Abstract
Background
Total atherosclerosis disease burden is associated with clinical outcomes in patients with coronary artery disease. However, the influence of sex on the relationship between total anatomical and physiologic disease burdens and their prognostic implications have not been well defined.
Methods and Results
A total of 1136 patients who underwent fractional flow reserve (FFR) measurement in all 3 major coronary arteries were included in this study. Anatomical and physiologic total disease burden was assessed by SYNTAX (Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery) score, residual SYNTAX score, a total sum of FFR in 3 vessels (3‐vessel FFR), and functional SYNTAX score. The primary end point was major adverse cardiac events, a composite of cardiac death, myocardial infarction, and ischemia‐driven revascularization at 2 years. There were no differences in angiographic diameter stenosis, SYNTAX score, or residual SYNTAX score between women and men. However, both per‐vessel FFR (0.89±0.10 versus 0.87±0.11, P<0.001) and 3‐vessel FFR (2.72±0.13 versus 2.69±0.15, P<0.001) were higher in women. Multivariable Cox regression analyses showed that total anatomical and physiologic disease burdens were significantly associated with 2‐year major adverse cardiac events, and there was no significant interaction between sex and total disease burden for clinical outcomes.
Conclusions
Despite similar angiographic disease severity, both per‐vessel and per‐patient physiologic disease severity was less in women than in men. There was no influence of sex on prognostic implications of total anatomical and physiologic disease burdens in patients with coronary artery disease.
Clinical Trial Registration
URL: https://www.clinicaltrials.gov. Unique identifier: NCT01621438.
Keywords: coronary artery disease, fractional flow reserve, prognosis, sex, SYNTAX score, total disease burden
Subject Categories: Diagnostic Testing, Catheter-Based Coronary and Valvular Interventions, Women, Mortality/Survival
Clinical Perspective
What Is New?
Despite no sex difference in total anatomical disease burden (SYNTAX [Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery] score and residual SYNTAX score), total physiologic disease burden assessed by 3‐vessel FFR and functional SYNTAX score was lower in women.
Although women showed a lower major adverse cardiac event rate than men, sex was not an independent predictor after adjustment for total disease burden.
There was no sex influence on prognostic implications of total disease burden.
What Are the Clinical Implications?
This study supports the importance and clinical benefit of performing comprehensive physiologic assessment in women.
Introduction
Total atherosclerotic disease burden is a prognostic indicator in patients with coronary artery disease.1, 2, 3 The SYNTAX (Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery) score is a comprehensive angiographic scoring system for coronary artery disease burden,4, 5 and the residual SYNTAX score can represent the angiographic disease burden after percutaneous coronary intervention (PCI).6, 7 However, it is well known that angiography alone has limitations in defining ischemia‐causing stenosis.8 Fractional flow reserve (FFR) is a pressure‐derived physiologic index that is regarded as a standard tool for assessing the functional significance of coronary artery stenosis in the cardiac catheterization laboratory. A total sum of FFR measured in all 3 major epicardial coronary arteries can reflect total physiologic disease burden and has been reported to have prognostic implications.9, 10
Previous studies showed that the FFR value is higher in women than in men with the same stenosis severity,11 and visual‐functional mismatch is more frequent in women.12 However, the association between total anatomical and physiologic disease burdens according to sex and whether there is an interaction of sex in the relationship between total coronary disease burden and clinical outcomes are not well known. The current study was performed to compare anatomical and physiologic disease burden between women and men and to evaluate the sex influence on prognostic implication of total anatomical and physiologic disease burdens assessed by SYNTAX score and 3‐vessel FFR, respectively.
Methods
The data and study materials will be available to other researchers on reasonable request after discussion with the steering committee.
Study Population
This study was a substudy of the 3V FFR‐FRIENDS study (3‐Vessel Fractional Flow Reserve for the Assessment of Total Stenosis Burden and its Clinical Impact in Patients With Coronary Artery Disease, NCT01621438), which was designed to investigate the clinical relevance of total stenosis burden assessed by 3‐vessel FFR measurement.9 A total of 1136 patients who underwent FFR measurement in all 3 major coronary arteries were included in this study. Inclusion criteria were at least 18 years of age and stenosis >30% in all major epicardial arteries. Patients with left ventricular systolic dysfunction (ejection fraction <35%), ST‐elevation myocardial infarction within 72 hours, previous coronary artery bypass graft surgery, chronic kidney disease (serum creatinine ≥2.0 mg/dL), or abnormal epicardial coronary flow (TIMI [Thrombolysis In Myocardial Infarction] flow grade <3) were excluded. The study protocol was approved by the institutional review board or ethics committee at each participating center, and all patients provided written informed consent.
