Abstract
Infarction of the posterior cerebral artery circulation arising from entrapment of the basilar artery in a fracture of the clivus has been reported in the medical literature, predominantly in the radiology and emergency medicine journals. Review of the medical literature on the topic revealed 14 published cases of entrapment of the basilar and/or vertebral artery within a longitudinal fracture of the clivus. These were all reported between 1964 and 2016 and postmortem examination had been conducted on seven cases.
To date, no case of entrapment of the basilar and/or vertebral artery in a fracture of the clivus has been reported in the forensic pathology literature, and the published literature on the entity is reviewed
Keywords: Forensic pathology, Clival fracture, Basilar artery entrapment, Vertebral artery entrapment, Vertebrobasilar artery entrapment, Posterior cerebral circulation infarction, Head injury, Head trauma
Introduction
Death from vertebrobasilar artery trauma is most commonly encountered in the setting of traumatic basal subarachnoid hemorrhage that develops in intoxicated individuals who receive a blow to either the jaw or upper neck that causes rotation of the head with hyperextension of the neck, such that tearing of the ipsilateral vertebral artery and resultant basal subarachnoid hemorrhage occurs as reported by Dymock from as far back as 1977 (1). Cases of infarction of the posterior cerebral artery circulation, which arise from entrapment of the basilar artery in a fracture of the clivus, have been reported in the medical literature, predominantly in the radiology and emergency medicine journals (2-15).
Review of the medical literature on the topic revealed 14 published cases of entrapment of the basilar and/or vertebral artery within a longitudinal fracture of the clivus, which were all reported between 1964 and 2016; however, until now, no such case has been reported in the forensic pathology literature. Following the case report, the previously published literature regarding this entity is reviewed.
Case Report
A 74-year-old woman with a history of alcohol abuse was witnessed to fall down three stairs within a residence and sustain an impact to the crown of her head on the floor. She was unconscious at the scene, Glasgow Coma Scale (GCS) score of 3, with some improvement (GCS 7) after she was conveyed to the emergency room.
Computed tomography (CT) scans of the brain with angiography (CTA) identified 1) an acute longitudinal fracture of the body of the clivus, 2) anterior displacement of the basilar artery, 3) nonvisualization and entrapment of the mid basilar artery in the fracture defect of the clivus (Images 1A-C), 4) an acute infarction of the left posterior inferior cerebellar artery (PICA) territory, and 5) irregular caliber, with moderate to severe segmental vascular narrowing, of the extracranial V3 segment of the left vertebral artery with complete thrombosis of the left V4 (intracranial) vertebral artery segment and left PICA. The right V4 segment showed irregular caliber with moderate to severe intraluminal stenosis, suspicious for acute traumatic subintimal dissection. Generalized osteopenia of the cervical spine with focal hemangiomas of the C3, C5, C6, and C7 vertebrae were background findings.
Image 1A.
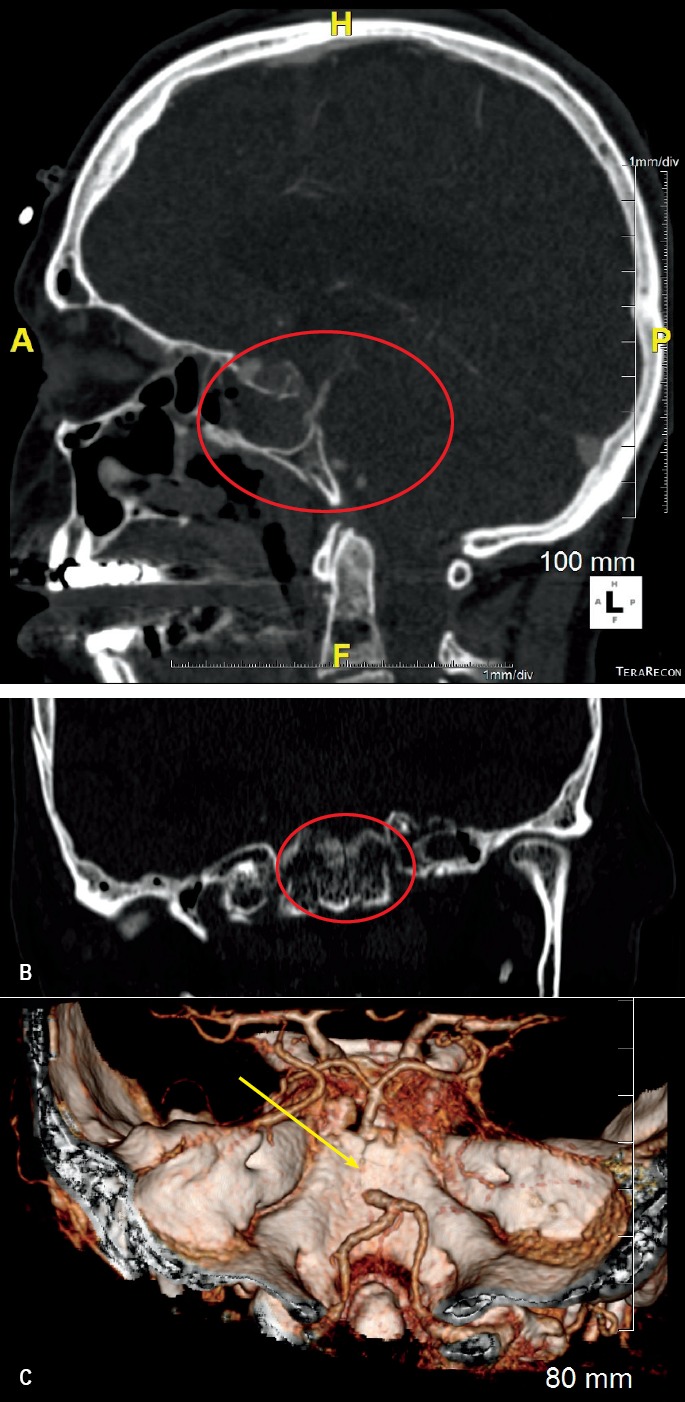
Computed tomography angiogram of the head showing entrapment of the basilar artery in an acute longitudinal fracture of the clivus (sagittal view). B) Computed tomography scan of the head showing longitudinal fracture of the clivus in coronal view (bone window). C) Three-dimensional computed tomography reconstruction of the head illustrating entrapment of the basilar artery in a longitudinal fracture of the clivus.
