Abstract
Drowning, which typically involves a watery environment, remains a serious public health concern claiming an estimated 362 000 lives per year worldwide across all socioeconomic classifications and has remained under close observation by the World Health Organization and its signatories. A significant number of water-related deaths are attributed to accidental drowning, while a smaller but still significant number represent suicidal or homicidal drowning. Others involve a combination of drowning precipitated by injury, intoxication, or environmental extremes. Still others involve victims that die from injury, intoxication, or a natural disease entity of such significance as to preclude the drowning process, while near or in water. While there may be an initial presumption that all water-related deaths are accidental drownings, other possibilities must be considered in the investigation of these types of deaths, as drowning as a cause of death is a diagnosis based on the exclusion of other potential causes. The coordinated investigative efforts of multiple agencies and disciplines are required not only for the designation as drowning as the cause of death but also for death certification. The ongoing analysis and dissemination of data generated from all levels of investigation augment our understanding of the impact on public health and safety, guiding allocation of monetary and educational resources in an effort to prevent further mortality and disability.
Keywords: Forensic pathology, Drowning, Water-related death investigation
Introduction
The scope of the impact of drowning deaths is far-reaching. While submersion in any fluid may result in drowning, more commonly these deaths result after prolonged submersion in watery environments, from small and shallow to vast and deep, and will be the primary focus of this review. A substantial number of submersion deaths are due to unintentional (accidental) drowning and occur in natural, watery environments or arise out of natural disasters such as foods and hurricanes. Globally, drowning is the third leading cause of unintentional injury death and accounts for nearly 4000 deaths per year in the United States, where it ranks as the tenth most common type of death due to injury (1, 2). Other deaths are water-related, involving bodies recovered near or from within such environments with findings of accidental, suicidal, or homicidal injuries or natural disease entities sufficient in and of themselves to constitute the cause of death and otherwise lack findings supportive of drowning. In water-related deaths involving submersion, efforts to explain how and why the body became submerged and why the individual was unable to self-extricate become necessary for the most accurate cause and manner of death determination. The postmortem diagnosis of drowning, attributes of the drowning environment, time of death determination, and postmortem interval determination continue to be topics of interest in an effort to improve medicolegal death investigation and resolution of water-related deaths. Case reports and case series of unusual findings and trends continue to populate the literature and, importantly, serve to confirm and/or expand our knowledge and sharpen our expertise. The ongoing analysis and dissemination of data generated from the investigation of water-related deaths aid in our understanding of the impact on public health and safety, which, in turn, guides allocation of resources and funding in an effort to prevent death and disability.
Water-related deaths often are prematurely, and at times subconsciously, labeled as accidental drownings. While this is often the case, the presumption that a body recovered from within or near a body of water is an accidental drowning can hinder timely recognition of indicators of foul play and other important clues present in or around the death scene (3, 4). This, in turn, may ultimately lead to false conclusions regarding cause and manner of death and adverse adjudication. Furthermore, failure to recognize certain scene attributes and bodily findings suggestive of homicide can hamper further investigation including interviews with witnesses and persons of interest or apprehension of suspects. The investigation of deaths associated with natural bodies of water can be particularly challenging due to the characteristics inherent in an environment that are constantly changing such as in lakes, rivers, and oceans. It is also important to recognize that not all water-related deaths can be presumed to be drownings and other factors such as water and weather temperature extremes, drug intoxication, or natural disease may be sufficient enough to be the cause of death and otherwise preclude drowning.
The investigation of the submerged body often requires the coordinated efforts and expertise of multiple agencies, especially when dealing with natural bodies of water. To varying degrees, those commonly involved include water-based emergency technical responders, law enforcement, medical first responders, medicolegal death investigators, forensic scientists, and forensic pathologists. Upon body recovery, assessment for vital signs and injuries followed by resuscitation and any stabilizing therapeutic interventions will occur as deemed necessary based on the condition of the body. Response by law enforcement personnel from various professional ranks and units will coincide with efforts of other first responders in the documentation of the scene and circumstances with focus on indicators of criminality.
Death scenes involving submerged bodies will warrant the response of medicolegal death scene investigators, forensic pathologists, and other professionals with varied forensic scientific expertise. The extent of their involvement will be dictated by the death circumstances.
Maintenance of an open line of communication amongst all involved investigative agencies is of paramount importance as this facilitates collection and preservation of evidence, interpretation of test results, and the determination of the cause and manner of death by the forensic pathologist. Such determination can have far-reaching effects including the identification of hazardous environments, uncovering of undiagnosed disease, and facilitating the adjudication of cases involving negligent acts or homicidal violence. Appendix 1 highlights investigative duties of select drowning death scenarios and the importance of the role of the technical, water-based first responder.
Discussion
Definitions
A complete review of submersion deaths must include the definition of drowning, which varies depending on the source, ranging from the broadest of description to the use of more concise medical terminology, mostly with an asphyxial basis. Merriam-Webster's Collegiate Dictionary defines drowning, in part, as “to suffocate by submersion, esp. in water” (5). Dorland's Illustrated Medical Dictionary defines drowning as “suffocation and death resulting from filling of the lungs with water or other substance or fluid, so that gas exchange becomes impossible” (6). The definition adopted by the World Congress on Drowning that convened in Amsterdam in 2002 and endorsed by the World Health Organization (WHO) defines drowning as “the process of experiencing respiratory impairment from submersion/immersion in liquid” (7). Forensic pathologists who are directly involved in the certification of these deaths generally define drowning as an asphyxial death in which the body is deprived of oxygen as a result of impairment of pulmonary oxygen exchange after partial or complete submersion in a liquid, most commonly water, with subsequent inhalation of some quantity of the liquid deep into the lungs (8). Near-drowning has been used to describe death following cardiopulmonary resuscitation with at least 24 hours of in-hospital survival and the development of one or more complications (9).
Epidemiology and Trends
As the third leading cause of unintentional injury death worldwide, drowning accounts for 7% of all injury-related deaths. In 2015, it is estimated that 360 000 individuals died from drowning (1). This figure underestimates, by possibly as much as 50%, the true number of drowning deaths, which excludes those caused by large-scale natural disasters such as foods and transportation accidents and intentional deaths resulting from suicide and homicide (10). This underestimation is reportedly due to the variation in reporting and categorization methods used by countries (1). Those disproportionately affected are males (2:1 male vs. female), the young (ages 1–24 years), those with unsupervised access to natural bodies of water, and those of lower socioeconomic status (1). Alcohol impairment is an additional well-known risk factor (1, 10).
In the United States, a total of 46 419 unintentional drowning deaths (including boating-related), or an average of 3868 deaths per year, were tabulated from 1999–2010, placing drowning as the tenth leading cause of injury death across all age groups (2, 11). The incidence of death due to unintentional drowning has fallen overall for individuals in age categories under 1 year of age (infants), 1–4 years of age, and 5–19 years of age categories over this time period (2) (Figure 1). Among these groups, children ages 1–4 years still had the highest incidence of drowning deaths, followed by individuals 85 years of age and older. The likelihood of drowning in a particular location has been found to vary by age group with infants and those age 85 years and over more likely to drown in bathtubs, children age 1–4 in swimming pools, and individuals in the 5–19 and 20–84-year age groups in natural bodies of water (2). Deaths from drowning have been found more likely to occur on weekends than weekdays at a rate of 18.8 versus 9.3 per 100 000 population, respectively (2). Males and African-Americans were found to be disproportionately affected as well (2). Other associated risk factors that have been cited include swim inability, lack of supervision, lack of physical barriers such as fences, failure to wear life-preserving equipment, alcohol impairment, and seizure disorders (2).
Figure 1.
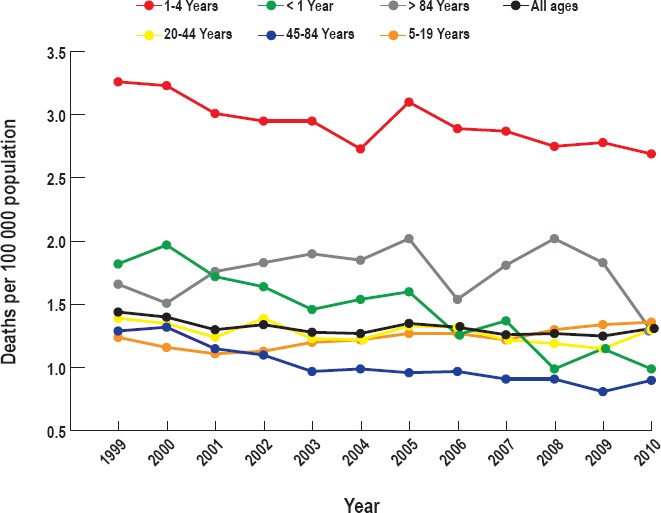
Death rates from unintentional drowning by age group, United States, 1999–2010, Source CDC/NCHS, National Vital Statistics System (2).
Suicidal and homicidal drownings represent a smaller but significant segment of drowning deaths. Suicidal drownings are uncommon, and the percentages of all suicides vary between less than 1% to nearly 9% of all manners of drowning, depending upon the geographic location and access to water, with lakes, oceans, and rivers the more common locales (12–16). Older Caucasian men tend to be the typical decedent in suicidal drowning deaths; however, a significant proportion of women utilize this less violent method of death (17, 18). A history of psychiatric illness and the postmortem detection of variable levels of psychiatric medications and ethanol has been reported (16). While a number of small case series and case reports of adult, child, and infant homicidal drownings exist (19–25), studies examining characteristics of large numbers of homicidal drownings (specifically homicide by drowning) are sparse. Its occurrence has, nevertheless, been noted to be far less common overall as compared to drownings by other manners of death, or even other types of homicidal asphyxial deaths such as strangulation. One such study of homicidal drowning found 12 out of 2617 homicides, or 0.46%, were a result of drowning (26). The subtlety or lack of autopsy findings that can present with homicidal drownings, insufficient investigative information, and statistical under-reporting may all perhaps contribute to the overall low incidence.
Process and Pathophysiology
Drowning is largely an asphyxial process with effects on multiple organ systems. The lungs, the anatomic center for respiration, are the primary organs affected by drowning. Respiration is an involuntary process under the control of the central nervous system in response to changes in blood and tissue oxygen (O2) and carbon dioxide (CO2) levels and the blood pH. Diffusion and exchange of these gases occurs across the alveolar-capillary membrane interface propelled by inhalation and exhalation (Figure 2). Cartilage and innervated smooth muscle help maintain patency of the airways in order to allow unobstructed movement of O2 and CO2. Activation of the laryngeal nerves by potentially obstructing foreign objects or fluids can trigger larygospasm, a protective mechanism. Ciliated respiratory epithelium, mucous, and the cough reflex help to trap bacteria and other particulates and keep the airways clear and free of obstruction. At the alveolar level, patency is further maintained by the action of surfactant. Prolonged obstruction at any level can lead to low or absent organ/tissue oxygen levels (hypoxia or anoxia) and low arterial blood oxygen levels (hypoxemia). This defines asphyxia. Ultimately irreversible neuronal cell injury and cardiorespiratory arrest will result if the cause of the obstruction is not removed.
Figure 2.
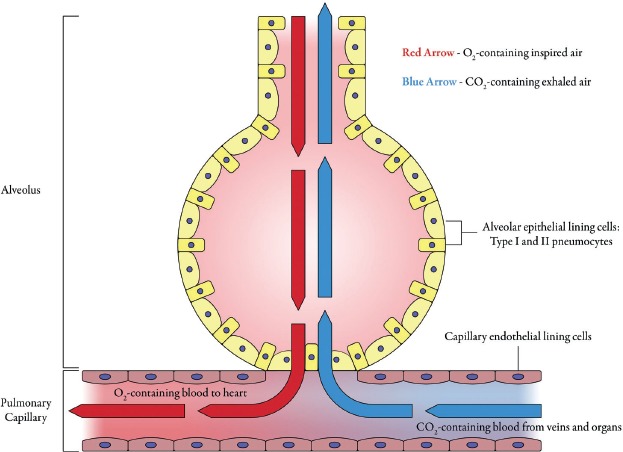
O2/CO2 alveolar-capillary interface. Reproduced with permission of CRC Press (4).
Animal drowning experiments and case series reports of human drownings have augmented our understanding of the sequence of events and physiological effects. Factors that precipitate drowning itself may be at play even before the actual drowning process begins and starts with contact with the watery environment. From the point of immersion of the body in which the face is not submerged, to submersion of the face with obstruction of the upper airway, multiorgan system physiological effects have been described (27–29). Immersion of a body, particularly at temperature extremes, has physiologic effects and can lead to submersion and precipitate drowning. Immersion in hot water, particularly at temperatures greater than 38°C, such as in hot tub environments, has known physiologic effects particularly on the cardiovascular and thermoregulatory systems. These effects include ventricular arrhythmia, tachycardia, vasodilation, and hyperthermia, which may be deleterious in individuals with ischemic cardiomyopathy due to coronary atherosclerosis and hypertensive cardiovascular disease. The effects of cold water immersion include rapid cooling of the skin (cold shock), gasping, cardiac arrhythmias, skeletal muscle fatigue, and rapid loss of body temperature leading to hypothermia with loss of consciousness and multiorgan failure. Temperatures at or below approximately 25°C evoke many of these known physiological responses. Ultimately, the inability to extricate oneself from the cold watery environment increases the likelihood of submersion with drowning. Other factors inherent in the body of water itself, such as swift-moving waters, strong currents, underwater fixed and moving objects, and dangerous aquatic life are also precipitants of drowning.
The immersion or more precisely the presubmersion phase in which the individual maintains the face above water by treading will continue until the point of fatigue in deep watery environments. This is followed by a submersion phase in which the covering of the nose and mouth will trigger a series of physiological responses beginning with voluntary breath holding or apnea (29). The entire head need not be submerged and thus drowning can occur in as little as a few inches of water that could exist in buckets, washbasins, and shallow natural bodies of water like streams.
