Abstract
Postmortem changes can both mask and mimic trauma, impairing interpretation of the injuries. Bones, while capable of surviving the postmortem period relatively intact, are not immune from these effects. Without attached soft tissue to aid an examiner, it can be difficult to determine the time frame of a fracture's occurrence (i.e., before death, at death, or after death). Bones are composed of both organic and inorganic material, each of which contribute to the biomechanical properties of the bones. With the loss of organic material, the biomechanical response of bones to trauma changes; however, the organic material can remain a part of the bone for an extended period after death. Bone with intact organic material is wet bone, and bone without the organic material is dry bone, and because of this difference, fractures of wet bone can appear different than fractures of dry bone. Important in distinguishing the two are differential coloration, various features of the fracture itself (e.g., angle, surface, outline), surrounding flaking of the cortex, and incomplete separation of bone fragments from the fracture. However, the changes are not absolute, and determination of the two types of fractures can be problematic. Although the terms antemortem, perimortem, and postmortem have been used to describe the general time frame of fractures in relation to the time of death of the individual, because of confusion among specialties regarding the definition of “perimortem,” its use may best be discontinued in favor of a descriptive approach when fractures are identified in skeletal remains.
Keywords: Forensic pathology, Postmortem changes, Anthropology, Fractures, Perimortem
Introduction
Postmortem changes introduce artifacts to the body that a forensic pathologist must distinguish from trauma (1). In addition, these postmortem changes can mask actual trauma (1). Although it may seem counterintuitive, one area of the body where postmortem changes affect the accurate assessment of injury is the skeleton; specifically, the timing of fractures.
Identification of hemorrhage in the surrounding soft tissue assists a forensic pathologist in helping to determine the time frame for the occurrence of a fracture in relation to the time of death (i.e., antemortem or postmortem). For example, in general, a fracture sustained just before the time of death or at the time of death will have hemorrhage in the surrounding soft tissue, while a fracture sustained even shortly after death (e.g., fracture of the hyoid bone caused by removal of the neck organs at autopsy or infant rib fractures caused by cardiopulmonary resuscitation) will have an absence of hemorrhage (or relative absence of hemorrhage) in the surrounding soft tissue (2,3). However, as the length of time from the death of the individual to the discovery of the body increases, decomposition, ultimately with loss of soft tissue, makes the determination of the timing of skeletal trauma in relation to the time of death more dependent upon osteologic features alone, unless microscopic techniques are employed (4). The purpose of this paper is to assist in the understanding of the use of osteologic features alone to make a determination of the time of the fracture in relation to the time of death, and the inherent difficulties therein.
To describe the relation of an injury to the actual time of death, both forensic pathologists and forensic anthropologists have used the terms antemortem, perimortem, and postmortem. However, while the use of the term antemortem is similar between the two groups, always referring to injuries sustained prior to death, the context for the use of the terms perimortem and postmortem has varied between the two specialities, with fractures determined to be perimortem by the forensic anthropologist having an actual time range since death that overlaps with the time range of trauma determined to be postmortem by the forensic pathologist (5,6). For example, in one case, a forensic anthropologist may determine that a fracture was perimortem based upon their examination alone, with subsequent history revealing that the fracture of the bone occurred two months after death, in what a forensic pathologic would normally consider the postmortem period. The reason for this discrepancy is based upon the condition of the remains each group tends to evaluate and the presence or absence of soft tissue changes to aid in the determination (4,7). One important point to appreciate is that while the terms antemortem, perimortem, and postmortem have been used to indicate time frames, it is not length of time since death that most affects the condition of the bone and appearance of resultant fractures, but instead the environment in which the body decomposes (5, 8, 9).
For the forensic anthropologist, usually lacking the contributing information of the surrounding soft tissue to aid in their examination, the distinction between perimortem fractures and postmortem fractures most often must be made by examination of the bone alone, and the difference between a perimortem or postmortem determination is based upon recognition of osteologic features that vary depending upon whether the fractured bone was wet or dry. Wet bone represents bone with intact, or relatively intact, organic matrix, whereas dry bone represents bone with loss of the organic matrix (5). The fracture patterns produced by trauma inflicted on wet bone or dry bone can be different because each may respond to trauma in a different fashion (5). For example, bowing fractures depend upon the presence of the organic matrix and should not occur in dry bone (10).
As such, for a forensic anthropologist, since wet bone can remain in such a state for a long period of time after death, what is interpreted as a perimortem fracture could be from trauma that occurred within a range of anywhere from days before death to weeks to months or longer after death (5,11), whereas for the forensic pathologist, if they choose to use to term, “perimortem,” the time frame is much more narrow, indicating the time immediately around death, either just before, during, or just after. Determining the time frame for when fractures were sustained in relation to the time of death can be of vital importance in the investigation of a death; however, despite reported differences in the characteristics of the fractures during each of the two time periods and supported by statistical analyses of study groups (12-16), reliable determination of whether a specific fracture is perimortem or postmortem is not necessarily an easy, or even in some cases, an achievable task (12, 13, 17). Highlighting the difficulties with interpretation of perimortem versus postmortem fractures, Cappella et al. presented the results of 210 fractures of known origin reviewed by two experienced forensic anthropologists, with an error rate of 16.7% for perimortem fractures of cortical long bone and an error rate of 15.9% for postmortem fractures of cortical long bones (18). Of note, the error rates were much higher (i.e., 83-84%) for interpretation of perimortem and postmortem fractures of trabecular bone or flat bones.
