. Thus, the model turns to the more local level of the “neighborhood” to address this gap, acknowledging that the neighborhood has been subject to myriad definitions in the prior literature.
Social environment.
Prior studies have examined associations between neighborhood social environment and individual health. The social environment includes several measures pertaining to the quality of social relationships in the neighborhood, such as perceived social cohesion and support, trust in neighbors, collective efficacy, and civic involvement. Broadly speaking, these measures constitute the concept of social capital. Higher levels of neighborhood social capital have been linked to better self-rated health (Kawachi et al. 1997, Boyce et al. 2008, Hibino et al. 2012), better self-reported mental health (Hamano et al. 2010, Kruger et al. 2007), less depression (Haines et al. 2011, Tomita and Burns 2013), lower mortality (Hutchinson et al. 2009, Lochner et al. 2003), greater physical activity (King 2008, Mohnen et al. 2011, Davison et al. 2012), lower likelihood of smoking (Mohnen et al. 2011, Sapag et al. 2010), lower use of drugs and alcohol (Winstanley et al. 2008), and better oral health (Pattussi et al. 2006, Aida et al. 2011). Kawachi et al. (1997) found that disinvestment in social capital was a mediating factor in an observed association between income inequality and increased mortality. King found that higher perceptions of neighborhood safety and social cohesion were associated with greater physical activity among older adults (King 2008).
Although numerous studies have shown significant associations between greater social capital and health, some have shown mixed results or even a possible “downside” to social capital. For example, Subramanian et al. found that higher levels of community social trust were associated with better self-rated health; however, this effect differed greatly depending on a person’s level of social trust (Subramanian et al. 2002). Caughy et al. found that, among African American preschool aged children, low social integration was associated with greater behavior problems in wealthy neighborhoods, whereas the opposite effect was seen in poorer neighborhoods (Caughy et al. 2003).
Despite a rich body of research examining the relationship between neighborhood social environment and health behavior and outcomes, less is known about how the social environment might influence the processes of healthcare navigation and the ability of individuals to make effective use of the healthcare resources available to them. The proposed conceptual model posits that social environmental factors could moderate the relationship between potential access and realized access to care by enabling or hindering the complex processes of navigation. Evidence in support of this hypothesis was found in a pilot study related to the current project on environmental factors in access to primary care among urban older adults. Specifically, higher scores in perceived neighborhood social cohesion were associated with a greater likelihood of primary care use among individuals who lived in areas with lower physician supply, even while controlling for individual-level social support, demographic, socio-economic, and health characteristics (Ryvicker et al. 2012). However, the mechanisms underlying this relationship remain unclear. One possible hypothesis is that greater social cohesion facilitates the use of public transportation and/or paratransit services, thereby enabling the use of primary care. Another possible hypothesis is that greater social cohesion facilitates the exchange of information about how to take care of one’s health, which, in turn, might make an individual more likely to use services. Further research is needed to better understand the potential mechanisms underlying this relationship.
Built environment.
During the past decade, a vast body of research has examined the relationship between the built environment and health. The term “built environment” refers to the physical infrastructures and configuration of public space of a neighborhood, city, town, or other small area. The concept of the built environment includes structures such as roads, highways, parks, playgrounds, public transportation, and the mix of residential and commercial use of land. These structures all have potential influence on individual behavior and the ways in which people travel, socialize, work, recreate, interact with the economy, and utilize social and health services. Given the variety of dimensions comprising the built environment, defining and validating the most relevant measures have proven challenging (Cunningham and Michael 2004). Some recent efforts have focused on developing an index of neighborhood walkability (Frank et al. 2010), as well as examining the relationship between perceived and objective measures of the built environment (Gebel et al. 2009, McGinn et al. 2007, Michael et al. 2006, Weiss et al. 2010).
Researchers have examined the ways in which physical activity and obesity are sensitive to the availability of parks and recreational spaces, neighborhood safety, and “walkability” measures – such as the presence of sidewalks, street connectivity, the mix of residential and commercial land use, and the flow and safety of traffic (Mobley et al. 2006, McGinn et al. 2007, Auchincloss et al. 2008, Carlson et al. 2012, Lovasi et al. 2009, Rundle et al. 2007, Sallis et al. 2009, Troped et al. 2011, Wen and Kowaleski-Jones 2012, Wen and Maloney 2011). Studies have shown that people who live in more walkable neighborhoods have higher levels of physical activity (Witten et al. 2012, de Vries et al. 2007, Fields et al. 2013, Frank et al. 2007), are less likely to be obese (Mobley et al. 2006, Frank et al. 2007, Heinrich et al. 2008, McAlexander et al. 2009, Singh et al. 2010), and have better cardiorespiratory fitness (Hoehner et al. 2011). Researchers have also examined the effect of walkability, access to public transit, and the presence of bicycle paths on the use of active transit, such as walking and cycling (Berrigan et al. 2010, Charreire et al. 2012, Coogan et al. 2007, Freeman et al. 2013, Kaczynski 2010, Lovasi et al. 2013, Winters et al. 2010). Some studies have also shown greater social capital in neighborhoods with greater walkability (Leyden 2003) and access to parks (Cohen et al. 2008).
Several studies have specifically focused on the relationship between the built environment and the health of older adults. Some have shown an association between greater walkability and greater physical activity among older adults (Berke et al. 2007, Li et al. 2008, Nagel et al. 2008), as well as greater lower-extremity strength (Michael et al. 2011) and lower blood pressure (Li et al. 2009b). Freedman et al. found that older men who live in neighborhoods with greater street connectivity had fewer limitations in activities of daily living (Freedman et al. 2008). Moreover, older women living in neighborhoods with greater street connectivity were less likely to be overweight or obese (Grafova et al. 2008). However, another study found that, while older adults living in more walkable neighborhoods did more walking for errands, overall physical activity levels were associated more with their perceptions of neighborhood safety and social cohesion than with built environment characteristics (King 2008). Other research on older adults has found that architectural features that allowed neighbors to observe street activity, such as porches and stoops, influenced social interaction in public settings, which in turn affected social support and psychological wellbeing (Brown et al. 2009). These architectural features have also been linked to greater physical function among older adults (Brown et al. 2008). This work suggests a complex interaction between the built and social environments as they influence health and wellbeing.
Despite the growing body of research on the built environment and health, the relationship between the built environment and healthcare navigation and access is relatively understudied. Some studies have examined distance to providers and travel time as indicators of access, with particular emphasis on rural settings (Rosenthal et al. 2005, Fortney et al. 1998, Gresenz et al. 2007, LaVela et al. 2004, Mayer et al. 2009). Although distances to providers may be relatively short in dense urban settings compared to sparse rural settings, urban dwellers may face a unique set of travel-related challenges that are affected by variations in the built environment. The proposed conceptual model posits that variations in walkability and access to public transportation might affect an individual’s ability to use the healthcare resources available to them locally, moderating the relationship between potential and realized access to care. Aside from home healthcare for home-bound individuals, the use of outpatient health services requires mobility and an ability to navigate the surrounding landscape through the use of public and/or private transportation and, if necessary, social support. In this regard, navigation of the built environment and navigation of the healthcare system may be intricately linked. Older adults with functional limitations may be particularly affected by variations in the built environment, especially those without adequate social, family, or paid caregiver support to help with transportation. Research is needed to investigate how variations in the built environment affect the processes of healthcare navigation and realized access to care, especially for vulnerable groups who may be particularly sensitive to transportation challenges, such as older adults with chronic illness and/or functional disabilities.
Summary and limitations
The behavioral-ecological model proposed in this paper synthesizes prior concepts of the healthcare environment, social environment, and built environment as causal and moderating factors in healthcare navigation and access. The proposed model builds on both the behavioral model of health service use and the social-ecological model of aging by highlighting healthcare navigation as a set of dynamic processes informed by multiple interacting factors at the individual and environmental levels. The model is designed to guide future research on the facilitators to and barriers of effective healthcare navigation, with particular emphasis on vulnerable populations who are disproportionately affected by health disparities. In summary, the model posits that the social and built environments may be important moderating factors in the relationships between individual characteristics, the healthcare environment and an individual’s ability to effectively navigate locally available healthcare resources.
