Abstract
Posttraumatic stress disorder (PTSD) has been linked to a wide array of risky and health-compromising behaviors, including risky sexual behavior (RSB). Cross-sectional studies reveal positive associations between emotion dysregulation and both PTSD and RSB. This study extended that work by exploring whether intermediate levels of emotion dysregulation across multiple dimensions account for the relation between baseline PTSD symptoms and RSB (i.e., number of vaginal sex partners, number of instances of condomless sex, and number of instances of risky/impulsive sex) 16 months later. Participants were 447 trauma-exposed young adult women from the community (60.0% White; M age = 21.80 years) who completed five assessments (separated by 4-month increments) over a 16-month period. Baseline PTSD symptoms were significantly positively associated with all emotion dysregulation dimensions at 8-months and the number of instances of risky/impulsive sex at 16-months. Further, results revealed significant indirect effects of baseline PTSD symptoms on (1) 16-month vaginal sex partners through both the nonacceptance of negative emotions and difficulties controlling impulsive behaviors when distressed at 8-months, and (2) 16-month risky/impulsive sex through difficulties engaging in goal-directed behaviors when distressed at 8-months. Results provide support for the mediating roles of nonacceptance of negative emotions and difficulties controlling behaviors when distressed in the relation between PTSD symptoms and later RSB.
Keywords: posttraumatic stress disorder, emotion dysregulation, emotion regulation, emotional nonacceptance, risky sexual behavior
INTRODUCTION
Findings of the World Mental Health Survey Consortium indicate that 29% to 85% of individuals worldwide experience at least one traumatic event (i.e., exposure to threatened death, serious injury, or sexual violence) in their lifetime, with estimates in most countries ranging from 61% to 76% (Benjet et al., 2016). Trauma exposure has been linked to deleterious mental and physical health outcomes (e.g., Keyes et al., 2013; Spitzer et al., 2009; Turner & Lloyd, 1995)–most notably the development of posttraumatic stress disorder (PTSD; Breslau et al., 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). PTSD is characterized by intrusions, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity following exposure to a traumatic event (American Psychiatric Association [APA], 2013), and has a lifetime prevalence rate of 8.3% among U.S. adults (Kilpatrick et al., 2013). The conditional probability of PTSD has been shown to vary as a function of Criterion A event type (with the highest prevalence rates found for interpersonal trauma and combat). The conditional prevalence of PTSD using DSM-5 criteria is 9.3% if assessed in relation to a single Criterion A event and 10.5% if assessed in relation to multiple Criterion A events (Kilpatrick et al., 2013).
PTSD is a serious clinical concern, associated with considerable functional impairment (Kessler & Frank, 1997) and high rates of co-occurring psychiatric disorders (Kessler, Chiu, Demler, Merikangas, & Walters, 1995). Moreover, individuals with PTSD are at-risk for engagement in a wide array of risky and health-compromising behaviors (e.g., Weiss, Tull, Sullivan, Dixon-Gordon, & Gratz, 2015b; Weiss, Tull, Viana, Anestis, & Gratz, 2012b), including risky sexual behavior (RSB; Cavanaugh, Hansen, & Sullivan, 2010; Gore-Felton & Koopman, 2002; Holmes, Foa, & Sammel, 2005; Hutton et al., 2001; Reisner, Mimiaga, Safren, & Mayer, 2009; Weiss, Tull, Borne, & Gratz, 2013b).
RSB can be defined as sexual behavior that increases the likelihood of HIV, other sexually tranmitted infections (STIs), and/or unintended pregnany, including the use of substances prior to or during sexual activity, sex with multiple partners, inconsistent condom use, and not engaging in safe sex communication (Turchick & Garske, 2009). Given these negative outcomes associated with RSB, research examining the factors that may underlie the association between PTSD and RSB is needed. Such research may improve our understanding of the ways in which PTSD contributes to RSB and highlight potential targets for intervention to prevent the occurrence of this behavior.
One potential factor highlighted in the literature is emotion dysregulation. As defined here, emotion dysregulation is a multidimensional construct involving maladaptive ways of responding to emotions, including deficits in the understanding, acceptance, and effective use and modulation of emotions (Gratz, Dixon, Kiel, & Tull, in press; Gratz & Roemer, 2004). Research underscores the relevance of emotion dysregulation to PTSD (e.g., Ehring & Quack, 2010; McDermott, Tull, Gratz, Daughters, & Lejuez, 2009; Tull, Barrett, McMillan, & Roemer, 2007; Weiss, Tull, Anestis, & Gratz, 2013a; Weiss et al., 2012a), revealing heightened levels of both overall emotion dysregulation and most of its specific dimensions (including emotional nonacceptance, difficulties controlling behaviors when distressed, limited access to effective emotion regulation strategies, and lack of emotional clarity) among individuals with (vs. without) PTSD (e.g., Tull et al., 2007; Weiss et al., 2012a). Moreover, emotion dysregulation has been found to underlie the relation between PTSD and overall risky behaviors (Weiss et al., 2015b; Weiss et al., 2012b).
Although no research to date has examined the mediating role of emotion dysregulation in the relation between PTSD and RSB per se, theories highlight the relevance of emotion dysregulation to RSB among individuals with PTSD. For example, findings that negative affect may increase the risk for engagement in RSB (e.g., Crepaz & Marks, 2001; Fortenberry, Temkit, Tu, Katz, & Orr, 2003; Lucenko, Malow, Sanchez-Martinez, Jennings, & Dévieux, 2003) have led researchers to theorize that RSB may function to down-regulate negative emotions by alleviating or distracting attention away from negative affective states (Crepaz & Marks, 2001)–a process that may be particularly relevant to individuals with heightened levels of emotion dysregulation, such as those with PTSD (e.g., Tull et al., 2007; Weiss et al., 2013a). Likewise, and consistent with positive reinforcement models of sexual risk taking (Cooper, Shapiro, & Powers, 1998), the short-term pleasure associated with RSB may function to counter or distract from negative affective states (Briere & Elliott, 1994). Finally, heightened levels of emotion dysregulation are theorized to interfere with the ability to control behaviors and increase the risk for maladaptive behavioral responses in general, including RSB (Linehan, 1993).
Consistent with this theoretical literature, a small but growing body of research provides support for the role of emotion dysregulation in RSB (Artime & Peterson, 2012; Messman-Moore, Walsh, & DiLillo, 2010; Tull, Weiss, Adams, & Gratz, 2012). For example, overall emotion dysregulation was uniquely associated with RSB among substance dependent patients, above and beyond demographics, depression, sensation seeking, traumatic exposure, and substance use severity (Tull et al., 2012). Additionally, overall emotion dysregulation was positively associated with past 6-month RSB among female college students with a history of childhood sexual and physical abuse (Messman-Moore et al., 2010). Finally, Artime and Peterson (2012) found that two dimensions of emotion dysregulation– difficulties controlling impulsive behaviors when distressed and limited access to effective emotion regulation strategies–were associated with RSB among heterosexual men, and deficits in the ability to access effective emotion regulation strategies in particular mediated the relation between childhood sexual abuse severity and number of lifetime sexual partners.