Case Report
A funeral home, when cleaning its facility, identified a mummified fetus, which was reportedly found in a trunk that had not been used by the funeral home in decades. The finding was reported to the coroner, who requested the assistance of the medical examiner. A hospital computed tomography scan obtained by the coroner prior to transport of the remains to the medical examiner and read by a hospital radiologist identified a fracture of the right femur and skull fractures. External examination revealed a completely mummified body, with a generalized gray to brown-gray discoloration of the skin (Image 1). There was brown head hair with an estimated average length of 2.5 cm. Scattered around the body, but prominently on the buttocks and lower extremities, were variably sized round defects up to several millimeters, some of which were confluent, representing postmortem insect activity. There were female external genitalia and the foot length was 6.7 cm. The gestational age, based upon foot length (19), was around 35 weeks, or, based upon the presence of the ossification centers for the distal epiphysis of the femora and for the proximal epiphysis of at least one of the tibia, around 36-40 weeks (20). As the mummified state of the body would affect measurement of the foot length, but not the presence of the secondary centers of ossification, the actual gestational age was most likely around term. Given the mummified state of the body, the determination of liveborn versus stillborn was impossible. After completion of an external examination, the medical examiner soaked the desiccated remains in water for several weeks, which rehydrated the soft tissue and allowed the medical examiner to dissect the remains and remove each individual skeletal element. There were fractures of the bones of the cranium (Image 2) and an incomplete fracture of the right femur, in that the shaft of the bone was still intact. The defects in the cranium were fractures and not normal sutures, as the fracture lines were in locations unoccupied by normal sutures, and the cranium was fragmented into smaller pieces of flat bone than would normally be present. The appearance of the right femoral fracture (i.e., a butterfly fracture morphology (Image 3) with incomplete separation of the shaft at the site of the fracture) suggested the bone was most likely wet, and not dry, at the time the fracture occurred, and therefore, the fracture would not be an artifact of the mummification and subsequent handling of the body. In addition, the fracture surface and the surrounding cortical surface were stained dark red-black, in contrast to the contralateral femur (Image 4). The staining may have represented hemorrhage. Of note, as reported by Ubelaker and Adams (21) and Wheatley (12), butterfly fractures can be a postmortem occurrence. The presence of the fractures suggested at least two scenarios for the death of the fetus: 1) birth followed by inflicted head trauma and an inflicted injury of the right thigh or 2) intrauterine trauma, such as if the mother of this infant was involved in a severe accident, such as a motor vehicle collision, and the fetus was stillborn due to the trauma.
Image 1:

Mummified fetus. The white arrow indicates the circular defects in the skin, consistent with prior evidence of insect activity.
Image 2:

Skeletal elements from remains, including cranium. Illustrated are multiple sections of the cranium from the mummified remains. Although normal suture lines (the serrated edges, e.g., the white arrow) are present, there are also sharp lines, where no normal suture line is present (red arrows), and small fragments of flat bone, not corresponding to normal complete cranial bones or normal segments of individual cranial bones (double white arrows).
Image 3:

Fracture of right femur. Note that the fracture of the right femur has a butterfly morphology. The white material on the bone is adipocere.
Image 4:

Left and right femur. The right femur (bottom) has a fracture (white arrow). Note the dark red-black discoloration of the surrounding cortex in contrast to the left femur above.
Discussion
While not defined in Stedman's medical dictionary (22), the term perimortem, derived from the Greek prefix, “peri,” meaning “around” or “near” and the Latin base, “mort,” meaning “death” (23), could be defined as “ around the time of death.” However, as described above, the boundaries of the time frame used for this term differ between forensic pathologists and forensic anthropologists. This difference and the reason for the difference is important to appreciate, as forensic pathologists consult forensic anthropologists, and misunderstanding of the use of the term, “perimortem,” could cause confusion. In fact, because of confusion with the use of this term and its inconsistent meaning across forensic specialties, discontinuation of its use is advocated (6,16).
The concept of wet bone and dry bone is important in understanding the distinction between perimortem fractures and postmortem fractures, as wet bone is more flexible because of its higher moisture and collagen content (8) and should fracture in a different manner than dry bone, and thus, exhibit morphologic differences that can be used to distinguish between the two time periods when evaluating skeletal trauma (5). Wet bone is alternatively called fresh or green bone (8). Perimortem fractures occur in wet bone and postmortem fractures occur in dry bone. However, there are no absolute time frames for the transition from wet to dry bone, as the state of the bone is very dependent upon the many factors that affect the rate of decomposition, including the environment in which it is placed (5). Bodies in wet environments (e.g., under the water table), bodies with saponification, or bodies with retention of decompositional fluid may retain wet bones, and thus, can develop perimortem fractures for a long period after death (8).
After bone is dried, it is more brittle than wet bone, fracturing with less deformation due to force (24). For example, energy delivered to dry bone can cause crushing of the bone and complete loss of anatomic relationships, while severe trauma to a wet bone can still allow for maintenance of anatomic relationships (25). Wet bone tends to splinter, so fractures tend to have irregular edges and small fragments of bone that are attached to the fracture margin, because the periosteum and other soft tissue was still present when the injury occurred (25,26). In addition, wet bone can have flaking of the cortex adjacent to the fracture margin (8,27). These described features and others are used to distinguish perimortem fractures from postmortem fractures.
