Abstract
Introduction:
Identifying the learners’ problems early enough and providing advice from the beginning is definitely an important investment in the training and progress of future practitioners. The current review aimed at examining factors related to academic failure of the preclinical medical students.
Methods:
The study was carried out as a systematic search of publications in the following databases published from January 1987 to January 2018: PubMed, Web of Knowledge, Educational Resources, Information Center and Scopus. No language limitation was set for searching the resources. As a comprehensive search, the following keywords were used for the abstract, title and keyword sections: academic performance, academic failure, academic achievement, drop out, academic engagement, learning disorder, medical student, struggle student and problem learner. A valid tool (STROBE) was used to determine the quality of the articles.
Results:
Most articles discussed personal causes, 7 discussed learning style, 7 discussed personality traits, 6 discussed motivational strategies and self‐efficacy, 4 discussed quality of sleep, 4 discussed the effect of stress, 9 discussed demographic factors, 3 discussed physical activity, 1 discussed coping strategies, 2 discussed class attendance and 4 discussed study strategy. Twenty-five articles described instructional design cause, 3 described teaching strategies, 2 described course assessments, 1 described the course structure, 3 described critical thinking, 3 described blended learning, 13 described predictive courses, 14 described admission tests, 1 described the learning environment, 2 described curriculum planning and 3 described the pre-matriculation program.
Conclusion:
Medical teachers often do not know which students are problem learners or what causes academic failure. The goal of this systematic review was to determine the origin of problems in learning to identify problem learners. The results indicates that managers, policymakers, instructors and counselors can monitor student academic achievement by careful planning of instructional design, attention to an educational environment, use of active teaching methods, continuous assessment of students and consideration of personal factors.
Keywords: Academic failure , Medical student , Medical education
Introduction
Medical teachers often work with students who have problems. Some of these students have knowledge deficits while others have attitude or behavioral problems (1). Sometimes, it is hard to understand if a learner is presenting with a problem. Distinguishing learner issues early and giving guidance from the beginning is an essential investment in the training and growth of potential practitioners. It will also help clinical educators, program directors and faculty developers (2).
The National Board of Internal Medicine (1999) has described the problem student as a trainee who reveals substantial problems that need the treatment of a program director or senior resident. Van, et al. (1998) describes a problem student as one with affective, cognitive, structural, and interpersonal problems (3). Therefore, the problem student is a learner who does not meet the objectives of the training program due to a substantial problem with knowledge, attitude or skill (4).
Studies revealing on the prevalence of problem students are limited (5,6). The rates vary from 5.8% around a 4-year period in a psychiatry program (6) to 9.1% around a 25-year period in a family medicine program (7). The absolute problems determined by educators were inefficient medical knowledge (48%), bad clinical judgment (44%) and inadequate use of time (44%) (2). Another study provides insufficient knowledge, attitudinal problems, interpersonal conflict, psychological illness, family tension and material abuse (7).
It is hard to recognize a struggle student. Improved counseling and supervision might impose economic costs on the resources of both the program and the faculty. Some medical teachers are worried that a troublesome learner may have a negative effect on educational programs and classmates. Medical educators would like to be able to predict who will become a problem learner, but studies predict different factors (8).
The reasons underlying the continuous scientific investigation of this phenomenon are based on the complexity of the factors involved (1,2). The different definitions of academic success and failure (2,3) make systematic comparison of research results difficult. There is rarely one single reason that determines why a student will leave or stay in a program (8,9). They seem to be the product of complex interactions between individual student factors and institutional and professional factors (1,2). Unfortunately, studies on academic success or failure have not been consistent with regard to the different factors (1,9). To identify students at risk of academic failure, the factors associated with it must be identified. A comprehensive and systematic investment of the academic failure literature to date has not focused on the factors that affect problem learners.
The current study focused on preclinical dropouts because previous studies have revealed that half of all medical dropouts were first year dropouts and that the factors influencing first year dropouts differed from those for later dropouts (9,10). By identifying the problem learner in the preclinical phase, academic failure can be prevented in the clinical phase, which is important for identifying and preventing the problem learner.
The complexity and implications of this issue can provide a pivotal approach with which managers, policymakers, instructors and counselors can monitor student academic failure. It is a priority to synthesize the evidence developed through high-quality studies to obtain useful information to reduce failure and promote success of medical students and to provide directions for future research. This systematic review describes the factors related to the problem learner in a preclinical medical career.