Breath-holding continues until a certain breakpoint or critical blood O2 concentration (and CO2) is reached, causing states of hypoxia, hypoxemia, and hypercarbia. This breakpoint triggers an involuntary gasping response, which would ideally lead to inhalation of air if head is above water, but by being submerged in the now hostile watery environment, water and any admixed debris enters the airway. There is interindividual variability in the amount of water inhaled and as little as 1 mL/kg up to 11 mL/kg of water can precipitate the drowning process (30, 31). Swallowing of water may occur simultaneously, increasing the risk of vomiting with aspiration of gastric contents, which can cause further alveolar injury. Transient laryngospasm or bronchospasm may occur as a result of stimulation of the innervated mucosa of the orpharynx and larynx by water. Whether this actually limits or precludes further entry of water into the lungs leading to so-called “dry drowning” remains unclear and unsubstantiated, prompting the World Congress on Drowning to abandon use of the term (26, 27, 32–34). Subsequent relaxation of the larynx will eventually permit water to be inhaled into the lungs. The worsening hypoxia and hypoxemia initiated by the impaired oxygen diffusion in the lungs leads to anoxia, depletion of brain energy reserves with deterioration of brain function, failure in brain energy metabolism, loss of consciousness, and irreversible neuronal cell injury. Irreversible neuronal cell injury may begin approximately four to six minutes after sustained oxygen deprivation and the degree of partial or total recovery after a submersion event is dependent on the extent and regions of the brain affected and the promptness of resuscitative efforts. Aside from the neurological effects arising from pulmonary oxygen impairment, worsening hypoxia may also trigger an asphyxial or hypoxic cardiac arrest (33, 35). Profound systemic hypoxia coupled with hypercarbia also leads to respiratory and metabolic acidosis, cardiovascular collapse with multisystem organ failure, and eventually death.
The presence of fluid, commonly water, within the terminal airways and alveoli disrupts the free diffusion of O2 across the alveolar-capillary interface. Com-pounding this process is the dilutional and/or disruptive effect of even small amounts of inhaled water on surfactant (30) (Figure 3). Surfactant, a lipoprotein secreted by Type II pneumocytes, coats the alveolar surface where it acts to reduce surface tension allowing the alveoli to remain open and available for O2 diffusion. With submersion and inhalation, the relatively hypotonic fresh water will also diffuse across the semi-permeable alveolar-capillary membrane into the pulmonary microcirculation and be circulated throughout the body causing dilution of electrolytes of historically debatable clinical significance (30, 31, 36, 37). The hypertonicity of seawater draws plasma out of circulation into the alveoli causing some degree of hemoconcentration. The semipermeable alveolar capillary membrane also allows for transudation of blood proteins into alveolar spaces causing pulmonary edema. The influx of alveolar fluid results in dilution or alteration of surfactant, whether caused by freshwater or saltwater, leading to collapse of alveoli and rendering them unavailable for O2 diffusion into the capillaries and diffusion of CO2 from the capillaries. As a result, venous blood is shunted past unventilated areas of the lung altering the ventilation-to-perfusion ratio and increasing pulmonary vascular resistance, leading to systemic hypoxia and acute respiratory distress syndrome (ARDS) (33).
Figure 3.
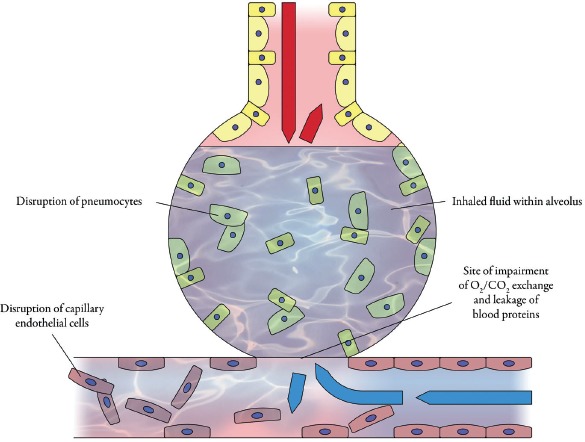
Disruption of O2/CO2 alveolar-capillary diffusion by inhalation of water. Reproduced with permission of CRC Press (4).
If submersion is prolonged (exceeding four to six minutes) without prompt resuscitation, irreversible neuronal cell injury along with the development of hypoxic-ischemic encephalopathy clinically ultimately results in cardiorespiratory arrest and death. The shorter the time frame from submersion to resuscitation, the more complete the recovery. Limited neurological sequelae and more complete recovery have been reported, especially in children or those with uncomplicated environmental or clinical hypothermia (36, 37).
Potentially lethal complications following drowning include acidosis, multiorgan failure, rhabdomyolysis, ischemic kidney injury, and coagulopathy. Even with prompt resuscitation, the effects of aspirated water and other fluids can persist and other complications can arise within the interval of in-hospital survival and following discharge. Postimmersion syndrome or secondary drowning have been used to describe both short-term and long-term pulmonary effects of water/fluid inhalation (27). Inhalation of chlorinated water from pools or cleaning products can cause a chemical pneumonitis. Swallowing and distention of the stomach can precipitate vomiting with aspiration of acidic gastric contents causing chemical pneumonitis or lead to aspiration pneumonia with subsequent respiratory failure and death, with or without sepsis. Pneumonia, sinusitis, and central nervous system infection may develop more than a month following the drowning event as a result of inhalation of waterborne bacteria, amoebas, and fungi (34). Clinical and pathologic sequela of drowning with inhalation of unusual fluids such as oils and syrup have been reported with features of asphyxia and distinctive findings relative to the drowning media (38–40). Near drowning has been used in certification of deaths occurring within 24 hours following submersion and encompasses complications arising from drowning asphyxia.
Pre-Autopsy Processing and the Importance of Historical Context
Ordinarily, routine and recreational water-related activities, whether indoors or out, pose little bodily threat. Alteration of human and/or environmental factors, however, may turn a docile watery environment into a hostile one and lead to drowning. The late and renowned Dr. Joseph H. Davis referred to this as the “drowning equation” in which drowning is the constant (and the end result) and human and environmental factors represent the variables (41). From this equation are derived specific questions of investigative importance: Was the victim alive or dead before entry into the water? Did the victim drown? Why or how did the victim get into the water in the first place? Why was the victim unable to survive the water? Addressing each question by way of a thorough investigation and autopsy performance with toxicological analysis will aid in answering them and properly certifying the death. Questions will arise regarding recovery of a nude body prompting a search for the explanation such as stripping off of clothing caused by rough water conditions or snagging against underwater debris versus a dumped body with death by other means.
Other questions may arise relative to specific locations or water conditions: Is a body found on the seashore representative of a drowning death left exposed by receding tides, transportation from another location, or a collapse and death from some other cause while near water? Is a body found in a bathtub representative of death due to natural disease with a terminal collapse, a homicidal drowning, or a drowning coupled with some precipitating factor such as drug or alcohol intoxication? Is the palpable or measured body temperature assessed on-scene consistent with the water conditions particularly cold water conditions, and are there signs of hypothermia? Drowning can take place in as little as a few inches in water such as in ditches, puddles, washbasins, hot tubs, and buckets which would ordinarily be escapable and thus identifying factors such as intoxication, catastrophic natural disease, injury, disability, young age, or underdevelopment is necessary for explanatory purposes. The condition and intactness of the body will prompt questions regarding time of death, postmortem submersion interval (PMSI), and identification where application of knowledge of taphonomic factors associated with different types of natural watery environments will be necessary (42). Tables 1 and 2 highlight considerations and basic approaches in the workup of drownings and water-related deaths.
Table 1.
Select Considerations in Water-Related Deaths with Corresponding Examples
| Natural death preceding or during submersion | Coronary artery thrombosis with sudden cardiac death while swimming; fatal arrhythmia due to cardiac channelopathy while underwater swimming; Nontraumatic seizure disorder with seizure onset while swimming |
| Homicidal drowning | Forcibly holding or pulling victim under water; pushing of victim into water; victim incapacitation by inflicted injury or intoxication while in/near water |
| Homicidal injury with body disposal | Lethal blunt, sharp, or asphyxial injury followed by weighted body submersion |
| Suicidal drowning | Submersion assisted by self-tying of hands and/or feet or use of weighted materials (i.e., backpack filled with large rocks) |
| Accidental drowning | Precipitated by swim fatigue, swim inability, drug and alcohol intoxication, equipment failure, carbon monoxide poisoning from motorized vessels, incapacitating injury, rough/swift waters, temperature extremes (i.e., causing hypothermia), entanglement by underwater objects, unsecured or unsupervised locations (i.e., ponds, lakes, pools), electrical current from defective pool lights, electrical current from appliance submerged in bathtub, entrapment by pool drains |
| Accidental death from trauma preceding or accompanying submersion with drowning | Lethal blunt force, head, neck, and torso trauma from fall, diving with impact, or watercraft collision |
| Nontraumatic accidental death precluding the drowning process | Pre- or peri-submersion lethal drug or medication overdose |
Table 2.
Investigative Approach and Workup of Water-Related Deaths
| Scene Investigation and Review of History |
| Body location, position, condition, temperature |
| Victim identification, medical, social, and psychiatric history |
| Environmental and water conditions |
| Recovery efforts and agencies involved |
| Resuscitation efforts |
| Witness statements |
| Evidence collection and preservation: clothing and personal effects, safety and diving gear, drowning medium |
| Collection, preservation and examination of underwater breathing gear, life vests, vessels and vehicles |
| Ancillary collection/examinations by forensic anthropologist, entomologist, botanist |
| Documentation: narrative reports, diagrams, photographs, video |
| Pre-Autopsy Preparation |
| Trace evidence examination and collection of on-body evidence |
| DNA collection: victim and foreign sources |
| Imaging: radiography, postmortem computed tomography |
| Autopsy-External Examination |
| Body/clothing: condition, wetness, intactness, aquatic debris |
| Wrinkling and pallor of palms and soles, froth/foam cone |
| Rigor mortis and lividity patterns and color, crepitance, body temperature |
| Decompositional changes |
| Injuries and injury patterns: acute vs. resolving, antemortem vs. postmortem |
| Supportive findings of drowning |
| Autopsy-Internal Examination |
| Injuries and injury patterns: acute vs. resolving, antemortem vs. postmortem, resuscitative |
| Decompositional changes |
| Supportive findings of drowning |
| Natural disease with lethal potential |
| Tissues and bodily fluids sampling and submission for toxicological analysis |
| Histological and toxicological sampling and submission |
| Special Case-Based Examinations and Procedures |
| Dissections: neck and spinal cord, cardiac conduction system |
| Flotation/hydrostatic test (infants and fetuses) |
| Assessment for cavity and intravascular air |
| Tissue/blood sampling for microbial analysis |
| Analysis for cardiac channelopathies |
| Microscopic examination/analysis of drowning media: diatoms, chemicals |
Pre-autopsy information of investigative importance is necessary for interpretive context in water-related deaths and may be sparse or nonexistent altogether and all efforts to obtain any available information is necessary. These include decedent identification, location of body, condition of the recovered body, type and extent of recovery efforts, the type and extent of resuscitative efforts (if any), and the presence or absence of any personal effects and life preservers. Witness accounts of the decedent's appearance and state of dress, state of mind, activities prior to submersion, and signs of impairment prior to entry into a body of water can provide explanation as to how and why the submersion happened. Establishing the identity of a victim can lead to information regarding medical history, psychiatric history, and substance use history and give direction and focus to the investigation and autopsy.
The medicolegal death investigator (MDI) performs the requisite functions, becomes instrumental in obtaining relevant death scene information through scene visitation and direct observation or from other first responders, and provides written and photographic documentation along with a report to be reviewed by the forensic pathologist. As representatives of the medical examiner's/coroner's (ME/C's) office, MDI also serve as an initial point of contact for law enforcement and technical recovery personnel and the conduit of information between these personnel and the forensic pathologist. Generally, the investigator will document bodily findings relative to immersion/submersion and drowning in addition to environmental and water conditions, whether in a natural setting or indoors. The position of the body as found prior to arrival becomes vitally important in determining if the victim was submerged at all, and if so to what degree as in the case of bystander resuscitation in which the body has been moved or repositioned. Noting the presence, condition, and state of dryness or wetness of the body and any attached or detached clothing is important for any scene. Certain scenes will require focus on documenting or uncovering additional pertinent findings. Signs of bathing such as wet towels, drain position, the proximity of electrical devices, the presence of a soap scum level, or signs that the body was moved, are some important factors for bathtub drownings. The presence of a lifeguard, video surveillance, witness observations, evidence of access through an unsecured gate, and swim ability are a few pertinent factors in pool drownings. In drownings occurring in natural environments, underwater and land topography, water temperature and conditions, the lack of safety gear, signs of intoxication, state and type of dress, and signs of bodily trauma are important to note. Other important information includes any medical and psychosocial history or history of trauma. Suspicious, homicidal, and equivocal death circumstances or unusual bodily findings may warrant consultation with and scene visitation by the forensic pathologist.
Obtaining and reviewing reports that document information including scene attributes, evidence recovery, body recovery efforts, weather and water conditions, indoor scenes, and resuscitative efforts may be helpful for the forensic pathologist to interpret autopsy findings and properly certify the death. These reports include police reports, technical dive team reports, coast guard reports, emergency medical services reports, and the report prepared by the MDI. Review of any ancillary reports relative to examination of safety gear, underwater breathing gear, watercraft, or implanted medical devices such as pacemakers may be helpful prior to any final cause and manner of death conclusion. In drownings that involve an in-hospital survival interval, medical records documenting clinicopathologic sequela can be helpful since the classical findings of acute drowning may be absent at autopsy. Due to ongoing investigation, many of these reports may not be completed at the time of autopsy, which will require verbal and/or electronic communication with the relevant investigator. These communications, inclusive of contact name, date, and summary of information relayed or received, must be documented in the case file.