Angiography, Quantitative Coronary Angiography, and SYNTAX Score
Coronary angiography was obtained using standard techniques after administration of intracoronary nitrate (100 or 200 μg). All angiograms were analyzed at a core laboratory (Seoul National University Hospital, Seoul, Korea) in a blinded fashion. Quantitative coronary angiography was performed with validated software (CAAS II, Pie Medical System, Maastricht, The Netherlands). Reference vessel size, minimum lumen diameter, percentage diameter stenosis (%DS), and lesion length were obtained. Per‐patient total angiographic disease severity was assessed by SYNTAX score by a blinded investigator.4 The residual SYNTAX Score was calculated based on the remaining stenotic coronary lesion after treatment with PCI.
FFR Measurements, 3‐Vessel FFR Calculation, and Functional SYNTAX Score
FFR measurements were performed after diagnostic angiography. The pressure‐temperature sensor guide wire (Abbott Vascular, Santa Clara, CA) was equalized to aortic pressure at the tip of the guide catheter and then positioned at the distal segment of a target vessel. Intracoronary nitrate (100 or 200 μg) was administered before each set of FFR measurements. Hyperemic aortic pressure and distal coronary arterial pressure were obtained, and FFR was calculated as the mean of distal coronary arterial pressure/aortic pressure during maximum hyperemia. PCI was performed according to the operator's discretion. Three‐vessel FFR was calculated as the sum of FFR values measured in 3 major epicardial arteries.9 In cases of PCI, post‐PCI FFR was used for the calculation of 3‐vessel FFR. Functional SYNTAX score was calculated as a sum of the SYNTAX score in vessels with FFR ≤0.80.13
Coronary Computed Tomographic Angiography Plaque Characteristics Analysis
Among the total population, 299 patients (772 vessels) underwent coronary computed tomographic angiography (CCTA) within 90 days of FFR measurement. CCTA images were obtained in accordance with the Society of Cardiovascular Computed Tomography Guidelines on Performance of CCTA.14 The CCTA images were analyzed at a core laboratory (Severance Cardiovascular Hospital, Seoul, Korea) in a blinded fashion. For each lesion, the presence of the following adverse plaque characteristics was analyzed: (1) low‐attenuation plaque (average density ≤30 HU); (2) positive remodeling (remodeling index ≥1.1); (3) napkin‐ring sign (ring‐like attenuation pattern with peripheral high‐attenuation tissue surrounding a central lower‐attenuation portion); and (4) spotty calcification (average density >130 HU and diameter <3 mm).15
Patient Follow‐Up and Outcome Measurements
Clinical data were obtained at outpatient clinic visits or by telephone contact when needed. An independent clinical events committee, whose members were unaware of clinical, angiographic, and physiologic data, adjudicated all events. The primary outcome was major adverse cardiac events (MACE) at 2 years, a composite of cardiac death, any myocardial infarction, and any ischemia‐driven revascularization. All clinical outcomes were defined according to the Academic Research Consortium, including the addendum to the definition of myocardial infarction. All deaths were considered cardiac unless a definite noncardiac cause could be established. Ischemia‐driven revascularization was defined as a revascularization for at least 1 of the following reasons: (1) recurrence of angina; (2) a positive noninvasive test; and (3) a positive invasive physiologic test.
Statistical Analysis
Continuous variables were presented as means with standard deviations and were compared using a Student t test. Categorical variables were presented as numbers with percentages and compared with the chi‐squared test. Clinical and lesion characteristics, SYNTAX score, residual SYNTAX score, 3‐vessel FFR, functional SYNTAX score, and clinical outcomes were analyzed on a per‐patient basis. Quantitative coronary angiography results, per‐vessel FFR, and CCTA plaque characteristics were analyzed on a per‐vessel basis. A comparison of per‐vessel measurements between sexes was performed with generalized estimating equations to account for clustering of vessel measurement within the same patient.
In order to evaluate the association between SYNTAX score, residual SYNTAX score, 3V‐FFR, and functional SYNTAX score and estimated 2‐year MACE risk according to sex, the probability of risk was estimated using the Cox proportional‐hazards model and was plotted using the locally weighted scatterplot smoothing regression line.9 Hazard ratios with 95% CIs were estimated using the multivariable Cox proportional‐hazards method to identify independent predictors of MACE.
Two‐sided comparisons were considered statistically significant when P<0.05. All analyses were performed using SPSS version 22.0 (IBM, Armonk, NY).
