Abstract
Background:
Opioids and stimulants (i.e., cocaine or methamphetamine/amphetamine [MAMP]) are major contributors to acute substance toxicity deaths. Causes of stimulant death have received little attention. We sought to characterize and compare causes of death and significant contributing conditions among persons who died from acute opioid, cocaine, or MAMP toxicity.
Methods:
We identified all opioid, cocaine, or MAMP deaths in San Francisco from 2005 to 2015 through the California Electronic Death Reporting System. Multivariable logistic regression analyses were used to estimate associations between acute substance toxicity deaths (opioid versus stimulant; cocaine versus MAMP), additional reported causes of death, and significant contributing conditions most often linked to opioid and stimulant use.
Results:
From 2005-2015, there were 1,252 opioid deaths and 749 stimulant deaths. Cocaine accounted for most stimulant deaths. Decedents with cardiac or cerebral hemorrhage causes of death had higher adjusted odds of death due to acute stimulant toxicity rather than acute opioid toxicity (aOR=4.79, 95%CI=2.88–7.96, p<0.01; aOR=58.58, 95%CI=21.06–162.91, p<0.01, respectively); no statistically significant associations were found for cocaine compared to MAMP deaths. Significant contributing cardiac conditions were associated with higher adjusted odds of stimulant compared to opioid (aOR=1.46, 95%CI=1.19–1.79, p<0.01) and cocaine compared to MAMP death (aOR=1.66, 95%CI=1.13–2.45, p=0.01).
Conclusions:
Stimulant compared to opioid deaths tended to involve cardiac or cerebrovascular causes of death, and cocaine deaths were more likely than MAMP deaths to involve significant contributing cardiac conditions. Mounting evidence suggests that stimulant use be considered a cardio/cerebrovascular risk factor and clinical care be adjusted to address this heightened risk.
Keywords: acute substance toxicity deaths, cocaine mortality, methamphetamine/amphetamine mortality, stimulant mortality, opioid mortality, multiple causes of death
1.0. Introduction
Drug poisoning has been the leading cause of injury-related death in the United States every year since 2009 (Paulozzi et al., 2011) and mortality from all drugs has increased from 2002–2015 (National Institute on Drug Abuse, 2017; Rudd et al., 2016). Though opioids are a major driver of the rise in all-drug mortality (Rudd et al., 2016), stimulants (e.g., cocaine or methamphetamine/amphetamine [MAMP]) are major contributors to opioid-related mortality and may, in fact, contribute to even more deaths than opioids (Coffin et al., 2003). Since 2010, the number of cocaine deaths (without opioids) increased by nine percent in the United States (National Institute on Drug Abuse, 2017). There was also an increase in psychostimulant (including MAMP) deaths from 1999–2006, followed by a decline until 2008, and then an upward shift in death from 2008 to 2015 (Calcaterra & Binswanger, 2013; Hedegaard et al., 2017).
Research suggests demographic differences between opioid and stimulant deaths. First, in New York City from 1990–2000, cocaine deaths were more likely than opioid deaths to occur among older and Black or African American persons (Bernstein et al., 2007). A study of mortality among illicit drug users in the United States found differential hazard rate ratios for all-cause mortality for heroin-only versus cocaine-only users from 1991 – 2006 (Muhuri & Gfroerer, 2011). Cocaine and opioid deaths likely represent distinct groups, highlighting the need for targeted interventions by substance of use. To our knowledge, no demographic comparisons have been made comparing MAMP to other acute substance toxicity deaths.
The well-understood pathophysiology of opioid deaths (reduced respiratory effort [Dahan et al., 2010, 2013; Oderda et al., 2013]) and that suspected in stimulant deaths (cardiac and cerebrovascular conditions) may affect distinct populations. Cocaine use is strongly associated with electrophysiological and cellular cardiac toxicity (Stankowski et al., 2015), and MAMP is known to increase heart rate and blood pressure (Huang et al., 2016; Karch, 2009; Kaye et al., 2007), likely exerting physiologic and anatomic strain on the cardiovascular system. In a national study, stimulant deaths were most common among men between the ages of 45–54 and hypertension or other cardiac causes of death were common (Calcaterra & Binswanger, 2013). Similarly, four studies of methamphetamine deaths found high prevalence of cardiovascular causes of death (Darke et al., 2017a; Darke et al., 2017b; Herbeck et al., 2015; Darke et al., 2008). Another two studies found high risk of ischemic stroke and cerebral hemorrhage among methamphetamine users (Lappin et al., 2017; Ho et al., 2009), and yet another identified elevated risk of cerebrovascular conditions among both amphetamine and cocaine users (Westover et al., 2007).
Given these differences, and the limited literature comparing the population-level distribution and co-morbidities of opioid and stimulant deaths, we compared clinical conditions (i.e., cause of death and significant contributing conditions) of all opioid, cocaine, and MAMP deaths in San Francisco from 2005 – 2015. We specifically examined whether stimulant deaths were more likely than opioid deaths to involve cardiac and cerebrovascular causes of death and significant contributing conditions, and whether these differences persisted for cocaine compared to MAMP deaths.
2.0. Materials and methods
2.1. Opioid and stimulant death classification
Demographic data, substances involved in death, and clinical conditions (e.g., causes of death and significant contributing conditions) were abstracted from the California Electronic Death Reporting System (CA-EDRS) to create a database of all acute substance toxicity deaths occurring within the City and County of San Francisco between January 1, 2005 and December 31, 2015. The process by which acute substance toxicity deaths were classified was described in detail elsewhere (Visconti et al., 2015). Briefly, the San Francisco Office of the Chief Medical Examiner’s (OCME) Forensic Laboratory Division performed toxicological screenings and confirmatory assessments of blood and urine specimens to identify substances that were causes or significant contributors of death. For the purposes of this study, “acute substance toxicity deaths” comprised cases with causes of death listed as acute toxicity from substances (e.g., morphine, oxycodone, cocaine, methamphetamine, amphetamine, etc.). Cases that listed “acute [substance] toxicity” but did not specify which substances were involved underwent manual review by two physicians in consultation with the chief forensic toxicologist of the San Francisco OCME to determine substances involved. We selected cases based on review of causes of death for acute substance toxicity, rather than International Classification of Disease (ICD) codes, because the latter method has been shown to underestimate deaths where acute substance toxicity is involved (Ruhm, 2016). This study met the criteria for Human Subjects research exemption by the University of California, San Francisco Committee on Human Research (IRB #: 17–23209).
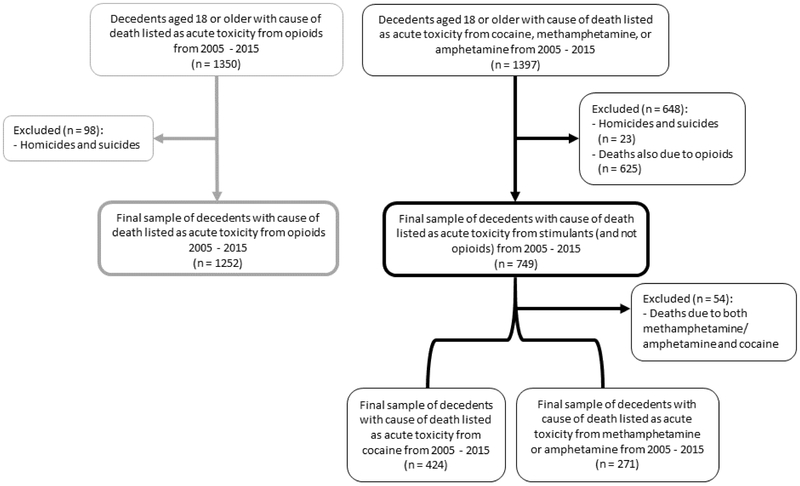
We restricted our analyses to decedents (i.e., cases who died) aged 18 and older with any acute opioid, cocaine, or MAMP toxicity listed as a cause of death and excluded cases that were non-accidental (i.e., due to homicide or suicide) (Figure 1). We defined “opioid deaths” as those with acute toxicity from prescription or non-prescription opioids (e.g., heroin, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, propoxyphene, etc.) listed as a cause of death. “Stimulant deaths” were those with acute toxicity from cocaine or MAMP as a cause of death without opioids as a cause of death. Deaths involving both stimulants and opioids were classified as opioid deaths because opioids have a clear mechanism of death and we hypothesized (and evaluated in the present study) that deaths involving both stimulants and opioids would be more mechanistically similar to opioid deaths. “Cocaine deaths” and “MAMP deaths” were those that identified acute toxicity from cocaine or methamphetamine/amphetamine as a cause of death, respectively. Throughout the present analysis, we referred to “opioid deaths” interchangeably as deaths due to “acute opioid toxicity”. This held for “stimulant deaths”, “cocaine deaths”, and “MAMP deaths.”
Figure 1.
