Abstract
The medical examiner/coroner (ME/C) death scene investigation systems of the United States play a pivotal role in the current public health crisis created by the expanding drug dependency epidemic in the United States. The first point of recognition of a drug-related death in a community is often the local ME/C agency. This circumstance places these entities in an ideal position to provide surveillance data regarding the epidemiology of drug-related deaths occurring within the jurisdiction of the agency. The ability to surveil for the distribution and determinants among drug-related deaths at the first point of contact enhances the capacity to recognize actionable trends at the local, state, and national levels, including the ability to identify secular (longer-term) trends among various drugs and population subgroups, as well as activity spikes (outbreaks) associated with high-potency formulations and drug combinations.
In this article, we describe the development and implementation of an online website that provides public access to a wide array of drug-related death surveillance resources and tools. The website gives users access to a detailed dataset that includes information regarding specific drugs, demographic information pertaining to the decedent, and to investigational findings related to the circumstances of the death. A unique aspect of the database is that it is populated by ME/C agencies and accessed by the public with no intermediary agency, so that the lag time between the identification and investigation of the death as drug-related and community knowledge of the circumstances of the death is minimized.
Wide dissemination of accurate drug death surveillance information in an easily accessible and customizable format promotes societal awareness of the drug death epidemic, but also provides information to public health, law enforcement, regulatory, and other community-based organizations that can benefit from the most up-to-date knowledge. We envision a national system of surveillance at the regional ME/C level that would allow for optimal information dissemination and sharing. Such a system would likely allow for more efficacious allocation of resources at the regional and national level.
Keywords: Forensic pathology, Drug overdose, Surveillance, Public access, Searchable
Introduction
Over the ten-year period from 2005 to 2014, drug overdose deaths in the United States increased at an alarming rate. Deaths due to illicit drug overdoses doubled during this time (from 8923 to 17 465), a rise driven almost entirely by a 5.3-fold increase in heroin-related deaths (from 2009 to 10 574) (1). Prescription drug deaths also increased during this same time, though at a lower rate (1.7-fold, from 15352 to 25 760), with the largest numbers of deaths resulting from opioid overdoses, which increased 1.7 times, from 10 928 to 18 893 (1). In 2015, there were more than 33 000 deaths attributable to either opioid prescription drugs or heroin, causing the Centers for Disease Control and Prevention to characterize the deaths as part of a nationwide epidemic (2).
The recognition of a death as drug-related is typically first made by the medical examiner or coroner's office, and the majority of such deaths are investigated via autopsy. Of the 55 403 deaths in 2015 deemed drug-related, 40 411 (73%) underwent autopsy examination (3).
Medical examiner/coroner (ME/C) agencies are ideally situated to provide comprehensive and contemporaneous information regarding drug-related deaths, such that they can function as epidemiologic surveillance sites. Surveillance is a critically important response to the nationwide drug death epidemic, given the high degree of secular variation in geographic distribution, victim demography, drug types and combinations, and other factors. Timely dissemination of surveillance data allows for rapid identification of outbreak-type spikes in deaths resulting from the introduction of particularly lethal street drugs. In an ideal system, ME/C agencies can make death investigation information that is routinely gathered for drug overdose deaths directly available to all local, statewide, and national stakeholders in an easily searchable format. Such a system would enhance strategies for prevention and deterrence, allowing for a more efficient allocation of resources.
In the following discussion, we present the background, methodology, and plan for a ME/C-based drug overdose surveillance system that is being successfully implemented in the Commonwealth of Pennsylvania.
Discussion
Drug Overdose Death Investigation in Pennsylvania
Pennsylvania has a population of approximately 13 million people, with 67 county jurisdictions divided into eight classes. Investigation of deaths that occur in the Commonwealth of Pennsylvania come under the jurisdiction of either a ME (two) or an elected lay-coroner (65). The two largest counties, Philadelphia (Class 1), with a population of 1.5 million, and Allegheny (Class 2), with a population of 1.2 million, have appointed medical examiner death scene investigation systems. The remaining Class 3 through Class 8 counties, ranging in population from 5000 to 800 000, have elected lay-coroners. The majority of these elected coroners are funeral directors.