Results
Patient and Lesion Characteristics
Of the total 1136 patients included in the study, 301 (26.5%) patients were women. The baseline patient characteristics are shown in Table 1. Women were significantly older (65.0±9.6 versus 60.8±9.7 years, P<0.001) and had a higher prevalence of hypertension (66.1% versus 58.7%, P=0.024). The reference vessel diameter (2.89±0.57 mm versus 3.03±0.61 mm, P<0.001) and minimum lumen diameter (1.66±0.71 mm versus 1.72±0.72 mm, P=0.044) were significantly lower in women. However, there was no difference in angiographic %DS (43.3±19.6% versus 43.8±19.1%, P=0.530) (Table 2 and Figure 1). Per‐vessel FFR was significantly higher (0.89±0.10 versus 0.87±0.11, P<0.001), and the proportion of low FFR was significantly lower (16.8% versus 22.1%, P=0.001), in women. Association between angiographic stenosis severity and FFR according to sex is shown in Figure 2. Mismatch (%DS≥50% and FFR>0.80) was numerically more frequent in women than in men, although without statistical significance (18.2% versus 15.4%, P=0.057). Among lesions with %DS≥50%, mismatch lesions were more frequent in women than in men (60.6% versus 52.0%, P=0.020). CCTA‐defined adverse plaque characteristics were less frequently shown in women (46.6% versus 59.0%, P=0.004).
Table 1.
Clinical Characteristics According to Sex
| Total (n=1136) | Women (n=301) | Men (n=835) | P Value | |
|---|---|---|---|---|
| Age, y | 61.9±9.8 | 65.0±9.6 | 60.8±9.7 | <0.001 |
| Hypertension | 689 (60.7%) | 199 (66.1%) | 490 (58.7%) | 0.024 |
| Diabetes mellitus | 363 (32.0%) | 107 (35.5%) | 256 (30.7%) | 0.119 |
| Hypercholesterolemia | 597 (52.6%) | 152 (50.5%) | 445 (53.3%) | 0.405 |
| Current smoker | 327 (28.8%) | 22 (7.3%) | 305 (36.5%) | <0.001 |
| Previous MI | 100 (8.8%) | 21 (7.0%) | 79 (9.5%) | 0.192 |
| Previous PCI | 360 (31.7%) | 88 (29.2%) | 272 (32.6%) | 0.286 |
| Multivessel disease | 499 (43.9%) | 123 (40.9%) | 376 (45.0%) | 0.212 |
| Clinical presentation | ||||
| Stable angina | 882 (77.6%) | 242 (80.4%) | 640 (76.6%) | 0.180 |
| Acute coronary syndrome | 254 (22.4%) | 59 (19.6%) | 195 (23.4%) | |
Values are mean±SD or n (%). MI indicates myocardial infarction; PCI, percutaneous coronary intervention.
Table 2.
Lesion Characteristics According to Sex
| Total | Women | Men | P Value | |
|---|---|---|---|---|
| Per Vessel | (n=3298) | (n=878) | (n=2420) | |
| Quantitative coronary angiography | ||||
| Reference vessel diameter, mm | 3.04±0.60 | 2.89±0.57 | 3.03±0.61 | <0.001 |
| Minimum lumen diameter, mm | 1.70±0.71 | 1.66±0.71 | 1.72±0.72 | 0.092 |
| Diameter stenosis, % | 43.7±19.3 | 43.3±19.6 | 43.8±19.1 | 0.608 |
| Lesion length, mm | 11.1±8.9 | 10.9±9.0 | 11.2±8.8 | 0.435 |
| FFR | 0.88±0.11 | 0.89±0.10 | 0.87±0.11 | <0.001 |
| FFR ≤0.80 | 641 (20.7%) | 139 (16.8%) | 502 (22.1%) | 0.001 |
| CCTA plaque characteristics | (n=672) | (n=179) | (n=493) | |
| Any of adverse plaque characteristics | 374 (55.7%) | 83 (46.6%) | 291 (59.0%) | 0.004 |
| Positive remodeling | 223 (33.2%) | 51 (28.5%) | 172 (34.9%) | 0.120 |
| Low‐attenuation plaque | 142 (21.1%) | 25 (14.0%) | 117 (23.6%) | 0.007 |
| Scattered calcification | 101 (15.0%) | 26 (14.5%) | 75 (15.2%) | 0.841 |
| Napkin‐ring sign | 11 (1.6%) | 2 (1.1%) | 9 (1.8%) | 0.531 |
| Per patient | (n=1136) | (n=301) | (n=835) | |
| SYNTAX score | 11.0±8.1 | 10.3±8.5 | 11.3±7.9 | 0.098 |
| Residual SYNTAX score | 8.2±6.8 | 7.9±7.0 | 8.4±6.8 | 0.306 |
| 3‐vessel FFR | 2.70±0.14 | 2.72±0.13 | 2.69±0.15 | <0.001 |
| Functional SYNTAX score | 4.3±6.4 | 3.3±5.8 | 4.7±6.6 | <0.001 |
Values are mean±SD, n (%). P‐values for per‐vessel comparisons were determined by generalized estimating equations. CCTA indicates coronary computed tomography angiography; FFR, fractional flow reserve; SYNTAX, Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery.
Figure 1.
