Abstract
The diagnosis of strangulation at autopsy is a persistent challenge for the forensic pathologist. The main difficulty is interpreting the observations made at the postmortem table and deciding whether the observations are a sufficient basis to render an expert opinion that death was caused by external compression of the neck. This may have considerable importance to the criminal justice system and may lead to a conviction for murder. There are five main pitfalls and artifacts encountered in the neck at postmortem examination. These five areas provide the majority of the interpretative difficulties experienced by the pathologist. These challenges include: 1) developmental anatomy of the hyoid bone; 2) triticeous cartilages; 3) Prinsloo-Gordon hemorrhage; 4) postmortem hypostatic hemorrhage; and 5) resuscitation-related neck injury. This review explores these five areas. Awareness of the pitfalls and artifacts in the neck is essential for a satisfactory and evidence-based approach to interpreting observations of the neck at autopsy.
Keywords: Forensic pathology, Postmortem changes, Anatomic variants, Strangulation
Introduction
One of the elementary challenges at autopsy is the correct interpretation of observations made on external and internal examination of the neck. The neck poses considerable difficulties to the forensic pathologist for two main reasons. First, the structures of the anterior neck have anatomical variations and characteristics that make differentiating artifacts from real pathologic findings challenging. Second, the diagnosis of strangulation (and other forms of external neck compression) can be vexing due to the wide spectrum of variation in the injuries associated with pressure applied to the neck (1). Specifically, the range of hemorrhagic lesions associated with neck compression can overlap with artifacts, thus frustrating the forensic pathologist's diagnosis of injury in the neck. In some cases, the artifacts in the neck, variant anatomy of internal neck structures, and the only partially developed pathologic features of strangulation make interpretation of postmortem findings in the neck difficult or impossible even in true cases of neck compression.
However, based upon systematic examination and study of the anterior neck over many years, certain trends have become apparent. The five main pitfalls and artifacts encountered in the neck at autopsy can be classified as follows: 1) development of the hyoid bone; 2) triticeous cartilage; 3) Prinsloo-Gordon hemorrhage; 4) postmortem hypostatic hemorrhage; and 5) resuscitation-related neck injury. These entities account for the majority of the interpretative difficulties experienced at autopsy.
To mitigate the practical difficulties in interpreting autopsy findings in the neck there are two important factors to consider. First, it is essential to dissect the neck properly at postmortem examination. This entails the layer by layer dissection of the anterior neck following vascular decompression of the neck by removal of the brain and the viscera (2). The dissection of the neck is best achieved by a series of incisions that provide for maximal exposure of the ventral, lateral and submental portions of the neck. This dissection can often be extended to involve the face. Second, it is vitally important to proactively recognize the pitfalls and artifacts that may be apparent based upon the history, scene and circumstances surrounding the case. The prepared mind will be unlikely to fall into diagnostic traps related to misinterpretation of observations of no significance.
Discussion
Developmental Segments of the Hyoid Bone
The hyoid bone is a U-shaped bone in the superior anterior neck situated between the larynx and the tongue. The hyoid is part of the hyoid-laryngeal complex which forms the internal hard structures of the throat. One of the persistent difficulties encountered at autopsy is the proper interpretation of the anatomical variations in the hyoid bone. It is known that the hyoid bone may be unilaterally or bilaterally fractured in cases of strangulation. On this basis, discontinuities of hyoid may be rightly or wrongly interpreted as fractures. The main pitfall related to the diagnosis of hyoid fracture is the fact that the hyoid develops in a segmented fashion such that the mature continuous hyoid bone found in adulthood may not be found in all adults, and certainly not found in infants, children, and youths (3). The hyoid is divided up into a horizontal component known as the body of the hyoid, which is present in the ventral aspect of the neck, and two greater cornua, which project posteriorly and slightly superiorly in the neck. The two lesser cornua (which are often very poorly visualized at autopsy) emerge from the body of the hyoid bone and project inferiorly. The greater cornua and the body of the hyoid bone in early development are three separate bony structures which are connected by two synchondrotic joints (4). The synchondrotic joints are composed of fibrous connective tissue, which is heavily collagenized. During the developmental progression of the hyoid bone in adulthood, the synchondrotic joints are progressively ossified. This transforms the three separate bones of the hyoid into one continuous structure. However, the developmental progression is variable in timing, and may not be symmetrical in all people (5,6). On this basis, the synchondrotic joints may be unfused or partially unfused on one or the other side of the hyoid bone. This can result in mobility and flexibility of the greater cornu at the junction point between the greater cornu and the body of the hyoid. This can be misdiagnosed as a fracture unless the developmental anatomy of the synchondrotic joint is known by the prosector. An important clue in diagnosing a fractured hyoid bone is discontinuity of the bone itself with the presence of hemorrhage. In the case where a flexible synchondrotic joint is encountered, hemorrhage will seldom be present without an explanation such as trauma. This is typically sufficient to differentiate a truly fractured hyoid compared to a flexible and unfused synchondrotic joint.
