Abstract
Sudden unexpected death of an individual with epilepsy (SUDEP) can pose a challenge to death investigators, as most deaths are unwitnessed and the individual is commonly found dead in bed. Anatomic findings (e.g., tongue/lip bite) are commonly absent and of varying specificity, limiting the evidence to implicate epilepsy as a cause of or contributor to death. Thus, it is likely that death certificates significantly underrepresent the true number of deaths in which epilepsy was a factor. To address this, members of the National Association of Medical Examiners, North American SUDEP Registry, Epilepsy Foundation SUDEP Institute, American Epilepsy Society, and the Centers for Disease Control and Prevention convened an expert panel to generate evidence-based recommendations for the practice of death investigation and autopsy, toxicological analysis, interpretation of autopsy and toxicology findings, and death certification to improve the precision of death certificate data available for public health surveillance of epilepsy-related deaths. The recommendations provided in this paper are intended to assist medical examiners, coroners, and death investigators when a sudden, unexpected death in a person with epilepsy is encountered.
Keywords: Forensic pathology, Epilepsy, Sudden unexpected death in epilepsy, SUDEP
Introduction
The investigation and certification of deaths in patients with seizures and epilepsy varies within and between medical examiners' and coroners' offices (1, 2). This variation, together with varied terms and criteria to diagnose and classify seizures and epilepsies and possible comorbid disease (e.g., cardiovascular) challenges the determination of cause of death (COD) in seizure- and epilepsy-related death, and likely underestimates the frequency of these deaths.
To help address these limitations, the National Association of Medical Examiners, North American SUDEP Registry, Epilepsy Foundation SUDEP Institute, American Epilepsy Society, and the Centers for Disease Control and Prevention (CDC) formed an expert panel (pathologists/medical examiners [7], epileptologists [6], epidemiologists [3], cardiologist [1], and a health sciences librarian [1]) to establish recommendations for death investigation and certification of epilepsy-related deaths. The peer-reviewed literature was examined for deaths among individuals with seizures and epilepsy. The goal was to better inform public health burden of seizures and epilepsy-related death and improve surveillance by developing evidence-based recommendations for the practice and interpretation of death investigation, autopsy, toxicological analysis, and death certification. The panel formulated seven questions to address best practices for effective identification of seizure- and epilepsy-related death (Table 1). These questions were arranged in the order that typically arises during death investigation. The recommendations were reviewed by each society for comments and eventual endorsement. Respective organizations at the CDC also provided review and comment.
Table 1.
Questions Formulated by the Panel to Address Seizure- and Epilepsy-Related Deaths
| Number | Question |
|---|---|
| 1 | Within the bounds of state law, which deaths require assumption of jurisdiction and performance of an autopsy? |
| 2 | What constitutes appropriate and necessary scene investigation, epilepsy screening, and follow-up? |
| 3 | When is it appropriate or necessary to perform toxicology and/or antiepileptic seizure medication testing? |
| 4 | What are the best samples to collect for laboratory testing and histologic analysis? |
| 5 | How are scene findings, autopsy findings, toxicology, and histology interpreted? |
| 6 | How are competing causes of sudden death assessed? |
| 7 | What are the optimal methods for determining and certifying cause of death, manner of death, and how injury occurred? |
Background
A seizure is a sudden behavioral change resulting from excessive synchronous electrical activity in the brain. Seizures may be provoked (also known as acute symptomatic; e.g., fever in a young child, drug intoxication or withdrawal, electrolyte imbalance) or unprovoked, resulting from a genetic, developmental, acquired (e.g., trauma, tumor, stroke), or unknown cause. Epilepsy is diagnosed when a person has two or more unprovoked seizures or has a single unprovoked seizure with an enduring tendency for additional seizures (3). “Seizure disorders” are aggregated with “seizures” in the National Vital Statistics System. However, seizure disorder can refer to individuals without epilepsy (e.g., two provoked seizures). Because of these potential confounds, we recommend the term epilepsy over seizure disorder when clinically defined.
Epilepsy affects 3.4 million Americans (4). Individuals with epilepsy have up to 11-fold higher mortality rates compared to matched controls (2). Natural causes of death are 15-fold increased. Nonnatural causes are also increased (falls, 8-fold; drowning, 7.7-fold; drug poisoning, 5.1-fold; suicide, 3.5– to 5-fold) (5). Psychiatric disorders occur in 75% of those with nonnatural causes. Among young adults in the United States with epilepsy and low socioeconomic status, deaths occur 17 years prematurely (6).
The incidence of sudden death among young adults with epilepsy is 24– to 27-fold higher than control populations (7, 8). Sudden unexpected death in epilepsy (SUDEP) is a sudden, unexpected, witnessed or unwitnessed, nontraumatic and nondrowning death, occurring in benign circumstances, in an individual with epilepsy, with or without evidence for a seizure and excluding documented status epilepticus, in which postmortem examination does not reveal a cause of death (Definite SUDEP), without postmortem examination but without other potential cause of death (Probable SUDEP), or with a competing cause of death (Possible SUDEP). The strongest risk factor for SUDEP is poor control of primary or secondary generalized tonic-clonic seizures (GTCS) (9). Structural brain lesions, focal abnormalities on neurological examination, intellectual disability, alcohol abuse, and anxiolytic use are associated with increased SUDEP risk in some studies (9, 10).
A potential confound in SUDEP is sudden cardiac death (SCD). Among “SCD” in epilepsy patients, 70% are unwitnessed; 34% of witnessed cases had seizure activity before “SCD” (11). Since 90% of SUDEPs are unwitnessed, a majority of epilepsy cases classified as “SCD” may have died from epilepsy. Misclassification of an epilepsy-related death as SCD is supported by higher rates of bradyarrhythmias and asystole (typical of epilepsy) and lower rates of ventricular arrhythmias in epilepsy patients with “SCD” than non-epilepsy patients. Also, moderate coronary artery disease can suggest a primary cardiac cause of death in a person with epilepsy (PWE) but cannot exclude an epilepsy-related death.
Methods
We conducted electronic literature searches using the databases Medline (Ovid), Medline In-Process & other Nonindexed Citations (Ovid), Embase (Ovid), and PubMed.gov for articles published in English from 1970 to January 2016. Databases were searched using both subject headings and text keywords that describe epilepsy-related mortality and death investigation (the complete search strategy is in Appendix 1). Academic Forensic Pathology was also searched with keywords related to epilepsy and seizure.
Pairs of authors reviewed all the references yielded from the literature search using a two-step process. First, the authors reviewed the titles and abstracts of the articles yielded from the search and excluded all irrelevant articles. The full-text of the remaining articles was then reviewed for potential inclusion based on relevance to at least one of the questions and the evidence quality.
Results/Discussion
Question 1: Within the bounds of state law, which deaths in people with epilepsy require assumption of jurisdiction and performance of an autopsy?
Medical examiners and coroners (ME/C) have the expertise and responsibility to determine the cause and manner of death in cases of sudden, unexpected deaths. These circumstances are commonly encountered in the deaths of epilepsy patients, leading to ME/C involvement in most of these death certifications (12). Medical examiners' and coroners' authority to assume jurisdiction or responsibility for these determinations is typically mandated by their respective state statutes. Beyond statute, the ME/C exercises their professional judgement on jurisdiction, taking into account the circumstances of the death and resources available in their jurisdiction.
The process of assuming jurisdiction begins when a death is reported to the local ME/C, which requires awareness by reporting agencies and medical personnel of established criteria of reportable deaths. This initial connection is critical to identify epilepsy-related deaths; ME/C staff must consider the potential role of epilepsy in such instances. Once jurisdiction is assumed, an investigation ensues to acquire the information necessary for cause and manner of death determinations, which in turn, are documented in the death certificate. In a retrospective study of SUDEP death certification in Britain, inconsistencies were identified in the depth of investigations. Causes of deaths varied, “with epilepsy stated as the primary cause of death in less than half the sample” (13).