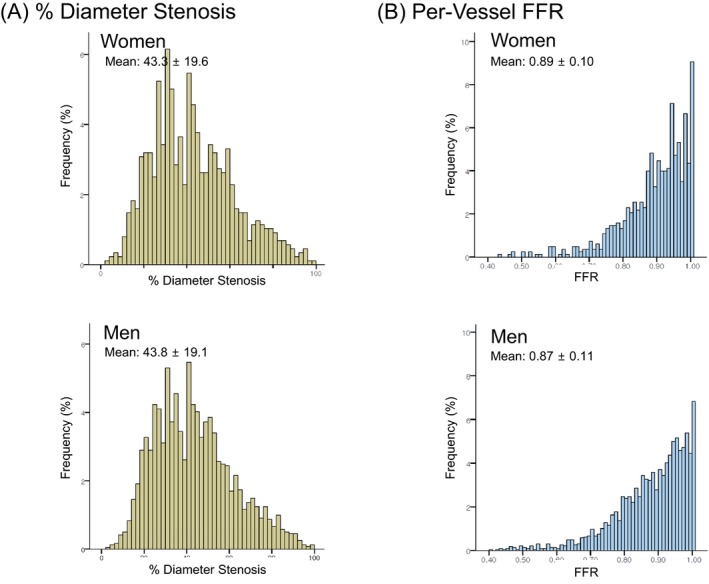
Distribution of angiographic percentage diameter stenosis and per‐vessel FFR. The distributions of percentage diameter stenosis (A) and per‐vessel FFR (B) according to sex are presented. FFR indicates fractional flow reserve.
Figure 2.
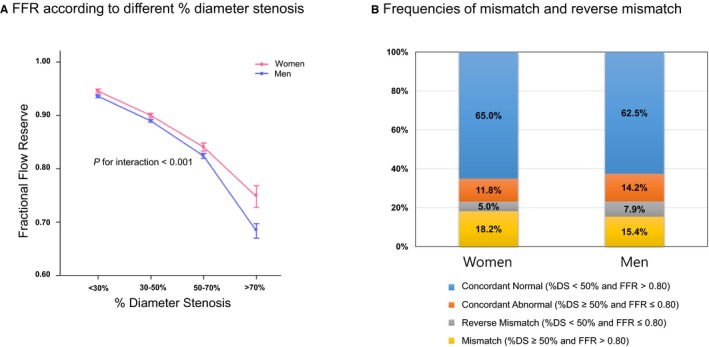
Association between angiographic stenosis severity and FFR according to sex. A, This figure shows the values of FFR according to different angiographic stenosis severity in women and men. B, When the proportions of concordant normal, concordant abnormal, reverse mismatch, and mismatch were compared, mismatch was more frequent in women than in men. %DS indicates percentage diameter stenosis; FFR, fractional flow reserve.
Total Anatomical and Physiologic Disease Burdens
Distributions of SYNTAX score, residual SYNTAX score, and 3‐vessel FFR are shown in Figure 3. There were no differences based on patient sex in total anatomical disease burden (SYNTAX score, 10.3±8.5 versus 11.3±7.9, P=0.098; residual SYNTAX score, 7.9±7.0 versus 8.4±6.8, P=0.306). However, 3‐vessel FFR, which represents the physiologic disease burden, was significantly higher in women (2.72±0.13 versus 2.69±0.15, P<0.001). Functional SYNTAX score was also lower in women than in men (3.3±5.8 versus 4.7±6.6, P<0.001) (Table 2).
Figure 3.
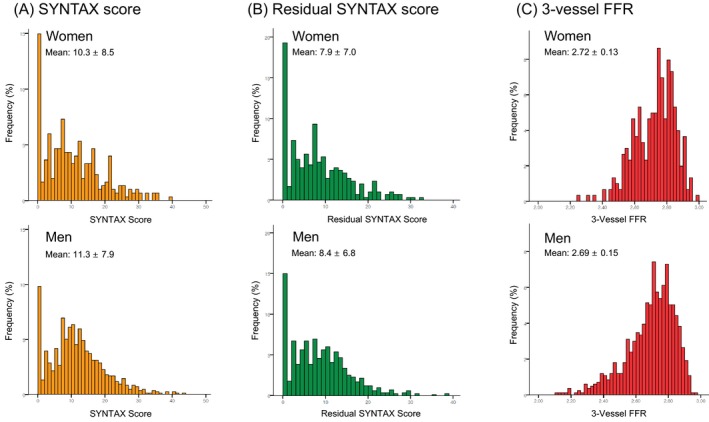
Distributions of SYNTAX Score (A), residual SYNTAX score (B), and 3‐vessel FFR (C) in women and men. There were no differences in SYNTAX score and residual SYNTAX score between women and men. However, 3‐vessel FFR was higher in women (2.72±0.13 vs 2.69±0.15, P<0.001). FFR indicates fractional flow reserve; SYNTAX, Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery.
Clinical Outcomes According to Total Anatomical and Physiologic Disease Burden
Table 3 shows the comparison of 2‐year MACE rates between women and men. Women showed a lower MACE rate than men (2.3% versus 5.0%, hazard ratio 0.457, 95% CI 0.243‐0.860, P=0.049). However, sex was not an independent predictor after adjustment for 3‐vessel FFR, residual SYNTAX score, and clinical risk factors (hazard ratio 0.534, 95% CI 0.230‐1.238, P=0.144).