The admission blood ethanol concentration was 43 mmol/L (198 mg/100 mL). She was transferred to the intensive care unit and developed the “locked-in syndrome” and was thus placed on palliative care until death occurred. A postmortem examination was requested to determine if vertebral artery dissection had precipitated the fall.
Postmortem examination revealed a 16 cm x 13 cm subgaleal bruise of the right side of the frontal scalp (Image 2).
Image 2.

Contusion of the scalp.
There was a hemorrhagic, vertical fracture with associated dural laceration along the clivus with associated entrapment of a short segment of the mid region of the basilar artery, which correlated with the radiological findings (Image 3).
Image 3.
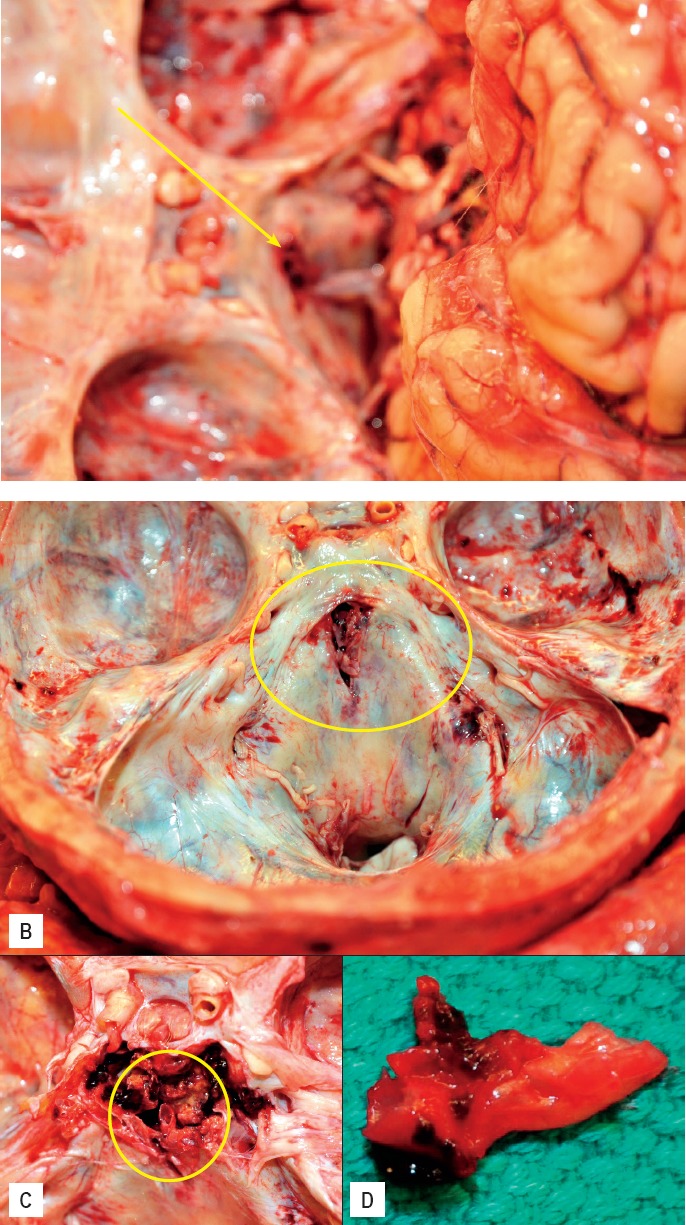
A: Entrapped basilar artery within the longitudinal fracture. B) Longitudinal fracture of the clivus with entrapped fragment of the basilar artery after removal of the brain. C) Entrapped segment of basilar artery. D) Removed entrapped segment of basilar artery.