One approach to further elucidating whether a gross flexibility in the hyoid bone is related to fracture or development of the hyoid is the use of radiography. Specifically, plain radiographs of the hyoid bone after excision from the neck can be used to determine if a fracture is present or if a synchondrotic joint explains the apparent discontinuity in the bone. The hyoid bone from a controversial and notable case that was misdiagnosed as strangulation is shown in Image 1. Image 1 shows the hyoid bone of an adult man with obvious segmentation of the greater cornu and the body and two obvious synchondrotic joints at the point of junction between the greater cornu and the body of the hyoid. The synchondrotic joint is more apparent on the right side compared to the left side. This discontinuity, explained by normal developmental variation, was misdiagnosed as a fracture. The radiograph, however, clearly shows the presence of an anatomical joint in the appropriate anatomic location.
Image 1:

Plain radiograph of excised hyoid bone shows synchondrotic joints prior to fusion.
In rare cases, it may be difficult to differentiate between a synchondrotic joint and a fracture. In these cases, histological examination following decalcification of the hyoid bone is often helpful. Furthermore, there is emerging experience with postmortem imaging which will enlarge the arsenal of techniques available to study the hyoid bone in situ prior to neck dissection.
Triticeous Cartilage of the Larynx
The other main forensically-relevant component of the hyoid-laryngeal complex are the triticeous cartilages (7,8). Specifically, triticeous cartilages are small pieces of fibrocartilage that are linear or round, in the millimeter-size range. These cartilages are present in the fibrous connective tissues that link the superior horns of the thyroid cartilage to the suspensory ligaments and soft tissues of the superior anterior neck, adjacent to the hyoid bone (Figure 1). In practice, triticeous cartilages are often very closely associated with the tip of the superior cornu of the thyroid cartilage. The triticeous cartilages are commonly bilateral although they may be asymmetrical. The main pitfall associated with triticeous cartilages is the misdiagnosis of fractures of the superior cornu of the thyroid cartilage. This is of great practical relevance because the most common fracture associated with strangulation is fracture of the superior cornu of the thyroid cartilage. Usually such fractures are present at the base of the superior cornua (the junction point of the superior cornu to the lamina); however, sometimes the tips or distal one-third of the superior cornu are fractured in cases of strangulation. Thus, triticeous cartilages present the same pitfall as the synchondrotic joint of the hyoid bone. The apparent discontinuity in the fibrocartilage emanating from the superior cornu of the thyroid cartilage can mimic fracture. This is a common basis for misdiagnosis of laryngeal fractures in cases where strangulation is considered but is not obvious. One of the main mainstays of differentiating laryngeal fracture from triticeous cartilages is the presence of hemorrhage. However, if interpretative difficulties persist after careful macroscopic examination, histological examination is often helpful. Histologically, triticeous cartilages are characterized by fibro-cartilaginous islands that are completely surrounded by perichondrium. On this basis, histological examination is usually definitive evidence that can be used to differentiate a fracture from a triticeous cartilage. Specifically, in the case of a fracture, the actual fracture line will pass through the cartilage itself and there will be no evidence of perichondrium surrounding the apparently fractured edge of the cartilage.
Figure 1:
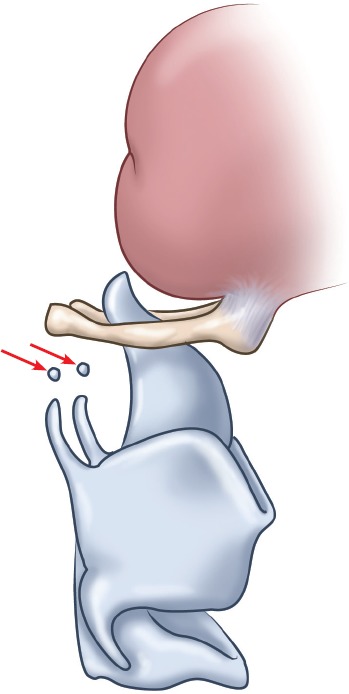
Diagram of the hyoid-larynx complex showing triticeous cartilages (arrows). Drawn under contract with professional medical illustrator Diana Kryski.
It is also worth mentioning that additional anatomic variations of the larynx are frequently encountered at autopsy. The most common developmental variation in the larynx, beyond triticeous cartilages, is aplasia of the superior cornu of the thyroid cartilage, which can be unilateral or bilateral.
Prinsloo-Gordon Hemorrhage
One of the most frequent hemorrhagic artifacts present at routine medicolegal autopsies is the so-called Prinsloo-Gordon hemorrhage. These hemorrhages were the topic of intensive study by the South African forensic pathologists, Prinsloo and Gordon, which culminated in their landmark paper on the subject (2). Further contributions on extending the concept of the Prinsloo-Gordon hemorrhage was provided by two British forensic pathologists, Camps and Hunt, in their important paper in 1959 (9).
Prinsloo and Gordon called attention to the misinterpretation of extravasation of blood into the soft tissues of the neck, entirely due to dissection, as a mimic of bruising related to trauma. Essentially, handling (blunt dissection) and incising congested blood vessels (sharp dissection) can cause blood to track between and within the strap muscles. These authors showed that by dissecting the neck after vascular decompression, such “hemorrhages” could be avoided. Thus, the layered dissection of the neck was introduced to medicolegal autopsy work in the 1950s.