Sample restriction in the analysis of opioid and stimulant deaths, San Francisco, 2005 - 2015 (n = 2,001)
2.2. Coding causes of death and significant contributing conditions
For the purposes of this study, “cause of death” was defined as the clinical condition(s) or events that directly lead to death according to the medical examiner determination. “Significant contributing conditions” were those that contributed to, but did not directly lead to death. Data abstracted from the CA-EDRS comprised multiple causes of death. For example, decedents with acute opioid toxicity listed as a cause of death could also have cerebral hemorrhage listed as a cause of death. For all deaths due to acute substance toxicity, we first enumerated all causes of death and significant contributing conditions. The study physician then categorized each result based on organ system or significant disease category (see Appendix Tables 1a, 1b, and 2 for the list of disease categories) and trained staff members in coding each case. To more concisely display descriptive results, causes of death and significant contributing conditions that could not be meaningfully grouped were categorized as “Other” (Tables 1 and 2). Though a large proportion of significant contributing conditions were categorized as “Other”, quantitative findings were not influenced since we did not include the “Other” disease category in bivariable or multivariable analyses. Study staff consulted the study physician for a final decision when coding was unclear for any case. Once study staff completed the clinical coding, the study physician reviewed a random sample of 15% of decedents for quality control purposes. If less than a 95% coding match was reached between the study staff and physician, then the differences were reconciled by the study team and updates were applied to the rest of the dataset (i.e., if the same cause of death discrepancy was present in other cases that were not reviewed by the physician, then those cases were updated by study staff as well). Randomly-selected samples of 15% of the remaining cases were repeatedly sent to the study physician until over 95% match was reached.
Table 1.
Demographic and clinical characteristics of stimulant and opioid deaths in San Francisco, 2005 - 2015 (n = 2001)
| Overall | Stimulant deaths† | Opioid deaths†† | Bivariable results | |||||
|---|---|---|---|---|---|---|---|---|
| N (%)‡ or M (SD) | N (%)δ or M (SD) | N (%)δ or M (SD) | Test statistic | P-value | ||||
| Total | 2001 | (100.00) | 749 | (37.43)‡ | 1252 | (62.57)‡ | ||
| Demographic characteristics* | ||||||||
| Age | 48.84 | (12.06) | 50.22 | (11.14) | 48.01 | (12.50) | t = 3.99 | p < 0.01 |
| Sex | χ2 = 17.30 | p < 0.01 | ||||||
| Male | 1470 | (73.46) | 590 | (78.77) | 880 | (70.29) | ||
| Female | 531 | (26.54) | 159 | (21.23) | 372 | (29.71) | ||
| Race/ethnicity | χ2 = 103.98 | p < 0.01 | ||||||
| White | 1089 | (54.42) | 306 | (40.85) | 783 | (62.54) | ||
| Black/African American | 552 | (27.59) | 281 | (37.52) | 271 | (21.65) | ||
| Hispanic/Latino(a) | 216 | (10.79) | 89 | (11.88) | 127 | (10.14) | ||
| Asian/Pacific Islander | 80 | (4.00) | 49 | (6.54) | 31 | (2.48) | ||
| Other/Mixed¶ | 64 | (3.20) | 24 | (3.20) | 40 | (3.19) | ||
| Death Year | χ2 = 28.07 | p < 0.01 | ||||||
| 2005 - 2007 | 517 | (25.84) | 223 | (29.77) | 294 | (23.48) | ||
| 2008 - 2010 | 522 | (26.09) | 153 | (20.43) | 369 | (29.47) | ||
| 2011 - 2013 | 568 | (28.39) | 203 | (27.10) | 365 | (29.15) | ||
| 2014 - 2015 | 394 | (19.69) | 170 | (22.70) | 224 | (17.89) | ||
| Death also due to alcohol†††* | χ2 = 25.96 | p < 0.01 | ||||||
| No | 1679 | (83.91) | 669 | (89.32) | 1010 | (80.67) | ||
| Yes | 322 | (16.09) | 80 | (10.68) | 242 | (19.33) | ||
| Cause of death | ||||||||
| Cardiac ~* | 83 | (4.15) | 59 | (7.88) | 24 | (1.92) | χ2 = 41.87 | p < 0.01 |
| Cerebral hemorrhage* | 102 | (5.10) | 98 | (13.08) | 4 | (0.32) | Fisher's exact | p < 0.01 |
| Neurologic or psychiatric | 5 | (0.25) | 3 | (0.40) | 2 | (0.16) | ||
| Infection | 23 | (1.15) | 9 | (1.20) | 14 | (1.12) | ||
| Trauma | 12 | (0.60) | 5 | (0.67) | 7 | (0.56) | ||
| Malignancy | 7 | (0.35) | 2 | (0.27) | 5 | (0.40) | ||
| Overdose Complication | 32 | (1.60) | 13 | (1.74) | 19 | (1.52) | ||
| Other | 42 | (2.10) | 18 | (2.40) | 24 | (1.92) | ||
| Significant contributing condition | ||||||||
| Cardiac ~* | 581 | (29.04) | 252 | (33.64) | 329 | (26.28) | χ2 = 12.34 | p < 0.01 |
| Cerebral hemorrhage | 6 | (0.30) | 2 | (0.27) | 4 | (0.32) | ||
| Neurologic or psychiatric | 30 | (1.50) | 10 | (1.34) | 20 | (1.60) | ||
| Infection | 83 | (4.15) | 24 | (3.20) | 59 | (4.71) | ||
| Trauma | 12 | (0.60) | 5 | (0.67) | 7 | (0.56) | ||
| Malignancy | 26 | (1.30) | 10 | (1.34) | 16 | (1.28) | ||
| Overdose complication | 1 | (0.05) | 0 | 0.00 | 1 | (0.08) | ||
| Other | 397 | (19.84) | 151 | (20.16) | 246 | (19.65) | ||
| Chronic infections | ||||||||
| HIV | 87 | (4.35) | 41 | (5.47) | 46 | (3.67) | ||
| HCV | 135 | (6.75) | 44 | (5.87) | 91 | (7.27) | ||
Causes of death and significant contributing conditions are not mutually exclusive. Except for 6/2001 (0.30%) cases with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or cocaine; excludes decedents with cause of death listed as acute toxicity from opioids.
Includes decedents with cause of death listed as acute toxicity from heroin, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, propoxyphene, and other opioids.
Percentages calculated out of a total of 2001 opioid or stimulant deaths from 2005-2015.
Percentages calculated out of the total deaths for that substance group (749 for stimulant deaths; 1252 for opioid deaths).
Included in bivariable analyses comparing stimulant and opioid deaths.
Includes American Indian/Alaska Native (n = 15), Other/Mixed (n = 43), and Unknown (n = 6) race/ethnicities.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Includes electrical conduction, aortic, pericardial, hypertension, atherosclerotic or myocardial infarction, congestive heart failure or cardiomyopathy clinical conditions; refer to Appendix Table 1a for detailed coding of cardiac and other clinical conditions.
Table 2.
Demographic and clinical characteristics of cocaine and methamphetamine/amphetamine (MAMP) deaths in San Francisco, 2005 - 2015 (n = 695)
| Cocaine deaths† | MAMP deaths†† | Bivariable results | ||||||
|---|---|---|---|---|---|---|---|---|
| N (%)δ or M (SD) | N (%)δ or M (SD) | Test statistic | P-value | |||||
| Total | 424 | (61.01)‡ | 271 | (38.99)‡ | ||||
| Demographic characteristics* | ||||||||
| Age | 52.40 | (10.53) | 47.47 | (11.13) | t = 5.89 | p < 0.01 | ||
| Sex | χ2 = 3.86 | p = 0.05 | ||||||
| Male | 324 | (76.42) | 224 | (82.66) | ||||
| Female | 100 | (23.58) | 47 | (17.34) | ||||
| Race/ethnicity | Fisher's exact | p < 0.01 | ||||||
| White | 120 | (28.30) | 166 | (61.25) | ||||
| Black/African American | 228 | (53.77) | 29 | (10.70) | ||||
| Hispanic/Latino(a) | 47 | (11.08) | 37 | (13.65) | ||||
| Asian/Pacific Islander | 17 | (4.01) | 30 | (11.07) | ||||
| Other/Mixed¶ | 12 | (2.83) | 9 | (3.32) | ||||
| Death Year | χ2 = 22.41 | p < 0.01 | ||||||
| 2005 - 2007 | 140 | (33.02) | 58 | (21.40) | ||||
| 2008 - 2010 | 98 | (23.11) | 51 | (18.82) | ||||
| 2011 - 2013 | 112 | (26.42) | 79 | (29.15) | ||||
| 2014 - 2015 | 74 | (17.45) | 83 | (30.63) | ||||
| Death also due to alcohol†††* | χ2 = 23.27 | p < 0.01 | ||||||
| No | 359 | (84.67) | 261 | (96.31) | ||||
| Yes | 65 | (15.33) | 10 | (3.69) | ||||
| Cause of death | ||||||||
| Cardiac ~* | 43 | (10.14) | 15 | (5.54) | χ2 = 4.59 | p = 0.03 | ||
| Cerebral hemorrhage* | 50 | (11.79) | 41 | (15.13) | χ2 = 1.62 | p = 0.20 | ||
| Neurologic or psychiatric | 2 | (0.47) | 1 | (0.37) | ||||
| Infection | 4 | (0.94) | 5 | (1.85) | ||||
| Trauma | 3 | (0.71) | 2 | (0.74) | ||||
| Malignancy | 2 | (0.47) | 0 | 0.00 | ||||
| Overdose complication | 12 | (2.83) | 1 | (0.37) | ||||
| Other | 7 | (1.65) | 9 | (3.32) | ||||
| Significant contributing condition | ||||||||
| Cardiac ~* | 162 | (38.21) | 78 | (28.78) | χ2 = 6.50 | p = 0.01 | ||
| Cerebral hemorrhage | 1 | (0.24) | 1 | (0.37) | ||||
| Neurologic or psychiatric | 6 | (1.42) | 2 | (0.74) | ||||
| Infection | 15 | (3.54) | 7 | (2.58) | ||||
| Trauma | 3 | (0.71) | 2 | (0.74) | ||||
| Malignancy | 8 | (1.89) | 2 | (0.74) | ||||
| Overdose Complication | 0 | 0.00 | 0 | 0.00 | ||||
| Other | 105 | (24.76) | 34 | (12.55) | ||||
| Chronic infections | ||||||||
| HIV | 20 | (4.72) | 20 | (7.38) | ||||
| HCV | 22 | (5.19) | 19 | (7.01) | ||||
Causes of death and significant contributing conditions are not mutually exclusive. Except for 4/695 (0.56%) cocaine or MAMP deaths with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from cocaine; excludes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or opioids.