The anterior aspect of the body of the C5 vertebra exhibited a transverse fracture that did not involve the spinal canal or cervical spinal cord (Image 4).
Image 4.

Hemorrhagic fracture of the C5 vertebral body.
The cervical spine was excised with a portion of the base of the skull around the foramen magnum utilizing the method described by Vanezis (16) and was subjected to formalin fixation, decalcification, and transverse sectioning prior to assessment for pathology in the extracranial vertebral arteries (Image 5). There was extensive retroclival hemorrhage associated with the longitudinal fracture of the clivus (Image 5C).
Image 5.
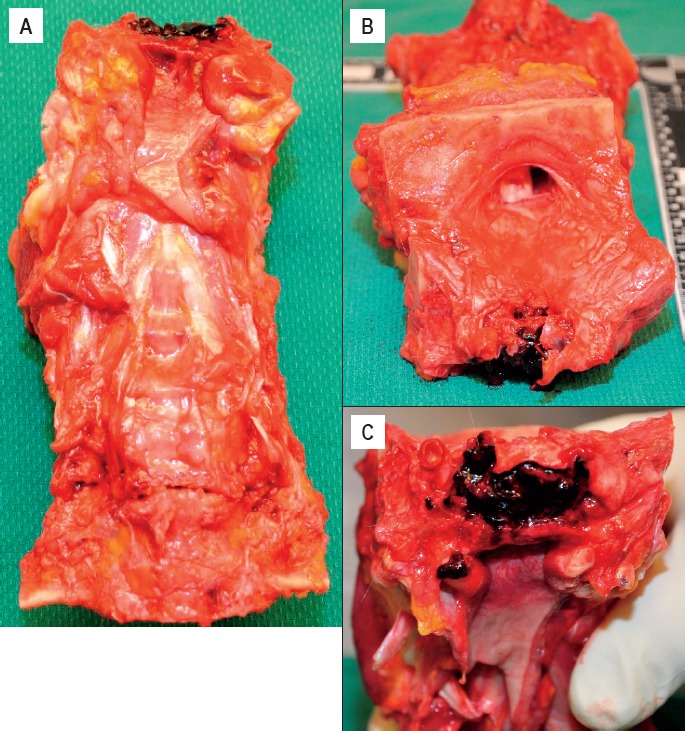
A) Anterior view of excised cervical spine. B) View of superior aspect of the excised cervical spine from the base of skull with the foramen magnum. C) Extensive retroclival hemorrhage.
Examination of serial sections of the decalcified, excised cervical spine did not reveal any evidence of dissection of the extracranial vertebral arteries (Image 6). The incidental hemangiomas described on imaging were identified.
Image 6.

Transverse sections of the decalcified cervical spine. No dissection of the extracranial vertebral arteries was identified (small circles). Three incidental hemangiomas were identified (short arrows).
Neuropathological examination of the formalin-fixed brain revealed that the cerebellum exhibited softening of the parenchyma of the left PICA territory. The brainstem exhibited a triangular-shaped infarct of the paramedian vascular territories of the upper and mid pons (Image 7A). Microscopically, the infarct was evident in the section from the junction of the pons and midbrain down to the level of the twelfth cranial nerve nuclei and the superior olivary nuclei with preservation of the dorsal midline structures at that level. (Images 7B-G). There was focal extension into the tegmentum of the pons. A careful analysis of the intracranial arteries did not reveal any significant finding. Although the PICA territory in the cerebellum was infarcted, it was normal in the medulla.
Image 7.
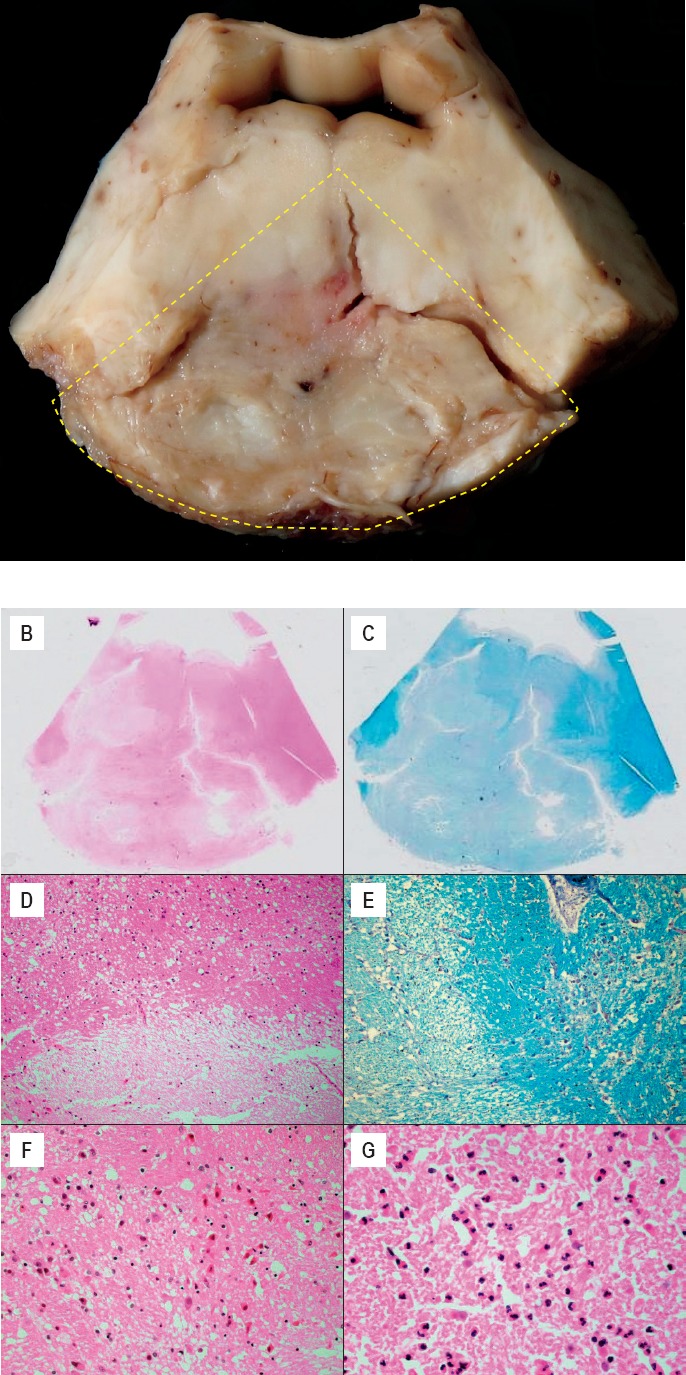