Taken together, this literature provides support for the role of emotion dysregulation in the PTSD-RSB relation. Nonetheless, important limitations exist. First, as noted above, although past studies have documented associations between both PTSD and emotion dysregulation, and emotion dysregulation and RSB, no studies have examined whether emotion dysregulation mediates the relation between PTSD and later RSB. Second, whereas cross-sectional studies provide preliminary evidence for the role of emotion dysregulation in the relation between PTSD and overall engagement in risky behaviors (Weiss et al., 2012b; 2015b), these relations have not been examined longitudinally. Finally, the vast majority of research has examined the relation of global emotion dysregulation to RSB. Research focused on elucidating the particular dimensions of emotion dysregulation most relevant to RSB may inform the development of more targeted treatments for reducing RSB among individuals with PTSD.
The present investigation addressed these limitations by examining PTSD symptoms as a prospective predictor of RSB among trauma-exposed community women and exploring the mediating role of emotion dysregulation dimensions in this association. To this end, we examined if baseline PTSD symptoms predicted emotion dysregulation at 8-months and RSB at 16-months. We also examined the indirect relation of PTSD symptoms to later RSB through intermediary levels of emotion dysregulation dimensions. We hypothesized that the relation of PTSD symptoms to later RSB would be indirect through emotion dysregulation dimensions.
METHOD
Participants
The current data were drawn from a large, multi-site, prospective study of emotion dysregulation and sexual revictimization among young adult women in the community (the population most at risk for sexual victimization; Breslau et al., 1998; Pimlott-Kubiak & Cortina, 2003). A convenience sample of 491 women aged 18–25 were recruited from four sites in the southern and midwestern United States (including Mississippi, Nebraska, and Ohio) for a study on “women’s life experiences and adjustment” (see Procedure for further details). Of these, 447 women (91.0%) reported the direct experience of at least one potentially traumatic event at the baseline assessment and, thus, were eligible for inclusion in the present study.
Participants ranged in age from 18 to 25 years (M = 21.80, SD = 2.22) at the time of the baseline assessment and were ethnically diverse (60.0% White, 36.2% Black/African American, 5.6% Latina, 4.5% American Indian, 4.3% Asian, 2.7% other). With regard to educational attainment, 97.0% of participants had received their high school diploma or GED, with many (70.2%) continuing on to complete at least some higher education. Just over half of the participants (52.3%) were full-time students and most (82%) were single.
Procedure
All procedures received prior approval by the Institutional Review Boards of the participating institutions. Recruitment methods included advertisements for a study on “women’s life experiences and adjustment” posted online and throughout the community (coffee shops, stores, clinics, etc.), in addition to random sampling from the community. With regard to random sampling, women within the targeted age range (18–25) were identified from a large database of residential mailing addresses compiled by Survey Sampling International (SSI), a private research organization that provides sampling services to government and academic research entities. Information used to identify household members matching the designated gender and age criteria was obtained by SSI from a variety of secondary sources, including school and voter registration lists. Randomly selected individuals from this list were sent a letter inviting them to participate in a longitudinal study of prior life events and current adjustment. The recruitment letter contained a description of the project, a post-paid response card to be mailed back by interested individuals, and a $1 cash incentive. The letter also informed recipients that project personnel would attempt to contact them by telephone to answer any questions they may have about the study. All participants provided written informed consent.
Participants completed five assessments (separated by 4-month increments) over a 16-month period. At the baseline, 8-month, and 16-month assessments, participants completed a series of online self-report questionnaires and laboratory tasks in the laboratory of one of the study sites. These laboratory assessments were supplemented by briefer assessments at 4-months and 12-months consisting of online self-report questionnaires only (which could be completed either at home or in the laboratory). Participants were compensated $75 for the baseline assessment, $50 for subsequent laboratory assessments, and $25 for the briefer assessments. The current study utilized data collected at all five time points; specifically, PTSD symptoms were assessed at baseline, intermediary emotion dysregulation was assessed at 8-months, and RSB was assessed at 4-, 8-, 12-, and 16-months, with data from the 4- and 8-month assessments summed to capture intermediary RSB occurring between baseline and 8-months (referred to as 8-month RSB) and data from the 12- and 16-month assessments summed to capture RSB occurring between 8- and 16-months (referred to as 16-month RSB).
Measures
Traumatic exposure
The Life Events Checklist (LEC; Gray, Litz, Hsu, & Lombardo, 2004) is a 17-item self-report measure designed to screen for potentially traumatic events in a respondent’s lifetime (e.g., sexual assault, physical assault, motor vehicle accident, life-threatening illness). The LEC has demonstrated convergent validity with measures assessing potentially traumatic event exposure and psychopathology known to relate to traumatic exposure (Gray et al., 2004). Participants were asked to indicate all of the events that they had directly experienced (i.e., “happened to me”). The current study used LEC data from the baseline assessment.
PTSD symptoms
The PTSD Checklist–Civilian Version (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993) is a widely used, 17-item self-report measure of re-experiencing, avoidance, emotional numbing, and hyperarousal symptoms of PTSD. Participants completed the PCL in reference to the event they identified as most traumatic on the LEC at the time of the assessment. The items on the PCL correspond to the Diagnostic and Statistical Manual of Mental Disorders (APA, 2000) criteria for a PTSD diagnosis. Using a 5-point Likert-type scale (1 = not at all, 5 = extremely), participants rated the extent to which each symptom had bothered them in the past month. The validity of the PCL has been demonstrated in civilian populations (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). The PCL has also been found to have strong test-retest reliability (r = .96), as well as moderate to strong correlations with other PTSD measures (Weathers et al., 1993). Further, the PCL demonstrates high levels of agreement with the Clinician Administered PTSD Scale (Blake et al., 1990), a well-established and empirically supported interview-based measure of PTSD (Grubaugh, Elhai, Cusack, Wells, & Frueh, 2007; Palmieri, Weathers, Difede, & King, 2007). Given evidence that PTSD is best represented as a dimensional construct (Broman-Fulks et al., 2006; Forbes, Haslam, Williams, & Creamer, 2005; Ruscio, Ruscio, & Keane, 2002), participants’ responses to each item were summed to provide a total score representing overall PTSD symptoms. The current study used PCL data from the baseline assessment (α = .94).
Emotion dysregulation
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report measure that assesses individuals’ current levels of emotion dysregulation across six domains: nonacceptance of negative emotions, difficulties engaging in goal-directed behaviors when distressed, difficulties controlling impulsive behaviors when distressed, limited access to emotion regulation strategies perceived as effective, lack of emotional awareness, and lack of emotional clarity. Participants rated each item using a 5-point Likert-type scale (1 = almost never, 5 = almost always). The DERS and its subscales demonstrate good test-retest reliability and construct and predictive validity and are significantly associated with objective measures of emotion regulation (Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007; Gratz & Roemer, 2004; Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Gratz & Tull, 2010; Vasilev, Crowell, Beauchaine, Mead, & Gatzke‐Kopp, 2009). Higher scores indicate greater emotion dysregulation. The current study used DERS data from the 8-month assessment (αs ≥ .82).