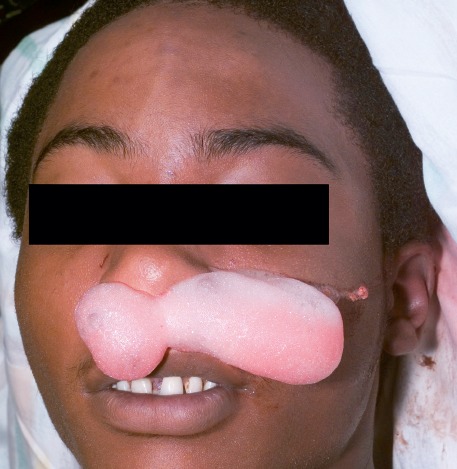
Depending on the known death circumstances and body condition, the initial pre-autopsy processing of a body may be necessary. This involves the collection, preservation, and examination of on-body evidence such as clothing, items found in clothing including articles of identification, body wrappings or binding materials, and sampling from body regions for foreign materials (Image 1). The identification of binding materials or items used as weights and the precise way in which they are affixed to the body is of particular importance and can have bearing on manner of death determination, especially suicide versus homicide (43, 44). Notation of the type, condition, and wetness of clothing and any adhered aquatic debris is important as it may correspond to victim's appearance when last seen or characteristics of the location where recovered. Biological material may contain DNA and while recovery of DNA from submerged biological fluids such as saliva, blood, and semen has been demonstrated, the success of recovery of undegraded DNA is greatly and sometimes rapidly reduced in the setting of prolonged submersion and decomposition (45–47). Successful identification using DNA of dismembered and disarticulated remains submerged for extended times has been reported (48, 49). Other more traditional scientific means of identification such as fingerprinting, radiographic documentation of surgically implanted devices, or unique skeletal attributes such as craniofacial sinuses, and odontological comparisons may be necessary. Fingerprint enhancement techniques have been used in the identification of submerged remains (50). Unique body features like piercings and tattoos and other on-body items such as engraved jewelry or dentures can provide presumptive or confirmatory identification. Any on-body diving and personal safety equipment should be retained for later examination by respective experts for examination of condition and functionality. If feasible, a submerged vehicle containing a body or bodies should be transported in its entirety to the ME/C office for in situ examination of the body or bodies and vehicle, which may provide clues regarding circumstances leading up to the vehicle becoming submerged. Pre-autopsy radiographic images can be helpful in locating projectiles; other retained foreign materials, and the identification of air within body cavities in incidents involving underwater breathing gear.
Image 1.

Decomposed clothed and tethered body from pond (A), with clothing defect (B), corresponding to stab wounds (C).
Autopsy
In forensic pathology practice, the diagnosis of drowning as a cause of death follows exclusion of other causes and requires the performance of a full autopsy with testing of bodily fluids and interpretation of all results in the context of all known historical and investigative information. In the absence of multiple supportive findings of drowning, consideration of another nonnatural cause of death is warranted. As stated previously and for emphasis, bodies recovered near or within a body of water can represent a death from a variety of different causes and manners other than accidental drowning. A list of select considerations appears in Table 1.
While autopsy performance affords external and internal access to much of the anatomy to assess for findings of drowning, postmortem whole body computed tomography (WBCT) has been shown to be increasingly useful in the noninvasive documentation of these findings (51). Excessive fluid and sedimentous material in the sinuses and cavities of the head and chest, oropharynx, lungs, stomach, and small intestine have been identified in drownings. Identification of density differences as result of hemodilution or hemoconcentration in viscera have been used in the differentiation of fresh versus saltwater drownings.
External Findings
External findings in drowning deaths vary and are both nonspecific and nondiagnostic. Some findings are merely indicative of a period submersion in which there has been contact with water of sufficient time to cause visible changes. The PMSI, characteristics such as water temperature and current, time elapsed between recovery and autopsy, medical interventions, and any in-hospital survival time are all factors affecting what may or may not be visible. The more prolonged the PMSI, the less prominent or potentially more confounding will be the findings by the time an autopsy performed.
Injuries of various types, number, and distribution may be found. Blunt force injuries (abrasions, contusions, and lacerations) are most common. These may have been sustained on land prior to submersion, on impact with water or objects in or near water, or while submerged. In larger bodies of water, the manner of entry, the presence of moving or fixed natural or manmade objects, water current and wave action, underwater topography, and predation by marine or terrestrial carnivorous animals will play a role. Resuscitative and recovery efforts may cause abrasions and contusions of the chest, face, neck, or the inner and proximal aspects of the upper extremities, and sparse facial or scleral petechiae may be present. The presence of injury may depend on factors that impede or protect the body from being impacted and include those that affect body buoyancy. These factors include adiposity, the presence of buoyant clothing or flotation devices such as life vests, and the amount of air contained in lungs and intestines and will determine the depth to which the body will sink along with the potential to sustain injury from contact with objects. Clothing and wet suits may protect the skin from injury. In deeper waters, the body often assumes a prone position with the head down and the extremities dangling downwards, known as the “drowner's pose,” as it sinks to the bottom. Postmortem travel abrasions and lacerations on exposed body surfaces such as the forehead, backs of the hands, knees, and tops of the feet can appear as the body is dragged against the bottom surface or propelled by a wave (Image 2). Injuries may be antemortem, with gross or microscopic evidence of vital reaction (hemorrhage and inflammatory infiltrates), or postmortem, with lack thereof. Questionable injuries should be examined microscopically. Whether sustained in the antermortem or postmortem setting, animal predation can cause superficial or deep disruption to organs, soft tissue, and bone and leave patterns characteristic of the type of animal. Postmortem predation by marine or freshwater fauna and environmental taphonomic changes can also alter, confound, or obscure antemortem injury and include dismemberment, disarticulation, tissue loss, and skeletonization (52–55). Identification of choplike cutaneous wounds with characteristic periodicity will be helpful in reconstruction of injuries caused by boat propellers (56) (Image 3). Leaching of blood out through open wounds and decompositional changes may make differentiation between antemortem versus postmortem injury difficult or impossible. Where bare skin is exposed to air, a parched, darkened, leathery appearance can result and obscure superficial injury. Physical injury may be lacking altogether in certain cases of drowning, such as those involving electrocution (57). Thermal and chemical injuries subsequent to immersion/submersion with drowning in liquid mediums such as gasolines, hot oils, and waxes have been reported (58, 59). Other injuries that are not related to drowning may give clues to the circumstances that may have precipitated drowning such as the presence of track marks indicating intravenous drug use, healed incised wounds of the wrists indicating previous suicide attempts, or surgical scars indicative of disability.
Image 2.

Travel abrasions.
Image 3.
Propeller injuries. Reproduced with permission of CRC Press (4).
In bodies without significant decomposition or prolonged resuscitation, the typical findings associated with drowning are more easily identified. Exudation of a column of white or pink froth from the nostrils and/or mouth is often apparent or becomes apparent by simply pressing down on the chest. It is a manifestation of the mechanistic action of terminal respiratory efforts on an admixture of residual intrapulmonary air with intrapulmonary drowning and edema fluid. The froth or foam cone is seen in other types of deaths with increased pulmonary edema, such as drug overdoses and congestive heart failure of various causes (Image 4). Depending on the time elapsed since recovery, the skin and hair may be wet, damp, or dry. Pallor with wrinkling of palms, soles, fingers, and toes (sometimes referred to as “washerwoman's hands” or “washerwoman's changes”) may be noted (Image 5). These changes are a result of dermal absorption of water appearing in fingertips in as little as 20–30 minutes after immersion/submersion and disappearing slowly upon exposure to open air and, thus, may be unapparent at autopsy (60). If recovered from natural water environments, adherent aquatic debris such as silt, mud, sand, gravel, vegetation, algae, and shell fragments may be adhered to the skin surface or found in body creases, cavities, or orifices such as the gluteal folds, nostrils and mouth, or found in the scalp hair. Rigor mortis will be apparent depending on water temperature and duration of submersion, except in decomposed bodies. Rigor mortis affects all skeletal muscles including the errector pili muscles in skin causing cutis anserine, or so-called “goose flesh,” and can be seen on submerged and nonsubmerged skin alike and is not specific only for cold water immersion. Lividity will be most apparent in the face, neck, chest, hands, lower extremities and feet in a prone body but may be unapparent or incompletely formed in bodies subject to fast flowing water. The color of lividity should also be noted, as it may be informative and direct specific postmortem testing. For example, bright red or pink lividity may be observed in cases of drowning precipitated by carbon monoxide poisoning from inhalation of boat exhaust fumes or deaths associated with hypothermia. Cyanotic congestion may be seen in the face and neck and indicates a state of terminal hypoxia (Image 6). SCUBA-related drowning deaths or those with impacts causing rib fractures and lung injury may exhibit palpable crepitance signifying subcutaneous emphysema.
Image 4.
Froth cone of drowning victim.
Image 5.

Wrinkling and pallor of skin.
Image 6.

Facial congestion and cyanosis in drowning victim.
The many alterations conferred by postmortem decomposition add another layer of difficulty in regard to the determination of the cause of death, time of death, and location of death in any death and especially in bodies recovered from water. Recognition of the environment and its inherent features is necessary for context in the interpretation of autopsy findings and serves as a caution against over-interpretation or misidentification of findings, as emphasized, along with illustrative photographs in a recent comprehensive publication by Caruso (61). Decompositional changes look similar to those occurring on land and include skin discoloration, skin sloughing, marbling, production of purge fluids, and bloating as well as corresponding visceral and soft tissue changes. These changes occur in part as a result of the body's autolytic and putrefactive processes with additional changes conferred by colonizing organisms, and will be accelerated in warmer water and slowed in cold water. Bloating of an untethered body will inevitably cause the sunken body to float to the surface maintaining the prone position allowing exposed body regions to dry out, darken, and mummify, or otherwise be exposed to predation, mold, and algal colonization (Image 7). Even a body tethered with attached weights can float to the surface with the weights in tow. Occasionally, the floating, decomposed body may present with the anterior side up allowing the face, chest, and abdomen to be exposed to artifacts of drying, predation, and larval colonization (62). Changes of decomposition generally occur more slowly in water than on land and are affected by factors inherent in the water such as salinity, temperature (especially cooler temperatures), marine life, bacterial composition, currents, absence of flies and fly larvae, and contact with underwater objects. Saltwater portends a slower rate of decomposition than fresh water due to the retardation of bacterial proliferation as a result of the higher salinity. Bodies found in deep, cool waters owing to entrapment, or are otherwise protected from marine predation, may have little in the way of decomposition. The body may be nearly or completely defleshed to the point of skeletonization, aided by warm temperatures and/or aquatic organisms, which may require the expertise of the forensic anthropologist to assist with identification and assessment of taphonomic changes (61, 62). Bodies in damp or wet environments for prolonged periods of months or years may develop a chunky gray-white substance known as adipocere as a result of bacteria-mediated hydrolysis of body fat. While the time frame of development of adipocere varies depending on factors inherent in different watery environments, its preservative qualities are recognized, including the preservation of anatomy, skeletal injury, and toxicological evidence (63). In addition to adipocere, colonization by algae, larvae, and bacteria as part of decomposition may be apparent and have been used in the estimation of the PMSI, time of death, and location of death, sometimes requiring expertise in entomology and botany. Determinations made by the forensic entomologist or botanist can be of great investigative importance in the reconstruction of the circumstances leading to the death and identification of the decedent (64–67). In cases of prolonged submersion, decomposition will proceed rapidly following recovery and these changes can obscure other preexisting antemortem or postmortem findings. Therefore, prompt refrigeration followed closely by autopsy performance is necessary.
Image 7.

Victim of lake drowning with drying of exposed skin and mold growth (elbow).
Internal Findings
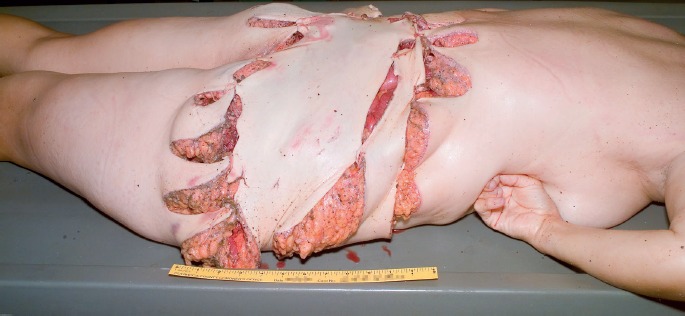
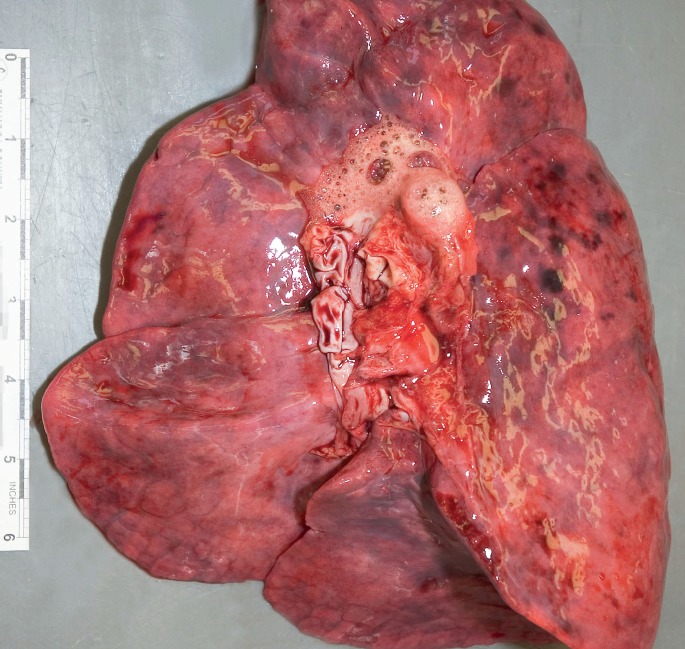
It must be emphasized that there is no one finding that is specific for drowning and all findings commonly associated with drowning must be interpreted within the context of the history and death circumstances. Many findings become less apparent or absent in the setting of significant decomposition, prolonged resuscitative efforts, and an in-hospital interval of survival. Classically, on in situ examination, the lungs will appear voluminous, boggy, and crepitant with apposition or overlapping of the medial edges (Image 8). Transudate fluid in the form pleural effusions may be present. The lung weights typically will be increased with combined weights in excess of 1 kg, without significant differences observed between fresh- and saltwater cases (68, 69). With increased postmortem submersion intervals, inclusive of decompositional changes, decreased lung weights along with increased amounts of pleural fluid have been described (69). As a result of overexpansion with rupture of alveolar capillaries, blotchy areas of hemorrhage (also referred to a Paltauf's spots) may be visible on the pleural surface. Extravasated blood resulting from alveolar capillary rupture is the likely source of the pink or red-tinged froth noted on examination. Typically, copious white, pink, or red froth and fluid exude from the lumen of the sectioned larynx, trachea, and bronchial tubes as well as the cut surfaces of the lung parenchyma (Image 9). The fluid also may be admixed with aquatic debris (Image 10).