Table 3.
Clinical Outcomes at 2 Years in Women and Men
| Outcomes | Womena | Mena | HR (95% CI) | P Value |
|---|---|---|---|---|
| Major adverse cardiac eventsb | 7 (2.3%) | 42 (5.0%) | 0.457 (0.243‐0.860) | 0.049 |
| Cardiac death | 1 (0.3%) | 9 (1.1%) | 0.305 (0.075‐1.236) | 0.232 |
| Myocardial infarction | 2 (0.7%) | 10 (1.2%) | 0.549 (0.153‐1.971) | 0.432 |
| Ischemia‐driven revascularization | 7 (2.3%) | 33 (4.0%) | 0.582 (0.289‐1.171) | 0.187 |
HR indicates hazard ratio.
Clinical outcomes are expressed with 2‐year cumulative events (incidence rate, %).
Major adverse cardiac events were defined as a composite of cardiac death, myocardial infarction, and ischemia‐driven revascularization.
SYNTAX score, residual SYNTAX score, and 3‐vessel FFR showed significant association with the estimated 2‐year MACE rates in both sexes (Figure 4). A multivariable adjusted Cox regression analyses adjusted with age and cardiac risk factors showed that SYNTAX score, residual SYNTAX score, 3‐vessel FFR, and functional SYNTAX score were independently associated with the risk of 2‐year MACE (Table 4). In these models, age and clinical risk factors were not independent predictors for 2‐year MACE (all P>0.05). There was no significant interaction of patient sex in the relationship between total disease burden and clinical outcomes (Figure 4).
Figure 4.
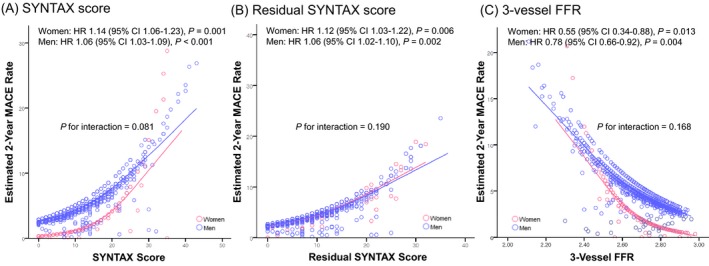
Association between estimated 2‐year major adverse cardiac event rate and anatomical and physiologic disease burden. SYNTAX score (A), residual SYNTAX score (B), and 3‐vessel FFR (C) showed significant association with the estimated 2‐year MACE rates in both sexes. There was no significant interaction of sex in the relationship between total disease burden and clinical outcomes. FFR indicates fractional flow reserve; HR, hazard ratio; MACE, major adverse cardiovascular events; SYNTAX, Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery.
Table 4.
Associations of Total Disease Burden for 2‐Year Major Adverse Cardiac Events According to Sex
| Variable | Total Population | Women | Men | P for Interaction | |||
|---|---|---|---|---|---|---|---|
| Adjusted HR (95% CI) | P Value | Adjusted HR (95% CI) | P Value | Adjusted HR (95% CI) | P Value | ||
| SYNTAX score (by 1 increase) | 1.067 (1.036‐1.098) | <0.001 | 1.160 (1.052‐1.278) | 0.003 | 1.054 (1.020‐1.089) | 0.002 | 0.078 |
| Residual SYNTAX score (by 1 increase) | 1.065 (1.031‐1.101) | <0.001 | 1.127 (1.018‐1.249) | 0.021 | 1.055 (1.018‐1.093) | 0.004 | 0.191 |
| 3‐vessel FFR (by 0.1 decrease) | 1.346 (1.146‐1.579) | <0.001 | 2.315 (1.237‐4.332) | 0.009 | 1.292 (1.090‐1.531) | 0.003 | 0.155 |
| Functional SYNTAX score (by 1 increase) | 1.066 (1.031‐1.102) | <0.001 | 1.095 (0.993‐1.208) | 0.070 | 1.059 (1.021‐1.099) | 0.002 | 0.309 |
Multivariable Cox regression analysis adjusted with age, hypertension, diabetes mellitus, hyperlipidemia, current smoking, acute coronary syndrome, and previous myocardial infarction. FFR indicates fractional flow reserve; HR, hazard ratio; SYNTAX, Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery.
Discussion
The current study evaluated the sex difference in anatomically and physiologically assessed total disease burdens and their prognostic implications. The main findings are as follows. (1) Despite similar per‐vessel angiographic %DS, FFR value was higher in women than in men. (2) Although there was no sex difference in total anatomical disease burden (SYNTAX score and residual SYNTAX score), total physiologic disease burden assessed by 3‐vessel FFR and functional SYNTAX score was lower in women. (3) Women showed a lower MACE rate than men. However, sex was not an independent predictor after adjustment for anatomical and physiologic disease burdens. In addition, there was no sex influence on prognostic implications of total disease burden.
