Abstract
Introduction
Rising rates of opioid abuse in the United States have generated an overdose epidemic. Particularly in the last few years, many offices across the country have seen a shift from prescription opioid toxicity to heroin, illicitly produced fentanyl, and, more recently, various fentanyl analogs.
Methods
A retrospective review was performed to better characterize the incidence of licit opioid, heroin, fentanyl, and fentanyl analog-associated deaths in South Carolina. Three-thousand three-hundred and fifty autopsy records from the Medical University of South Carolina's forensic pathology division were reviewed to identify cases in which oxycodone, hydrocodone, heroin, fentanyl, and/or fentanyl analogs were detected.
Results
In 2013, the incidence of both heroin and fentanyl-associated deaths was relatively rare (2.2% and 0.4%, respectively), but increased somewhat steadily throughout the ensuing years. The incidence of fentanyl-associated death increased from 0.4% to 2.4% between 2013 and 2016. A decrease in fentanyl-associated deaths was noted between 2015 and 2016; however, 2016 saw a dramatic increase in fentanyl analogs, likely accounting for this slight dip. Heroin rose from 2.2% to 4.5% between 2013 and 2016. Combined, heroin and fentanyl accounted for 2.6% of autopsy deaths in 2013 and increased to 7.6% in 2016, with more substantial increases in 2014 and 2015. Licit opioid-associated deaths remained relatively stable throughout the study period and, when identified, were almost always polydrug comixtures.
Discussion
These data illustrate general increases in illicit opioid-related deaths. In contrast to larger jurisdictions, particularly in the Midwest and Northeast, heroin continues to contribute most significantly to intoxication deaths, although synthetic fentanyl and fentanyl analog-associated deaths increased dramatically beginning in 2014.
Keywords: Forensic pathology, Heroin, Fentanyl, Fentanyl analogs, Opioids
Introduction
Rising drug abuse in the United States has generated an overdose epidemic. Within the national context, the origins of this crisis are thought to be traced to the overprescribing practices of opioid analgesics (e.g., oxycodone, hydrocodone) starting in the late 1990s and into the 2000s. In 2006, 72.4 opioid prescriptions were written per 100 persons in the United States. This rate increased 4.1% annually between 2006 and 2008 and 1.1% between 2008 and 2012. With public awareness, local and regional intervention, and improved prescribing practices, prescriptions for opioids decreased 4.9% annually between 2012 and 2016, leading to an overall 46.8% reduction from 2006 to 2016 (1).
This decrease in prescription practices saw a concurrent rise in opiate and opioid associated deaths (2–4). Unlike heroin, which is grown from poppy seeds dependent on ideal growing seasons and increased labor, fentanyl is highly potent and cheaply synthesized from readily available precursors, leading to its increased popularity as a street drug. Between 2013 and 2014, heroin and fentanyl overdoses nationally increased 26% and 80%, respectively (2), resulting in nationwide alerts from the Drug Enforcement Administration (DEA) and the Centers for Disease Control and Prevention (5, 6).
In 2014 and 2015, South Carolina saw 57.1% and 43.5% increases in fatal toxicity involving heroin and synthetic opioids such as fentanyl, respectively (7). To further characterize these trends in South Carolina, a retrospective review was performed using autopsy data from the Medical University of South Carolina, a practice that serves roughly one-third of the state.
Methods
The Medical University of South Carolina is a large academic medical center in Charleston, South Carolina. The Division of Autopsy and Forensic Pathology performs medical autopsies for deaths occurring internally and also serves as a referral autopsy service for medical autopsies from other healthcare centers and forensic autopsies for roughly one-third of the state. South Carolina is predominantly a coroner-based death investigation system. As such, the Division is not routinely involved in scene investigation or selecting cases for postmortem examination, but performs examinations, including full toxicology the vast majority of the time, on cases referred from the coroners of various surrounding counties and relies on the coroners for the other aspects of death investigation.
Autopsy records between 2013 and 2016 were reviewed to identify cases in which heroin, fentanyl, and/or fentanyl analogs were detected. 2013 was chosen as an initial starting period because an updated electronic medical record keeping system was initiated at that time, making it difficult to extract data from previous years. Because hydrocodone and oxycodone are commonly abused prescription opioids, they were chosen to better characterize and compare licit opioid to illicit opioid-associated deaths. Cases in which hydrocodone, oxycodone, heroin, fentanyl, and/or fentanyl analogs were identified were then queried based on the following: the manner and cause of death; concentration; presence of other drugs; whether natural disease contributed to death; demographic information; and, in cases in which fentanyl was detected, if there was any indication for legitimate medical use. Those cases in which fentanyl was the cause of death rather than incidental to medical therapy were then focused on in order to identify trends associated with abuse.
