Abstract
Objective:
To evaluate the association between non-custodial grandparent caregiving and cognition using the Health and Retirement Study (HRS), a population-based study of older adults.
Methods:
Participants were White and African-American grandparents aged ≥ 65 years. Only non-custodial grandparents who reported not living with their grandchildren over the 3 waves were included in our analyses. Grandparent caregiving status and cognition were assessed in 2006, 2008, and 2010. Analyses controlled for demographics, baseline health, depressive symptoms, and baseline cognition.
Results:
Both the number of waves of grandparent caregiving and the total number of grandparent caregiving hours across the 3 waves were associated with better cognitive functioning at 4-year follow-up in 2010. Associations were observed among Whites, but not among African-Americans.
Discussion:
This study uses longitudinal data to evaluate the association between grandparent caregiving and cognitive functioning. Findings suggest that providing care may be beneficial for some grandparents.
Keywords: Helping, Intergenerational Ties, Health Disparities, Grandparents, Caregiving
Eighty-three percent of U.S. adults aged ≥65 years are grandparents (Pew Research, 2015). Within the larger family structure, grandparents play a number of different roles, providing varying levels of support based on family composition and needs. In some instances, grandparents serve as the primary caregiver, replacing parents who are unable to provide support due to mental/physical health issues, substance abuse, incarceration, abandonment, and/or death. Of the 65 million grandparents in the United States, nearly 10% (7 million) live with at least one grandchild. Among those living with a grandchild 37% also serve as their grandchildren’s primary caregiver (U.S. Census Bureau, 2012). These grandparents are likely to experience caregiving as a stressor, as they often assume the caregiving role due to parental crises (Burton & Dilworth-Anderson, 1991). Further, these caregivers are typically responsible for the most basic needs of their grandchildren while at the same time facing economic distress, age-related physical decline, and legal challenges associated with obtaining custodial rights (see review by Hayslip & Kaminski, 2005). Studies that focus on grandparents raising grandchildren (i.e. grandparents serving as custodial caregivers) generally associate the provision of this form of support with numerous adverse physical health outcomes, including poorer self-rated health (Chen & Liu, 2012; Minkler & Fuller-Thomson, 1999), increased frailty (Chen, Bair, Mao, & Yang, 2015) and greater coronary heart disease risk (Lee, Colditz, Berkman, & Kawachi, 2003).
Aside from raising grandchildren, grandparents can also provide supplemental support to families by serving as secondary support providers (i.e. caregivers). This form of caregiving may involve babysitting when parents are unavailable, or actively choosing to spend time with grandchildren in order to strengthen familial bonds. Unlike custodial grandparent caregiving, this form of grandparent caregiving may be less stressful, as it may be voluntary and/or require less overall responsibility. Most American grandparents provide care in this manner. Among grandparents who report providing care to grandchildren, 72% report doing so only occasionally (Pew Research Center, 2015). A small literature has begun to focus on grandparents who provide support in this manner. Unlike existing studies on custodial grandparent caregiving, studies that focus on non-custodial caregiving suggest that providing this form of support may be linked to positive outcomes. Hughes, Waite, LaPierre & Luo (2007) observed in longitudinal analyses that grandparents who babysat their grandchildren reported better self-rated health, more frequent exercise, and fewer functional limitations compared to their noncaregiving counterparts. In another study, Hilbrand and colleagues (2017) used data from the Berlin Aging Study to demonstrate that non-custodial grandparents who provided childcare had decreased mortality hazards when compared to grandparents who did not provide childcare.
Recent studies of non-custodial grandparents have linked this form of grandparent caregiving to positive cognitive outcomes. Cognitive loss is common with aging and is an important predictor of mortality (Shipley, Der, Taylor, & Deary, 2006). A few studies suggest that grandparent caregiving may be related to better cognitive performance (Burn, Henderson, Ames, Dennerstein, & Szoeke, 2014; Arpino & Bordone, 2014). Arpino & Bordone (2014) observed that grandparents who provided care to their grandchildren at least once a week demonstrated greater verbal fluency than non-caregiving grandparents. This study, however, had limitations, as it relied on cross-sectional data. While cross-sectional data can provide useful information, temporality is uncertain, as grandparents with higher cognitive abilities may differentially select into the caregiving role. In another study, Burn and colleagues (2014) utilized longitudinal, prospective data to demonstrate that postmenopausal grandmothers who provided care to their grandchildren about one day a week demonstrated better immediate word recall than non-caregiving grandmothers. This study, however, was conducted among a small (n=186) population-based sample of white women ages 57–68 in Australia. Thus, its findings may not be generalizable to a larger, more diverse population of grandparents. Further, this study failed to control for depressive symptoms, which have been associated with greater incidence of mild cognitive impairment (Wilson, Arnold, Schneider, & Bennett, 2007), dementia (Wilson, Krueger, Arnold, Schneider, Kelly, and Barnes, 2007) and cognitive decline (Sachs-Ericsson, Joiner, Plant, & Blazer, 2005).
We propose that non-custodial grandparent caregiving provides some of the social, physical and mental health benefits described under the cognitive enrichment hypothesis, which suggests that engagement in beneficial intellectual, physical and social activities promotes successful cognitive aging (Hertzog, Kramer, and Lindenberger, 2009). Spending time with grandchildren may offer social engagement for older adults, as they may have reduced social involvement due to transitions such as retirement, bereavement, or transition of children out of the home. Contact with grandchildren may help to replenish lost social ties. Additionally, caregiving may improve cognitive performance among grandparents by increasing engagement in mentally stimulating activities such as playing games, helping with homework, and/or reading. Likewise, grandparent caregiving may promote more physical exercise, as it may result in more time spent engaged in physical activities, such as going to the park, taking outdoor trips, walking, or hiking. Non-custodial grandparent caregiving may be an ideal vehicle for promoting cognitive enrichment among older adults, as it may provide the social, psychological, physical and intellectual benefits of caregiving without the strain of custodial responsibility.
In the broader caregiving literature, findings on links between caregiving and health have been mixed. The bulk of literature on family caregiving focuses on the provision of support to individuals with ongoing physical disability. Historically, this literature has suggested that family caregiving is associated with a range of adverse physical health outcomes, including metabolic dysregulation, poorer self-rated health, and increased mortality (see reviews by Schulz & Sherwood, 2008; Vitaliano, Zhang, & Scanlan). A growing body of literature, however, posits that these negative effects are not universal. Rather, they are moderated by a host of care recipient and caregiver variables. For example, family caregivers who report having no choice in assuming the caregiving role report more negative health effects and greater physical strain than their counterparts (Schulz, Beach, Cook, Martire, Tomlinson, & Monin, 2012). Other factors that have been linked to poor health outcomes among caregivers include living with the care recipient and recipient health impairments (see reviews by Pinquart & Sorenson, 2003; Pinquart & Sorenson, 2007). We propose that non-custodial grandparent caregiving may have positive rather than negative effects, as it likely does not share structural similarities with the caregiving experiences typically linked to adverse outcomes.