A: Gross image of the triangular shaped infarct of the pons, at the level of the middle cerebellar peduncles. B and C) Whole mount section of the pontine infarct in the paramedian territories with focal extension into the tegmentum (H&E and Luxol Fast Blue, x1.25). D-G) Histology of the pontine infarct with sharp limit and surrounding edematous spongiosis (H&E, Luxol Fast Blue - D and E, x100; F and G, x400), anoxic neurons on the right side (F) and early neutrophilic reaction (G).
Death was ascribed to infarction of the posterior cerebral circulation secondary to entrapment of the basilar artery within a longitudinal fracture of the clivus as a consequence of blunt force head injury.
Discussion
Cases of infarction of the posterior cerebral artery circulation which arise a result of entrapment of the basilar artery in a fracture of the clivus have been reported in the medical literature in radiology, neurosurgery, and emergency medicine journals from as far back as 1964 to the present (2-15).
Fractures of the clivus are uncommon and were previously reported in the historical literature with a rare incidence in the range of 0.21% to 0.56% (8, 17-19) until more recently when one team of investigators reported an incidence of 1.2% (20). Of all skull base fractures, 20% occur in the middle central region of the skull base that includes the clivus (Figure 1) (21). Clivus is the Latin word for “slope.” The clivus is a bone in the posterior central aspect of the base of the skull and is composed of the occipital and sphenoid bones. It is located at the anterior-most portion of the basilar occipital bone at its junction with the sphenoid bone and sits just posterior to the sphenoid sinuses in the axial plane (Figure 1). It is the backward sloping bony process and shallow depression behind the dorsum sellae on the base of the skull near the brainstem, cranial nerves, and vertebrobasilar system (22). The basilar artery and pons lie posterior to it. Its cranial surface is covered by dura mater, which is perforated by the abducens nerve in the central part.
Figure 1.
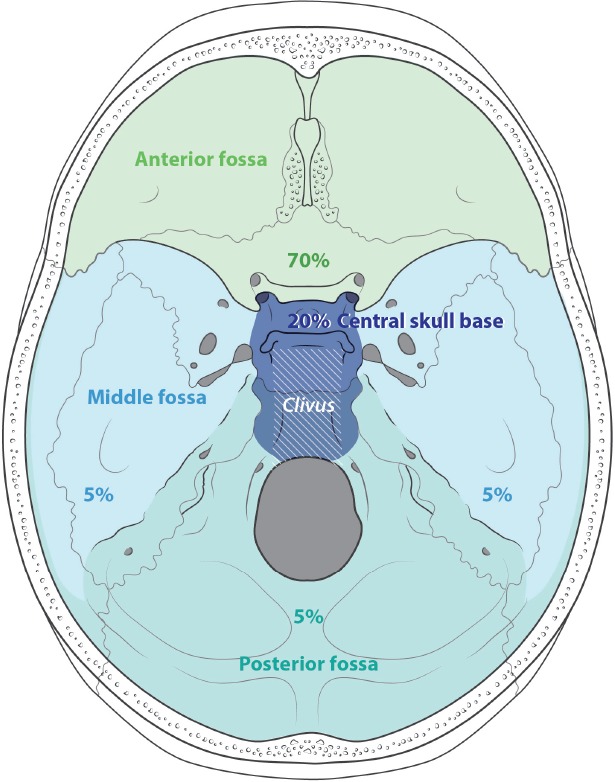
Relative percentages of skull base fractures and ocation of the clivus. Created under contract by professional medical illustrator Diana Kryski.