Methods
The present systematic review intends to determine the causes of academic failure in preclinical medical students.
The databases from January 1987 to January 2018 were searched because the outset of this topic, i.e. problem learner, was in 1987 in PubMed, Web of Knowledge (Thomson Reuters), Educational Resources and Information Center (ERIC) and Scopus.
An expert in systematic reviews developed a comprehensive and systematic search strategy using keywords about problem learners and the unique functions associated with each database searched (medical subject headings [MeSH], truncation symbols and Boolean operators). The reference lists of included articles were reviewed to identify other articles meeting the inclusion criteria. The ontological search was for keywords related to the problem learner. Those chosen were: academic performance, academic failure, academic achievement, drop out, academic engagement, learning disorder, medical student, struggling student, problem learner (Table 1).
Table 1.
Search strategies for different databases
| Pubmed: ("academic performance"[MeSH Terms] OR academic performance [Text Word] OR "academic performance" OR "performance, academic" OR "performance, academic" OR "academic test performance" OR "academic test performance" OR "performance, academic test" OR "test performance, academic" OR "academic test scores" OR "academic test score" OR "score, academic test" OR "test scores, academic" OR "educational test scores" OR "educational test score" OR "score, educational test" OR "scores, educational test" OR "test score, educational" OR "test scores, educational" OR "educational test performance" OR "educational test performances" OR "performance, educational test" OR "performances, educational test" OR "test performance, educational" OR "test performance, educational") OR ("academic failure" OR "failure, academic" OR "failure, academic" OR "academic failure"[MeSH Terms] OR academic failure [Text Word]) OR ("academic success" OR "success, academic" OR "success, academic" OR "academic achievement" OR "academic achievements" OR "achievement, academic" OR "achievements, academic" OR "academic success" [MeSH Terms] OR academic achievement [Text Word]) OR drop out) OR (academic [All Fields] AND engagement [All Fields] OR "academic successes" OR "success, academic" OR "successes, academic" OR "academic achievement" OR "academic achievements" OR "achievement, academic" OR "achievements, academic")) OR ("learning disorders"[MeSH Terms] OR learning disorder [Text Word]) AND ("students, medical" [MeSH Terms] OR medical student [Text Word] OR "medical students" OR "student, medical" OR "medical student") OR problem learner) |
| Scopus: (TITLE-ABS-KEY (academic AND performance)) OR (TITLE-ABS-KEY ( academic AND performances)) OR (TITLE-ABS-KEY (academic AND test AND performance)) OR (TITLE-ABS-KEY (academic AND test AND performances)) OR (TITLE-ABS-KEY (performance AND academic AND test)) OR (TITLE-ABS-KEY (educational AND test AND score*)) OR (TITLE-ABS-KEY (educational AND test AND performance)) OR (TITLE-ABS-KEY (performances AND educational AND test)) OR (TITLE-ABS-KEY (test AND performance AND educational)) OR (TITLE-ABS-KEY (academic AND failures)) OR (TITLE-ABS-KEY (academic AND successes)) OR (TITLE-ABS-KEY (academic AND achievement)) OR (TITLE-ABS-KEY (academic AND success)) OR (TITLE-ABS-KEY (drop AND out)) OR (TITLE-ABS-KEY (academic AND engagement)) OR (TITLE-ABS-KEY (academic AND successes)) OR (TITLE-ABS-KEY (academic AND achievement)) OR (TITLE-ABS-KEY (learning AND disorder*)) OR (TITLE-ABS-KEY (academic AND performance)) OR (TITLE-ABS-KEY (educational AND development)) OR (TITLE-ABS-KEY (academic AND achievement)) AND (TITLE-ABS-KEY (medical AND student*)) OR (TITLE-ABS-KEY (problem AND learner)) OR (TITLE-ABS-KEY (medical AND college AND student)) OR (TITLE-ABS-KEY (medical AND undergraduate AND student)) |
| ISI: (TS = (academic performance) OR TS = (academic failure) OR TS = (academic successes) OR TS = (academic achievement) OR TS = (academic engagement) OR TS = (drop out) OR TS = (learning disorder)) AND (TS = (medical student) OR TS = (problem learner)) |
| ERIC: ((academic performance) OR (academic failure) OR (academic success) OR (academic achievement) OR (academic engagement) OR (drop out) OR (learning disorder)) AND ((medical student) OR (problem learner)) |
Two independent researchers applied the inclusion criteria (see: Study eligibility) to the database hits by first reviewing each study title and abstract. The full text of the study was subsequently reviewed if the study appeared to meet the selection criteria or if there was any doubt regarding eligibility. A third independent researcher resolved any disagreements. Hand searching was also carried out in the Medical Teacher and Medical Education journals. Reference lists of all papers meeting the quality criteria were reviewed to identify and select the relevant papers. The most prominent authors were contacted with a request for gray literature: conference proceedings, unpublished studies, internal reports, etc., and the data was included in the study.