In the broader caregiving literature, links between caregiving and cognition have been unclear. While some studies link family caregiving to positive cognitive outcomes (Bertrand, Saczynski, Mezzacappa, Hulse, Ensrud, & Fredman, 2012), others suggest that caregiving has negative effects on cognition. Most studies in this area, however, have suffered from methodological weaknesses, including reliance on cross-sectional design (Bertrand, Saczynski, Mezzacappa, Hulse, Ensrud, & Fredman, 2012; Herrera, Mendez-Luck, Crist, Smith, Warre, Ory, & Markides, 2013; Mackenzie, Smith, Hasher, Leach, & Behl, 2007; Mackenzie, Wiprzycka, Hasher, & Goldstein, 2009) and/or failure to control for important covariates with known links to cognition, such as education and income (Mackenzie et al., 2007). Additionally, most studies utilize convenience samples of highly stressed caregivers, such as those caring for individuals with dementia (Caswell, Vitaliano, Croyle, Scanlan, Zhang, & Daruwala, 2003; de Vugt, M. E., Jolles, J., Van Osch, L., Stevens, F., Aalten, P., Lousberg, R., & Verhey, F. R. 2006; Mackenzie et al., 2009; Mackenize et al., 2011; Vitaliano, Zhang, Young, Caswell, Scanlan, & Echeverria, 2009; Vitaliano, Murphy, Young, Echeverria, & Borson, 2011). While those providing support to individuals with dementia are an important subgroup, they represent only 22% of all informal caregivers (National Alliance for Caregiving, 2015). Only one large-scale prospective analysis has evaluated associations between caregiving and cognition (Lee, Kawachi, & Grodstein, 2004). This study, a secondary analysis of data from the Nurses Health, study suggested that caregiving is associated with poor cognitive outcomes.
In the current study, we build on the extant literature by using a large, population-based sample to evaluate longitudinally the extent to which non-custodial grandparent caregiving is related to cognitive function among older adults. Furthermore, we control for a wide array of potential confounding variables, including affect, that typically are not considered in the existing research, and we consider race/ethnicity differences in grandparent caregiving.
We are interested in the extent to which race moderates the association between grandparent caregiving and cognitive function. African-Americans are disproportionally represented as grandparent caregivers. While making up only 9.2% of the total U.S. population aged ≥60 years, African-Americans make up 21.4% of the grandparent caregiver population in this age group (U.S. Census Bureau, 2012). Most studies of African-American caregivers to date have been cross-sectional. Further, few have made direct comparisons between caregivers and non-caregivers or between African-Americans and Whites. Additionally, most studies of African-American grandparent caregiving have focused on custodial grandparents. The literature overwhelmingly suggests that African-American grandparents raising grandchildren face considerable challenges in taking on caregiving responsibilities. With respect to mental health, custodial grandparent caregiving has been linked to greater psychological distress (Kelley, Whitley, & Campos, 2013) and more depressive symptoms (Blustein, Chan, & Guanais, 2004). In the realm of physical health, the literature suggests that these grandparent caregivers report poorer self-rated health (Hughes, Waite, LaPierre, & Luo, 2007), more functional limitations (Hughes et al., 2007), and increased frailty (Chen et al., 2014). There is little data, however, on African-Americans who serve as non-custodial grandparent caregivers. Understanding racial differences in the effects of non-custodial grandparent caregiving may be particularly useful with respect to cognitive outcomes, as African-Americans consistently demonstrate lower levels of cognitive performance than Whites (Schwartz, Glass, Bolla, Stewart, Glass, Rasmussen, et al., 2004). Thus, identifying factors that may impact cognitive functioning may be particularly important in this group. In addition to race, we also evaluate the extent to which other demographic variables (age, sex, education, marital status) moderate the association between grandparent caregiving and cognitive functioning.
We address our questions using data from the Health and Retirement study (HRS), a population-based longitudinal panel survey of community dwelling U.S. adults aged >50 years. We limited the study sample to grandparents aged ≥65 years, as complete cognitive performance measures were not available for younger participants. Our study considered participant scores on 4 tests of cognitive function. We only included African-American and Whites in our sample, as sample sizes in other groups were too small for meaningful analyses. We also exclude included non-custodial grandparent caregivers who currently lived with their grandchildren. Due to the HRS design, these grandparents did not provide complete data on grandparent caregiving hours. Non-residential grandparent caregivers were compared to non-caregiving, non-residential grandparents at three waves over a 4-year follow-up period, controlling for baseline cognition scores, demographic characteristics, depressive symptoms, and baseline health status. We evaluated the relationship between grandparent caregiving and cognition by considering a) the total hours of grandparent caregiving across the three waves, b) the number of waves of grandparent caregiving, and c) the change in cognition over time according to total hours of grandparent caregiving across waves.
Methods
Participants and Procedure
Study participants were drawn from the 2006, 2008, and 2010 waves of the Health and Retirement Study, a population-based longitudinal panel survey of community dwelling U.S. older adults. The HRS sampling procedures and study design are available elsewhere (Heeringa & Connor, 1995). At each wave, participants completed an interview that included assessment of grandparent status, demographic characteristics, health status and cognitive function.
A total of 5787 White and African-American grandparents aged ≥65 years completed an HRS household interview in 2006. We excluded 767 participants who were not interviewed in 2008 either because they died prior to the interview (n=564) or because they were lost to follow-up (n=203). We excluded an additional 816 participants who were not interviewed in 2010 either because they died prior to the interview (n=646) or because they were lost-to follow-up (n=170). From there, we excluded 292 participants with missing grandparent caregiving or cognition data in 2006, 335 participants with missing grandparent caregiving or cognition data in 2008, and 352 participants with missing grandparent caregiving or cognition data in 2010. We also excluded 159 grandparents who reported living with their grandchildren at least once during the period. Finally, we excluded 37 participants who were missing data on at least one of our standard control variables. The final sample included 3029 individuals ages 65–96 (87.6% White, 12.4 % African-American, 83.6% female; mean age 73.82; SD 6.64).
Assessment of Grandparent and Caregiving Status
At all three waves, participants were asked about their household structure and family relationships. In cases where participants were from the same household (e.g. married/partnered couples), one household member was designated as the family respondent and provided data on behalf of the entire household. Participants were asked: “Altogether, how many grandchildren do you and your husband/wife/partner have?, “Did you (or your (late) [husband/wife/partner]) spend 100 or more hours in total in the last two years] taking care of [grand or great- grandchildren/grandchildren]?, and “Roughly how many hours altogether did you, yourself spend?” Participants provided data on all members of their household, (e.g. name, relationship to the participant, sex, and age). Based on this information, we determined if participants lived with grandchildren. We limited our analyses to only include one member of each household (i.e. the household respondent). We chose not to include proxy reports of grandparent caregiving, as they may be subject to larger reporting biases. Further, utilizing information from only one member of each household eliminated issues of interdependence between household members that could bias the results.
Participants were considered to be grandparent caregivers if they provided at least 100 hours of care for grandchildren in the past two years. Those who provided less care were considered to be noncaregiving grandparents. Grandparent caregivers were then asked to quantify their hours of care based on the following groupings pre-determined by HRS study staff: 100–199 hours, 200–499 hours, or 500 hours or more. We excluded participants who lived in the same households as their grandchildren during any of the waves, and subsequent analyses include only nonresidential grandparents.