Camps and Hunt extended this concept by generalizing it to include hemorrhages that emerge from congested blood vessels in the perimortem periods; specifically, posterior pharyngeal hemorrhage. This hemorrhage is present in the adventitia of the posterior pharyngeal wall and sometimes may involve the intramural components of the posterior pharynx (Image 2). These hemorrhages may be only localized to the upper posterior pharynx or may extend extensively along the posterior pharyngeal wall and spread into the posterior mediastinum. Such hemorrhages are perimortem or postmortem in origin and are related to the nearly unique venous anatomy of the posterior pharyngeal wall. The veins of the posterior pharynx are organized in an extensive anastomosing array of small, thin-walled channels known as the laryngo-pharyngeal venous plexus. In the agonal period, if there is congestion of the veins cephalad to the heart, the engorgement of the laryngeo-pharyngeal plexus can result in rupture. This results in hemorrhagic infiltration of the posterior pharyngeal tissues. This is often present in cases of sudden cardiac death where there is florid congestion of the head and neck, particularly in large men. The main pitfall with the Prinsloo-Gordon hemorrhage has been to confuse this artifact with hemorrhages that may occur with strangulation.
Image 2:
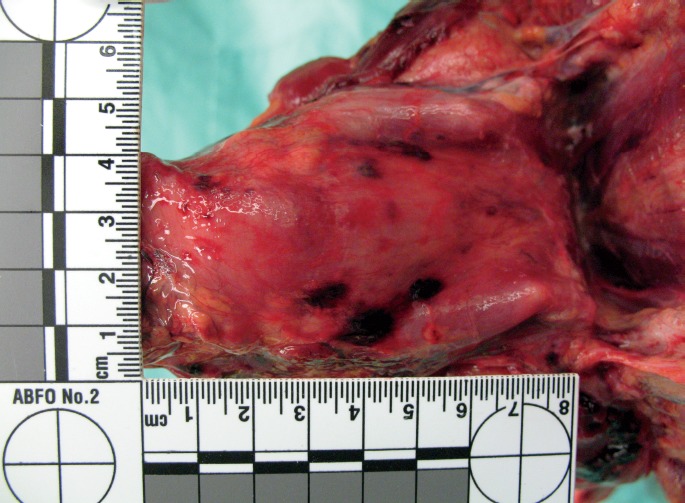
Prinsloo-Gordon hemorrhage in the posterior wall of the pharynx.
Furthermore, the Prinsloo-Gordon hemorrhage and the associated laryngeal pharyngeal venous plexus has proven to be an excellent model to understand other hydrostatic-related hemorrhagic phenomenon, such as the postmortem hypostatic hemorrhage, which is discussed below. Interestingly, a Prinsloo-Gordontype mechanism also explains the artifactual hemorrhages that occur in the spinal epidural space, typically in infants and children. Specifically, postmortem distension and rupture of the meningo-rachidian venous plexus (the complex series of venous channels in the spinal epidural space) leads to artifactual epidural hemorrhage that must not be misdiagnosed as traumatic epidural hemorrhage (10).
Postmortem Hypostatic Hemorrhage
The postmortem hypostatic hemorrhage is the extravasation of blood into the interstitium when two conditions are met (11). First, a congested venous plexus is distended with blood due to the gravitational effects of livor mortis. Second, there is loss of vascular integrity of the venous channels due to autolysis or decomposition. When these two factors operate together, the combined effect is the formation of focal perivascular extravasation of blood or extensive interstitial infiltration of blood. The most commonly encountered and trivial examples of this phenomenon are the small, postmortem hemorrhages that occur in the skin in cases of hanging with pronounced lividity in the lower extremities. These postmortem hypostatic petechial hemorrhages (often known as Tardieu spots) are a typical example of postmortem hypostatic hemorrhages.
However, when postmortem hypostatic hemorrhages occur in the anterior neck, their presence may wrongly signal the possibility of strangulation. Specifically, if a case of sudden and unexpected death occurs with the body in the prone position (or the head down position) there may be extensive livor mortis (postmortem hypostasis) involving the face and neck which may result in hypostatic hemorrhages within the soft tissues of the neck. Most experienced forensic pathologists have encountered such cases and are familiar with the range of hemorrhagic artifacts that can occur in the neck. Images 3 through 6 show a range of postmortem cases of hypostatic hemorrhages involving the scalp, face, eye, and neck and reveal the remarkable spectrum of the postmortem hypostatic hemorrhage. The most extensive postmortem hypostatic hemorrhages are present in the fibrous connective tissue between strap muscles, within the endomyomesium of the strap muscles, within the galea of the scalp, and within the subconjunctival connective tissues. The phenomenon can even cause retrobulbar perioptic nerve sheath hemorrhage.
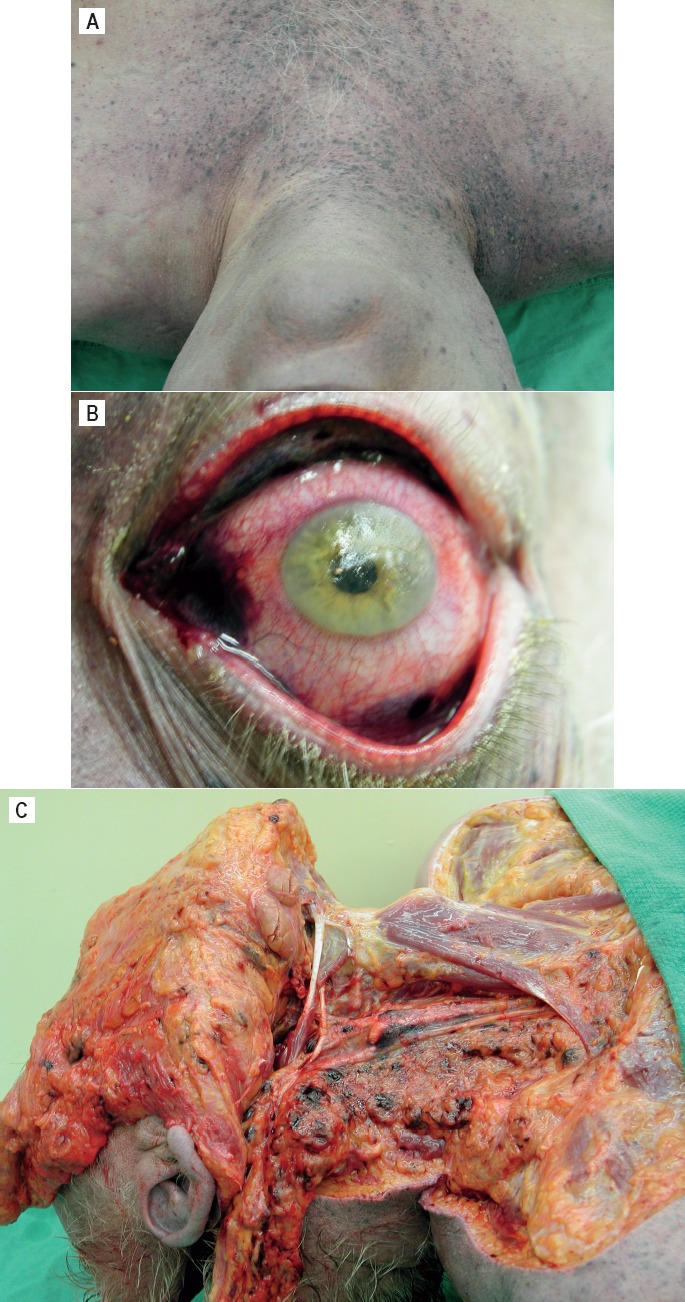
Image 3:
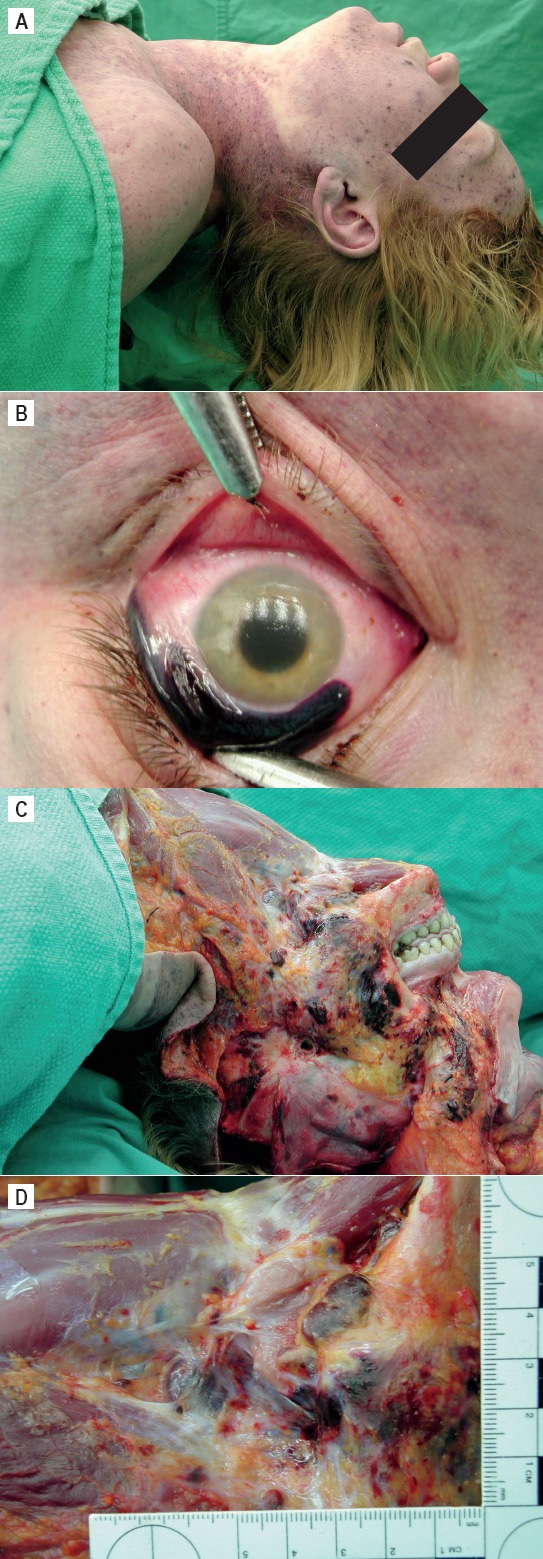
Postmortem hypostatic hemorrhages in a 36-year-old female who died of multiple drug intoxication and was found in the prone position. A) Left side of neck and face with extensive postmortem hypostasis (lividity). B) Marked diffuse subconjunctival hemorrhage. Postmortem hypostatic hemorrhages in a 36-year-old female who died of multiple drug intoxication and was found in the prone position. C) Hypostatic hemorrhages in the subcutaneous tissues of the left side of the face. D) Hypostatic hemorrhages in the subcutaneous tissues of the left upper neck.
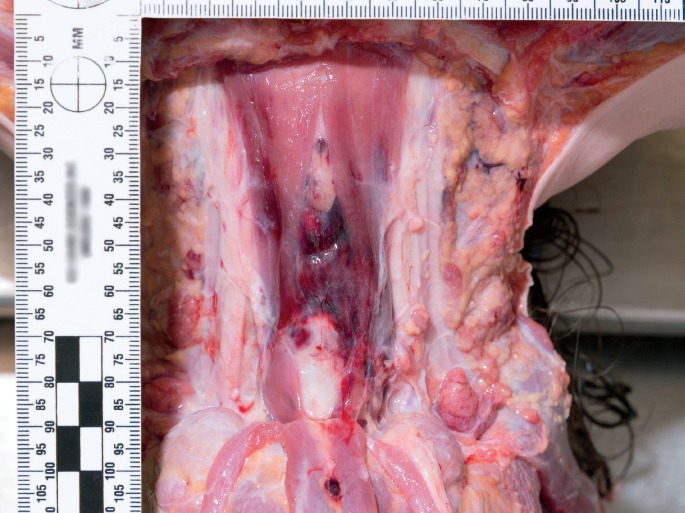
Image 6:
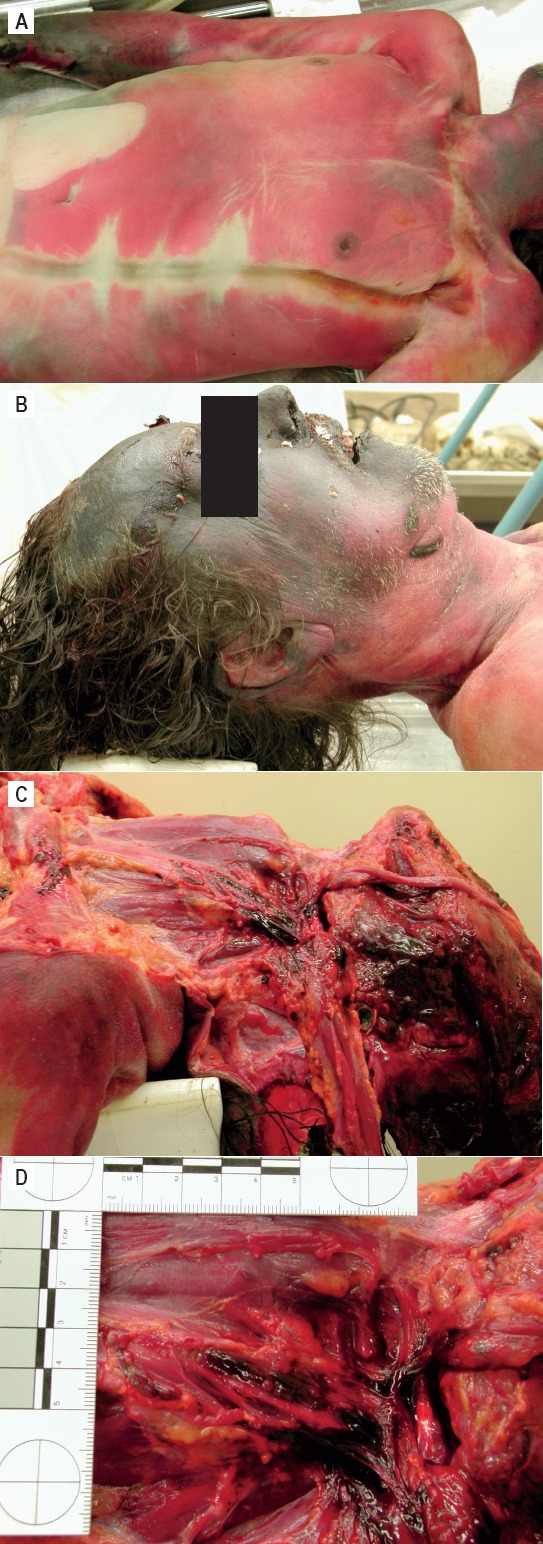
Postmortem hypostatic hemorrhages in a 52-year-old male who died of diphenhydramine intoxication and was found in the prone position in a moderately advanced state of decomposition. A) Decomposition and lividity of the chest. B) Decomposition and lividity of the face and neck. Postmortem hypostatic hemorrhages in a 52-year-old male who died of diphenhydramine intoxication and was found in the prone position, in a moderately advanced state of decomposition. C and D) Hypostatic hemorrhage in the neck.
Image 4:
Postmortem hypostatic hemorrhages in an adult male who died of multiple drug intoxication and was found in the prone position. A) Marked hypostasis and petechial hypostatic hemorrhage in the upper chest and neck. B) Marked subconjunctival hemorrhage. Postmortem hypostatic hemorrhages in an adult male who died of multiple drug intoxication and was found in the prone position. C) Hypostatic hemorrhages in the tissues of the right neck.