As there is no crime lab or forensic toxicology testing available in-house, all specimens were sent to one of two nationally certified toxicology laboratories. All heroin deaths had positive 6-monoacetylmorphine (6-MAM) in the blood, vitreous, or urine. In all but two cases, free morphine was present in the blood as well. Fentanyl was routinely screened for during all years of the study at both laboratories. Fentanyl analogs were tested based on the pathologist's suspicion (e.g., unremarkable routine toxicology despite history and scene findings suggestive of recent drug abuse). Additionally, as knowledge of new analogs increased, directed testing was initiated in several cases in which the fentanyl screen was positive but confirmatory testing was negative.
Results
Heroin
A total of 3350 autopsy reports were reviewed. Heroin was identified with a yearly incidence of 2.1% (n=15), 3.0% (n=24), 4.0% (n=36), and 4.5% (n=43) between 2013 and 2016 (Table 1). With rare exception, when heroin was present, it was attributed as a cause of death for a total of 118 deaths. A polydrug mixture involving heroin was identified in 40%, 62.5%, 66.7%, and 70.7% of cases between 2013 and 2016. Natural disease was said to have contributed to death in 6.7%, 4.2%, 25%, and 17% of heroin deaths during those same years, with an average age of 40.8 years. Demographically, the decedents were predominantly white males in their late thirties (Table 2).
Table 1.
Heroin Incidence, Change in Incidence, Proportion of Overall Deaths, and Incidence of Other Drugs Detected Along with Heroin
| Incidence | Change | Overall Cause of Death | Mixture | |
|---|---|---|---|---|
| 2013 (n=15) | 0.022 | — | 0.022 | 0.4 |
| 2014 (n=24) | 0.030 | 0.379 | 0.030 | 0.625 |
| 2015 (n=36) | 0.04 | 0.328 | 0.04 | 0.667 |
| 2016 (n=43) | 0.045 | 0.113 | 0.042 | 0.707 |
Table 2.
Demographics of Individuals Dying From Heroin, Fentanyl, and Fentanyl Analogs From 2013-2016
| Sex | Age (mean years) | Race | |
|---|---|---|---|
| Heroin (n=118) | Male: 0.81 | 38.63 | White: 0.89 |
| Female: 0.19 | Black: 0.11 | ||
| Fentanyl (n=61) | Male: 0.51 | 39.43 | White: 0.93 |
| Female: 0.49 | Black: 0.07 | ||
| Fentanyl Analogs (n=11) | Male: 0.91 | 34.18 | White: 1.0 |
| Female: 0.09 |
Fentanyl
Between 2013 and 2016, fentanyl was identified with a yearly incidence of 1.5%, 3.4%, 3.6%, and 5.1%, respectively, and was attributed as a cause of death in 30%, 48.1%, 75%, and 59.2% of these cases (Table 3). A total of 61 fentanyl-associated deaths were identified during this study period. When refined to cases in which fentanyl was the cause of death rather than secondary to medical therapy (e.g., palliative use in intensive care), the incidence dropped to 0.4% (n=3), 1.4% (n=11), 2.7% (n=24), and 2.3% (n=23). Focusing on these cases, a polydrug mixture was identified in 33.3%, 69.2%, 66.7%, and 82.7% of cases during that timeframe. Heroin was discovered as a polydrug mixture with fentanyl beginning in 2014 through 2016 in 9.1%, 12.5%, and 18.4% of cases, respectively. Additionally, polydrug mixtures involving fentanyl analogs were present in 8.3% and 4.3% of cases in 2015 and 2016. In all deaths where fentanyl was identified, therapeutic fentanyl decreased from 90% to 36.7% between 2013 and 2016. In cases where fentanyl was a cause of death, therapeutic fentanyl decreased from 100% to 26.1% between 2013 and 2016. Natural disease contributed to 7.7%, 8.3%, and 3.4% of all deaths involving fentanyl between 2014 and 2016. In fentanyl-associated deaths, natural disease contributed in 9.1%, 8.3%, and 4.3% of deaths with an average age of 38.2 years. Demographically, decedents were nearly half males and half females in their late 30's and predominantly white (Table 2).
Table 3.
Incidence of Fentanyl-Associated Deaths, Change in Incidence, Proportion of Overall Deaths, Incidence of Other Drugs Detected Along with Fentanyl, and Presence of Therapeutic Fentanyl
| Incidence | Change | Overall Cause of Death | Mixture | Therapeutic Fentanyl | |
|---|---|---|---|---|---|
| 2013 (n=3) | 0.004 | — | 0.004 | 0.333 | 1.0 |
| 2014 (n=11) | 0.014 | 2.161 | 0.016 | 0.818 | 0.363 |
| 2015 (n=24) | 0.027 | 0.932 | 0.027 | 0.667 | 0.333 |
| 2016 (n=23) | 0.023 | -0.107 | 0.030 | 0.828 | 0.261 |
Fentanyl Analogs
Fentanyl analogs were not identified until 2014 (Table 4). Beginning then, the incidence rose from 0.3% (n=2) in 2014 to 0.7% (n=7) in 2016. Two cases in both 2014 and 2015 involved acetylfentanyl. In 2016, seven cases with 11 fentanyl analogs were identified, including acetylfentanyl (n=3), acrylfentanyl (n=2), furanylfentanyl (n=2), 4-ANPP (n=2), carfentanil (n=1), and para-fluorobutryl fentanyl (n=1). Although not technically a fentanyl analog, U-47700 was discovered in a polydrug-associated death and included in the analog classification. Of the 11 deaths involving fentanyl analogs, a polydrug mixture was discovered in 81.8% of cases. Comixtures with fentanyl accounted for 36.4% of cases, while no comixtures were identified involving heroin. In every case, the fentanyl analog was attributed as a cause of death. Of the 11 cases identified, the majority of decedents were white males in their mid-thirties.
Table 4.
Fentanyl Analog Concentrations
| Acetyl (n=7) | Acryl (n=2) | Furanyl (n=2) | 4-ANPP (n=2) | Carfentanil (n=1) | U-47700 (n=1) | PFB† (n=1) | |
|---|---|---|---|---|---|---|---|
| 2013 (n=0) | |||||||
| 2014 (n=2) | 140.0 ng/mL | ||||||
| 14.0 ng/mL | |||||||
| 2015 (n=2) | 150.0 ng/mL | ||||||
| 220.0 ng/mL | |||||||
| 2016 (n=11) | 4.2 ng/mL | 0.3 ng/mL | 5.3 ng/mL* | 0.12 ng/mL‡ | 0.20 ng/mL‡ | 0.22 ng/mL‡ | 1.1 ng/mL‡ |
| 97.1 ng/mL | 0.95 ng/mL | Not Quantified† | 5.5 ng/mL* | ||||
| Not Quantified† |
Mixture in decedent #1
Mixture in decedent #3
Mixture in decedent #2
Para fluorobutryl fentanyl
Hydrocodone/Oxycodone
Between 2013 and 2016, hydrocodone was identified in 4.9% (n=34), 4.8% (n=38), 5.0% (n=45) and 5.0% (n=48) of cases and was a cause of death in a total of 62 cases (Figure 1). The yearly incidence of associated death was 2.3% (n=16), 1.3% (n=10), 1.8% (16), 2.1% (n=20). Oxycodone was identified in 7.7% (n=53), 5.9% (n=47), 6.3% (n=57), and 6.6% (n=64) of cases and was a cause of death in a total of 101 cases. The yearly incidence of associated deaths from 2013-2016 was 4.5% (n=31), 2.8% (n=22), 2.7% (n=24), and 2.5% (n=24). When attributed as a cause of death, hydrocodone and oxycodone were part of polydrug mixtures in 95.2% and 93.1% of cases, respectively. Natural disease contributed to death in 25.8% and 18.8% of hydrocodone and oxycodone cases, respectively.
Figure 1.
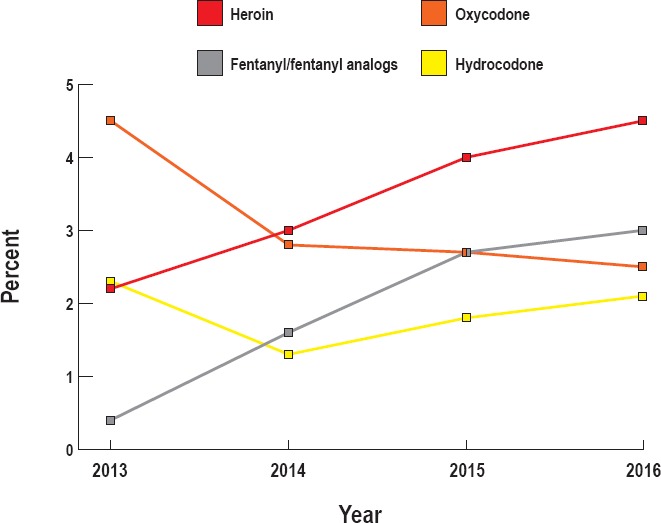
Yearly incidence of associated deaths.
Discussion
Keeping in line with national trends, the incidence of heroin, fentanyl, and fentanyl analog-associated deaths increased between 2013 and 2016, while hydrocodone and oxycodone decreased and then remained relatively stable (Figure 1). Deaths in which fentanyl was attributed as a cause of death rose from 0.4% to 2.3%. Between 2015 and 2016, a drop was noted in fentanyl-associated deaths from 2.7% to 2.3%; however, 2016 saw an increase in seven cases of fentanyl analog associated deaths. When combined, the incidence of fentanyl and fentanyl analog-associated deaths increased to 3.0% in 2016, indicating an upward trend in synthetic opioid-associated mortality. Heroin-associated deaths also saw a significant increase from 2.2% to 4.5% between 2013 and 2016. Natural disease contributing to heroin-associated death increased throughout the study. One might expect a broadened age demographic as heroin increased in popularity throughout the study, and with this increased age demographic attendant comorbidities (e.g., heart disease, chronic obstructive pulmonary disease) not typical in younger age groups. However, there was no correlation between overall age and the increase in natural disease. One possible explanation for this rise is that the ubiquity of heroin-associated deaths propagated a “numbing” effect in which pathologists were more likely to contribute additional factors to cause of death in addition to heroin toxicity. Of the 3350 autopsy cases reviewed, fentanyl and heroin accounted for 2.6% of total deaths in 2013 and increased to 7.2% by 2016. 2014 and 2015 saw the most significant increases in overall cause of death due to both fentanyl and heroin. With rare exception, heroin was attributed as a cause of death when identified on toxicology as opposed to fentanyl, which was attributed as a cause of death in 30-75% of cases. Cases in which fentanyl may have been used in a legitimate, therapeutic fashion steadily decreased from 90% to 37%. When refined to cases in which fentanyl was a cause of death, therapeutic indications decreased from 100% to 26.1%. Hydrocodone and oxycodone-associated deaths decreased in 2013 and then remained relatively stable through 2016. The overwhelming majority of these cases involved polydrug mixtures.
The trends characterized by this study tend to follow national data. Between 1999 and 2015, opioid deaths have quadrupled in the United States from 8050 to 33 091 (1). In a study examining national and regional (Northeast, Midwest, South, West) trends involving unintentional deaths associated with heroin and synthetic opioids between 2006 and 2015, heroin overdose increased significantly beginning in 2010, both regionally and nationally. The Northeast and Midwest were particularly afflicted, experiencing steady yearly increases in heroin drug reports throughout 2006-2015 (8).
Regionally, the Northeast, Midwest, and South have seen significant rises in synthetic opioid deaths not involving heroin between 2013 and 2015 (8). Fentanyl produces euphoric effects indistinguishable from heroin, but with a shorter onset of action and a potency 50-100 times higher than morphine. This, in addition to cheap costs, ease of manufacture, and limited detectability have contributed to its increased popularity as a street drug, often being either laced with or sold as heroin (9, 10). This trend was not reflected in the study, as heroin-associated deaths continued to lead in mortality compared to fentanyl and fentanyl analogs combined. Nonetheless, South Carolina did see a significant rise in the incidence of fentanyl-associated deaths throughout the study. One hypothesis for the increased incidence of heroin toxicity is its local availability. However, given the limitations of the investigation system in South Carolina, it was not possible to acquire drug seizure data from each jurisdiction in order to correlate this upward trend.