Number of Waves of Grandparent Caregiving.
To approximate the length of time over which each participant acted as a grandparent caregiver, we determined the number of waves in which participants reported acting as grandparent caregivers at each of the three interviews. Possible values ranged from 0 to 3.
Total Hours of Grandparent Caregiving.
Response categories for the grandparent caregiving questions were 100–199 hours, 200–499 hours, and 500 hours or more. To compute total hours of grandparent caregiving across the 3 interview waves, midpoint values were assigned to represent each category. For those who were noncaregivers at a particular wave, a value of 0 was assigned. For the top category, a value of 500 was assigned. The assigned values were then summed across the waves, for possible values ranging from 0 to 1500.
Assessment of Cognitive Function
Several performance measures were used to ascertain cognitive function at each wave. These included measures of immediate word recall, delayed word recall, serial 7s, and mental status measures (Rodgers, Ofstedal, & Herzog, 2003). Detailed descriptions of these measures have been previously published (Ofstedal, Fisher, & Herzog, 2005). Below are brief descriptions of each measure. In addition to evaluating outcomes on each measure separately, we also created a total composite score of cognitive function ranging from 0 to 35 by summing the scores from each of these measures. The total composite score has been used in numerous epidemiological studies (Hung, Wisnivesky, Siu, & Ross, 2009; Karlamangla, Miller-Martinez, Aneshensel, Seeman, Wight, & Chodosh, 2009) and has demonstrated good internal consistency in prior work (Ofstedal, Fisher, & Herzog, 2005). Although the HRS uses a mixture of both telephone and face-to-face interviews to collect data on cognitive function, formal studies of the effects of mode of administration on cognitive measures suggest no significant differences in average cognitive scores for interviews based on mode of administration (Herzog & Wallace, 1999).
Immediate Word Recall.
To assess immediate word recall, participants were randomly assigned one of four possible lists of 10 nouns to recall. These lists did not overlap with respect to word content. Participants were assigned a different set of words at each wave, and no two participants in the same household were assigned the same word lists in the same or adjacent waves. There was only one trial per wave. Participants received one point for each correct word, for a possible score ranging from 0–10.
Delayed Word Recall.
After about 5 minutes of asking other survey questions, participants were asked to recall the 10 nouns that were used during the immediate recall task. Participants were not told ahead of time that they would need to recall the nouns used during the previous immediate recall task. Participants received one point for each correct word, for a possible score ranging from 0–10.
Serial 7s.
To evaluate working memory and mental processing, participants were asked to count backwards from 100s by 7s for five trials. Participants received one point for each correct response, with possible scores ranging from 0–5.
Mental Status Measures.
Participants were asked to count backwards from 20, name the U.S. president and vice president by last name, and name two objects based on a brief description. They were also asked to provide the date (month, day, year, and day of week). The possible score for these measures ranged from 0–10.
Standard Control Variables
The following variables were assessed at baseline and used as covariates in all analyses: baseline cognitive function (continuous), age (continuous), self-reported race (White or African-American), years of education (continuous), employment status (employed, not employed), marital status (never married, divorced, separated, widowed, married), sex (male, female), self-reported hearing and vision (excellent to poor on a 5-point scale), number of difficulties with activities of daily living (ADLs), number of difficulties with instrumental activities of daily living (IADLs), whether the participant served as a caregiver for a parent (yes/no) or a spouse/partner (yes/no), and self-reported history of diabetes, cancer, heart problems, stroke, or lung problems (yes/no). We also controlled for baseline depressive symptoms using an 8-item modified version of the Center for Epidemiologic Studies Depression Scale (CES-D; Wallace, Herzog, Ofstedal, Steffick, Fonda, & Langa, 2000). This scale asks participants to indicate (with yes/no responses) whether they experienced 8 types of feelings (e.g. felt depressed, had trouble concentrating, had thoughts about death) over the past week. Each “yes” response was assigned one point and responses were summed to generate a total score ranging from 0 to 8.
Finally, we also account for chronic diseases and/or functional limitations that develop during the follow-up period by controlling for the development of new chronic illnesses during the follow-up period (yes/no) and the development of new ADLs (yes/no) or IADLs (yes/no) during the follow-up period.
Statistical Analyses
Multiple linear regression was used to evaluate associations between a) the number of waves of grandparent caregiving and cognition at 4-year follow-up (2010) and b) the total hours of caregiving across the three waves and each cognition at 4-year follow-up (2010), adjusting for the standard control variables. Our outcomes included both the total cognition score at follow-up as well as scores on each individual cognitive test (e.g. immediate recall, delayed recall, serial 7s, mental status). Categorical variables were dummy coded. To determine if race and other demographic variables interacted with grandparent caregiving in predicting cognitive function at 4-year follow-up, we used first-order cross-product terms for the grandparent caregiving categories and each of these variables. Interaction terms were entered into individual regression equations with standard controls and the corresponding main effects.
We used a linear mixed model to evaluate the association between total hours of grandparent caregiving and total cognition scores over the follow-up period. Repeated total cognition scores in 2006, 2008, and 2010 were examined as dependent variables and the total hours of grandparent caregiving across the three waves were examined as predictors. The standard controls were included as time-invariant covariates. We specified an unstructured covariance structure (TYPE=UN) for estimation of intercept (average baseline total cognition score) and slope (total cognition score trajectory) values (between-person), and a first-order autoregressive error structure (AR1) to model autocorrelation between adjacent total cognition score measurements (within-person).
Results
Of the 3029 grandparents who participated in this study, 656 (21.6%) were grandparent caregivers at least once over the study period (Table 1). Among grandparent caregivers, 330 provided care at only one wave, 180 provided care over two study waves, and 146 provided care over all 3 study waves. The mean total number of caregiving hours per wave among all participants over the 3 study waves was 135.84 (SD 316.94). The mean total number of grandparent caregiving hours per wave among caregiving grandparents was 627.21 (SD 394.59)
Table 1.