Risky sexual behavior
RSB was assessed via 10 items drawn from and modeled after the Sexual Risk Survey (SRS; Turchik & Garske, 2009), an empirically-supported measure designed to assess RSB in young adult populations. Specifically, items assessed three types of RSB: (1) the number of different vaginal sexual partners; (2) the number of instances of condomless sex (i.e., consensual oral, vaginal, or anal sex [separately] without a condom); and (3) the number of instances of risky/impulsive sexual behaviors (e.g., sex in exchange for money, drugs, or other services). For the condomless sex outcome, items were weighted to reflect increased risk for HIV/STI transmission via anal sex (compared to vaginal sex) and decreased risk via oral sex (compared to vaginal sex). Specifically, the following risk score was computed for condomless sex at each wave: risk score = (number of vaginal episodes) + (2x number of anal episodes) + (0.1x number of oral episodes; see Susser, Desvarieux, & Wittkowski, 1998). Items assessing the number of instances of risky/impulsive sexual behaviors were summed at each wave. At baseline, participants indicated the number of lifetime instances of each of the aforementioned experiences; at each subsequent wave, they indicated the number of instances over the past 4 months. Of note, because the baseline RSB measure assessed lifetime experiences, RSB at 4- and 8-months was included as a covariate to control for participant’s recent patterns of sexual behavior. The current study used RSB data from the 4-, 8-, 12-, and 16-month assessments.
Missing Data
Among the 447 eligible participants, the percentages of missing data at each assessment were as follows: 7.8% at baseline, 13.9% at 4-months, 19.0% at 8-months, 25.1% at 12-months, and 30.2% at 16-months. Participants who completed all assessments differed significantly from those who did not on baseline measures of income (F [1, 441] = 9.54, p = .002; M = 3.20 [SD = 2.61] vs. M = 2.45 [SD = 2.12]), PTSD symptoms (F [1, 410] = 17.47, p < .001; M = 30.56 [SD = 13.92] vs. M = 37.21 [SD = 17.90], respectively), number of vaginal sexual partners (F [1, 488] = 9.80, p = .002; M = 7.43 [SD = 9.18] vs. M = 10.36 [SD = 11.28], respectively), number of instances of condomless sex (F [1, 478] = 6.37, p = .012; M = 20.9 [SD = 26.8] vs. M = 27.3 [SD = 27.2], respectively), and number of instances of risky/impulsive sexual behaviors (F [1, 478] = 5.46, p = .020; M = 12.9 [SD = 17.1] vs. M = 17.1 [SD = 21.5], respectively). There were no other significant baseline differences in demographic characteristics or the variables of interest between participants who completed all assessments (vs. those who did not; ps > .12).
Missing item-level outcome data were handled via multiple imputation with linear regression using income, PCL, and RSB scores at baseline as auxiliary variables to impute RSB items at subsequent waves. Five imputed datasets were produced and the resulting imputed items were averaged across the five datasets to produce a single imputed item per participant. Then, the imputed RSB items at the 4- and 8-month assessments were summed to capture RSB that occurred between baseline and the 8-month assessment (i.e., 8-month RSB) and the imputed RSB items at the 12- and 16-month assessments were summed to capture RSB that occurred between the 8- and 16-month assessments (i.e., 16-month RSB). Missing DERS scores at the 8-month assessment were imputed using the same methods (i.e., five imputed datasets with DERS scores at baseline serving as auxiliary variables).
Analytic Strategy
Associations between 16-month RSB and both baseline demographic variables (i.e., age, race/ethnicity, past-year household income, education, and marital status) and 12- and 16-month relationship status (coded as 0 = not in a romantic relationship and 1 = in a romantic relationship) were examined using correlation analyses and analyses of variance. Any variable found to demonstrate a significant relation to any of the RSB outcome variables was included as a covariate in the primary analyses. Descriptive statistics and intercorrelations among the primary study variables were also calculated.
A path model was specified in Mplus version 7.4. Following procedures outlined by Preacher and Hayes (2004), analyses were conducted to examine whether emotion dysregulation at 8-months mediated the relation between baseline PTSD symptoms and 16-month RSB, controlling for 8-month RSB. The bootstrap method was used to estimate the standard errors of parameter estimates and the bias-corrected confidence intervals of the indirect effects (see MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Preacher & Hayes, 2004). The bias-corrected confidence interval is based on a non-parametric resampling procedure that has been recommended when estimating confidence intervals of the mediated effect due to the adjustment it applies over a large number of bootstrapped samples (Efron, 1987). The mediated effect is significant if the 95% confidence interval does not contain zero (Preacher & Hayes, 2004). In this study, 5000 bootstrap samples were used to derive estimates of the indirect effect.
RESULTS
Preliminary Analyses
Both the number of different vaginal sexual partners and the number of instances of risky/impulsive sexual behaviors at 16-months were kurtotic (> 3.75; Gravetter & Wallnau, 2014). As noted by Brown (2006), the maximum likelihood robust (MLR) estimator, which is robust to non-normality and, thus, can be used with kurtotic continuous outcomes, was used in the present analyses. None of the dependent variables (i.e., 16-month RSB variables) were significantly associated with baseline age, education level, or marital status; however, the number of different vaginal sexual partners was significantly negatively associated with income (r(445) = −.13, p <.01), and the number of instances of condomless sex was higher among White (vs. non-White) participants (r(445) = .20, p < .001). Likewise, relationship status (both 12- and 16-month) was significantly associated with RSB outcomes, such that women in a relationship at the 12- and 16-month assessments reported significantly more vaginal sexual partners (Fs ≥ 7.86, ps < .01) and condomless sex (Fs ≥ 13.25, ps < .001) than those not in a romantic relationship. Further, women in a relationship at the 16-month assessment reported fewer instances of risky/impulsive sexual behaviors than those not in a relationship (F [1, 444] = 14.18, p <.001). Thus, in addition to 8-month RSB, mediation models controlled for baseline income and racial/ethnic background as well as relationship status at the 12- and 16-month assessments.
Descriptive data, as well as zero-order correlations among the primary study variables, are shown in Table 1. Baseline PTSD symptoms were significantly positively associated with all of the emotion dysregulation dimensions at 8-months, and with the number of different vaginal sexual partners and the number of instances of risky/impulsive sexual behaviors at 16-months, although only modestly. Baseline PTSD symptoms were not significantly correlated with the number of instances of condomless sex. Further, several emotion dysregulation dimensions at 8-months were significantly positively associated with 16-month RSB outcomes; specifically, emotional nonacceptance was significantly associated with the number of instances of both condomless sex and risky/impulsive sex, difficulties both controlling impulsive behaviors and engaging in goal-directed behaviors when distressed were significantly associated with the number of different vaginal sex partners and the number of instances of risky/impulsive sex, and limited access to effective emotion regulation strategies was significantly associated with the number of instances of risky/impulsive sex.
Table 1.