Some limitations in the presentation of this model should be noted. Although the synthesis of relevant literature covers a broad range of areas, the paper does not present a systematic review of evidence within the domains described in the model. To do so would likely require several systematic reviews focused on each of the domains, which could each constitute a separate paper. Nevertheless, the targeted literature review presented here helps to identify gaps in the prior work that are relevant to the proposed model. Additionally, the current discussion does not aim to cover the full array of healthcare systems and provider factors that influence navigation processes. Whereas a more detailed treatment of these domains is provided by Sofaer (2009), the model proposed here expands on the prior work by going into further depth on the environmental domains that may be important influences in healthcare navigation and access. It is possible that there are yet other environmental domains not addressed here, and there may be yet unaccounted for bidirectional relationships or causal feedback loops among the factors presented. The proposed model does not assume to cover the full array of possible factors, interactions, and causal relationships, but aims to provide a foundation that could be used for further conceptual development as other potential mechanisms are investigated. Finally, healthcare navigation processes are only a portion of a much larger system that determines health outcomes. Nevertheless, given that navigation is relatively understudied, it is worthwhile to establish a foundational theory of navigation within a multi-faceted behavioral-ecological framework.
Future directions, challenges, and implications
As previously proposed by experts on patient navigation, a research agenda on navigation would include efforts in four main areas (Sofaer 2009). First, it would establish a baseline “epidemiology” of navigation issues and how consumers deal with system complexity under different circumstances. The conceptual model proposed in this paper could be used to guide the design of such studies and to outline the different types of individual and environmental circumstances to be examined in the “epidemiology” of navigation. Second, research is needed to take an inventory and assess the impacts of different interventions and models of care currently being used to address navigation issues. Third, there is a need for new approaches to redesign healthcare to make it more easily navigable. Finally, research is needed to document the health and financial impacts of navigation problems (Sofaer 2009).
The latter three of these research endeavors depends heavily on the ability to establish a baseline understanding of the ‘who, what, when, where and how’ of navigation problems. However, some methodological challenges need to be addressed in order to establish this evidence base. First, there is a relative dearth of measurement tools related specifically to navigation (Haun et al. 2015). Although some validated health literacy measures include specific questions related to navigation, as of yet there are no validated measures specifically designed to capture an individual’s understanding of how to navigate the healthcare system and ability to cope with navigation challenges (Haun et al. 2015). How would we define such a construct? Developing such a measure would be an important contribution to the research agenda on navigation and its relationship to disparities in healthcare access, outcomes, and patient experiences. This would likely require a combination of qualitative and quantitative pilot work in order to identify the relevant domains that comprise such a construct.
A second and related challenge is in identifying existing data sources that could support this research agenda. In addition to the pilot data needed to develop measurement tools, an epidemiology of navigation would require a variety of data sources to examine the array of individual-level and environmental phenomena potentially influencing navigation processes and associated variation in realized access and health outcomes. One possibility going forward could be to add a newly validated measure of navigation ability to existing national health surveys, such as the National Health and Aging Trends Study (NHATS) (Johns Hopkins School of Public Health and Westat 2015) and the National Health Interview Survey (NHIS) (Centers for Disease Control and Prevention 2016). The ability to link the NHATS to Medicare claims data would allow investigators to analyze the relationship between navigation ability and actual health service use. Nevertheless, this would still leave a gap in our understanding of the patient’s experience of navigation processes. To fill this gap would require a rigorous qualitative examination of patients’ navigation experiences in different circumstances, focusing on subpopulations with different combinations of demographic and health characteristics as well as environmental surroundings. Thus, a comprehensive research agenda aimed at identifying potential solutions to healthcare navigation problems would likely require a mixed methods approach.