Baseline Demographic and Health Characteristics of Study Participants
| Characteristic | Noncaregiving Grandparents (n=2373) |
Caregiving Grandparents (n=656) |
p value |
|---|---|---|---|
| Age (mean; SD) | 74.7 | 70.5 | <.0001 |
| % Female | 82.2 | 88.9 | <.0001 |
| Race | |||
| % White | 87.9 | 86.3 | |
| % African-American | 12.1 | 13.7 | 0.26 |
| Marital Status | |||
| % Married | 44.7 | 58.2 | <.0001 |
| % Separated | 0.9 | 1.1 | 0.75 |
| % Divorced | 13.0 | 13.4 | 0.77 |
| % Widowed | 40.9 | 26.5 | <.0001 |
| % Never Married | 0.5 | 0.8 | 0.44 |
| % Employed | 17.4 | 24.7 | <.0001 |
| Years of Education (mean; SD) | 12.4 (2.4) | 12.9 (2.5) | <.0001 |
| % With History of Stroke | 8.2 | 6.3 | 0.10 |
| % With History of Cancer | 17.6 | 14.8 | 0.09 |
| % With History of Heart Problems | 26.9 | 21.0 | 0.007 |
| % With History of Diabetes | 17.3 | 16.6 | 0.69 |
| % With History of Lung Disease | 10.4 | 9.6 | 0.55 |
| Baseline Immediate Recall Score; possible range 0 to 10 (mean; SD) | 5.39 (1.53) | 5.85 (1.56) | <.0001 |
| Baseline Delayed Recall Score; possible range 0 to 10 (mean; SD) | 4.27 (1.94) | 4.92 (1.91) | <.0001 |
| Baseline Serial Subtraction Score; possible range 0–5 (mean; SD) | 3.57 (1.59) | 3.78 (1.61) | .003 |
| Baseline Mental Status Score; possible range 0 to 10 (mean; SD) | 9.47 | 9.54 | .002 |
| Baseline Total Cognitive Score (mean; SD) | 22.7 (4.4) | 24.1 (4.4) | <.0001 |
| % with Difficulties with any IADLs at baseline | 31.9 | 38.2 | 0.03 |
| % With Difficulties with any ADLs at baseline | 17.3 | 11.3 | <.0001 |
| Baseline CES-D Score; possible range 0 to 8; (mean; SD) | 1.5 (1.9) | 1.2 (1.8) | 0.009 |
At baseline, the mean total cognition score among all study participants was 23.0 out of 35 (SD 4.43; Table 1). The mean baseline scores for immediate recall, delayed recall, serial 7 and mental status are in Table 1. The mean total cognitive score for study participants at two year-follow-up (2008) was 22.52 (SD 4.61) and at four year follow-up (2010) was 21.0 (SD 5.11).
The following standard control variables measured at baseline were related to lower total scores at 4-year follow-up when entered into the linear regression model together: increased age (B=−0.16; Beta=−0.21; p<.0001), more depressive symptoms (B=−0.08; Beta=−0.03; p=0.04), African-American race (B=−1.04; Beta=−0.07; p <.0001), and more limitations with instrumental activities of daily living (B=−0.38, Beta=−0.06; p <.0001).
The following variables were related to higher total cognition scores at 4-year follow-up in 2010: more years of education (B=0.24; Beta=0.12; p<.0001), higher baseline total cognition scores (B=0.57; Beta=0.49; p<.0001), and being currently employed (B=0.46; Beta=0.04; p=0.01). The other standard control variables were not related to total cognition scores at follow-up.
We were interested in whether grandparent caregiving was associated with cognition over a 4-year follow-up. To examine this, we considered the relationship between our cognitive measures and the number of waves of grandparent caregiving. We observed that the number of waves of grandparent caregiving was associated with higher total cognition scores at 4-year follow-up (B=0.23; Beta=0.04; p=.007). We were also interested in whether this effect was driven by scores on particular tests of cognitive function (Table 2). Test-specific analyses demonstrated that the number of waves of grandparent caregiving was associated with higher cognition when examining scores on the immediate recall (B=0.10; SE=.03; Beta=0.05; p=0.002) and delayed recall tests (B=0.08; SE=0.04; Beta=0.03; p=0.04). The number of waves of grandparent caregiving was not associated with scores on the serial 7s test (B=0.03; SE=0.03; Beta=0.02; p=0.27) or the mental status test (B=0.03; SE=0.03; Beta=0.02; p=0.22)
Table 2.
Linear Regression Models for Association Between Number of Waves of Grandparent Caregiving and Cognitive Measures at 4-Year Follow-Up
| Cognitive Measure |
B | SE | Beta | p value |
|---|---|---|---|---|
| Immediate Recall | .10 | .03 | .05 | .002 |
| Delayed Recall | .08 | .04 | .03 | .04 |
| Serial 7s | .03 | .03 | .02 | .27 |
| Mental Status | .03 | .03 | .02 | .22 |
| Total Cognition Score | .23 | .09 | .04 | .007 |
Each line represents a separate regression model.
Analyses adjust for age, race, education, baseline total cognition score, sex, marital status, employment status, difficulties with activities of daily living (ADLs), difficulties with instrumental activities of daily living (IADLs), baseline depressive symptoms, history of stroke, diabetes, heart problems, lung disease, and cancer.
We also evaluated the association between the mean total hours of grandparent caregiving across the three waves and cognition at 4-year follow-up. We observed that the mean total hours of grandparent caregiving across the three waves was associated with higher total cognition scores at follow-up (B=.001; Beta=.06; p=.002). Test-specific analyses demonstrated that the mean total hours of grandparent caregiving across the three waves was associated with higher cognition when examining scores on the immediate recall (Table 3; B=0.000; SE=.000; Beta=0.06; p=0.001) and delayed recall tests (Table 3; B=0.000; SE=0.0000; Beta=0.03; p=0.03). The mean total hours of grandparent caregiving was not associated with scores on the serial 7s test (Table 3; B=0.000; SE=0.000; Beta=0.02; p=0.13) or the mental status test (Table 3; B=0.000; SE=0.000; Beta=0.03; p=0.09)
Table 3.
Linear Regression Models for Association Between Total Grandparent Caregiving Hours Per Week Across Waves and Cognitive Measures
| Cognitive Measure |
B | SE | Beta | p value |
|---|---|---|---|---|
| Immediate Recall | .000 | .000 | .06 | .0001 |
| Delayed Recall | .000 | .000 | .03 | .03 |
| Serial 7s | .000 | .000 | .02 | .13 |
| Mental Status | .000 | .000 | .03 | .09 |
| Total Cognition Score | .001 | .000 | .04 | .002 |
Each line represents a separate regression model.
Analyses adjust for age, race, education, baseline total cognition score, sex, marital status, employment status, difficulties with activities of daily living (ADLs), difficulties with instrumental activities of daily living (IADLs), baseline depressive symptoms, history of stroke, diabetes, heart problems, lung disease, and cancer.
We used linear mixed models to evaluate the association between total grandparent caregiving hours over the period with cognitive trajectories. There was a significant interaction of total grandparent caregiving hours with time in predicting both immediate and delayed recall. Specifically, more hours spent providing care were associated with less decline in both immediate recall scores (Estimate: 0.000103; SE .00002; p<.00001) and delayed recall scores over time (Estimate: 0.000046; SE 0.00011; p<.00001). To illustrate these effects, we divided the total hours of grandparent caregiving into quartiles and calculated mean total cognition scores at each wave by quartiles (Figures 2 and 3).
Figure 2. Total Hours of Grandparent Caregiving Per Week Across Waves by Immediate Recall Scores Over Time.