Provision of autopsy services is by salaried, board-certified forensic pathologists in the two ME systems, and by a mixture of individual and group forensic practices, also staffed in virtually all instances by forensic pathologists, in the remaining jurisdictions. Throughout the state, these local agencies suffer from historic and chronic underfunding, now accentuated by the continually increasing demand from the overdose epidemic. Death investigation practices and customs are nonstandardized in the Commonwealth, and there is no statewide mandate, as in some jurisdictions, to include specific drugs on the death certificate. This is one of the reasons that Pennsylvania ranks within the bottom five percent of accuracy of death certification with the United States (4).
Although there is significant variation in practice, the investigation of the vast majority of apparent drug overdoses in Pennsylvania generally includes performance of a complete autopsy, including testing of urine and at least one source of blood. Most, but not all, jurisdictions follow the investigation protocol recommended by the National Association of Medical Examiners, which includes review of the death scene and available documentation of history of drug abuse, identification of drugs found at the scene, and prescription drug history (5).
Each of the two ME systems in the Commonwealth have independent toxicology sections. Toxicology for the majority of the elected Pennsylvania Coroners is most commonly performed by National Medical Services of Willow Grove, Pennsylvania. In both instances, testing is performed on specimens of blood and/or urine and includes all major drugs of abuse. As would expected, and as between any jurisdictions outside PA, variation between the specific specimens submitted, methodology employed, composition of test panels, and ability to perform expanded and focused testing creates an additional element of nonstandardization.
The Allegheny County Office of the Medical Examiner (ACOME) is unusual in that it has independent toxicology and drug chemistry sections located within the same facility as where autopsies are performed. This arrangement allows for expanded and/or focused testing on drugs seized from the death scene, as necessary, as well as readily available consultation with scene investigators and pathologists. Drug seizures from the scenes of overdose deaths in counties represented by coroners are typically submitted to the crime laboratories of the Pennsylvania State Police (PSP), a statewide system of six regional labs.
OverDoseFreePA
In 2010, the Allegheny County Overdose Prevention Coalition (ACOPC) was established to address the expanding overdose crisis in Allegheny County (6). The Coalition is hosted by the School of Pharmacy of the University of Pittsburgh, and consists of a broad-based alliance of community, law enforcement, governmental, and pharmaceutical entities, along with academic stakeholders. In 2013, the coalition was expanded to establish OverDoseFreePA (OFPA), a group focused more directly on overdose deaths in Pennsylvania (7).
The primary aims of ACOPC are twofold. The first is to provide a comprehensive source of advice on approaches to the overdose crisis through its web-based catalogue of resource and a Technical Advisory Center (TAC) (8). To this end, the TAC has established strategic alliances with 14 counties.
The second goal is to establish and publish through OFPA a standardized, publically available dataset of drug overdose deaths in the Commonwealth. Currently, an overlapping subset of 11 counties in the Commonwealth actively contributes their overdose data to OFPA. The site is designed to enable data entry by either ME/C personnel, such that the results could be incorporated into this publicly available, web-based interface in a timely manner. For jurisdictions with more advanced information systems, submission to the site can be handled as a bulk upload.
Overdose Death Registry Data Entry Protocol
Participating ME/C agencies submit information into an online form that includes all available demographic and scene investigation findings in addition to the information from the toxicology reports (Figure 1). Medical examiner/coroner staff tasked with submitting data to OFPA receive training from OFPA personnel in basic toxicology and use of the drug entry form. Additionally, OFPA provides online support and a dictionary of drugs and metabolites via the TAC. Turnaround time from the date of death to toxicology results is typically two to three weeks in the ME/C agencies throughout the Commonwealth, and once the results are received they are submitted to OFPA within one to four weeks. Thus, the lag time between an overdose death and online publication is typically no more than two months for any death.
Figure 1.
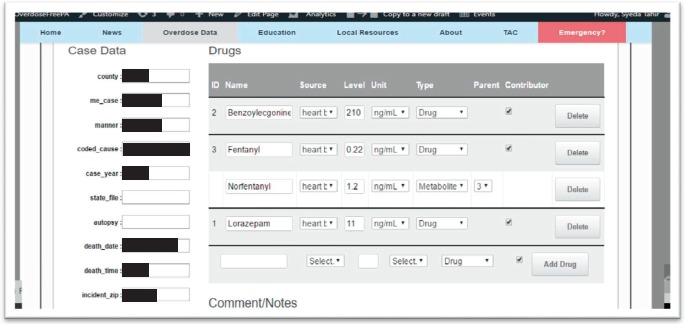
Screenshot of portion of data entry form.