Insofar as systems navigation is a critical aspect of patients’ involvement in their care and related health outcomes, addressing barriers to navigation in vulnerable populations may be essential to reducing and, ultimately, eliminating health disparities. A comprehensive research agenda on navigation and its relationship with access and health outcomes could therefore be an important element of broader efforts to address disparities. Approaching this agenda through a spatially and ecologically informed framework could ultimately be useful for “mapping” the epidemiology of navigation barriers and identifying geographic areas where particular navigation barriers are especially concentrated. The framework could be applied to research on both rural and urban settings and used to investigate how navigation facilitators and barriers operate differently across these settings. This approach could help to guide policy and practice decisions aimed at ameliorating navigation problems. For example, some geographic areas might have a particular need for transportation services combined with healthcare companion support, whereas other areas might have a heightened need for education about underutilized healthcare resources, tailored for individuals with low health literacy. In conclusion, navigation is a spatially informed process not only because of the spatial distribution of health services, but because of the spatial distribution of enabling, predisposing and need factors that influence decision-making about how and when to use particular services, as well as the environmental factors that moderate these decisions and behavioral processes. A behavioral-ecological approach to investigating and addressing navigation barriers may be an important step in promoting health equity.
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number K01AG039463. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health. The author would like to thank Penny Feldman, Ph.D., William Gallo, Ph.D., and David Russell, Ph.D. for their input on previous drafts of the paper.
References
- Sofaer S (2009) Navigating poorly charted territory: patient dilemmas in health care “nonsystems”. Med Care Res Rev 66(1 Suppl), 75S–93S. [DOI] [PubMed] [Google Scholar]
- Bynum JP, Andrews A, Sharp S, et al. (2011) Fewer hospitalizations result when primary care is highly integrated into a continuing care retirement community. Health Aff (Millwood) 30(5), 975–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CH, Stukel TA, Flood AB, et al. (2011) Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA 305(20), 2096–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB and Probst J (2005) More may be better: Evidence that a greater supply of primary care physicians reduces hospitalization for ambulatory care sensitive conditions. Health Serv Res 40(4), 1148–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laditka SB and Laditka JN (1999) Geographic variation in preventable hospitalization of older women and men: implications for access to primary health care. J Women Aging 11(4), 43–56. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV (2004) Estimating neighborhood health effects: the challenges of causal inference in a complex world. Social Science & Medicine 58(10), 1953–1960. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV (2007) Neighborhoods and health: where are we and where do we go from here? Rev Epidemiol Sante Publique 55(1), 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Michael YL and Perdue L (2009) Neighborhood environment in studies of health of older adults: a systematic review. American Journal of Preventive Medicine 37(5), 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Grafova IB and Rogowski J (2011) Neighborhoods and Chronic Disease Onset in Later Life. American Journal of Public Health 101(1), 79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Grafova IB, Schoeni RF, et al. (2008) Neighborhoods and disability in later life. Social Science & Medicine 66(11), 2253–2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grafova IB, Freedman VA, Kumar R, et al. (2008) Neighborhoods and obesity in later life. American Journal of Public Health 98(11), 2065–2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP, Lochner K, et al. (1997) Social capital, income inequality, and mortality. Am J Public Health 87(9), 1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer P, Cardinal BJ, et al. (2009a) Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am J Health Promot 23(3), 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer P, Cardinal BJ, et al. (2009b) Built environment and changes in blood pressure in middle aged and older adults. Preventive Medicine 48(3), 237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobley LR, Root ED, Finkelstein EA, et