Descriptive Data and Intercorrelations among Baseline Posttraumatic Stress Disorder (PTSD) Symptoms, 8-Month Emotion Dysregulation Dimensions, and 16-Month Risky Sexual Behavior Outcomes
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Baseline PTSD Symptoms | -- | .32*** | .27*** | .37*** | .40*** | .18** | .26*** | .14** | .05 | .10* |
| 2. 8-mo DERS Nonaccept | -- | -- | .51*** | .58*** | .71*** | .32*** | .42*** | .07 | .15** | .19*** |
| 3. 8-mo DERS Goals | -- | -- | -- | .59*** | .63*** | .26*** | .40*** | .11* | .05 | .18*** |
| 4. 8-mo DERS Impulse | -- | -- | -- | -- | .72*** | .36*** | .47*** | .15** | .06 | .15** |
| 5. 8-mo DERS Strategies | -- | -- | -- | -- | -- | .40*** | .51*** | .11* | .05 | .14** |
| 6. 8-mo DERS Aware | -- | -- | -- | -- | -- | -- | .62*** | .13* | −.02 | .03 |
| 7. 8-mo DERS Clarity | -- | -- | -- | -- | -- | -- | -- | .10 | .003 | .09 |
| 8. 16-mo number vaginal sex partners | -- | -- | -- | -- | -- | -- | -- | .18*** | .22*** | |
| 9. 16-mo condomless sex frequency | -- | -- | -- | -- | -- | -- | -- | -- | -- | .15** |
| 10. 16-mo risky/impulsive sex frequency | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| M | 32.92 | 11.95 | 12.72 | 10.29 | 14.83 | 12.99 | 9.55 | 3.90 | 26.37 | 4.20 |
| SD | 15.75 | 5.75 | 5.12 | 4.30 | 6.22 | 5.26 | 3.50 | 4.43 | 33.03 | 7.31 |
Note. DERS=Difficulties in Emotion Regulation Scale; DERS Nonaccept = Emotional Nonacceptance subscale; DERS Goals = Difficulties Engaging in Goal-Directed Behavior When Distressed subscale; DERS Impulse = Difficulties Controlling Impulsive Behaviors When Distressed subscale; DERS Strategy = Lack of Access to Effective Emotion Regulation Strategies subscale; DERS Aware = Lack of Emotional Awareness subscale; DERS Clarity = Lack of Emotional Clarity subscale.
p < .05.
p < .01.
p < .001.
Primary Analyses
A path model was specified to examine the role of emotion dysregulation dimensions at 8-months in the relation between baseline PTSD symptoms and 16-month RSB (controlling for racial/ethnic background, baseline income, 12-month and 16-month relationship status, and 8-month RSB). Emotion dysregulation dimensions were entered simultaneously and allowed to correlate; the three RSB outcomes (i.e., number of vaginal sex partners, number of instances of condomless sex, and number of instances of risky/impulsive sex) were also allowed to correlate. Notably, although previous approaches to mediation required demonstration of a significant relation between the independent variable and dependent variable (see Baron & Kenny, 1986; Judd & Kenny, 1981; James & Brett, 1984), more recent evidence (see Hayes, 2009; MacKinnon et al., 2000; Rucker, Preacher, Zakary, Tormala, & Petty, 2011; Shrout & Bolder, 2002; Zhao et al., 2010) suggests that this perspective is too restrictive and may impair theory development and testing. Moreover, simulation studies show that mediation can occur when the total or direct effects are missing (Rucker et al., 2011). Thus, consistent with these latter approaches, we examined the indirect relations of PTSD symptoms to RSB outcomes through emotion dysregulation dimensions even in the absence of a significant direct relation.
Although a significant chi square was found, χ2(df = 63) = 132.73, p < .001, the other fit indices indicated that the model fit the data adequately, CFI = .93, RMSEA = .06, SRMR = .07. Further, the model accounted for 21%, 47%, and 8% of the variance in 16-month number of vaginal sex partners, instances of condomless sex, and instances of risky/impulsive sex, respectively (Table 2). Consistent with hypotheses, baseline PTSD symptoms were significantly positively associated with each of the emotion dysregulation dimensions at 8-months. Further, results provided support for the mediating role of intermediary emotion dysregulation in the relation between PTSD symptoms and later RSB, revealing significant indirect effects of baseline PTSD symptoms on (1) 16-month vaginal sexual partners through both nonacceptance of negative emotions and difficulties controlling impulsive behaviors when distressed at 8-months; (2) 16-month condomless sex through nonacceptance of negative emotions at 8-months; and (3) 16-month risky/impulsive sex through difficulties engaging in goal-directed behaviors when distressed at 8-months.
Table 2.
Summary of Mediation Analyses Examining the Role of 8-Month Emotion Dysregulation Dimensions in the Relation between Baseline Posttraumatic Stress Disorder Symptoms and 16-Month Risky Sexual Behavior (5000 bootstrap samples; N = 447)
| Mediating Variable | Effect of PTSD on MV | Effect of MV on RSB | Indirect Effect | Total Effect | ||
|---|---|---|---|---|---|---|
| (MV) | (a) | (b) | (a x b) | 95% CI | (c) | R2 |
| Number of vaginal sex partners | .06+ (.03) | .21*** (.05) | ||||
| DERS Nonaccept | .33***(.06) | .21*(.08) | .07*(.03) | .02, .12 | ||
| DERS Goals | .29***(.06) | .13*(.06) | .04+(.02) | .00, .07 | ||
| DERS Impulse | .35***(.06) | .20*(.09) | .07*(.04) | .01, .13 | ||
| DERS Strategies | .43***(.06) | .03(.07) | .01 (.03) | −.04, .07 | ||
| DERS Aware | .17**(.06) | .03(.06) | .004 (.01) | −.01, .02 | ||
| DERS Clarity | .29***(.06) | −.005(.07) | −.001 (.02) | −.04, .03 | ||
| Frequency of condomless sex | .01 (.03) | .47*** (.06) | ||||
| DERS Nonaccept | .33***(.06) | .17* (.09) | .06* (.03) | .01, .10 | ||
| DERS Goals | .29***(.06) | −.04 (.45) | −.001 (.02) | −.03, .03 | ||
| DERS Impulse | .35***(.06) | .08 (.63) | .003 (.03) | −.04, .05 | ||
| DERS Strategies | .43***(.06) | −.37 (.48) | −.03 (.04) | −.09, .04 | ||
| DERS Aware | .17**(.06) | −.31 (.47) | −.007 (.01) | −.03, .01 | ||
| DERS Clarity | .29***(.06) | −.28 (.62) | −.009 (.02) | −.04, .02 | ||
| Frequency of risky/impulsive sex | .06+ (.03) | .08* (.04) | ||||
| DERS Nonaccept | .33***(.06) | .20 (.16) | .05 (.04) | −.02, .11 | ||
| DERS Goals | .29***(.06) | .25* (.13) | .05* (.03) | .002, .09 | ||
| DERS Impulse | .35***(.06) | −.04 (.17) | −.009 (.04) | −.07, .05 | ||
| DERS Strategies | .43***(.06) | −.11 (.11) | −.03 (.04) | −.10, .04 | ||
| DERS Aware | .17**(.06) | −.06 (.09) | −.008 (.01) | −.03, .01 | ||
| DERS Clarity | .29***(.06) | .05 (.17) | .007 (.03) | −.03, .05 | ||
Note. DERS=Difficulties in Emotion Regulation Scale; DERS Nonaccept = Emotional Nonacceptance subscale; DERS Goals = Difficulties Engaging in Goal-Directed Behavior When Distressed subscale; DERS Impulse = Difficulties Controlling Impulsive Behaviors When Distressed subscale; DERS Strategy = Lack of Access to Effective Emotion Regulation Strategies subscale; DERS Aware = Lack of Emotional Awareness subscale; DERS Clarity = Lack of Emotional Clarity subscale. Model controlled for race/ethnicity, baseline income, 8-month RSB, and relationship status at 12- and 16-months. All coefficients are reported as standardized estimates.
p<.10.
p < .05.
p < .01.
p < .001.