Autopsy may provide otherwise unavailable information necessary for death certification. The importance of a complete autopsy is highlighted by a multidisciplinary team study of 335 consecutive presumed sudden cardiac deaths over a two-year period. This study, which included complete autopsy and investigative data, concluded that 18 cases (5.4%) were actually neurologic deaths, including six due to SUDEP (14). A national survey was done to assess the depth and frequency of forensic autopsies in SUDEP. Generally, the autopsies were done in a consistent manner but they identified a trend of nonurban offices performing fewer autopsies (15). If the circumstances surrounding a seizure death clearly indicate a natural event, jurisdiction may be declined by the ME/C, and an autopsy is not performed unless the family consents to a hospital autopsy or private autopsy. However, since this population tends to be younger and their deaths are frequently unwitnessed, autopsy is often required due to absence of an obvious natural cause.
Epilepsy death investigation is strongly dependent on history and scene findings, yet an autopsy is essential in excluding other causes of death, documenting comorbidities, obtaining toxicologic and histology samples, and providing neuropathologic correlation.
Question 2: What constitutes appropriate and necessary scene investigation, epilepsy screening, and follow-up?
The panel supports the practices recommended in the United States Department of Justice (USDOJ) National Institute of Justice (NIJ) Death Investigation Guidelines published by the USDOJ (16). When death occurs outside the hospital, the environment and position of the body should be detailed to help objectively interpret the circumstances. For example, understanding whether a PWE was found submerged in a bathtub full of water or prone on a bed with the external airways occluded by bedding material is crucial for eventual death certification. Knowing whether a death was witnessed or unwitnessed is also important. If witnessed, investigators should ask if the decedent had a seizure before becoming unresponsive and attempt to describe the initial behavioral changes or seizure movements. Documentation should include observations supportive of a tonic-clonic seizure event, such as disheveled bedding; biting of the tongue, lip, or cheek; or saliva/foam around mouth. Medications and medication containers at the scene should be inventoried, especially antiepileptic drugs (AEDs).
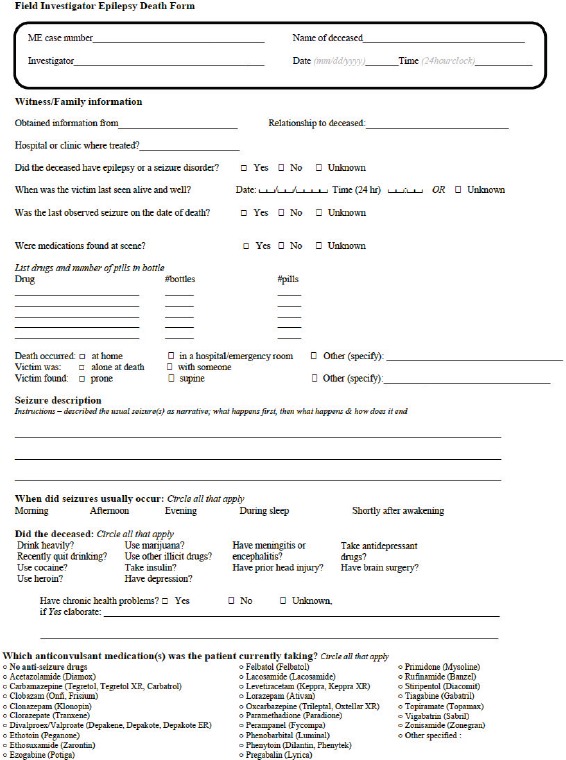
Investigators should ask family or other witnesses at the scene about the decedent's medical history, striving for as specific of an epilepsy diagnosis as possible. At a minimum, the investigator should try to determine whether a decedent suffered from convulsive or nonconvulsive seizures because this history may only be obtained with specific questions and convulsive seizures significantly increase the risk of SUDEP (an example of questions to assist death investigators in gathering such information is provided in Appendix 2). Primary care providers and neurologists should be contacted in follow-up when known. If emergency medical personnel responded to the scene, those records should be reviewed and a copy of available electrocardiograph tracings/interpretations should be sought.
Question 3: When is it appropriate or necessary to perform toxicology and/or antiepileptic seizure medication testing?
In the absence of a specific anatomic cause of death following autopsy, toxicology testing, including antiepileptic drug concentrations, should be performed when specimens are available. Results may reveal drug toxicity from illicit or prescribed substances as a potential cause of death. Documentation of postmortem antiepileptic drug concentrations can aid the investigation when death is potentially epilepsy-related. If the decedent was admitted to an emergency department or hospital before death, postmortem testing should be performed on the earliest blood specimen.
Question 4: What are the best samples to collect for laboratory testing and histologic analysis?
Blood, tissue, and other fluid samples should be retained as per the jurisdiction's usual protocol for routine toxicology testing. Special consideration should be given for potential genetic studies, given the more than 100 genetic disorders associated with epilepsy, with new genes identified each year. Genetic channelopathies, most often sodium and potassium channel gene mutations, may contribute to SUDEP since these genes are expressed in the brain and heart and may lower seizure threshold and cause cardiac arrhythmias (17, 18). Given the possible implications for surviving relatives, collection of proper samples is essential. An EDTA (purple top) tube of blood is the preferred specimen for genetic testing, but a blood spot card or frozen tissue (1 cubic centimeter of liver, spleen, or heart at −80°C) can also be used (19).
Extended brain examination is recommended in potential epilepsy-related death cases, following brain fixation in formalin solution for a minimum of two weeks. Although examination by a neuropathologist is preferred, limitation of resources, objection to organ retention, or other factors will necessitate the autopsy pathologist's discretion for such consultation. Previously published recommendations for microscopic analysis of the brain are outlined in Table 2. Patients with epilepsy may have cardiac pathology resulting from seizures as well as comorbid disorders (e.g., hypertension, hyperlipidemia), with findings of irreversible changes characterized by myocyte hypertrophy and perivascular and interstitial fibrosis, and reversible change characterized by subendocardial myocyte vacuolization (20). Others have recommended inclusion of three left ventricle and one right ventricle heart sections, lung, and any grossly abnormal organs for histologic examination, but individual practice varies (21).
Table 2.
Recommended Sections for Microscopic Analysis of the Brain (22)
| Hippocampus (right and left) |
| Amygdala (right and left) |
| Watershed (frontal and parieto-occipital parasagittal regions) |
| Basal ganglia |
| Midbrain |
| Pons |
| Medulla (at area postrema) |
| Hypothalamus |
Question 5: How are Scene Findings, Autopsy Findings, Toxicology, and Histology Interpreted?
In epilepsy-related deaths, the purposes of the scene investigation, autopsy, and ancillary tests are to 1) determine that epilepsy has/has not caused or contributed to the death, 2) identify the underlying etiology of epilepsy, if present, and 3) assess comorbidities. Autopsy and ancillary test findings must be interpreted in the context of a thorough death investigation to accurately determine the cause and manner of death. The utility and limitations of several anatomic findings frequently encountered in epilepsy-related deaths are discussed.
Livor Pattern/Body Position
The distribution of livor mortis may help in the context of positional asphyxia or smothering by revealing pressure marks from objects against the chest, neck, nose, or mouth that may have restricted breathing. The extent to which such external factors contribute to death vary from case to case. Prone position is associated with SUDEP (23). The significance of finding the decedent's face (nose/mouth) against a surface (often bedding) must be interpreted in the totality of autopsy and scene findings. Such a position is potentially threatening when the brain's reflexive response to the environmental challenge is impaired, for example during intoxication or during/after seizure. Without the seizure or postictal state, the environmental challenge would have been nonlethal. In some cases, livor pattern and scene reconstruction reveal evidence of an asphyxial component by compression of the chest or neck, with or without petechiae. While historically considered an indicator of asphyxia and found in some SUDEPs (24, 25), petechiae occur in deaths resulting from diverse mechanisms and causes and, therefore, do not establish terminal asphyxia without corroborating findings and circumstances.