al. (2006) Environment, obesity, and cardiovascular disease risk in low-income women. American Journal of Preventive Medicine 30(4), 327–332. [DOI] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, et al. (2008) The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend 92(1–3), 173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witten K, Blakely T, Bagheri N, et al. (2012) Neighborhood built environment and transport and leisure physical activity: findings using objective exposure and outcome measures in New Zealand. Environmental Health Perspectives 120(7), 971–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovasi GS, Jacobson JS, Quinn JW, et al. (2011) Is the environment near home and school associated with physical activity and adiposity of urban preschool children? J Urban Health 88(6), 1143–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohnen SM, Volker B, Flap H, et al. (2012) Health-related behavior as a mechanism behind the relationship between neighborhood social capital and individual health--a multilevel analysis. BMC Public Health 12, 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R (1968) A Behavioral Model of Families’ Use of Health Services, Center for Health Administration Studies, University of Chicago, Chicago. [Google Scholar]
- Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36(1), 1–10. [PubMed] [Google Scholar]
- Gelberg L, Andersen RM and Leake BD (2000) The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res 34(6), 1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Davidson PL, Andersen RM, Wyn R, et al. (2004) A framework for evaluating safety-net and other community-level factors on access for low-income populations. Inquiry 41(1), 21–38. [DOI] [PubMed] [Google Scholar]
- Satariano W (2006) Epidemiology of Aging: An Ecological Approach, Jones and Bartlett Publishers, Sudbury, MA. [Google Scholar]
- Lawton M (1986) Environment and Aging, Center for the Study of Aging, Albany, NY. [Google Scholar]
- Gwynn KB, Winter MR, Cabral HJ, et al. (2016) Racial disparities in patient activation: Evaluating the mediating role of health literacy with path analyses. Patient Educ Couns 99(6), 1033–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche-Orlow M (2011) Caring for patients with limited health literacy: a 76-year-old man with multiple medical problems. JAMA 306(10), 1122–1129. [DOI] [PubMed] [Google Scholar]
- Bayliss EA, Ellis JL and Steiner JF (2007) Barriers to self-management and quality-of-life outcomes in seniors with multimorbidities. Ann Fam Med 5(5), 395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganter C, Chuang E, Aftosmes-Tobio A, et al. (2015) Community stakeholders’ perceptions of barriers to childhood obesity prevention in low-income families, Massachusetts 2012–2013. Prev Chronic Dis 12, E42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa D, Schulz R, Harris R, et al. (2009) Trust in the health care system and the use of preventive health services by older black and white adults. American Journal of Public Health 99(7), 1293–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge ME, Sclar ED and Biswas P (2003) Sorting out the connections between the built environment and health: a conceptual framework for navigating pathways and planning healthy cities. J Urban Health 80(4), 556–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM, Yu H, Wyn R, et al. (2002) Access to medical care for low-income persons: how do communities make a difference? Med Care Res Rev 59(4), 384–411. [DOI] [PubMed] [Google Scholar]
- Billings J, Anderson GM and Newman LS (1996) Recent findings on preventable hospitalizations. Health Aff (Millwood) 15(3), 239–249. [DOI] [PubMed] [Google Scholar]
- Bindman AB, Grumbach K, Osmond D, et al. (1995) Preventable hospitalizations and access to health care. JAMA 274(4), 305–311. [PubMed] [Google Scholar]
- Laditka SB and Johnston JM (1999) Preventable hospitalization and avoidable maternity outcomes: implications for access to health services for Medicaid recipients. J Health Soc Policy 11(2), 41–56. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ (1999) Pressures on safety net access: the level of managed care penetration and uninsurance rate in a community. Health Serv Res 34(1 Pt 2), 255–270. [PMC free article] [PubMed] [Google Scholar]
- Rosenthal MB, Zaslavsky A and Newhouse JP (2005) The geographic distribution of physicians revisited. Health Serv Res 40(6 Pt 1), 1931–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman DC, Mick SS, Bott D, et al. (2003) Primary care service areas: a new tool for the evaluation of primary care services. Health Services Research 38(1 Pt 1), 287–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner J and Wennberg J (1998) How much is enough? Efficiency and Medicare spending in the last six months of life.
- Wennberg J and Gittelsohn (1973) Small area variations in health care delivery. Science 182(4117), 1102–1108. [DOI] [PubMed] [Google Scholar]
- Brown EJ, Grande DT, Barbu CM, et al. (2015) Location Matters: Differences in Primary Care Supply by Neighborhood in Philadelphia, Leonard Davis Institute of Health Economics. [Google Scholar]
- Guagliardo MF (2004) Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr 3(1), 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delamater PL, Messina JP, Shortridge AM, et al. (2012) Measuring geographic access to health care: raster and network-based methods. Int J Health Geogr 11(1), 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce WF, Davies D, Gallupe O, et al. (2008) Adolescent risk taking, neighborhood social capital, and health. J Adolesc Health 43(3), 246–252. [DOI] [PubMed] [Google Scholar]
- Hibino Y, Takaki J, Ogino K, et al. (2012) The relationship between social capital and self-rated health in a Japanese population: a multilevel analysis. Environ Health Prev Med 17(1), 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamano T, Fujisawa Y, Ishida Y, et al. (2010) Social capital and mental health in Japan: a multilevel analysis. PLoS One 5(10), e13214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger DJ, Reischl TM and Gee GC (2007) Neighborhood social conditions mediate the association between physical deterioration and mental health. Am J Community Psychol 40(3–4), 261–271. [DOI] [PubMed] [Google Scholar]
- Haines VA, Beggs JJ and Hurlbert JS (2011) Neighborhood disadvantage, network social capital, and depressive symptoms. J Health Soc Behav 52(1), 58–73. [DOI] [PubMed] [Google Scholar]
- Tomita A and Burns JK (2013) A multilevel analysis of association between neighborhood social capital and depression: evidence from the first South African National Income Dynamics Study. J Affect Disord 144(1–2), 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson RN, Putt MA, Dean LT, et al. (2009) Neighborhood racial composition, social capital and black all-cause mortality in Philadelphia. Soc Sci Med 68(10), 1859–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochner KA, Kawachi I, Brennan RT, et al. (2003) Social capital and neighborhood mortality rates in Chicago. Soc Sci Med 56(8), 1797–1805. [DOI] [PubMed] [Google Scholar]
- King D (2008) Neighborhood and individual factors in activity in older adults: results from the neighborhood and senior health study. Journal of Aging and Physical Activity 16(2), 144–170. [DOI] [PubMed] [Google Scholar]
- Mohnen SM, Groenewegen PP, Volker B, et al. (2011) Neighborhood social capital and individual health. Soc Sci Med 72(5), 660–667. [DOI] [PubMed] [Google Scholar]
- Davison KK, Nishi A, Kranz S, et al. (2012) Associations among social capital, parenting for active lifestyles, and youth physical activity in rural families living in upstate New York. Soc Sci Med 75(8), 1488–1496. [DOI] [PubMed] [Google Scholar]
- Sapag JC, Poblete FC, Eicher C, et al. (2010) Tobacco smoking in urban neighborhoods: exploring social capital as a protective factor in Santiago, Chile. Nicotine Tob Res 12(9), 927–936. [DOI] [PubMed] [Google Scholar]
- Pattussi MP, Hardy R and Sheiham A (2006) The potential impact of neighborhood empowerment on dental caries among adolescents. Community Dent Oral Epidemiol 34(5), 344–350. [DOI] [PubMed] [Google Scholar]
- Aida J, Kuriyama S, Ohmori-Matsuda K, et al. (2011) The association between neighborhood social capital and self-reported dentate status in elderly Japanese--the Ohsaki Cohort 2006 Study. Community Dent Oral Epidemiol 39(3), 239–249. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Kim DJ and Kawachi I (2002) Social trust and self-rated health in US communities: a multilevel analysis. J Urban Health 79(4 Suppl 1), S21–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caughy MO, O’Campo PJ and Muntaner C (2003) When being alone might be better: neighborhood poverty, social capital, and child mental health. Soc Sci Med 57(2), 227–237. [DOI] [PubMed] [Google Scholar]
- Ryvicker M, Gallo WT and Fahs MC (2012) Environmental factors associated with primary care access among urban older adults. Soc Sci Med 75(5), 914–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham GO and Michael YL (2004) Concepts guiding the study of the impact of the built environment on physical activity for older adults: a review of the literature. Am J Health Promot 18(6), 435–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank LD, Sallis JF, Saelens BE, et al. (2010) The development of a walkability index: application to the Neighborhood Quality of Life Study. Br J Sports Med 44(13), 924–933. [DOI] [PubMed] [Google Scholar]