Includes decedents with cause of death listed as acute toxicity from methamphetamine or amphetamine; excludes decedents with cause of death listed as acute toxicity from cocaine or opioids.
Percentages calculated out of a total of 695 cocaine or MAMP deaths from 2005-2015.
Percentages calculated out of the total deaths for that substance group (424 for cocaine deaths; 271 for MAMP deaths).
Included in bivariable analyses comparing cocaine and MAMP deaths.
Includes American Indian/Alaska Native (n = 3), Other/Mixed (n = 14), and Unknown (n = 4) race/ethnicities.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Includes electrical conduction, aortic, pericardial, hypertension, atherosclerotic or myocardial infarction, congestive heart failure or cardiomyopathy clinical conditions; refer to Appendix Table 2 for detailed coding of cardiac and other clinical conditions.
Cardiac significant contributing conditions were ascribed to decedents with a cause of death or significant contributing condition listed as cardiac-related, since a medical examiner that coded a cause of death as due to a cardiac condition, such as coronary artery disease, generally did not also list that condition under significant contributing conditions.
2.3. Statistical Analyses
Decedent race/ethnicity, sex, and age were included in bivariable analyses (chi-square test, t-test, or Fisher’s exact test for small counts) to assess demographic differences for stimulant compared to opioid deaths and cocaine compared to MAMP deaths. We also adjusted for these variables in multivariable analyses given the disparities in acute substance toxicity deaths observed for these demographic groups (Rudd et al., 2016; Bernstein et al., 2007; Muhuri & Gfroerer, 2011). Race/ethnicity was coded according to Office of Management and Budget (OMB) standards (1997) and was collapsed further (Non-Hispanic/Latino[a] White, Black/African American, Asian/Pacific Islander, Other/Mixed, or Hispanic/Latino[a]) for bivariable and multivariable analyses due to small cell sizes. We additionally adjusted for acute alcohol toxicity (e.g., whether or not acute alcohol toxicity was also listed as a cause of death) given its implications for comorbid substance use and mortality (Coffin et al., 2003), and death year as a proxy for trends in acute substance toxicity deaths. Due to skewedness, death years were collapsed into two- or three-year intervals (see Tables 1–4). Except for six cases with unknown race/ethnicity (which were included in the “Other/Mixed” racial/ethnic group), no data were missing.
Table 4.
Multivariable comparison of demographic and select clinical characteristics for cocaine compared to methamphetamine/amphetamine (MAMP) deaths in San Francisco, 2005 - 2015 (n = 695)
| MV4: Adjusted odds of cocaine† compared to MAMP†† death for those with cardiac causes of death |
MV5: Adjusted odds of cocaine† compared to MAMP†† death for those with cerebral hemorrhagic causes of death |
MV6: Adjusted odds of cocaine† compared to MAMP†† death for those with cardiac significant conditions |
||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Demographic characteristics | ||||||
| Age | 1.05 | 1.03 - 1.06** | 1.05 | 1.03 - 1.07** | 1.04 | 1.02 - 1.06** |
| Sex | ||||||
| Male | 1.00 | 1.00 | 1.00 | |||
| Female | 1.25 | 0.78 - 1.99 | 1.31 | 0.81 - 2.11 | 1.25 | 0.78 - 2.00 |
| Race/ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Black/African American | 11.37 | 7.05 - 18.33** | 11.22 | 6.96 - 18.10** | 11.31 | 7.00 - 18.28** |
| Hispanic/Latino(a) | 2.16 | 1.24 - 3.78** | 2.23 | 1.28 - 3.88** | 2.25 | 1.29 - 3.93** |
| Asian/Pacific Islander | 1.32 | 0.67 - 2.58 | 1.33 | 0.68 - 2.61 | 1.28 | 0.65 - 2.51 |
| Other/Mixed | 2.18 | 0.80 - 5.95 | 2.18 | 0.80 - 5.94 | 2.00 | 0.74 - 5.41 |
| Death Year | ||||||
| 2005 - 2007 | 1.00 | 1.00 | 1.00 | |||
| 2008 - 2010 | 0.65 | 0.38 - 1.12 | 0.68 | 0.40 - 1.16 | 0.65 | 0.38 - 1.11 |
| 2011 - 2013 | 0.45 | 0.27 - 0.75** | 0.45 | 0.27 - 0.74** | 0.43 | 0.26 - 0.71** |
| 2014 - 2015 | 0.26 | 0.15 - 0.44** | 0.25 | 0.15 - 0.42** | 0.24 | 0.14 - 0.41** |
| Death also due to alcohol††† | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 7.69 | 3.62 - 16.31** | 7.39 | 3.47 - 15.73** | 8.12 | 3.81 - 17.28** |
| Cause of death | ||||||
| Cardiac δ | 1.80 | 0.89 - 3.63 | – | – | ||
| Cerebral hemorrhage | – | 0.83 | 0.48 - 1.42 | – | ||
| Significant contributing condition | ||||||
| Cardiac δ‡ | – | – | 1.66 | 1.13 - 2.45* | ||
MV: multivariable model. aOR: adjusted odds ratio. CI: confidence interval. Odds ratios compare cocaine to MAMP deaths. Except for 4/695 (0.56%) cocaine or MAMP deaths with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from cocaine; excludes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or opioids.
Includes decedents with cause of death listed as acute toxicity from methamphetamine or amphetamine; excludes decedents with cause of death listed as acute toxicity from cocaine or opioids.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Includes electrical conduction, aortic, pericardial, hypertension, atherosclerotic or myocardial infarction, congestive heart failure or cardiomyopathy clinical conditions.
Composite variable: cardiac cause of death or significant contributing condition.
p < 0.05.
p < 0.01.
We conducted multivariable logistic regression analyses to test the associations between (1) cerebral hemorrhage cause of death and whether the deaths were (a) opioid deaths versus stimulant deaths and (b) cocaine deaths versus MAMP deaths; (2) cardiac causes of death and whether the deaths were (a) opioid deaths versus stimulant deaths and (b) cocaine deaths versus MAMP deaths; and (3) significant contributing cardiac conditions and whether the deaths were (a) opioid deaths versus stimulant deaths and (b) cocaine deaths versus MAMP deaths.
Finally, we conducted a sensitivity analysis to assess whether multivariable findings qualitatively changed when we re-defined the opioid deaths to exclude deaths also due to acute stimulant toxicity (n = 631).
All statistical analyses were conducted in Stata 14 (StataCorp, 2015). This study was reported in accordance with STROBE guidelines (von Elm et al., 2008).
3.0. Results
3.1. Sample Characteristics
We identified 2,001 opioid or stimulant deaths in the City and County of San Francisco from 2005–2015 (Figure 1). Of those, most were opioid deaths and over a third were stimulant deaths without opioids (Table 1). The majority of stimulant deaths were due to acute cocaine toxicity compared to acute MAMP toxicity; fifty-four involved both cocaine and MAMP. The mean age of all decedents in the sample was 49 years and most were white and male (Table 1); this pattern was similar for opioid (Table 1) and MAMP deaths (Table 2). Those who died from acute cocaine toxicity tended to be older (p<0.01) and most were Black or African American (p<0.01) (Table 2). Opioid compared to stimulant deaths and cocaine compared to MAMP deaths were more likely to also be due to acute alcohol toxicity (p < 0.01 for both comparisons) (Table 1 and Table 2).
With regard to causes of death and significant contributing conditions, a 95% match or higher for the quality control check between study staff and the study physician was achieved after the second round of review. Cardiac conditions and cerebral hemorrhage were the most frequently reported causes of death for the overall sample (Table 1). While 1.9% and 0.3% of opioid deaths were also caused by cardiac conditions or cerebral hemorrhage (Table 1), respectively, those proportions were 10.1% and 11.8% for cocaine deaths and 5.5% and 15.1% for MAMP deaths (Table 2). Distributions of other clinical causes of death and significant contributing conditions for opioid compared to stimulant deaths and cocaine compared to MAMP deaths were similar (see Tables 1 and 2, respectively).
3.2. Multivariable Analyses
Cardiac causes of death were associated with significantly greater odds of stimulant compared to opioid death (adjusted odds ratio, aOR=4.79, 95%CI=2.88–7.96, p<0.01), adjusting for age, sex, race/ethnicity, acute alcohol toxicity, and year of death. Similarly, cardiac significant contributing conditions were associated with significantly higher adjusted odds of stimulant compared to opioid death (aOR=1.46, 95%CI=1.19–1.79, p<0.01). Cerebral hemorrhage cause of death was also associated with higher adjusted odds of stimulant versus opioid death (aOR=58.58, 95%CI=21.06–162.91, p<0.01) (Table 3).
