Abstract
The Virginia Prescription Monitoring Program (VPMP) has been in effect since 2002, providing reports for prescribers, pharmacists, and other stakeholders in the growing opioid epidemic. The Office of the Chief Medical Examiner is one such stakeholder and has found great efficacy in the program in investigating suspected drug-related deaths. This review examines the origins of the VPMP, its benefits, and limitations for use during death investigation.
Keywords: Forensic pathology, Prescription monitoring program, Opioids, Medical examiner, Coroner, Death investigation
Introduction
The current heroin crisis in the United States largely has its origins in prescription opioid abuse. The abuse of opiates or opioid substances for the purposes of euphoria require ever increasing doses to achieve the “high” while increasing the risk of the respiratory depressant effects, for which there is no tolerance. Every day, physicians are tasked with the challenge of determining how best to treat their patients, which may include prescribing controlled and potentially addictive substances. It may be difficult, if not impossible, to determine who is a “drug-seeker” and who has legitimate physical pain (which may be one and the same person). Prescription monitoring programs can assist in reviewing a patient's prescription drug habits in an objective format. Medical examiners and coroners are also tasked with determining what role, if any, that medications or drugs played in the person's death. Toxicology results cannot be interpreted without putting them into the context of a specific case; what is lethal in one person may not be lethal in another. The Office of the Chief Medical Examiner of Virginia (OCME) utilized the Virginia Prescription Monitoring Program (VPMP) to facilitate death investigation in the deaths that fall under its jurisdiction.
Discussion
History of the Virginia Prescription Monitoring Program
The mission of the Virginia Prescription Monitoring Program is
To promote the appropriate use of controlled substances for legitimate medical purposes while deterring the misuse, abuse, and diversion of controlled substances (1).
In 2002, the Virginia General Assembly passed legislation that established a pilot program covering counties of the southwestern region of the state, which traditionally had the highest rates of prescription drug abuse and overdose. The region included 29 counties and 12 cities, covered 18% of the state's population, and involved approximately 310 pharmacies and 200 000 prescriptions annually (2). Within three years, the number of reports of alleged drug diversion by patients (through doctor shopping, fraud, or forged prescriptions) and prescribers received by the state's drug diversion unit of the Virginia state police had decreased by 47% in the program area while increasing across other regions of the state. An advisory committee reviewing the preliminary results determined that this established the need for a statewide system as well as allowing access for pharmacists, including all schedule II-IV medications and allowing for unsolicited reports to prescribers when the program managers identified patterns of behavior by patients to indicate doctor shopping or drug diversion. All recommendations were accepted by the General Assembly in 2005 and the system became a true state system. Within one year (from 2005-2006), the number of queries to the system increased from 1773 to 6333, which again more than quadrupled the following year to 22 156 (2).
Currently, 49 states, the District of Columbia, and territory of Guam all have prescription monitoring programs in place or in development, and many systems are beginning to develop interstate sharing of data (3). The sharing of data across state lines is promoted to stop patients from crossing state lines to obtain multiple prescriptions from different prescribers and pharmacies. Prior to these agreements being in place, it was impossible for a prescriber in Virginia to see any prescriptions on the report except those filled at a Virginia pharmacy. Since agreements have been in place with most neighboring states as well as many non-neighboring states, the “border-hopping” behavior can clearly be seen and identified by prescribers using the VPMP. The system includes all schedule II-IV drugs and “drugs of concern” identified by the Board of Pharmacy (which currently includes tramadol).
In 2015, automated registration of all prescribers and pharmacists with active licenses in Virginia occurred, more than doubling the number of registered users. There are requirements for all prescribers who expect opioid treatment to last longer than 14 days to query the system, and pharmacists must enter all medication records within seven days of dispensing the medication.
Of the various programs available in the United States, 41 provide the authority for some access by the medical examiner/coroner system. In 2005, as the Virginia system prepared to expand statewide, the code section (§ 54.1-2523 C. 6.) pertaining to confidentiality of the system allowed the “designated employees” of the Office of the Chief Medical Examiner to obtain information “relevant to determination of the cause of death of a specific recipient” (4). The VPMP has become an invaluable resource during death investigations in multiple ways.
The Office of the Chief Medical Examiner and Drug Deaths in Virginia
In 1946, the General Assembly abolished the coroner position and established the role of Chief Medical Examiner, with the OCME officially becoming a part of the Virginia Department of Health in 1950. Pursuant to Section 32.1-283 of the Code of Virginia, the OCME jurisdiction includes any death from trauma, injury, violence, or poisoning attributable to accident, suicide, or homicide; sudden deaths to persons in apparent good health or deaths unattended by a physician; deaths of persons in jail, prison, or another correctional institution, or in police custody (this includes deaths from legal intervention); deaths of persons receiving services in a state hospital or training center operated by the Department of Behavioral Health and Developmental Services; the sudden death of any infant; and any other suspicious, unusual, or unnatural death (5). The system is divided into four districts (Central, Northern, Tidewater and Western) based on population. The Western district comprises 34 counties, 16 cities, and borders four different states (West Virginia, Kentucky, Tennessee, and North Carolina).
In 2015, drug-related deaths occurred in 1028 persons in Virginia and based upon the first half of 2016, the number of fatal overdoses for all of 2016 is expected to increase by nearly 25% (6). Prior to 2013, the Western District typically received a third of the state's drug deaths (despite covering a quarter of the state's population), but in 2013, this began to even out across districts due to the ever increasing heroin and, more currently, illicit fentanyl epidemics. Prior to 2014, prescription drug deaths occurred most frequently in rural areas (Western District) and fatal illicit opioid overdoses occurred in urban areas.
In 2014 (the most recent complete available data), a total of 992 drug deaths occurred, 511 of which were caused solely by prescription drugs and 182 were “mixed” category (often a combination of prescription and over-the-counter or prescription and illicit drugs). The remainder of cases predominantly involved illicit drugs, with rare cases involving heavy metals, over-the-counter drugs alone, or inhalants. In all drug deaths that year, narcotics were the most commonly detected drug category in toxicology results (present in 35.5% of all drug deaths, 1309 individual narcotic drugs detected). Anti-anxiety (627) and anti-depressant (413) medications were the next most common drug types detected. Alprazolam was present in 6.9% of all drug deaths, representing the most common anti-anxiety medication. Citalopram (2.0%), fluoxetine (1.5%), and trazodone (1.5%) were the most common antidepressant medications detected. Diphenhydramine (active ingredient in many over-the-counter allergy or sleep aid medications) was present in 3.0% of all drug deaths (7).
The most common narcotic detected was morphine (322 instances, 8.9% of cases), with 6-acetylmorphine also detected in 159 instances (4.3%) indicating heroin usage. It is uncertain what percentage of the morphine cases without detectable 6-acetylmorphine represent heroin usage (due to prolonged hospitalization with lack of admission samples or unavailability of urine or vitreous samples hampering interpretation). Of the 163 cases positive for morphine without clear heroin metabolite (6-acetylmorphine), 11 were positive for codeine. Eight of these 11 had a morphine-to-codeine ratio greater than one and circumstances suggestive of heroin (8). Also, beginning in 2014, the Virginia OCME started tracking cases that were thought to be heroin-related based on scene investigation and history regardless of the detection of 6-acetylmorphine. Of the cases that were positive for morphine (but not 6-acetylmorphine or codeine), 23 were thought by the pathologist to be due to heroin based on scene investigation or history.
Oxycodone (196 instances, 5.3%), fentanyl (133 instances, 3.6%), methadone (112 instances, 3.0%) and hydrocodone (96 instances, 2.6%) were the most common prescription narcotics after morphine. During the time period in this report (calendar year 2014), various illicit forms of fentanyl became available in a powdered street version, which was being sold as heroin in many instances. It is uncertain how many of the 2014 fentanyl cases were from this illicit powdered form of fentanyl and how many from use/abuse of prescription fentanyl patches; this problem became even more apparent in 2015 when most fatal fentanyl overdoses statewide were due to illicitly produced versions of the drug. Beginning in 2016, the OCME began categorizing the suspected origin of fentanyl (i.e., illicit, prescription, or unknown) in fatal fentanyl overdoses (9).
In 2015, the total number of drug deaths was highest in large population centers (around Richmond City, Northern Virginia, in the Washington, D.C. suburb communities, and in the Tidewater district around Norfolk and Virginia Beach). However, when rates by population are determined, the southwestern region (along the Appalachian and Blue Ridge regions) has very high rates compared to other regions (Figure 1). The highest rates (per 100 000 population) in the state occurred in Dickenson County (45.6, western district), Winchester (40.0, northern district), Buchanan County (39.2, western district), Patrick County (37.9, western district), and Warren (36.1, northern district). The western counties with the highest rates are predominantly rural and coal-producing parts of the state.
Figure 1.

The rate of fatal drug overdose by locality. Counties in the southwestern portion of the state have some of the highest rates of overdose, with large number involving prescription medications.
In 2015, one or more prescription opioids (excluding fentanyl) caused or contributed to 38.7% of all fatal drug overdoses in Virginia (6). This percentage has been higher in previous years, before the onset of the heroin and illicit fentanyl epidemic. White males aged 35-54 had the highest rate of fatal prescription opioid overdoses when compared to other demographic groups. This group often falls into the jurisdiction of the OCME due to unclear cause and manner of death (natural disease vs. drugs). Many families of the men of this age range do not know their medical history and can often provide only sketchy details of their medical treatment or medications. Not having the basic medical history when beginning a death investigation is akin to trying to put together a puzzle with only half the pieces. One may be able to figure out what the picture is supposed to be, but one is just as likely to misinterpret what one are seeing at the autopsy table or in supplemental test results.
The OCME and Use of the Prescription Monitoring Program
Since 2008, the Western District of the OCME queries the VPMP on all deaths accepted under their jurisdiction. The system is occasionally queried as well to determine if patients are truly “unattended” by a physician in the year preceding their death, as families and friends may not be able to tell law enforcement if the decedent had a physician. The VPMP provides information on any prescription of a controlled substance filled during the requested time frame. The VPMP received more than 4.8 million requests for records in 2015 (Figure 2), with the OCME representing 0.15% of those requests (7260 requests) (Figure 3) (10). The query is done by medicolegal death investigators upon acceptance of a case under the Medical Examiner's jurisdiction. The standard request is for any controlled medications prescribed during the year preceding the decedent's death. This allows for medical records to be requested as soon as possible and, in this day and age of electronic medical records, often facilitates records being received and available for review by the pathologist prior to the autopsy. All Western OCME investigators are certified by the American Board of Medicolegal Death Investigation and are familiar with the different drug classes and commonly abused medications. Pathologists also query the system if they wish to expand the search time frame or if records from neighboring states need to be searched.
Figure 2.
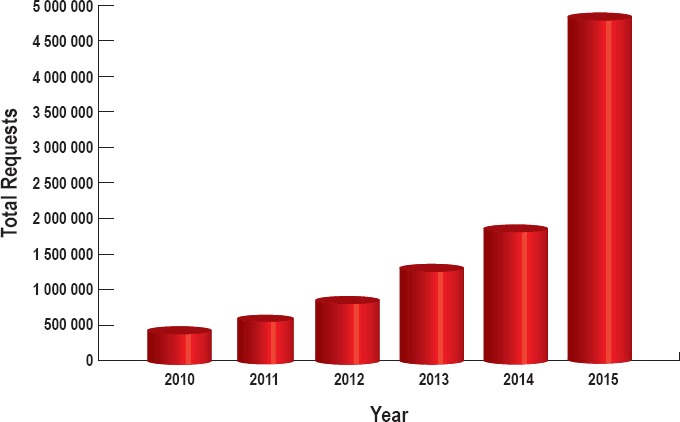
Total requests for reports from the Virginia Prescription Monitoring Program. Interoperability with other state systems, which largely took effect in 2015, has greatly increased the number of requests.
Figure 3.
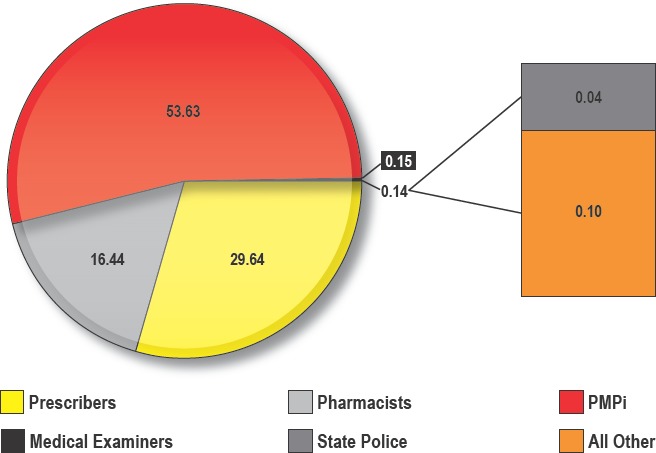
The Office of the Chief Medical Examiner of Virginia accounts for 0.15% of all queries to the Virginia Prescription Monitoring Program. The interoperability (PMPi) with other states accounts for the largest number of queries to the system.
The VPMP report provides not only a list of all prescriptions filled, but the name of the physician who wrote the prescription, the pharmacy at which it was filled, when it was filled, and for how many doses. It also provides the patient's morphine equivalent daily dose (MEDD). Many studies have shown increased risk of opioid overdose in patients receiving a MEDD greater than or equal to 100 mg/day, particularly in patients who have already experienced a prior overdose event (6, 11-13).
Every pathologist faced with reviewing toxicology reports knows the frustration of looking at a number and attempting to determine its role in the patient's death. While quick references with therapeutic and lethal ranges are helpful, there is often a significant overlap in what is considered lethal and what is not. It is vital that the toxicology results be interpreted in light of the specific patient's history and circumstances, including death scene investigation and their medical and prescription history. The VPMP is often the best resource the OCME has to determine a patient's prescription history so that tolerance can be considered as well as possible drug interactions and combined drug toxic effects.
It also allows us to utilize our toxicology testing effectively. Toxicology testing is often costly, time consuming and adds significant delays to turnaround time, frustrating families and law enforcement alike. Being able to review a patient's medication history can give us a head start on what medications and drug classes we should look for first. It also can save toxicology testing altogether if the patient has no drug history, nothing suspicious at the scene, and no controlled substances are prescribed to them. The VPMP also provides a quick reference of which physicians the decedent has seen in the previous year (or longer if requested), providing the medicolegal death investigators a fast route to collecting medical records without having to directly contact grieving families.
Conclusion
It is not unusual that OCME is referred a case in which there is initially no suspicion of overdose by scene investigation but the VPMP indicates that the decedent has been prescribed numerous controlled substances from multiple doctors, frequently a combination of pain clinics, ER visits, and dentist visits and are getting their prescriptions filled at multiple pharmacies. This can prompt toxicology testing that might otherwise not have been done. The VPMP has become an invaluable resource to guide our testing and interpretation of results to achieve the most accurate cause and manner of death determinations.
Footnotes
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
FINANCIAL DISCLOSURE The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
References
- 1.Orr R.A. Virginia's prescription monitoring program: promoting management, reducing risk [Internet]. Henrico (VA): Virginia Department of Health Professions; 2010. May 1 [cited 2016 Dec 5]. 18 p. Available from: https://www.dhp.virginia.gov/dhp_programs/pmp/docs/May2010/PMPpresentationUVAconf5-1-10.pdf. [Google Scholar]
- 2.Orr R.A. Virginia's prescription monitoring program: 2002-2007 and beyond [Internet]. Henrico (VA): Virginia Department of Health Professions; 2007. Nov 16 [cited 2016 Dec 5]. 21 p. Available from: https://www.dhp.virginia.gov/dhp_programs/pmp/docs/Virginia%27s%20PMP%202002-2007%20and%20Beyond.pps. [Google Scholar]
- 3.Compilation of Prescription Monitoring Program Maps [Internet]. Manchester (IA): National Alliance for Model State Drug Laws; 2016. May [cited 2016 Nov 8]. 34 p. Available from: http://www.namsdl.org/library/CAE654BF-BBEA-211E-694C755E16C2DD21/. [Google Scholar]
- 4.2006 Code of Virginia § 54.1-2523 - Confidentiality of data; disclosure of information; discretionary authority of Director.
- 5.2014 Virginia Code Title 32.1 - Health § 32.1-283. Investigation of deaths; obtaining consent to removal of organs, etc.; fees.
- 6.Bohnert A.S., Valenstein M., Bair M.J. et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011. Apr 6; 305(13): 1315–21. PMID: 21467284. 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 7.Hobron K. Office of the Chief Medical Examiner's Annual Report, 2014. Richmond: Virginia Department of Health; 2014. [cited 2016 Dec 5]. 263 p. Available from: http://www.vdh.virginia.gov/content/uploads/sites/18/2016/04/Annual-Report-2014-FINAL.pdf. [Google Scholar]
- 8.Davis GG; National Association of Medical Examiners and American College of Medical Toxicology Expert Panel on Evaluating and Reporting Opioid Deaths. National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. Acad Forensic Pathol. 2013. Mar; 3(1): 77–83. [Google Scholar]
- 9.Hobron K. Fatal drug overdose quarterly report. Edition 2016.2 [Internet]. Richmond: Virginia Office of the Chief Medical Examiner; 2016. Oct [cited 2016 Dec 5]. 28 p. Available from: http://www.vdh.virginia.gov/content/uploads/sites/18/2016/04/Quarterly-Drug-Death-Report-FINAL_10.2016.pdf. [Google Scholar]
- 10.Orr R.A. Virginia prescription monitoring program annual statistics, 2015. Henrico (VA): Virginia Department of Health Professions; 2016. [cited 2016 Nov 14]. 3 p. Available from: https://www.dhp.virginia.gov/dhp_programs/pmp/docs/ProgramStats/2015PMPStatsFinal.pdf. [Google Scholar]
- 11.Larochelle M.R., Liebschutz J.M., Zhang F. et al. Opioid prescribing after nonfatal overdose and association with repeated overdose. Ann Intern Med. 2016. Jan 5; 164(1): 1–9. PMID: 26720742. 10.7326/M15-0038. [DOI] [PubMed] [Google Scholar]
- 12.Dilokthornsakul P., Moore G., Campbell J.D. et al. Risk factors of prescription opioid overdose among Colorado Medicaid beneficiaries. J Pain. 2016. Apr; 17(4): 436–43. PMID: 26721613. 10.1016/j.jpain.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 13.Zedler B., Xie L., Wang L., Joyce A. et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014. Nov; 15(11): 1911–29. PMID: 24931395. 10.1111/pme.12480. [DOI] [PubMed] [Google Scholar]