- Gebel K, Bauman A and Owen N (2009) Correlates of non-concordance between perceived and objective measures of walkability. Ann Behav Med 37(2), 228–238. [DOI] [PubMed] [Google Scholar]
- McGinn AP, Evenson KR, Herring AH, et al. (2007) Exploring associations between physical activity and perceived and objective measures of the built environment. Journal of Urban Health 84(2), 162–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Y, Beard T, Choi D, et al. (2006) Measuring the influence of built neighborhood environments on walking in older adults. J Aging Phys Act 14(3), 302–312. [DOI] [PubMed] [Google Scholar]
- Weiss RL, Maantay JA and Fahs M (2010) Promoting Active Urban Aging: A Measurement Approach to Neighborhood Walkability for Older Adults. Cities Environ 3(1), 12. [PMC free article] [PubMed] [Google Scholar]
- Auchincloss AH, Diez Roux AV, Brown DG, et al. (2008) Neighborhood resources for physical activity and healthy foods and their association with insulin resistance. Epidemiology 19(1), 146–157. [DOI] [PubMed] [Google Scholar]
- Carlson C, Aytur S, Gardner K, et al. (2012) Complexity in built environment, health, and destination walking: a neighborhood-scale analysis. Journal of Urban Health 89(2), 270–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovasi GS, Hutson MA, Guerra M, et al. (2009) Built environments and obesity in disadvantaged populations. Epidemiologic Reviews 31, 7–20. [DOI] [PubMed] [Google Scholar]
- Rundle A, Diez Roux AV, Free LM, et al. (2007) The urban built environment and obesity in New York City: a multilevel analysis. American Journal of Health Promotion 21(4 Suppl), 326–334. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Saelens BE, Frank LD, et al. (2009) Neighborhood built environment and income: examining multiple health outcomes. Soc Sci Med 68(7), 1285–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troped PJ, Tamura K, Whitcomb HA, et al. (2011) Perceived built environment and physical activity in U.S. women by sprawl and region. Am J Prev Med 41(5), 473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M and Kowaleski-Jones L (2012) The built environment and risk of obesity in the United States: racial-ethnic disparities. Health Place 18(6), 1314–1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M and Maloney TN (2011) Latino residential isolation and the risk of obesity in Utah: the role of neighborhood socioeconomic, built-environmental, and subcultural context. J Immigr Minor Health 13(6), 1134–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries SI, Bakker I, van Mechelen W, et al. (2007) Determinants of activity-friendly neighborhoods for children: results from the SPACE study. Am J Health Promot 21(4 Suppl), 312–316. [DOI] [PubMed] [Google Scholar]
- Fields R, Kaczynski AT, Bopp M, et al. (2013) Built Environment Associations With Health Behaviors Among Hispanics. Journal of Physical Activity and Health. [DOI] [PubMed] [Google Scholar]
- Frank LD, Saelens BE, Powell KE, et al. (2007) Stepping towards causation: do built environments or neighborhood and travel preferences explain physical activity, driving, and obesity? Social Science & Medicine 65(9), 1898–1914. [DOI] [PubMed] [Google Scholar]
- Heinrich KM, Lee RE, Regan GR, et al. (2008) How does the built environment relate to body mass index and obesity prevalence among public housing residents? Am J Health Promot 22(3), 187–194. [DOI] [PubMed] [Google Scholar]
- McAlexander KM, Banda JA, McAlexander JW, et al. (2009) Physical activity resource attributes and obesity in low-income African Americans. J Urban Health 86(5), 696–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M and Kogan MD (2010) Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff (Millwood) 29(3), 503–512. [DOI] [PubMed] [Google Scholar]