Table 3.
Multivariable comparison of demographic and select clinical characteristics for stimulant compared to opioid deaths in San Francisco, 2005 - 2015 (n = 2001)
| MV1: Adjusted odds of stimulant† compared to opioid†† death for those with cardiac causes of death |
MV2: Adjusted odds of stimulant† compared to opioid†† death for those with cerebral hemorrhagic causes of death |
MV3: Adjusted odds of stimulant† compared to opioid†† death for those with cardiac significant conditions |
||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Demographic characteristics | ||||||
| Age | 1.01 | 1.00 - 1.02* | 1.01 | 1.00 - 1.02* | 1.01 | 1.00 - 1.02 |
| Sex | ||||||
| Male | 1.00 | 1.00 | 1.00 | |||
| Female | 0.57 | 0.46 - 0.72** | 0.46 | 0.36 - 0.58** | 0.58 | 0.46 - 0.72** |
| Race/ethnicity | ||||||
| White | 1.00 | 1.00 | 1.00 | |||
| Black/African American | 2.60 | 2.07 - 3.26** | 2.74 | 2.17 - 3.46** | 2.57 | 2.06 - 3.22** |
| Hispanic/Latino(a) | 1.83 | 1.33 - 2.50** | 1.81 | 1.31 - 2.51** | 1.88 | 1.38 - 2.57** |
| Asian/Pacific Islander | 3.53 | 2.17 - 5.73** | 3.66 | 2.23 - 6.02** | 3.65 | 2.26 - 5.90** |
| Other/Mixed | 1.66 | 0.97 - 2.86 | 1.57 | 0.89 - 2.77 | 1.62 | 0.94 - 2.78 |
| Death Year | ||||||
| 2005 - 2007 | 1.00 | 1.00 | 1.00 | |||
| 2008 - 2010 | 0.51 | 0.39 - 0.67** | 0.56 | 0.42 - 0.74** | 0.55 | 0.42 - 0.72** |
| 2011 - 2013 | 0.75 | 0.58 - 0.97* | 0.77 | 0.59 - 1.01 | 0.72 | 0.56 - 0.93* |
| 2014 - 2015 | 1.01 | 0.76 - 1.34 | 1.01 | 0.76 - 1.35 | 0.94 | 0.71 - 1.25 |
| Death also due to alcohol††† | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 0.53 | 0.40 - 0.70** | 0.58 | 0.43 - 0.77** | 0.53 | 0.40 - 0.70** |
| Cause of death | ||||||
| Cardiac δ | 4.79 | 2.88 - 7.96** | – | – | ||
| Cerebral hemorrhage | – | 58.58 | 21.06 - 162.91** | – | ||
| Significant contributing condition | ||||||
| Cardiac δ‡ | – | – | 1.46 | 1.19 - 1.79** | ||
MV: multivariable model. aOR: adjusted odds ratio. CI: confidence interval. Odds ratios compare stimulant to opioid deaths. Except for 6/2001 (0.30%) cases with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or cocaine; excludes decedents with cause of death listed as acute toxicity from opioids.
Includes decedents with cause of death listed as acute toxicity from heroin, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, propoxyphene, and other opioids.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Includes electrical conduction, aortic, pericardial, hypertension, atherosclerotic or myocardial infarction, congestive heart failure or cardiomyopathy clinical conditions.
Composite variable: cardiac cause of death or significant contributing condition.
p < 0.05.
p < 0.01.
There was no statistically significant adjusted association between cardiac or cerebral hemorrhage causes of death when comparing cocaine to MAMP deaths. However, adjusting for age, sex, race/ethnicity, acute alcohol toxicity, and year of death, cardiac significant contributing conditions were associated with higher odds of cocaine compared to MAMP death (aOR=1.66, 95%CI=1.13–2.45, p=0.01) (Table 4).
The sensitivity analysis that re-defined opioid deaths to exclude deaths also due to acute stimulant toxicity produced one qualitative difference. The association between cardiac significant contributing conditions was not statistically significant for stimulant compared to opioid (excluding stimulant) deaths (aOR=1.18, 95%CI=0.92–1.52, p=0.19). To better understand this finding, we explored demographic and clinical characteristics among opioid-only, opioid-plus-stimulant, and stimulant-only deaths and found a lower prevalence of cardiac significant contributing conditions for opioid-plus-stimulant deaths (p<0.01), which may explain the discrepancy in findings between opioid-plus-stimulant and opioid-only deaths (Appendix Table 1b).
4.0. Discussion
We found that decedents with cardiac conditions or cerebral hemorrhage listed as a cause of death had higher odds of death due to acute toxicity from stimulants (cocaine or MAMP) compared to opioids. Cardiac significant contributing conditions were also associated with higher odds of stimulant compared to opioid death, and cocaine compared to MAMP death. Differences in clinical conditions remained after adjusting for age, sex, race/ethnicity, death year, and acute alcohol toxicity. While we cannot infer causality based on these associations, the known toxicities of stimulants suggest that use of cocaine and MAMP either contributed to or directly caused the acute cardiac and cerebrovascular diseases resulting in death, emphasizing the need to proactively address cardiac and cerebrovascular risk among persons who use stimulants.
Consistencies and discrepancies exist between substance use and clinical characteristics from the present study compared to other studies of drug-related mortality. As suspected, cerebral hemorrhage causes of death, cardiac causes of death, and cardiac significant contributing conditions were the most prevalent clinical conditions among all decedents in the sample. In a study of deaths due to opioid and cocaine toxicity, a similar prevalence of cardiac conditions was detected among opioid deaths and cardiac and cerebrovascular pathology was higher among cocaine compared to opioid deaths (Darke et al., 2006). However, no comparisons were made to MAMP deaths. Prevalence of cardiac causes of death were higher among MAMP deaths in an Australian sample (Darke et al., 2017b) than MAMP deaths in the present study, possibly because our analyses focused on death record data rather than pathological findings from full autopsy reports. Even so, our analyses detected statistically significant differences in the odds of cardiac causes of death for stimulant versus opioid deaths. A review of postmortem case series found that between 1% to 5% of methamphetamine deaths among those less than 44 years of age were also due to cerebral hemorrhage (Lappin et al., 2017). We found a 15% prevalence of MAMP deaths with cerebral hemorrhage also listed as a cause of death, which may be explained by the wider age range of our sample. The study by Lappin and colleagues (2017) also suggested that methamphetamine, with a longer half-life than cocaine (Karch et al., 2009), would more often subject its users to hypertension and produce increased risk of cerebrovascular events (Petitti et al., 1998; Westover et al., 2007; Huang et al., 2016). While the prevalence of cerebral hemorrhage was higher for MAMP compared to cocaine deaths in the present study, there were no statistically significant differences in multivariable analyses. Although this study could be underpowered to detect a difference, or the substance use histories of decedents could be more complex than our death record data allow us to assess, these data are consistent with another study finding similar rates of cerebrovascular hemorrhage among cocaine and amphetamine users (Westover et al., 2007).
The present study confirms the demographic disparities in acute substance toxicity deaths (Bernstein et al., 2007). While a majority of the 2,001 decedents were White and non-Hispanic, cocaine death disproportionately burdened those who were non-Hispanic Black/African American. Only 6.1% of San Francisco’s population is composed of Black or African American persons (United States Census Bureau, 2010), yet we found that they make up almost a quarter of opioid deaths and over half of cocaine deaths in San Francisco from 2005–2015. To our knowledge, this is one of few studies to examine racial/ethnic characteristics of MAMP deaths, precluding comparisons to other samples. In terms of age, MAMP deaths averaged 47.5 years in the sample, compared to 36.9 years in another study of MAMP deaths in Australia (Darke et al., 2017b). In a national sample of psychostimulant deaths, the highest death rates occurred among those who were 35–54 years of age (Calcaterra & Binswanger, 2013). We found that MAMP deaths were younger than cocaine deaths in this sample, supporting previous observations that cocaine deaths represent a relatively older group (Bernstein et al., 2007). Similar to other studies of cocaine, opioid, or MAMP deaths, we found that a majority of decedents in this sample were male (Bernstein et al., 2007; Calcaterra & Binswanger, 2013; Darke et al., 2017a; Darke et al., 2017b).
This analysis also adds to prior evidence of the cardiac and cerebrovascular implications of cocaine (Stankowski, 2015; Westover, 2007) and MAMP (Lappin et al., 2017; Darke et al., 2017a; Darke et al., 2017b; Calcaterra & Binswanger, 2013; Herbeck et al., 2015; Darke et al., 2008; Ho et al., 2009; Westover, 2007). Notwithstanding the elevated risk for cardiac conditions among opioid users, cardiac conditions and causes of death were significantly more common with stimulant deaths, supporting the call for stimulant use to be considered as a cardiac risk factor (Riley et al., 2017). Stimulant use is not currently considered a cardiac or cerebrovascular risk factor in the professional guidelines that drive medical care (National Center for Chronic Disease Prevention and Health Promotion, 2015; American Heart Association, 2016). Incorporation of stimulant use routinely as a cardiac risk factor could lead to more aggressive blood pressure and cholesterol management, as well as smoking cessation, among patients who use stimulants, conceivably reducing related mortality.
