Abstract
Though medicolegal death investigation (MDI) systems are generally associated with criminal justice, they serve an integral role in the realm of public health and safety. Medicolegal death investigation offices collect information, including medical records, from a variety of outside sources. For data to travel efficiently, transmission should be fully integrated between the MDI office and external organizations. This is often not the case. Delays in the transmission of medical records in particular lead to subsequent delays in autopsy report completion and death certification or to resource waste in cases where a timely record would have let the pathologist know an autopsy was not required. Almost no peer-reviewed literature currently exists regarding the problem of record acquisition by MDI systems. To develop a better understanding of how electronic medical records have impacted MDI systems, we conducted a mixed methods survey through the National Association of Medical Examiners (NAME) e-mail listserv. We inquired about the medical records acquisition processes at MDI systems around the nation to gauge opinions about the use of electronic health data and the integration of MDI data in public health. Concurrently, we piloted a quality improvement project at the Alameda County Sheriff-Coroner's Office (ACSCO) in Oakland, California, in which we worked with various hospitals to get ACSCO employees direct access to decedents' electronic health records. With data from the survey and pilot project, we were able to document the barriers encountered when attempting to reform medical record acquisition and to suggest systemic changes to reduce delays and wasted resources.
Keywords: Forensic pathology, Public health, Electronic health record, Electronic medical record, Medical record acquisition
Introduction
Though medicolegal death investigation (MDI) systems are generally associated with criminal justice, they serve an integral role in the realms of public health and safety (1–6). Historically, the majority of a medical examiner's caseload has been due to sudden, natural death, making public health the primary function of MDI systems (7). Even the 10 – 15% of the total caseload that constitute homicides can be considered within the realm of public health due to the fairly recent recognition of violence as a public health problem (7, 8). The information obtained from MDI has a broad impact as it is the largest source of national mortality statistics, which are used to monitor trends and patterns of specific causes of disease and to identify health and safety problems in the community (1, 5, 9). Medicolegal death investigation data are used for population-level surveillance of injury, infectious disease, violent crime, and incidents of bioterrorism to determine where to focus public health resources (1, 4, 6, 10–15). Medicolegal death investigation findings can drive the development of policy and lead to the evaluation of the effectiveness, accessibility, and the quality of services provided to the community (5). Feedback can then be given to healthcare systems to inform quality improvement (2, 5). For example, voluntary reporting of deaths caused by consumer products to the Consumer Products Safety Commission has resulted in merchandise recalls and improved standards (6).
In order to investigate death, MDIs collect data from a variety of outside sources, including health records from hospitals and doctors' offices both within and outside of their jurisdiction (14, 16). For improved efficiency, data transmission should be fully integrated between MDI offices and the external organizations giving information to and receiving information from those offices (16). Due to technological, financial, and administrative challenges, this is often not the case (3, 10, 13). Current inefficiencies in data transmission from hospitals to their regional MDI are the area of focus for this project.
Almost no peer-reviewed literature currently exists regarding the particular problem of record acquisition by MDI systems. Dibdin identified the flow of information through MDI systems as a potential area for continuous quality improvement, but did not focus on a specific area of need (16). Most literature focuses on the transmission of data either to the MDI office from laboratory services (14, 17), or from the MDI to public health instruments, such as surveillance databases (6, 12).
Clinical informatics is a relatively new subspecialty that focuses on evaluating information and communication systems (6). Within the field are the pathology informatics and public health informatics subdomains, which are both applicable to MDI systems (6). Levy provides the single mention of the inefficiencies of the medical record acquisition process in MDI found in reviewing the literature (7); therefore it is unclear how many MDIs consider it a problem. Of particular interest is if and how the widespread transition to electronic medical records (EMR), spurred by the American Recovery and Reinvestment Act of 2009, which encouraged clinical providers to develop these systems, has impacted MDI offices (18).
To develop a better understanding of how EMRs have impacted MDI systems, the authors conducted an online mixed methods survey through the National Association of Medical Examiners (NAME) e-mail listserv. In the survey, we inquired about the medical records acquisition processes at MDI systems around the nation to gauge forensic pathologists' opinions about the use of electronic health data and subsequent integration of MDI data in public health.
In an effort to directly contribute to increased efficiency of MDI, the authors concurrently piloted a quality improvement project at the Alameda County Sheriff-Coroner's Office (ACSCO) in Oakland, California. The ACSCO serves a population of 1 510 271 people who reside in 14 cities and several unincorporated communities (19). Improved efficiency of the medical record acquisition process at the ACSCO will hasten the office's ability to communicate important public health information to the people who can utilize it to improve population outcomes.
The ACSCO has had many difficulties with their current system of medical record acquisition. At the start of the study, investigators had to phone hospitals and wait for records to be faxed to the ACSCO or assign personnel to physically pick up the copied paper records at the hospital. This led to delays in the investigation depending on how speedily records were sent over and whether the necessary sections of the requested record were sent. If a record was faxed but important information was missing, another phone call had to be made and a repeat fax sent to the ACSCO. The length of faxes was also an issue, as there is only one fax machine in the office and it often ran out of paper or jammed when numerous records were sent.
Security is another issue with the current system. A medical examiner at the ACSCO described an incident wherein a patient's medical record was sent to her home fax machine. The clinic had the wrong number written down in their records. Luckily, the fax was sent to the home of a physician, who notified them and discarded the record securely, but it highlights the risk with the current system. One misdialed digit could send personal health information into the hands of an unauthorized individual. Disposal of the faxed records poses an additional opportunity for security lapses (7). As several of the hospitals the ACSCO deals with have electronic health records (EHR) systems, this laborious and resource-intensive method of record acquisition was clearly outdated.
For the pilot project, the authors attempted to expedite the ACSCO's acquisition of medical records by getting the ACSCO employees, including forensic pathologists and deputy coroners, direct access to decedents' EHR. Throughout the process, the authors were able to document the barriers encountered while attempting to reform medical record acquisition.
Methods
The NAME needs assessment survey was developed with the primary goal of investigating the medical record acquisition procedures at MDI systems around the nation, particularly surrounding the impact EMR reform has had on medical record acquisition. The secondary goal was to examine whether and how current death investigators see their work fitting into the larger sphere of public health and safety. A mixed methods approach was selected for the needs assessment because while certain variables, such as average time to receive records and average length of records, can be analyzed quantitatively, qualitative methods are uniquely structured to explore complex and/or previously unstudied topics (20). The authors chose to use an online survey instrument because there was a convenient avenue of distribution to the target population. The survey was created using the online tool, SurveyMonkey. It underwent three rounds of pretesting with an experienced forensic pathologist. After each round, changes were made to the survey. Figure 1 presents a copy of the final form of the survey.
Figure 1.
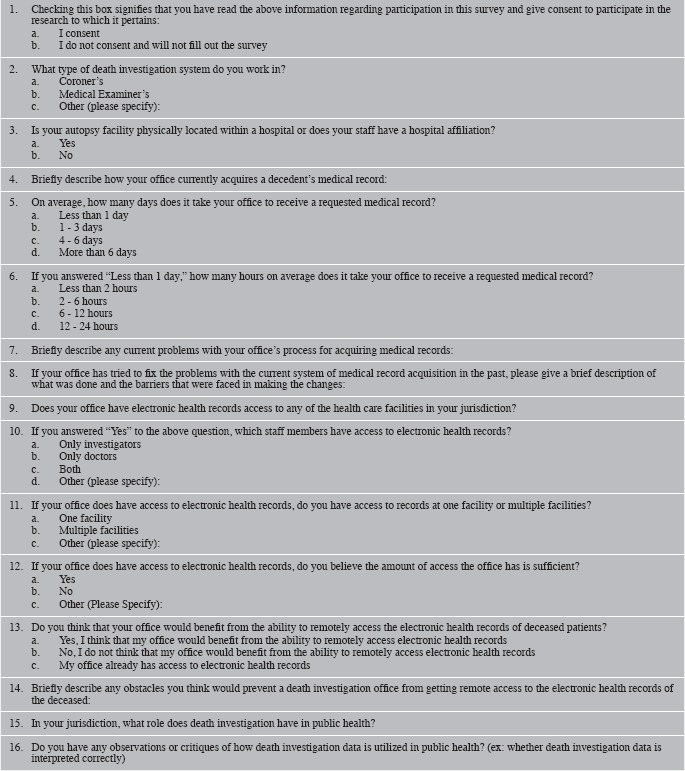
Needs Assessment Survey (Nationwide Medical Record Acquisition Survey for Death Investigation Offices)
The survey was sent to the NAME listserv on February 22, 2016. The link to the survey remained open until March 4, 2016. It was closed temporarily due to concerns from the Office for the Protection of Human Services at the University of California, Berkeley (UCB). On April 20, 2016, the UCB Committee for Protection of Human Subjects (CPHS) granted the project exempt status and the survey was re-opened. On April 22, 2016, a second e-mail was sent to the NAME listserv with the link to the newly re-opened survey. The survey was closed at midnight on May 4, 2016.
The same rationale described under the “NAME Medical Record Acquisition Process Needs Assessment” section was used to decide that online mixed methods surveys would be the best way to collect pre- and post-EMR access data at the ACSCO.
To measure baseline data at the ACSCO, a pre-EMR access survey was created in Google Forms. The survey was pretested by two employees of the ACSCO. Over two rounds of testing, changes were made to the survey based on their suggestions. A copy of the final version of the survey is in Figure 2. The survey link to the pre-EMR access survey was sent to the ACSCO employees on October 12, 2015. The survey was closed on October 28, 2015. To encourage participation, one reminder e-mail was sent to ACSCO employees during the open period of the survey.
Figure 2.
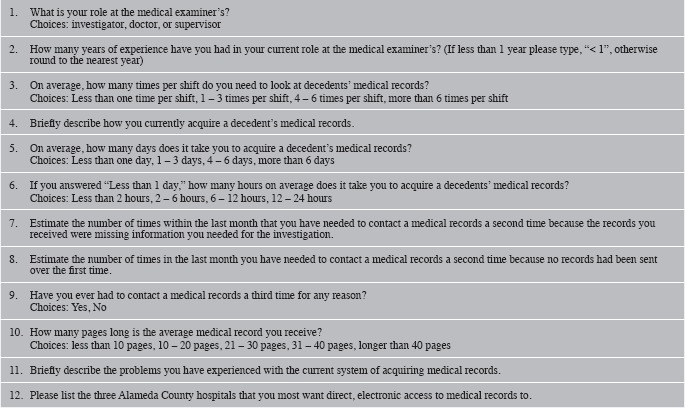
Alameda County Sheriff-Coroner's Office Employee Pre-Electronic Medical Records Access Survey
To measure any changes in baseline data, a post-EMR access survey was also created in Google Forms. The survey was pre-tested by the same two employees who vetted the pre-EMR survey. Due to the similarity to the pre-EMR access survey, the post-EMR access survey underwent only one round of testing. No changes were suggested. A copy of the final version of the survey is in Figure 3. The link to the post-EMR access survey was sent to the ACSCO employees requesting access to hospital EMRs on July 15, 2016. The survey was closed on July 31, 2016. To encourage participation, one reminder e-mail was sent to ACSCO employees during the open period of the survey.
Figure 3.
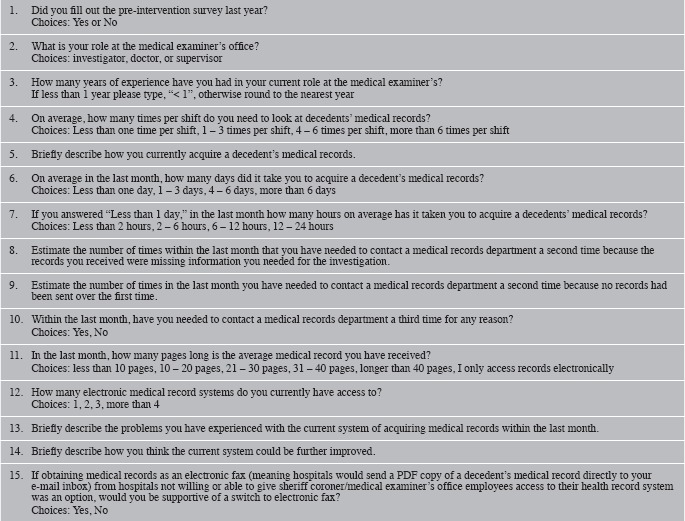
Alameda County Sheriff-Coroner's Office Employee Post-Electronic Medical Records Access Survey
The authors were provided a list of all the hospitals within the ACSCO's jurisdiction along with current contact information for the medical records department at each hospital. Beginning November 2015, the hospitals were contacted to find out if and how login credentials could be assigned to each of the ACSCO employees. The order in which hospitals were contacted was based on the results of question 12 on the pre-intervention survey (Figure 2).
As previously described, all three surveys contained questions that gathered both quantitative and qualitative data. Quantitative results were analyzed in Stata/IC version 14.0. Different statistical tests were used to calculate the significance of results depending on whether the variables were categorical or numerical (21). For all calculations, a p-value < 0.05 was considered significant. The authors operated under the grounded theory research strategy for analyzing qualitative data (20). Qualitative answers were coded and then unified into larger themes by the author using the practical techniques presented by Dr. Ryan Greysen (22).
Results
NAME Needs Assessment
About 5% (36/700) of the forensic pathologists and death investigators subscribed to the NAME listserv responded to the online survey. Not all participants gave responses to every question.
The majority of participants (57%; 20/35) who chose to answer responded that their MDI office receives medical records an average of one to three days after the request is submitted. Twenty-six percent (9/35) of participants answered that it takes less than one day; 3% (1/35) answered four to six days, and 14 % (5/35) answered more than six days.
Nearly half, 46% (16/35), of respondents answered that their MDI office already has some level of EMR access. Having an autopsy facility located in a hospital was significantly correlated with having EMR access (Fisher's Exact Test, p = 0.003).
Of those participants who work in offices that do have some amount of EMR access, 63% (10/16) work in offices that have EMR credentials for both investigators and doctors and 31% (5/16) work in offices that have credentials for doctors or hospital-employed assistants only. Sixty-three percent (10/16) responded that their office has EMR access at multiple facilities and 31% (5/16) responded that their office has access at only one facility. Overall, having EMR access was not significantly associated with average length of time to receive medical records (chi-square statistic 0.9333; p = 0.817). The lack of significance remained when looking specifically at the types of employees who have access (chi-square statistic 4.0238; p = 0.403) or the number of facilities an institution had EMR access at (chi-square statistic 3.8304; p = 0.429).
One third, 33% (12/36), of participants gave an example of a change that their office has tried to make to improve the efficiency of their medical record acquisition process and the barriers that were faced when making that change. One office had attempted reform at the institution level by switching to virtual fax. The respondent wrote,
We stopped printing out records received by fax; instead of the old-fashioned fax machine which prints them as they arrive, we receive a PDF and make that available in our own in-house records system…
Eighty-three percent (10/12) of the offices who have attempted reform are trying to work with hospitals within their jurisdiction or the local government to expedite record acquisition, 80% (8/10) by asking for EMR access.
A majority, 70% (23/33), of respondents felt that medical record providers' fear of the legal ramifications of security breaches was the biggest obstacle to gaining remote EMR access. One respondent wrote,
HIPAA [Health Insurance Portability and Accountability Act]. This is what most institutions cite when this has come up before, even though there is a clear HIPAA exclusion for death investigation; the argument has been that we would have the technical ability to access any patient records, not just those whose death or possible death (as in an unidentified individual) we are investigating. While that argument fails on logic since it is no different from the access hospital staff have (not allowed to access records for anyone except ‘their’ patients, even though they have the technical ability to access anyone's), it is what has been cited…
Another respondent expanded on this idea further by writing,
… I can see hospitals not being comfortable with granting access to individuals who have not undergone their security clearance and who are not a part of their organization.
Other obstacles mentioned included the scope of an office's jurisdiction and the current limitations of EMR systems. One respondent discussed all three, stating that,
Having to somehow register with all the hospitals in the area (we serve 5.5 million people, roughly); teach everyone how to use multiple EMRs; the potential to accidentally access someone else's medical record by mistake is staggering.
In terms of the relationship between MDI and public health, 23% of participants (7/30) indicated that their offices are considered part of the local or state public health department. Fifty-three percent of participants (16/30) responded that their MDI office's role in public health has to do with surveillance, including the discovery of notifiable diseases, trends in causes of death, and consumer product safety. Some respondents cited advocacy as a primary role of MDI in public health, an example of which stated,
Military: Suicide prevention is our #1 problem. Motor vehicle accidents is #2. Family advocacy (child abuse and domestic violence) is #3.
The most commonly reported hindrances to the correct use of MDI data for public health were that differences in cause of death determination and coding lead to skewed data and that MDI data are interpreted incorrectly by certain entities, such as the “media and special interest groups.” One respondent summarized this by writing,
Coding of deaths in certain populations at the government level is not always correct because the persons who created the coding system and persons who use the coding system do not understand the differences in what various causes of death mean (example is that SUID deaths the last time I checked were still coded the same as SIDS). The other issue is the lack of consistency with how medical examiner's certify deaths which is an issue that cannot be completely corrected, but with appropriate CME [continuing medical education] can at least be minimized and become the result of differences in the intellectual approach of the pathologist instead of ignorance of the current recommendations.
Quality Improvement Project at the ACSCO
Many of the complications with the current ACSCO medical record acquisition system were highlighted in the introduction. Over half, 56.5% (10/23), of pre-EMR survey respondents mentioned time delays as being problematic, particularly if the respondent predominantly worked night shifts because medical records departments are only open during regular daytime hours. All respondents cited some form of wasted resources, whether due to lost time spent trying to acquire the appropriate records, the copious amounts of paper used due to the length of faxes, or, as several respondents discuss, the performance of unnecessary autopsies, which,
…can cause families additional cost/suffering when we have to bring cases in to the Coroner's Bureau for examination simply because a hospital/medical office could not provide the needed information in a timely fashion.
Table 1 highlights several results from the pre- and post-EMR access surveys. By the time of the post-EMR access survey, most employees only had access to one EMR system. The majority of respondents in both the pre- and post-EMR access groups answered that they receive records one to three days after requesting them. The association between average length of time to receive records and whether a respondent was answering the pre- or post-access survey was not significant (chi-square statistic = 1.0802; p-value = 0.583). The difference between the pre- and post-EMR access mean number of times ACSCO employees have to call hospitals a second time: 1) was not statistically significant when a second call is made because a record is never received (t-test, p-value = 0.2324) and 2) was not statistically significant when a second call is made because vital information was missing from the record that was received (t-test, p-value = 0.0588). There was, however, a significant reduction in the number of employees who needed to call a medical records office a third time for any reason (Fisher's Exact Test, p = 0.043).
Table 1.
Summary of Alameda County Sheriff-Coroner's Office Survey Results
| Pre-Electronic Medical Records Access Survey | Post-Electronic Medical Records Access Survey | |||
|---|---|---|---|---|
| Participation rate | 19/23 | 83% | 8/23 | 35% |
| Average time to get records | 1 – 3 days | 11/19 (58%) | 1 – 3 days | 5/8 (63%) |
| Average number of times record was not sent in the past month | Range: 0 – 20 times/month | Avg. = 3.8 times/month | Range: 0 – 5 times/month | Avg. = 2.6 times/month |
| Average number of times important information was missing from the record in the past month | Range: 0 – 10 times/month | Avg. = 3.1 times/month | Range: 0 – 8 times/month | Avg. = 1.1 time/month |
| Has needed to make third call to record provider's office in past month | 11/19 | 58% | 1/8 | 13% |
| Average length of faxes | 10 – 30 pages | 10/19 (53%) | 21 – 40 pages | 6/8 (75%) |
Table 2 summarizes the progress of the quality improvement project to date and the barriers to gaining EMR access to several of the health systems within the ACSCO jurisdiction. A major challenge to completing the quality improvement project was finding the employee at each hospital system who has the power to grant EMR access. We began by contacting the medical records department at each institution and, after repeating our project objective and reasoning to several different employees, would typically be transferred up the ladder to the staff member with the appropriate authority. This process could take anywhere from hours to months depending on the institution and often took multiple follow-up phone calls.
Table 2.
Current Status of Alameda County Sheriff-Coroner's Office Quality Improvement Project
| Hospital | Last Action as of August 30, 2016 |
|---|---|
| Alameda Health System - Fairmont Hospital, Highland Hospital, Alameda Hospital, San Leandro Hospital | Denied: Hybrid system (still have paper charts in some departments) |
| Sutter and Sutter-Affiliated - Alta Bates (Ashby and Summit), Eden Medical Center | Log-in credentials with limited access acquired |
| Children's Hospital Oakland | Individual employees need to apply through the online form |
| Kaiser - Emergency Prospective Review Program, Fremont, San Leandro, Oakland, Pleasanton, and Union City | Written request submitted; awaiting Regional Director's reply |
| St. Rose Hospital | Log-in credentials with full access acquired |
| Veterans Affairs Hospital Livermore | Denied: Electronic medical record firewall; D.C. is decision maker for all Veterans Affairs Hospitals |
| Valley Care Medical Center | Denied: Paper charts only |
| Total number of hospitals: 17 |
Another barrier to accessing regional EMR was that two local systems don't have a fully integrated EMR system. The American Recovery and Reinvestment Act of 2009 stipulated that as of January 1, 2014, healthcare systems had to convert to EMR and prove the conversion was successful by demonstrating and documenting “meaningful use” or risk getting less than full Medicare/Medicaid reimbursement (23). Despite the law, two systems in the ACSCO's jurisdiction have not fully transitioned to EMR (23).
The other two barriers we encountered were specific to the Livermore Veteran Affairs Hospital (VAH). Per their Director of Medical Records, individual VAHs cannot make major decisions without consulting the VA Department in Washington, D.C. Getting access to the VAH EMR would require national policy changes. According to the director, the VAH also has a strong firewall that prevents those not on a VAH computer from accessing the system. Apparently, technological workarounds would need to be developed in order for employees at the ACSCO to access the VAH EMR system from the office, even if they could be granted access by the local VAH.
Discussion
This is the first study to examine the process of medical record acquisition at MDI offices in depth. We have shown that inefficiencies in the medical record acquisition process are widespread and that there is need for intervention as timely MDI data is used for public health and safety research, and delays in medical record receipt can lead to resource waste in the forms of investigators' time, paper, and the performance of unnecessary autopsies. Though many MDI offices have made attempts to reform there are perceived and true barriers to change that make reform difficult.
In qualitative research, credibility, dependability, and transferability are the analogous concepts of validity, reliability, and generalizability (20). Credibility is hard to measure; however, the facts that our results offer plausible explanations and are coherent between the NAME survey and ACSCO pre-EMR access survey are evidence of its presence in this study (20). To enhance dependability, the authors altered the research design as findings emerged, adding the NAME needs assessment component a few months after the initiation of the ACSCO pilot project. Using a multi-coder team could have further enhanced dependability. Our study of medical record acquisition is possibly applicable to another environment, though transferability outside of the population of death investigators was not an important component of this project (20). Though the participation rate for the NAME survey was only 5%, the number of participants appeared to reach theoretical saturation. For all open-ended questions, no new themes were generated after reviewing 30 or fewer responses. This gives the authors confidence that the response rate was sufficient for qualitative data.
The same was not true for the quantitative data. The power to calculate a chi-square statistic with a p-value of 0.05 or less with three degrees of freedom (the parameters used when looking for an association between EMR access and average length of time to receive records, was a mere 11% (24). This lack of power could explain why a statistically significant association between EMR access and length of time to receive medical records was not found, although another explanation could be that the complications that arise in dealing with EMR, such as having to learn how to use different systems for different providers or having difficulty with log-in credentials, lead to similar length of delays in record acquisition.
A similar paucity of power was present when comparing the pre-EMR access survey results to the post-EMR access survey results due to the low participation rate in the post-EMR access survey. For example, the power to detect a p-value 0.05 or less for the t-test comparing average number of times a second call needed to be made to a record provider's office because received records were missing vital information was only 58%. A paired t-test would have been the preferred way of comparing the groups since they were matched samples, but the number of participants in each would have needed to be equal (21).
Due to the voluntary nature of the survey instruments, selection bias was almost certainly present in this study. However, to what degree and in which direction this might have influenced the results is unknown.
Recommendations and Future Actions
Mandatory Training for Medical Record Providers
Both the NAME and ACSCO surveys found that medical record providers lack understanding about both the current statutes regarding the HIPAA-exempt status of MDI offices and the importance of timely medical record acquisition for MDI offices. Title 45 of the Code of Federal Regulations, Part 164, Subpart E specifies that,
A covered entity may disclose protected health information to a coroner or medical examiner for the purpose of identifying a deceased person, determining a cause of death, or other duties as authorized by law (25, 26).
NAME survey responses indicate that educating medical record providers about the existence of this regulation has led to minor improvements in paper medical record turnarounds time.
During the quality improvement project, we also found that educating medical record providers about the ACSCO's HIPAA-exempt status was sufficient to assuage security concerns and be granted EMR access. However, as was mentioned by one of the respondents, MDI offices that attempt to replicate this work may find that HIPAA-exempt status is not enough to appease all healthcare institutions. The Sutter and Sutter-affiliated hospital system had a technological solution for this security dilemma. Alameda County Sheriff-Coroner's Office employees now have login credentials for the Sutter EMR system, but can only open the EMRs of approved patients. While this does add an extra step in acquiring these medical records, employees are able to call and get approval at any time of day, including outside of normal business hours.
This recommendation can be a joint venture between MDI offices and the providers within their jurisdiction, can speed paper record acquisition, can possibly convince providers to grant an MDI office EMR access, and is relatively easy to implement.
Standardization of Death Certification and Death Codes
To prevent MDI data from being skewed at the public health level, there should be national standards for completing death certificates and national coding standards. Standardization will help to maintain validity and accuracy of MDI data.
Future Studies to Spur Policy Development and Implementation
Policymakers who want to avoid scandals like the one surrounding the San Francisco medical examiner's office's backlog of 802 cases in 2013 (27) will be interested in implementing any method shown to expedite investigations. Unfortunately, our study did not show significant reductions in length of time to acquire medical records when an MDI office had EMR access. Before policymakers can be convinced that policies mandating MDI offices be given EMR access are a necessity, more studies are needed to directly address why access to records does not improve turn around time. A potential follow-up study that would have adequate power to detect the significance of EMR access could be a national telephone survey of all NAME offices (28).
Footnotes
Disclosures
The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
This work was presented at the 2016 NAME Annual Meeting. The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
References
- 1.Hanzlick R. Medical examiners, coroners, and public health: a review and update. Arch Pathol Lab Med. 2006. Sep; 130(9): 1274–82. PMID: 16948511. 10.1043/1543-2165(2006)130[1274:MECAPH]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.McGowan C.R., Viens A.M. Reform of the coroner system: a potential public health failure. J Public Health (Oxf). 2010. Sep; 32(3): 427–30. PMID: 20335184. 10.1093/pubmed/fdq015. [DOI] [PubMed] [Google Scholar]
- 3.Drake S.A., Nolte K.B. Essential medicolegal death investigation services: standardization of a survey instrument based on the Essential Public Health Services. J Forensic Sci. 2011. Jul; 56(4): 1034–40. PMID: 21496017. 10.1111/j.1556-4029.2011.01783.x. [DOI] [PubMed] [Google Scholar]
- 4.McGowan C.R., Viens A.M. Death investigation systems and disease surveillance. Epidemiol Infect. 2011. Jul; 139(7): 986–90. PMID: 21156100. 10.1017/S0950268810002840. [DOI] [PubMed] [Google Scholar]
- 5.Drake S.A., Cron S.G., Giardino A. et al. Comparative analysis of the public health role of two types of death investigation systems in Texas: application of essential services. J Forensic Sci. 2015. Jul; 60(4): 914–8. PMID: 25786511. 10.1111/1556-4029.12748. [DOI] [PubMed] [Google Scholar]
- 6.Levy B.P. The need for informatics to support forensic pathology and death investigation. J Pathol Inform. 2015. Jun 23; 6: 32 PMID: 26167376. PMCID: PMC4485186. 10.4103/2153-3539.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy B.P. Informatics and forensic medicine: two peas in a pod. Paper presented at: Pathology Informatics Summit; 2014. May 13-16; Pittsburgh, PA. [Google Scholar]
- 8.Dahlberg L.L., Mercy J.A. History of violence as a public health problem. Virtual Mentor. 2009. Feb 1; 11(2): 167–72. PMID: 23190546. 10.1001/virtualmentor.2009.11.2.mhst1-0902. [DOI] [PubMed] [Google Scholar]
- 9.Parrish R.G. Assessing and improving the quality of data from medical examiners and coroners. Proceedings of the International Collaborative Effort on Injury Statistics; 1995; Bethesda, MD. National Center for Health Statistics (DHHS Publication PHS 95-1252). [Google Scholar]
- 10.Hanzlick R., Parrish R.G. The role of medical examiners and coroners in public health surveillance and epidemiologic research. Annu Rev Public Health. 1996; 17: 383–409. PMID: 8724233. 10.1146/annurev.pu.17.050196.002123. [DOI] [PubMed] [Google Scholar]
- 11.Bugeja L., Ibrahim J.E., Brodie L.R. Occupational death investigation and prevention model for coroners and medical examiners. Inj Prev. 2010. Feb; 16(1): 2–6. PMID: 20179026. 10.1136/ip.2009.021808. [DOI] [PubMed] [Google Scholar]
- 12.Bugeja L., Ibrahim J.E., Ozanne-Smith J. et al. Application of a public health framework to examine the characteristics of coroners' recommendations for injury prevention. Inj Prev. 2012. Oct; 18(5): 326–33. PMID: 22200637. 10.1136/injuryprev-2011-040146. [DOI] [PubMed] [Google Scholar]
- 13.Zaki S., Blau D.M., Hughes J.M. et al. CDC Grand Rounds: discovering new diseases via enhanced partnership between public health and pathology experts. MMWR Morb Mortal Wkly Rep. 2014. Feb 14; 63(6): 121–6. PMID: 24522095. [PMC free article] [PubMed] [Google Scholar]
- 14.Levy B.P. Implementation and user satisfaction with forensic laboratory information systems in death investigation offices. Am J Forensic Med Pathol. 2013. Mar; 34(1): 63–7. PMID: 23361076. 10.1097/PAF.0b013e31827ab5c6. [DOI] [PubMed] [Google Scholar]
- 15.Nolte K.B., Hanzlick R.L., Payne D.C. et al. Medical examiners, coroners, and biological terrorism: a guidebook for surveillance and case management. MMWR Recomm Rep. 2004. Jun 11; 53(RR-8): 1–27. PMID: 15192550. [PubMed] [Google Scholar]
- 16.Dibdin J.D. Continuous quality improvement as a management concept for death investigation systems. J Forensic Sci. 2001. Jan; 46(1): 94–7. PMID: 11210931. 10.1520/jfs14917j. [DOI] [PubMed] [Google Scholar]
- 17.Committee on Identifying the Needs of the Forensic Sciences Community, National Research Council. Strengthening forensic science in the United States: a path forward. Washington: National Academies Press; 2009. 352 p. [Google Scholar]
- 18.Steinbrook R. Health care and the American Recovery and Reinvestment Act. N Engl J Med. 2009. Mar 12; 360(11): 1057–60. PMID: 19224738. 10.1056/NEJMp0900665. [DOI] [PubMed] [Google Scholar]
- 19.ACGOV.org - Alameda County's official website [Internet]. Oakland: County of Alameda; c2016. Demographics; 2010 [cited 2016 May 4]. Available from: https://www.acgov.org/about/demographics.htm. [Google Scholar]
- 20.Curry L.A., Nembhard I.M., Bradley E.H. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009. Mar 17; 119(10): 1442–52. PMID: 19289649. 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 21.UCLA Institute for Digital Research and Education [Internet]. Los Angeles: UCLA; c2006. What statistical analysis should I use? [cited 2016 Aug 30]. Available from: http://www.ats.ucla.edu/stat/mult_pkg/whatstat/. [Google Scholar]
- 22.Greysen R. (University of California, San Francisco, San Francisco, CA). Intro to qualitative analysis [Unpublished lecture notes]. Lecture for: Interdisciplinary Master of Public Health Seminar (University of California, Berkeley, Berkeley, CA: ). 2015. Sep 11. [Google Scholar]
- 23.HealthIT.gov [Internet]. Washington: U.S. Department of Health and Human Services; c2016. EHR incentive payment timeline; 2014. Mar 4 [cited 2016 May 4]. Available from: https://www.healthit.gov/providers-professionals/ehr-incentive-payment-timeline. [Google Scholar]
- 24.UCLA Institute for Digital Research and Education [Internet]. Los Angeles: UCLA; c2016. Stata FAQ: How can I compute power for contingency tables in Stata?; [cited: 2016. Aug 30]. Available from: http://www.ats.ucla.edu/stat/stata/faq/chi2power.htm. [Google Scholar]
- 25.HHS.gov - Health information privacy [Internet]. Washington: U.S. Department of Health & Human Services; c2016. Summary of the HIPAA Privacy Rule; [cited 2016 Oct. 10]. Available from: https://www.hhs.gov/hipaa/for-professionals/privacy/laws-regulations/. [Google Scholar]
- 26.U.S. Government Publishing Office (GPO) [Internet]. Washington: U.S. Government Publishing Office; c2016. Electronic code of federal regulations; 2016 Oct 6 [cited 2016 Oct 10]. Available from: http://www.ecfr.gov/cgi-bin/text-idx?SID=363351646d5bb12a2d5e769a7dc7d9b1&mc=true&node=se45.1.164_1512&rgn=div8. [Google Scholar]
- 27.Huet E. S.F. medical examiner lags in ruling on deaths. SFGate [Internet]. 2012. Nov. 23 [cited 2016 May 4]. Available from: http://www.sfgate.com/bayarea/article/S-F-medical-examiner-lags-in-ruling-on-deaths-5006771.php.
- 28.National Association of Medical Examiners [Internet]. Walnut Shade (MO): National Association of Medical Examiners; c2016. Organization directory search results; [cited 2016 May 5]. Available from: https://netforum.avectra.com/eweb/DynamicPage.aspx?Site=NAME&WebCode=OrgResult&FromSearchControl=Yes&FromSearchControl=Yes. [Google Scholar]