- Hoehner CM, Handy SL, Yan Y, et al. (2011) Association between neighborhood walkability, cardiorespiratory fitness and body-mass index. Social Science & Medicine 73(12), 1707–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrigan D, Pickle LW and Dill J (2010) Associations between street connectivity and active transportation. Int J Health Geogr 9, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charreire H, Weber C, Chaix B, et al. (2012) Identifying built environmental patterns using cluster analysis and GIS: relationships with walking, cycling and body mass index in French adults. Int J Behav Nutr Phys Act 9, 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coogan MA, Karash KH, Adler T, et al. (2007) The role of personal values, urban form, and auto availability in the analysis of walking for transportation. Am J Health Promot 21(4 Suppl), 363–370. [DOI] [PubMed] [Google Scholar]
- Freeman L, Neckerman K, Schwartz-Soicher O, et al. (2013) Neighborhood Walkability and Active Travel (Walking and Cycling) in New York City. J Urban Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaczynski AT (2010) Neighborhood walkability perceptions: associations with amount of neighborhood-based physical activity by intensity and purpose. J Phys Act Health 7(1), 3–10. [DOI] [PubMed] [Google Scholar]
- Lovasi GS, Schwartz-Soicher O, Neckerman KM, et al. (2013) Aesthetic amenities and safety hazards associated with walking and bicycling for transportation in new york city. Ann Behav Med 45 Suppl 1, 76–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters M, Brauer M, Setton EM, et al. (2010) Built environment influences on healthy transportation choices: bicycling versus driving. J Urban Health 87(6), 969–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyden KM (2003) Social capital and the built environment: the importance of walkable neighborhoods. Am J Public Health 93(9), 1546–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DA, Inagami S and Finch B (2008) The built environment and collective efficacy. Health Place 14(2), 198–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berke EM, Koepsell TD, Moudon AV, et al. (2007) Association of the built environment with physical activity and obesity in older persons. American Journal of Public Health 97(3), 486–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer PA, Cardinal BJ, et al. (2008) Built environment, adiposity, and physical activity in adults aged 50–75. Am J Prev Med 35(1), 38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagel CL, Carlson NE, Bosworth M, et al. (2008) The relation between neighborhood built environment and walking activity among older adults. Am J Epidemiol 168(4), 461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael YL, Gold R, Perrin NA, et al. (2011) Built environment and lower extremity physical performance: prospective findings from the study of osteoporotic fractures in women. Journal of Aging and Health 23(8), 1246–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SC, Mason CA, Lombard JL, et al. (2009) The relationship of built environment to perceived social support and psychological distress in Hispanic elders: the role of “eyes on the street”. J Gerontol B Psychol Sci Soc Sci 64(2), 234–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SC, Mason CA, Perrino T, et al. (2008) Built environment and physical functioning in Hispanic elders: the role of “eyes on the street”. Environ Health Perspect 116(10), 1300–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortney JC, Lancaster AE, Owen RR, et al. (1998) Geographic market areas for psychiatric and medical outpatient treatment. J Behav Health Serv Res 25(1), 108–116. [DOI] [PubMed] [Google Scholar]
- Gresenz CR, Rogowski J and Escarce JJ (2007) Health care markets, the safety net, and utilization of care among the uninsured. Health Serv Res 42(1 Pt 1), 239–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVela SL, Smith B, Weaver FM, et al. (2004) Geographical proximity and health care utilization in veterans with SCI&D in the USA. Soc Sci Med 59(11), 2387–2399. [DOI] [PubMed] [Google Scholar]
- Mayer ML, Beil HA and von Allmen D (2009) Distance to care and relative supply among pediatric surgical subspecialties. J Pediatr Surg 44(3), 483–495. [DOI] [PubMed] [Google Scholar]
- Haun JN, Valerio MA, McCormack LA, et al. (2015) Health literacy measurement: An inventory and descriptive summary of 51 instruments. Journal of Health Communication: International Perspectives 19(sup2), 302–333. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins School of Public Health and Westat (2015) The National Health & Aging Trends Study. [Google Scholar]
- Centers for Disease Control and Prevention (2016) National Health Interview Survey. [Google Scholar]