Image 5:
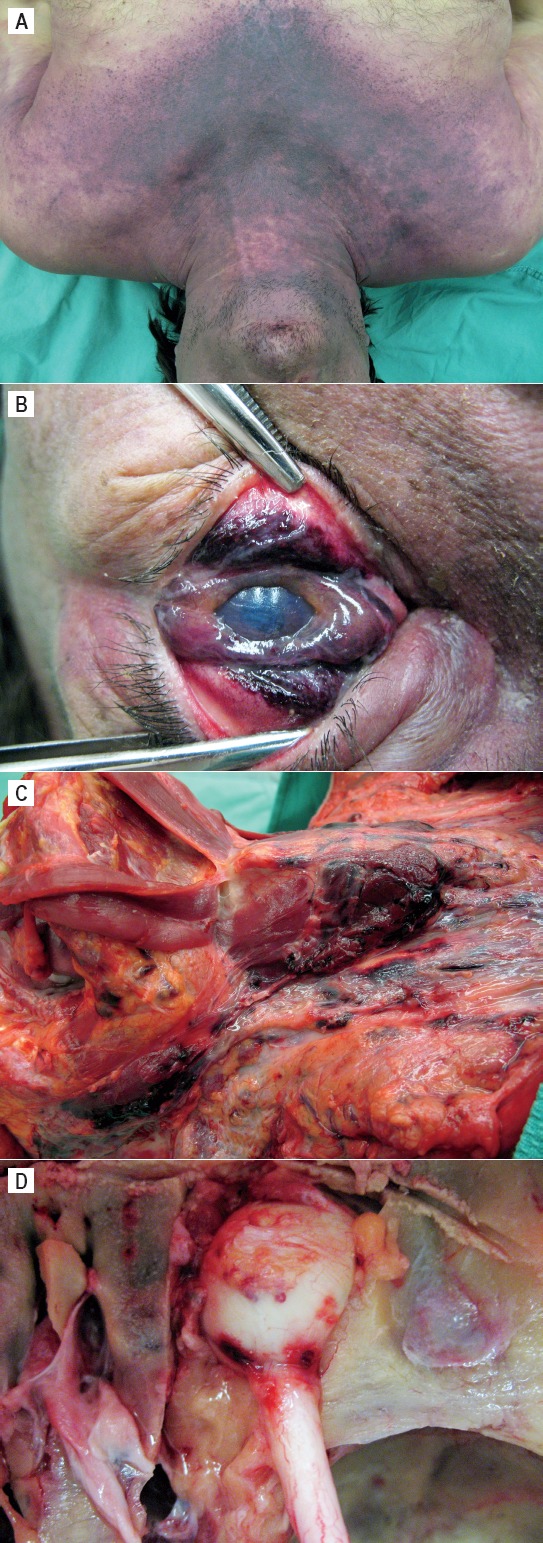
Postmortem hypostatic hemorrhages in a 48-year-old male who died of bronchopneumonia due to chronic alcoholism and was found in the prone position. A) Marked hypostasis and petechial hypostatic hemorrhage in the upper chest and neck. B) Marked diffuse subconjunctival hemorrhage. Postmortem hypostatic hemorrhages in a 48-year-old male who died of bronchopneumonia due to chronic alcoholism and was found in the prone position. C) Hypostatic hemorrhages in the tissues of the right neck, mostly in the carotid sheath. D) Hypostatic hemorrhage of the posterior periscleral tissues and the retrobulbar optic nerve sheath.
It can be difficult to differentiate the hemorrhages associated with postmortem hypostasis from true bruising caused by strangulation. However, the diagnosis of strangulation can usually be correctly ascertained by careful examination of the other structures of the neck, as well as the presence of external injuries on the neck. Despite this assertion, miscarriages in justice related to over interpretation of these pseudo-injuries have been documented (12).
Our understanding of the nature of postmortem hypostatic hemorrhages in the neck has been facilitated by an experimental cadaveric model that allows for the controlled induction of hypostatic neck hemorrhages (11). Briefly, in a series of experiments with donated cadavers, the postmortem hypostatic hemorrhage was created through the combination of body position and autolysis. In the experimental protocol, bodies donated for medical research were placed in the prone position for a period of 48 hours shortly after death. The position was used to concentrate the development of lividity in the ventral neck. Subsequent dissection of the neck using the layer by layer technique revealed a range of subcutaneous and intramuscular hemorrhages that were, in some cases, surprisingly similar to those present in strangulation (Image 7). On the basis of these results, there is both practical case-based evidence and experimental evidence that postmortem hypostatic hemorrhage is a robust phenomenon in medicolegal casework.
Image 7:
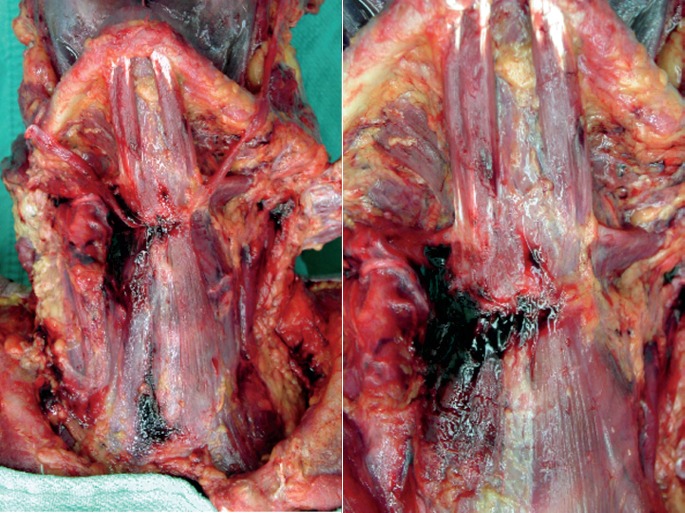
Experimentally induced postmortem hypostatic hemorrhages in the neck, in the model described in reference 10.