Our analysis has several limitations. First, we relied upon medical examiner determinations for causes of death and significant contributing conditions. Given that drug testing at autopsy is at the discretion of the medical examiner, it is possible that some San Francisco overdose deaths were missed due to a failure to test. It is also conceivable that interpretation of drug testing results was based at least in part on assumptions about substance use prevalence among sub-populations and the known toxicities of selected substances. Furthermore, the cross-sectional nature of the data does not allow us to establish the substance use history of decedents, such that the etiology of a compromised organ system may have been unrelated to the substance used at the time of death. However, in a study examining substance mortality data from 1999 – 2009, it was shown that death patterns mirrored use patterns for amphetamine users (Calcaterra & Binswanger, 2013); this may have held for our sample as well. In addition, our results may not be generalizable beyond San Francisco, especially to rural settings or other regions where substance use patterns may be different. Small sample size presented another limitation in some of our subgroup analyses. The small number of opioid deaths due to cerebral hemorrhage produced imprecise confidence intervals; however, the magnitude of the effect we observed was still large. And finally, due to the small number of American Indian/Alaska Native-identified decedents, we had limited precision in detecting the disparity of amphetamine death observed among this group in a previous study (Calcaterra & Binswanger, 2013).
5.0. Conclusions
Stimulant compared to opioid deaths tended to involve cardiac or cerebrovascular causes of death, and cocaine deaths were more likely than MAMP deaths to involve significant contributing cardiac conditions. The present analysis adds evidence that those whose cause of death was acute stimulant toxicity represent a demographically and clinically distinct population from those whose cause of death was acute opioid toxicity, requiring more targeted intervention efforts. Findings suggest that emphasis be placed on prevention of cardiac and cerebrovascular conditions among stimulant users in primary care.
Acknowledgments
Funding: This work was supported by National Institutes of Health, National Institute on Drug Abuse [grant number K24DA042720]
Appendix Table 1a. Demographic and detailed clinical characteristics of stimulant and opioid deaths in San Francisco, 2005 - 2015 (n = 2001)
| Overall | Stimulant deaths† | Opioid deaths†† | |||||
|---|---|---|---|---|---|---|---|
| N (%)‡ or M (SD) | N (%)δ or M (SD) | N (%)δ or M (SD) | |||||
| Total | 2001 | (100.00) | 749 | (37.43)‡ | 1252 | (62.57)‡ | |
| Demographic characteristics* | |||||||
| Age | 48.84 | (12.06) | 50.22 | (11.14) | 48.01 | (12.50) | |
| Sex | |||||||
| Male | 1470 | (73.46) | 590 | (78.77) | 880 | (70.29) | |
| Female | 531 | (26.54) | 159 | (21.23) | 372 | (29.71) | |
| Race/ethnicity | |||||||
| White | 1089 | (54.42) | 306 | (40.85) | 783 | (62.54) | |
| Black/African American | 552 | (27.59) | 281 | (37.52) | 271 | (21.65) | |
| Hispanic/Latino(a) | 216 | (10.79) | 89 | (11.88) | 127 | (10.14) | |
| Asian/Pacific Islander | 80 | (4.00) | 49 | (6.54) | 31 | (2.48) | |
| Other/Mixed¶ | 64 | (3.20) | 24 | (3.20) | 40 | (3.19) | |
| Death Year | |||||||
| 2005 - 2007 | 517 | (25.84) | 223 | (29.77) | 294 | (23.48) | |
| 2008 - 2010 | 522 | (26.09) | 153 | (20.43) | 369 | (29.47) | |
| 2011 - 2013 | 568 | (28.39) | 203 | (27.10) | 365 | (29.15) | |
| 2014 - 2015 | 394 | (19.69) | 170 | (22.70) | 224 | (17.89) | |
| Death also due to alcohol†††* | |||||||
| No | 1679 | (83.91) | 669 | (89.32) | 1010 | (80.67) | |
| Yes | 322 | (16.09) | 80 | (10.68) | 242 | (19.33) | |
| Cause of death | |||||||
| Cardiac* | 83 | (4.15) | 59 | (7.88) | 24 | (1.92) | |
| Electrical conduction | 16 | (0.80) | 11 | (1.47) | 5 | (0.40) | |
| Aortic | 9 | (0.45) | 8 | (1.07) | 1 | (0.08) | |
| Pericardial | 3 | (0.15) | 3 | (0.40) | 0 | 0.00 | |
| Hypertension | 21 | (1.05) | 11 | (1.47) | 10 | (0.80) | |
| Atherosclerotic disease or myocardial infarction | 28 | (1.40) | 22 | (2.94) | 6 | (0.48) | |
| Congestive heart failure or cardiomyopathy | 16 | (0.80) | 11 | (1.47) | 5 | (0.40) | |
| Cerebral hemorrhage* | 102 | (5.10) | 98 | (13.08) | 4 | (0.32) | |
| Neurologic or psychiatric | 5 | (0.25) | 3 | (0.40) | 2 | (0.16) | |
| Chronic neurologic | 1 | (0.05) | 0 | 0.00 | 1 | (0.08) | |
| Other neurologic | 1 | (0.05) | 0 | 0.00 | 1 | (0.08) | |
| Seizure | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | |
| Psychiatric | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | |
| Herniation | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | |
| Infection | 23 | (1.15) | 9 | (1.20) | 14 | (1.12) | |
| Pneumonia | 12 | (0.60) | 4 | (0.53) | 8 | (0.64) | |
| Endocarditis | 4 | (0.20) | 2 | (0.27) | 2 | (0.16) | |
| Infection NOS | 9 | (0.45) | 4 | (0.53) | 5 | (0.40) | |
| Trauma | 12 | (0.60) | 5 | (0.67) | 7 | (0.56) | |
| Malignancy | 7 | (0.35) | 2 | (0.27) | 5 | (0.40) | |
| Overdose Complication | 32 | (1.60) | 13 | (1.74) | 19 | (1.52) | |
| Aspiration | 7 | (0.35) | 2 | (0.27) | 5 | (0.40) | |
| Anoxia | 28 | (1.40) | 12 | (1.60) | 16 | (1.28) | |
| Other | 42 | (2.10) | 18 | (2.40) | 24 | (1.92) | |
| Rheumatologic | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | |
| Metabolic/endocrine | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | |
| Liver disease | 11 | (0.55) | 1 | (0.13) | 10 | (0.80) | |
| Renal disease | 3 | (0.15) | 2 | (0.27) | 1 | (0.08) | |
| Chronic pulmonary disease | 5 | (0.25) | 3 | (0.40) | 2 | (0.16) | |
| Sleep Apnea | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | |
| Multi-organ failure | 10 | (0.50) | 5 | (0.67) | 5 | (0.40) | |
| Other hemorrhage | 4 | (0.20) | 3 | (0.40) | 1 | (0.08) | |
| Bowel ischemia | 4 | (0.20) | 2 | (0.27) | 2 | (0.16) | |
| Thromboembolic | 4 | (0.20) | 1 | (0.13) | 3 | (0.24) | |
| Significant contributing condition | |||||||
| Cardiac* | 581 | (29.04) | 252 | (33.64) | 329 | (26.28) | |
| Electrical conduction | 5 | (0.25) | 2 | (0.27) | 3 | (0.24) | |
| Aortic | 6 | (0.30) | 3 | (0.40) | 3 | (0.24) | |
| Pericardial | 5 | (0.25) | 4 | (0.53) | 1 | (0.08) | |
| Hypertension | 333 | (16.64) | 148 | (19.76) | 185 | (14.78) | |
| Atherosclerotic disease or myocardial infarction | 246 | (12.29) | 118 | (15.75) | 128 | (10.22) | |
| Congestive heart failure or cardiomyopathy | 165 | (8.25) | 69 | (9.21) | 96 | (7.67) | |
| Cerebral hemorrhage | 6 | (0.30) | 2 | (0.27) | 4 | (0.32) | |
| Neurologic or psychiatric | 30 | (1.50) | 10 | (1.34) | 20 | (1.60) | |
| Chronic neurologic | 14 | (0.70) | 2 | (0.27) | 12 | (0.96) | |
| Other neurologic | 1 | (0.05) | 0 | 0.00 | 1 | (0.08) | |
| Seizure | 13 | (0.65) | 6 | (0.80) | 7 | (0.56) | |
| Psychiatric | 2 | (0.10) | 2 | (0.27) | 0 | 0.00 | |
| Herniation | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | |
| Infection | 83 | (4.15) | 24 | (3.20) | 59 | (4.71) | |
| Pneumonia | 54 | (2.70) | 13 | (1.74) | 41 | (3.27) | |
| Endocarditis | 3 | (0.15) | 2 | (0.27) | 1 | (0.08) | |
| Infection NOS | 30 | (1.50) | 12 | (1.60) | 18 | (1.44) | |
| Trauma | 12 | (0.60) | 5 | (0.67) | 7 | (0.56) | |
| Malignancy | 26 | (1.30) | 10 | (1.34) | 16 | (1.28) | |
| Overdose complication | 1 | (0.05) | 0 | 0.00 | 1 | (0.08) | |
| Aspiration | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | |
| Anoxia | 1 | (0.05) | 0 | 0.00 | 1 | (0.08) | |
| Other | 397 | (19.84) | 151 | (20.16) | 246 | (19.65) | |
| Rheumatologic | 2 | (0.10) | 0 | 0.00 | 2 | (0.16) | |
| Metabolic/endocrine | 140 | (7.00) | 48 | (6.41) | 92 | (7.35) | |
| Liver disease | 118 | (5.90) | 41 | (5.47) | 77 | (6.15) | |
| Renal disease | 54 | (2.70) | 20 | (2.67) | 34 | (2.72) | |
| Chronic pulmonary disease | 133 | (6.65) | 57 | (7.61) | 76 | (6.07) | |
| Sleep Apnea | 7 | (0.35) | 2 | (0.27) | 5 | (0.40) | |
| Multi-organ failure | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | |
| Other hemorrhage | 8 | (0.40) | 4 | (0.53) | 4 | (0.32) | |
| Bowel ischemia | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | |
| Thromboembolic | 2 | (0.10) | 1 | (0.13) | 1 | (0.08) | |
| Chronic infections | |||||||
| HIV | 87 | (4.35) | 41 | (5.47) | 46 | (3.67) | |
| HCV | 135 | (6.75) | 44 | (5.87) | 91 | (7.27) | |
Causes of death and significant contributing conditions are not mutually exclusive. Except for 6/2001 (0.30%) cases with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or cocaine; excludes decedents with cause of death listed as acute toxicity from opioids.