The studies that met the inclusion criteria were selected. Table 2 shows the inclusion and exclusion criteria of the systematic review. A second generation search of the list of papers was performed by searching (reference lists of the included studies) and forward tracing (as cited by Scopus and Google Scholar). The corresponding authors were contacted for additional information or full-text requests.
Table 2.
Inclusion and exclusion criteria
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Population | Medical student | Other health promotion |
| Subject | Causes of failure undergraduate medical program | |
| Study design | Case study, cohort, cross-sectional | Secondary research |
| Language | No limitation | |
| Time | 1987-2018 | |
Quality assessment
The quality of the included studies was evaluated by two researchers using standardized critical appraisal tools using STROBE guidelines. STROBE was selected because most of the studies were observational; hence, many elements of CONSORT did not apply and because the STROBE guidelines have been endorsed by over 100 journals (http://www.strobe-statement.org) (11-14).
Most articles (57 articles) were of high-quality 15-22 and 32 were of medium-quality (8-14). No low-quality papers were included. All the papers were compared using the following categories: title and abstract, introduction, methods, results, discussion, data collection methods, and other information. A total of 22 items were considered relevant: the article title and abstract (1 item), introduction (2 items), methods (8 items), results (5 items), discussion sections (4 items), and other information (1 item). Eighteen items were common to all three designs and four were design unique with various versions for all or selection of an item. For many items (asterisk), information was presented with independently for case and control groups in case-control studies, or exposed and unexposed groups in cohort and cross-sectional studies. The most commonly met indicators were analysis of the results and conclusions of data. On many occasions, the data collection method was not clear due to insufficient data, although the data gathering method was reliable and valid for the research question and context (Table 3).
Table 3.
Quality of studies included
| Items on checklist | Details | Indicator met | Indicator not met |
|---|---|---|---|
| Title and abstract | Study design, providing the abstract with an informative and balanced summary | 42 | 47 |
| Introduction | Scientific background and rationale, specific objectives | 44 | 45 |
| Methods | Key elements of study design, setting, participants, variables, data sources/measurement*, bias, study size, quantitative variables, statistical methods | 21 | 68 |
| Results | Participants*, descriptive data,* outcome data*, main results, other analyses | 52 | 37 |
| Discussion | Key results, limitations, interpretation, generalizability | 49 | 40 |
| Other information | Funding | 10 | 79 |
Disagreements were resolved by discussion with a third independent researcher. Scores were calculated using the appropriate tool. The researchers extracted the following data using a purpose-built, standardized data-extraction tool:
Personal effective factors, learning style, demographic, personality trait, stress, quality of sleep, study strategies, self-efficacy, critical thinking, curriculum (teaching strategies, environment, admissions test)
Type of study
Definition of academic achievement
Measurement method
Agreement between the researchers on the methodological quality of the studies was established as the percentage of agreement and the Kappa statistic. Frequency tables were used to summarize the study characteristics. The details of the causes leading to problem learning were summarized. Statistical integration of the data was not possible as there was no consistency in the areas of effective factors, designs employed or measures of effectiveness assessed. The synthesis of findings was integrated by narrative structured to address the objectives of the review.
Results
Summary of study characteristics
Number of studies
The search identified 6305 abstracts and 480 articles were selected for further review. The final review included 90 articles. The majority of articles [80] were identified from electronic databases and the balance [10] was identified from reference lists. The articles were most likely on medical education and medical teachers (Figure 1).
Figure1.