Resuscitation-Related Neck Injuries
There are three main resuscitation-related neck injuries that can lead to observations that overlap with strangulation (13-15). The most common is injury to the sternomastoid muscle associated with the placement of a cannula in the internal jugular vein. Often during resuscitation, a central line is placed in the internal jugular vein through a puncture in the lateral aspect of the neck. The course of the cannula may perforate the main body of the sternomastoid muscle. This may lead to intramuscular hemorrhage within the belly of the sternomastoid muscle, which often dissects between muscle bundles causing a hematoma. In some cases it is necessary to clearly differentiate this intramuscular hemorrhage from bruising sustained from neck compression. This can usually be ascertained by careful examination of the overlying skin which will show needle puncture. However, in some cases, a needle puncture may not be readily apparent. On this basis, a careful layer by layer dissection of the neck with exposure of the internal jugular vein often will provide conclusive evidence that an attempt to place a cannula has occurred. Specifically, there will be a needle puncture in the wall of the internal jugular vein with focal perivascular hemorrhage.
Another frequent resuscitative artifact encountered in the neck is laryngeal mucosal hemorrhage and edema which is related to endotracheal intubation (13). Furthermore, if there is a difficult intubation, there may be edema and hemorrhage involving the entire glottis and extending into the epiglottis with maximal involvement of the aryepiglottic folds. The mucosal hemorrhages caused by intubation overlap in nature with hemorrhages that are frequently observed in the laryngeal mucosa in cases of strangulation. However, this seldom gives rise to practical difficulties because when laryngeal hemorrhages are present in strangulation, usually there are other indicators of external neck compression.
The third most frequent (but comparative rare) injury associated with resuscitation is laryngeal fracture as a consequence of cricoid pressure. Cricoid fractures are rarely encountered at medicolegal autopsy and are most frequently due to strangulation. However, in the case of resuscitation with difficult intubation it may be necessary for the resuscitator to manually stabilize the larynx by digital pressure applied to the cricoid. This may give rise to paralaryngeal hemorrhage or fracture. On a practical basis, if laryngeal injuries from resuscitation are a possible consideration in a case, it is frequently necessary to obtain a detailed history of the precise resuscitative measures attempted by paramedics and emergency room personnel. This is usually sufficient to resolve the issue of whether cricoid pressure was a factor in causing the laryngeal injuries.
Other Entities
There are other causes of strap muscle hemorrhage that may not relate to external neck compression. Perhaps the best described alternative cause is drowning (16-18). In some cases of drowning, there is extensive acute hemorrhage within the strap muscles of the neck, often involving the platysma. The hemorrhages are often symmetrical and streaky and run along the longitudinal bundles of the strap muscles. The precise mechanism for how these hemorrhages occur is not known, but it has been suggested that violent struggling with contraction of the neck musculature during drowning may be responsible for this form of intramuscular hemorrhage. These hemorrhages are usually more extensive than the hemorrhages observed with strangulation and are always associated with a history of immersion in water and drowning.
Finally, blunt impact trauma to the neck can produce the same range of injuries in the soft and hard tissues of the neck as are encountered in strangulation. These injuries are either produced by hitting the neck or thrusting the neck against an unyielding surface (19). The medicolegal issue in such cases is to differentiate between injuries produced by impact rather than compression. The main guide is the presence of petechial hemorrhages in the eyes and face. Compression of the neck gives rise to petechiae, whereas a simple impact to the neck does not cause jugular venous compression with increased intravenous pressure that is required to rupture blood vessels and cause petechial hemorrhages (Image 8).
Image 8:
Bruising in the central anterior neck likely related to blunt impact neck trauma in a toddler who died under criminally suspicious circumstances.
Conclusions
Awareness of the anatomical variations, postmortem artifacts and other pitfalls in the neck is essential for forensic pathologists. The neck represents a critically important anatomical structure in forensic pathology due to the persistent diagnostic challenges associated with strangulation and other forms of neck compression. It is essential that increased awareness be developed in this area of forensic pathology through the publication of case reports and case series that document the spectrum of variation associated with the various categories that are described in this review. Only through the systematic analysis of these observations can we develop a satisfactory and evidence-based approach to interpreting observations of the neck made at autopsy.
ACKNOWLEDGEMENTS
I thank many of my colleagues who have provided me with their feedback and input on the subject of this review, over the course of many years. These include Drs. Stephen Cordner, Noel McAuliffe, Jacqueline Parai, Christopher Milroy, Kristopher Cunningham, Jack Crane, Charles Hirsch, and David Chiasson. I would also like to recognize the technical assistance of Jeff Arnold and David Clutterbuck in the preparation of the images for this review.