Participation in OFPA is uncompensated at the present time. The motivation to contribute data is primarily attributable to a sense of community service and the widely recognized need in the ME/C system for accurate and timely data regarding overdose deaths.
The drug data portion of the entry form permits categorization of each agent as either a parent drug or metabolite, with only the parent drug listed as contributing to the death. There is an additional capability to enter specific measured concentrations of the identified agents. The online drug dictionary includes any drug or metabolite that has appeared in a submitted case from any jurisdiction and allows ME/C personnel to have specific information as to the nature of each agent identified in their particular toxicology report. This capability assists contributors in determining whether the specific agent is a parent drug and main cause of death, a contributory agent, or a metabolite. It also aids in understanding metabolic pathways. Commonly found agents such as cannabinoids, nicotine, and therapeutic levels of nonscheduled drugs are not included as a contributor but are retained in the ultimate dataset for possible future consideration.
Following completion of the entry form, the individual case is placed into the “Review Case Data” queue for vetting by the technical staff of OFPA for accuracy and consistency (Figure 2). Staff consists of personnel with at least master's level training in pharmacology or toxicology. The review process initiates a two-way, online conversation with the submitting jurisdiction concerning details of the particular case (Figure 3). The process for filing the majority reports is relatively straightforward.
Figure 2.
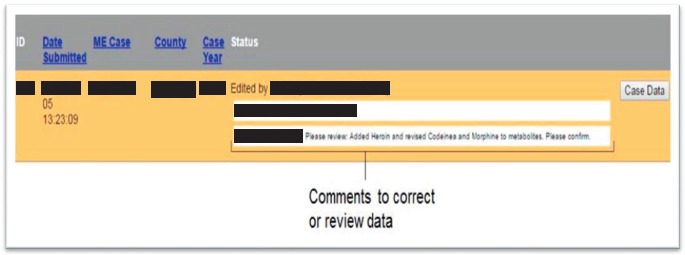
Screenshot of online communication with contributor during case review.
Figure 3.
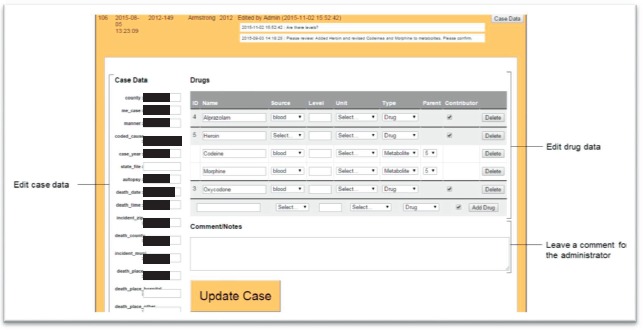
Screenshot demonstrating editing and revision of original drug data.
At this stage of the process, consultation on more complex issues, such as postmortem redistribution and metabolism, can be provided by OFPA personnel with specific training and with backup assistance from consulting forensic toxicologists and medical examiners.
While in most cases the offending drug is readily identified, in some cases, the relative contribution of several drugs needs to be assessed. The general rule followed in multidrug cases is that it is not typically feasible to quantify the role that an individual drug played in causing a death. Thus, the procedure in OFPA is to be inclusive and consider all drugs identified at more than trace amounts as contributing to the death (9). This practice sidesteps the wide variety of interpretive and technical issues that can arise when analyzing the results of a toxicological analysis. Some of these issues present difficulties even for the larger ME jurisdictions with in-house toxicologists. Despite these potential difficulties, the vast majority of cases are using a rational “best effort” approach.
The most common problems with interpreting toxicology reports occur with opioid drugs and benzodiazepines. For opioids, the problem results from finding morphine in the urine without the presence of either heroin or 6-monoacetylmorphine (6-MAM) in any other tested fluids. The presence of one or the other would indicate that the parent drug was heroin, but when neither is found, the cause of the overdose is less certain. While this issue has been addressed in the literature with sophisticated algorithms (10, 11), the approach used when the paradox is encountered for OFPA data is to consider the presence of morphine as representing the “last man standing” of a heroin overdose. When considered along with secondary factors such as evidence of active drug use from the scene, history of drug abuse, injection sites on the body, and urine drug screens, this probabilistic approach is most practicable (12).