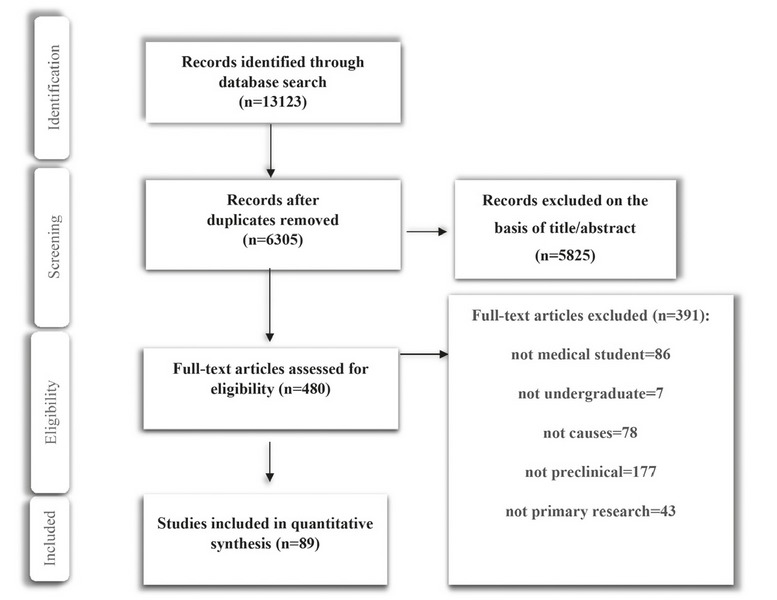
Study flowchart demonstrates the inclusion-exclusion process
Source of studies
The majority of studies [31] were carried out in Asia, followed by Europe [24] and the USA [24], Australia [7] and South Africa [4].
Type of design
The majority design in the articles was cross-sectional, following by cohort and case control (Table 4).
Table 4.
Causes and design of articles
| Total number of articles and reference number(s) | R (Pearson) | |||
|---|---|---|---|---|
| Type of design | Cross sectional (N=48) | (9,10, 13-58) | ||
| Cohort (N=25) | (59-83) | |||
| Case control (N=17) | (84-99) | |||
| Causes of academic failure | Instructional design | Teaching strategies | (68,90,99) | |
| In course assessment | (87,89) | |||
| Structure of course | (96) | |||
| Critical thinking | (33,38,48) | |||
| Blended learning | (88,93,94) | |||
| Predictive courses | (9,10,18,24, 27,49,59,62, 64,65,73,79, 85) | Chemistry (r=0.35) | ||
| Physics (r=0.19) | ||||
| Anatomy (r=0.66) | ||||
| Physiology (r=0.52) | ||||
| Biochemistry (r=0.65) | ||||
| Personal causes | Learning style | (13,26,31,32, 36,39,54) | ||
| Personality trait | (19,22,25,30, 40,75,86) | |||
| Motivation strategy | (23,28,29,42, 72,83) | |||
| Self‐efficacy | (25,34,41,50, 78,84) | R=0.19 | ||
| Quality of sleep | (14,15,17,97) | |||
| Effect of stress | (37,51,67,80) | R=-0.3 | ||
| Demographic factors | (18,20,66,69, 70,71,82,83, 92) | |||
| Physical activity | (44,53,76) | |||
| Coping strategies | (46) | |||
| Class attendance | (35,43) | |||
| Study strategies | (56,58,67,73) | R=0.4 | ||
| Admission test | (16,21,42,45, 57,60,61,71, 74,75,77,82, 91,96) | |||
| Learning environment | (55) | |||
| Curriculum planning | (63,81) | |||
| Pre-matriculation program | (47,52,98) | |||
Aims of studies
The aim of the studies was to report on the causes of academic failure in preclinical medical courses (Table 4).
Definition of academic failure
Using the articles obtained in the data extraction phase, the definition of academic failure in Jiraporncharoen (2015) was less than 3 out of 5 [32], in Shantakumar (2017) was below 60% [97] and in Abdulghani (2012) was less than 3.75 out of 5 14. Other articles defined it as failing to pass the test.