Footnotes
Financial Disclosure
The author has indicated that he does not have financial relationships to disclose that are relevant to this manuscript
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The author, reviewers, editors, and publication staff do not report any relevant conflicts of interest
References
- 1.Pollanen M.S. A triad of laryngeal hemorrhages in strangulation: a report of eight cases. J Forensic Sci. 2000. May; 45(3): 614–8. PMID: 10855967. [PubMed] [Google Scholar]
- 2.O'Halloran R.L., Lundy J.K. Age and ossification of the hyoid bone: forensic implications. J Forensic Sci. 1987. Nov; 32(6): 1655–9. PMID: 3430133. [PubMed] [Google Scholar]
- 3.Prinsloo I., Gordon I. Post-mortem dissection artifacts of the neck; their differentiation from ante-mortem bruises. S Afr Med J. 1951. May 26; 25(21): 358–61. PMID: 14855047. [PubMed] [Google Scholar]
- 4.Kanetaka H., Shimizu Y., Kano M., Kikuchi M. Synostosis of the joint between the body and greater cornu of the human hyoid bone. Clin Anat. 2011. Oct; 24(7): 837–42. PMID: 21538567. 10.1002/ca.21183. [DOI] [PubMed] [Google Scholar]
- 5.Pollanen M.S., Chiasson D.A. Fracture of the hyoid bone in strangulation: comparison of fractured and unfractured hyoids from victims of strangulation. J Forensic Sci. 1996. Jan; 41(1): 110–3. [PubMed] [Google Scholar]
- 6.Di Nunno N., Lombardo S., Costantinides F., Di Nunno C. Anomalies and alterations of the hyoid-larynx complex in forensic radiographic studies. Am J Forensic Med Pathol. 2004. Mar; 25(1): 14–9. PMID: 15075682. 10.1097/01.paf.0000113931.49721.e4. [DOI] [PubMed] [Google Scholar]
- 7.Grossman J.W. The triticeous cartilages. Am J Roentgenol Radium Ther. 1945; 53(2): 166–70. [Google Scholar]
- 8.Alqahtani E., Marrero D.E., Champion W.L. et al. Triticeous cartilage CT imaging characteristics, prevalence, extent, and distribution of ossification. Otolaryngol Head Neck Surg. 2016. Jan; 154(1): 131–7. PMID: 26556461. 10.1177/0194599815615350. [DOI] [PubMed] [Google Scholar]
- 9.Camps F.E., Hunt A.C. Pressure on the neck. J Forensic Med. 1959; 6(3): 116–135. [Google Scholar]
- 10.Rutty G.N., Squier W.M., Padfield C.J. Epidural haemorrhage of the cervical spinal cord: a post-mortem artefact? Neuropathol Appl Neurobiol. 2005. Jun; 31(3): 247–57. PMID: 15885062. 10.1111/j.1365-2990.2004.00633.x. [DOI] [PubMed] [Google Scholar]
- 11.Pollanen M.S., Perera S.D., Clutterbuck D.J. Hemorrhagic lividity of the neck: controlled induction of postmortem hypostatic hemorrhages. Am J Forensic Med Pathol. 2009. Dec; 30(4): 322–6. PMID: 19901802. 10.1097/paf.0b013e3181c17ec2. [DOI] [PubMed] [Google Scholar]
- 12.Pollanen M.S. Forensic pathology and the miscarriage of justice. Forensic Sci Med Pathol. 2012. Sep; 8(3): 285–9. PMID: 22116733. 10.1007/s12024-011-9299-5. [DOI] [PubMed] [Google Scholar]
- 13.Raven K.P., Reay D.T., Harruff R.C. Artifactual injuries of the larynx produced by resuscitative intubation. Am J Forensic Med Pathol. 1999. Mar; 20(1): 31–6. PMID: 10208333. 10.1097/00000433-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Buschmann C.T., Tsokos M. Frequent and rare complications of resuscitation attempts. Intensive Care Med. 2009. Mar; 35(3): 397–404. PMID: 18807013. 10.1007/s00134-008-1255-9. [DOI] [PubMed] [Google Scholar]
- 15.Olds K., Byard R.W., Langlois N.E. Injuries associated with resuscitation – an overview. J Forensic Leg Med. 2015. Jul; 33: 39–43. PMID: 26048495. 10.1016/j.jflm.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Carter N., Ali F., Green M.A. Problems in the interpretation of hemorrhage into neck musculature in cases of drowning. Am J Forensic Med Pathol. 1998. Sep; 19(3): 223–5. PMID: 9760085. 10.1097/00000433-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Püschel K., Schulz F., Darrmann I., Tsokos M. Macromorphology and histology of intramuscular hemorrhages in cases of drowning. Int J Legal Med. 1999; 112(2): 101–6. PMID: 10048667. 10.1007/s004140050210. [DOI] [PubMed] [Google Scholar]
- 18.Alexander R.T., Jentzen J.M. Neck and scleral hemorrhage in drowning. J Forensic Sci. 2011. Mar; 56(2): 522–5. PMID: 21198626. 10.1111/j.1556-4029.2010.01636.x. [DOI] [PubMed] [Google Scholar]
- 19.Bux R., Padosch S.A., Ramsthaler F, Schmidt P.H. Laryngohyoid fractures after agonal falls: not always a certain sign of strangulation. Forensic Sci Int. 2006. Jan 27; 156(2-3): 219–22. PMID: 16024196. 10.1016/j.forsciint.2005.05.030. [DOI] [PubMed] [Google Scholar]