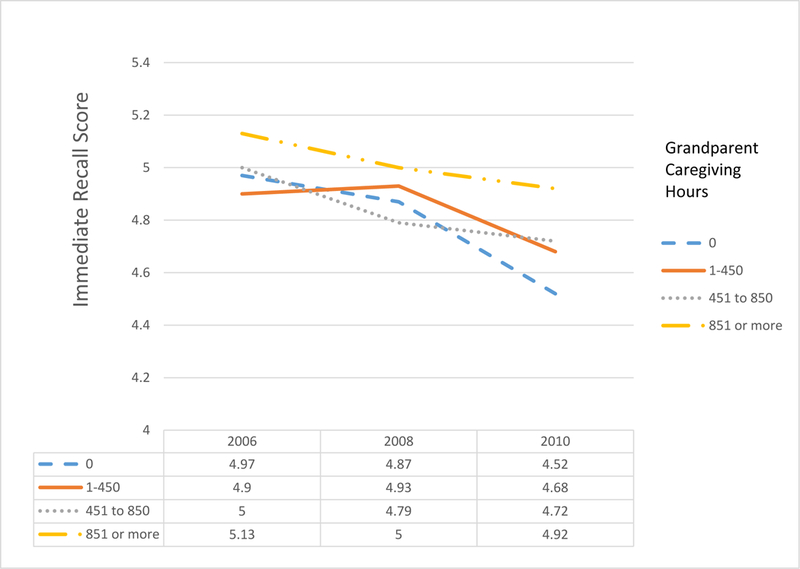
(Estimate: 0.000103; SE .00002; p<.00001)
Analyses adjust for age, race, education, baseline total cognition score, sex, marital status, employment status, difficulties with activities of daily living (ADLs), difficulties with instrumental activities of daily living (IADLs), baseline depressive symptoms, history of stroke, diabetes, heart problems, lung disease, and cancer.
Figure 3. Total Hours of Grandparent Caregiving Per Week Across Waves by Delayed Recall Scores Over Time.
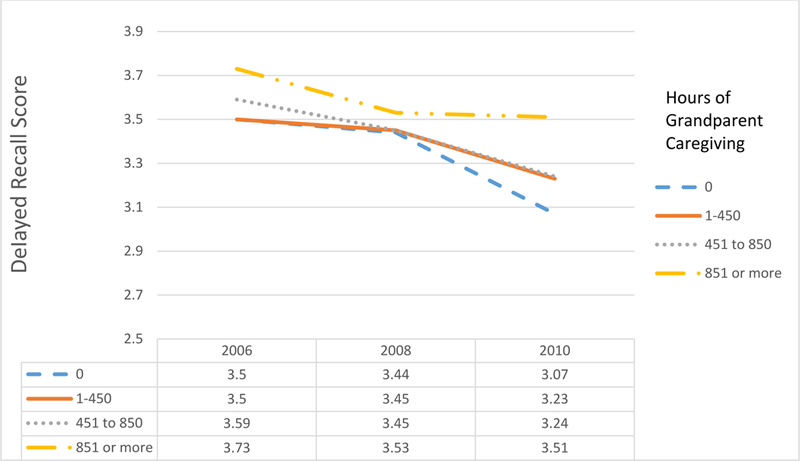
Analyses adjust for age, race, education, baseline total cognition score, sex, marital status, employment status, difficulties with activities of daily living (ADLs), difficulties with instrumental activities of daily living (IADLs), baseline depressive symptoms, history of stroke, diabetes, heart problems, lung disease, and cancer.
We also evaluated whether demographic characteristics moderated the association between grandparent caregiving and cognitive function. We observed a statistically significant interaction between number of waves of grandparent caregiving and race in predicting immediate recall scores at follow-up (B=−0.19; p=.04; Figure 1). Among Whites, the number of waves of grandparent caregiving was associated with higher immediate recall scores at 4-year follow-up (Figure 1; B=0.12; Beta=.06; p<.0001). White grandparents who provided care over all three study waves had higher immediate recall scores in 2010 than noncaregiving grandparents (mean 5.29 versus 4.96; p=.004). There was no difference in immediate recall scores among African-American based on waves of caregiving (B=−0.04; Beta=−0.02; p=0.71). There was no significant interaction between number of waves of grandparent caregiving and race in predicting scores on the delayed recall, serial 7s, or mental status measures.
Figure 1. Association of Number of Waves of Grandparent Caregiving with Immediate Recall Score at 4-Year Follow-up by Race.
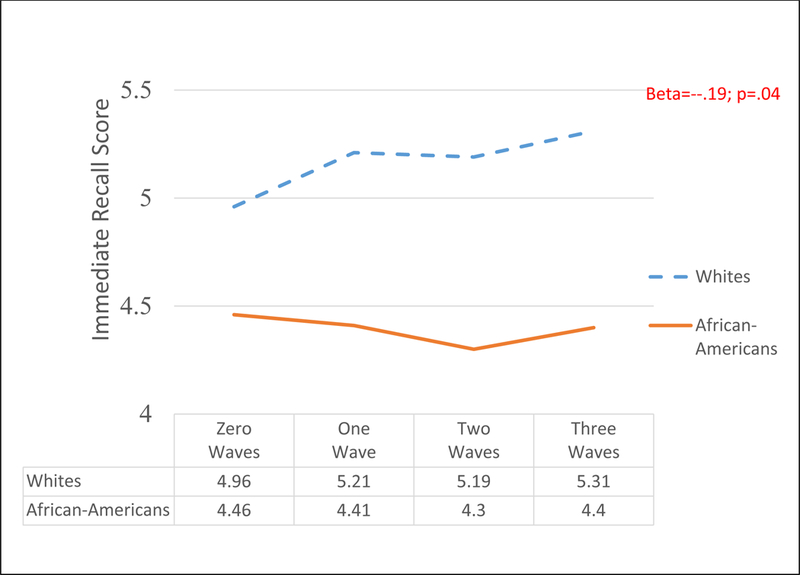
Analyses adjust for age, race, education, baseline immediate recall score, sex, marital status, employment status, difficulties with activities of daily living (ADLs), difficulties with instrumental activities of daily living (IADLs), baseline depressive symptoms, history of stroke, diabetes, heart problems, lung disease, and cancer.
There was no significant interaction between the total number of grandparent caregiving across the 3 waves and race in predicting either total cognition scores or any scores on the individual cognitive measures (i.e. immediate recall, delayed recall, serial 7s, mental status). We also observed no significant interactions between grandparent caregiving and other demographic variables (age, sex, marital status, education) in predicting cognitive function at follow-up.
Discussion
We observed that non-residential grandparent caregiving was positively associated with cognitive function over a 4-year follow-up in a population-based sample of older adults. We performed two types of analyses in this study. In the first, we evaluated associations between grandparent caregiving and cognitive scores at 4-year follow-up, adjusting for baseline scores. We observed that the number of waves of grandparent caregiving as well as the mean total hours of grandparent caregiving were both associated with higher immediate and delayed recall scores at follow-up. In the second type of analysis, we evaluated associations between the total hours of grandparent caregiving and cognitive trajectories across the three waves. Here, we observed that the total of hours of grandparent caregiving predicted change in immediate and delayed recall scores across the three waves. While all grandparents demonstrated an overall decline in these scores during the study period, caregiving grandparents showed slower rates of decline than non-caregiving grandparents. Further, declines were smallest among caregivers who provided more hours of care. Our analyses controlled for numerous demographic and health-related variables that might be related both to selection into caregiving and cognitive status. Further, our findings are consistent with previous studies link grandparent caregiving to higher cognitive function.