Includes decedents with cause of death listed as acute toxicity from heroin, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, propoxyphene, and other opioids.
Percentages calculated out of a total of 2001 opioid or stimulant deaths from 2005-2015.
Percentages calculated out of the total deaths for that substance group (749 for stimulant deaths; 1252 for opioid deaths).
Included in bivariable analyses comparing stimulant and opioid deaths.
Includes American Indian/Alaska Native (n = 15), Other/Mixed (n = 43), and Unknown (n = 6) race/ethnicities.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Appendix Table 1b. Demographic and detailed clinical characteristics of stimulant-only, opioid-plus-stimulant, and opioid-only deaths in San Francisco, 2005 - 2015 (n = 2001)
| Overall | Stimulant-only deaths† |
Opioid-plus - stimulant deaths†† |
Opioid-only deaths††† |
Bivariable results | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%)‡ or M (SD) | N (%)δ or M (SD) | N (%)δ or M (SD) | N (%)δ or M (SD) | Test statistic | P-value | |||||||
| Total | 2001 | (100.00) | 749 | (37.43)‡ | 624 | (31.18)‡ | 628 | (31.38)‡ | ||||
| Demographic characteristics* | ||||||||||||
| Age | 48.84 | (12.06) | 50.22 | (11.14) | 47.43 | (11.31) | 48.60 | (13.57) | F = 9.43 | p < 0.01 | ||
| Sex | χ2 = 22.27 | p < 0.01 | ||||||||||
| Male | 1470 | (73.46) | 590 | (78.77) | 456 | (73.08) | 424 | (67.52) | ||||
| Female | 531 | (26.54) | 159 | (21.23) | 168 | (26.92) | 204 | (32.48) | ||||
| Race/ethnicity | χ2 = 139.82 | p < 0.01 | ||||||||||
| White | 1089 | (54.42) | 306 | (40.85) | 358 | (57.37) | 425 | (67.68) | ||||
| Black/African American | 552 | (27.59) | 281 | (37.52) | 182 | (29.17) | 89 | (14.17) | ||||
| Hispanic/Latino(a) | 216 | (10.79) | 89 | (11.88) | 54 | (8.65) | 73 | (11.62) | ||||
| Asian/Pacific Islander | 80 | (4.00) | 49 | (6.54) | 11 | (1.76) | 20 | (3.18) | ||||
| Other/Mixed | 64 | (3.20) | 24 | (3.20) | 19 | (3.04) | 21 | (3.34) | ||||
| Death Year | χ2 = 82.11 | p < 0.01 | ||||||||||
| 2005 - 2007 | 517 | (25.84) | 223 | (29.77) | 202 | (32.37) | 92 | (14.65) | ||||
| 2008 - 2010 | 522 | (26.09) | 153 | (20.43) | 158 | (25.32) | 211 | (33.60) | ||||
| 2011 - 2013 | 568 | (28.39) | 203 | (27.10) | 156 | (25.00) | 209 | (33.28) | ||||
| 2014 - 2015 | 394 | (19.69) | 170 | (22.70) | 108 | (17.31) | 116 | (18.47) | ||||
| Death also due to alcohol†††* | χ2 = 38.06 | p < 0.01 | ||||||||||
| No | 1679 | (83.91) | 669 | (89.32) | 526 | (84.29) | 484 | (77.07) | ||||
| Yes | 322 | (16.09) | 80 | (10.68) | 98 | (15.71) | 144 | (22.93) | ||||
| Cause of death | ||||||||||||
| Cardiac* | 83 | (4.15) | 59 | (7.88) | 9 | (1.44) | 15 | (2.39) | χ2 = 42.58 | p < 0.01 | ||
| Electrical conduction | 16 | (0.80) | 11 | (1.47) | 1 | (0.16) | 4 | (0.64) | ||||
| Aortic | 9 | (0.45) | 8 | (1.07) | 1 | (0.16) | 0 | 0.00 | ||||
| Pericardial | 3 | (0.15) | 3 | (0.40) | 0 | 0.00 | 0 | 0.00 | ||||
| Hypertension | 21 | (1.05) | 11 | (1.47) | 3 | (0.48) | 7 | (1.11) | ||||
| Atherosclerotic disease ormyocardial infarction | 28 | (1.40) | 22 | (21.23) | 2 | (0.32) | 4 | (0.64) | ||||
| Congestive heart failure or cardiomyopathy | 16 | (0.80) | 11 | (21.23) | 2 | (0.32) | 3 | (0.48) | ||||
| Cerebral hemorrhage* | 102 | (5.10) | 98 | (13.08) | 1 | (0.16) | 3 | (0.48) | Fisher's exact | p < 0.01 | ||
| Neurologic or psychiatric | 5 | (0.25) | 3 | (0.40) | 0 | 0.00 | 2 | (0.32) | ||||
| Chronic neurologic | 1 | (0.05) | 0 | 0.00 | 0 | 0.00 | 1 | (0.16) | ||||
| Other neurologic | 1 | (0.05) | 0 | 0.00 | 0 | 0.00 | 1 | (0.16) | ||||
| Seizure | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | 0 | 0.00 | ||||
| Psychiatric | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | 0 | 0.00 | ||||
| Herniation | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | 0 | 0.00 | ||||
| Infection | 23 | (1.15) | 9 | (1.20) | 5 | (0.80) | 9 | (1.43) | ||||
| Pneumonia | 12 | (0.60) | 4 | (0.53) | 3 | (0.48) | 5 | (0.80) | ||||
| Endocarditis | 4 | (0.20) | 2 | (0.27) | 2 | (0.32) | 0 | 0.00 | ||||
| Infection NOS | 9 | (0.45) | 4 | (0.53) | 0 | 0.00 | 5 | (0.80) | ||||
| Trauma | 12 | (0.60) | 5 | (0.67) | 5 | (0.80) | 2 | (0.32) | ||||
| Malignancy | 7 | (0.35) | 2 | (0.27) | 2 | (0.32) | 3 | (0.48) | ||||
| Overdose Complication | 32 | (1.60) | 13 | (1.74) | 7 | (1.12) | 12 | (1.91) | ||||
| Aspiration | 7 | (0.35) | 2 | (0.27) | 2 | (0.32) | 3 | (0.48) | ||||
| Anoxia | 28 | (1.40) | 12 | (1.60) | 5 | (0.80) | 11 | (1.75) | ||||
| Other | 42 | (2.10) | 18 | (2.40) | 8 | (1.28) | 16 | (2.55) | ||||
| Rheumatologic | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | ||||
| Metabolic/endocrine | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | 0 | 0.00 | ||||
| Liver disease | 11 | (0.55) | 1 | (0.13) | 2 | (0.32) | 8 | (1.27) | ||||
| Renal disease | 3 | (0.15) | 2 | (0.27) | 0 | 0.00 | 1 | (0.16) | ||||
| Chronic pulmonary disease | 5 | (0.25) | 3 | (0.40) | 0 | 0.00 | 2 | (0.32) | ||||
| Sleep Apnea | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | ||||
| Multi-organ failure | 10 | (0.50) | 5 | (0.67) | 3 | (0.48) | 2 | (0.32) | ||||
| Other hemorrhage | 4 | (0.20) | 3 | (0.40) | 0 | 0.00 | 1 | (0.16) | ||||
| Bowel ischemia | 4 | (0.20) | 2 | (0.27) | 1 | (0.16) | 1 | (0.16) | ||||
| Thromboembolic | 4 | (0.20) | 1 | (0.13) | 2 | (0.32) | 1 | (0.16) | ||||
| Significant contributing condition | ||||||||||||
| Cardiac* | 581 | (29.04) | 252 | (33.64) | 136 | (21.79) | 193 | (30.73) | χ2 = 24.48 | p < 0.01 | ||
| Electrical conduction | 5 | (0.25) | 2 | (0.27) | 1 | (0.16) | 2 | (0.32) | ||||
| Aortic | 6 | (0.30) | 3 | (0.40) | 1 | (0.16) | 2 | (0.32) | ||||
| Pericardial | 5 | (0.25) | 4 | (0.53) | 0 | 0.00 | 1 | (0.16) | ||||
| Hypertension | 333 | (16.64) | 148 | (19.76) | 73 | (11.70) | 112 | (17.83) | ||||
| Atherosclerotic disease or myocardial infarction | 246 | (12.29) | 118 | (19.76) | 58 | (9.29) | 70 | (11.15) | ||||
| Congestive heart failure or cardiomyopathy | 165 | (8.25) | 69 | (19.76) | 42 | (6.73) | 54 | (8.60) | ||||
| Cerebral hemorrhage | 6 | (0.30) | 2 | (0.27) | 0 | 0.00 | 4 | (0.64) | ||||
| Neurologic or psychiatric | 30 | (1.50) | 10 | (1.34) | 6 | (0.96) | 14 | (2.23) | ||||
| Chronic neurologic | 14 | (0.70) | 2 | (0.27) | 4 | (0.64) | 8 | (1.27) | ||||
| Other neurologic | 1 | (0.05) | 0 | 0.00 | 1 | (0.16) | 0 | 0.00 | ||||
| Seizure | 13 | (0.65) | 6 | (0.80) | 1 | (0.16) | 6 | (0.96) | ||||
| Psychiatric | 2 | (0.10) | 2 | (0.27) | 0 | 0.00 | 0 | 0.00 | ||||
| Herniation | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | 0 | 0.00 | ||||
| Infection | 83 | (4.15) | 24 | (3.20) | 22 | (3.53) | 37 | (5.89) | ||||
| Pneumonia | 54 | (2.70) | 13 | (1.74) | 14 | (2.24) | 27 | (4.30) | ||||
| Endocarditis | 3 | (0.15) | 2 | (0.27) | 1 | (0.16) | 0 | 0.00 | ||||
| Infection NOS | 30 | (1.50) | 12 | (1.60) | 7 | (1.12) | 11 | (1.75) | ||||
| Trauma | 12 | (0.60) | 5 | (0.67) | 5 | (0.80) | 2 | (0.32) | ||||
| Malignancy | 26 | (1.30) | 10 | (1.34) | 7 | (1.12) | 9 | (1.43) | ||||