To understand the difference in fracture patterns between wet and dry bone, it is important to understand the basic mechanical properties of bone. Bone is a composite material composed of both organic materials (collagen and other proteins) and inorganic materials (hydroxyapatite crystals composed of calcium and phosphorus) (28). As a composite material, bone contains both brittle material (minerals) and ductile material (collagen). This composite nature of bone contributes to its fracture mechanics.
In a discussion of the biomechanics of bone fractures, understanding the definition of several terms is necessary: force, load (including stress and strain), elastic deformation, Young's modulus, stiffness, yield point, and plastic deformation. Load is the amount of force applied to a bone. To provide for a more uniform measurement (i.e., across all sizes of bones), load is related to the area. Stress is load (or force) applied per unit of area and strain is the ratio of change in length to original length (29-31). Load can be plotted versus degree of deformation to produce the load-deformation curve, or stress can be plotted versus strain to produce a stress-strain curve (Figure 1). Examination of the stress-strain curve can reveal other mechanical properties of the bone.
Figure 1:

Schematic of a stress-strain curve.
Initially, the stress (y-axis) and strain (x-axis) increase proportionally (Figure 1). As force is applied, the bone deforms in proportion to the amount of force; however, the deformation is not permanent and will reverse if the force is removed (30-32). This segment of the stress-strain curve is termed the elastic phase, the strain produced in the bone is elastic deformation (Figure 1), and the slope of the line is the elastic modulus, or Young's modulus (31). The elastic modulus is a measure of the stiffness of the bone, with a steeper slope indicating a stiffer substance (31).
At some level of stress, the bone reaches the yield point (Figure 1). At this point, the bone enters the plastic phase. In the plastic phase, the increase in stress is no longer proportional to the increase in strain. Instead, for a small increase in stress, there is a large increase in strain (31-33). The strain produced in the bone is termed plastic deformation (Figure 1). The yield point is also referred to as the yield strength (34). Plastic deformation, unlike elastic deformation, will not reverse when the stress is removed. Plastic deformation of the bone will occur until the level of stress reaches the ultimate strength of the bone and fracture occurs (31,34). The amount of strain that can occur in a material after the yield point and before fracture occurs is a measure of the ductility of the material (24).
On the stress-strain curve, a pure brittle substance such as glass has a line that nearly parallels the y-axis, with no change in strain produced with increasing stress, until failure is reached; whereas a pure ductile substance such as rubber has a line that nearly parallels the x-axis for a certain length, with an extensive plastic phase with increase in stress just prior to fracture (31). Brittle material breaks inside or just beyond the zone of elastic deformation, while ductile material can undergo much plastic deformation before fracture occurs (24, 29, 30). However, with a viscoelastic material such as bone, which has both brittle and ductile properties, the rate of application of the stress also affects the stress-strain curve shape, and thus, the mechanical properties of the bone (31). A rapidly loaded bone has increased stiffness and greater ultimate tensile strength and thus, failure of the bone will more represent failure of a brittle substance, whereas a slowly loaded bone has decreased stiffness and lower ultimate tensile strength and thus, failure will more represent failure of a ductile substance (29). This viscoelastic nature of the bone affects the fracture morphology with slow loading more likely to produce linear fractures and rapid loading more likely to produce comminuted fractures (35). For whole bone, the response to stress depends upon the individual bone (e.g., the femur is weaker to tension than the tibia) and whether the bone is wet or dry (30).
As stated, bone is a composite material, and each material (organic and inorganic) contributes differently to the overall biomechanical behavior of bone. Conducting experiments on wet unembalmed bone tissue decalcified to various degrees with hydrochloric acid, Burstein et al. found that as the mineral content of the bone decreased, the elastic modulus decreased, the amount of stress required to enter the zone of plastic deformation decreased, and the ultimate tensile strength (or point of fracture) decreased (28). Therefore, bone obtains most of its elastic stiffness from its mineral content, and the mineral content of bone is the source of its tensile strength (28). The slope of the stress/strain curve after the yield point in nondecalcified bone and incompletely calcified bone was the same as the slope of the stress/strain curve for completely decalcified bone (28). This finding would indicate that the collagen content of the bone is responsible for its behavior in the zone of plasticity.
The area under the stress-strain curve is the amount of energy required to cause fracture of the bone and is referred to as the toughness (24,30). Toughness occurs in three stages: diffuse damage (energy absorbed prior to development of a major crack), initiation of the fracture crack, and progression of the fracture through the bone (36). Saha and Hayes described the total energy required to fracture bone as divided into the elastic deformation stage, the plastic deformation stage, and energy absorbed during fracturing (37).
Most of the studies to assess the biomechanical behavior of bone involve the use of small segments of bone (a few centimeters in size) and not the entire bone, with sizes of the segment sometimes chosen to correspond to specifications for testing of plastics (36-41). The reason for this use of bone segments instead of whole bones is that values (e.g., for elastic modulus) derived from the study of whole bones are only useful for comparison and not for determining material characteristics (29). These small segments of bone allow for testing of a homogenous substance; however, whole bones themselves are not homogenous, being composed of both cortical and cancellous bone, and varying in shape throughout their length.