Image 8.
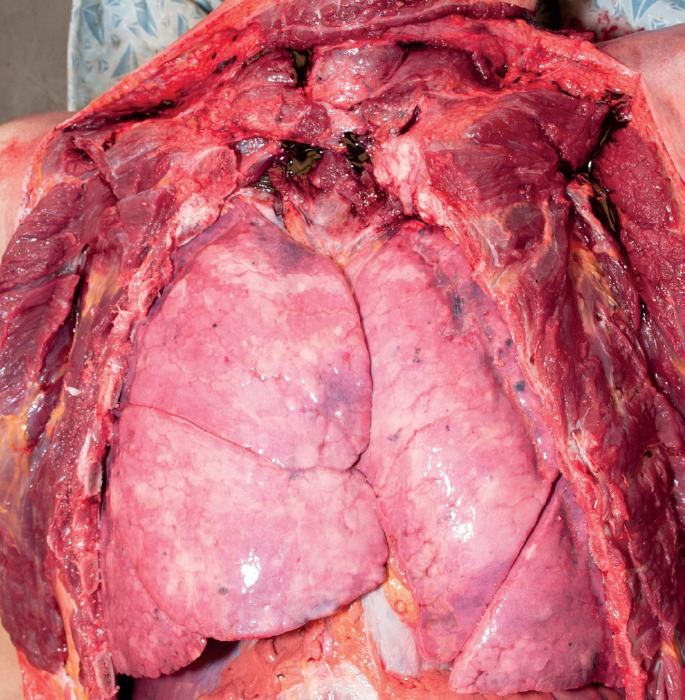
Voluminous lungs with apposition of medial edges.
Image 9.
Pulmonary edema with exudation of bronchial froth. Reproduced with permission of CRC Press (4).
Image 10.
Silt in tracheobronchial tree.
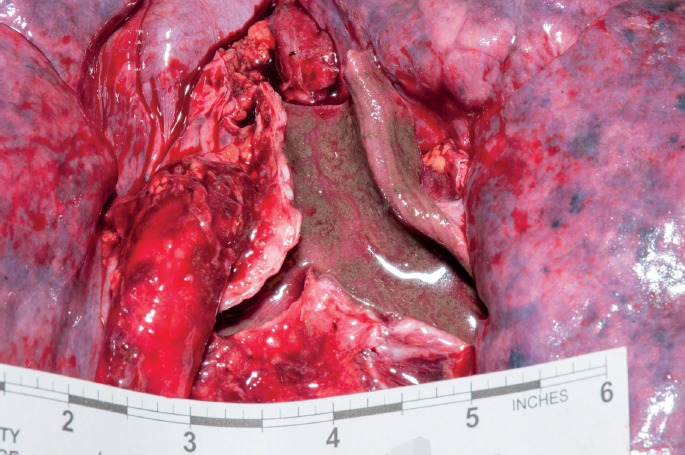
On histological examination of the lungs, intra-alveolar hemorrhagic edema fluid in a patchy or confluent distribution is found and an emphysematous-like alveolar pattern (emphysema aquosum) can be seen (Image 11). Polymorphous aquatic debris such as sand, silt, shell fragments, diatoms, and fragments of aquatic vegetation may also be found (Image 12). Though not scientifically reliable or commonly performed, extractions from lung tissue have been analyzed for the presence of diatoms to assist in the diagnosis of drowning or identification of drowning location with some limitation owing to the widespread domestic, industrial, and environmental distribution and their presence in tissues and organs in persons who have not drowned (70, 71). In near-drownings with an in-hospital survival interval, pink hyaline alveolar membranes representative of ARDS or bronchopneumonia may be noted. Marked dilatation of the right ventricle may be observed. Watery fluid admixed with aquatic debris may be found in the stomach as a result of ingestion during or after the drowning process. In cold water drownings, signs of vital reaction associated with hypothermia may be present including punctate green-black gastric erosions, also known as Wischnewsky's ulcers. Histologically, corresponding mucosal necrosis with hemorrhage and neutrophilic reaction may be seen. Cerebral edema may or may not be present and with prolonged cardiopulmonary arrest followed by resuscitation with an interval of hospital survival there may be histological evidence of neuronal eosinophilia as a manifestation of anoxic-ischemic encephalopathy. Upon brain removal, the petrous ridges may appear dark-red as a result of subcortical congestion with hemorrhage, purportedly as a result of pressure changes in middle ear pressure incurred by a sinking body (72) (Image 13). Five to 10 milliliters of red-tinged watery fluid sometimes admixed with aquatic debris can at times be aspirated from the sphenoid sinus and has been used in quantitative analysis of diatoms to support the diagnosis of drowning (73), though again, this is not commonly performed as water could also enter this area after death (Image 14). The finding of hemolytic intimal staining of the aorta in freshwater drownings is described and an added supportive finding knowing that this finding is also seen in other types of deaths and is a common finding in decomposed bodies (74). Multifocal hemorrhage may be seen in the skeletal muscles of the head, neck, and torso, in addition to the sclerae which, in the absence of other evidence of impact or strangulation injury, has been attributed to hypercontraction during struggling in the initial stages of drowning and elevated venous pressure (75, 76). In acute drowning deaths, the remainder of the viscera and soft tissues will exhibit varying degrees of congestion.
Image 11.
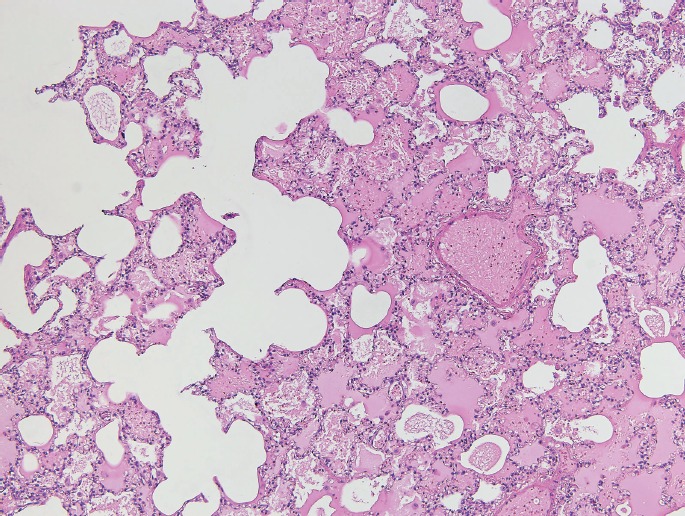
“Emphysema aquosum” and intra-alveolar edema (H&E, x100). Reproduced with permission of CRC Press (4).
Image 12.
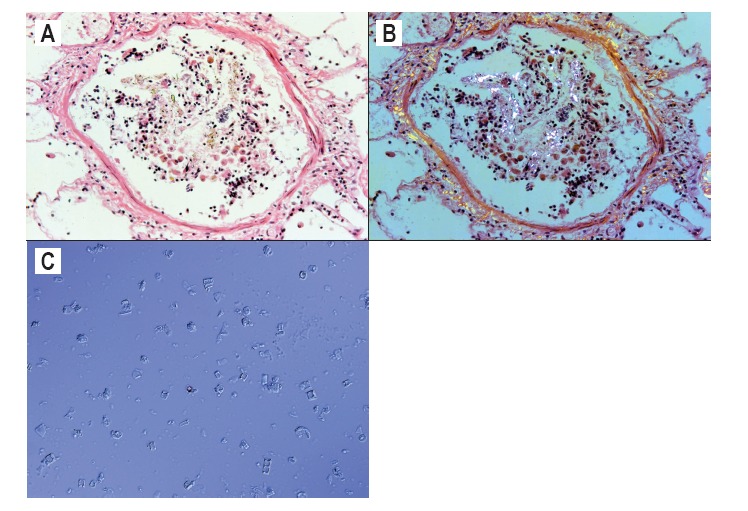
Bronchiole containing polarized aquatic debris, (A, B) (H&E, x400) which may contain diatoms (C) (phase contrast microscopy). Reproduced with permission of CRC Press (4).
Image 13.
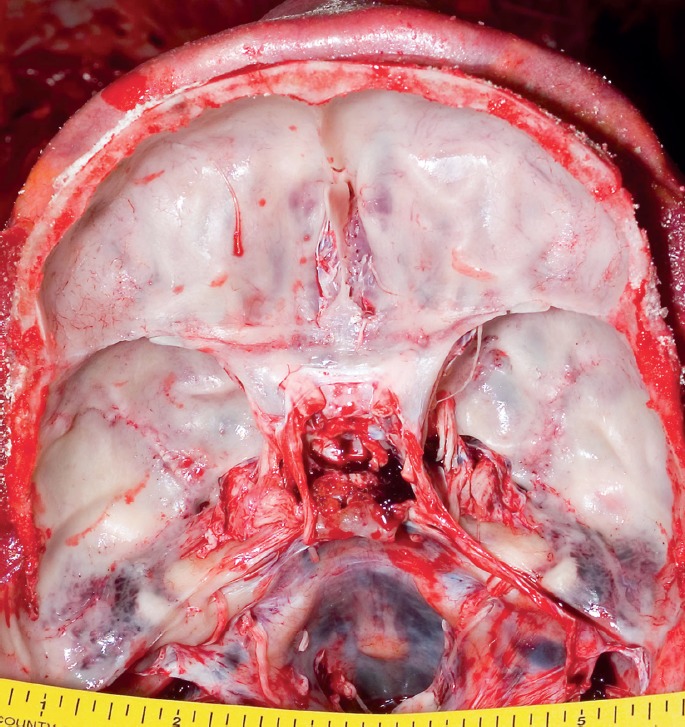
Petrous ridge hemorrhage. Reproduced with permission of CRC Press (4).
Image 14.
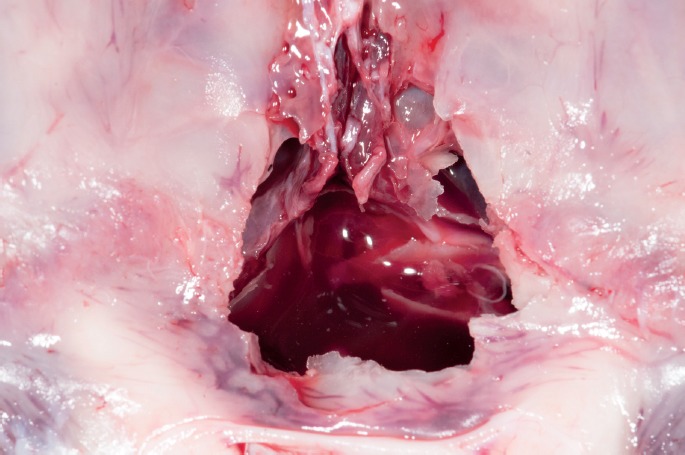
Fluid level in sphenoid sinus of drowning victim.
Injuries of various types resulting from impact with the water surface, bottom surface, fixed or moving objects, predation, or as a result of watercraft and boat collisions may be found and are important to document. Resuscitative injuries are often recognizable by virtue of their location and pattern such as sternal fracture, anterior rib fractures, and tongue and pharyngeal tissue contusions. Tongue contusions and lacerations may also be supportive findings of terminal seizure activity. Determination as to whether the injury(ies) have lethal potential or are contributory as a result of their incapacitating effects is necessary. Similarly, the identification of natural disease entities with obvious lethality (i.e., aortic dissection with hemoperitoneum) or lethal potential (e.g., severe coronary atherosclerosis) sufficient enough to preclude the drowning process (along with absence of supportive findings) has obvious cause and manner of death implications.
Infant/Fetal Deaths
Newborn infants or fetuses recovered from toilets, bathtubs, or other fluid-filled confined spaces may represent death resulting from precipitous delivery and drowning, delivery of a nonviable fetus, or unattended delivery of an otherwise viable infant with unanticipated obstetrical complications. Infant mortality associated with water birth, a method of planned delivery in an aqueous environment to ease maternal delivery, is reported and an additional consideration in the workup (77). Owing to the inherent physical disparity between a caretaker and an infant or small child, child abuse by homicidal drowning or in conjunction with blunt force trauma or asphyxia must be considered (20). Corroboration of findings with any statements given by the mother or other witnesses is necessary for proper interpretation and determination of cause and manner of death (78). The developmental stage in regards to mobility and access to bodies of water, whether in the bathtub, pool, pond, or other environment, becomes particularly relevant in the corroboration of statements. Signs of a recent delivery may be evident at the death scene with finding of items such as bloody garments or towels or finding of the discarded placenta, which should be retrieved. There may exist medical records of recent hospitalization that confirm a recent delivery.
Subsequent to a postmortem radiography, examination for external and internal signs of injury in addition to any supportive signs of drowning is in order. Patterned or clustered injuries, especially blunt force types and especially of the face and neck, are worrisome for inflicted injury inclusive of suffocation and strangulation. Documentation of signs of infection with microbial analysis as necessary, natural disease, and congenital abnormalities along with utilizing anthropometric measurements to assess the degree of maturation is also of importance. The findings of nontraumatic pathology with lethal potential or previability can be helpful in ruling out death by drowning. Signs of maceration signaling intrauterine fetal demise with stillbirth would support a historical account of lack of in utero movement or no movement or respiratory effort upon delivery. Gross and microscopic examination of the placenta and any attached umbilical cord, if available, may reveal pathologies associated with premature delivery such as placental abruption, cord abnormalities, and chorioamnionitis. A pediatric pathologist could be consulted on cases with uncertain placental findings or when there is a need to discern or characterize congenital abnormalities.
Importantly, in cases of a fetus or infant found submerged in confined locations such as the toilet or bathtub, the determination of a live birth, stillbirth, or evidence of resuscitative efforts must be attempted. While many of these indicators are unreliable, determination may be aided by in situ examination of the lungs for inflation versus atelectasis, performance of the hydrostatic or float test on lungs and viscera, or documentation of air in the gastrointestinal system. Underwater birth with death or decompositional changes may preclude or confound this determination, however. The finding of food in the stomach will provide more definitive evidence of an interval of extra-uterine survival. Microscopic examination for signs of aspiration, over/underexpansion of alveoli, pulmonary edema, diffuse alveolar damage, and pneumonia may be helpful in the determination of the periterminal death circumstances including documentation of any evidence of a survival interval. Microscopic examination of a sample of the drowning media with comparison to lung tissue and gastric contents may be helpful for the determination of drowning. Even chemical analysis of the drowning media for comparison with bodily fluids can be done (20). It should be noted, though, that neither of these analyses are performed with any frequency due to unreliability. Histological examination of cutaneous, visceral, or skeletal injuries for signs of inflammation and healing stage may be useful in confirming or refuting statements, documenting repeated physical abuse, or clarifying the timeline of events leading to death.
Special Procedures
Death circumstances or autopsy findings that indicate the possibility of internal injury should prompt application of special dissection techniques. Cases in which barotrauma associated with deep-diving deaths are suspected, such as identifying subcutaneous emphysema or thoracic cavity hypodensities seen on pre-autopsy imaging, warrant examination for gas embolism. This includes subcutaneous dissection of the outer chest wall for the identification of pneumothorax and/or in situ puncture through the right ventricle in the evaluation for intraventricular air, though again these procedures can be difficult to perform and interpret (79). In deaths following diving into shallow water with potential head impact on fixed underwater structures, dissection of the anterior and posterior neck, possibly including in situ examination and removal of the spinal cord, is necessary to look for cervical spine injury including vertebral fracture(s) (especially C5–7), dural-based hemorrhage, and spinal cord contusion (80). Anterior neck dissection should be prompted by the finding of facial petechiae and cutaneous neck injuries in order to document any injuries of the cervical strap muscles, laryngotracheal skeleton, or hyoid bone that indicate anterolateral neck compression caused by ligature of manual strangulation. Dissection of the sinoatrial and atrioventricular nodal tissues should be performed at least for retention and otherwise for histological examination especially in an unexplained drowning such as that involving an experienced swimmer or an autopsy lacking findings of lethality (81). Retention with archival storage of heart muscle and whole blood samples are necessary in drowning deaths that are unexplained, have a decedent or family history of syncope or arrhythmia, or a family history of sudden unexplained death, in anticipation of submission for genetic analysis for cardiac channelopathies as mutations have been identified (82).
Postmortem Toxicological Testing
Ancillary testing of bodily fluids and, sometimes by necessity, tissues is imperative in all water-related deaths. Vitreous fluid, blood (central and peripheral), gastric fluid, urine, skeletal muscle, visceral, adipose tissue, sequestered hematomas, and even body hair are all candidates for submission and analysis. The choice of matrices will be limited or suboptimal in cases with prolonged submersion and decomposition, but even with these limitations, qualitative or quantitative results are possible (83). Toxicological analysis of adipocere has yielded useful results (63). In the instance of an empty urinary bladder encountered at autopsy, sterile water can be instilled into the bladder and the resulting fluid from the “bladder wash” can be submitted for qualitative testing.
Evaluation of the causative or contributory effects of drugs and medication levels requires interpretation within the context of the death circumstances and decedent's history. The finding of certain drugs and medications can give insight into the decedent's medical history, psychiatric history, drug use history, degree of impairment around the time of death, and assist in the reconstruction of events leading to the death and is particularly relevant in cases in which the decedent's history is unknown (84). The absence of certain medications in persons with known medical history and a prescribed therapeutic regimen can be just as revealing, such as in the case of the history of seizures with subtherapeutic or negative results found on testing. Depending on the drug or medication in question and its end-organ effects, the concentration may be sufficient to preclude the drowning process with few or absent supportive findings of drowning noted at autopsy. In multidrug intoxications, the cumulative or synergistic effects and any propensity to precipitate drowning must be considered, such as sedation causing impairment to a degree that prevents extrication from or leads to collapse with submersion into a watery environment. Ethanol, with its physiological and psychological effects, is the most common drug found in drownings, particularly accidental cases (10, 85). While interpretation of the degree of ethanol impairment may be difficult in bodies submerged for prolonged periods due to the dilutional effect of water on bodily fluids and/or the confounding effects of postmortem ethanol production, analysis of urine for the presence of ethyl glucuronide has been found to be useful in the differentiation between antemortem ingestion and postmortem production of ethanol (86). Ethanol and certain medications are associated with prolongation of the QT interval and when combined with extended breath holding during swimming, may trigger an incapacitating arrhythmia and precipitate drowning (87).
Comprehensive quantitative and qualitative testing should include ethanol, illicit drugs, and commonly prescribed medications with as needed use of reference laboratories for testing for less common substances. If available, admission blood and urine samples should be promptly obtained in near-drowning cases as any results would be representative of concentrations around the time of death. Carbon monoxide testing must be requested in drowning deaths associated with use of SCUBA equipment or cases involving possible inhalation of exhaust from motorized watercraft.
Special Tests for Drowning
With the knowledge that drowning fluid diffuses across the alveolar-capillary membrane and into the blood with active circulation during the drowning process, various tests have been developed in attempts to quantify a number of diffused substances in order to aid in the diagnosis of drowning. While studies utilizing these tests abound, efforts to develop a single, validated, widely available, cost-efficient, and timely diagnostic test that is highly reliable, sensitive, and specific for drowning, particularly in cases of prolonged submersion and decomposition, are ongoing. Such a test would be of immense value as it could help differentiate deaths due to drowning versus those caused by other means followed by dumping of the body into a body of water for concealment in order to mimic the appearance of an accidental drowning. Therefore, currently, the diagnosis of drowning is one that is based largely on accrued supportive autopsy findings with the exclusion of other causes of death, interpreted within the context of features of the death circumstances. Moreover, a reliable test that consistently and reliably differentiates freshwater from saltwater drowning remains elusive, which otherwise could be of importance for confirming the drowning location. Prolonged submersion with decomposition adds another dimension of diagnostic difficulty (88).
Historically, tests such as those that measured ocular fluid electrolyte levels, measured and compared serum chloride concentrations in the cardiac chambers (i.e., Gettler test), or measured and compared plasma specific gravity in the cardiac chambers were devised in attempts to diagnose and differentiate fresh from saltwater drowning with inconsistent and unreliable results (89–92). Hemodilution tests that identify lowered levels of certain blood proteins have likewise been found to have limited applicability, being potentially useful only in those drowning deaths with a short post-recovery interval and not useful in deaths associated with prolonged PMSI or interim resuscitation followed by a survival interval (93, 94). Owing to the higher concentrations of magnesium and strontium in salt- and brackish waters, investigations into the measurement of these markers in cardiac blood to aid in the diagnosis of saltwater drowning have identified differences; however, investigators caution that contextual interpretation such as comparison of the measured constituents of the actual drowning medium or consideration of potential of nondrowning related exposure is warranted (94, 95).
More recent efforts to develop tests applicable in or supportive to the diagnosis of drowning for the differentiation between fresh- and saltwater drowning have focused on identifying drowning-associated alterations at the molecular level or microorganisms unique to certain drowning environments. These include analyses of electrolyte and protein concentrations in pleural effusions and sphenoid sinus fluid, measurement of pulmonary surfactant protein expression, measurement of aquaporin tissue expression, and genomic identification of waterborne bacteria in tissue samples (96–99).
Forensic limnology is the science that examines the presence of diatoms in crime scene, suspect, and victim samples with application in the resolution of crimes (100). Continued focus via experimental study and casework application has been on the utility of diatom examination in the diagnosis of drowning. Researchers are careful to remind investigators of the importance of interpretive context of results and recognition of limitations including low abundance in certain natural bodies of water giving rise to low/negative tissue levels, positive findings in individuals who have not drowned or have not been submerged, positive findings in individuals that have not drowned but have been submerged for prolonged periods, and methodological limitations of extraction from samples (101). Diatoms are also known for their ubiquitous nature being found in natural bodies of water, soils, and even tree bark and can also enter lung tissue passively during prolonged submersion. Furthermore, certain diatom species are unique to freshwater and saltwater environments with concentrations affected by conditions inherent in the water, which could have direct bearing on interpretation regarding drowning location (102). Contamination leading to false positives for the presence of diatoms that could lead to a misdiagnosis also remains one of the issues of concern cited by researchers (70). With the development of more streamlined extraction methods with shorter turnaround-times and overall higher sensitivity and specificity, the successful recovery of diatoms from a variety of tissues and fluids (lung, liver, kidney, bone marrow, and cavity fluid) along with comparison to that found in the drowning medium has been shown to be an occasionally useful adjunct to not only the diagnosis of drowning but also in the ruling out of drowning as the cause of death (70, 71, 103, 104). That being said, due to the various difficulties discussed, diatom examination is not considered standard of practice when investigating potential water-related deaths.
Conclusion
While the tendency to presume that a water-related death has occurred as a result of a drowning, by accident or other means, a comprehensive investigation must be performed to ensure accurate death certification while also unearthing any criminality. Multidisciplinary and multiagency efforts are required for the gathering of vital pre-autopsy information, which provide context within which the forensic pathologist can interpret autopsy and toxicological findings. When considering the possibility of a drowning, a thorough medicolegal/forensic autopsy must follow in order to rule out other possible causes of death before one can feel confident the death was due to drowning. The ramifications of our conclusions regarding water-related deaths are far-reaching affecting decisions that ultimately affect the health, safety, and well-being of the public.
Acknowledgements
The authors would like to thank forensic photographers Ms. Kate Snyder and Ms. Amy Koons for for-matting and acquisition of images.
Appendix 1. Investigative Duties of Select Scene Types
Common death scenes encountered by first responders include bathrooms, pools, and various natural bodies of water. Death circumstances may also involve watercraft, safety gear, or underwater breathing gear. The approach to the investigation will be dictated by the characteristics of the environment such as that involving cold water submersion. A brief discussion from the perspective a master water-related death investigator follows (1, 2).
Sinks and Bathtubs
Upon the initial discovery of a body in a bathtub or sink, the investigator acts quickly to document evidence that may soon become absent or impossible to collect. Examples of this type of evidence may include documenting if the floor, counter top, sink area, or any immediate surface near the body is wet. Often times, suspects will claim attempts to rescue the victim in an attempt to hide the fact that they committed a crime or in some way played a part in the victim's death. A wet floor, for example, in a bathtub drowning may soon become trampled upon by investigating personnel as well as personnel from the medical examiner's/coroner's (ME/C) office removing the body from the scene. Alternatively, an extremely warm home environment may cause water of the surrounding area to dry before it can be documented. It is also important for the investigator to document the ambient temperature of the room. This may be used later to determine if a wet floor, for example, dried before the body was located. It is perfectly natural for a person finding a submerged body in a sink, and more likely in a bathtub, to instinctively pull the plug and drain the tub or sink. This act should not immediately influence the investigator to believe that an individual is trying to hide or destroy evidence of a crime. However, it is imperative that the investigator makes an effort to collect the fluid which has been drained. A sample can be collected if any still remains in the tub or sink. If not, simply use a bulb syringe to collect a sample from the drain trap. Lab analysis may be needed to determine if a witness claims to have been bathing the victim, only to find that the water sample does not contain soap, urine, mucus, etc. If water is still present, its appearance as well as depth needs to be documented. Appearance documentation may include whether soap suds, soap scum, blood, or any other detectable substance such as petroleum products were present. Also, in cases of bathtub drowning, documentation of the area surrounding the tub may include the presence of regular bathing products such as wash rags, towels, toys, and bottles of shampoo or body soap. Any electrical devices near the area must also be documented and collected. Accidental electrocution by a falling hair dryer, curling iron, or radio may be the cause of or a contributing factor to the death. The water temperature must be checked as well. An extremely high temperature, even after a time delay in emergency personnel response, may indicate scalding torture or skin burns, whereas a cold temperature may indicate a delayed call for help. A cursory search of the home should include a search for indicators that the scene was cleaned up. Some of these items may include a bucket and mop, wet towels in the hamper or dryer, cleaning agents uncapped and nearby, etc. Finally, a detailed sketch of the interior of the home must be completed. This will prove to be invaluable when attempting to determine the accuracy of the statement obtained by the reporting person. For example, the mother claims she was in the kitchen when she saw her daughter fall in the tub. The drawing will be able to determine if, in fact, she was able to see her daughter fall in the tub from the kitchen, or was there an obstacle, or wall in the way, preventing this observation.