Fractures of the clivus can be classified as longitudinal, transverse, or oblique, based on their orientation (8). High impact injury of the cranium is involved in all fracture types. Lateral impacts and transverse compressive forces of the skull are well-known mechanisms for the development of transverse fractures of the clivus (23, 24), but a variety of impacts that include forces transmitted along the vertebral column in the axial direction have been described as the mechanism of development for longitudinal fractures (6). Review of the literature indicates that an impact directed to the middle of the sagittal plane of the skull is, therefore, the most likely cause of longitudinal fractures (10).
Clival fractures are associated with a high mortality rate of 67-80% due to the high incidence of associated vascular injury (6, 8, 13). The high mortality rate is due to the development of infarction of the posterior circulation (brainstem and cerebellum) secondary to vertebrobasilar artery injury, either from arterial occlusion or dissection. Computed tomography and CTA are useful in the clinical diagnosis (11, 25). The sequelae of clival fractures include partial or complete occlusion of vertebrobasilar arteries (via physical pinching, thrombosis, or dissection), direct trauma to the brain stem, and death.
Longitudinal clival fractures associated with entrapment of the vertebrobasilar arteries are unusual entities with a low prevalence (8, 17-20). Partial or complete occlusion of the vertebrobasilar arteries can occur via physical pinching, thrombosis, or dissection, but associated deaths have been the result of direct brainstem trauma or systemic complications. The spectrum of arterial involvement can be basilar artery (2, 4, 7), proximal basilar and distal vertebral arteries (6, 9), the vertebrobasilar arterial junction (13), or a unilateral vertebral artery (3, 15).
The mechanism of basilar artery incarceration was first proposed by Sights in 1968 and involved two components with contributions from three contributing postulates of fontal, occipital, and axial impact (4). It was initially proposed that a force delivered in the anteroposterior direction via either frontal or occipital impact is necessary for its etiology (4). The first component involves an axial load injury that leads to a linear longitudinal fracture in the coronal plane of the clivus. The second component involves the momentum and subsequent inertia of the basilar artery in the forward direction, leading to entrapment of the artery at the fracture site such that its lumen is compromised with predictable pathological consequences (4). There has only been one case reported in the literature with persistent patency of a herniated basilar artery through a clival fracture (26).
In frontal impact, there is momentary deformation of the skull with increased coronal dimensions that results in a longitudinal fracture with dural laceration (12). Due to inertia, the forward-moving basilar artery becomes instantaneously trapped or the inertial forward movement of the brainstem and cerebellum presses the basilar artery into the fracture cleft, which then closes on the artery (11, 12). Occipital impact may cause a similar chain of events as frontal impact. With axial impact (either vertex or feet), there is transmission of an axial force that compresses the clivus between the petrous bones and the vertebral body to create the injury. The clivus is vulnerable to transmitted force from any aspect of the head due to its proximity to the axis of symmetry.
In essence, a blunt impact of the skull is necessary to invoke deformation of the skull with a resultant “bursting” longitudinal linear fracture along the clivus with associated laceration of the dura mater. Inertia of the brain stem and cerebellum thrusts the basilar artery into the breach as they continue to move forward relative to the skull. The fracture cleft then closes on the artery with its resultant occlusion and that of its tributaries (10). Variation in the site of arterial entrapment may result from anatomic variations, direction of impact, and location of the clival fracture (10).
Longitudinal clival fractures are more rare than transverse and oblique clival fractures with a higher likelihood of vascular injury and a rather high mortality rate (67-80%) from the associated vascular injury (6, 8, 19). A very recent 2015 publication out of a Canadian Level 1 Trauma Center, which reported the highest incidence of clival fractures (1.2%) as part of basal skull fractures to date, also reported that 60% were oblique, 26.1% were longitudinal, and 13.8% were transverse (20). Their findings suggest that the most commonly occurring clival fractures, in order of decreasing frequency, were oblique, longitudinal, and transverse, and was similar to that previously reported in the largest series of 41 patients as published in 2009 by Ochalski et al. (17). Smaller case series have described an equal incidence of longitudinal, oblique, and transverse clival fractures (8, 27).
Transverse clival fractures carry a lower mortality rate than longitudinal fractures and are more associated with multiple cranial nerve defects and vascular injuries of the anterior cerebral circulation (8, 24, 28).
Lateral impacts and transverse compressive forces of the skull are well-known mechanisms for the development of transverse fractures of the clivus (23, 24), but a variety of impacts that include forces transmitted along the vertebral column in the axial direction have been described as the mechanism of development for longitudinal fractures (6).
Oblique clival fractures extend from the lateral aspect of dorsum sellae on one side to the contralateral petroclival fissure (29).
Overall, the potential complications of clival fractures are 1) death (from either vascular complications or direct brain stem injury) and 2) cranial nerve deficits in those who survive. Meguro and Rowed reported a case of traumatic (dissecting) aneurysm of the PICA produced by fracture of the clivus (30).
Mechanical trauma is a risk factor for the development of acute dissection of the intracranial and extracranial arteries (31). The extracranial arteries are more commonly affected than the intracranial arteries (32).