In general, forensic anthropologists use three terms to describe timing of skeletal injuries in relation to time of death: antemortem, perimortem, and postmortem. Antemortem injuries are those injuries that definitely occurred before death. Postmortem injuries are those injuries that definitely occurred after death. Perimortem injuries are those injuries that occurred around the time of death (25), perhaps a few days or a few hours before death, or a few hours, few days, a few weeks, or even possibly a few months or longer after death. In short, a perimortem fracture is a fracture that cannot definitively be determined to have occurred prior to death (i.e., it is not antemortem) or definitively after death (i.e., it is not postmortem). Correct determination of the perimortem nature of a fracture is important because such a fracture indicates trauma that occurred either at the time of death, and therefore, is potentially indicative of the cause and possibly the manner of death, or occurred after death, but within a relatively short time frame and may be unrelated to the cause and manner of death, but instead may represent postmortem handling of the body.
Sauer proposed five steps to distinguish the three time periods of fracture formation: 1) identification of the fracture, 2) identification of general mechanism of injury responsible for the fracture (e.g., gunshot wound, sharp force injury, or blunt force injury) 3) identification of any osteogenic response, 4) identification of animal activity, and 5) identification of differential staining (26). However, Sauer's approach does not incorporate the features of fractures studied to help distinguish perimortem fractures from postmortem fractures, namely fracture angle, fracture surface (i.e., fracture edge), and fracture outline, which will be described below. Sauer does indicate that more research is needed to help distinguish the three time periods of fracture formation.
Antemortem fractures have some form of osteologic reaction to the injury, which may include a callus (Image 5), fiber-bone periostitis, or an etched line parallel to the fracture line, which is indicative of periosteal uplifting (25). In the first few days after a fracture, inflammatory cells, red blood cells, and edema are found at the site. These features would enable the identification of an antemortem fracture in a fleshed body; however, with loss of tissue, inflammatory cells and red blood cells would also be lost. Thus, these features are not useful in the evaluation of the defleshed skeleton. Over the next week, tissue fills the fracture line and, within the surrounding periosteum, fibrocartilage and collagen are deposited. Once again, with loss of soft tissue, the fibrocartilage and collagen would also be lost, and thus, would not help differentiate the fracture as an antemortem injury in a skeletonized individual. Within the next few weeks, the fibrocartilage becomes calcified, and the fracture site can become visible with radiography (42). This calcified fibrocartilage may persist in a defleshed skeletal element. Therefore, for a fracture to be identified as antemortem in a skeletonized (i.e., defleshed) individual, the time frame between the injury and death would most likely have to be at least two to three weeks.
Image 5:

Callus of rib.
Postmortem fractures occur due to burial circumstances or poor recovery techniques (25–26). In addition to postmortem breakage, which must be distinguished from a perimortem fracture, additional postmortem changes, including postmortem warping, animal activity (Image 6), and bone weathering, must also be distinguished from perimortem trauma (43–44). Postmortem warping due to pressure is curvature of the bone that must be distinguished from plastic deformation (such as produces a bowing fracture), a condition occurring in wet bone (8). Bone weathering is cracking, splitting, exfoliation, and fragmentation of bone exposed to the weather (8,44).
Image 6:

Rodent gnawing. Note the side-by-side parallel linear defects in the bone. Although the rodent gnawing is present throughout the specimen, the white arrow specifically indicates one example.
Distinguishing perimortem from postmortem fractures is critical, as one fracture type definitely occurred after death, while the other fracture type may have occurred at the time of death and therefore, be of importance in understanding the circumstances of the death. However, the distinction is not simple. The study by Cappella et al. indicated that even experienced forensic anthropologists have a fairly high error rate (around 15%) when attempting to distinguish known perimortem and postmortem fractures (18). Ubelaker and Adams reinforce the difficulty in that the authors found three butterfly fractures, fractures they indicate are normally associated with the perimortem period, but, in their case, were obviously postmortem in nature (21). They determined that the butterfly fractures were postmortem and not perimortem based upon 1) differential coloration of the fracture edge and the adjacent cortex and 2) the observation that the direction of forces producing the butterfly fractures on the left tibia and left fibula were in opposite directions, and therefore, could not have occurred in a living individual or even in articulated human remains.
As discussed above, color differences are one feature that can help distinguish perimortem fractures from postmortem fractures (Image 7), with perimortem fractures having the same color of bone at the fracture surface as at the adjacent cortical surface (8, 11, 16, 21, 25, 26, 45). The concept being that if the bone is fractured prior to decomposition and skeletonization, both the fracture surface and the adjacent un-fractured cortical surface are exposed to the same conditions and thereby have the same coloration; however, if the fracture occurs postmortem and after the cortex of the bone is discolored, the now exposed fracture surface will not have the same coloration as the adjacent cortex. However, color differences are not an absolute indicator of postmortem fractures as differential staining of the cortical surface and fracture margin can be due to various environmental and postmortem factors such as decompositional fluids, soil, foliage (such as leaves), and dirty water, but could also be due to more perimortem phenomena such as hemorrhage; therefore, this feature as a marker for postmortem versus perimortem fracture should be used cautiously (8,46). Also, postmortem handling of the bones could affect the distribution of color changes. For example, if a body is buried in the ground for a long enough period for skeletonization to occur, the outer surface of the bones may be brown discolored from contact with the soil. If these bones are removed from the ground and fractures occur during the process, the color differential between the outer cortical surface (i.e., brown) and the fracture surface (i.e., white, or yellow-white) will assist in the determination that the fractures are postmortem. However, if the bones are then reburied and exhumed at a later time, the fracture surface would then potentially appear brown and the postmortem fractures could be misinterpreted as perimortem fractures. Scene investigation and historical information would be especially important to assist in the correct evaluation of the nature of the fractures in this second situation.