The presence of myocardial ischemia is a prerequisite for a benefit of coronary revascularization.16, 17 Due to the limitation of angiography in defining functionally significant lesions,8, 18 invasive physiologic indices such as FFR have been developed for the assessment of the functional significance of coronary artery stenosis in the cardiac catheterization laboratory.19 Because FFR‐guided revascularization strategy improved clinical outcomes compared with angiography‐guided revascularization or medical treatment only,20, 21 physiology‐guided revascularization has been adopted as a standard treatment strategy.22, 23 Previous studies have suggested that FFR value is higher for women with the same stenosis severity,11 and visual‐functional mismatch is more frequent in women.12 In our study the mismatch (angiographically significant stenosis and high FFR) was more common in women than in men. In addition, this sex influence on mismatch becomes higher as angiographic stenosis severity increases. When this comparison was extended to a per‐patient level, it was also found that total physiologic disease burden assessed by 3‐vessel FFR was also lower in women despite similar SYNTAX and residual SYNTAX scores. These findings suggest that a similar degree of anatomical disease burden might result in different physiologic outcomes according to sex.
Differences in myocardial mass and microvascular function are suggested as a mechanism of higher FFR in women than in men for the same stenosis severity.24, 25 Recent studies showed that plaque characteristics can influence FFR values. Ahmadi et al showed that a large necrotic core may induce greater ischemia and reduced FFR compared with non–lipid‐rich plaques.26 It is interesting to note that CCTA‐defined low‐attenuation plaque was more frequent in men than in women in our study. Further studies are needed to investigate the sex influence on plaque characteristics.
It is interesting to see that women have less physiologic disease burden even though they are older than men. This reflects a slower progression of atherosclerosis in women.27 And the 2‐year MACE rate was lower in women than in men in our study despite higher age and more clinical risk factors in women. However, sex, age, and clinical risk factors were not independent predictors for clinical outcomes after adjustment of angiographic and physiologic disease burden.
Total atherosclerotic disease burden is an important prognostic indicator in patients with coronary artery disease.1 The SYNTAX score was primarily developed for visual grading of coronary artery disease complexity and showed its prognostic implication.4 In addition, residual SYNTAX score is also a prognostic indicator in patients undergoing PCI.7 In a study by Lee et al, total physiologic disease burden assessed by 3‐vessel FFR also showed a prognostic implication.9 However, the influence of sex on the association between the clinical outcomes and anatomical or physiologic disease burden has not been well defined. In our study, 3‐vessel FFR was higher and functional SYNTAX score was lower in women than in men despite similar SYNTAX and residual SYNTAX scores. However, there was no interaction of sex on the association between clinical outcomes and anatomical and physiologic disease burden. These findings suggest that the controversial results of previous studies on clinical outcomes according to sex in patients with coronary artery disease11, 28, 29, 30 may, in part, be due to the greater mismatch between anatomical and physiologic disease severity in women than in men.
When the previous study results are combined with ours, characteristics of coronary artery disease according to sex can be summarized as follows. Women tend to have more clinical risk factors (older age, hypertension) and less per‐vessel and per‐patient physiologic disease severity with similar anatomical disease burden. Total anatomical and physiologic disease burdens had prognostic implication regardless of sex, and there is no interaction between sex and prognostic implication of total disease burden. These findings support the importance and clinical benefit of performing physiologic assessment in women.
Limitations
Some limitations of the current study should be considered. First, this was a post hoc analysis of the 3V FFR‐FRIENDS registry. Second, most of the lesions had mild to intermediate stenosis, and the number of low‐FFR vessels was relatively small. Therefore, the rate of clinical events was relatively low compared with that of other studies. Third, total plaque burden assessed by invasive imaging modalities was not available in this study. Anatomical disease burden assessed by angiography might be less accurate than intravascular imaging–based measurement.
Conclusion
Despite similar angiographic disease severity, both per‐vessel and per‐patient physiologic disease severity were less in women than in men. There was no influence of patient sex on the prognostic implications of total anatomical and physiologic disease burdens in patients with coronary artery disease.
Sources of Funding
This study was supported by an unrestricted research grant from Abbott Vascular (Santa Clara, CA, USA). The company had no role in the study design, conduct, data analysis, or manuscript preparation.
Disclosures
Dr Koo received an Institutional Research Grant from Abbott Vascular and Philips Volcano. Dr Lee received a Research Grant from Abbott Vascular and Philips Volcano. The remaining authors have no disclosures to report.
(J Am Heart Assoc. 2019;8:e011002 DOI: 10.1161/JAHA.118.011002.)
References
- 1. Min JK, Dunning A, Lin FY, Achenbach S, Al‐Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang H‐J, Cheng V, Chinnaiyan K, Chow BJ, Delago A, Hadamitzky M, Hausleiter J, Kaufmann P, Maffei E, Raff G, Shaw LJ, Villines T, Berman DS; CONFIRM Investigators . Age‐and sex‐related differences in all‐cause mortality risk based on coronary computed tomography angiography findings: results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol. 2011;58:849–860. [DOI] [PubMed] [Google Scholar]
- 2. Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP, Parise H, Templin B, White R, Zhang Z, Serruys PW; PROSPECT Investigators . A prospective natural‐ history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–235. [DOI] [PubMed] [Google Scholar]
- 3. Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, Jørgensen E, Kelbæk H, Prescott E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2011;33:734–744. [DOI] [PubMed] [Google Scholar]
- 4. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein A‐P, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50–56. [DOI] [PubMed] [Google Scholar]
- 5. Wykrzykowska JJ, Garg S, Girasis C, de Vries T, Morel M‐A, van Es G‐A, Buszman P, Linke A, Ischinger T, Klauss V, Corti R, Eberli F, Wijns W, Morice MC, di Mario C, van Geuns RJ, Juni P, Windecker S, Serruys PW. Value of the SYNTAX score for risk assessment in the all‐comers population of the randomized multicenter LEADERS (Limus Eluted from A Durable versus Erodable Stent Coating) trial. J Am Coll Cardiol. 2010;56:272–277. [DOI] [PubMed] [Google Scholar]
- 6. Généreux P, Palmerini T, Caixeta A, Rosner G, Green P, Dressler O, Xu K, Parise H, Mehran R, Serruys PW, Stone GW. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol. 2012;59:2165–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Farooq V, Serruys PW, Bourantas CV, Zhang Y, Muramatsu T, Feldman T, Holmes DR, Mack M, Morice MC, Ståhle E, Colombo A, de Vries T, Morel MA, Dawkins KD, Kappetein AP, Mohr FW. Quantification of incomplete revascularization and its association with five‐year mortality in the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. 2013;128:141–151. [DOI] [PubMed] [Google Scholar]
- 8. Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92:2333–2342. [DOI] [PubMed] [Google Scholar]
- 9. Lee JM, Koo B‐K, Shin E‐S, Nam C‐W, Doh J‐H, Hwang D, Park J, Kim K‐J, Zhang J, Hu X, Wang J, Ahn C, Ye F, Chen S, Yang J, Chen J, Tanaka N, Yokoi H, Matsuo H, Takashima H, Shiono Y, Akasaka T. Clinical implications of three‐vessel fractional flow reserve measurement in patients with coronary artery disease. Eur Heart J. 2017;39:945–951. [DOI] [PubMed] [Google Scholar]
- 10. Park J, Lee JM, Koo BK, Shin ES, Nam CW, Doh JH, Hwang D, Zhang J, Hu X, Wang J, Ye F, Chen S, Yang J, Chen J, Tanaka N, Yokoi H, Matsuo H, Takashima H, Shiono Y, Akasaka T. Clinical relevance of functionally insignificant moderate coronary artery stenosis assessed by 3‐vessel fractional flow reserve measurement. J Am Heart Assoc. 2018;7:e008055 DOI: 10.1161/JAHA.117.00805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim H‐S, Tonino PA, De Bruyne B, Yong AS, Tremmel JA, Pijls NH, Fearon WF; Investigators FS . The impact of sex differences on fractional flow reserve–guided percutaneous coronary intervention: a FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) substudy. JACC Cardiovasc Interv. 2012;5:1037–1042. [DOI] [PubMed] [Google Scholar]
- 12. Kang S‐J, Ahn J‐M, Han S, Lee J‐Y, Kim W‐J, Park D‐W, Lee S‐W, Kim Y‐H, Lee CW, Park S‐W, Mintz GS, Park SJ. Sex differences in the visual‐functional mismatch between coronary angiography or intravascular ultrasound versus fractional flow reserve. JACC Cardiovasc Interv. 2013;6:562–568. [DOI] [PubMed] [Google Scholar]
- 13. Choi KH, Lee JM, Koo B‐K, Nam C‐W, Shin E‐S, Doh J‐H, Rhee T‐M, Hwang D, Park J, Zhang J, Kim KJ, Hu X, Wang J, Ye F, Chen S, Yang J, Chen J, Tanaka N, Yokoi H, Matsuo H, Takashima H, Shiono Y, Akasaka T. Prognostic implication of functional incomplete revascularization and residual functional SYNTAX score in patients with coronary artery disease. JACC Cardiovasc Interv. 2018;11:237–245. [DOI] [PubMed] [Google Scholar]
- 14. Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, Rubin GD, Kramer CM, Berman D, Brown A, Chaudhry FA, Cury RC, Desai MY, Einstein AJ, Gomes AS, Harrington R, Hoffmann U, Khare R, Lesser J, McGann C, Rosenberg A, Schwartz R, Shelton M, Smetana GW, Smith SC Jr. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894. [DOI] [PubMed] [Google Scholar]
- 15. Lee JM, Choi G, Koo B‐K, Hwang D, Park J, Zhang J, Kim K‐J, Tong Y, Kim HJ, Grady L. Identification of high‐risk plaques destined to cause acute coronary syndrome using coronary computed tomographic angiography and computational fluid dynamics. JACC Cardiovasc Imaging. 2018:2554 S1936‐878X(18)30134–S1936‐878X(18)30137. [DOI] [PubMed] [Google Scholar]
- 16. Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short‐term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–2907. [DOI] [PubMed] [Google Scholar]
- 17. Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech J‐W, van't Veer M, Bär F, Hoorntje J, Koolen J, Wijns W, de Bruyne B. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5‐year follow‐up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105–2111. [DOI] [PubMed] [Google Scholar]
- 18. Toth G, Hamilos M, Pyxaras S, Mangiacapra F, Nelis O, De Vroey F, Di Serafino L, Muller O, Van Mieghem C, Wyffels E, Heyndrickx GR, Bartunek J, Vanderheyden M, Barbato E, Wijns W, De Bruyne B. Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J. 2014;35:2831–2838. [DOI] [PubMed] [Google Scholar]
- 19. De Bruyne B, Pijls NH, Heyndrickx GR, Hodeige D, Kirkeeide R, Gould KL. Pressure‐derived fractional flow reserve to assess serial epicardial stenoses: theoretical basis and animal validation. Circulation. 2000;101:1840–1847. [DOI] [PubMed] [Google Scholar]
- 20. Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van't Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF; FAME Study Investigators . Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–224. [DOI] [PubMed] [Google Scholar]
- 21. De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, Jagic N, Möbius‐Winkler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engström T, Oldroyd KG, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Jüni P, Fearon WF; FAME 2 Trial Investigators . Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991–1001. [DOI] [PubMed] [Google Scholar]
- 22. Authors/Task Force members , Windecker S, Kolh P, Alfonso F, Collet J‐P, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio‐Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–2619. [DOI] [PubMed] [Google Scholar]
- 23. Lee JM, Doh J‐H, Nam C‐W, Shin E‐S, Koo B‐K. Functional approach for coronary artery disease: filling the gap between evidence and practice. Korean Circ J. 2018;48:179–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crystal GJ, Klein LW. Fractional flow reserve: physiological basis, advantages and limitations, and potential gender differences. Curr Cardiol Rev. 2015;11:209–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kim HY, Lim H‐S, Doh J‐H, Nam C‐W, Shin E‐S, Koo B‐K, Yoon M‐H, Tahk S‐J, Kang DK, Song YB, Hahn JY, Choi SH, Gwon HC, Lee SH, Kim EK, Kim SM, Choe Y, Choi JH. Physiological severity of coronary artery stenosis depends on the amount of myocardial mass subtended by the coronary artery. JACC Cardiovasc Interv. 2016;9:1548–1560. [DOI] [PubMed] [Google Scholar]
- 26. Ahmadi A, Stone GW, Leipsic J, Serruys PW, Shaw L, Hecht H, Wong G, Nørgaard BL, O'Gara PT, Chandrashekhar Y, Narula J. Association of coronary stenosis and plaque morphology with fractional flow reserve and outcomes. JAMA Cardiol. 2016;1:350–357. [DOI] [PubMed] [Google Scholar]
- 27. Merz AA, Cheng S. Sex differences in cardiovascular ageing. Heart. 2016;102:825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kelsey SF, James M, Holubkov AL, Holubkov R, Cowley MJ, Detre KM. Results of percutaneous transluminal coronary angioplasty in women. 1985–1986 National Heart, Lung, and Blood Institute's Coronary Angioplasty Registry. Circulation. 1993;87:720–727. [DOI] [PubMed] [Google Scholar]
- 29. Chandrasekhar J, Baber U, Sartori S, Faggioni M, Aquino M, Kini A, Weintraub W, Rao S, Kapadia S, Weiss S, Strauss C, Toma C, Muhlestein B, DeFranco A, Effron M, Keller S, Baker B, Pocock S, Henry T, Mehran R. Sex‐related differences in outcomes among men and women under 55 years of age with acute coronary syndrome undergoing percutaneous coronary intervention: results from the PROMETHEUS study. Catheter Cardiovasc Interv. 2017;89:629–637. [DOI] [PubMed] [Google Scholar]
- 30. Udell JA, Koh M, Qiu F, Austin PC, Wijeysundera HC, Bagai A, Yan AT, Goodman SG, Tu JV, Ko DT. Outcomes of women and men with acute coronary syndrome treated with and without percutaneous coronary revascularization. J Am Heart Assoc. 2017;6:e004319 DOI: 10.1161/JAHA.116.004319. [DOI] [PMC free article] [PubMed] [Google Scholar]