The rise in fentanyl-associated deaths both nationally (8) and in South Carolina is likely traced to illicitly manufactured fentanyl (IMF). Beginning in 2013, fentanyl exhibits rose dramatically in the US, with nearly an eight-fold increase in 2015 compared to 2006 (9). A strong correlation exists between this rise in IMF submissions and the increase in synthetic opioid-associated overdoses without significant increases in prescribed fentanyl, suggesting that, although a minority of pharmaceutical fentanyl may be diverted for abuse, the majority of fentanyl causing acute toxicity is illicitly manufactured (11). Many of these seizures are thought to have originated in clandestine labs later trafficked from Mexico (5). The eastern United States is particularly affected by this influx (11). White powder heroin is popular east of the Mississippi River, whereas black tar heroin more popular west of the Mississippi River, which allows for fentanyl to be easily laced in or disguised as heroin to unsuspecting users (4).
In addition to an increase in fentanyl-associated deaths, while limited in number, South Carolina likewise saw a dramatic increase in fentanyl analogs. Although not part of this study, the appearance of fentanyl analogs has anecdotally been trending upward into 2017. Fentanyl analogs pose a unique challenge in the forensic setting, as the structure of fentanyl allows for large variation in synthetic derivatives. The variety of these analogs, in addition to the marginal concentrations required for overdose, complicate postmortem toxicological identification, as novel analogs are not included in standard drug testing and analytical methods for detecting these novel agents are in need of continuous update. This complicates the reporting of fentanyl analogs, as a high index of suspicion is required for directed testing. Similar to fentanyl, fentanyl analogs are often used as an adulterant or substitute for heroin. In the current study, while heroin was not identified as a comixture in cases where fentanyl analogs were present, the clinical history for several of these cases suggested that the decedents were abusing what they thought to be heroin.
Analogs are thought to be sold as precursor chemicals under the guise of “research chemicals” from countries including China, which are then processed and trafficked into the US through Mexico and Canada (10). Novel analogs are continuously emerging. Acetylfentanyl (10, 12), butyrylfentanyl (13, 14), and furanylfentanyl (15) are examples of the more commonly described derivatives in the scientific literature. In the current study, acetylfentanyl was the most commonly encountered analog, however other novel analogs, such as acrylfentanyl, are arising with increased frequency. Recent reports in Ohio have documented the increasing presence of IMFs and fentanyl analogs involved in overdose mortality, supplanting heroin, and pharmaceutical overdose. Beginning in 2017, fentanyl, fentanyl analogs, or a combination of both accounted for 90% of unintentional overdoses. Furanylfentanyl and acrylfentanyl were the most commonly encountered analogs (16).
As mentioned, the analogs detected in this study were identified when directed testing was requested based on a highly suspicious scenario for an overdose (e.g., younger individual, no evidence of trauma or natural disease, high risk lifestyle) yet routine testing was unremarkable, or cases in which a fentanyl screen was reported as positive but could not be confirmed on directed testing for fentanyl. Given this algorithm, there are very likely additional cases in which fentanyl analogs were present but directed testing was not performed due to a lack of suspicion by death investigators or another cause of death was identified. Additionally, due South Carolina's death investigation system, certainly some deaths due to fentanyl analogs, and other drugs, were not examined at our institution if a coroner denied jurisdiction or performed their own external examination and toxicology draw without utilizing our services.
Conclusion
Between 2013 and 2016, illicit opioid-related deaths have steadily increased in South Carolina. Compared to other larger jurisdictions, particularly in the Midwest and Northeast, heroin has contributed the highest burden to overall deaths. Nonetheless, a significant increase in fentanyl-associated deaths emerged beginning in 2014. Although fentanyl-associated deaths decreased between 2015 and 2016, a dramatic increase in fentanyl analogs was noted in 2016. When combined, the incidence of mortality associated with these synthetic opioids continues on an upward trend. Licit opioid-associated deaths decreased in 2013 and then remained relatively stable into 2016. Fentanyl analogs pose a particular threat given their extreme potency and absence from standard drug testing, and, anecdotally, at the conclusion of this study appear to be trending upward into 2017. The data presented may offer insight into one practice's experience with a national epidemic, and, in particular, aid authorities in identifying drugs most frequently causing death in our community.
Footnotes
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
Nicholas I. Batalis is the Associate Editor-in-Chief of Academic Forensic Pathology: The Official Publication of the National Association of Medical Examiners. This work was presented at the 2017 NAME Annual Meeting. The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
FINANCIAL DISCLOSURE The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
References
- 1.Annual surveillance report of drug-related risks and outcomes — United States, 2017 [Internet]. Atlanta: Centers for Drug Control and Prevention; 2017. [cited 2017 Sep 20]. 83 p. Available from: https://www.cdc.gov/drugoverdose/pdf/pubs/2017-cdc-drug-surveillance-report.pdf. [Google Scholar]
- 2.Rudd R.A., Aleshire N., Zibbell J.E., Gladden R.M. Increases in drug and opioid overdose deaths-United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016. Jan 1; 64(50-51): 1378–82. PMID: 26720857. 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- 3.Cicero T.J., Ellis M.S., Harney J. Shifting patterns of prescription opioid and heroin abuse in the United States. N Engl J Med. 2015. Oct 29; 373(18): 1789–90. PMID: 26510045. 10.1056/NEJMc1505541. [DOI] [PubMed] [Google Scholar]
- 4.National heroin threat assessment summary – updated [Internet]. Washington: US Department of Justice, Drug Enforcement Administration; 2016. [cited 2017 Sep 1]. 13 p. Available from: https://www.dea.gov/divisions/hq/2016/hq062716_attach.pdf. [Google Scholar]
- 5.Drug Enforcement Administration [Internet]. Washington: US Department of Justice, Drug Enforcement Administration; c2017. DEA issues nationwide alert on fentanyl as threat to health and public safety; 2015 Mar 18 [cited 2017. Aug 5]. Available from: http://www.dea.gov/divisions/hq/2015/hq031815.shtml. [Google Scholar]
- 6.Centers for Disease Control and Prevention [Internet]. Atlanta: Centers for Disease Control and Prevention; c2017. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities; 2015 Oct 26 [cited 2017. Aug 5]. Available from: http://emergency.cdc.gov/han/han00384.asp. [Google Scholar]
- 7.CDC WONDER [Internet]. Atlanta: Centers for Disease Control and Prevention; 2017. [cited 2017 Sep 9]. Available from: https://wonder.cdc.gov/. [Google Scholar]
- 8.O'Donnell J.K., Gladden R.M., Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region - United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017. Sep 1; 66(34): 897–903. PMID: 28859052. 10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Counterfeit prescription pills containing fentanyl: a global threat. Washington: US Department of Justice, Drug Enforcement Administration; 2016. [cited 2017 Aug 5]. 10 p. Available from: https://content.govdelivery.com/attachments/USDOJDEA/2016/07/22/file_attachments/590360/fentanyl%2Bpills%2Breport.pdf. [Google Scholar]
- 10.2015 National drug threat assessment summary. Washington: US Department of Justice, Drug Enforcement Administration; 2015. [cited 2017 Aug 5]. 135 p. Available from: https://www.dea.gov/docs/2015%20NDTA%20Report.pdf. [Google Scholar]
- 11.Gladden R.M., Martinez P., Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths - 27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016. Aug 26; 65(33): 837–43. PMID: 27560775. 10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham S.M., Haikal N.A., Kraner J.C. Fatal intoxication with acetyl fentanyl. J Forensic Sci. 2016. Jan; 61 Suppl 1: S276–80. PMID: 26389815. 10.1111/1556-4029.12953. [DOI] [PubMed] [Google Scholar]
- 13.McIntyre I.M., Trochta A., Gary R.D. et al. An acute butyr-fentanyl fatality: a case report with postmortem concentrations. J Anal Toxicol. 2016. Mar; 40(2): 162–6. PMID: 26683128. 10.1093/jat/bkv138. [DOI] [PubMed] [Google Scholar]
- 14.Poklis J., Poklis A., Wolf C. et al. Two fatal intoxications involving butyryl fentanyl. J Anal Toxicol. 2016. Oct; 40(8): 703–8. PMID: 27339481. PMCID: PMC5048708. 10.1093/jat/bkw048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohr A.L., Friscia M., Papsun D. et al. Analysis of novel synthetic opioids U-47700, U-50488 and furanyl fentanyl by LC-MS/MS in postmortem casework. J Anal Toxicol. 2016. Nov; 40(9): 709–17. PMID: 27590036. 10.1093/jat/bkw086. [DOI] [PubMed] [Google Scholar]
- 16.Daniulaityte R., Juhascik M.P., Strayer K.E. et al. Overdose deaths related to fentanyl and its analogs - Ohio, January-February 2017. MMWR Morb Mortal Wkly Rep. 2017. Sep 1; 66(34): 904–8. PMID: 28859050. 10.15585/mmwr.mm6634a3. [DOI] [PMC free article] [PubMed] [Google Scholar]