The second class of drugs that can present issues in interpretation of toxicology reports is benzodiazepines. These drugs share common structures and are extensively metabolized, often to clinically active agents that can be utilized for their therapeutic effect. This can result in difficulties determining the drug of origin. OverDoseFreePA provides guidance in the resolution of problem cases.
For remaining drug classes (central nervous system stimulants/selective serotonin release inhibitors) and individual agents, such as fentanyl and its analogues, ethanol, and prescription opioids, the determination of contribution to the overdose is typically made without difficulty.
Data Synthesis and Publication
Following approval of the individual case by the submitting jurisdiction, the data are moved to the “Live Data” section of the site and made available for public access. The view presented on entry into the OFPA site is static, and includes the following: total overdoses by region (by specific county or aggregate of one or more contiguous jurisdictions, and for variable number of specified years dating back to 2007), gender, race, age, place of injury ZIP code, top ten drugs detected, and top ten fatal drugs over time (Figures 4, 5, and 6).
Figure 4.
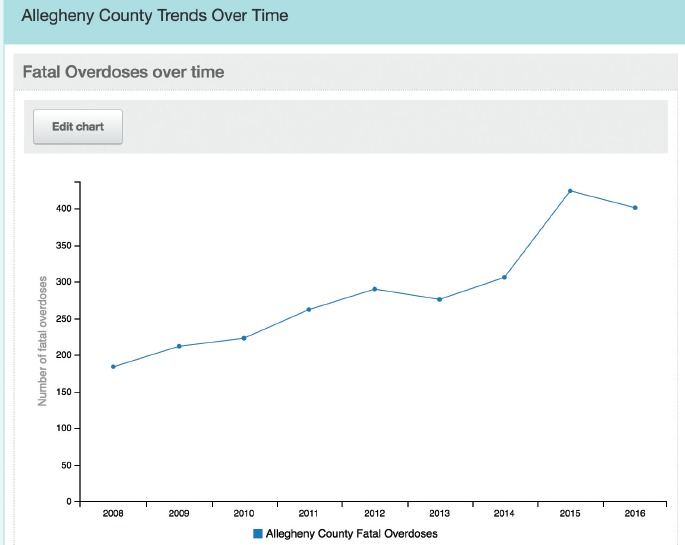
Screenshot showing fatal overdoses in Allegheny County over time.
Figure 5.
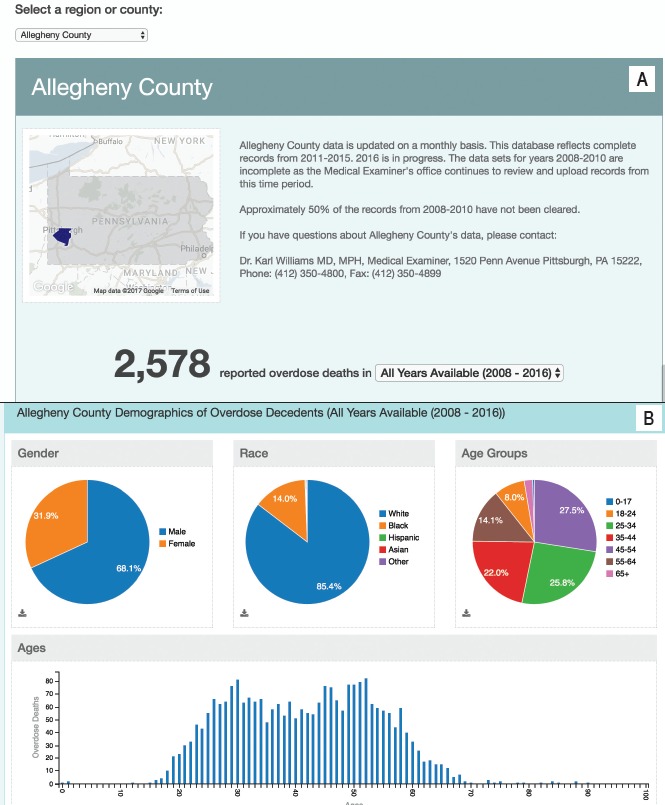
A) Screenshot showing reported overdose deaths in Allegheny County over all years in the database. B) Screenshot showing demographics of fatal overdose decedents.