Causes of academic failure
Most articles referred to personal causes. Seven articles referred to learning style, seven to personality traits, six to motivational strategies and self-efficacy, four to quality of sleep, four to effect of stress, nine to demographic factors, three to physical activity, one to coping strategies, two to class attendance and four to study strategies (Table 2). Twenty-five articles described instructional design cause, three teaching strategies, two course assessment, one structure of course, three critical thinking, three blended learning, and 13 predictive courses (Table 2). Fourteen articles described admission tests, one learning environment, two curriculum planning and three pre-matriculation programs. A more detailed overview of the synthesis of the research evidence is provided below. The findings were synthesized into six categories and 17 subcategories.
Instructional design
Teaching strategies
Koles (2010) found that TBL enhances mastery of course content. Students in the lowest academic quartile may benefit more than the highest quartile students from TBL strategy (68). Williams (2017) confirmed that academic performance improves with a self-directed teaching approach (99). Rashid-Doubell, et al. found that ARS (audience response system) did not improve academic performance in a preclinical course, but students reported that the use of clickers during lectures provided a more interactive learning environment, increased student participation, promoted active-learning and helped students identify gaps in knowledge (90). Three articles used quality assessment and the power of the evidence to indicate that the use of active strategies can prevent a problem learner.
Course assessment
Poljicanin (2009) found that daily quizzes were associated with better academic success in an anatomy course (87). Pratten (2014) also confirmed that short frequent objective-led summative assessments of individuals in a group context can effectively increase individual active engagement and improve academic achievement 89. Two articles were found in which the power of evidence showed that formative evaluation can prevent the problem learner.
Structure of course
Salopek (2009) found that the type of temporal delivery of a basic course in a medical curriculum is not a major determinant of student academic courses when delivered in alternating temporal blocks or when spread over the academic year (95). One article addressed this subject, which was not sufficient for comment and there was need for an original article.
Critical thinking
Joshi (2012) found a positive correlation between emotional intelligence and academic performance in undergraduate medical students (33). Lee (2016) showed that critical thinking may be a meaningful factor for predicting academic achievement. He investigated the effect of multiple mini-interviews as a predictor of academic achievement. The results showed that critical thinking skills predicted academic success during the preclinical years of medical education (38). Scott (1994) confirmed that critical thinking skills were moderately predictive of academic success during the preclinical years of medical education (48). Three articles addressed the topics of critical thinking and quality assessment and the power of evidence and showed that fostering critical thinking in medical students could avert the development of a problem learner.
Blended learning
Popovic (2018) found that Moodle accompanied by lectures increased the interest of students, attendance at face-to-face lectures and formative and summative scores (88). Romanov (2007) confirmed that lectures with eLearning materials have a positive correlation with academic achievement (93). Sajid (2016) highlighted blended learning as helpful for exam preparation and concept clarification, but did not find a significant increase in academic performance of students taught using this method (94). The three articles about blended learning, according to quality assessment and the power of evidence showed that using blended learning was one element for preventing problem learners.
Predictive courses
Six articles indicated that biology was the best predictor of optimal academic performance in preclinical medical students (9,18,59,64,73,85), nine articles indicated chemistry and physics (9,10,24,27,59,62,64,73,85), five articles highlighted mathematics (27,59,62,64,85) and one article cited anatomy, physiology and biochemistry (85). hree articles highlighted the importance of the first semester (65,79), one article high school grade (18) and two articles previous university (18,70). Thirteen articles addressed this subject and the power of evidence showed that students with high grades in biology, chemistry and physics were less likely to drop out of medical school.
Based on the results, score in chemistry showed a relatively stronger and significant relationship with the MBBS professional examinations compared with other science subjects. The correlation was significant (r= 0.35); for physics it was not significant at all (r=0.19). Positive correlations were found between the premedical year grade point average (pre-MD GPA) and anatomy, physiology, and biochemistry scores (R =0.664, 0.521, and 0.653).
Pre-matriculation program
Schneid (2018) found that pre-matriculation programs could help students to succeed in the first year of medical school (47). Strayhorn (1999) indicated that summer premedical programs were suitable for determining whether participants would be able to handle the academic rigors of medical school (52). Tucker (2008) confirmed this finding (98). Three articles showed that a power of evidence pre-matriculation program could prevent a medical student from dropping out.
Personal causes
Learning style
Two studies found that assimilators received significantly higher grades in theoretical examinations than the other groups (13,26), one study highlighted convergent style (13), another study highlighted a sensing-intuitive learning style (31) another indicated a reflective learning style (32), another cited competition (36) and two studies reported no correlation between learning style and academic achievement (39,54). