Abstract
Men’s satisfaction and sexual function is influenced by discomfort over genital size which leads to seek surgical and non-surgical solutions for penis alteration. In this article we report the results of a retrospective study of 355 cases of cosmetic elongation, enlargement and combined elongation and enlargement phalloplasty. We found a significant improvement in length at rest, stretched length and circumference at rest at 2, 6 and 12 months post-surgical procedure (all p < 0.0001). 5-item International Index of Erectile Function (IIEF-5) was also increased at 12 months post-surgery compared to baseline (p < 0.0001). This was consistent with an IIEF-5 improvement of 6.74% compared to baseline. This study is clinically relevant due to the large cohort of patients included and because it is the first study to use an inverse periosteal-fascial suture not described previously as part of the surgical methodology.
Subject terms: Anatomy, Testis
Introduction
Male genital image is correlated, albeit not in a necessarily linear manner1, to overall body image, psychosocial variables and sexual health2; in turn, sexual health is correlated to genital image3. Concern over genital endowment has archaic roots4,5. It typically emerges during adolescence6,7 and is triggered more by comparison among men than by the fear of not satisfying the partner8. Discomfort over genital size can influence satisfaction and man’s sexual function and push him to look for surgical and non-surgical solutions for penis alteration. We present a retrospective study of 355 cases of phalloplasty performed between 2012 and 2014.
Penile size
The remarkable differences in the penile measurements reported by various authors can be explained by the methodological differences and the variety of the characteristics, even ethnic, of the populations studied (Tables 1 and 2). Furthermore, these measurements were rarely conducted on statistically adequate samples. The availability of regulatory data per defined population would be essential not only for diagnostic and therapeutic purposes, but also to reassure patients who display feelings of inadequacy1,7,9,10 and to manufacture correctly sized prophylactics11. Penis size is an anthropometric measurement12 and is correlated to anthropometric measurements such as height, weight and body mass index (BMI)12,13. These measurements are intercorrelated13 and they are polygenic traits subject to multifactorial influences14.
Table 1.
Global published data of mean penile size (excluding self-reported measurements).
| First author, year | Country | N | Age (years; range) | FPL (cm) | SPL (cm) | EPL (cm) | FPG (cm) | EPG (cm) |
|---|---|---|---|---|---|---|---|---|
| Loeb, 189950 | Germany | 50 | 17–35 | 9.41 | ||||
| Schonfeld, 194251 | USA | 71 | 18–19 | 13.11 | 8.50 | |||
| 54 | 20–25 | 13.02 | ||||||
| Kinsey, 194852 | USA | 2,770 | 20–59 | 9.07 | 15.05 | |||
| Aimani, 198553 | Nigeria | 320 | 17–23 | 8.16 | 8.83 | |||
| Bondil, 199254 | France | 905 | 17–91 | 10.07 | 16.74 | |||
| Da Ros, 199455 | Brasil | 150 | 14.05 | 11.92 proximal 11.05 distal | ||||
| Wessells, 19969 | USA | 80 | 21–82 | 8.85 | 12.45 | 12.89 | 9.71 | 12.3 |
| Smith, 199856 | Australia | 184 | 15.71 | |||||
| Chen, 200057 | Israel | 55 | 21–78 | 8.03 | 12.05 | 13.06 | ||
| Ponchietti, 200112 | Italy | 3,300 | 17–19 | 9.0 | 12.5 | 10.0 | ||
| Schneider, 200111 | Germany | 111 | 18–19 | 8.60 | 14.48 | 9.68 | ||
| 32 | 40–68 | 9.22 | 14.48 | 9.02 | ||||
| Sengezer, 200258 | Turkey | 200 | 20–22 | 8.98 | ||||
| Shah, 200259 | UK | 104 | 17–84 | 13.0 | ||||
| Spyropoulos, 200260 | Greece | 52 | 19–38 | 12.18 | ||||
| Son, 200361 | Korea | 123 | 19–27 | 6.9 | 9.6 | 8.5 | ||
| Savoie, 200362 | USA | 124 | 59.1 (avg.) | 9.0 | 13.0 | |||
| Pereira, 200463 | Portugal | 498 | 20:26 | 9.85 | 15.14 | 9.39 | ||
| Awwad, 200564 | Jordan | 271 | 17–83 | 9.3 | 13.5 | 8.98 | ||
| 109 | 22–68 | 7.7 | 11.6 | 11.8 | ||||
| Mehraban, 200726 | Iran | 92 | 20–40 | 11.58 | 8.66 | |||
| Promodu, 200713 | India | 500 | 18–60 | 8.21 | 10.88 | 13.01 | 9.14 | |
| Kamel, 200965 | Egypt | 949 | 12.9 | 8.9 | ||||
| 78 | 11.2 | 8.8 | ||||||
| Nasar, 201114 | Egypt | 1,000 | 8.37 | 13.77 | 10.48 | |||
| Khan, 201223 | Scotland | 609 | 16–90 | 10.2 | 14.3 | |||
| Söylemez, 201266 | Turkey | 2,276 | 18–39 | 8.95 | 13.98 | 8.89 | ||
| Chen, 201467 | China | 5,196 | 6.5 | 12.9 | 8.0 | |||
| 311≈ | 12.9 | 10.5 | ||||||
| Shalabi, 201568 | Egypt | 2,000 | 22–40 | 13.84 | ||||
| Veale, 201569 | UK | 15,521 | 17–91 | 9.16 | 13.12 | 9.31 | 11.66 | |
| Habous, 201570 | Saudi Arabia | 778 | 20–82 | 12.53/14.34 | 11.50 | |||
| Salama, 201671 | Egypt | 239 | 7.4 | 11.8 | 8.7 | 11.3 | ||
| Hussein, 201772 | Afghanistan | 223 | 9.8 | 12.6 |
FPL = Flaccid Penile Length; SPL = Stretched Penile Length; EPL = Erect Penile Length; FPG = Flaccid Penile Girth; EPG = Erect Penile Girth; (avg.) = average.
Table 2.
Global published data of mean penile size (self-reported measurements only).
| First author, year | Country | N | Age (range) | FPL (cm) | SPL (cm) | EPL (cm) | FPG (cm) | EPG (cm) |
|---|---|---|---|---|---|---|---|---|
| Richters, 199573 | Australia | 156 | 15.99 | |||||
| Bogaert, 199974 | USA | 935 | 30 (avg.) | 10.41 | 16.4 | 16.4 | 9.65 | 12.57 |
| 4,187 | 30 (avg.) | 9.83 | 15.6 | 9.40 | 12.19 | |||
| Harding, 200275 | UK | 312 | 15.25 | 12.55 | ||||
| Schaeer, 201276 | Middle East | 804 | 15.6 | |||||
| Herbenick, 201377 | USA | 1,661 | 17–91 | 14.15 | 12.23 | |||
| Shaeer, 201378 | USA | 1,133 | 52.38 (avg.) | 13.1 | 15.6 | 16.3 | 10.6 |
FPL = Flaccid Penile Length; SPL = Stretched Penile Length; EPL = Erect Penile Length; FPG = Flaccid Penile Girth; EPG = Erect Penile Girth; (avg.) = average.
Materials and Methods
All methods and procedures were carried out in accordance with the principles contained in the Declaration of Helsinki.
Patients
This study was registered on 04/04/2017 (ISRCTN number: ISRCTN60774878). 355 men participated in this retrospective clinical study. They came to our centre in Milan (Italy) for a cosmetic phalloplasty between 2012 and 2014 [cosmetic elongation (21), enlargement (33) and combined elongation and enlargement (301)]. The patients’ medical history was gathered and they underwent a medical examination that included an objective examination of the external genitals and the prostate, routine blood tests, basal penile ultrasound scan to verify the presence of nodules, plaques or lesions in the internal tissues of the penis and measurement of the length and circumference of the penis at rest (flaccid) and stretched. The stretched penis length (SPL) is considered a trustworthy approximation of the penis length during erection1. The 5-item International Index of Erectile Function (IIEF-5) is a validated diagnostic test that we administered to all the patients included in this study. All patients signed the informed consent to undergo the procedure and for the video to be published.
Measurement was always performed in the same room, by the same operator and using the same flexible measure after a brief introductory interview, performed to put the patient at ease. The measurement was performed before the ultrasound scan to avoid variations caused by changes in temperature. The measurement of the length was performed according to Mondaini et al.7. The length of the penis is defined as the linear distance along the dorsal side of the penis between the pubo-penile junction and the tip of the glans, either in the flaccid or stretched states. The circumference of the penis was measured at rest at mid-shaft. In all cases we found that the measurements were coherent with the morphometric values of reference of adult men according to Wessels and Ponchietti9,12 and this information was shared with the patients. After measuring height and weight using methods routinely employed in the clinical setting, the general medical examination continued with an in-depth interview conducted in order to investigate the patients’ motivations and expectations, discuss the foreseen method and the results and provide in-depth answers to the patients’ questions. A meeting between the patients and the anaesthetist occurred separately. At the end of the general examination, patients received instructions to be followed the night before and the morning prior to the surgical operation. In addition, we gave our availability to answer the patients’ questions at any time until the procedure took place. The information summarised in Table 3 was also discussed with all the patients during the general medical examination.
Table 3.
Information regarding the phalloplasty discussed with the patients during their general examination.
| Elements discussed by the physician with the patients during the general medical examination |
|---|
| (a) The estimated results given by our centre (+1.5–4.0 length, +20–35% circumference) refer to an increase between a minimum and maximum obtained from a historic average of all the patients operated both for elongation and enlargement. The availability of a vast collection of pre- and post-surgical photographs shown during the general examination confirmed such variability; |
| (b) it is possible that an increase cannot be achieved following the procedure and the achievable increase in each case can only be partially foreseen and depends on 1) the consistency and especially the depth of the suspensory ligament which can be overall evaluated sonographically (evaluation of the penopubic space superficially) concerning the elongation of the penis; 2) subjective variables such as metabolism and lifestyle which can increase or accelerate the reabsorption of the implanted fat concerning the enlargement of the penis; |
| (c) the increase acquired in terms of length is markedly more visible in conditions of flaccidity than in erection, with a ratio of about 3:1; |
| (d) occasionally, implanted fat can be subject to excessive reabsorption during the first three months after surgery and, in that case, if the patient wishes, a new definite transplant can be performed; |
| (e) in enlargement phalloplasty, the different consistency between the fat and the cavernous bodies causes a change in the tactile consistency of the penis; along the shaft, such change is progressive so that no “steps” are felt, and there is no variation in the quality of the erection or local sensitivity; |
| (f) after an elongation procedure, a slight change in the angle of erection can occur, more marked if the increase is significant (10–15 degrees); |
| (g) exceptionally, nodularity can occur in the implanted fat; such nodularity is, however, transitory and almost always resolves spontaneously. |
The cosmetic phalloplasty candidate is a healthy and potent man with no congenital or acquired abnormalities or urogenital diseases. In this study, exclusion criteria were:
coagulopathies, cardiopathies, neoplasies, chemo-radiotherapy, infections in progress, prior pelvic surgeries for urogenital conditions or trauma, severe systemic conditions and psychiatric conditions;
unrealistic expectations; patients who requested results superior to those declared by the centre or who felt entitled to obtain the maximum penile increase within our historic series were excluded;
revision surgery; patients requesting a re-operation because of the failure of a previous cosmetic phalloplasty were excluded;
true hypoplasia (micropenis) defined as length <2.5 percentile points according to Mondaini6 (these patients were referred to an andrology centre);
significant anxiety, distorted body image, a history of suicidal thoughts and/or attempted suicide linked to presumed genital inadequacy with psychogenic sexual dysfunction.
In line with data shown in the literature2,5,7, penis dimensions at rest were the most critical (78%) for patients but the circumference of the penis was more determinant than length (69%). This may depend, at least in part, on the concept that enlargement phalloplasty is less invasive than lengthening phalloplasty. The desire to increase both dimensions was the most frequent (82%); in many cases it was conditioned by the fear of losing the right penile proportions by intervening in only one aspect (66%) and it was probably facilitated by the advantages in terms of down-time connected with performing the two procedures simultaneously. The time that elapsed between the first examination and the surgical procedure was 2–6 months. Among the motivations for seeking this surgical procedure, the most frequently cited by patients were psychological discomfort in homosocial situations, discomfort towards women – almost always linked to one or more devaluing observations made during intimacy, the desire to “dazzle” women, the well-founded perception that genital size was incoherent with their body, the desire to improve an already generous natural endowment for narcissistic or professional reasons, the desire for better correlation or proportions between dimensions at rest and during erection and between length and girth and the desire to move from the lowest limits of the normal range towards the morphometric median. The most common concerns relative to the operation, which coincided with the patient’s expectations from the procedure, were: (a) the surgery being imperceptible (b) the preservation of the quality of erection and local sensitivity, (c) achievement of the mathematical average of the declared results, in terms of penis length and/or of the circumference and (d) the results being aesthetically impeccable.
Anaesthesia
The choice of anaesthesia for cosmetic phalloplasty must be in line with the criteria of clinical adequacy, minimum invasiveness and rapid discharge. Among the different choices of anaesthesia, a vast array of scientific documentation15 exists to support the decided clinical advantages of sedation methods associated with local and loco-regional anaesthesia techniques. On the basis of such scientific support, we have opted for the following anaesthesia protocol:
Sedation
Premedication: Midazolam 0.04–0.05 mg/kg
Induction: Fentanyl 0.7–0.8 g/kg + Propofol 0.8–1.6 mg/kg
Maintenance: Propofol 0.3–0.5 mg/kg/hour
Only in rare cases (n = 6) it was necessary to use additional amounts of Propofol (0.5–0.8 mg/kg) and/or Fentanyl (0.4–0.8 g/kg) to guarantee adequate sedation.
Local anaesthesia
Anaesthesia in the pubic and penile region was executed by the surgeon using deep infiltration in the zone of the suspensory ligament of the penis and the cutaneous/sub-cutaneous zone affected by the surgical aggression:
Lidocaine 2%, 20 ml
Mepivacaine/carbocaine 2%, 10 ml (total solution 30 ml)
10 ml of the above mentioned solution was used in its pure form for cutaneous and deep peri-nervous infiltration, while the same was diluted in 230 ml of 0,9% sodium chloride with 1 mg epinephrine (1/250.000) for infiltration in the subcutaneous region where adipocytes will be harvested. In our experience, such procedure resulted to be fully ideal to allow surgical treatment, devoid of complications and major side effects, widely liked by patients and guaranteed brief protected discharge times (180 ± 30 minutes).