The fixed intraforaminal (V2) and the mobile (V3) vertebral artery segments are particularly susceptible to traumatic dissection (27, 28). In the present case, the autopsy showed the intraluminal stenosis found in the radiological tests was not reflective of traumatic arterial dissection. Both the blunt trauma itself and the presence of extensive retroclival hemorrhage may explain the luminal irregularities found in CT angiography and magnetic resonance angiography, which most probably represented vasospasm in our case.
Review of the medical literature on the topic revealed 14 reported cases of entrapped basilar artery (+/- vertebral) within a longitudinal fracture of the clivus. These were all reported between 1964 and 2016. The summary of the clinicopathological findings in each case can be found in Table 1. Postmortem examination was conducted on seven cases.
Table 1.
Reported Cases of Entrapped Vertebrobasilar Artery in a Longitudinal Fracture of the Clivus
| Reference | Age (years) | Sex | Cause of Injury | GCS Score | Entrapped Artery | Outcome | Diagnostic Method | Autopsy |
|---|---|---|---|---|---|---|---|---|
| Loop et al. 1964 (2) | 59 | M | Hit by a falling beam | 3 | Basilar | Death day 14 | Yes | |
| Lindenberg 1966 (3) | 42 | M | Fall | 15 | Vertebral | Death day 14 | Yes | |
| Sight et al. 1968 (4) | 23 | M | MVC | 3 | Basilar | Death day 35 | Yes | |
| Shaw et al. 1972 (5) | 59 | M | Hit by tree | 3 | Basilar | Death day 13 | Yes | |
| Anthony et al. 1987 (6) | 70 | M | Fall | 3 | Basilar | Death day 5 | Yes | |
| Guha et al. 1989 (7) | 27 | M | Fall | 3 | Basilar | Vegetative | VA | |
| Corradino et al. 1990 (8) | NA | NA | NA | NA | Vertebral | Death | VA | |
| Sato et al. 1990 (9) | 80 | M | MVC | 3 | Vertebral and basilar | Death day 1 | Yes | |
| Taguchi et al. 2000 (10) | 52 | M | Fall | 3 | Basilar | Quadriparesis | CTA | |
| Sato et al. 2001 (11) | 56 | M | Fall | 3 | Basilar | Death day 4 | VA | Yes |
| Bala et al. 2003 (12) | 46 | M | Fall | 15 | Basilar | Hemiparesthesia | CTA, MRA | |
| Cho et al. 2008 (13) | 54 | M | Bicycle crash | 8 | Vertebral | Dependent | VA, CTA | |
| Garcia et al. 2012 (14) | 37 | M | Fall | 15 | Basilar | Hemiparesis | CTA, MRA | |
| Yamamoto et al. 2015 (15) | 62 | M | Bicycle crash | 15 | Vertebral | Disorientation | 3D-DSA | |
| Present Case, 2017 | 74 | F | Fall onto crown | 3 | Basilar | Death | CTA, MRA | Yes |
GCS – Glasgow Coma Scale
F – Female
MVC – motor vehicle collision
VA – vertebral angiography
NA – not available
M – Male
CTA – computed tomography angiography
MRA – magnetic resonance angiography
3D-DSA – three-dimensional digital subtraction angiography
Sato et al. had included an image of the longitudinal fracture with its dural laceration and a photomicrograph of the entrapped basilar artery within the fracture cleft with occlusion of the arterial lumen and loss of the integrity of the inner elastic layer (11).
Conclusion
Fractures of the clivus are rare and the longitudinal subtype of clival fractures are often fatal from associated entrapment of the vertebrobasilar arterial circulation. This is the first case reported in the forensic pathology literature. The nature of precipitating incident that initiated the injury, the resultant clinical presentation, and associated radiological and pathological findings at autopsy have been presented to highlight and provide an understanding of the entity for the forensic pathology community and add to the number of published cases. The diagnostic utility of both CT and CTA in raising suspicion for intracranial and extracranial arterial traumatic injury has been highlighted.
Although radiological imaging had diagnosed the nature of the underlying injurious pathology, which provided a clear explanation of the clinical course and resultant death of the patient, the performance of the postmortem examination to answer a specific clinical query was invaluable in providing clinicopathological correlation, an overall understanding of the nature of this rare entity, and the operative underlying mechanism of injury in this type of case, which may not have undergone a medicolegal autopsy in many death investigation jurisdictions and therefore may never been seen by forensic pathologists in a postmortem setting. For this reason, it has been presented in the forensic pathology literature to alert forensic pathologists of its existence, especially in the setting of a criminal assault.