Tongue, Lip, or Inner Cheek Trauma
Contusion or laceration of the tongue, lip, or inner cheek supports, but is not diagnostic of a seizure. Tongue trauma occurs in 17–50% of seizure-related deaths (24, 26, 27). Tongue trauma in other causes of death is uncommon; one study found tongue/lip contusions in 37% of SUDEP cases but no controls (25). It is worth removing the tongue for examination. Trauma to the sides of the tongue or involving the buccal mucosa may be more helpful, since small contusions of the tongue tip may occur during intubation/attempted intubation.
Incontinence of Urine
While a helpful sign in evaluating living patients with epilepsy, it is so ubiquitous at death scenes that it cannot establish a terminal seizure.
Gastric Contents in Airway
Gastric contents are frequently found in the airways at autopsy, having been displaced there during compressions of the chest for resuscitation, during manipulation of the body after death, or by increased abdominal pressure during decomposition. The presence of gastric contents in the trachea and proximal bronchi should not be interpreted as mechanistically significant to the cause of death or as evidence of seizure activity and therefore does not exclude SUDEP (28). Abundant gastric contents in distal airways is more concerning for true aspiration if there was no mechanical ventilation or chest compressions. Occlusion of the upper airway by food is a significant finding and a choking event must be considered; such a death is not SUDEP but is epilepsy-related if the individual was eating when a seizure occurred (28).
Pulmonary Edema
Pulmonary edema is a nonspecific finding, commonly found at autopsy in deaths of various neurogenic or cardiogenic causes, including SUDEP. In animal models, neurogenic pulmonary edema in seizure deaths may result from a sympathetic surge with increased hydrostatic pressure in the left atrium, pulmonary artery, and pulmonary microvasculature, leading to a capillary-alveolar membrane with increased permeability (29). Autopsy series of SUDEP show pulmonary edema and congestion occur in 62% to 100% of cases (20, 27, 30–32), but fail to demonstrate a statistically significant increase between SUDEP and controls (25, 33). The absence of pulmonary edema does not exclude an epilepsy-related death.
Bronchopneumonia
Aspiration during seizure may lead to bronchopneumonia and result in a delayed, epilepsy-related death. Bronchopneumonia as a mechanism of death is 2.7- to 10.3-fold more common among people with epilepsy (2). Since delayed deaths would not be classified as SUDEP, it is useful to include the mechanism (bronchopneumonia) as well as the cause (epilepsy) on the death certificate for correct coding.
Neuropathologic Findings
Neuropathologic examination can exclude competing causes of death, identify potentially epileptogenic lesions, and determine whether repeated seizures have caused brain injury (e.g., hippocampal sclerosis, cerebellar atrophy). The brain should be examined after formalin fixation in seizure-related deaths when possible. Many lesions are easily identified (e.g., trauma, tumors, vascular malformations, abscesses, cysts), but some are difficult to identify and microscopic findings can be subtle. Ideally, the brain should be examined by a neuropathologist. In one series, abnormalities were found in 66% of formalin-fixed brains by formal neuropathologic examination versus 8.8% of brains examined in the fresh state (34). Histologic examination should be performed even when no macroscopic pathology is identified. However, absence of neuronal injury or identifiable pathology is consistent with the clinical diagnosis of epilepsy.
A common misconception is that the brain is normal anatomically in most SUDEP cases. Neuropathologic abnormalities in autopsy series of SUDEP and epilepsy-related deaths occur in 46% to 71% (26, 30, 35). The SUDEP criterion that no anatomic cause of death be identified refers to competing (nonepilepsy-related) causes, not to the lack of an anatomic etiology for the epilepsy. Persons with epilepsy of any etiology may die suddenly and unexpectedly.
Seizure and epilepsy can result from diverse brain pathologies such as trauma, tumor, vascular malformation, cerebral infarct, abscess, parasitic cysts, Rasmussen encephalitis, other chronic encephalitis, and malformations of cortical development. Mesial temporal sclerosis refers to chronic changes in the hippocampus (hippocampal sclerosis), amygdala, and entorhinal cortex that are closely associated with temporal lobe epilepsy. Mesial temporal sclerosis/hippocampal sclerosis may be a complication or cause of epilepsy and does not need to be on the death certificate. The diverse neuropathologic findings in epilepsy patients have been reviewed (36–38) and are beyond the scope of this paper. When a neuropathologic lesion or disease is a probable cause of epilepsy, it should be listed as the underlying etiology. Traumatic brain injury may be either an etiology for epilepsy, a consequence of epilepsy, or both, and one must seek historical data to determine whether the traumatic lesions predate the onset of epilepsy (e.g., posttraumatic epilepsy) or whether the brain injury occurred during a seizure of unknown or other cause. Since late sequelae of traumatic brain injury are a common etiology for epilepsy, not all SUDEP cases will have a natural manner of death.
Alcohol and Drugs of Abuse
The cooccurrence of epilepsy, acute symptomatic seizures, and substance abuse is common, with at least one third of seizure-related deaths having a history of alcohol and/or street drug use (26, 27). Among 83 deaths in persons with epilepsy/seizure history and no macroscopically obvious cause of death at autopsy, 21% of deaths were attributed to alcohol and or drugs (39). Death due to acute intoxication or withdrawal precludes classification as SUDEP, but should not prohibit inclusion of epilepsy as a contributor to death. Patients whose seizures occur exclusively in association with alcohol intoxication or withdrawal (provoked or acute symptomatic seizure) do not meet diagnostic criteria for epilepsy. However, alcohol use is a seizure trigger in people with epilepsy. Such seizures typically occur within 48 hours after peak blood concentrations, when the brain rebounds into a hyperexcitable state. Therefore, alcohol intoxication/withdrawal may contribute to the sudden death of a PWE, similar to other provocative factors such as missed medication or sleep deprivation. Complicating the dichotomy of epilepsy versus acute symptomatic seizures, alcohol abuse is an independent risk factor for epilepsy and may result from traumatic brain injury during intoxication, neurotoxic effects of alcohol, or kindling of epilepsy following repetitive bouts of alcohol withdrawal (40). Therefore, determining whether recurrent seizures in individuals with alcohol abuse are due to alcohol withdrawal or spontaneous, unprovoked seizures (epilepsy) can be very difficult. One study of first seizures in individuals with alcohol abuse found no consistent temporal relationship of seizure to last drink (41), suggesting that alcohol use and terminal seizure may be incidental in some decedents.
Cocaine (42) or methamphetamine intoxication (43) can trigger seizure activity in persons with or without epilepsy and is certified as an accidental drug death. However, if a person with documented epilepsy dies several hours after cocaine use and cocaine concentrations are low, then epilepsy may be a contributory cause of death. Many patients with epilepsy use cannabinoid oils and marijuana. The relevance of these substances to sudden death is unknown. However, synthetic cannabinoids (e.g., spice, K2, bath salts) are proconvulsant and intoxication can cause seizures in individuals without epilepsy (44). Other drugs of abuse can provoke seizures, such as 3,4-methylene-dioxymethamphetamine (MDMA, ecstasy, “Molly”), phencyclidine (PCP), and some opiates, typically in severe intoxication (45).
Antiepileptic Drugs
Antiepileptic drugs at effective doses may be associated with a reduced incidence of SUDEP (46). Subtherapeutic or absent AED concentrations are found in 57–92% of SUDEP cases (27, 30, 35, 47–49). However, finding subtherapeutic AED concentrations at autopsy has limited value in determining the cause of death due to uncertainties in the correlation of postmortem whole blood concentrations to antemortem serum concentrations and the definition of a therapeutic concentration. Postmortem AED concentrations may not be comparable to antemortem concentrations. Among 16 institutionalized adults with epilepsy, paired antemortem and postmortem serum samples revealed that phenobarbital, phenytoin, and carbamazepine were significantly lower in postmortem samples than antemortem (50). An animal study found that phenytoin concentrations were higher antemortem, whereas carbamazepine concentrations were similar in antemortem and postmortem samples (51). Postmortem alterations, rather than patient noncompliance, may explain the high incidence of subtherapeutic AED concentrations in SUDEP. Supporting this, there were no significant differences between postmortem AED concentrations between 44 SUDEP cases and 44 persons with epilepsy who died from nonepilepsy-related causes (52). The definition of a “therapeutic” range is limited since individual patients require different concentrations for efficacy. Antiepileptic drug concentrations are informative postmortem when below detectable limits or in the lethal range.
Some AEDs can prolong the QT interval, but do not increase risk of arrhythmia for most patients (53). When additional risk factors for arrhythmia are present, such as underlying cardiac dysfunction, electrolyte imbalance (e.g., hypokalemia or hypomagnesemia), or concurrent use of other medications which prolong QT interval, an additive effect from the AED may be considered, but is not definitive. Fatal adverse drug reactions to AEDs (e.g., hepatic failure, bone marrow suppression, Stevens-Johnson syndrome, disseminated intravascular coagulation, and pancreatitis) should be considered, but such deaths would not be classified as SUDEP. In the setting of very high, toxic concentrations of AEDs, suicide may be a consideration.
Questions 6: How are competing causes of sudden death assessed?
A PWE may have a medical history, or at postmortem examination may have natural disease findings, which can explain the sudden death. The most common is atherosclerotic cardiovascular disease (54); others include cardiomegaly (33) and myocarditis (55). Epilepsy is associated with such findings in some studies (20, 56, 57) and seizures can affect the cardiovascular system (58, 59). Cardiac arrhythmia may be an undetectable cause of some SUDEPs (60). Although cardiovascular disease is the most frequent competing cause of death, the following recommendations apply to other findings associated with sudden death such as liver or pulmonary disease.
Coronary Artery Disease
Coronary atherosclerosis is highly prevalent in the developed world and is a common postmortem finding which may or may not contribute to or cause sudden death in a PWE. In up to half of cases, sudden death is the initial manifestation of coronary artery disease (61). Characteristics of the plaque and vessel, degree of luminal stenosis, and location (62, 63) should be considered when weighing coronary disease as a competing cause of sudden death. These frequent pathological findings in a PWE may represent concurrent cardiac disease that is incidental to or explains the sudden death. Close examination of gross and microscopic findings, rather than just an estimate of the percent of coronary stenosis, may facilitate deciphering these two competing causes of death. In a PWE, finding severe coronary stenosis, coronary thrombus, cardiomegaly, large ventricular chambers, and/or acute myocardial infarction or ischemia in territories served by stenotic coronary arteries may support cardiac disease rather than epilepsy as the cause of sudden death.
In a PWE with terminal seizure and postmortem acute coronary findings, the elevated stress and sympathetic response to the seizure may have triggered the acute coronary event. Seizures can also cause fatal arrhythmias (14, 60) or pulmonary dysfunction (64–66). Thus, even when a PWE has acute cardiac findings it is possible that a seizure triggered the cardiac ischemic event or arrhythmia, especially in the setting of preexisting cardiac disease, or vice versa. This scenario should be considered when there is evidence of seizure (e.g., witnessed or tongue bite) and acute cardiac changes.
Structural Cardiomyopathies and Primary Electrical Causes of Sudden Cardiac Death
Other cardiac causes of sudden death include structural cardiac diseases such as hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy, and valvular disease (e.g., critical aortic stenosis); these causes are apparent on postmortem examination in a PWE. Non-structural or “autopsy negative” molecular cardiac (primary electrical) diseases affecting cardiac channels and causing sudden arrhythmic death (e.g., congenital long QT or Brugada syndromes, catecholaminergic polymorphic ventricular tachycardia [CPVT]) are uncommon but potential causes of sudden death in a PWE. As with the general population, a cardiac etiology for sudden death cannot be entirely excluded with postmortem findings of a normal heart in a PWE.
Cardiac Syncope Mimicking Seizure
Epilepsy is not the only cause for seizures. Some patients initially diagnosed with epilepsy are later found to have seizures due to a cardiovascular cause such as an arrhythmia (67, 68). Rhythmic movements mistaken for generalized seizure can result from cerebral hypoperfusion during cardiac events such as ventricular tachycardia (VT), ventricular fibrillation (VF), idioventricular rhythms, or pulseless electrical activity (68). Detailed description of the duration (cardiac syncopal movements often less than 20 seconds; ton ic-clonic seizures often greater than 45 seconds) and type of movements witnessed (classic tonic phase [5–10 seconds] followed by clonic movements that progressively become less frequent over 30–180 seconds suggest a tonic-clonic seizure) may help determine seizure versus cardiac cause, but witness reports can be unreliable.
Supportive Data: Medical History, Circumstances, and Cardiac Rhythms
Data such as medical history, family history, witness account of terminal seizure event, and paramedic run-sheets with description of the fatal event and presenting rhythm, can help distinguish between epilepsy and a cardiac cause. A history of symptomatic cardiac disease or uncontrolled seizures while on multiple AEDs may support one diagnosis over another. Structural cardiomyopathies, such as HCM, and many primary electrical diseases have genetic causes, often with autosomal dominant inheritance patterns. Therefore, a family history of sudden cardiac death, particularly under age 45 years, or sudden infant deaths suggest the possibility of a genetic cause of sudden death in a PWE.
Circumstances and details surrounding the fatal seizure event can also be very helpful. Sudden deaths due to cardiac primary electrical diseases (e.g., LQT1, CPVT) occur during or just following peak exercise. Therefore, a report of seizure activity following collapse after vigorous exercise would favor a cardiac cause, while seizure activity at rest or in bed would favor epilepsy.
A rhythm recorded by paramedics during attempted resuscitation can also be helpful. The most common rhythms found during SUDEP are bradyarrhythmias (69), while VT or VF are commonly found in sudden cardiac deaths. Although VF is often considered the sine qua non of cardiac/arrhythmic death, acute neurologic events can also cause neurocardiogenic VF (70); therefore, VF at the time of fatal event does not exclude a neurologic cause.
7. What are the optimal methods for determining and certifying cause of death, manner of death, and how injury occurred?
Death certificates are useful for families of the deceased, public health agencies, and researchers. Sections of the certificate relevant to this discussion include: Cause of Death (Part I), Other Significant Conditions Contributing to Death (Part II), Manner of Death, and, for unnatural deaths, the section labeled “Describe How Injury Occurred.” Recommendations for certifying deaths for several common vignettes in which epilepsy or a seizure-related event is thought to have contributed are provided in Table 3.
Table 3.
Questions Formulated by the Panel to Address Seizure- and Epilepsy-Related Deaths
| History | Cause of Death (Part I) | Other Significant Conditions (Part II) | How Injury Occurred | Manner |
|---|---|---|---|---|
| Decedent with epilepsy found dead in bed; no other cause of death discovered | Sudden death due to epilepsy | N/A | N | |
| Decedent with epilepsy found dead in bed; competing cause of death such as severe coronary artery disease discovered | Atherosclerotic coronary artery disease | Epilepsy | N/A | N |
| Decedent with epilepsy found dead in bed; contributing factor such as moderate coronary artery disease discovered | Sudden death due to epilepsy | Atherosclerotic coronary artery disease | N/A | N |
| Decedent with epilepsy found dead in bed; ethanol concentration reported as 0.41 g/dL | Acute ethanol intoxication | Epilepsy | Decedent with epilepsy ingested an excess of ethanol | A |
| Decedent with epilepsy due to blunt head trauma occurring from an accidental fall 10 years prior | Epilepsy due to blunt head trauma due to fall | Decedent with epilepsy found dead; suffered head injury in fall 10 years prior | A | |
| Decedent with epilepsy due to blunt head trauma occurring from an assault 10 years prior | Epilepsy due to blunt head trauma due to assault | Decedent with epilepsy found dead; suffered head injury in assault 10 years prior | H | |
| Decedent with epilepsy found dead, submerged in bathtub; no other cause of death discovered | Drowning | Epilepsy | Decedent with epilepsy found submerged in bathtub | A |
| Driver with epilepsy had witnessed seizure in motor vehicle accident; examination revealed no competing cause of death | Sudden death due to epilepsy | N/A | N |
N - Natural;
A - Accident;
H - Homicide;
N/A - Not applicable
Cause of Death
In sudden deaths among people with epilepsy for which no other cause of death is found, the sudden nature of death and its relationship to epilepsy should be emphasized on the death certificate. In such circumstances, there is no correct terminology that satisfies all. We suggest the following can be used inter-changeably as the cause of death: “sudden death due to epilepsy,” “epilepsy,” or “sudden unexpected death in epilepsy.” When an individual with seizures that are not due to epilepsy dies under similar circumstances, listing “seizure disorder” as the cause of death is recommended. Acknowledging that clinical inconsistencies exist in use of the terms epilepsy and seizure disorder, and that forensic case history terminology is variable, the medical examiner might substitute “seizure disorder” when a clinical diagnosis of epilepsy is not provided. In cases of sudden death due to epilepsy or seizure disorder in which the underlying etiology is known, the underlying etiology should be indicated (e.g., epilepsy due to blunt head trauma or seizure disorder due to chronic alcoholism). In cases of death due to status epilepticus, epilepsy should also be mentioned if it is the underlying cause.
Other Significant Conditions
Part II of the death certificate should list factors contributing to death that did not result in the underlying cause of death indicated in Part I. Since the mechanism of death in epilepsy- or seizure-related deaths is considered a neurological event fatally disrupting cardiopulmonary function, coexisting cardiovascular or pulmonary disease (e.g., moderate coronary artery disease, emphysema) could be interpreted as contributing factors. In decedents with a history of epilepsy or seizure disorder in which there is witnessed seizure activity at the time of death (or suggestive postmortem evidence) and cardiac or pulmonary pathology is considered insufficient to be a competing cause, deaths could still be certified as epilepsy or one of the variations listed above in Part I with the cardiac and/or pulmonary findings listed as contributing factors in Part II.
In more frequent scenarios involving unwitnessed deaths with a clear competing cause of death (e.g., severe coronary artery atherosclerosis), it is recommended that both possible causes of death be indicated on the death certificate. An example would be an individual with epilepsy found dead in bed with 90% atherosclerotic narrowing of the left anterior descending coronary artery. One way to certify this death would be to put “atherosclerotic coronary artery disease” in Part I and “epilepsy” in Part II of the death certificate. Similarly, in an individual with epilepsy who is also found to have alcohol intoxication, both factors should be listed on the death certificate. In such a circumstance, the placement of each diagnosis in either Part I or Part II will depend on the alcohol concentration.
Manner of Death
A determination of seizure-related death does not preclude a nonnatural manner of death. When drowning cannot be excluded (e.g., a decedent with epilepsy found dead, submerged in a bathtub), traditional practice is to attribute death to drowning and the manner as accident. However, addition of “epilepsy” or “seizure disorder” in Part II is encouraged when appropriate, since drowning of a PWE in a bathtub without drug intoxication would be extremely rare, making a seizure-related death likely. It is possible that deaths associated with epilepsy caused by prior injuries can be the result of an accident, homicide, or even suicide, and should be certified as such (71).
How Injury Occurred
As this death certificate section will only pertain to nonnatural deaths, details regarding how an injury occurred should follow standard practices that often indicate the means and circumstances that led to the injury.
Conclusion
The recommendations of this panel are based on the best evidence provided in the medical literature for the investigation, evaluation, and certification of epilepsy-related deaths at the time of review. The likely significant underreporting of such deaths by medical examiners and coroners hampers advancements in research and public health, but more importantly fails to meet the responsibility of a medicolegal death investigation to provide accurate death certification. Use of these recommendations will improve the detection and reporting of epilepsy-related deaths.
Acknowledgements
The authors wish to express their appreciation for travel cost funding provided by the American Epilepsy Society and for the valuable input provided by Dr. Margaret Warner from the National Center for Health Statistics, Division of Vital Statistics, Mortality Statistics Branch.
Appendix 1. Literature Search Strategy
Databases: Medline, Medline In-Process & other Nonindexed Citations*, Embase
(* Medline In-Process & Other Nonindexed Citations not limited to humans)
-
1.
exp mortality/
-
2.
exp epilepsy/
-
3.
1 and 2
-
4.
epilep*.ti,ab.
-
5.
seizure?.ti,ab.
-
6.
4 or 5
-
7.
death?.ti,ab.
-
8.
mortality.mp. or exp Mortality/
-
9.
7 or 8
-
10.
6 and 9
-
11.
SUDEP.ti,ab.
-
12.
exp Epilepsy/mo [Mortality]
-
13.
“sudden death”.ti,ab.
-
14.
exp Death, Sudden/
-
15.
13 or 14
-
16.
6 and 15
-
17.
3 or 10 or 11 or 12 or 16
-
18.
exp toxicology/
-
19.
toxicology.ti,ab.
-
20.
exp histology/
-
21.
histology.ti,ab.
-
22.
exp Autopsy/
-
23.
exp “Cause of Death”/
-
24.
exp “Coroners and Medical Examiners”/
-
25.
exp Jurisprudence/
-
26.
exp Forensic Medicine/
-
27.
Autopsy.ti,ab.
-
28.
forensic pathology.ti,ab.
-
29.
Autopsies.ti,ab.
-
30.
Autopsied.ti,ab.
-
31.
Postmortem.ti,ab.
-
32.
“Post mortem”.ti,ab.
-
33.
“cause of death”.ti,ab.
-
34.
Coroner?.ti,ab.
-
35.
((Medical or Forensic) adj Examiner?).ti,ab.
-
36.
Jurisdiction.ti,ab.
-
37.
Jurisprudence.ti,ab.
-
38.
18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37
-
39.
(scene adj3 (findings or investigation or examination or death)).ti,ab.
-
40.
(death adj3 (classification or classify or investigate or investigation or certify or certification or determine or determination or cause)).ti,ab.
-
41.
38 or 39 or 40
-
42.
17 and 41
-
43.
limit 42 to (english language and humans and yr=”1970 -Current”)
Database: PubMed.gov (excludes MEDLINE)
(((epilepsy[tiab] OR epileptic[tiab] OR epilepsia[-tiab] OR seizure[tiab] OR seizures[tiab]) AND (death[tiab] OR deaths[tiab] OR mortality[tiab])) OR SUDEP[-tiab] OR “Epilepsy/mortality”[Mesh] OR ((“sudden death” [tiab] OR “death, sudden”[mesh]) AND epilepsy[tiab])) AND (“Autopsy”[Mesh] OR “Cause of Death”[Mesh] OR “Coroners and Medical Examiners”[Mesh] OR “Jurisprudence”[Mesh] OR “Forensic Medicine”[Mesh] OR Autopsy[tiab] OR Autopsies[tiab] OR Autopsied[tiab] OR Postmortem[tiab] OR “Post mortem”[tiab] OR “cause of death”[tiab] OR Coroners[tiab] OR Coroner[tiab] OR “Medical Examiners” [tiab] OR “Medical Examiner”[tiab] OR “Jurisdiction” [tiab] OR “Jurisprudence” [tiab] OR “toxicology”[mesh] OR toxicology[tiab] OR “anatomy and histology” [Subheading] OR histology[tiab] OR (scene[tiab] AND (findings[tiab] OR investigation[tiab] OR examination[tiab] OR death[-tiab])) OR (death[tiab] AND (classification[tiab] OR classify[tiab] OR investigate[tiab] OR investigation[-tiab] OR certify[tiab] OR certification[tiab] OR determine[tiab] OR determination[tiab] OR cause[tiab]))) NOT medline[sb] AND ((“1970/01/01”[PDAT] : “2016/12/31”[PDAT]) AND English[lang])
Legend: [mesh]=medical subject heading,
[tiab]=term appears within title or abstract
AFP Journal
Keywords: Epilepsy OR epileptic OR epilepsia OR seizure OR seizures
Years: 2011–2015
Appendix 2
Footnotes
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The opinions and conclusions of this paper have been reviewed and approved by the NAME Board of Directors and as such are endorsed by the National Association of Medical Examiners. These opinions and positions are based on a consensus of the current literature, knowledge, and prevailing theories on this topic. As scientific knowledge and experience grow and change, the National Association of Medical Examiners reserves the right to revise or update these opinions. The process by which NAME position papers are initiated, written, reviewed, and approved is publically available on the NAME website (www.thename.org). All scientific position papers endorsed by the National Association of Medical Examiners automatically expire five years after publication unless reaffirmed, revised, or retired at or before that time. This work is a product of NAME and as such, was not subjected to Academic Forensic Pathology editorial review. The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
This paper has been simultaneously published in Epilepsia, Volume 59, #3 and Academic Forensic Pathology: The Official Publication of the National Association of Medical Examiners, Volume 8, #1
FINANCIAL DISCLOSURE The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
References
- 1).Atherton D.S., Devinsky O., Hesdorffer D.C. et al. Implications of death certification on sudden unexpected death in epilepsy (SUDEP) research. Acad Forensic Pathol. 2016. Mar; 6(1): 96–102. 10.23907/2016.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Devinsky O., Spruill T., Thurman D., Friedman D. Recognizing and preventing epilepsy-related mortality: A call for action. Neurology. 2016. Feb 23; 86(8): 779–86. PMID: 26674330. PMCID: PMC4763802. 10.1212/WNL.0000000000002253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Fisher R.S., Acevedo C., Arzimanoglou A. et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014. Apr; 55(4): 475–82. PMID: 24730690. 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 4).Zack M.M., Kobau R. National and state estimates of the numbers of adults and children with active epilepsy — United States, 2015. MMWR Morb Mortal Wkly Rep. 2017. Aug 11; 66(31): 821–5. PMID: 28796763. PMCID: PMC5687788. 10.15585/mmwr.mm6631a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Fazel S., Wolf A., Långström N. et al. Premature mortality in epilepsy and the role of psychiatric comorbidity: a total population study. Lancet. 2013. Nov 16; 382(9905): 1646–54. PMID: 23883699. PMCID: PMC3899026. 10.1016/S0140-6736(13)60899-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Kaiboriboon K., Schiltz N.K., Bakaki P.M. et al. Premature mortality in poor health and low income adults with epilepsy. Epilepsia. 2014. Nov; 55(11): 1781–8. PMID: 25244361. PMCID: PMC4232978. 10.1111/epi.12789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Holst A.G., Winkel B.G., Risgaard B. et al. Epilepsy and risk of death and sudden unexpected death in the young: a nationwide study. Epilepsia. 2013. Sep; 54(9): 1613–20. PMID: 23895621. 10.1111/epi.12328. [DOI] [PubMed] [Google Scholar]
- 8).Ficker D.M., So E.L., Shen W.K. et al. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology. 1998. Nov; 51(5): 1270–4. PMID: 9818844. 10.1212/wnl.51.5.1270. [DOI] [PubMed] [Google Scholar]
- 9).Hesdorffer D.C., Tomson T., Benn E. et al. Combined analysis of risk factors for SUDEP. Epilepsia. 2011. Jun; 52(6): 1150–9. PMID: 21671925. 10.1111/j.1528-1167.2010.02952.x. [DOI] [PubMed] [Google Scholar]
- 10).Devinsky O., Hesdorffer D.C., Thurman D.J. et al. Sudden unexpected death in epilepsy: epidemiology, mechanisms and prevention. Lancet Neurol. 2016. Sep; 15(10): 1075–88. PMID: 27571159. 10.1016/S1474-4422(16)30158-2. [DOI] [PubMed] [Google Scholar]
- 11).Stecker E.C., Reinier K., Uy-Evanado A. et al. Relationship between seizure episode and sudden cardiac arrest in patients with epilepsy: a community-based study. Circ Arrhythm Electrophysiol. 2013. Oct; 6(5): 912–6. PMID: 23965297. 10.1161/CIRCEP.113.000544. [DOI] [PubMed] [Google Scholar]
- 12).Leestma J.E., Hughes J.R., Teas S.S., Kalelkar M.B. Sudden epilepsy deaths and the forensic pathologist. Am J Forensic Med Pathol. 1985. Sep; 6(3): 215–8. PMID: 3870673. 10.1097/00000433-198509000-00008. [DOI] [PubMed] [Google Scholar]
- 13).Coyle H.P., Baker-Brian N., Brown S.W. Coroners' autopsy reporting of sudden unexplained death in epilepsy (SUDEP) in the UK. Seizure. 1994. Dec; 3(4): 247–54. PMID: 7894834. 10.1016/s1059-1311(05)80171-2. [DOI] [PubMed] [Google Scholar]
- 14).Kim A.S., Moffatt E., Ursell P. et al. Sudden neurologic death masqueradingas out-of-hospital sudden cardiac death. Neurology. 2016. Oct 18; 87(16): 1669–73. PMID: 27638923. PMCID: PMC5085076. 10.1212/WNL.0000000000003238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Schraeder P.L., Delin K., McClelland R.L., So E.L. A nationwide survey of the extent of autopsy in sudden unexplained death in epilepsy. Am J Forensic Med Pathol. 2009. Jun; 30(2): 123–6. PMID: 19465799. 10.1097/PAF.0b013e318187a266. [DOI] [PubMed] [Google Scholar]
- 16).Office of Justice Programs [Internet]. Washington: U.S. National Institute of Justice; c2018. Death investigation: a guide for the scene investigator; [updated 2011. Jun; cited 2016 Jul 6]. 52 p. Available from: https://www.ncjrs.gov/pdffiles1/nij/234457.pdf. [Google Scholar]
- 17).Partemi S., Vidal M.C., Striano P. et al. Genetic and forensic implications in epilepsy and cardiac arrhythmias: a case series. Int J Legal Med. 2015. May; 129(3): 495–504. PMID: 25119684. 10.1007/s00414-014-1063-4. [DOI] [PubMed] [Google Scholar]
- 18).Bagnall R.D., Crompton D.E., Petrovski S. et al. Exome-based analysis of cardiac arrhythmia, respiratory control, and epilepsy genes in sudden unexpected death in epilepsy. Ann Neurol. 2016. Apr; 79(4): 522–34. PMID: 26704558. 10.1002/ana.24596. [DOI] [PubMed] [Google Scholar]
- 19).Skinner J.R., Chong B., Fawkner M. et al. Use of the newborn screening card to define cause of death in a 12-year-old diagnosed with epilepsy. J Paediatr Child Health. 2004. Nov; 40(11): 651–3. PMID: 15469540. 10.1111/j.1440-1754.2004.00498.x. [DOI] [PubMed] [Google Scholar]
- 20).Zhuo L., Zhang Y., Zielke H.R. et al. Sudden unexpected death in epilepsy: Evaluation of forensic autopsy cases. Forensic Sci Int. 2012. Nov 30; 223(1-3): 171–5. PMID: 22999232. 10.1016/j.forsciint.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 21).Guidelines on autopsy practice scenario 6: deaths associated with epilepsy. London: Royal College of Pathologists; 2005. 5 p. [Google Scholar]
- 22).Reichard R.R., Vaubel R. Investigation of deaths in seizure patients. Acad Forensic Pathol. 2014. Sep; 4(3): 331–7. 10.23907/2014.045. [DOI] [Google Scholar]
- 23).Liebenthal J.A., Wu S., Rose S. et al. Association of prone position with sudden unexpected death in epilepsy. Neurology. 2015. Feb 17; 84(7): 703–9. PMID: 25609764. 10.1212/WNL.0000000000001260. [DOI] [PubMed] [Google Scholar]
- 24).Black M., Graham D.I. Sudden unexplained death in adults caused by intracranial pathology. J Clin Pathol. 2002. Jan; 55(1): 44–50. PMID: 11825924. PMCID: PMC1769576. 10.1136/jcp.55.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Shields L.B., Hunsaker D.M., Hunsaker JC 3rd, Parker J.C. Jr.. Sudden unexpected death in epilepsy: neuropathologic findings. Am J Forensic Med Pathol. 2002. Dec; 23(4): 307–14. PMID: 12464802. 10.1097/01.PAF.0000043305.50912.17. [DOI] [PubMed] [Google Scholar]
- 26).Copeland A.R. Seizure disorders. The Dade County experience from 1978 to 1982. Am J Forensic Med Pathol. 1984. Sep; 5(3): 211–5. PMID: 6496433. 10.1097/00000433-198409000-00004. [DOI] [PubMed] [Google Scholar]
- 27).Earnest M.P., Thomas G.E., Eden R.A., Hossack K.F. The sudden unexplained death syndrome in epilepsy: demographic, clinical, and postmortem features. Epilepsia. 1992. Mar-Apr; 33(2): 310–6. PMID: 1547760. 10.1111/j.1528-1157.1992.tb02321.x. [DOI] [PubMed] [Google Scholar]
- 28).Nashef L. Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia. 1997. Nov; 38(11 Suppl): S6–8. PMID: 19909329. 10.1111/j.1528-1157.1997.tb06130.x. [DOI] [PubMed] [Google Scholar]
- 29).Kennedy J.D., Hardin K.A., Parikh P. et al. Pulmonary edema following generalized tonic clonic seizures is directly associated with seizure duration. Seizure. 2015. Apr; 27: 19–24. PMID: 25844030. PMCID: PMC4383169. 10.1016/j.seizure.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Kloster R., Engelskjøn T. Sudden unexpected death in epilepsy (SUDEP): a clinical perspective and a search for risk factors. J Neurol Neurosurg Psychiatry. 1999. Oct; 67(4): 439–44. PMID: 10486388. PMCID: PMC1736592. 10.1136/jnnp.67.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31).Leestma J.E., Walczak T., Hughes J.R. et al. A prospective study on sudden unexpected death in epilepsy. Ann Neurol. 1989. Aug; 26(2): 195–203. PMID: 2774506. 10.1002/ana.410260203. [DOI] [PubMed] [Google Scholar]
- 32).Terrence C.F., Rao G.R., Perper J.A. Neurogenic pulmonary edema in unexpected, unexplained death of epileptic patients. Ann Neurol. 1981. May; 9(5): 458–64. PMID: 7271241. 10.1002/ana.410090508. [DOI] [PubMed] [Google Scholar]
- 33).Davis G.G., McGwin G. Jr.. Comparison of heart mass in seizure patients dying of sudden unexplained death in epilepsy to sudden death due to some other cause. Am J Forensic Med Pathol. 2004. Mar; 25(1): 23–8. PMID: 15075684. 10.1097/01.paf.0000113930.53578.f8. [DOI] [PubMed] [Google Scholar]
- 34).Black M., Graham D.I. Sudden death in epilepsy. Curr Diagn Pathol. 2002. Dec; 8(6): 365–72. 10.1054/cdip.2002.0140. [DOI] [Google Scholar]
- 35).Leestma J.E., Kalelkar M.B., Teas S.S. et al. Sudden unexpected death associated with seizures: analysis of 66 cases. Epilepsia. 1984. Feb; 25(1): 84–8. PMID: 6692796. 10.1111/j.1528-1157.1984.tb04159.x. [DOI] [PubMed] [Google Scholar]
- 36).Al Sufiani F., Ang L.C. Neuropathology of temporal lobe epilepsy. Epilepsy Res Treat. 2012; 2012: 624519 PMID: 22957233. PMCID: PMC3420738. 10.1155/2012/624519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37).Frater J.L., Prayson R.A., Morris H.H. III, Bingaman W.E. Surgical pathologic findings of extratemporal-based intractable epilepsy: a study of 133 consecutive resections. Arch Pathol Lab Med. 2000. Apr; 124(4): 545–9. PMID: 10747311. SPFOEB%3E2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 38).Thom M. Neuropathological findings in epilepsy. Curr Diagn Pathol. 2004; 10(2): 93–105. 10.1016/j.cdip.2004.01.005. [DOI] [Google Scholar]
- 39).Barrow M., Roberts I.S., Soilleux E.J. Sudden death in epilepsy: standards of reporting and the value of toxicological analysis. J Clin Pathol. 2011. Nov; 64(11): 1025–8. PMID: 22021565. 10.1136/jclinpath-2011-200109. [DOI] [PubMed] [Google Scholar]
- 40).Samokhvalov A.V., Irving H., Mohapatra S., Rehm J. Alcohol consumption, unprovoked seizures, and epilepsy: a systematic review and meta-analysis. Epilepsia. 2010. Jul; 51(7): 1177–84. PMID: 20074233. 10.1111/j.1528-1167.2009.02426.x. [DOI] [PubMed] [Google Scholar]
- 41).Ng S.K., Hause W.A., Brust J.C., Susser M. Alcohol consumption and withdrawal in new-onset seizures. N Engl J Med. 1988. Sep 15; 319(11): 666–73. PMID: 3412384. 10.1056/NEJM198809153191102. [DOI] [PubMed] [Google Scholar]
- 42).Koppel B.S., Samkoff L., Daras M. Relation of cocaine use to seizures and epilepsy. Epilepsia. 1996. Sep; 37(9): 875–8. PMID: 8814101. 10.1111/j.1528-1157.1996.tb00041.x. [DOI] [PubMed] [Google Scholar]
- 43).Brown J.W., Dunne J.W., Fatovich D.M. et al. Amphetamine-associated seizures: clinical features and prognosis. Epilepsia. 2011. Feb; 52(2): 401–4. PMID: 21314677. 10.1111/j.1528-1167.2010.02924.x. [DOI] [PubMed] [Google Scholar]
- 44).Tofighi B., Lee J.D. Internet highs–seizures after consumption of synthetic cannabinoids purchased online. J Addict Med. 2012. Sep; 6(3): 240–1. PMID: 22824736. 10.1097/ADM.0b013e3182619004. [DOI] [PubMed] [Google Scholar]
- 45).Brust J.C. Seizures and substance abuse: treatment considerations. Neurology. 2006. Dec 26; 67(12 suppl 4): S45–8. PMID: 17190922. 10.1212/wnl.67.12_suppl_4.s45. [DOI] [PubMed] [Google Scholar]
- 46).Ryvlin P., Cucherat M., Rheims S. Risk of sudden unexpected death in epilepsy in patients given adjunctive antiepileptic treatment for refractory seizures: a meta-analysis of placebo-controlled randomised trials. Lancet Neurol. 2011. Nov; 10(11): 961–8. PMID: 21937278. 10.1016/S1474-4422(11)70193-4. [DOI] [PubMed] [Google Scholar]
- 47).George J.R., Davis G.G. Comparison of anti-epileptic drug levels in different cases of sudden death. J Forensic Sci. 1998. May; 43(3): 598–603. PMID: 9608695. 10.1520/jfs16186j. [DOI] [PubMed] [Google Scholar]
- 48).Schwender L.A., Troncoso J.C. Evaluation of sudden death in epilepsy. Am J Forensic Med Pathol. 1986. Dec; 7(4): 283–7. PMID: 3799558. [DOI] [PubMed] [Google Scholar]
- 49).Lathers C.M., Koehler S.A., Wecht C.H., Schraeder P.L. Forensic anti-epileptic drug levels in autopsy cases of epilepsy. Epilepsy Behav. 2011. Dec; 22(4): 778–85. PMID: 22088487. 10.1016/j.yebeh.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 50).May T., Jürgens U., Rambeck B., Schnabel R. Comparison between premortem and postmortem serum concentrations of phenobarbital, phenytoin, carbamazepine and its 10,11-epoxide metabolite in institutionalized patients with epilepsy. Epilepsy Res. 1999. Jan; 33(1): 57–65. PMID: 10022366. 10.1016/s0920-1211(98)00071-0. [DOI] [PubMed] [Google Scholar]
- 51).Tomson T., Sköld A.C., Holmgen P. et al. Postmortem changes in blood concentrations of phenytoin and carbamazepine: an experimental study. Ther Drug Monit. 1998. Jun; 20(3): 309–12. PMID: 9631928. 10.1097/00007691-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 52).Opeskin K., Burke M.P., Cordner S.M., Berkovic S.F. Comparison of antiepileptic drug levels in sudden unexpected deaths in epilepsy with deaths from other causes. Epilepsia. 1999. Dec; 40(12): 1795–8. PMID: 10612346. 10.1111/j.1528-1157.1999.tb01600.x. [DOI] [PubMed] [Google Scholar]
- 53).Feldman A.E., Gidal B.E. QTc prolongation by antiepileptic drugs and the risk of torsade de pointes in patients with epilepsy. Epilepsy Behav. 2013. Mar; 26(3): 421–6. PMID: 23218812. 10.1016/j.yebeh.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 54).Murphy S.L., Kochanek K.D., Xu J., Arias E. Mortality in the United States, 2014 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2015. [cited 2016 Jul 6]. 7 p. Available from: http://www.cdc.gov/nchs/data/databriefs/db229.pdf. [Google Scholar]
- 55).Opeskin K., Thomas A., Berkovic S.F. Does cardiac conduction pathology contribute to sudden unexpected death in epilepsy? Epilepsy Res. 2000. Jun; 40(1): 17–24. PMID: 10771254. 10.1016/s0920-1211(00)00098-x. [DOI] [PubMed] [Google Scholar]
- 56).Natelson B.H., Suarez R.V., Terrence C.F., Turizo R. Patients with epilepsy who die suddenly have cardiac disease. Arch Neurol. 1998. Jun; 55(6): 857–60. PMID: 9626779. 10.1001/archneur.55.6.857. [DOI] [PubMed] [Google Scholar]
- 57).P-Codrea Tigaran S., Dalager-Pedersen S., Baandrup U. et al. Sudden unexpected death in epilepsy: is death by seizures a cardiac disease? Am J Forensic Med Pathol. 2005. Jun; 26(2): 99–105. PMID: 15897710. [PubMed] [Google Scholar]
- 58).Lamberts R.J., Blom M.T., Novy J. et al. Increased prevalence of ECG markers for sudden cardiac arrest in refractory epilepsy. J Neurol Neurosurg Psychiatry. 2015. Mar; 86(3): 309–13. PMID: 24946773. PMCID: PMC4345521. 10.1136/jnnp-2014-307772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59).Nei M., Ho R.T., Abou-Khalil B.W. et al. EEG and ECG in sudden unexplained death in epilepsy. Epilepsia. 2004. Apr; 45(4): 338–45. PMID: 15030496. 10.1111/j.0013-9580.2004.05503.x. [DOI] [PubMed] [Google Scholar]
- 60).Devinsky O. Effects of seizures on autonomic and cardiovasular function. Epilepsy Curr. 2004. Mar; 4(2): 43–6. PMID: 15562299. PMCID: PMC531654. 10.1111/j.1535-7597.2004.42001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61).Mehta D., Curwin J., Gomes J.A., Fuster V. Sudden death in coronary artery disease: acute ischemia versus myocardial substrate. Circulation. 1997. Nov 4; 96(9): 3215–23. PMID: 9386195. 10.1161/01.cir.96.9.3215. [DOI] [PubMed] [Google Scholar]
- 62).Virmani R., Kolodgie F.D., Burke A.P. et al. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000. May; 20(5): 1262–75. PMID: 10807742. 10.1161/01.atv.20.5.1262. [DOI] [PubMed] [Google Scholar]
- 63).Kolodgie F.D., Virmani R., Burke A.P. et al. Pathologic assessment of the vulnerable human coronary plaque. Heart. 2004. Dec; 90(12): 1385–91. PMID: 15547008. PMCID: PMC1768577. 10.1136/hrt.2004.041798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64).So E.L., Sam M.C., Lagerlund T.L. Postictal central apnea as a cause of SUDEP: evidence from near-SUDEP incident. Epilepsia. 2000. Nov; 41(11): 1494–7. PMID: 11077466. 10.1111/j.1528-1157.2000.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 65).Ficker D.M. Sudden unexplained death and injury in epilepsy. Epilepsia. 2000; 41 Suppl 2: S7–12. PMID: 10885735. 10.1111/j.1528-1157.2000.tb01519.x. [DOI] [PubMed] [Google Scholar]
- 66).Swallow R.A., Hillier C.E., Smith P.E. Sudden unexplained death in epilepsy (SUDEP) following previous seizure-related pulmonary oedema: case report and review of possible preventative treatment. Seizure. 2002. Oct; 11(7): 446–8. PMID: 12237072. 10.1053/seiz.2002.0683. [DOI] [PubMed] [Google Scholar]
- 67).Linzer M., Grubb B.P., Ho S. et al. Cardiovascular causes of loss of consciousness in patients with presumed epilepsy: a cause of the increased sudden death rate in people with epilepsy? Am J Med. 1994. Feb; 96(2): 146–54. PMID: 8109599. 10.1016/0002-9343(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 68).Zaidi A., Clough P., Cooper P. et al. Misdiagnosis of epilepsy: many seizure-like attacks have a cardiovascular cause. J Am Coll Cardiol. 2000. Jul; 36(1): 181–4. PMID: 10898432. 10.1016/s0735-1097(00)00700-2. [DOI] [PubMed] [Google Scholar]
- 69).Ryvlin P., Nashef L., Lhatoo S.D. et al. Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study. Lancet Neurol. 2013. Oct; 12(10): 966–77. PMID: 24012372. 10.1016/S1474-4422(13)70214-X. [DOI] [PubMed] [Google Scholar]
- 70).Kopelnik A., Zaroff J.G. Neurocardiogenic injury in neurovascular disorders. Crit Care Clin. 2006. Oct; 22(4): 733–52. PMID: 17239752. 10.1016/j.ccc.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 71).Lin P., Gill J.R. Delayed homicides and the proximate cause. Am J Forensic Med Pathol. 2009. Dec; 30(4): 354–7. PMID: 19901806. 10.1097/PAF.0b013e3181c1582a. [DOI] [PubMed] [Google Scholar]