Surgical procedure
Fat Harvesting and Purification
Prior to the operation, the patients were photographed while standing. The operation began after disinfection of the skin, with the harvesting of the adipose tissue. This was performed by explanting fat bilaterally from the thighs if the patient was tendentially thin and from the periumbilical region if the patient was normo-weight or overweight and from the suprapubic region if there was any localised adiposity. This latter area of harvesting permitted, in certain cases, the reduction of the suprapubic adipose panniculus (suprapubic lipectomy) rendering the point of insertion of the penis deeper and visually increasing the length of the external portion of the penis (see supplementary file).
Thereafter infiltration of the donor site was performed with a tumescent solution. After a few minutes of waiting, necessary to consolidate the vasoconstrictor effect of the epinephrine, adipose explant was performed using a thin cannula (2 mm) and a 10 cc Luer-lock syringe. The quantity of fat explanted varied from subject to subject on the basis of the volume to be filled, but it was never less than 80 ml. That volume was comprised of infiltration material which was then removed by decantation first and centrifugation later. Such a process of purification is of primary importance since it determines the percentage integration of fat in the penis. In our surgical centre we first performed the decantation through sedimentation of each 10 cc syringe in such a way as to put the harvested material through an initial process of purification. Each syringe was filled with fat again and each time the infiltration material was removed, repeating the decantation by sedimentation process many times. Once a seemingly stable mixture was obtained, the syringes of crudely purified fat underwent centrifugation for two minutes at 1000 rpm. Reducing the time and the number of rpms, with respect to the original Coleman’s technique which involves centrifugation for 3 minutes at 3000 rpm, the integrity of the adipose globules, whose integrity is in turn responsible for the good integration of the fat, was safeguarded. In the meantime, for the patients who received elongation phalloplasty, a 980 nm diode laser was used.
V-Y Plasty and Dissection of the Suspensory Ligament
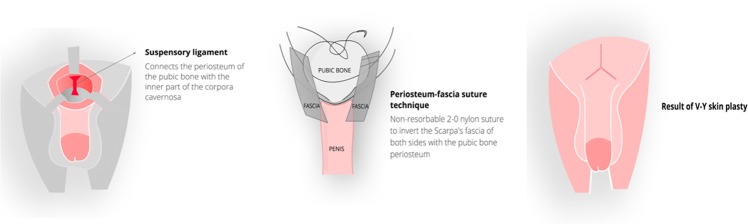
The suprapubic area was incised using the inverted V technique (V-Y Plasty), which is more preferable than the Z technique or other techniques since it guarantees a better aesthetic result16 and is widely used in plastic surgery (Fig. 1). This was followed by a complete section of the suspensory ligament of the penis, taking care to adequately section the lateral ligaments as well. Only in this way it is possible to obtain the best achievable results. The suspensory ligament of the penis is a deep structure that joins the cavernous bodies of the penis to the pubic symphysis; its section entails the forward translation of the internal portion of the penis with the consequent increase in the length of the visible penile volume. In order to avoid post-surgical scar retraction of the ligament, inverse periosteal-fascial sutures were used. This technique ensured that the most superficial ligamentous tissues, which had been sectioned, were inverted into the newly formed cavity and then anchored with 2-0 nylon stitches in the deepest portion of the periosteum of the pubic symphysis. A first deep layer of suture was performed using a 3-0 slow resorption material suturing the ligament in a longitudinal direction. In effect, the ligament was initially sectioned horizontally and then sutured longitudinally thereby obtaining a postero-anterior increment in length that supported the increment obtained through the section of the deep ligaments. We used a technique similar to that employed by Brisson, 200117. His technique allowed him to obtain a valid increase in the length of the external part of the penis and, at the same time, avoid scar-retraction phenomena that in the past nullified the increase obtained after a few weeks. Moreover, this quick and simple technique avoided the use of materials foreign to the organism, such as spacers of various kinds. A second layer of sutures was then performed always longitudinally using resorbable 3-0 sutures. Finally, the cosmetic closure of the cutaneous cut was performed using resorbable intradermal 4-0 sutures (V-Y plasty).
Figure 1.
The inverse periosteal-fascial suture is intended to prevent the post-operative scar retraction of the dissected suspensory ligament. In order to reach and dissect the suspensory ligament, the Scarpa’s fascia (fundiform ligament) is first sectioned. Once the severing of the suspensory ligament is completed, a non-resorbable 2-0 suture is applied. It initially involves the left side Scarpa’s fascia, then the pubic bone periosteum in the deepest possible portion and then again the contralateral, right side Scarpa’s fascia. When tightening the suture knot, an introflection (inversion) of both bands towards the sloping point of the pubis is obtained. It thus fills the space formed by the section of the suspensory ligament and allows for the forward sliding of the penis. This technique prevents the post-operative retraction of the suspensory ligament, a frequent cause of surgical failure, and ensures a permanent and gratifying result.
Fat Transfer
Once the penile elongation operation had been performed, the test-tubes containing the purified adipose material were extracted. They typically contained three layers: the most superficial was oily, the middle contained the purified fat and the lower was made up of blood and infiltration material18. The inferior and superior layers were eliminated and the purified material was implanted. Two mini-incisions of about 4 mm were made close to the pubo-penile junction at 10 o’clock and 2 o’clock respectively. The purified adipose material contained in the 10 cc syringes was decanted using a specific connector into 2.5 cc syringes better suited for the job. A blunt-tip cannula 2 mm in diameter was used for the implantation. The purified fat was then implanted into the subdartoic space taking care of the tunnel using the cannula and arranging the implant symmetrically. The space addressed was relatively avascular and, as a result, the formation of localized haematomas was rarely observed. In the few cases where hematomas were observed, bandaging was applied. Adverse events are summarised in Table 4. The quantity to be implanted varied considerably depending on the space to be filled, also considering that 30% of the implant would be resorbed within the first/second month. Therefore we decided to inject a modestly superior quantity to take into account its predicted partial resorption. At the end of the implantation, the surgical wound was closed and sutured using resorbable thread, a manoeuvre of manual “kneading” of the penis was then performed19 to aid in the uniform distribution of the implanted fat and finally a cohesive elastic bandage of adequate thickness was applied. The bandage has the important function of preventing the formation of crude asymmetries caused by posture and/or frequent erections during the first month after the operation. In fact, statistically at least 30 days are needed for the implant to be consolidated and the fat integrated and it is useful to limit the movement of the fat during this period using the elastic bandage. At the end of the operation a modestly compressive dressing was applied to the supra-pubic area and ice locally. The patient was discharged that evening with directions for medical therapy at home and adequately informed of the recovery period. In particular, the patient was urged to abstain from intense physical activity for 30 days and from sexual and masturbatory activity for 60 days. The duration of the operation was recorded from the moment of sedation until the final suture and it was about 80 minutes.
Table 4.
Summary of adverse events.
| Adverse events | PL + GE (N = 301) (n) | PL (N = 21) (n) | GE (N = 33) (n) | (N = 355) Total (%) |
|---|---|---|---|---|
| Loss of erectile function | 0 | 0 | 0 | |
| Decrease of erectile function (temporary) | 2 | 1 | 0 | 0.008 |
| Penile oedema | 0 | 0 | 0 | |
| Long-standing haematoma | 2 | 1 | 1 | 0.011 |
| Seroma | 2 | 0 | 0 | 0.005 |
| Dehiscence | 0 | 0 | N/A | |
| No increase in girth | 0 | N/A | 0 | |
| Fat loss (>30%) | 15 | N/A | 6 | 0.059 |
| Fat nodules, fat lumps | 1 | N/A | 1 | 0.005 |
| Fat migration | 1 | N/A | 0 | 0.003 |
| Sclerosing lipogranuloma | 0 | N/A | 0 | |
| Loss of sensation (mild) | 3 | 0 | 2 | 0.001 |
| Fibrosis | 0 | 0 | 0 | |
| Superficial infection | 1 | 0 | 1 | 0.005 |
| Deep infection | 0 | 0 | 0 | |
| Paradoxical penile shortening | 0 | 0 | N/A | |
| No increase in length | 0 | 0 | N/A | |
| Delayed wound healing | 3 | 1 | N/A | 0.011 |
| Penile deformity | 0 | 0 | 0 | |
| Penile asimmetry | 1 | N/A | 1 | 0.005 |
| Penile curvature | 0 | 0 | N/A | |
| Decreased erection angle (penile instability) | 1 | 1 | N/A | 0.005 |
| Hypertrophic wound scarring | 2 | 1 | N/A | 0.008 |
| Keloid | 1 | 0 | 0 | 0.003 |
| Scrotalization | 0 | 0 | 0 | |
| Disfiguring advancement of suprapubic hairy skin | 2 | 0 | N/A | 0.005 |
PL = Penile Lengthening; GE = Girth Enhancement; N/A = not applicable.
Statistical analysis
Penis length at rest, stretched length and circumference data were analysed using a One-Way Analysis of Variance (ANOVA) with Dunnet’s post-hoc test for comparison of each time point with baseline. IIEF-5 data were analysed using an unpaired two-sample Student’s t-test. All the data are presented as mean ± standard error of the mean (SEM). A p < 0.05 was considered significant.
Results
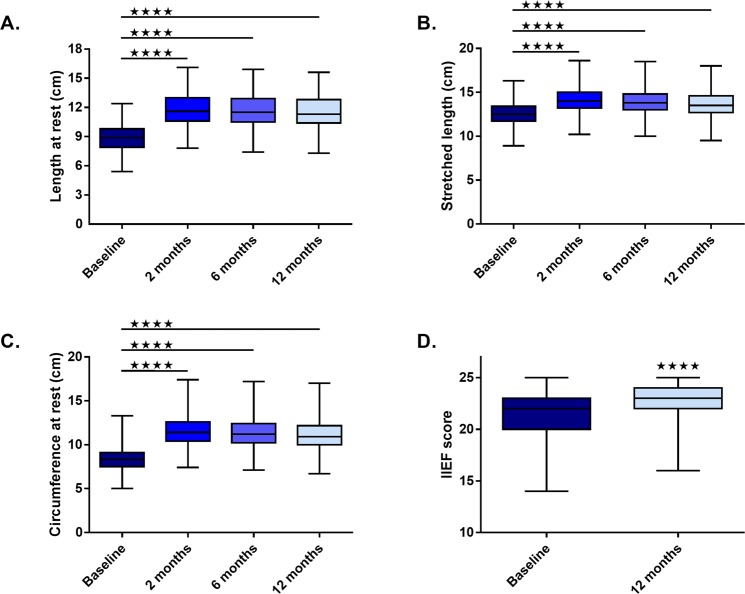
The baseline characteristics of the patients are summarized in Table 5. Following the surgical procedure, length at rest significantly increased at 2 (11.6 ± 0.08), 6 (11.5 ± 0.09) and 12 months (11.4 ± 0.1), compared to baseline (8.8 ± 0.07) (all p < 0.0001, respectively) (Fig. 2A). Stretched length significantly increased at 2 (14.02 ± 0.07), 6 (13.7 ± 0.08) and 12 (13.5 ± 0.09) months, compared to baseline (12.4 ± 0.06) (all p < 0.0001) (Fig. 2B). Circumference at rest significantly increased at 2 (11.5 ± 0.09), 6 (11.36 ± 0.09) and 12 (11.06 ± 0.1) months, compared to baseline (8.3 ± 0.06) (all p < 0.0001) (Fig. 2C). IIEF-5 increased at 12 months (23 ± 0.08) compared to baseline (21.5 ± 0.08) (p < 0.0001; 6.74% improvement) (Fig. 2D).
Table 5.
Baseline descriptive statistics of patients’ demographics.
| Age (years) | Weight (kg) | Height (cm) | Baseline IIEF-5 | Baseline length at rest (cm) | Baseline stretched length (cm) | Baseline circumference at rest (cm) | |
|---|---|---|---|---|---|---|---|
| Number of values | 355 | 355 | 355 | 327 | 354 | 355 | 354 |
| Minimum | 19 | 56 | 167 | 14 | 5.4 | 8.9 | 5 |
| 25% Percentile | 29 | 68 | 173 | 20 | 7.9 | 11.7 | 7.5 |
| Median | 36 | 74 | 178 | 22 | 8.9 | 12.5 | 8.3 |
| 75% Percentile | 46 | 81 | 181 | 23 | 9.8 | 13.4 | 9.1 |
| Maximum | 63 | 99 | 192 | 25 | 12.4 | 16.3 | 13.3 |
| Mean | 38.08 | 75.13 | 177.4 | 21.5 | 8.882 | 12.45 | 8.377 |
| Std. Deviation | 10.81 | 8.969 | 5.126 | 2.41 | 1.362 | 1.314 | 1.213 |
| Std. Error of Mean | 0.5737 | 0.476 | 0.2721 | 0.1333 | 0.07237 | 0.06974 | 0.06445 |
| Lower 95% CI of mean | 36.95 | 74.2 | 176.8 | 21.24 | 8.739 | 12.31 | 8.25 |
| Upper 95% CI of mean | 39.21 | 76.07 | 177.9 | 21.76 | 9.024 | 12.58 | 8.504 |
| Sum | 13519 | 26672 | 62962 | 7031 | 3144 | 4419 | 2965 |
IIEF-5 = 5-item International Index of Erectile Function.
Figure 2.
Cosmetic phalloplasty significantly improves penis length at rest (A), stretched length (B), circumference at rest (C) and 5-item International Index of Erectile Function (IIEF-5) score (D) at 2, 6 and 12 months post-surgical procedure. Line represents median. Four stars indicate statistical significance (p < 0.0001).
Discussion
We found that cosmetic phalloplasty significantly improves length at rest, stretched length, circumference at rest and IIEF-5 score at 2, 6 and 12 months post-surgery.
Hypoplasia of the penis is associated with medical conditions which include low flow priapism20, Peyronie’s disease21, congenital abnormalities22, erectile dysfunction23 and surgical conditions such as radical prostatectomy/radiotherapy for prostatic carcinoma24–26 and surgical correction of Peyronie’s disease27. Evidence shows cases of apparent hypoplasia distinguishing it from (a) “hidden” penis, secondary to the presence of abdominal fat or the cutaneous relaxation of the abdomen28 and (b) a “buried” penis where the penis shaft is beneath the suprapubic skin as a result of obesity and/or radical circumcision29.
Associated with a cutaneous V-Y plasty, ligamentolysis is the main and most common method of surgical elongation of the penis19,29–34. Omission of the cutaneous plasty contrasts the result achieved from the release of the ligament because it impedes the advancement of the shaft35. Detachment of the suspensory ligament and the pubic symphysis, which is obtained through ligamentolysis, causes a forward movement of the cavernous bodies and allows the penis to reach its maximum extracorporeal projection. The elongation is considered purely apparent (“apparent lengthening” vs “genuine lengthening”) since the length of the penis remains unvaried; such elongation is in fact significantly more visible at rest than during erection36. Nevertheless, the operation produces a visible and available increase in the length of the penis as expected by the patient.
Several techniques have been proposed in order to impede retraction of the sectioned ligament and therefore nullify the surgical result. They include positioning of the fat obtained from the spermatic funniculi between the suspensory ligament and the pubic symphysis19,37, use of silicone spacers38, the application of weights38 and postsurgical penile stretching39. In a previous study, the post-surgical use of extensors, for at least three consecutive months, resulted in an increase of length of no more than 1.3 cm40.
The growing demand for autologous fat transplant (AFT) beginning at the end of the 80 s is linked to the advent of liposuction. The current methods of fat transfer were popularised and extensively described by Sydney Coleman18,41,42 who in 1986 began to transplant fat in iatrogenic deformities from liposuction and subsequently in the face. AFT is today a widely tested procedure, appreciated by patients and very widespread among plastic surgeons even for reconstructive surgery43–49 despite no consensus has been reached regarding the best technique or its success rate.
The fat injection is the most common technique of penile girth enhancement. The fat harvested from the patient is implanted into the subdartoic space with the objective to symmetrically and uniformly increase the circumference of the penis29.
The inhomogeneities of the surgical techniques and the selection criteria of the patients render it difficult to compare the results obtained by our centre with those found in the literature and reported from other clinics (an overview of surgical techniques employed for phalloplasty and results obtained is summarised in Table 6).
Table 6.
Overview of surgical techniques employed for phalloplasty and results obtained.
| First author, year | N | Method | Follow-up (months) | Gain in Length (cm) | Gain in Girth (cm) | ||
|---|---|---|---|---|---|---|---|
| flaccid | erect | flaccid | erect | ||||
| Austoni, 200279 | 39 | Autologous safenous graft | 9 | 1.1–2.1 (∅) | |||
| Perovic, 200634 | 204 | Biodegr. scaffolds coated w/augologous fibroblasts | 24 (N = 84) | 3.15 | |||
| Shaeer, 200680 | 1 | Superficial circumflex iliac artery island flap | 6 | 9.5 | 8.5 | ||
| Bin, 200981 | 20 | Saphenous grafts, PTFE artificial vessel patches | 1–5 years | 1.0–2.3 | 1.5–3.0 | ||
| Jin, 201182 | 69 | Biodegr. scaffolds coated w/autologous fibroblasts | 1,3,6 | 4.01 | 2.92 | ||
| Alei, 201283 | 69 | Porcine dermis graft | 6.12 | 3.1 | 2.4 | ||
| Wessels, 1996 84 | 12 | SLD (N = 12) + VYP, FI (N = 10) | |||||
| Alter, 1997 85 | 30 | SLD + VYP, FI | |||||
| Klein, 1999 6 | 58¹ | SLD (N = 10), FI (N = 1), SLD + DFG (N = 6), SDL, FI (N = 41) | 12.2 | 3.0 | 0.76 | 2.52 | 2.03 |
| Roos, 19948 | 260 | SLD, Y(Z/M flap) | 4 (N = 100) | 4.0 | |||
| Shirong, 200086 | 52 | SLD + scrotal flap/skin graft, VYP | 6 (N = 20) | 3.5–6.5 | |||
| Spyropoulos, 200531 | 11 | SLD, VYP (N = 5) SLD, DFG (N = 3) SBL, SLD (N = 2) | 1.6 | 2.3/2.6 | |||
| Li, 200638 | 42 | SLD (N = 42) + silicone spacer (N = 27), VYP (N = 17) | 16 | 1.3 (stretched) | |||
| Panfilov, 200619 | 88 | SDL, FI (N = 31) FI (N = 57) | 12 | 2.42 | 1.0–4.0 | ||
| Mertziotis, 201387 | 82 | SLD + VYP, DFF (N = 35) | 12 | 1.92 | 2.21 | ||
| circumcision ligamentolisys, DFF (N = 47) | 2.11 | 2.0 | |||||
| Monreal, 201540 | 259° | SLD, FI (N = 148) FI (N = 127) | 6 (N = 160) 12 (N = 87) |
3.1 3.2 |
1.7 1.6 |
||
| Xu, 201688 | 23 | SLD + DFT | 2.27 | 1.67 | |||
DFF = dermal fat flap; DFT = dermal fat transfer; FI = fat injection; SBL = suprapubic lipectomy; SLD = suspensory ligament dissection; VYP = V-Y plasty.
¹Data obtained from questionnaires administered in several surgical centers by at least 10 different surgeons.
°Total number of procedures: 275.
In our experience, cosmetic phalloplasty has evolved in time moving in a direction of increased safety. The substitution of silicone spacers with inverse periosteal fascial sutures, which we have already described, and the use of autologous fat have marked the end of rare but significant complications that in the past led to reoperation. At the moment, we employ a surgical technique that keeps complications to a minimum and and results in great patients’ satisfaction. Patients who undergo combined elongation and girth enhancement phalloplasty are particularly satisfied compared to those who undergo a single operation which is probably linked to the availability of an overall greater penile volume40. In Italy, there is no validated test for the measurement of patients’ satisfaction in cosmetic penoplasty and the absence of a measurement of patients’ satisfaction is also a limitation of our study.
In line with other authors, we believe that, even in its relative simplicity, cosmetic phalloplasty requires a profound knowledge of anatomy and surgical technique and that the selection of candidates is a fundamental and essential element together with scrupulous gathering of information regarding not only the operation and the obtainable results, but also post-surgical conduct since resuming of sexual activity prior to 60 days after the operation can compromise the results.
While confirming that cosmetic phalloplasty very rarely produces spectacular results and that there is an objective necessity to improve the stability of the fat in time, we retain that the data from our centre show that the surgical technique we utilise is safe, repeatable and produces concrete and measurable results. Finally the operation, last resort to improve the patient’s discomfort, can considerably improve the patient’s self-esteem and improve the quality of his sex life and, in turn, his relationships.
Conclusions
The limited literature regarding cosmetic phalloplasty consists of studies performed using diverse surgical techniques and candidate selection criteria which include patients who should in fact be excluded (e.g. men with psychiatric conditions, namely body dysmorphic disorder) or whose existing conditions (e.g. failure of previous phalloplasty and trauma) make it impossible to compare results. If we consider the lack of universally shared morphometric values, we see how this niche of cosmetic surgery suffers from an inevitable lack of methodological rigour. In the present study we show the efficacy of cosmetic phalloplasty in a large cohort of patients up to 1-year follow-up. In addition, we describe in detail inclusion and exclusion criteria for patient selection and technical aspects of our surgical procedure which ensure reproducibility of our findings and should be adopted in future clinical studies of cosmetic phalloplasty. We are confident that this study will encourage other authors to publish their experiences with cosmetic phalloplasty and that the method we have described in this article will contribute to the consolidation of a standard for this type of surgery.
Supplementary information
Author Contributions
A.L. performed procedures and wrote the manuscript. R.M. performed procedures. T.I. performed statistical analysis, created tables and figures and wrote the manuscript. T.I., J.C.M.M., A.L. and B.P. participated in acquisition of relevant literature and revised the manuscript critically for intellectual content. A.L. and B.P. participated in conception and design of the work. All the authors approved the final version of the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-41652-w.
References
- 1.Lever J, Frederick D, Peplau L. Does size matter? Men’s and women’s views on penis size across the lifespan. Psychology of Men &Masculinity. 2006;7:129–143. doi: 10.1037/1524-9220.7.3.129. [DOI] [Google Scholar]
- 2.Davis SN, Binik YM, Amsel R, Carrier S. The Index of Male Genital Image: a new scale to assess male genital satisfaction. The Journal of urology. 2013;190:1335–1339. doi: 10.1016/j.juro.2013.03.121. [DOI] [PubMed] [Google Scholar]
- 3.Shaeer O, Shaeer K. Impact of penile size on male sexual function and role of penile augmentation surgery. Current urology reports. 2012;13:285–289. doi: 10.1007/s11934-012-0260-2. [DOI] [PubMed] [Google Scholar]
- 4.Francoeur, R. T. & Perper, T. A descriptive dictionary and atlas of sexology. (Greenwood Press, 1991).
- 5.Cleaveland P, Ali Z, Parnham A, Pearce I. The history of penile enhancement–to cut a short story long. Bju International. 2015;115:33. doi: 10.1111/bju.13085. [DOI] [PubMed] [Google Scholar]
- 6.Klein, R. Penile augmentation surgery. San Francisco. CA: Electronic Journal of Human Sexuality (1999).
- 7.Mondaini N, et al. Penile length is normal in most men seeking penile lengthening procedures. International Journal of Impotence Research. 2002;14:283. doi: 10.1038/sj.ijir.3900887. [DOI] [PubMed] [Google Scholar]
- 8.Roos H, Lissoos I. Penis lengthening. Int J Aesthetic Restorative Surg. 1994;2:89–96. [Google Scholar]
- 9.Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: guidelines for penile augmentation. The Journal of urology. 1996;156:995–997. doi: 10.1016/S0022-5347(01)65682-9. [DOI] [PubMed] [Google Scholar]
- 10.Alter GJ. Penile enhancement. Aesthetic Surgery Journal. 1996;16:226–230. doi: 10.1016/S1090-820X(96)70061-4. [DOI] [Google Scholar]
- 11.Schneider T, Sperling H, Lümmen G, Syllwasschy J, Rübben H. Does penile size in younger men cause problems in condom use? A prospective measurement of penile dimensions in 111 young and 32 older men. Urology. 2001;57:314–318. doi: 10.1016/S0090-4295(00)00925-0. [DOI] [PubMed] [Google Scholar]
- 12.Ponchietti R, et al. Penile length and circumference: a study on 3,300 young Italian males. European urology. 2001;39:183–186. doi: 10.1159/000052434. [DOI] [PubMed] [Google Scholar]
- 13.Promodu K, Shanmughadas K, Bhat S, Nair K. Penile length and circumference: an Indian study. International journal of impotence research. 2007;19:558. doi: 10.1038/sj.ijir.3901569. [DOI] [PubMed] [Google Scholar]
- 14.Nasar TA, Gadalla A, Zeidan A, El Batrawy M, Ghanem H. Relationship between penile size and body measurements. Human Andrology. 2011;1:48–50. doi: 10.1097/01.XHA.0000399177.60827.7e. [DOI] [Google Scholar]
- 15.SIAARTI C. Raccomandazioni clinico organizzative per l’anestesia in day surgery. Minerva Anestesiol. 2000;66:915–926. [PubMed] [Google Scholar]
- 16.Pribaz JJ, Chester CH, Barrall DT. The extended VY flap. Plastic and reconstructive surgery. 1992;90:275–280. doi: 10.1097/00006534-199290020-00017. [DOI] [PubMed] [Google Scholar]
- 17.Brisson P, Patel H, Chan M, Feins N. Penoplasty for buried penis in children: report of 50 cases. Journal of pediatric surgery. 2001;36:421–425. doi: 10.1053/jpsu.2001.21605. [DOI] [PubMed] [Google Scholar]
- 18.Pu LL, Coleman SR, Cui X, Ferguson RE, Jr., Vasconez HC. Autologous fat grafts harvested and refined by the Coleman technique: a comparative study. Plastic and reconstructive surgery. 2008;122:932–937. doi: 10.1097/PRS.0b013e3181811ff0. [DOI] [PubMed] [Google Scholar]
- 19.Panfilov DE. Augmentative phalloplasty. Aesthetic plastic surgery. 2006;30:183–197. doi: 10.1007/s00266-004-0153-y. [DOI] [PubMed] [Google Scholar]
- 20.Garaffa, G. & Ralph, D. J. In Problem Based Urology 49–54 (Springer, 2013).
- 21.Wu AK, Lue TF. Commentary on the myths of Peyronie’s disease. Translational andrology and urology. 2012;1:239. doi: 10.3978/j.issn.2223-4683.2012.12.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silver RI, Yang A, Ben-Chaim J, Jeffs RD, Gearhart JP. Penile length in adulthood after exstrophy reconstruction. The Journal of urology. 1997;157:999–1003. doi: 10.1016/S0022-5347(01)65131-0. [DOI] [PubMed] [Google Scholar]
- 23.Khan S, Somani B, Lam W, Donat R. Establishing a reference range for penile length in Caucasian British men: a prospective study of 609 men. BJU Int. 2012;109:740–744. doi: 10.1111/j.1464-410X.2011.10338.x. [DOI] [PubMed] [Google Scholar]
- 24.Munding MD, Wessells HB, Dalkin BL. Pilot study of changes in stretched penile length 3 months after radical retropubic prostatectomy. Urology. 2001;58:567–569. doi: 10.1016/S0090-4295(01)01270-5. [DOI] [PubMed] [Google Scholar]
- 25.Haliloglu A, Baltaci S, Yaman O. Penile length changes in men treated with androgen suppression plus radiation therapy for local or locally advanced prostate cancer. The Journal of urology. 2007;177:128–130. doi: 10.1016/j.juro.2006.08.113. [DOI] [PubMed] [Google Scholar]
- 26.Mehraban D, Salehi M, Zayeri F. Penile size and somatometric parameters among Iranian normal adult men. Int J Impot Res. 2007;19:303–309. doi: 10.1038/sj.ijir.3901532. [DOI] [PubMed] [Google Scholar]
- 27.Pryor J, et al. Peyronie’s disease. The journal of sexual medicine. 2004;1:110–115. doi: 10.1111/j.1743-6109.2004.10116.x. [DOI] [PubMed] [Google Scholar]
- 28.Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. The Journal of urology. 1999;161:455–459. doi: 10.1016/S0022-5347(01)61922-0. [DOI] [PubMed] [Google Scholar]
- 29.Dillon B, Chama N, Honig S. Penile size and penile enlargement surgery: a review. International journal of impotence research. 2008;20:519. doi: 10.1038/ijir.2008.14. [DOI] [PubMed] [Google Scholar]
- 30.Vardi Y, Harshai Y, Gil T, Gruenwald I. A critical analysis of penile enhancement procedures for patients with normal penile size: surgical techniques, success, and complications. European urology. 2008;54:1042–1050. doi: 10.1016/j.eururo.2008.07.080. [DOI] [PubMed] [Google Scholar]
- 31.Spyropoulos E, et al. Augmentation phalloplasty surgery for penile dysmorphophobia in young adults: considerations regarding patient selection, outcome evaluation and techniques applied. European urology. 2005;48:121–128. doi: 10.1016/j.eururo.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 32.Alter GJ. Augmentation phalloplasty. The Urologic clinics of North America. 1995;22:887–902. [PubMed] [Google Scholar]
- 33.Li C, Kumar P, Agrawal V, Minhas S, Ralph D. The role of surgery for penile dysmorphophobia and congenital micropenis. Bju International-Supplement. 2004;93:71. doi: 10.1111/j.1464-410X.2004.04561.x. [DOI] [Google Scholar]
- 34.Perovic SV, et al. New perspectives of penile enhancement surgery: tissue engineering with biodegradable scaffolds. European urology. 2006;49:139–147. doi: 10.1016/j.eururo.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 35.Bondil P, Delmas V. Is the section of the suspensory ligament of penis really efficient for penile lengthening: preliminary results of an anatomical study. Int. J. Impotence Res. 1995;7:32. [Google Scholar]
- 36.Perovic S, Djordjevic M. Penile lengthening. BJU international. 2000;86:1028–1033. doi: 10.1046/j.1464-410x.2000.00970.x. [DOI] [PubMed] [Google Scholar]
- 37.Alter G. Penile enlargement surgery. Techniques in urology. 1998;4:70–76. [PubMed] [Google Scholar]
- 38.Li C-Y, et al. Penile suspensory ligament division for penile augmentation: indications and results. European urology. 2006;49:729–733. doi: 10.1016/j.eururo.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 39.Murtagh, J. The ‘small’ penis syndrome. Australian family physician18, 218, 220–218, 220 (1989). [PubMed]
- 40.Monreal Juan. Composite augmentation phalloplasty: personal experience after 275 patients. Plastic and Aesthetic Research. 2015;2(1):27. doi: 10.4103/2347-9264.149374. [DOI] [Google Scholar]
- 41.Coleman SR. Long-term survival of fat transplants: controlled demonstrations. Aesthetic plastic surgery. 1995;19:421–425. doi: 10.1007/BF00453875. [DOI] [PubMed] [Google Scholar]
- 42.Zeltzer AA, Tonnard PL, Verpaele AM. Sharp-needle intradermal fat grafting (SNIF) Aesthetic surgery journal. 2012;32:554–561. doi: 10.1177/1090820X12445082. [DOI] [PubMed] [Google Scholar]
- 43.Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic plastic surgery. 2009;33:706–715. doi: 10.1007/s00266-009-9377-1. [DOI] [PubMed] [Google Scholar]
- 44.Dickinson, B. P. Autologous Fat Transfer National Consensus Survey: Trends in Techniques for Harvest, Preparation and Application; and Perception of Short and Long Term Results (2006). [DOI] [PubMed]
- 45.Kling RE, et al. Trends in autologous fat grafting to the breast: a national survey of the American society of plastic surgeons. Plastic and reconstructive surgery. 2013;132:35–46. doi: 10.1097/PRS.0b013e318290fad1. [DOI] [PubMed] [Google Scholar]
- 46.Gutowski KA, Force AFGT. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plastic and reconstructive surgery. 2009;124:272–280. doi: 10.1097/PRS.0b013e3181a09506. [DOI] [PubMed] [Google Scholar]
- 47.Leopardi D, Thavaneswaran P, Mutimer KL, Olbourne NA, Maddern GJ. Autologous fat transfer for breast augmentation: a systematic review. ANZ journal of surgery. 2014;84:225–230. doi: 10.1111/ans.12202. [DOI] [PubMed] [Google Scholar]
- 48.Claro F, Figueiredo J, Zampar A, Pinto‐Neto A. Applicability and safety of autologous fat for reconstruction of the breast. British Journal of Surgery. 2012;99:768–780. doi: 10.1002/bjs.8722. [DOI] [PubMed] [Google Scholar]
- 49.Villani F, Caviggioli F, Giannasi S, Klinger M, Klinger F. Current applications and safety of autologous fat grafts: a report of the ASPS Fat Graft Task Force. Plastic and reconstructive surgery. 2010;125:758–759. doi: 10.1097/PRS.0b013e3181c722cf. [DOI] [PubMed] [Google Scholar]
- 50.Loeb, H. Harnrohren capacitat und tripperspritzen. Munch Med Wochenschr46 (1899).
- 51.Schonfeld W, Beebe G. Normal growth and variation in the male genitalia from birth to maturity. The Journal of urology. 1942;48:759–777. doi: 10.1016/S0022-5347(17)70767-7. [DOI] [Google Scholar]
- 52.Kinsey, A. C., Pomeroy, W. B., Martin, C. E. & Sloan, S. Sexual behavior in the human male. Vol. 1 (Saunders Philadelphia, 1948).