This study is also consistent with a broader literature linking family caregiving to positive outcomes. Although studies documenting the negative effects of caregiving have traditionally dominated the literature, these negative effects are not universal (Fredman et al., 2010; Pinquart & Sorensen, 2003; Pinquart & Sorensen, 2007; Schulz & Beach, 1999). More recent work suggests that the provision of support to others may convey health benefits, including decreased mortality risk (Fredman et al., 2010; O’Reilly, Connolly, Rosato, & Patterson, 2008). Our study supports this growing body of literature by demonstrating positive aspects of the grandparent caregiving experience.
We found that race moderated the association between grandparent caregiving and immediate recall, one of four cognitive tests utilized in our study. Specifically, we found that beneficial effects on immediate recall were observed among Whites but not African-Americans. There are several possible explanations for this difference. First, African-American and White grandparents may serve different roles as caregivers. Culturally, African-American families have strong traditions in which grandparents often serve as surrogate parents (Bertera & Crewe, 2013). African-American grandparents often assume a caregiving role due to parental need, frequently filling gaps that exist due to single parenthood or young parental age (Hunter, 1997). As a result, African-American grandparents are often expected to hold positions of authority and provide discipline and guidance (Kennedy, 1990). In contrast, White grandparents are often expected to occupy more companionate roles with their grandchildren, with more differences between the grandparenting and the parenting role (Kennedy, 1990). These differences in role expectations may cause African-American grandparents to experience caregiving as more of a stressor, which could have implications for immediate recall. In post hoc analyses, we evaluated differences in physical health status and depressive symptoms between White and African-American grandparent caregivers. While we observed no differences in the presence of chronic illnesses between the two groups, we found that African-American grandparent caregivers reported more depressive symptoms at baseline than White grandparent caregivers (mean score 1.68 versus 1.17; p=0.01.) This difference in psychological well-being may impact recall scores. Finally, White and African-American grandparents may also engage in different types of activities with their grandchildren or care for more children. We could not account for these differences in our analyses.
Overall, this study has many strengths. It uses a population-based sample to evaluate longitudinally the association between grandparent caregiving and cognition. Further, it uses a large sample of Whites and African-Americans It is also one of few studies to formally evaluate racial differences in cognitive outcomes among grandparent caregivers. Finally, it provides data on non-residential grandparents, a group often neglected in the grandparent caregiving literature.
This study does have some limitations. It is possible that the effects observed in our study are spurious findings that reflect unmeasured confounding health-related variables. The healthy caregiver hypothesis suggests that caregivers may have better health outcomes than non-caregivers because individuals with better health status differentially select into the caregiver role, and that being a caregiver may help to preserve caregiver health (Fredman, Cauley, Satterfield, Simonsick, Spencer, Ayonayon, & Harris, 2008). While we controlled for a number of health-related factors measured at baseline, it is possible that some other unmeasured markers of health may confound the associations we observe between grandparent caregiving and cognition. Future studies might use more robust methods to address these issues. For example, propensity-based analyses have been used in studies of family caregiving to match caregivers with non-caregivers using propensity scores that balance the two groups on a range of potential confounding factors (Roth, Haley, Hovater, Perkins, Wadley, & Judd, 2013). Future studies should consider such strategies.
Our measurement of grandparent caregiving may also be subject to recall bias, as participants were asked to retrospectively evaluate the hours of care that they provided. Some studies of dementia caregiving suggest that self-report measures of time may be unreliable over long time periods, particularly when the caregiving role is stressful (Jarrott, Zaritt, & Stevens, 2000). In such instances, more stress may be associated with greater time estimates. Given that more time was associated with better outcomes in our study, a positive correlation between grandparent caregiving time and stress is less plausible. There is still, however, the potential for recall bias here. We also had no basic information on the nature of the grandparent caregiving experience among participants. Information on grandchildren’s ages, the number of grandchildren receiving care, and the type of caregiving activities were beyond the scope of this dataset. Thus, explanations for our findings are mostly speculative. Additionally, the HRS was designed such that one member of each household was designated as the family respondent, and only this person answered questions about grandparent caregiving. Thus, our study sample was overwhelmingly female, as male household members were much less likely to act as the HRS family respondent. Further, this study does not evaluate the precise mechanisms linking grandparent caregiving to cognitive function. Several studies suggest that psychological distress can have a negative impact on cognitive functioning; however, positive psychological variables may also be linked to cognition. A few studies have linked self-efficacy (belief in one’s own capability to achieve a desired outcome) to reduced cognitive decline (Albert, Jones, Savage, Berkman, Seeman, Blazer, et al. 1995; Seeman, McAvay, Merrill, Albert, & Rodin, 1996). The feelings of reward, generativity, and accomplishment that grandparents may experience as a result of caregiving may promote psychological well-being in ways that positively impact cognition. Future studies should address the role of positive psychological variables in mediating the effects of grandparent caregiving on cognition. Finally, the effects observed in our study are small, likely due to the brief time period over which we examined our outcomes. Cognitively decline is a gradual process that requires long periods of observation. Future studies should evaluate associations between grandparent caregiving and cognitive trajectories over longer periods of time.
This study has some important implications. Eighty-three percent of all U.S. adults aged ≥65 years are grandparents (Pew Research Center, 2015). Further, cognitive decline is an issue of significant public health concern in the United States, and increased age is its single greatest risk factor. Although our effect sizes are small, our findings are consistent with other studies of grandparent caregiving and cognition drawn from cross-sectional and convenience samples.
Our findings are consistent with cognitive enrichment theory, which proposes that engagement in beneficial intellectual, physical, and social activities promotes successful cognitive aging (Hertzog, Kramer, and Lindenberger, 2009). Numerous empirical studies have tested this hypothesis, and the literature suggests that an individual’s activities and behaviors can both slow the rates of cognitive aging and improve cognitive function in late life. For example, several prospective studies have demonstrated that higher engagement in activities that are mentally stimulating (e.g. reading, writing for pleasure, playing musical instruments; (Wilson, Scherr, Schneider, Li, & Bennett,2007), physically active (Weuve, Kang, Manson, Breteler, Ware, & Grodstein, 2004), and/or involve social interaction (e.g. going to museums, visiting friends, attending religious services; Barnes, De Leon, Wilson, Bienias, & Evans, 2004; Lovden, Ghisletta, & Lindenberger, 2005) is associated with reduced cognitive decline and lower dementia risk. Our study suggests that non-custodial grandparent caregiving may help to promote successful cognitive aging among older adults in a similar fashion.