DISCUSSION
The present longitudinal study is the first to examine the role of emotion dysregulation dimensions in the relation between PTSD symptoms and later RSB. Extending cross-sectional research linking emotion dysregulation to RSB (Artime & Peterson, 2012; Messman-Moore et al., 2010; Tull et al., 2012), the current results provide support for the mediating role of intermediary levels of three dimensions of emotion dysregulation–nonacceptance of negative emotions, difficulties controlling impulsive behaviors when distressed, and difficulties engaging in goal-directed behaviors when distressed–in the relation between baseline PTSD symptoms and 16-month RSB outcomes in a large community sample of young adult women. Specifically, findings revealed indirect effects of baseline PTSD symptoms on later vaginal sexual partners through both the nonacceptance of negative emotions and difficulties controlling impulsive behaviors when distressed, on later condomless sex through the nonacceptance of negative emotions, and on later risky/impulsive sex through difficulties engaging in goal-directed behaviors when distressed.
Findings highlighting the relevance of nonacceptance of negative emotions in the relations between PTSD symptoms and both later vaginal sex partners and later condomless sex are consistent with past theory and research linking this emotion dysregulation dimension to risky behaviors in general (Chapman, Gratz, & Brown, 2006; Weiss et al., 2015s; Weiss, Williams, & Connolly, 2015c). Specifically, nonacceptance can increase distress and related efforts to avoid emotions (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996) which, in turn, may increase risk for maladaptive ER strategies (e.g., Chapman et al., 2006; Gratz & Tull, 2010) such as sexual intercourse (Batten, Follette, & Aban, 2002). Indeed, research suggests that trauma-exposed women may engage in sexual behavior to reduce both negative affect in general (Orcutt, Cooper, & Garcia, 2005) and PTSD symptoms in particular (Filipas & Ullman, 2006).
Findings also underscore the relevance of difficulties controlling impulsive behaviors when distressed to the relation between PTSD symptoms and later vaginal sexual partners. Difficulty controlling impulsive behaviors when distressed has been linked to both risky behaviors in general (Weiss et al., 2015a; 2015b; 2015c) and RSB in the form of sexual partners in particular (Artime & Peterson, 2012; Tull et al., 2012). Moreover, this dimension of emotion dysregulation is closely associated with both inhibitory dyscontrol and impulsivity (Whiteside & Lynam, 2001)–constructs that have been linked to RSB (Deckman & DeWall, 2011; Schuster, Crane, Mermelstein, & Gonzalez, 2012).
Finally, result provide support for the relevance of intermediary levels of difficulties engaging in goal-directed behaviors when distressed to the relation between PTSD symptoms and later risky/impulsive sex. Past research suggests that individuals with heightened PTSD symptoms may have greater difficulties engaging in goal-directed behaviors in the context of emotional distress (e.g., Tull et al., 2007; Weiss et al., 2012a). Difficulties focusing attention and completing tasks when experiencing distress may interfere with the implementation of adaptive strategies for regulating distress and/or effective interpersonal behaviors, such as setting limits, saying no, or initiating uncomfortable conversations. Given that several of the items included in this RSB measure reflect sexual behaviors that are later regretted or a failure to discuss important topics related to sexual activity, this particular dimension of emotion dysregulation may interfere with the ability to engage in effective interpersonal behaviors.
Of note, although baseline PTSD symptoms demonstrated significant bivariate associations with both later vaginal sexual partners and later risky/impulsive sexual behaviors, they were not significantly associated with later condomless sex at a bivariate level. These findings suggest that other, more proximal factors–such as nonacceptance of negative emotions and/or difficulties controlling impulsive behaviors when distressed–may play a more important role in this RSB outcome than distal PTSD symptoms. Indeed, researchers have suggested that it is the impact of PTSD symptoms on more proximal processes that may explain the long-term consequences of trauma exposure and related symptoms on negative health outcomes (see DeLongis, Coyne, Dakof, Folkman, & Lazarus, 1982; Felner, Farber, & Primavera, 1983; Felner, Rowlinson, & Terre, 1986). Likewise, although results provided evidence for an indirect relation of PTSD symptoms to all three RSB outcomes through intermediary levels of nonacceptance of negative emotions and difficulties controlling behaviors when distressed, these relations were small. Thus, future research is needed to examine other potential mechanisms that may account for the relation between PTSD symptoms and later RSB, such as the need for approval (Cooper et al., 1998) or a desire for intimacy (Gebhardt, Kuyper, & Greunsven, 2003). Another variable that may be particularly important to examine in this regard is substance use, given evidence that PTSD symptoms predict later substance use (e.g., Chilcoat & Breslau, 1998; Shipherd, Stafford, & Tanner, 2005) and substance use predicts later RSB (e.g., Crockett, Raffaelli, & Shen, 2006; Guo et al., 2002).
Although the results of this study highlight one mechanism that may underlie the association between PTSD symptoms and later RSB, several limitations warrant consideration. First and foremost, although the use of a diverse community sample of young adult women is a strength of this study, the extent to which these findings generalize to clinical samples of patients with PTSD or STIs or other nonclinical or community samples (e.g., men, older adults) remains unclear. Results of this study should be replicated in these and other samples. Likewise, participants with lower incomes and higher levels of baseline PTSD symptoms and RSB were less likely to complete all assessments, which may have influenced the results. Future studies that retain the most symptomatic participants are needed to clarify the generalizability of these findings. Indeed, the differential loss of participants with greater baseline PTSD and RSB may account, at least in part, for the relatively modest indirect relations observed in this study, which may have been stronger for participants with more severe PTSD symptoms and RSB. The extent to which our model accounts for more variance in RSB among patients with PTSD diagnoses or individuals with HIV or other STI warrants examination. Nonetheless, given the relatively small size of the indirect relations found in this study, future research is also needed to explore the clinical meaningfulness of the observed mediating role of emotion dysregulation in the PTSD-RSB relation. Of relevance to this question, there is some evidence suggesting that targeting emotion dysregulation in treatment results in significant reductions (accompanied by medium to large effect sizes) in risky behaviors including RSB (Gratz et al., 2014; Gratz & Tull, 2011).