Image 7:

Postmortem cranial defect. This defect in the bone was identified in a cranium that was inadvertently found while an individual was digging in the ground. Note that the bone, for the most part, is brown-discolored from the soil; however, the rim of the defect is more white-tan discolored. The appearance of this fracture is consistent with the history, with trauma caused to the bone during the digging.
In addition to a color differential between the fracture surface and adjacent cortical surface, the appearance of the fracture angle, the fracture surface, and the fracture outline may help distinguish perimortem and postmortem fractures (16). The fracture angle (the angle formed by the surface of the fracture and the surface of the cortical bone) is obtuse or acute in wet bones, whereas those in dry bones are at or nearly at right angles (8, 14, 47). Thus, a perimortem fracture should have an obtuse or acute angle, while a postmortem fracture should have a right angle (Image 8, Figure 2). The fracture surface (i.e., fracture edge) is the surface of the fractured end of the bone and is usually smooth, sharp, and sometimes beveled in wet bone, and irregular (Image 9) or jagged in dry bone (8, 14, 15, 45). However, this texture of the fracture surface may also depend upon the source of the load, with low-energy force producing a rough fracture surface as a result of spread around vascular spaces and high-energy force producing a smooth fracture surface as a result of propagation through vascular spaces (48). Therefore, a low-energy force could produce a fracture surface that mimics a postmortem fracture, while a high-energy force could produce a fracture surface that is consistent with a perimortem fracture. The fracture outline is the general shape of the fractured end of the bone. Designation of fracture outline includes 1) transverse, 2) curved, and 3) intermediate (47) (Images 10 and 11). Intermediate fracture outlines are those fracture outlines that are straight but oblique or those with a stepped outline. Postmortem fractures tend to be transverse while perimortem fractures tend to be curved (47).
Image 8:

Fracture of dry bone, example of fracture angle. The white arrow indicates a fracture angle that is right angled. See also Figure 2 Also note the color difference between the fracture surface (which is lighter in color) and the surrounding cortical surface.
Figure 2:
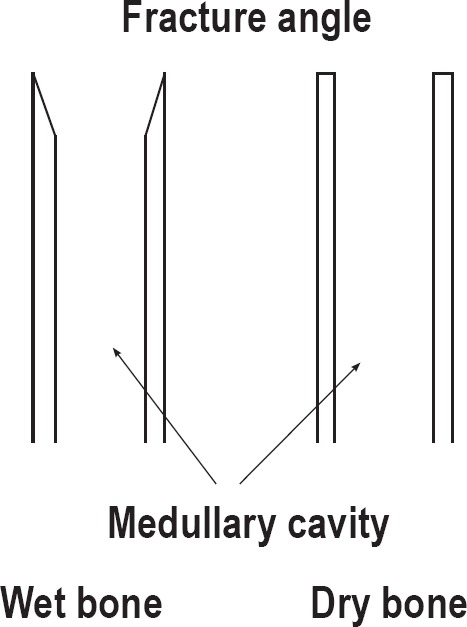
Schematic of fracture angles. Figure 2 illustrates two segments of bone, wet bone on the left side and dry bone on the right side. Each segment has a fracture at the top. The figure illustrates the difference between an acute angle, which are associated with wet bone and the right angle, which are associated with dry bone.
Image 9:

Fracture of dry bone, example of fracture surface. The white arrow indicates the fracture surface. Note that it is irregular and not smooth.
Image 10:

Fracture of wet bone, example of fracture outline. Note the curved appearance of the fracture outline (contrast this image with Image 11).
Image 11:

Fracture of dry bone, example of fracture outline. Note the transverse appearance of the fracture outline. At the white arrow is postmortem animal activity, with puncture of the cortex of the bone.
In support of these fracture features being used to help separate perimortem from postmortem fractures, Wieberg and Wescott, based upon their study of 60 porcine long bones each fractured after a variable postmortem interval, determined that, in general with increasing postmortem interval, fracture morphology changes from acute angles, smooth surfaces, and curved outlines to transverse angles, rough surfaces, and fewer curved outlines; however, some groups of bones with the same postmortem interval had both perimortem and postmortem features (13). In support of this finding, Wheatley (12) found characteristics of wet bone (i.e., acute fracture angle, smooth fracture surface, and curved outlines) in bones that were one year postmortem.
Although studies may show that perimortem and postmortem fractures may present osteologic features that are different from each other, Cappella et al. indicated that perimortem fractures can acquire postmortem features (7). The authors examined seven individuals who had been autopsied, and then exhumed 15 years later, stored in an ossuary for five years, and then examined. They indicated that additional postmortem fractures can mask perimortem fractures, that warping and abrasion of the bone can modify fractured edges, and that taphonomic variables (e.g., environmental conditions) can alter the color or outline of the fracture.