Natural Bodies of Water
Most likely, if a jurisdiction has any type of natural bodies of water, that agency will be challenged with a drowning incident. It is important to learn about these bodies of water before an incident occurs. Water depth, clarity, seasonal averages of temperature, surface and submerged hazards are just some of the complexities an investigator may need to contend with at the scene of a water incident. It is important for responding personnel to be familiar with techniques used to locate a missing person in these bodies of water. Unnecessary delays can make the difference between a rescue and recovery. The last-seen point of a missing person is important to establish so rescue personnel can begin a hasty search of the area, retrieve the victim, and commence rescue efforts. Responding personnel need to interview as many witnesses as possible from different points of the area. The further apart witnesses are, the better chance of determining a last seen point. This is because triangulation from two to three witnesses will establish not only the general area in which the missing person was seen, but a distance from shore. It is of the utmost importance to have would-be witnesses lead personnel to the water's edge and physically point to the last seen point. Also, a professional rescuer such as a diver or lifeguard can be placed in the water and the witness can direct that person to the last seen point. Many times, I have seen department personnel interview a witness, leave that witness to attempt to locate the missing person, and never make contact with the witness again. Body drop rates are also a very important “tool” to use when attempting to locate a missing person in moving water. In any moving water incident, it is imperative the personnel conduct a simple test, as soon as possible, to determine current speed. This is needed to help locate the missing person. Current speed can change so again it is important that it be done as soon as possible. To determine current speed, drop a floating object in the water and measure how far it travels in one minute. If it travels 100 feet in one minute, the current speed is one knot. Two hundred feet in one-minute equals two knots, etc. In fresh water, a body drops approximately 2 feet per second. In salt water, 1.5 feet. For this example, let's say the freshwater depth is 20 feet and the current speed is 2 knots. 1) Convert the current speed to a fraction: 200 feet divided by 60 seconds=3.33 seconds. 2) Locate the last seen point based on eye witness accounts, evidence, etc. 3) Determine the water depth. In this example, we will use 20 feet. Calculate drop time in seconds (20 feet divided by 2 feet rate for fresh water=10 seconds). 4) Multiply drop time by the current (3.3 × 10=33 feet). In this example, a body leaving the surface in a two-knot current in 20 feet of water should be located 33 feet from the last seen point. If it is not located there, then either your last seen point is inaccurate or witness accounts of what took place are inaccurate. It is the duty of the investigator involved to determine which of these applies. In nonmoving water such as a pond, lake, or pool, a body sinking in a water column will generally not move horizontally any further than one foot for each foot of depth. So, if the water is 30 feet deep, the body will most often be located within a 30-foot radius of the last seen point (3). There are other means often used to locate a missing person in bodies of water such as side scan sonar, submersible hand-held sonar for divers, and controlled sweep patterns for divers, all of which require special training and lots of practice to become efficient in their use.
Pools
According to the National Safe Kids campaign (4), a swimming pool is 14 times more likely than a motor vehicle to be involved in the death of a child four years old and under. The investigators first actions should entail documenting the location and position of the body, if it is still on scene. If the body has already been removed from the scene, the location found needs to be determined through extensive witness interviewing. Other important observations will include determining if there is any indication of a delayed call for rescue personnel. If the complainant states they pulled the child out of the water and began cardiopulmonary resuscitation, the pool sides or pool deck may be wet. Likewise, the would-be rescuers clothes may be wet. As in any drowning incident, it is imperative the investigator determine the accuracy of information obtained on scene. Does the evidence on scene support or contradict witness statements? Additional documentation includes recording ambient and water temperature, collection of water samples, examination and seizure of clothing worn by decedent, assessment of evidence of clean up (towels, mops, buckets), and scene sketch. Photographs of the scene and any barriers placed for the purpose of restricting access to the pool are essential. Recordings from poolside audiovisual equipment such as security cameras should be obtained with a copy sent to the ME/C.
Hotel, school, and recreation center pools are larger and most often indoors and present additional circumstances the investigator needs to be aware of when conducting an investigation in this type of environment. Unlike outdoor backyard pools, these pools have a variety of different circumstances that may hinder visibility, safety, and judgment of those who are using them. All these circumstances must be considered when drawing conclusions regarding a drowning incident. Documentation should include location and positioning of lighting, presence of lifeguards, normal hours of operation, and number of swimmers permitted. During the interviewing of witnesses, it is important to use the “Show Me” technique by leading any potential witnesses through their actions, starting with what they were doing just before the incident and leading them through what they did during the incident. This will establish positioning of the witness, which may expose potential problems in determining what they could or could not see. In some instances, a reenactment may be warranted to clarify information or resolve questions that remain unanswered, such as “Why didn't anyone see the victim at the bottom of the pool?” In this instance, the investigator should obtain a rescue manikin or other object that can be used to show the victims position and location. The manikin or other object should resemble the victim's description as close as possible to allow for the most accurate assessment. Place the manikin in the position in which the decedent was located and have each potential witness stand where they were at the time the incident occurred. Many will be surprised at how difficult it can be to see a body at the bottom of a swimming pool, even in the best of conditions.
Boating Fatalities
Vessels involved in a watercraft fatality pose many challenges for the investigator. Injuries to any victims will usually be caused by a collision or propellers. Collision injuries need to be documented as thoroughly as possible and consultation with a forensic pathologist may be necessary. This is because pre-accident injuries may also be present and the investigator will need to determine when these injuries occurred. Post-accident injuries will be the result of the body striking an object or an object striking the victim. This is also the reason it is very important to document damage to the vessel. Does the injury match the damage? Is damage present that could have caused a head injury, for example? If not, the investigator needs to find out who and what caused those injuries. Propeller injury will usually be easier to determine when it has occurred in the antemortem period. Propeller injuries will most likely be located below the waist and along the extremities but can be also be found on the head and torso. This is because when a person is in the water, the body is usually vertical and the legs are submerged, where propellers can cause these injuries. If the propeller damage is located along the back, then they typically are postmortem injuries. When floating, bodies typically assume a face- and extremities-down position, with the back exposed to the surface. A passing boat would then cause injuries to the back. Propeller injuries will appear as multiple and parallel chop wounds. Faster, high-speed boats will cause shallower injuries and the lacerations will be close together. Larger, slower vessels will cause deeper penetrating injuries that are further apart. The type of propeller injuries can help an investigator build a description of a possible involved vessel that left the scene.
Much like diving fatalities, boating-related fatalities also require the testing of any safety equipment involved to assure that it did not play a part in the fatality. Inspection of any personal flotation devices (PFDs) or life jackets used will include checking to make sure they are US Coast Guard approved, checking the size to make sure it was a proper fit for the victim, the condition for rips or worn or broken straps and buckles, the buoyancy of the material which must not be crushed or deteriorated, and for evidence of any non-factory alterations.
A fatal boating accident can present many challenges for the investigator. Establishment of physical contact between two or more vessels, vessel to person, or vessel to a stationary object must be determined. The most reliable evidence of contact is material transfer. Some examples of material transfer include: human tissue, hair, paint, skin, and blood which must be properly collected and submitted following established chain-of-custody procedures as must be done with recovery of any type of evidence.
Diving Fatalities
Generally speaking, many SCUBA fatalities can be attributed to diver panic and lack of training. In order to come to this conclusion, it is important to remember that all equipment used by a diver must be tested to assure it was working properly at the time of the death. Therefore, it is highly recommended that an investigating agency seek assistance from a reputable organization in testing this equipment. Due to the special knowledge involved in SCUBA equipment, testing procedures will not be covered in this article. However, there are several common factors in SCUBA fatalities: there is usually sufficient air left in the tank, there is very little air contained in the buoyancy control device (BCD), the weight belt is still worn which divers are trained to remove (drop) in an emergency, inspection of equipment such as the regulator and the BCD fail to reveal any flaws or malfunctions and was worn correctly, and the air quality in the SCUBA tank is well within safety limits. Considering all these factors, one can conclude that diving fatalities are usually caused by panic (5).
Cold Water
Cold water drowning is often the result of hypothermia, in which the victim's body temperature drops drastically, affecting their motor skills and normal thought process. In ice drowning incidents, this is very common. The victim may survive the initial submergence in water or under the ice, but suffer from the effects of hypothermia and can no longer hold on to the ice shelf or assist would-be rescuers in their rescue. Hazards to consider during rescue/recovery efforts include hypothermia in rescue personnel, overhead environment dangers such as ice or surface debris, and entanglement. It is important for responding rescue personnel to remember that cold water immersion can slow the effects of drowning in young children. This phenomenon is believed to be due in part to the mammalian dive reflex and there have been documented cases of a full recovery by victims in excess of one hour. Therefore, every effort must be taken to remain diligent in rescue efforts until the victim reaches a medical facility.
Electrical Hazards
This type of hazard can lead to multiple victims in one incident. This happens when one person becomes incapacitated by the effects of electrical shock and would-be rescuers jump into the body of water to save them and similarly experience cardiac arrest from electrocution or respiratory paralysis brought on by the electrical current. Causes may include faulty wiring of submerged lighting; underwater pool lighting that lack ground fault circuit interrupters (GFCI); or appliances such as radios, televisions, or hair dryers plugged into outlets lacking GFCIs that fall into water. No external burns will be evident for an in-water electrocution.
Complicated and Unusual Sites of Recovery
Investigators should be familiar with these types of complicated recovery sites within their jurisdictional boundaries and formulate standard operating procedures for each. Settling tanks, for instance, in a sewage treatment plant pose a challenge for recovery personnel, which may include visibility hazards, mechanical hazards, health hazards, and liability. Special training is required to enable a safe and effective recovery from this type of environment. Submerged vehicle hazards include entanglement or entrapment for recovery divers, location and recovery of any persons inside, and documentation of the scene. Every effort should be made to determine the location of each victim within the vehicle. It is important to remember that a submerged vehicle with occupants is a crime scene, so diligence must be taken to preserve evidence inside the vehicle. Documentation of interior and exterior evidence, such as damage, should be done prior to removing the vehicle from the water. This is because in many cases the vehicle will be damaged in the recovery process. Having divers close any windows prior to removal from the water will help eliminate evidence loss.
Body Assessment
Every body recovered from water requires an on-scene assessment by a trained investigator. This on-scene assessment needs to be done as soon as possible because much of the observations that will be recorded will change drastically as time passes, resulting in less accurate information. Red flag indicators of foul play may be noted, which will alert the investigator to take further actions with witnesses and the reporting person, possible suspects, and evidence. Often, during recovery efforts, wounds result from recovery over rough terrain, so documenting them prior to moving the body is essential.
The assessment should be conducted by an investigator using new, unused protective latex or rubber gloves. Care must be taken not to disturb on-body evidence or make worse any injury, which could lead to erroneous conclusions. The investigator starts in the head region, checking all areas of the head, behind the ears, in the eyes, etc. before moving on to the trunk and extremities, taking care not to disturb any on-body evidence. Changes in the eyes may include tache noire and corneal opacity (possibly indicating the body was deceased before entering the water) and petechial hemorrhages (an indicator of possible strangulation). External abrasions of the skin may be indicative of postmortem traveling of the body. As gases build up in the body cavities and organs, the body becomes buoyant. When it becomes buoyant enough to lift off the bottom, current and wave action cause it to move. This movement causes certain areas of the face, hands, and feet to scrape along the bottom, causing trauma. Another observation, which will be more obvious to the investigator, is a foam column. It appears as a mixture of water, air from the lungs, pulmonary edema, and sometimes blood, and may have the consistency of meringue. The feet and hands often appear pale and wrinkled. The degree and stage of rigor mortis should be documented. This observation may assist the pathologist in determining a time of death. The appearance and location of livor mortis should also be noted, and it may not be apparent in some cases in which the body encountered constant water pressure while submerged.
Injuries may also result from feeding by aquatic animals including but not limited to larva, fish, crabs, turtles, and various types of large sea life such as sharks. Injuries from feeding by smaller animals often will appear as chewing marks on the tip of the nose, lips, finger tips, toes, and ears. Any presence of maggots, especially in submerged parts of the body, should raise questions regarding its place of death or brief periods of exposure to air, such as during low tide. These can be collected and preserved according to protocol or at the direction of an entomologist for possible future analysis. The life stage of the maggot can be examined by an entomologist to determine how old they are. A lab technician can process them to determine the presence of many drugs, medications, and chemicals that may no longer be present in the blood. All these observations and findings must be recorded with as much accuracy as possible. Many of these observations will not be present a day or two later when the postmortem exam is conducted, so any of this information included helps the pathologist drastically with any final interpretations and findings.
The use of a body recovery checklist and body diagrams will assist in documenting the location of wounding. The appearance of the wounds can be drawn directly onto the diagram with a small notation beside it. Injuries will be documented in greater detail at the time of the autopsy.
Footnotes
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
FINANCIAL DISCLOSURE The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
References
- 1).World Health Organization [Internet]. Geneva: World Health Organization; c2017. Drowning fact sheet; 2017. May [cited 2017 Dec 1]. Available from: http://www.who.int/mediacentre/factsheets/fs347/en/. [Google Scholar]
- 2).Centers for Disease Control and Prevention [Internet]. Atlanta: US Department of Health & Human Services; c2017. Unintentional drowning deaths in the United States, 1999–2010; [cited 2017 Dec 1]. Available from: https://www.cdc.gov/nchs/data/databriefs/db149.htm. [Google Scholar]
- 3).Erskine K.L. Water-related death investigation: practical methods and forensic applications. 1st ed. Boca Raton: CRC Press; c2011. Chapter 2, Investigative duties on scene; p. 27–108. [Google Scholar]
- 4).Erskine K.L. Water-related death investigation: practical methods and forensic applications. 1st ed. Boca Raton: CRC Press; c2011. Chapter 3, On-scene body assessment; p. 109–132. [Google Scholar]
- 5).Merriam-Webster's collegiate dictionary. 10th ed. Springfield (MA): Merriam-Webster; 1997. 1600 p. [Google Scholar]
- 6).Dorland's Illustrated Medical Dictionary. 27th ed. Philadelphia: WB Saunders; 1988. 1888 p. [Google Scholar]
- 7).Final recommendations of the world congress on drowning: Amsterdam 26–28 June 2002 [Internet]. Huntington Beach (CA): California Surf Lifesaving Association; 2002. [cited 2017 Dec 1]. 11 p. Available from: http://ww.cslsa.org/events/ArchiveAttachments/Spr03Minutes/AttachmentG2.pdf. [Google Scholar]
- 8).Armstrong E.J. Water-related death investigation: practical methods and forensic applications. 1st ed. Boca Raton: CRC Press; c2011. Chapter 1, Introduction; p. 1–26. [Google Scholar]
- 9).Zuckerman G.B., Conway E.E. Drowning and near drowning: a pediatric epidemic. Pediatr Ann. 2000. Jun; 29(6): 360–6. PMID: 10868432. 10.3928/0090-4481-20000601-09. [DOI] [PubMed] [Google Scholar]
- 10).Lunetta P., Smith G.S., Penttilä A., Sajantila A. Unintentional drowning in Finland 1970–2000: a population-based study. Int J Epidemiol. 2004. Oct; 33(5): 1053–63. PMID: 15218012. 10.1093/ije/dyh194. [DOI] [PubMed] [Google Scholar]
- 11).Ten leading causes of injury deaths by age group highlighting unintentional injury deaths, United States-2015. Atlanta: US Department of Health & Human Services; c2017. 1 p. Available from: https://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_injury_deaths_highlighting_unintentional_injury_2015-a.pdf. [Google Scholar]
- 12).Byard R.W., Houldsworth G., James R.A., Gilbert J.D. Characteristic features of suicidal drowning-A 20-year study. Am J Forensic Med Pathol. 2001. Jun; 22(2): 134–8. PMID: 11394746. 10.1097/00000433-200106000-00005. [DOI] [PubMed] [Google Scholar]
- 13).Copeland A.R. Suicide by drowning. Am J Forensic Med Pathol. 1987. Mar; 8(1): 18–22. PMID: 3578200. 10.1097/00000433-198703000-00005. [DOI] [PubMed] [Google Scholar]
- 14).Davis L.G. Suicidal drowning in South Florida. J Forensic Sci. 1999. Sep; 44(5): 902–5. PMID: 10486938. 10.1520/jfs12013j. [DOI] [PubMed] [Google Scholar]
- 15).Avis S.P. Suicidal drowning. J Forensic Sci. 1993. Nov; 38(6): 1422–6. PMID: 8263484. 10.1520/jfs13546j. [DOI] [PubMed] [Google Scholar]
- 16).Wirthwein D.P., Barnard J.J., Prahlow J.A. Suicide by drowning: a 20-year review. J Forensic Sci. 2002. Jan; 47(1): 131–6. PMID: 12064640. 10.1520/jfs15213j. [DOI] [PubMed] [Google Scholar]
- 17).Ahlm K., Saveman B.I., Bjornstig U. Drowning deaths in Sweden with emphasis on the presence of alcohol and drugs - a retrospective study, 1992–2009. BMC Public Health. 2013. Mar 11; 13: 216 PMID: 23497055. 10.1186/1471-2458-13-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Fisher L.B., Overholser J.C., Dieter L. Methods of committing suicide among 2,347 people in Ohio. Death Stud. 2015. Jan-Jun; 39(1-5): 39–43. PMID: 24932592. 10.1080/07481187.2013.851130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Schmidt P., Madea B. Homicide in bathtub. Forensic Sci Int. 1995. Mar 31; 72(2): 135–46. PMID: 7750869. 10.1016/0379-0738(95)01695-f. [DOI] [PubMed] [Google Scholar]
- 20).Griest K.J., Zumwalt R.E. Child abuse by drowning. Pediatrics. 1989. Jan; 83(1): 41–6. PMID: 2909975. [PubMed] [Google Scholar]
- 21).DiMaio V.J. Homicidal asphyxia. Am J Forensic Med Pathol. 2000. Mar; 21(1): 1–4. PMID: 10739219. [DOI] [PubMed] [Google Scholar]
- 22).Geertinger P., Voigt J. Death in the bath. A survey of bathtub deaths in Copenhagen, Denmark, and Gothenburg, Sweden, from 1961 to 1969. J Forensic Med. 1970. Oct-Dec; 17(4): 136–47. PMID: 4250437. [PubMed] [Google Scholar]
- 23).Somers G.R., Chiasson D.A., Smith C.R. Pediatric drowning: a 20-year review of autopsied cases: II. Pathologic features. Am J Forensic Med Pathol. 2006. Mar; 27(1): 20–4. 10.1097/01.paf.0000201103.67465.6a. [DOI] [PubMed] [Google Scholar]
- 24).Nixon J., Pearn J. Non-accidental immersion in bathwater: another aspect of child abuse. Br Med J. 1977. Jan 29; 1(6056): 271–2. PMID: 837067. 10.1136/bmj.1.6056.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Copeland A.R. Homicidal drowning. Forensic Sci Int. 1986. Jul 31; 31(4): 247–52. PMID: 3744216. 10.1016/0379-0738(86)90163-5. [DOI] [PubMed] [Google Scholar]
- 26).Modell J.H., Bellefluer M., Davis J.H. Drowning without aspiration: is this an appropriate diagnosis? J Forensic Sci. 1999. Nov; 44(6): 1119–23. PMID: 10582353. 10.1520/jfs14580j. [DOI] [PubMed] [Google Scholar]
- 27).Pearn J. Pathophysiology of drowning. Med J Aust. 1985. May 27; 142(11): 586–8. PMID: 4000018. [DOI] [PubMed] [Google Scholar]
- 28).Bierens JJLM, Lunetta P., Tipton M., Warner D.S. Physiology of drowning: a review. Physiology (Bethesda). 2016. Mar; 31(2): 147–66. PMID: 26889019. 10.1152/physiol.00002.2015. [DOI] [PubMed] [Google Scholar]
- 29).Orlowski J.P., Szpilman D. Drowning. Rescue, resuscitation, and reanimation. Pediatr Clin North Am. 2001. Jun; 48(3): 627–46. PMID: 11411297. [DOI] [PubMed] [Google Scholar]
- 30).Modell J.H., Davis J.H. Electrolyte changes in human drowning victims. Anesthesiology. 1969. Apr; 30(4): 414–20. PMID: 5773952. 10.1097/00000542-196904000-00011. [DOI] [PubMed] [Google Scholar]
- 31).Layon A.J., Modell J.H. Drowning: Update 2009. Anesthesiology. 2009. Jun; 110(6): 1390–401. PMID: 19417599. 10.1097/aln.0b013e3181a4c3b8. [DOI] [PubMed] [Google Scholar]
- 32).Modell J.H. The pathophysiology and treatment of drowning and near-drowning. Springfield (IL): Charles C. Thomas; 1971. 119 p. [Google Scholar]
- 33).Cantwell G.P., Verive M.J. Medscape [Internet]. New York: WebMD LLC; c2017. Drowning; 2017 May 18 [cited 2017 Dec 1]. Available from: http://emedicine.medscape.com/article/772753-overview. [Google Scholar]
- 34).Handbook on drowning: prevention, rescue, treatment. 1st ed. Berlin: Springer Verlag; 2006. 713 p. [Google Scholar]
- 35).Orolowski J.P., Abulleil M.M., Phillips J.M. The hemodynamic and cardiovascular effects of near-drowning in hypotonic, isotonic, or hypertonic solutions. Ann Emerg Med. 1989. Oct; 18(10): 1044–9. PMID: 2802278. 10.1016/s0196-0644(89)80927-8. [DOI] [PubMed] [Google Scholar]
- 36).Orolowski J.P. Drowning, near-drowning, and ice-water submersion. Pediatr Clin North Am. 1987. Feb; 34(1): 75–92. PMID: 3543828. 10.1016/s0031-3955(16)36182-x. [DOI] [PubMed] [Google Scholar]
- 37).Edwards N.D., Timmins A.C., Randalls B. et al. Survival in adults after cardiac arrest due to drowning. Intensive Care Med. 1990; 16(5): 336–7. PMID: 2212263. 10.1007/bf01706363. [DOI] [PubMed] [Google Scholar]
- 38).Hussain I.R., Edenborough F.P., Wilson R.S., Stableforth D.E. Severe lipoid pneumonia following attempted suicide by mineral oil immersion. Thorax. 1996. Jun; 51(6): 652–3; discussion 656–7. PMID: 8693453. 10.1136/thx.51.6.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39).Talwar V., Sood N., Verma P.K. Drowning in concentrated syrup. Indian Pediatr. 2009. Apr; 46(4): 352–3. PMID: 19383994. [PubMed] [Google Scholar]
- 40).Spagnolo E.V., Mondello C., Cardia L., Cardia G. Peculiar and unusual drowning in waste oil from motor vehicles: case report. J Forensic Res. 2016. Sep 30; 7(4): 1–2. 10.4172/2157-7145.1000335. [DOI] [Google Scholar]
- 41).Davis J.H. Bodies found in the water. An investigative approach. Am J Forensic Med Pathol. 1986. Dec; 7(4): 291–7. PMID: 3799560. 10.1097/00000433-198612000-00005. [DOI] [PubMed] [Google Scholar]
- 42).Ellingham S.T.D., Perich P., Tidball-Binz M. The fate of human remains in maritime context and feasibility for forensic humanitarian action to assist in their recovery and identification. Forensic Sci Int. 2017. Oct; 279: 229–234. PMID: 28934682. 10.1016/j.forsciint.2017.07.039. [DOI] [PubMed] [Google Scholar]
- 43).D'Ovidio C., Rosato E., Carnevale A. An unusual case of murder-suicide: The importance of studying knots. J Forensic Leg Med. 2017. Jan; 45: 17–20. PMID: 27865156. 10.1016/j.jflm.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 44).Todt M., Ast F., Wolff-Maras R. et al. Suicide by drowning: A forensic challenge. Forensic Sci Int. 2014. Jul; 240: e22–4. PMID: 24793320. 10.1016/j.forsciint.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 45).Sweet J., Shutler G.G. Analysis of salivary DNA evidence from a bite mark on a body submerged in water. J Forensic Sci. 1999. Sep; 44(5): 1069–72. PMID: 10486961. 10.1520/jfs12045j. [DOI] [PubMed] [Google Scholar]
- 46).Borde Y.M., Tonnany M.B., Champod C. Study on the effects of immersion in river water and seawater on blood, saliva, and sperm placed on objects mimicking crime scene exibits. Can Soc Forensic Sci J. 2008. Jan; 41(3): 149–63. 10.1080/00085030.2008.10757172. [DOI] [Google Scholar]
- 47).Frippiat C., Gastaldi A., Van Grunderbeeck S. Persistence of immersed blood and hair DNA: a preliminary study based on casework. J Forensic Leg Med. 2017. Oct; 51: 1–8. PMID: 28709047. 10.1016/j.jflm.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 48).Crainic K., Paraire F., Leterreux M. et al. Skeletal remains presumed submerged in water for three years identified using PCR-STR analysis. J Forensic Sci. 2002. Sep; 47(5): 1025–7. PMID: 12353539. 10.1520/jfs15490j. [DOI] [PubMed] [Google Scholar]
- 49).Byard R.W., James R.A., Heath K.J. Recovery of human remains after shark attack. Am J Forensic Med Pathol. 2006. Sep; 27(3): 256–9. PMID: 16936505. 10.1097/01.paf.0000221081.80866.5c. [DOI] [PubMed] [Google Scholar]
- 50).Khoo L.S., Hasmi A.H., Mahmood M.S., Vanezis P. Underwater DVI: simple fingerprint technique for positive identification. Forensic Sci Int. 2016. Sep; 266: e4–e9. PMID: 27567043. 10.1016/j.forsciint.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 51).Plaetsen S.V., De Letter E., Piette M. et al. Postmortem evaluation of drowning with whole body CT. Forensic Sci Int. 2015. Apr; 249: 35–41. PMID: 25656400. 10.1016/j.forsciint.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 52).Byard R.W., Gilbert J.D., Brown K. Pathologic features of fatal shark attacks. Am J Forensic Med Pathol. 2000. Sep; 21(3): 225–9. PMID: 10990281. 10.1097/00000433-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 53).Vanin S., Zancaner S. Post-mortal lesions in freshwater environment. Forensic Sci Int. 2011. Oct 10; 212(1-3): e18–20. PMID: 21708437. 10.1016/j.forsciint.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 54).Haglund W.D. The disappearance of soft tissue and the disarticulation of human remains from aqueous environments. J Forensic Sci. 1993. Jul; 38(4): 806–15. PMID: 8355001. 10.1520/jfs13476j. [DOI] [PubMed] [Google Scholar]
- 55).Sinton T.J., Byard R.W. Pathological features of fatal crocodile attacks in Northern Australia. J Forensic Sci. 2016. Nov; 61(6): 1553–1555. PMID: 27488932. 10.1111/1556-4029.13171. [DOI] [PubMed] [Google Scholar]
- 56).Ihama Y., Ninomiya K., Noguchi M. et al. Fatal propeller injuries: three autopsy case reports. J Forensic Leg Med. 2009. Oct; 16(7): 420–3. PMID: 19733336. 10.1016/j.jflm.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 57).Karger B., Suggeler S., Brinkman B. Electrocution-autopsy study with emphasis on “electrical petechiae”. Forensic Sci Int. 2002. May 23; 126(3): 210–3. PMID: 12062943. 10.1016/s0379-0738(02)00061-0. [DOI] [PubMed] [Google Scholar]
- 58).Capovilla M., Durigon M., de la Grandmaison G.L. An original cause of drowning in an industrial environment. Am J Forensic Med Pathol. 2007. Mar; 28(1): 91–3. PMID: 17325473. 10.1097/01.paf.0000257389.59801.9c. [DOI] [PubMed] [Google Scholar]
- 59).Mugdlimath A.B., Sane M.R., Zine K.U., Hiremath R.M. Quenching tank: accidental drowning in hot quenching oil. Med Leg J. 2017. Jun; 85(2): 108–110. PMID: 27672133. 10.1177/0025817216671108. [DOI] [PubMed] [Google Scholar]