References
- Albert MS, Jones K, Savage CR, Berkman L, Seeman T, Blazer D, et al. (1995). Predictors of cognitive change in older persons. MacArthur Studies of Successful Aging. Psychology & Aging, 10, 578–589. [DOI] [PubMed] [Google Scholar]
- Albert R, (2000). Legal issues for custodial grandparents In Hayslip B & Goldberg-Glen R (Eds.), Grandparents raising grandchildren: Theoretical, empirical, and clinical perspectives (pp. 327–340). New York: Springer. [Google Scholar]
- Andrews-Hanna JR, Snyder AZ, Vincent JL, Lustig C, Head D, Raichle ME, & Buckner RL (2007). Disruption of large-scale systems in advanced aging. Neuron, 56, 924–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpino B, & Bordone V (2014). Does Grandparenting Pay Off? The Effect of Child Care on Grandparents’ Cognitive Functioning. Journal of Marriage and Family, 76, 337–351. [Google Scholar]
- Barnes LL, De Leon CM, Wilson RS, Bienias JL, & Evans DA (2004). Social resources and cognitive decline in a population of older African Americans and whites. Neurology, 63, 2322–2326. [DOI] [PubMed] [Google Scholar]
- Bassuk SS, Glass TA, & Berkman LF (1999). Social disengagement and incident cognitive decline in community-dwelling elderly persons. Annals of Internal Medicine, 131, 165–173. [DOI] [PubMed] [Google Scholar]
- Bertera EM, & Crewe SE (2013). Parenthood in the twenty-first century: African American grandparents as surrogate parents. Journal of Human Behavior in the Social Environment, 23, 178–192. [Google Scholar]
- Bertrand RM, Saczynski JS, Mezzacappa C, Hulse M, Ensrud K, & Fredman L (2012). Caregiving and cognitive function in older women: Evidence for the healthy caregiver hypothesis. Journal of Aging and Health, 24, 48–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blustein J, Chan S, & Guanais FC (2004). Elevated depressive symptoms among caregiving grandparents. Health Services Research, 39, 1671–1689. doi: 10.1111/j.1475-6773.2004.00312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S, Cohon D, & Wheeler R (2002). African American extended families and kinship care: how relevant is the foster care model for kinship care?. Children and Youth Services Review, 24, 53–77. [Google Scholar]
- Burn KF, Henderson VW, Ames D, Dennerstein L, & Szoeke C (2014). Role of grandparenting in postmenopausal women’s cognitive health: results from the Women’s Healthy Aging Project. Menopause, 21, 1069–1074. [DOI] [PubMed] [Google Scholar]
- Burton LM, Dilworth-Anderson P (1991). The intergenerational roles of aged black Americans. Marriage and Family Review, 16, 311–330. [Google Scholar]
- Carlson MC, Hasher L, Zacks RT, Connelly SL (1995). Aging, distraction, and the benefits of predictable location. Psychology and Aging, 10, 427–36. [DOI] [PubMed] [Google Scholar]
- Carlson MC, Erickson KI, Kramer AF, Voss MW, Bolea N, Mielke M, … & Fried LP (2009). Evidence for neurocognitive plasticity in at-risk older adults: the experience corps program. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, glp117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson MC, Saczynski JS, Rebok GW, Seeman T, Glass TA, McGill S, … & Fried LP (2008). Exploring the effects of an “everyday” activity program on executive function and memory in older adults: Experience Corps®. The Gerontologist, 48, 793–801. [DOI] [PubMed] [Google Scholar]
- Caswell LW, Vitaliano PP, Croyle KL, Scanlan JM, Zhang J, & Daruwala A (2003). Negative associations of chronic stress and cognitive performance in older adult spouse caregivers. Experimental Aging Research,29, 303–318. [DOI] [PubMed] [Google Scholar]
- Chen F, Mair CA, Bao L, & Yang YC (2015). Race/Ethnic Differentials in the Health Consequences of Caring for Grandchildren for Grandparents. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 70, 793–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F, & Liu G (2012). The health implications of grandparents caring for grandchildren in China. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 67, 99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vugt ME, Jolles J, Van Osch L, Stevens F, Aalten P, Lousberg R, & Verhey FR (2006). Cognitive functioning in spousal caregivers of dementia patients: findings from the prospective MAASBED study. Age and Ageing, 35, 160–166. [DOI] [PubMed] [Google Scholar]
- Erikson EH (1963). Childhood and society. New York: W. W. Norton & Company. [Google Scholar]
- Erikson EH (1982). The life cycle completed: A review. New York: W. W. Norton & Company. [Google Scholar]
- Fredman L, Cauley JA, Satterfield S, Simonsick E, Spencer SM, Ayonayon HN, & Harris TB (2008). Caregiving, mortality, and mobility decline: The health, aging, and body composition (Health ABC) study. Archives of Internal Medicine, 168, 2154–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman L, Cauley JA, Hochberg M, Ensrud KE, & Doros G (2010). Mortality Associated with Caregiving, General Stress, and Caregiving‐Related Stress in Elderly Women: Results of Caregiver‐Study of Osteoporotic Fractures. Journal of the American Geriatrics Society, 58, 937–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter AG (1997). Counting on grandmothers: Black mothers’ and fathers’ reliance on grandmothers for parenting support. Journal of Family Issues, 18, 251–269. [Google Scholar]
- Goode WJ (1960). A theory of role strain. American Sociological Review, 483–496. [Google Scholar]
- Hayslip B, & Kaminski PL (2005). Grandparents raising their grandchildren: A review of the literature and suggestions for practice. the Gerontologist, 45(2), 262–269. [DOI] [PubMed] [Google Scholar]
- Herrera AP, Mendez-Luck CA, Crist JD, Smith ML, Warre R, Ory MG, & Markides K (2013). Psychosocial and cognitive health differences by caregiver status among older Mexican Americans. Community Mental Health Journal, 49, 61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa SG, & Connor J (1995). Technical description of the Health and Retirement Study sample design. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/HRSSAMP.pdf
- Herzog AR, & Rodgers WL (1999). Cognitive performance measures in survey research on older adults In Schwarz N, Park DC, Knauper B, & Sudman S (Eds.), Cognition, aging, and self-reports. Philadelphia: Psychology Press. [Google Scholar]
- Hilbrand S, Coall DA, Gerstorf D, & Hertwig R (2017). Caregiving within and beyond the family is associated with lower mortality for the caregiver: A prospective study. Evolution and Human Behavior, 38, 397–403. [Google Scholar]
- Holtzman RE, Rebok GW, Saczynski JS, Kouzis AC, Doyle KW, & Eaton WW (2004). Social network characteristics and cognition in middle-aged and older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 59, P278–P284. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, LaPierre TA, & Luo Y (2007). All in the family: The impact of caring for grandchildren on grandparents’ health. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62, S108–S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung WW, Wisnivesky JP, Siu AL, & Ross JS (2009). Cognitive decline among patients with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 180(2), 134–137. [DOI] [PubMed] [Google Scholar]
- Jarrott SE, Zarit SH, Stephens MAP, Townsend AL, & Greene R (2000). Effects of adult day service programs on time usage by employed and non-employed caregivers. Journal of Applied Gerontology, 19, 371–388. [Google Scholar]