Conclusion
With increasing postmortem interval, the ability of a forensic pathologist to identify and interpret injuries becomes more difficult. In the case of decomposition, and especially skeletonization, forensic pathologists will often consult with forensic anthropologists to assist in the identification of and interpretation of skeletal trauma, because determining when a skeletal injury occurred in relation to the time of death can be of importance to a death investigation.
When only the skeletal elements are available for examination, forensic anthropologists can use certain features of the fracture to assist in determining whether or not an injury was sustained prior to death or is postmortem, with those injuries sustained prior to death exhibiting some form of osteologic reaction to the injury (e.g., callus formation). However, for a variable length of time after death, depending upon the environment in which the body decomposes, the biomechanical behavior of bone in response to load is the same as if the bone were still in a living individual. It is considered wet bone. Once sufficient time has elapsed and the correct conditions exist and the bone has lost its organic matrix, its biomechanical behavior in response to load is no longer the same as if it were in a living individual and it is now considered dry bone. Thus, in the true postmortem period (i.e., the time following the death of the individual), fractures of a bone, depending upon the state of the bone, either wet or dry, can appear differently. A fracture bearing the features of one occurring in wet bone could have happened at the time of death, or up to several weeks or months after death. Obviously, each of these time frames has a different connotation for a death investigation. The term, “perimortem” has been used in the past and currently by some authors to describe a fracture that was not definitely antemortem or definitely postmortem; however, the use of this term, and the range of time around the actual death of the individual that it encompasses, varies between specialties and thereby, the use of the term, “perimortem” has led to potential confusion.
The features of a fracture commonly associated with wet bone include an acute angle, a smooth fracture surface and a curved outline, which differ from the features of a fracture commonly associated with dry bone, which include a right angle, a rough fracture surface, and a transverse outline; however, the distinction is not absolute. Also, the transition from wet bone to dry bone is gradual, and thus, it could be expected that during that transition, a bone may respond to trauma as neither a bone within a living individual nor as a bone that has been without soft tissue for five years and buried in dry soil. Other features such as attached fragments of bone and chipping of the surrounding cortex in wet bone and differential coloration between the fracture surface and adjacent cortical surface in dry bone can also assist in the determination of the time frame of the fracture. Although the term is used in the literature, avoidance of the confusion associated with the use of the word “perimortem” is preferable, and Symes et al. advocate a descriptive approach to skeletal trauma, and an interpretation based upon wet versus dry bone, instead of perimortem versus postmortem (16).
Footnotes
Financial Disclosure
The author has indicated that he does not have financial relationships to disclose that are relevant to this manuscript
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The author, reviewers, editors, and publication staff do not report any relevant conflicts of interest
References
- 1.Lew E., Matshes E. Forensic pathology: principles and practice. 1st ed. Amsterdam: Elsevier Press; c2005. Chapter 24, Postmortem changes; p. 527–54. [Google Scholar]
- 2.Dolinak D., Matshes E. Forensic pathology: principles and practice. 1st ed. Amsterdam: Elsevier Press; c2005. Chapter 17, Child abuse; p. 369–412. [Google Scholar]
- 3.Dolinak D. Forensic pathology: principles and practice. 1st ed. Amsterdam: Elsevier Press; c2005. Matshes E. Chapter 8, Asphyxia; p. 201–25. [Google Scholar]
- 4.Cattaneo C., Andreola S., Marinelli E. et al. The detection of microscopic markers of hemorrhaging and wound age on dry bone: a pilot study. Am J Forensic Med Pathol. 2010. Mar; 31(1): 22–6. PMID: 19935396. 10.1097/paf.0b013e3181c15d74. [DOI] [PubMed] [Google Scholar]
- 5.Symes S.A., L'Abbé E.N., Chapman E.N. et al. A companion to forensic anthropology. West Sussex (UK): Wiley-Blackwell; c2012. Chapter 17, Interpreting traumatic injury to bone in medicolegal investigations; p. 340–89. [Google Scholar]
- 6.Bunch A.W. National Academy of Sciences “standardization”: on what terms? J Forensic Sci. 2014. Jul; 59(4): 1041–5. PMID: 24854677. 10.1111/1556-4029.12496. [DOI] [PubMed] [Google Scholar]
- 7.Cappella A., Castoldi E., Sforza C., Catteneo C. An osteological revisitation of autopsies: comparing anthropological findings on exhumed skeletons to their respective autopsy reports in seven cases. Forensic Sci Int. 2014. Nov; 244: 315.e1–10. PMID: 25315679. 10.1016/j.forsciint.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Moraitis K., Spiliopoulou C. Identification and differential diagnosis of perimortem blunt force trauma in tubular long bones. Forensic Sci Med Pathol. 2006. Dec; 2(4): 221–9. PMID: 25868767. 10.1385/fsmp:2:4:221. [DOI] [PubMed] [Google Scholar]
- 9.Coelho L., Cardoso F.V. Timing of blunt force injuries in long bones: the effects of the environment, PMI length and human surrogate model. Forensic Sci Int. 2013. Dec 10; 233(1-3): 230–7. PMID: 24314524. 10.1016/j.forsciint.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Matshes E., Lew E. Forensic pathology: principles and practice. 1st ed. Amsterdam: Elsevier Press; c2005. Chapter 26, Forensic osteology; p. 563–604. [Google Scholar]
- 11.Galloway A., Symes S., Haglund W.D., France D.L. Broken bones: anthropological analysis of blunt force trauma. 1st ed. Springfield (IL): Charles C. Thomas; 1999. Chapter 1, The role of forensic anthropology in trauma analysis; p. 5–31. [Google Scholar]
- 12.Wheatley B.P. Perimortem or postmortem bone fractures? An experimental study of fracture patterns in deer femora. J Forensic Sci. 2008. Jan; 53(1): 69–72. PMID: 18005007. 10.1111/j.1556-4029.2008.00593.x. [DOI] [PubMed] [Google Scholar]
- 13.Wieberg D.A., Wescott D.J. Estimating the timing of long bone fractures: correlation between the postmortem interval, bone moisture content, and blunt force trauma fracture characteristics. J Forensic Sci. 2008. Sep; 53(5): 1028–34. PMID: 18624891. 10.1111/j.1556-4029.2008.00801.x. [DOI] [PubMed] [Google Scholar]
- 14.Wright C.S. Perimortem and postmortem fracture patterns in deer femora [master's thesis]. Tuscaloosa (AB): University of Alabama; 2009. [cited 2016 Jan 1]. 64 p. Available from: http://acumen.lib.ua.edu/content/u0015/0000001/0000030/u0015_0000001_0000030.pdf. [Google Scholar]
- 15.Shattuck R.E. Perimortem fracture patterns in south-central Texas: a preliminary investigation into the perimortem interval [master's thesis]. San Marcos (TX): Texas State University-San Marcos; 2010. [cited 2016 Jan 1]. 59 p. Available from: https://digital.library.txstate.edu/bitstream/handle/10877/4066/fulltext.pdf. [Google Scholar]
- 16.Symes S.A., L'Abbé E.N., Stull K.E. et al. Manual of forensic taphonomy. Boca Raton: CRC Press; c2014. Chapter 13, Taphonomy and the timing of bone fractures in trauma analysis; p. 341–66. [Google Scholar]
- 17.Kroman A.M., Symes S.A. Research methods in human skeletal biology. Waltham (MA): Academic Press; c2013. Chapter 8, Investigation of skeletal trauma; p. 219–39. [Google Scholar]
- 18.Cappella A., Amadasi A., Castoldi E. et al. The difficult task of assessing perimortem and postmortem fractures on the skeleton: a blind text on 210 fractures of known origin. J Forensic Sci. 2014. Nov; 59(6): 1598–601. PMID: 24990801. 10.1111/1556-4029.12539. [DOI] [PubMed] [Google Scholar]
- 19.Ludwig J. Handbook of autopsy practice. 3rd ed. Totowa (NJ): Humana Press; 2002. 592 p. [Google Scholar]
- 20.Scheuer L., Black S. Developmental juvenile osteology. San Diego: Elsevier Academic Press; 2000. 587 p. [Google Scholar]
- 21.Ubelaker D.H., and Adams B.J. Differentiation of perimortem and postmortem trauma using taphonomic indicators. J Forensic Sci. 1995. May; 40(3): 509–12. PMID: 7782760. [PubMed] [Google Scholar]
- 22.Stedman T.L. Stedman's medical dictionary. 25th ed. Baltimore: Williams and Wilkins; 1990. 1784 p. [Google Scholar]
- 23.Ayers D.M. Bioscientific terminology: words from Latin and Greek stems. Tucson: University of Arizona Press; 1972. 325 p. [Google Scholar]
- 24.Turner C.H., Burr D.B. Basic biomechanical measurements of bone: a tutorial. Bone. 1993. Jul-Aug; 14(4): 595–608. PMID: 8274302. 10.1016/8756-3282(93)90081-k. [DOI] [PubMed] [Google Scholar]
- 25.Rodríguez-Martín C. Forensic anthropology and medicine: complementary sciences from recovery to cause of death. Totowa (NJ): Human Press; c2006. Chapter 8, Identification and differential diagnosis of traumatic lesions of the skeleton; p. 197–224. [Google Scholar]
- 26.Sauer N.J. Forensic osteology: advances in the identification of human remains. 2nd ed. Springfield (IL): Charles C Thomas; c1998. Chapter 15, The timing of injuries and manner of death: distinguishing among antemortem, perimortem, and postmortem trauma; p. 321–32. [Google Scholar]