Footnotes
ETHICAL APPROVAL
As per Journal Policies, ethical approval was not required for this manuscript
STATEMENT OF HUMAN AND ANIMAL RIGHTS
This article does not contain any studies conducted with animals or on living human subjects
STATEMENT OF INFORMED CONSENT
No identifiable personal data were presented in this manuscsript
DISCLOSURES & DECLARATION OF CONFLICTS OF INTEREST
The authors, reviewers, editors, and publication staff do not report any relevant conflicts of interest
FINANCIAL DISCLOSURE The authors have indicated that they do not have financial relationships to disclose that are relevant to this manuscript
References
- 1.Dymock R.B.. Traumatic basal subarachnoid haemorrhage. Med J Aust. 1977. Aug 13; 2(7): 216–8. PMID: 909485. [DOI] [PubMed] [Google Scholar]
- 2.Loop J.W. White L.E. Jr. Shaw C.M.. Traumatic occlusion of the basilar artery within a clivus fracture. Radiology. 1964. Jul; 83: 36–40. PMID: 14191653. 10.1148/83.1.36. [DOI] [PubMed] [Google Scholar]
- 3.Lindenberg R.. Incarceration of a vertebral artery in the cleft of a longitudinal fracture of the skull. Case report. J Neurosurg. 1966. May; 24(5): 908–10. PMID: 5943227. 10.3171/jns.1966.24.5.0908. [DOI] [PubMed] [Google Scholar]
- 4.Sights W.P. Jr.. Incarceration of the basilar artery in a fracture of the clivus. Case report. J Neurosurg. 1968. Jun; 28(6): 588–91. PMID: 5671294. 10.3171/jns.1968.28.6.0588. [DOI] [PubMed] [Google Scholar]
- 5.Shaw C.M. Alvord E.C. Jr.. Injury of the basilar artery associated with closed head trauma. J Neurol Neurosurg Psychiatry. 1972. Apr; 35(2): 247–57. PMID: 5037036. PMCID: PMC494044. 10.1136/jnnp.35.2.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anthony D.C. Atwater S.K. Rozear M.P. Burger P.C.. Occlusion of the basilar artery within a fracture of the clivus: case report. J Neurosurg. 1987. Jun; 66(6): 929–31. PMID: 3572522. 10.3171/jns.1987.66.6.0929. [DOI] [PubMed] [Google Scholar]
- 7.Guha A. Fazl M. Cooper P.W.. Isolated basilar artery occlusion associated with a clivus fracture. Can J Neurol Sci. 1989. Feb; 16(1): 81–3. PMID: 2924213. 10.1017/s0317167100028560. [DOI] [PubMed] [Google Scholar]
- 8.Corradino G. Wolf A.L. Mirvis S. Joslyn J.. Fractures of the clivus: classification and clinical features. Neurosurgery. 1990. Oct; 27(4): 592–6. PMID: 2234364. 10.1227/00006123-199010000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Sato H. Sakai T. Uemura K.. [A case of incarceration of the vertebral and basilar arteries in a longitudinal fracture of the clivus]. No Shinkei Geka. 1990. Dec; 18(12): 1147–50. Japanese. PMID: 2280817. [PubMed] [Google Scholar]
- 10.Taguchi Y. Matsuzawa M. Morishima H. et al. Incarceration of the basilar artery in a longitudinal fracture of the clivus: case report and literature review. J Trauma. 2000. Jun; 48(6): 1148–52. PMID: 10866264. 10.1097/00005373-200006000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Sato S. Iida H. Hirayama H. et al. Traumatic basilar artery occlusion caused by a fracture of the clivus–case report. Neurol Med Chir (Tokyo). 2001. Nov; 41(11): 541–4. PMID: 11758706. 10.2176/nmc.41.541. [DOI] [PubMed] [Google Scholar]
- 12.Bala A. Knuckey N. Wong G. Lee G.Y.. Longitudinal clivus fracture associated with trapped basilar artery: unusual survival with good neurological recovery. J Clin Neurosci. 2004. Aug; 11(6): 660–3. PMID: 15261246. 10.1016/j.jocn.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Cho J. Moon C.T. Kang H.S. et al. Traumatic entrapment of the vertebrobasilar junction due to a longitudinal clival fracture: a case report. J Korean Med Sci. 2008. Aug; 23(4): 747–51. PMID: 18756072. PMCID: PMC2526400. 10.3346/jkms.2008.23.4.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.García-García J. Villar-Garcia M. Abad L. Segura T.. Brainstem infarct due to traumatic basilar artery entrapment caused by longitudinal clival fracture. Arch Neurol. 2012. May; 69(5): 662–3. PMID: 22248477. 10.1001/archneurol.2011.1155. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto S. Toyota S. Nakamura H. et al. Traumatic entrapment of the vertebral artery demonstrated by a 3D angiographic study. World Neurosurg. 2016. Nov; 95: 623.e5–623.e9. PMID: 27350302. 10.1016/j.wneu.2016.06.067. [DOI] [PubMed] [Google Scholar]