Figure 6.
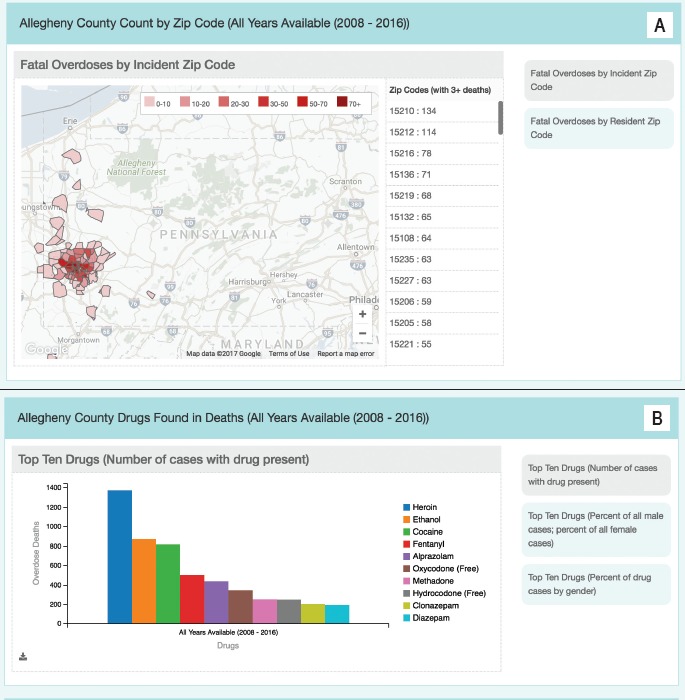
A) Screenshot showing fatal overdoses by zip code. B) Screenshot showing the top ten drugs involved in overdose deaths.
The OFPA site allows for the ability to create customized queries of the entire dataset using the above-listed set of variables.
Data and Examples
OverDoseFreePA currently includes participation, at some level, by 46 of the 67 counties of the Commonwealth, including two overlapping subsets of counties. There are ME/C agencies in 11 counties that are currently submitting overdose data as of December 2016, and an additional 26 counties with an alliance with the University of Pittsburgh School of Pharmacy Technical Assistance Center. The total group represents approximately half of the population of the Commonwealth. Data from more than 4000 overdose deaths are currently available on the OFPA website, and for two of the counties complete data on the site dates back to 2007.
A prominent feature of the OFPA website is the contemporaneous availability of raw data concerning drug overdose deaths to the public, as well as the ability for any site user to formulate unique queries of the data. Anonymized overdose information is considered to be in the public domain. With the OFPA website, this information is made immediately available to all stakeholders, including law enforcement at local, state, and national levels, local public health groups, media, and concerned individuals.
The following examples demonstrate a small sample of the flexibility and utility of the website:
-
1)
Allegheny County's fentanyl experience, 2007-2016 (Figure 7). Prior to the obvious inflection point occurring in 2014, the experience in the county was primarily with diverted pharmaceutical fentanyl in the form of Duragesic patches. In January 2014, Allegheny County experienced a brief epidemic consisting of 27 heroin/fentanyl deaths occurring over a three-week period (13). The deaths marked the beginning of a steady rise in fentanyl-related deaths that has been observed nationwide. As can be seen in the incomplete data for 2016 in Figure 7 (11 months of data), the increase in fentanyl-related overdose deaths has persisted.
-
2)
Heroin experience in Westmoreland County by sex, age group, and race, 2009-2016 (Figure 8). The chart illustrates a comparison in the frequency of heroin overdose among 18- to 34-year-old white males and females in Westmoreland County, PA. At a glance, the chart communicates an alarming sex-specific increase in heroin-related deaths occurring in males, beginning in 2011.
Figure 7.
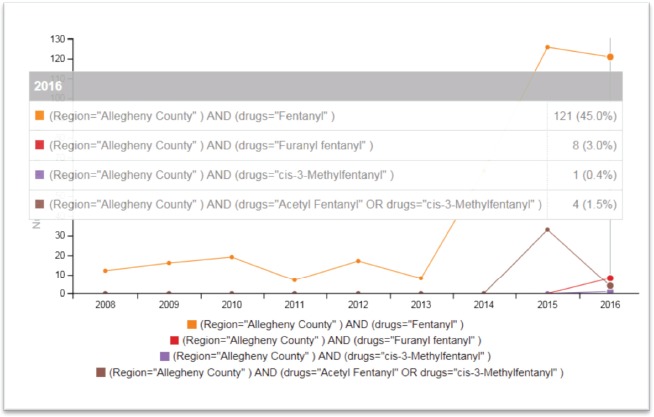
Screenshot generated by a query on Allegheny County's experience with fentanyl and fentanyl analogues (2007 – 2016).
Figure 8.
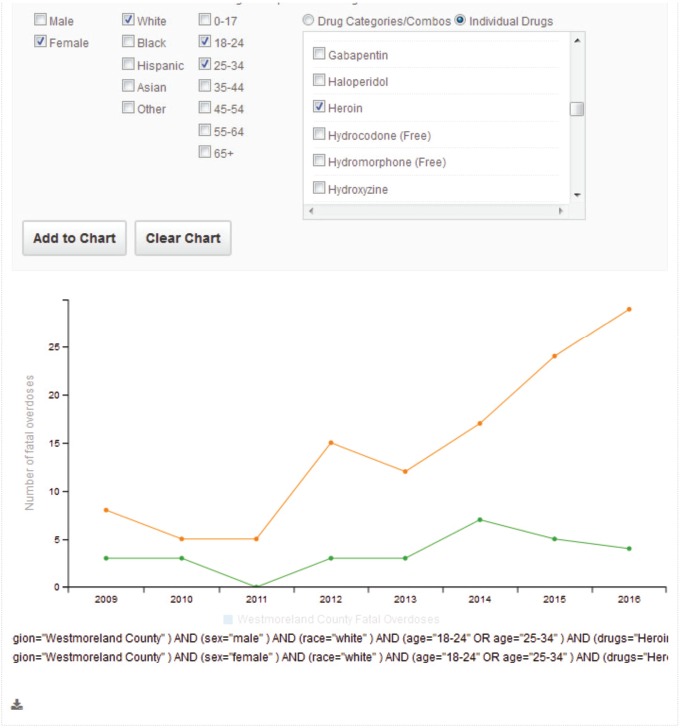
Screenshot showing experience in Westmoreland County of heroin overdoses in the white male and female populations between the ages of 18 and 34.
Conclusion
The OverdoseFreePA website is a tool created to provide the most current and specific knowledge of the current addiction and overdose epidemic, such that it serves as a surveillance tool. The data on the site are made available in conjunction with other information, including discussion of potential solutions. The current crisis exists at all jurisdictional levels, but it starts at, and is most intimate at, the local level. As the name suggests, OFPA exists first and foremost as an effort to assist these local communities in the Commonwealth of Pennsylvania.
Two primary community services are provided by OFPA, aside from the previously described overdose death website. One is to provide a broad source of up-to-date educational and other resources for various stakeholders in the law enforcement, rehabilitation, educational, and public health communities (e.g., a list of current naloxone providers in the Commonwealth). The other service, created by the School of Pharmacy of the University of Pittsburgh, is the previously mentioned TAC, which provides conceptual and practical tools for the individual counties in the Commonwealth in dealing with the crisis in their communities.
The previously described arrangement at the ACOME, in which both toxicology and drug chemistry services are housed in the same location, allows for a more completely integrated investigation of the implicated drugs and circumstances surrounding the death, allowing for more accurate certification of the cause and manner of death. The arrangement is optimal, and a desirable standard to emulate on a broader scale.
Without denying the epidemiologic significance of aggregate data at all geographic and jurisdictional levels, having the most current data possible is essential to keep abreast of the overdose epidemic, as such a system offers the closest thing to real-time surveillance. The standardization of data required by the website may also yield additional benefits for the critically important activity of death certification. The foundation for an epidemiologic basis for assessing the current overdose crisis is accurately classified data, which stems from standardized protocols for determination of incidents of drug overdose.
It is hoped that this article provides an example of a data-driven approach to the current overdose crisis, as well as a format for others to emulate and improve. OverdoseFreePA is committed to sharing ideas and approaches and welcomes feedback, contribution, and collaboration from other like-minded entities.
Footnotes
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
FINANCIAL DISCLOSURE The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
References
- 1.National Institute on Drug Abuse [Internet]. Rockville (MD): National Institute on Drug Abuse; c2016. Overdose death rates; [updated 2015. Dec; cited 2016 Dec 20]. Available from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. [Google Scholar]
- 2.Centers for Disease Control and Prevention [Internet]. Atlanta: Centers for Disease Control and Prevention; c2016. Injury prevention & control: opioid overdose. Understanding the epidemic; [updated 2016. Dec 16; cited 2016 Dec 19]. Available from: https://www.cdc.gov/drugoverdose/epidemic/. [Google Scholar]
- 3.CDC Wonder [Internet]. Atlanta: Centers for Disease Control and Prevention; c2016. Multiple cause of death data; [reviewed 2016. Dec 8; cited 2016 Dec 20]. Available from: https://wonder.cdc.gov/mcd.html. [Google Scholar]
- 4.Percent of drug poisoning deaths that mention the type of drug(s) involved, by state: 2013–2014 [Internet]. 1 p. Available from: https://www.cdc.gov/nchs/data/health_policy/unspecified_drugs_by_state_2013-2014.pdf. [Google Scholar]
- 5.Davis GG; National Association of Medical Examiners and American College of Medical Toxicology Expert Panel on Evaluating and Reporting Opioid Deaths. National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. Acad Forensic Pathol. 2013. Mar; 3(1): 77–83. 10.23907/2013.011. [DOI] [Google Scholar]
- 6.Allegheny County Overdose Prevention Coalition [Internet]. Pittsburgh: the Coalition; 2016. [updated 2016 Aug 12; cited 2016 Dec 24]. Available from: http://www.acopc.pitt.edu/. [Google Scholar]
- 7.OverdoseFreePA [Internet]. Pittsburgh: University of Pittsburgh, Program Evaluation and Research Unit; 2016. [cited 2016 Dec 15]. Available from: http://www.overdosefreepa.pitt.edu/. [Google Scholar]
- 8.Pringle J. The Pennsylvania Heroin Overdose Prevention Technical Assistance Center manual. Pittsburgh: University of Pittsburgh, Program Evaluation and Research Unit; 2016. [cited 2016 Dec 20]. 106 p. Available from: http://www.overdosefreepa.pitt.edu/tactraining-materials-2/tac-manual_20160711_v3-0/. [Google Scholar]
- 9.Gill J.R. From death to death certificate: what do the dead say? J Med Toxicol. 2016. May 2. [Epub ahead of print]. PMID: 27139707. 10.1007/s13181-016-0551-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harruff R.C., Couper F.J., Banta-Green C.J. Tracking the opioid drug overdose epidemic in King County, Washington using an improved methodology for certifying heroin related deaths. Acad Forensic Pathol. 2015. Sep; 5(3): 499–506. 10.23907/2015.055. [DOI] [Google Scholar]
- 11.Ellis A.D., McGwin G., Davis G.G., Dye D.W. Identifying cases of heroin toxicity where 6-acetylmorphine (6-AM) is not detected by toxicological analyses. Forensic Sci Med Pathol. 2016. Sep; 12(3): 243–7. PMID: 27114260. PMCID: PMC4967084. 10.1007/s12024-016-9780-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mertz K.J., Janssen J.K., Williams K.E. Underrepresentation of heroin involvement in unintentional drug overdose deaths in Allegheny County, PA. J Forensic Sci. 2014. Nov; 59(6): 1583–5. PMID: 25041514. 10.1111/1556-4029.12541. [DOI] [PubMed] [Google Scholar]
- 13.Williams K.E., Freeman M.D. The investigation of a cluster of fentanyl overdose deaths: how the use of epidemiologic surveillance and outbreak methods resulted in the rapid identification of the source of a public health crisis. Acad Forensic Pathol. 2014. Nov; 4(Suppl): S4. [Google Scholar]