- Kelley SJ, Whitley DM, & Campos PE (2013). Psychological distress in African American grandmothers raising grandchildren: The contribution of child behavior problems, physical health, and family resources. Research in Nursing and Health, 36, 373–385. doi: 10.1002/nur.21542. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Miller-Martinez D, Aneshensel CS, Seeman TE, Wight RG, & Chodosh J (2009). Trajectories of cognitive function in late life in the United States: demographic and socioeconomic predictors. American Journal of Epidemiology, 331–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy GE (1990). College students’ expectations of grandparent and grandchild role behaviors. The Gerontologist, 30, 43–48. [DOI] [PubMed] [Google Scholar]
- Lee S, Colditz G, Berkman L, & Kawachi I (2003). Caregiving to children and grandchildren and risk of coronary heart disease in women.American Journal of Public Health, 93(11), 1939–1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Kawachi I, & Grodstein F (2004). Does caregiving stress affect cognitive function in older women?. The Journal of Nervous and Mental Disease, 192, 51–57. [DOI] [PubMed] [Google Scholar]
- Lum TY, & Lightfoot E (2005). The effects of volunteering on the physical and mental health of older people. Research on Aging, 27, 31–55. [Google Scholar]
- Luoh M, & Herzog AR (2002). Individual consequences of volunteer and paid work in old age: Health and mortality. Journal of Health and Social Behavior, 43, 490–509. [PubMed] [Google Scholar]
- Mackenzie CS, Wiprzycka UJ, Hasher L, & Goldstein D (2009). Associations between psychological distress, learning, and memory in spouse caregivers of older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 64(6), 742–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, & Fuller-Thomson E (1999). The health of grandparents raising grandchildren: results of a national study. American Journal of Public Health,89, 1384–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, & Fuller-Thomson E (2005). African American grandparents raising grandchildren: A national study using the Census 2000 American Community Survey. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60, S82–S92. [DOI] [PubMed] [Google Scholar]
- Minkler M, Fuller-Thomson E, Miller D, & Driver D (1997). Depression in grandparents raising grandchildren: Results of a national longitudinal study. Archives of Family Medicine, 6, 445–452. [DOI] [PubMed] [Google Scholar]
- Musick MA, Herzog AR, & House JS (1999). Volunteering and mortality among older adults: Findings from a national sample. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54, S173–S180. [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving (2015). Caregiving in the U.S. Retrieved from http://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf
- Odulana J, Camblin LD, & White P (1996). Cultural roles and health status of contemporary African American young grandmothers. The Journal of Multicultural Nursing and Health, 2, 28–35. [Google Scholar]
- Ofstedal MB, Fisher GG, & Herzog AR (2005). Documentation of cognitive functioning measures in the health and retirement study HRS/AHEAD Documentation Report DR- 006. Available through the Survey Research Center at the Institute for Social Research, University of Michigan; Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-006.pdf [Google Scholar]
- Park DC, Lautenschlager G, Hedden T, Davidson NS, Smith AD, & Smith PK (2002). Models of visuospatial and verbal memory across the adult life span. Psychology and Aging, 17, 299–320. [PubMed] [Google Scholar]
- Pew Research Center (2015). Family Support in Graying Societies How Americans, Germans and Italians Are Coping with an Aging Population. Retrieved from http://www.pewsocialtrends.org/2015/05/21/family-support-in-graying-societies/
- Pinquart M, & Sörensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychology and Aging, 18, 250–267. [DOI] [PubMed] [Google Scholar]
- Raz N (2000). Aging of the brain and its impact on cognitive performance: Integration of structural and functional findings In Craik FIM & Salthouse TA (Eds.), Handbook of aging and cognition (2nd ed., pp. 1–90). Mahwah, NJ: Erlbaum. [Google Scholar]
- Rodgers WL, Ofstedal MB, & Herzog AR (2003). Trends in scores on tests of cognitive ability in the elderly U.S. population, 1993–2000. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58, S338–S346. [DOI] [PubMed] [Google Scholar]
- Roth DL, Haley WE, Hovater M, Perkins M, Wadley VG, & Judd S (2013). Familycaregiving and all-cause mortality: findings from a population-based propensity-matched analysis. American Journal of Epidemiology, 178, 1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA, Fristoe NM, Lineweaver TT, Coon VE (1995). Aging of attention: does the ability to divide decline? Memory & Cognition, 23, 59–71. [DOI] [PubMed] [Google Scholar]
- Salthouse TA (1996). The processing-speed theory of adult age differences in cognition. Psychological Review, 103, 403–428. [DOI] [PubMed] [Google Scholar]
- Schulz R, & Beach SR (1999). Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. Journal of the American Medical Association, 282, 2215–2219. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Cook TB, Martire LM, Tomlinson JM, & Monin JK (2012). Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging & Mental Health, 16, 712–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz BS, Glass TA, Bolla KI, Stewart WF, Glass G, Rasmussen M, … & Bandeen-Roche K (2004). Disparities in cognitive functioning by race/ethnicity in the Baltimore Memory Study. Environmental Health Perspectives, 112, 314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, McAvay G, Merrill S, Albert M, & Rodin J (1996). Self-efficacy beliefs and changes in cognitive performance: MacArthur Studies of Successful Aging. Psychology and Aging, 11, 538–551. [DOI] [PubMed] [Google Scholar]
- Shipley BA, Der G, Taylor MD, & Deary IJ (2006). Cognition and all-cause mortality across the entire adult age range: health and lifestyle survey. Psychosomatic Medicine, 68, 17–24. [DOI] [PubMed] [Google Scholar]
- Snarey JR (1993). How fathers care for the next generation: A four-decade study. Harvard University Press. [Google Scholar]
- Stryker S, & Burke PJ (2000). The past, present, and future of an identity theory. Social Psychology Quarterly, 284–297. [Google Scholar]
- U.S. Census Bureau (2012). American Community Survey. [Google Scholar]
- Vitaliano PP, Zhang J, Young HM, Caswell LW, Scanlan JM, & Echeverria D (2009). Depressed mood mediates decline in cognitive processing speed in caregivers. The Gerontologist, 49, 12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Murphy M, Young HM, Echeverria D, & Borson S (2011). Does caring for a spouse with dementia promote cognitive decline? A hypothesis and proposed mechanisms. Journal of the American Geriatrics Society, 59, 900–908. [DOI] [PubMed] [Google Scholar]
- Wallace RB, Herzog AR, Ofstedal MB, Steffick D, Fonda S, & Langa K (2000). Documentation of Affective Functioning Measures in the Health and Retirement Study. Available through the Survey Research Center at the Institute for Social Research, University of Michigan; Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf [Google Scholar]
- Wilson RS, Arnold SE, Schneider JA, Kelly JF, Tang Y, & Bennett DA (2006). Chronic psychological distress and risk of Alzheimer’s disease in old age. Neuroepidemiology, 27, 143–153. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Arnold SE, Schneider JA, Li Y, & Bennett DA (2007). Chronic distress, age-related neuropathology, and late life dementia. Psychosomatic Medicine, 69, 47–53. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. (2007). Loneliness and risk of Alzheimer’s disease. Archives of General Psychiatry, 64, 234–240. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Schneider JA, Boyle PA, Arnold SE, Tang Y, & Bennett DA (2007). Chronic distress and incidence of mild cognitive impairment. Neurology, 68, 2085–2092. [DOI] [PubMed] [Google Scholar]