- 16.Vanezis P.. Techniques used in the evaluation of vertebral artery trauma at post-mortem. Forensic Sci Int. 1979. Mar-Apr; 13(2): 159–65. PMID: 447149. 10.1016/0379-0738(79)90280-9. [DOI] [PubMed] [Google Scholar]
- 17.Ochalski PG1 Spiro R.M. Fabio A. et al. Fractures of the clivus: a contemporary series in the computed tomography era. Neurosurgery. 2009. Dec; 65(6): 1063–9; discussion 1069. PMID: 19934965. 10.1227/01.NEU.0000360154.18604.28. [DOI] [PubMed] [Google Scholar]
- 18.Menkü A. Koç R.K. Tucer B. et al. Clivus fractures: clinical presentations and courses. Neurosurg Rev. 2004. Jul; 27(3): 194–8. PMID: 15034764. 10.1007/s10143-004-0320-2. [DOI] [PubMed] [Google Scholar]
- 19.Joslyn J.N. Mirvis S.E. Markowitz B.. Complex fractures of the clivus: diagnosis with CT and clinical outcome in 11 patients. Radiology. 1988. Mar; 166(3): 817–21. PMID: 3340778. 10.1148/radiology.166.3.3340778. [DOI] [PubMed] [Google Scholar]
- 20.Winkler-Schwartz A. Correa J.A. Marcoux J.. Clival fractures in a Level I trauma center. J Neurosurg. 2015. Jan; 122(1): 227–35. PMID: 25343182. 10.3171/2014.9.JNS14245. [DOI] [PubMed] [Google Scholar]
- 21.AO Foundation [Internet]. Davos (Switzerland): AO Foundation; c2017. Diagnosis: skull base fractures; [cited 2017 May 8]. Available from: https://www2.aofoundation.org/wps/portal/!ut/p/a0/04_Sj9CPykssy0xPLMnMz0vMAfGjzOKN_A0M3D2DDbz9_UMMDRyDXQ3dw9wMDAx8jfULsh0VAdAsNSU!/?bone=CMF&segment=Cranium&soloState=lyteframe&teaserTitle=&contentUrl=srg/93/01-Diagnosis/skull_base-skull_base.jsp. [Google Scholar]
- 22.Hoffmann E. Prescher A.. The clivus: anatomy, normal variants and imaging pathology. Clin Neuroradiol. 2012. Jun; 22(2): 123–39. PMID: 21710384. 10.1007/s00062-011-0083-4. [DOI] [PubMed] [Google Scholar]
- 23.Kapila A. Chakeres D.W.. Clivus fracture: CT demonstration. J Comput Assist Tomogr. 1985. Nov-Dec; 9(6): 1142–4. PMID: 4056156. 10.1097/00004728-198511000-00033. [DOI] [PubMed] [Google Scholar]
- 24.Sanders B.B. VanderArk G.D.. Transverse fracture of the clivus. J Neurosurg. 1973. Nov; 39(5): 610–4. PMID: 4743568. 10.3171/jns.1973.39.5.0610. [DOI] [PubMed] [Google Scholar]
- 25.Wang A. Wainwright J. Cooper J. et al. Basilar artery herniation into the sphenoid sinus secondary to traumatic skull base fractures: case report and review of the literature. World Neurosurg. 2017. Feb; 98: 878.e7–878.e10. PMID: 27888078. 10.1016/j.wneu.2016.11.068. [DOI] [PubMed] [Google Scholar]
- 26.Kaakaji R. Russell E.J.. Basilar artery herniation into the sphenoid sinus resulting in pontine and cerebellar infarction: demonstration by three-dimensional time-of-flight MR angiography. AJNR Am J Neuroradiol. 2004. Sep; 25(8): 1348–50. PMID: 15466330. [PMC free article] [PubMed] [Google Scholar]
- 27.Ochalski P.G. Adamo M.A. Adelson P.D. et al. Fractures of the clivus and traumatic diastasis of the central skull base in the pediatric population. J Neurosurg Pediatr. 2011. Mar; 7(3): 261–7. PMID: 21361764. 10.3171/2010.12.PEDS10190. [DOI] [PubMed] [Google Scholar]
- 28.Khanna P. Bobinski M.. Computed tomography and magnetic resonance imaging of a basilar artery herniation into the sphenoid sinus. Skull Base. 2010. Jul; 20(4): 269–73. PMID: 21311620. PMCID: PMC3023321. 10.1055/s-0030-1247629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hofmann E. Prescher A.. The clivus: anatomy, normal variants and imaging pathology. Clin Neuroradiol. 2012. Jun; 22(2): 123–39. PMID: 21710384. 10.1007/s00062-011-0083-4. [DOI] [PubMed] [Google Scholar]
- 30.Meguro K. Rowed D.W.. Traumatic aneurysm of the posterior inferior cerebellar artery caused by fracture of the clivus. Neurosurgery. 1985. May; 16(5): 666–8. PMID: 4000439. 10.1227/00006123-198505000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Metso T.. Cervicocerebral artery dissections: risk factors and clinical features [dissertation] [Online]. Helsinki: University of Helsinki; 2013. 63 p. [cited 2017 May 8]. Available from: http://urn.fi/URN: ISBN: 978-952-10-8524-6. [Google Scholar]
- 32.Yesilot Barlas N. Putaala J. Waje Andreassen U. et al. Etiology of first-ever ischaemic stroke in European young adults: the 15 cities young stroke study. Eur J Neurol. 2013. Nov; 20(11): 1431–9. PMID: 23837733. 10.1111/ene.12228. [DOI] [PubMed] [Google Scholar]