- 53.Ajmani, M., Jain, S. & Saxena, S. Anthropometric study of male external genitalia of 320 healthy Nigerian adults. Anthropologischer Anzeiger, 179–186 (1985). [PubMed]
- 54.Bondli P, Costa P, Daures JP, Louis JF, Navratil H. Clinical study of the longitudinal deformation of the flaccid penis and of its variations with aging. European urology. 1992;21:284–286. doi: 10.1159/000474858. [DOI] [PubMed] [Google Scholar]
- 55.da Ros C, et al. Caucasian penis: what is the normal size. J Urol. 1994;151:323A–325A. [Google Scholar]
- 56.Smith AM, Jolley D, Hocking J, Benton K, Gerofi J. Does penis size influence condom slippage and breakage? International journal of STD & AIDS. 1998;9:444–447. doi: 10.1258/0956462981922593. [DOI] [PubMed] [Google Scholar]
- 57.Chen J, Gefen A, Greenstein A, Matzkin H, Elad D. Predicting penile size during erection. International journal of impotence research. 2000;12:328. doi: 10.1038/sj.ijir.3900627. [DOI] [PubMed] [Google Scholar]
- 58.Sengezer M, Ozturk S, Deveci M. Accurate method for determining functional penile length in Turkish young men. Ann Plast Surg. 2002;48:381–385. doi: 10.1097/00000637-200204000-00008. [DOI] [PubMed] [Google Scholar]
- 59.Shah J, Christopher N. Can shoe size predict penile length? Bju International. 2002;90:586–587. doi: 10.1046/j.1464-410X.2002.02974.x. [DOI] [PubMed] [Google Scholar]
- 60.Spyropoulos Evangelos, Borousas Dimitrios, Mavrikos Stamatios, Dellis Athanasios, Bourounis Michael, Athanasiadis Sotirios. Size of external genital organs and somatometric parameters among physically normal men younger than 40 years old. Urology. 2002;60(3):485–489. doi: 10.1016/S0090-4295(02)01869-1. [DOI] [PubMed] [Google Scholar]
- 61.Son H, Lee H, Huh JS, Kim SW, Paick JS. Studies on self-esteem of penile size in young Korean military men. Asian J Androl. 2003;5:185–189. [PubMed] [Google Scholar]
- 62.Savoie M, Kim SS, Soloway MS. A prospective study measuring penile length in men treated with radical prostatectomy for prostate cancer. J Urol. 2003;169:1462–1464. doi: 10.1097/01.ju.0000053720.93303.33. [DOI] [PubMed] [Google Scholar]
- 63.Pereira N. Estudo do tamanho do pénis na população portuguesa. Rev Int Androl. 2004;2:15–21. [Google Scholar]
- 64.Awwad Z, et al. Penile measurements in normal adult Jordanians and in patients with erectile dysfunction. Int J Impot Res. 2005;17:191–195. doi: 10.1038/sj.ijir.3901272. [DOI] [PubMed] [Google Scholar]
- 65.Kamel I, Gadalla A, Ghanem H, Oraby M. Comparing penile measurements in normal and erectile dysfunction subjects. J Sex Med. 2009;6:2305–2310. doi: 10.1111/j.1743-6109.2009.01305.x. [DOI] [PubMed] [Google Scholar]
- 66.Soylemez H, et al. Relationship between penile size and somatometric parameters in 2276 healthy young men. Int J Impot Res. 2012;24:126–129. doi: 10.1038/ijir.2011.53. [DOI] [PubMed] [Google Scholar]
- 67.Chen XB, Li RX, Yang HN, Dai JC. A comprehensive, prospective study of penile dimensions in Chinese men of multiple ethnicities. Int J Impot Res. 2014;26:172–176. doi: 10.1038/ijir.2014.9. [DOI] [PubMed] [Google Scholar]
- 68.Shalaby ME, Almohsen AE, El Shahid AR, Abd Al-Sameaa MT, Mostafa T. Penile length-somatometric parameters relationship in healthy Egyptian men. Andrologia. 2015;47:402–406. doi: 10.1111/and.12275. [DOI] [PubMed] [Google Scholar]
- 69.Veale D, Miles S, Bramley S, Muir G, Hodsoll J. Am I normal? A systematic review and construction of nomograms for flaccid and erect penis length and circumference in up to 15,521 men. BJU Int. 2015;115:978–986. doi: 10.1111/bju.13010. [DOI] [PubMed] [Google Scholar]
- 70.Habous M, et al. Erect penile dimensions in a cohort of 778 Middle Eastern men: establishment of a nomogram. J Sex Med. 2015;12:1402–1406. doi: 10.1111/jsm.12894. [DOI] [PubMed] [Google Scholar]
- 71.Salama N. Consultation for Small-Sized Penis in the Egyptian Males: A Case Control Study. Am J Mens Health. 2016;10:220–227. doi: 10.1177/1557988314565167. [DOI] [PubMed] [Google Scholar]
- 72.Hussein NS, Abid AF, Alnuaimi AS. Reference range of flaccid and stretched penile lengths of adult males in Baghdad: A cross-sectional study. Arab J Urol. 2017;15:68–73. doi: 10.1016/j.aju.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Richters J, Gerofi J, Donovan B. Are condoms the right size? A method for self-measurement of the erect penis. Venereology. 1995;8:77–81. [Google Scholar]
- 74.Bogaert AF, Hershberger S. The relation between sexual orientation and penile size. Arch Sex Behav. 1999;28:213–221. doi: 10.1023/A:1018780108597. [DOI] [PubMed] [Google Scholar]
- 75.Harding R, Golombok SE. Test-retest reliability of the measurement of penile dimensions in a sample of gay men. Arch Sex Behav. 2002;31:351–357. doi: 10.1023/A:1016276310371. [DOI] [PubMed] [Google Scholar]
- 76.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): ejaculatory function, penile anatomy, and contraceptive usage among Arabic-speaking Internet users in the Middle East. J Sex Med. 2012;9:425–433. doi: 10.1111/j.1743-6109.2011.02338.x. [DOI] [PubMed] [Google Scholar]
- 77.Herbenick D, Reece M, Schick V, Sanders SA. Erect penile length and circumference dimensions of 1,661 sexually active men in the United States. J Sex Med. 2014;11:93–101. doi: 10.1111/jsm.12244. [DOI] [PubMed] [Google Scholar]
- 78.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): The United States of America in 2011 penile size and form among English speakers. Human Andrology. 2013;3:46–53. doi: 10.1097/01.XHA.0000428124.12510.a8. [DOI] [Google Scholar]
- 79.Austoni, E., Guarneri, A. & Cazzaniga, A. A New Technique for Augmentation Phalloplasty: Albugineal Surgery with Bilateral Saphenous Grafts—Three Years of Experience. 42, 245–253 (2002). [DOI] [PubMed]
- 80.Shaeer O, Shaeer K. Penile girth augmentation using flaps “Shaeer’s augmentation phalloplasty”: a case report. J Sex Med. 2006;3:164–169. doi: 10.1111/j.1743-6109.2005.00104.x. [DOI] [PubMed] [Google Scholar]
- 81.Bin Y. A comparative study on two kinds of surgical procedures of penile corpora cavernosa augmentation. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2009;62:357–364. doi: 10.1016/j.bjps.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 82.Jin Z, et al. Tissue engineering penoplasty with biodegradable scaffold Maxpol-T cografted autologous fibroblasts for small penis syndrome. J Androl. 2011;32:491–495. doi: 10.2164/jandrol.110.011247. [DOI] [PubMed] [Google Scholar]
- 83.Alei G, et al. Original technique for penile girth augmentation through porcine dermal acellular grafts: results in a 69-patient series. J Sex Med. 2012;9:1945–1953. doi: 10.1111/j.1743-6109.2012.02744.x. [DOI] [PubMed] [Google Scholar]
- 84.Wessells H, Tom FL, Jack WMA. Complications of penile lengthening and augmentation seen at 1 referral center. The Journal of urology. 1996;155.5:1617–1620. doi: 10.1016/S0022-5347(01)66144-5. [DOI] [PubMed] [Google Scholar]
- 85.Alter G. Reconstruction of deformities resulting from penile enlargement surgery. The Journal of urology. 1997;158:2153–2157. doi: 10.1016/S0022-5347(01)68185-0. [DOI] [PubMed] [Google Scholar]
- 86.Shirong L, et al. Modified penis lengthening surgery: review of 52 cases. Plast Reconstr Surg. 2000;105:596–599. doi: 10.1097/00006534-200002000-00018. [DOI] [PubMed] [Google Scholar]
- 87.Mertziotis N, Kozyrakis D, Bogris E. Is V-Y plasty necessary for penile lengthening? Girth enhancement and increased length solely through circumcision: description of a novel technique. Asian J Androl. 2013;15:819–823. doi: 10.1038/aja.2013.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xu L, et al. Augmentation Phalloplasty With Autologous Dermal Fat Graft in the Treatment of “Small Penis”. Ann Plast Surg. 2016;77(Suppl 1):S60–65. doi: 10.1097/SAP.0000000000000782. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.