- 27.Jordana F., Colat-Parros J., Bénézech M. Diagnosis of skull fractures according to postmortem interval: an experimental approach in a porcine model. J Forensic Sci. 2013. Jan; 58 Suppl 1: S156–62. PMID: 23106527. 10.1111/1556-4029.12012. [DOI] [PubMed] [Google Scholar]
- 28.Burstein A.H., Zika J.M., Heiple K.G., Klein L. Contribution of collagen and mineral to the elastic-plastic properties of bone. J Bone Joint Surg Am. 1975. Oct; 57(7): 956–61. PMID: 1184645. [PubMed] [Google Scholar]
- 29.Reilly D.T., Burstein A.H. Review article: the mechanical properties of cortical bone. J Bone Joint Surg Am. 1974. Jul; 56(5): 1001–22. PMID: 4603167. [PubMed] [Google Scholar]
- 30.Rogers L.F. Radiology of skeletal trauma. New York: Churchill-Livingstone; 1982. 939 p. [Google Scholar]
- 31.Porta D.J. Forensic medicine of the lower extremity. Totowa (NJ): Humana Press; c2005. Chapter 9, Biomechanics of impact injury; p 279–310. [Google Scholar]
- 32.Crowe J.E., Swischuk L.E. Acute bowing fractures of the forearm in children: a frequently missed injury. AJR Am J Roentgenol. 1977. Jun; 128(6): 981–4. PMID: 414566. 10.2214/ajr.128.6.981. [DOI] [PubMed] [Google Scholar]
- 33.Pierce M.C., Bertocci G.E., Vogeley E., Moreland M.S. Evaluating long bone fractures in children: a biomechanical approach with illustrative cases. Child Abuse Negl. 2004. May; 28(5): 505–24. PMID: 15206413. 10.1016/j.chiabu.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 34.Daegling D.J., Warren M.W., Hotzman J.L., Self C.J. Structural analysis of human rib fractures and implications for forensic interpretation. J Forensic Sci. 2008. Nov; 53(6): 1301–7. PMID: 18798775. 10.1111/j.1556-4029.2008.00876.x. [DOI] [PubMed] [Google Scholar]
- 35.Smith O.C., Peters C.E. Biomechanics and the bone. In: Symes SA, editor. Bones: bullets, burns, bludgeons, blunders and why. Proceedings of the 48th Annual Meeting of the American Academy of Forensic Sciences; 1996 Feb 19-24; Nashville, TN. Nashville: University of Tennessee; 1996. p. 6–14. [Google Scholar]
- 36.Zioupos P., Currey J.D. Changes in the stiffness, strength, and toughness of human cortical bone with age. Bone. 1998. Jan; 22(1): 57–66. PMID: 9437514. 10.1016/s8756-3282(97)00228-7. [DOI] [PubMed] [Google Scholar]
- 37.Saha S., Hayes W.C. Tensile impact properties of human compact bone. J Biomech. 1976; 9(4): 243–51. PMID: 1262359. 10.1016/0021-9290(76)90010-5. [DOI] [PubMed] [Google Scholar]
- 38.Bayraktar H.H., Morgan E.F., Niebur G.L. et al. Comparison of the elastic and yield properties of human femoral trabecular and cortical bone tissue. J Biomech. 2004. Jan; 37(1): 27–35. PMID: 14672565. 10.1016/s0021-9290(03)00257-4. [DOI] [PubMed] [Google Scholar]
- 39.Norman T.L., Vashishth D., Burr D.B. Fracture toughness of human bone under tension. J Biomech. 1995. Mar; 28(3): 309–20. PMID: 7730389. 10.1016/0021-9290(94)00069-g. [DOI] [PubMed] [Google Scholar]
- 40.Laird G.W., Kingsbury H.B. Complex viscoelastic moduli of bovine bone. J Biomech. 1973. Jan; 6(1): 59–67. PMID: 4735081. 10.1016/0021-9290(73)90038-9. [DOI] [PubMed] [Google Scholar]
- 41.Reilly D.T., Burstein A.H., Frankel V.H. The elastic modulus for bone. J Biomech. 1974. May; 7(3): 271–5. PMID: 4846264. 10.1016/0021-9290(74)90018-9. [DOI] [PubMed] [Google Scholar]
- 42.Calmar E.A., Vinci R.J. The anatomy and physiology of bone fracture and healing. Clin Ped Emerg Med. 2002; 3(2): 85–93. 10.1053/epem.2002.127037. [DOI] [Google Scholar]
- 43.Quatrehomme G., Ïşcan M.Y. Postmortem skeletal lesions. Forensic Sci Int. 1997. Oct 6; 89(3): 155–65. PMID: 9363624. 10.1016/s0379-0738(97)00113-8. [DOI] [PubMed] [Google Scholar]
- 44.Marden K., Sorg M.H., Haglund W.D. Research methods in human skeletal biology. Waltham (MA): Academic Press; c2013. Chapter 9, Taphonomy; p. 241–62. [Google Scholar]
- 45.Moraitis K, Eliopoulos C, Spiliopoulou C. Fracture characteristics of perimortem trauma in skeletal material. Internet J Biol Anthropol. 2008; 3(2): [8 p.]. 10.5580/20a2. [DOI] [Google Scholar]
- 46.Dupras T.L., Schultz J.J. Manual of forensic taphonomy. Boca Raton: CRC Press; c2013. Chapter 12, Taphonomic bone staining and color changes in forensic contexts; p. 315–40. [Google Scholar]
- 47.Villa P., Mahieu E. Breakage patterns of human long bones. J Hum Evol. 1991. Jul; 21(1): 27–48. 10.1016/0047-2484(91)90034-s. [DOI] [Google Scholar]
- 48.Herrmann N.P., Bennett J.L. The differentiation of traumatic and heat-related fractures in burned bone. J Forensic Sci. 1999. May; 44(3): 461–9. PMID: 10408102. [PubMed] [Google Scholar]