| Overdose complication | 1 | (0.05) | 0 | 0.00 | 1 | (0.16) | 0 | 0.00 | ||||
| Aspiration | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | ||||
| Anoxia | 1 | (0.05) | 0 | 0.00 | 1 | (0.16) | 0 | 0.00 | ||||
| Other | 397 | (19.84) | 151 | (20.16) | 111 | (17.79) | 135 | (21.50) | ||||
| Rheumatologic | 2 | (0.10) | 0 | 0.00 | 0 | 0.00 | 2 | (0.32) | ||||
| Metabolic/endocrine | 140 | (7.00) | 48 | (6.41) | 40 | (6.41) | 52 | (8.28) | ||||
| Liver disease | 118 | (5.90) | 41 | (5.47) | 31 | (4.97) | 46 | (7.32) | ||||
| Renal disease | 54 | (2.70) | 20 | (2.67) | 15 | (2.40) | 19 | (3.03) | ||||
| Chronic pulmonary disease | 133 | (6.65) | 57 | (7.61) | 33 | (5.29) | 43 | (6.85) | ||||
| Sleep Apnea | 7 | (0.35) | 2 | (0.27) | 1 | (0.16) | 4 | (0.64) | ||||
| Multi-organ failure | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | ||||
| Other hemorrhage | 8 | (0.40) | 4 | (0.53) | 2 | (0.32) | 2 | (0.32) | ||||
| Bowel ischemia | 1 | (0.05) | 1 | (0.13) | 0 | 0.00 | 0 | 0.00 | ||||
| Thromboembolic | 2 | (0.10) | 1 | (0.13) | 0 | 0.00 | 1 | (0.16) | ||||
| Chronic infections | ||||||||||||
| HIV | 87 | (4.35) | 41 | (5.47) | 29 | (4.65) | 17 | (2.71) | ||||
| HCV | 135 | (6.75) | 44 | (5.87) | 50 | (8.01) | 41 | (6.53) | ||||
Causes of death and significant contributing conditions are not mutually exclusive. Except for 6/2001 (0.30%) cases with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or cocaine; excludes decedents with cause of death listed as acute toxicity from opioids.
Includes decedents with cause of death listed as acute toxicity from stimulants (methamphetamine, amphetamine, or cocaine) and opioids (heroin, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, propoxyphene, and other opioids).
Includes decedents with cause of death listed as acute toxicity from heroin, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, propoxyphene, and other opioids; excludes decedents with cause of death listed as acute toxicity from stimulants.
Percentages calculated out of a total of 2001 opioid or stimulant deaths from 2005-2015.
Percentages calculated out of the total deaths for that substance group (749 for stimulant-only deaths; 624 for opioid-plus-stimulant deaths; 628 for opioid-only deaths).
Included in bivariable analyses comparing stimulant-only, opioid-plus-stimulant, or opioid-only deaths.
Includes American Indian/Alaska Native (n = 15), Other/Mixed (n = 43), and Unknown (n = 6) race/ethnicities.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Appendix Table 2. Demographic and detailed clinical characteristics of cocaine and methamphetamine/amphetamine (MAMP) deaths in San Francisco, 2005 - 2015 (n = 695)
| Cocaine deaths† | MAMP deaths†† | |||
|---|---|---|---|---|
| N (%)δ or M (SD) | N (%)δ or M (SD) | |||
| Total | 424 | (61.01)‡ | 271 | (38.99)‡ |
| Demographic characteristic* | ||||
| Age | 52.40 | (10.53) | 47.47 | (11.13) |
| Sex | ||||
| Male | 324 | (76.42) | 224 | (82.66) |
| Female | 100 | (23.58) | 47 | (17.34) |
| Race/ethnicity | ||||
| White | 120 | (28.30) | 166 | (61.25) |
| Black/African American | 228 | (53.77) | 29 | (10.70) |
| Hispanic/Latino(a) | 47 | (11.08) | 37 | (13.65) |
| Asian/Pacific Islander | 17 | (4.01) | 30 | (11.07) |
| Other/Mixed | 12 | (2.83) | 9 | (3.32) |
| Death Year | ||||
| 2005 - 2007 | 140 | (33.02) | 58 | (21.40) |
| 2008 - 2010 | 98 | (23.11) | 51 | (18.82) |
| 2011 - 2013 | 112 | (26.42) | 79 | (29.15) |
| 2014 - 2015 | 74 | (17.45) | 83 | (30.63) |
| Death also due to alcohol†††* | ||||
| No | 359 | (84.67) | 261 | (96.31) |
| Yes | 65 | (15.33) | 10 | (3.69) |
| Cause of death | ||||
| Cardiac* | 43 | (10.14) | 15 | (5.54) |
| Electrical conduction | 10 | (2.36) | 1 | (0.37) |
| Aortic | 6 | (1.42) | 2 | (0.74) |
| Pericardial | 2 | (0.47) | 1 | (0.37) |
| Hypertension | 8 | (1.89) | 2 | (0.74) |
| Atherosclerotic disease or myocardial infarction | 12 | (2.83) | 9 | (3.32) |
| Congestive heart failure or cardiomyopathy | 9 | (2.12) | 2 | (0.74) |
| Cerebral hemorrhage* | 50 | (11.79) | 41 | (15.13) |
| Neurologic or psychiatric | 2 | (0.47) | 1 | (0.37) |
| Chronic neurologic | 0 | 0.00 | 0 | 0.00 |
| Other neurologic | 0 | 0.00 | 0 | 0.00 |
| Seizure | 1 | (0.24) | 0 | 0.00 |
| Psychiatric | 1 | (0.24) | 0 | 0.00 |
| Herniation | 0 | 0.00 | 1 | (0.37) |
| Infection | 4 | (0.94) | 5 | (1.85) |
| Pneumonia | 2 | (0.47) | 2 | (0.74) |
| Endocarditis | 0 | 0.00 | 2 | (0.74) |
| Infection NOS | 2 | (0.47) | 2 | (0.74) |
| Trauma | 3 | (0.71) | 2 | (0.74) |
| Malignancy | 2 | (0.47) | 0 | 0.00 |
| Overdose complication | 12 | (2.83) | 1 | (0.37) |
| Aspiration | 2 | (0.47) | 0 | 0.00 |
| Anoxia | 11 | (2.59) | 1 | (0.37) |
| Other | 7 | (1.65) | 9 | (3.32) |
| Rheumatologic | 0 | 0.00 | 0 | 0.00 |
| Metabolic/endocrine | 0 | 0.00 | 1 | (0.37) |
| Liver disease | 1 | (0.24) | 0 | 0.00 |
| Renal disease | 1 | (0.24) | 1 | (0.37) |
| Chronic pulmonary disease | 2 | (0.47) | 1 | (0.37) |
| Sleep Apnea | 0 | 0.00 | 0 | 0.00 |
| Multi-organ failure | 2 | (0.47) | 3 | (1.11) |
| Other hemorrhage | 1 | (0.24) | 1 | (0.37) |
| Bowel ischemia | 0 | 0.00 | 1 | (0.37) |
| Thromboembolic | 0 | 0.00 | 1 | (0.37) |
| Significant contributing condition | ||||
| Cardiac* | 162 | (38.21) | 78 | (28.78) |
| Electrical conduction | 1 | (0.24) | 1 | (0.37) |
| Aortic | 2 | (0.47) | 1 | (0.37) |
| Pericardial | 3 | (0.71) | 1 | (0.37) |
| Hypertension | 103 | (24.29) | 39 | (14.39) |
| Atherosclerotic disease or myocardial infarction | 76 | (17.92) | 37 | (13.65) |
| Congestive heart failure or cardiomyopathy | 41 | (9.67) | 24 | (8.86) |
| Cerebral hemorrhage | 1 | (0.24) | 1 | (0.37) |
| Neurologic or psychiatric | 6 | (1.42) | 2 | (0.74) |
| Chronic neurologic | 1 | (0.24) | 1 | (0.37) |
| Other neurologic | 0 | 0.00 | 0 | 0.00 |
| Seizure | 5 | (1.18) | 0 | 0.00 |
| Psychiatric | 1 | (0.24) | 1 | (0.37) |
| Herniation | 0 | 0.00 | 0 | 0.00 |
| Infection | 15 | (3.54) | 7 | (2.58) |
| Pneumonia | 9 | (2.12) | 3 | (1.11) |
| Endocarditis | 2 | (0.47) | 0 | 0.00 |
| Infection NOS | 6 | (1.42) | 4 | (1.48) |
| Trauma | 3 | (0.71) | 2 | (0.74) |
| Malignancy | 8 | (1.89) | 2 | (0.74) |
| Overdose Complication | 0 | 0.00 | 0 | 0.00 |
| Aspiration | 0 | 0.00 | 0 | 0.00 |
| Anoxia | 0 | 0.00 | 0 | 0.00 |
| Other | 105 | (24.76) | 34 | (12.55) |
| Rheumatologic | 0 | 0.00 | 0 | 0.00 |
| Metabolic/endocrine | 35 | (8.25) | 10 | (3.69) |
| Liver disease | 22 | (5.19) | 15 | (5.54) |
| Renal disease | 14 | (3.30) | 3 | (1.11) |
| Chronic pulmonary disease | 48 | (11.32) | 7 | (2.58) |
| Sleep Apnea | 0 | 0.00 | 2 | (0.74) |
| Multi-organ failure | 0 | 0.00 | 0 | 0.00 |
| Other hemorrhage | 2 | (0.47) | 1 | (0.37) |
| Bowel ischemia | 0 | 0.00 | 1 | (0.37) |
| Thromboembolic | 1 | (0.24) | 0 | 0.00 |
| Chronic infections | ||||
| HIV | 20 | (4.72) | 20 | (7.38) |
| HCV | 22 | (5.19) | 19 | (7.01) |
Causes of death and significant contributing conditions are not mutually exclusive. Except for 4/695 (0.56%) cocaine or MAMP deaths with unknown race/ethnicity (coded into "Other/Mixed" race/ethnicity), no data were missing.
Includes decedents with cause of death listed as acute toxicity from cocaine; excludes decedents with cause of death listed as acute toxicity from methamphetamine, amphetamine, or opioids.
Includes decedents with cause of death listed as acute toxicity from methamphetamine or amphetamine; excludes decedents with cause of death listed as acute toxicity from cocaine or opioids.
Percentages calculated out of a total of 695 cocaine or MAMP deaths from 2005-2015.
Percentages calculated out of the total deaths for that substance group (424 for cocaine deaths; 271 for MAMP deaths).
Included in bivariable analyses.
Includes American Indian/Alaska Native (n = 3), Other/Mixed (n = 14), and Unknown (n = 4) race/ethnicities.
Includes decedents with cause of death listed as acute toxicity from alcohol.
Footnotes
Declarations of competing interests: The authors declare that they have no competing interests. Dr. Coffin has directed National Institutes of Health-funded trials that received donated study drug from Alkermes (2014–2015) and Gilead (2016–2017).
6.0 References
- American Heart Association. Understand Your Risks to Prevent a Heart Attack. September 2016. http://www.heart.org/HEARTORG/Conditions/HeartAttack/UnderstandYourRiskstoPreventaHeartAttack/Understand-Your-Risks-to-Prevent-a-Heart-Attack_UCM_002040_Article.jsp
- Bernstein KT, Bucciarelli A, Piper TM, Gross C, Tardiff K, Galea S, 2007. Cocaine- and opiate-related fatal overdose in New York City, 1990–2000. BMC Public Health. 7, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcaterra S, Binswanger IA, 2013. National trends in psychostimulant-related deaths: 1999–2009. Subst. Abus. 34, 129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K, 2003. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 98, 739–747. [DOI] [PubMed] [Google Scholar]
- Dahan A, Niesters M, Olofsen E, Smith T, Overdyk F, 2013. Opioids In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R (Eds.), Clinical Anesthesia Lippincott, Williams & Wilkins, Philadelphia, pp. 501–522. [Google Scholar]
- Dahan A, Aarts L, Smith TW, 2010. Incidence, Reversal, and Prevention of Opioid-induced Respiratory Depression. Anesthesiology. 112, 226–238. [DOI] [PubMed] [Google Scholar]
- Darke S, Kaye S, Duflou J, 2017a. Rates, characteristics and circumstances of methamphetamine-related death in Australia: a national 7-year study. Addiction. 112, 2191–2201. [DOI] [PubMed] [Google Scholar]
- Darke S, Duflou J, Kaye S, 2017b. Prevalence and nature of cardiovascular disease in methamphetamine-related death: A national study. Drug and Alcohol Dependence. 179, 174–179. [DOI] [PubMed] [Google Scholar]
- Darke S, Kaye S, McKetin R, Duflou J, 2008. Major physical and psychological harms of methamphetamine use. Drug and Alcohol Rev. 27, 253–262. [DOI] [PubMed] [Google Scholar]
- Darke S, Kaye S, Duflou J, 2006. Comparative cardiac pathology among deaths due to cocaine toxicity, opioid toxicity and non-drug-related causes. Addiction. 101, 1771–1777. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, Minino AM, 2017. Drug Overdose Deaths in the United States, 1999–2015. National Center for Health Statistics Data Brief. (273), 1–8. [PubMed] [Google Scholar]
- Herbeck DM, Brecht ML, Lovinger K, 2015. Mortality, causes of death, and health status among methamphetamine users. J. Addict. Dis. 34, 88–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho EL, Josephson SA, Lee HS, Smith WS, 2009. Cerebrovascular complications of methamphetamine abuse. Neurocrit. Care. 10, 295–305. [DOI] [PubMed] [Google Scholar]
- Huang MC, Yang SY, Lin SK, Chen KY, Chen YY, Kuo CJ, Hung YN, 2016. Risk of Cardiovascular Diseases and Stroke Events in Methamphetamine Users: A 10-Year Follow-Up Study. J. Clin. Psychiatry. 77, 1396–1403. [DOI] [PubMed] [Google Scholar]
- Karch SB, 2009. Karch’s Pathology of Drug Abuse. CRC Press, Boca Raton. [Google Scholar]
- Kaye S, McKetin R, Duflou J, Darke S, 2007. Methamphetamine and cardiovascular pathology: a review of the evidence. Addiction. 102, 1204–1211. [DOI] [PubMed] [Google Scholar]
- Lappin JM, Darke S, Farrell M, 2017. Stroke and methamphetamine use in young adults: a review. J. Neurol. Neurosurg. Psychiatry. [DOI] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC, 2011. Mortality associated with illegal drug use among adults in the United States. Am. J. Drug Alcohol Abuse. 37, 155–164. [DOI] [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. Heart Disease Behavior. August 2015. https://www.cdc.gov/heartdisease/behavior.htm
- National Institute on Drug Abuse. Overdose death rates. January 2017. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-ratesRecommendationStatementFinal/drug-use-illicit-screening
- Oderda GM, Gan TJ, Johnson BH, Robinson SB, 2013. Effect of opioid-related adverse events on outcomes in selected surgical patients. J. Pain Palliat. Care Pharmacother. 27, 62–70. [DOI] [PubMed] [Google Scholar]
- Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Federal Registrar. 1997; 62(210): 58781–90. [Google Scholar]
- Paulozzi L, Dellinger A, Degutis L, 2012. Lessons from the past. Inj. Prev. 18, 70–2011-040294. Epub 2011 Dec 30. [DOI] [PubMed] [Google Scholar]
- Petitti DB, Sidney S, Quesenberry C, Bernstein A, 1998. Stroke and cocaine or amphetamine use. Epidemiology. 9, 596–600. [PubMed] [Google Scholar]
- Riley ED, Hsue PY, Vittinghoff E, Wu AH, Coffin PO, Moore PK, Lynch KL, 2017. Higher prevalence of detectable troponin I among cocaine-users without known cardiovascular disease. Drug and Alcohol Dependence. 172, 88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM, 2016. Increases in Drug and Opioid Overdose Deaths — United States, 2000–2014. Morbidity and Mortality Weekly Report (MMWR). 64, 1378. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ, 2016. Drug poisoning deaths in the United States, 1999–2012: a statistical adjustment analysis. Popul. Health. Metr. 14(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stankowski RV, Kloner RA, Rezkalla SH, 2015. Cardiovascular consequences of cocaine use. Trends Cardiovasc. Med. 25, 517–526. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- United States Census Bureau. P1: total population. 2010 Census Summary File 1. 2010 [Google Scholar]
- Visconti AJ, Santos GM, Lemos NP, Burke C, Coffin PO, 2015. Opioid Overdose Deaths in the City and County of San Francisco: Prevalence, Distribution, and Disparities. J. Urban Health. 92, 758–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol. 2008. April; 61(4):344–9. PMID: 18313558 [DOI] [PubMed] [Google Scholar]
- Westover AN, McBride S, Haley RW, 2007. Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients. Arch. Gen. Psychiatry. 64, 495–502. [DOI] [PubMed] [Google Scholar]