- 60).Reh H. Early postmortem course of washerwoman's skin of the fingers. Z Rechtsmed. 1984; 92(3): 183–8. PMID: 6741294. [DOI] [PubMed] [Google Scholar]
- 61).Caruso J.L. Decomposition changes in bodies recovered from water. Acad Forensic Pathol. 2016. Mar; 6(1): 19–27. 10.23907/2016.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62).Haglund W.D., Sorg M.H. Advances in forensic taphonomy: method, theory, and archeological perspectives. 1st ed. Boca Raton: CRC Press; 2001. Chapter 11, Human remains in water environments; p. 201–18. [Google Scholar]
- 63).Ubelaker D.H., Zarenko K.M. Adipocere: what is known after over two centuries of research. Forensic Sci Int. 2011. May 20; 208(1-3): 167–72. PMID: 21185137. 10.1016/j.forsciint.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 64).Heaton V., Lagden A., Moffaat C., Simmons T. Predicting the postmortem submersion interval for human remains recovered from the U.K. waterways. J Forensic Sci. 2010. Mar 1; 55(2): 302–7. PMID: 20102465. 10.1111/j.1556-4029.2009.01291.x. [DOI] [PubMed] [Google Scholar]
- 65).Doberentz E., Madea B. Estimating the time of immersion of bodies found in water: an evaluation of a common method to estimate the minimum time interval of immersion. Revista Espanola Med Legal. 2010. May; 36(2): 51–61. 10.1016/s0377-4732(10)70045-6. [DOI] [Google Scholar]
- 66).Wallace J.R., Merritt R.W., Kimbirauskas R. et al. Caddisflies assist with homicide case: determining a postmortem submersion interval using aquatic insects. J Forensic Sci. 2008. Jan; 53(1): 219–21. PMID: 18279261. 10.1111/j.1556-4029.2007.00605.x. [DOI] [PubMed] [Google Scholar]
- 67).Van Daalen M.A., De Kat D.S., Oude Grotebevelsborg B.F. et al. An aquatic decomposition scoring method to potentially predict the postmortem submersion interval of bodies recovered from the North Sea. J Forensic Sci. 2017. Mar; 62(2): 369–373. PMID: 28247448. 10.1111/1556-4029.13258. [DOI] [PubMed] [Google Scholar]
- 68).Copeland A.R. An assessment of lung weights in drowning cases: the Metro Dade County experience from 1978–1982. Am J Forensic Med Pathol. 1985. Dec; 6(4): 301–4. PMID: 4072984. 10.1097/00000433-198512000-00006. [DOI] [PubMed] [Google Scholar]
- 69).Kringsholm B., Filskov A., Kock K. Autopsied cases of drowning in Denmark 1987–1989. Forensic Sci Int. 1991. Dec; 52(1): 85–92. PMID: 1783341. 10.1016/0379-0738(91)90099-5. [DOI] [PubMed] [Google Scholar]
- 70).Ago K., Hayashi T., Ago M., Ogata M. The number of diatoms recovered from lungs and other organs in drowning deaths in bathwater. Leg Med (Tokyo). 2011. Jul; 13(4): 186–90. PMID: 21565542. 10.1016/j.legalmed.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 71).Kakizaki E., Yukawa N. Simple protocol for extracting diatoms from lung tissues of suspected drowning cases with 3h: First practical application. Forensic Sci Int. 2015. Jun; 251: 179–85. PMID: 25911496. 10.1016/j.forsciint.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 72).Robbins R.D., Sekhar H.K., Siverls V. Temporal bone histopathologic findings in drowning victims. Arch Otolaryngol Head Neck Surg. 1988. Sep; 114(9): 1020–3. PMID: 3408568. 10.1001/archotol.1988.01860210086022. [DOI] [PubMed] [Google Scholar]
- 73).Lin C.Y., Yen W.C., Hsieh H.M. et al. Diatomological investigation in sphenoid sinus fluid and lung tissue from cases of suspected drowning. Forensic Sci Int. 2014. Nov; 244: 111–5. PMID: 25233019. 10.1016/j.forsciint.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 74).Tsokos M.T., Cains G., Byard R.W. Hemolytic staining of the intima of the aortic root in freshwater drowning. Am J Forensic Med Pathol. 2008. Jun; 29(2): 128–30. PMID: 18520478. 10.1097/paf.0b013e318173efed. [DOI] [PubMed] [Google Scholar]
- 75).Puschel K., Schulz F., Darrmann I., Tsokos M. Macromorphology and histology of intramuscular hemorrhage in cases of drowning. Int J Legal Med. 1999; 112(2): 101–6. PMID: 10048667. 10.1007/s004140050210. [DOI] [PubMed] [Google Scholar]
- 76).Alexander R.T., Jentzen J.M. Neck and scleral hemorrhage in drowning. J Forensic Sci. 2011. Mar; 56(2): 522–5. PMID: 21198626. 10.1111/j.1556-4029.2010.01636.x. [DOI] [PubMed] [Google Scholar]
- 77).Byard R.W., Zuccollo J.M. Forensic issues in cases of water birth fatalities. Am J Forensic Med Pathol. 2010. Sep; 31(3): 258–60. PMID: 20436337. 10.1097/PAF.0b013e3181e12eb8. [DOI] [PubMed] [Google Scholar]
- 78).Dressler J., Schmidt U., Hanisch U. et al. Neonatal freshwater drowning after birth in the bathroom. Am J Forensic Med Pathol. 2011. Jun; 32(2): 119–23. PMID: 21297437. 10.1097/PAF.0b013e318187dff9. [DOI] [PubMed] [Google Scholar]
- 79).Spitz W.U. Spitz and Fisher's medicolegal investigation of death: guidelines for the application of pathology to crime scene investigation. 4th ed. Springfield (IL): Charles C Thomas; c2006. Chapter 25, Selected procedures at autopsy; p. 1243–74. [Google Scholar]
- 80).Voland C., Vilarino R., Grabherr S. et al. Fatal cervical spine injury from diving accident. Am J Forensic Med Pathol. 2015. Sep; 36(3): 216–8. PMID: 26108039. 10.1097/PAF.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 81).Gulino S.P. Examination of the cardiac conduction system: forensic application in cases of sudden cardiac death. Am J Forensic Med Pathol. 2003. Sep; 24(3): 227–38. PMID: 12960658. 10.1097/01.paf.0000083453.43318.74. [DOI] [PubMed] [Google Scholar]
- 82).Tester D.J., Medeiros-Domingo A., Will M.L., Ackerman M.J. Unexplained drownings and the cardiac channelopathies: a molecular autopsy series. Mayo Clin Proc. 2011. Oct; 86(10): 941–7. PMID: 21964171. PMCID: PMC3184023. 10.4065/mcp.2011.0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83).Morini L., Vignali C., Tricomi P., Groppi A. Analytical challenge in postmortem toxicology applied to a human body found into a lake after three years immersion. J Forensic Sci. 2015. Sep; 60(5): 1383–6. PMID: 26258895. 10.1111/1556-4029.12815. [DOI] [PubMed] [Google Scholar]
- 84).Gruszecki A.C., Booth J., and Davis G.G. The predictive value of history and scene investigation for toxicology results in a medical examiner population. Am J Forensic Med Pathol. 2007. Jun; 28(2): 103–6. PMID: 17525557. 10.1097/PAF.0b013e318061956d. [DOI] [PubMed] [Google Scholar]
- 85).Driscoll T.R., Harrison J.A., Steenkamp M. Review of the role of alcohol in drowning associated with recreational aquatic activity. Inj Prev. 2004. Apr; 10(2): 107–13. PMID: 15066977. PMCID: PMC1730083. 10.1136/ip.2003.004390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86).Kugelberg F.C., Jones A.W. Interpreting results of ethanol analysis in postmortem specimens: a review of the literature. Forensic Sci Int. 2007. Jan 5; 165(1): 10–29. PMID: 16782292. 10.1016/j.forsciint.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 87).Vincenzi F.F. Drug-induced long QT syndrome increases the risk of drowning. Med Hypotheses. 2016. Feb; 87: 11–3. PMID: 26826633. 10.1016/j.mehy.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 88).Piette M.H.A., De Letter E.A. Drowning: still a difficult autopsy diagnosis. Forensic Sci Int. 2006. Nov 10; 163(1-2): 1–9. PMID: 16378701. 10.1016/j.forsciint.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 89).Adjutantis G., Coutselinis A. Changes in magnesium concentration of the vitreous humour of exenterated human eyeballs immersed in sea water. Forensic Sci. 1974. Aug; 4(1): 63–5. PMID: 4850963. 10.1016/0300-9432(74)90077-6. [DOI] [PubMed] [Google Scholar]
- 90).Gettler A.O. A Method for the determination of death by drowning. JAMA. 1921. Nov 19; 77(21): 1650–2. 10.1001/jama.1921.02630470036013. [DOI] [Google Scholar]
- 91).Moritz A.R. Chemical methods for the determination of death by drowning. Physiol Rev. 1944. Jan; 24(1): 70–88. 10.1152/physrev.1944.24.1.70. [DOI] [Google Scholar]
- 92).Durlacher S.H., Freimuth H.C., Swann H.E. Jr.. Blood changes in man following death due to drowning, with comments on tests for drowning. AMA Arch Pathol. 1953. Nov; 56(5): 454–61. PMID: 13091589. [PubMed] [Google Scholar]
- 93).Zhu B.L., Ishida M., Taniguchi L. et al. Possible postmortem serum markers for differentiation between fresh-, saltwater drowning and acute cardiac death: a preliminary investigation. Leg Med (Tokyo). 2003. Mar; 5 Suppl 1: S298–301. PMID: 12935616. 10.1016/s1344-6223(02)00155-4. [DOI] [PubMed] [Google Scholar]
- 94).Jeanmonod R., Staub B., Mermillod B. The reliability of cardiac haemodilution as a diagnostic test of drowning. Forensic Sci Int. 1992. Jan; 52(2): 171–80. PMID: 1601349. 10.1016/0379-0738(92)90105-6. [DOI] [PubMed] [Google Scholar]
- 95).Azparren J., de la Rosa I., Sancho M. Biventricular measurement of blood strontium in real cases of drowning. Forensic Sci Int. 1994. Dec 1; 69(2): 139–48. PMID: 7813997. 10.1016/0379-0738(94)90250-x. [DOI] [PubMed] [Google Scholar]
- 96).Yajima D., Saito H., Sato K. et al. Diagnosis of drowning by summation of sodium, potassium and chloride ion levels in pleural effusion: differentiating between freshwater and seawater drowning and application to bathtub deaths. Forensic Sci Int. 2013. Dec 10; 233(1-3): 167–73. PMID: 24314517. 10.1016/j.forsciint.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 97).Hayakawa A., Terazawa K., Matoba K. et al. Diagnosis of drowning: electrolytes and total protein in sphenoid sinus fluid. Forensic Sci Int. 2017. Apr; 273: 102–105. PMID: 28260644. 10.1016/j.forsciint.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 98).Kakizaki E., Ogura Y., Kozawa S. et al. Detection of diverse aquatic microbes in blood and organs of drowning victims: first metagenomic approach using high-throughput 454-pyrosequencing. Forensic Sci Int. 2012. Jul 10; 220(1-3): 135–46. PMID: 22424673. 10.1016/j.forsciint.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 99).An J.L., Ishida Y., Kimura A., Kondo T. Immunohistochemical examination of intracerebral aquaporin-4 expression and its application for differential diagnosis between freshwater and saltwater drowning. Int J Legal Med. 2011. Jan; 125(1): 59–65. PMID: 21069372. 10.1007/s00414-010-0523-8. [DOI] [PubMed] [Google Scholar]
- 100).Siver P.A., Lord W.D., McCarthy D.J. Forensic limnology: the use of freshwater algal community ecology to link suspects to an aquatic crime scene in southern New England. J Forensic Sci. 1994. May; 39(3): 847–53. 10.1520/jfs13663j. [DOI] [Google Scholar]
- 101).Levkov Z., Williams D.M., Nikolovska D. et al. The use of diatoms in forensic science: advantages and limitations of the diatom test in cases of drowning. In: The archaeological and forensic applications of microfossils: a deeper understanding of human history. Bath (UK): The Geological Society; 2017. p. 261–77. [Google Scholar]
- 102).Kakizaki E., Kozawa S., Sakai M., Yukawa N. Numbers, sizes and types of diatoms around estuaries for a diatom test. Am J Forensic Med Pathol. 2011. Sep; 32(3): 269–74. PMID: 21725229. 10.1097/PAF.0b013e318221b857. [DOI] [PubMed] [Google Scholar]
- 103).Lin C.Y., Yen W.C., Hsieh H.M. et al. Diatomological investigation in sphenoid sinus fluid and lung tissue from cases of suspected drowning. Forensic Sci Int. 2014. Nov; 244: 111–5. PMID: 25233019. 10.1016/j.forsciint.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 104).Zhao J., Liu C., Bardeesi A.S.A. et al. The diagnostic value of quantitative assessment of diatom test for drowning: an analysis of 128 water related death cases using microwave digestion-vacuum filtration-automated scanning electron microscopy. J Forensic Sci. 2017. Nov; 62(6): 1638–42. PMID: 28205216. 10.1111/1556-4029.13455. [DOI] [PubMed] [Google Scholar]
References
- 1).Erskine K.L. Water-related death investigation: practical methods and forensic applications. 1st ed. Boca Raton: CRC Press; c2011. Chapter 2, Investigative duties on scene; p. 27–108. [Google Scholar]
- 2).Erskine K.L. Water-related death investigation: practical methods and forensic applications. 1st ed. Boca Raton: CRC Press; c2011. Chapter 3, On-scene body assessment; p. 109–132. [Google Scholar]
- 3).Hendricks W., Zaferes A., Nelson C. Homicide by drowning. Hurley (NY): Lifeguard Systems; 1998. 60 p. [Google Scholar]
- 4).Safe Kids Worldwide [Internet]. Washington: Safe Kids Worldwide; c2016. Water safety at home; [cited 2017 Dec 1]. Available from: https://www.safekids.org/watersafety. [Google Scholar]
- 5).Report on decompression illness and diving fatalities. Durham (NC): Divers Alert Network; 1999. [cited 2017 Dec 1]. 128 p. Available from: https://www.diversalertnetwork.org/medical/report/DAN1999DCIreport.pdf. [Google Scholar]