Additionally, our measure of PTSD in the present study was based on the DSM-IV classification of PTSD. Thus, research is needed to replicate these findings using DSM-5 guidelines for the assessment of PTSD. Given evidence that different types of traumatic events (e.g., childhood abuse vs. natural disaster) may be differentially related to RSB (consistent with the differential effects model; Senn & Carey, 2010), research examining the influence of trauma type on the relations among PTSD, emotion dysregulation, and RSB is needed. Further, we relied on a self-report measure of emotion dysregulation– responses to which may be influenced by an individual’s willingness and/or ability to report accurately on emotional responses. Future studies would benefit from the inclusion of objective indices of emotion dysregulation (e.g., behavioral and physiological measures; Gratz et al., 2006; Gratz, Tull, Matusiewicz, Breetz, & Lejuez, 2013). Likewise, whereas retrospective self-report measures of sexual behavior have been shown to be moderately reliable (Saltzman, Stoddard, McCusker, & Moon, 1987) and more valid than other retrospective assessment methods (e.g., interviews; Fenton, Johnson, McManus, & Erens, 2001), it is possible that participants overestimated or underestimated RSB. Future research would benefit from examining the relations among PTSD symptoms, emotion dysregulation dimensions, and RSB utilizing methods that reduce error and recall bias, such as micro-longitudinal data collection (Searles, Perrine, Mundt, & Helzer, 1995; Simpson et al., 2011).
Finally, the level of risk associated with some of the RSB items (e.g., condomless sex) may vary as a function of both relationship status and type of relationship (e.g., committed vs. not). Although we included relationship status as a covariate in our model, it is important to note that we did not assess—and participants may not know—whether their partners had additional sexual partners, making some of the reported relationships likely non-monogamous. Indeed, results of epidemiological studies suggest that non-monogamy is relatively prevalent, with 17.6% of women and 23.0% of men reporting non-monogamy over a one-year period (Aral & Leichliter, 2010). Thus, although future research is needed to examine differences in the level of risk associated with the RSB outcomes of interest as a function of relationship status and type, the aforementioned findings suggest that condomless sex, even in the context of a romantic relationship, may be risky.
Despite limitations, the results of this study add to the literature on the interrelations among PTSD symptoms, emotion dysregulation, and RSB, highlighting the relevance of dimensions of emotion dysregulation involving the acceptance of emotions and control of behaviors when distressed in the relation between PTSD symptoms and later RSB. These findings highlight potential targets for prevention and early intervention efforts aimed at reducing the risk for RSB among trauma-exposed young adult women in the community. Specifically, findings suggest the utility of teaching young women skills for facilitating both emotional acceptance and behavioral control in the context of negative emotional states, including approaching emotions in a nonjudgmental and non-evaluative way, redirecting attention to non-emotional stimuli, and promoting more adaptive actions in the face of negative emotional arousal. Given past research highlighting the utility of treatments that target these dimensions of emotion dysregulation (e.g., skills training in affect and interpersonal regulation plus modified prolonged exposure, dialectical behavior therapy prolonged exposure, and emotion regulation group therapy; Cloitre, Koenen, Cohen, & Han, 2002; Gratz, Tull, & Levy, 2014; Harned, Korslund, Foa, & Linehan, 2012) for both PTSD (see Cloitre et al., 2002; Harned, Korslund, & Linehan, 2014) and risky behaviors (including RSB; see Gratz & Tull, 2011; Gratz et al., 2014), future research is needed to examine whether these or related interventions may reduce the risk for RSB among trauma-exposed women with PTSD symptoms.
Figure 1.
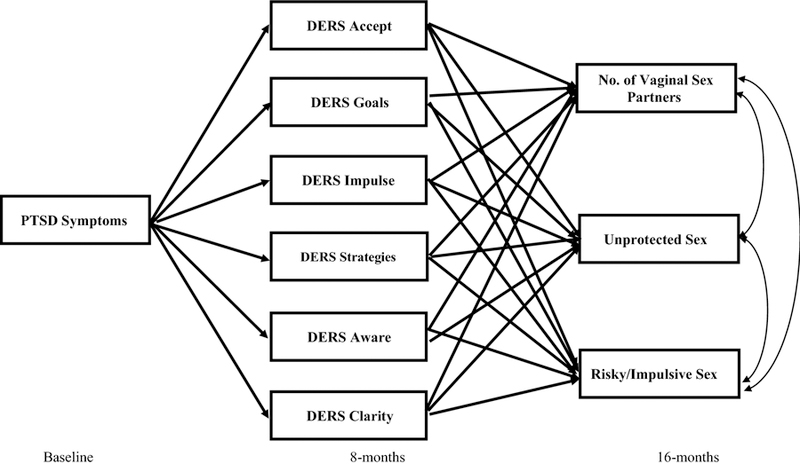
Caption. Hypothesized path model examining which emotion regulation dimensions at 8 months mediate the association between PTSD symptoms at baseline and three correlated aspects of risky sexual behavior at 16 months (although not depicted here, the emotion regulation dimensions at 8 months were allowed to correlate).
ACKNOWLEDGEMENTS
This research was supported by National Institute of Child Health and Human Development Grant R01 HD062226, awarded to the third author (DD). Work on this paper by the first author (NHW) was supported by National Institute on Drug Abuse grants K23 DA039327, T32 DA019426, and L30 DA038349.
REFERENCES
- Albarracin D, Johnson BT, Fishbein M, & Muellerleile PA (2001). Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin, 127, 142–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- Aral SO, & Leichliter JS (2010). Non-monogamy: Risk factor for STI transmission and acquisition and determinant of STI spread in populations. Sexually Transmitted Infections, 86, 29–36. [DOI] [PubMed] [Google Scholar]
- Artime TM, & Peterson ZD (2012). The relationships among childhood maltreatment, emotion regulation, and sexual risk taking in men from urban STD clinics. Journal of Aggression, Maltreatment & Trauma, 21, 277–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Batten SV, Follette VM, & Aban IB (2002). Experiential avoidance and high-risk sexual behavior in survivors of child sexual abuse. Journal of Child Sexual Abuse, 10, 101–120. [DOI] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, … Hill E (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46, 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek D, Klauminzer G, Charney DS, & Keane TM (1990). The Clinician Administered PTSD Scale Boston, MA: National Center for PTSD-Behavioral Science Division. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P (1998). Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry, 55, 626–632. [DOI] [PubMed] [Google Scholar]
- Briere JN, & Elliott DM (1994). Immediate and long-term impacts of child sexual abuse. The Future of Children, 4, 54–69. [PubMed] [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, & Saunders BE (2006). Taxometric investigation of PTSD: Data from two nationally representative samples. Behavior Therapy, 37, 364–380. [DOI] [PubMed] [Google Scholar]
- Brown TA (2006). Confirmatory factor analysis for applied research New York: Guilford Press. [Google Scholar]
- Cavanaugh CE, Hansen NB, & Sullivan TP (2010). HIV sexual risk behavior among low-income women experiencing intimate partner violence: The role of posttraumatic stress disorder. AIDS and Behavior, 14, 318–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy, 44, 371–394. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, & Breslau N (1998). Investigations of causal pathways between PTSD and drug use disorders. Addictive Behaviors, 23, 827–840. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, & Han H (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70, 1067–1074. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Shapiro CM, & Powers AM (1998). Motivations for sex and risky sexual behavior among adolescents and young adults: A functional perspective. Journal of Personality and Social Psychology, 75, 1528–1558. [DOI] [PubMed] [Google Scholar]
- Crepaz N, & Marks G (2001). Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology, 20, 291–299. [DOI] [PubMed] [Google Scholar]
- Crockett LJ, Raffaelli M, & Shen Y (2006). Linking self‐regulation and risk proneness to risky sexual behavior: Pathways through peer pressure and early substance use. Journal of Research on Adolescence, 16, 503–525. [Google Scholar]
- Cyders MA, & Smith GT (2008). Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin, 134, 807–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckman T, & DeWall CN (2011). Negative urgency and risky sexual behaviors: A clarification of the relationship between impulsivity and risky sexual behavior. Personality and Individual Differences, 51, 674–678. [Google Scholar]
- DeLongis A, Coyne JC, Dakof G, Folkman S, & Lazarus RS (1982). Relationship of daily hassles, uplifts, and major life events to health status. Health Psychology, 1, 119–136. [Google Scholar]
- Efron B (1987). Better bootstrap confidence intervals. Journal of the American Statistical Association, 82, 171–185. [Google Scholar]
- Ehring T, & Quack D (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41, 587–598. [DOI] [PubMed] [Google Scholar]
- Felner RD, Farber SS, & Primavera J (1983). Transitions and stressful life events: A model for primary prevention New York: Plenum Press. [Google Scholar]
- Felner RD, Rowlinson RI, & Terre L (1986). Unraveling the Gordian knot in life change inquiry: A critical examination of crisis, stress and transitional frameworks of prevention Washington, DC: Hemisphere. [Google Scholar]
- Fenton KA, Johnson AM, McManus S, & Erens B (2001). Measuring sexual behaviour: Methodological challenges in survey research. Sexually Transmitted Infections, 77, 84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipas HH, & Ullman SE (2006). Child sexual abuse, coping responses, self-blame, posttraumatic stress disorder, and adult sexual revictimization. Journal of Interpersonal Violence, 21, 652–672. [DOI] [PubMed] [Google Scholar]
- Forbes D, Haslam N, Williams BJ, & Creamer M (2005). Testing the latent structure of posttraumatic stress disorder: A taxometric study of combat veterans. Journal of Traumatic Stress, 18, 647–656. [DOI] [PubMed] [Google Scholar]
- Fortenberry JD, Temkit M, Tu W, Katz BP, & Orr DP (2003). Mood, mood change, sexual activity and condom use among adolescent women. Journal of Adolescent Health, 32, 157. [Google Scholar]
- Gebhardt WA, Kuyper L, & Greunsven G (2003). Need for intimacy in relationships and motives for sex as determinants of adolescent condom use. Journal of Adolescent Health, 33, 154–164. [DOI] [PubMed] [Google Scholar]
- Gore-Felton C, & Koopman C (2002). Traumatic experiences: Harbinger of risk behavior among HIV-positive adults. Journal of Trauma & Dissociation, 3, 121–135. [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, & Lejuez CW (2007). A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy, 38, 256–268. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Dixon LJ, Kiel EJ, & Tull MT (in press). Emotion regulation: Theoretical models, associated outcomes, and recent advances London, UK: Sage Publications [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, & Gunderson JG (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology, 115, 850–855. [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Tull MT (2010). Emotion regulation as a mechanism of change in acceptance-and mindfulness-based treatments. In Baer RA (Ed.), Assessing mindfulness and acceptance: Illuminating the theory and practice of change (pp. 105–133). Oakland, CA: New Harbinger Publications. [Google Scholar]
- Gratz KL, & Tull MT (2011). Extending research on the utility of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Personality Disorders: Theory, Research, and Treatment, 2, 316–326. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, & Levy R (2014). Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine, 44, 2099–2112. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Matusiewicz AM, Breetz AA, & Lejuez CW (2013). Multimodal examination of emotion regulation difficulties as a function of co-occurring avoidant personality disorder among women with borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 4, 304–314. [DOI] [PubMed] [Google Scholar]
- Gravetter F, & Wallnau L (2014). Essentials of statistics for the behavioral sciences (8th ed.). Belmont, CA: Wadsworth. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the Life Events Checklist. Assessment, 11, 330–341. [DOI] [PubMed] [Google Scholar]
- Grubaugh AL, Elhai JD, Cusack KJ, Wells C, & Frueh BC (2007). Screening for PTSD in public‐sector mental health settings: The diagnostic utility of the PTSD checklist. Depression and Anxiety, 24, 124–129. [DOI] [PubMed] [Google Scholar]
- Guo J, Chung I, Hill KG, Hawkins JD, Catalano RF, & Abbott RD (2002). Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. Journal of Adolescent Health, 31, 354–362. [DOI] [PubMed] [Google Scholar]
- Harned MS, Korslund KE, Foa EB, & Linehan MM (2012). Treating PTSD in suicidal and self-injuring women with borderline personality disorder: Development and preliminary evaluation of a dialectical behavior therapy prolonged exposure protocol. Behaviour Research and Therapy, 50, 381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned MS, Korslund KE, & Linehan MM (2014). A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy, 55, 7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, & Strosahl K (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64, 1152–1168. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millenium. Communication Monographs, 76, 408–420. [Google Scholar]
- Holmes WC, Foa EB, & Sammel MD (2005). Men’s pathways to risky sexual behavior: Role of co-occurring childhood sexual abuse, posttraumatic stress disorder, and depression histories. Journal of Urban Health, 82, 89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton HE, Treisman GJ, Hunt WR, Fishman M, Kendig N, Swetz A, & Lyketsos CG (2001). HIV risk behaviors and their relationship to posttraumatic stress disorder among women prisoners. Psychiatric Services, 52, 508–513. [DOI] [PubMed] [Google Scholar]
- James LR, & Brett JM (1984). Mediators, moderators, and tests for mediation. Journal of Applied Psychology, 69, 307–321. [Google Scholar]
- Judd CM, & Kenny DA (1981). Process analysis: Estimating mediation in treatment evaluations. Evaluation Review, 5, 602–619. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (1995). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Archives of General Psychiatry, 52, 1048–1060.7492257 [Google Scholar]
- Kessler RC, & Frank RG (1997). The impact of psychiatric disorders on work loss days. Psychological Medicine, 27, 861–873. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Keyes KM, McLaughlin KA, Demmer RT, Cerdá M, Koenen KC, Uddin M, & Galea S (2013). Potentially traumatic events and the risk of six physical health conditions in a population-based sample. Depression and Anxiety, 30, 451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM‐ IV and DSM‐ 5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotchick BA, Shaffer A, Miller KS, & Forehand R (2001). Adolescent sexual risk behavior: A multi-system perspective. Clinical Psychology Review, 21, 493–519. [DOI] [PubMed] [Google Scholar]
- New York: Guilford Press. [Google Scholar]
- Lucenko BA, Malow RM, Sanchez-Martinez M, Jennings T, & Dévieux JG (2003). Negative affect and HIV risk in alcohol and other drug (AOD) abusing adolescent offenders. Journal of Child & Adolescent Substance Abuse, 13, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, & Lockwood CM (2000). Equivalence of the mediation, confounding, and suppression effect. Prevention Science, 1, 173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott MJ, Tull MT, Gratz KL, Daughters SB, & Lejuez CW (2009). The role of anxiety sensitivity and difficulties in emotion regulation in posttraumatic stress disorder among crack/cocaine dependent patients in residential substance abuse treatment. Journal of Anxiety Disorders, 23, 591–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Walsh KL, & DiLillo D (2010). Emotion dysregulation and risky sexual behavior in revictimization. Child Abuse & Neglect, 34, 967–976. [DOI] [PubMed] [Google Scholar]
- Morrison DM, Gillmore MR, & Baker SA (1995). Determinants of condom use among high‐risk heterosexual adults: A test of the theory of reasoned action. Journal of Applied Social Psychology, 25, 651–676. [Google Scholar]
- Orcutt HK, Cooper ML, & Garcia M (2005). Use of sexual intercourse to reduce negative affect as a prospective mediator of sexual revictimization. Journal of Traumatic Stress, 18, 729–739. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Weathers FW, Difede J, & King DW (2007). Confirmatory factor analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in disaster workers exposed to the World Trade Center Ground Zero. Journal of Abnormal Psychology, 116, 329–341. [DOI] [PubMed] [Google Scholar]
- Patel P, Borkowf CB, Brooks JT, Lasry A, Lansky A, & Mermin J (2014). Estimating per-act HIV transmission risk: A systematic review. AIDS, 28, 1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pimlott-Kubiak S, & Cortina LM (2003). Gender, victimization, and outcomes: Reconceptualizing risk. Journal of Consulting and Clinical Psychology, 71, 528–539. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Safren SA, & Mayer KH (2009). Stressful or traumatic life events, post-traumatic stress disorder (PTSD) symptoms, and HIV sexual risk taking among men who have sex with men. AIDS Care, 21, 1481–1489. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, & Becker MJ (1994). The health belief model and HIV risk behaviour change New York: Plenum Press. [Google Scholar]
- Roye CF (1998). Condom use by Hispanic and African-American adolescent girls who use hormonal contraception. Journal of Adolescent Health, 23, 205–211. [DOI] [PubMed] [Google Scholar]
- Rucker DD, Preacher KJ, Tormala ZL, & Petty RE (2011). Mediation analysis in social psychology: Current practices and new recommendations. Social and Personality Psychology Compass, 5, 359–371. [Google Scholar]
- Ruscio AM, Ruscio J, & Keane TM (2002). The latent structure of posttraumatic stress disorder: A taxometric investigation of reactions to extreme stress. Journal of Abnormal Psychology, 111, 290–301. [PubMed] [Google Scholar]
- Saltzman SP, Stoddard AM, McCusker J, & Moon MW (1987). Reliability of self-reported sexual behavior risk factors for HIV-1 infection in homosexual men. Public Health Reports, 102, 692–697. [PMC free article] [PubMed] [Google Scholar]
- Schuster RM, Crane NA, Mermelstein R, & Gonzalez R (2012). The influence of inhibitory control and episodic memory on the risky sexual behavior of young adult cannabis users. Journal of the International Neuropsychological Society, 18, 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searles JS, Perrine M, Mundt JC, & Helzer JE (1995). Self-report of drinking using touch-tone telephone: Extending the limits of reliable daily contact. Journal of Studies on Alcohol, 56, 375–382. [DOI] [PubMed] [Google Scholar]
- Senn TE, & Carey MP (2010). Child maltreatment and women’s adult sexual risk behavior: Childhood sexual abuse as a unique risk factor. Child Maltreatment, 15, 324–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipherd JC, Stafford J, & Tanner LR (2005). Predicting alcohol and drug abuse in Persian Gulf War veterans: What role do PTSD symptoms play? Addictive Behaviors, 30, 595–599. [DOI] [PubMed] [Google Scholar]
- Shrout PE, & Bolger N (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7, 422–445. [PubMed] [Google Scholar]
- Simpson TL, Galloway C, Rosenthal CF, Bush KR, McBride B, & Kivlahan DR (2011). Daily telephone monitoring compared with retrospective recall of alcohol use among patients in early recovery. American Journal on Addictions, 20, 63–68. [DOI] [PubMed] [Google Scholar]
- Spitzer C, Barnow S, Völzke H, John U, Freyberger HJ, & Grabe HJ (2009). Trauma, posttraumatic stress disorder, and physical illness: Findings from the general population. Psychosomatic Medicine, 71, 1012–1017. [DOI] [PubMed] [Google Scholar]
- Susser E, Desvarieux M, & Wittkowski KM (1998). Reporting sexual risk behavior for HIV: A practical risk index and a method for improving risk indices. American Journal of Public Health, 88, 671–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, & Roemer L (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38, 303–313. [DOI] [PubMed] [Google Scholar]
- Tull MT, Weiss NH, Adams CE, & Gratz KL (2012). The contribution of emotion regulation difficulties to risky sexual behavior within a sample of patients in residential substance abuse treatment. Addictive Behaviors, 37, 1084–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turchik JA, & Garske JP (2009). Measurement of sexual risk taking among college students. Archives of Sexual Behavior, 38, 936–948. [DOI] [PubMed] [Google Scholar]
- Turner RJ, & Lloyd DA (1995). Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior, 36, 360–376. [PubMed] [Google Scholar]
- Van der Velde FW, & Van der Pligt J (1991). AIDS-related health behavior: Coping, protection motivation, and previous behavior. Journal of Behavioral Medicine, 14, 429–451. [DOI] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, & Gatzke‐Kopp LM (2009). Correspondence between physiological and self‐report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry, 50, 1357–1364. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the International Society for Traumatic Stress Studies, San Antonio, TX [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, & Gratz KL (2013a). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Borne ME, & Gratz KL (2013b). Posttraumatic stress disorder symptom severity and HIV-risk behaviors among substance-dependent inpatients. AIDS Care, 25, 1219–1226. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Davis LT, Dehon EE, Fulton JJ, & Gratz KL (2012a). Examining the association between emotion regulation difficulties and probable posttraumatic stress disorder within a sample of African Americans. Cognitive Behaviour Therapy, 41, 5–14. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Davis LT, Searcy J, Williams I, & Gratz KL (2015a). A preliminary experimental investigation of emotion dysregulation and impulsivity in risky behaviours. Behaviour Change, 32, 127–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, & Gratz KL (2015b). Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence, 155, 147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012b). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26, 453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Williams DC, & Connolly KM (2015c). A preliminary examination of negative affect, emotion dysregulation, and risky behaviors among military veterans in residential substance abuse treatment. Military Behavioral Health, 3, 212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30, 669–689. [Google Scholar]
- Zhao X, Lynch JG, & Chen Q (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37, 197–206. [Google Scholar]


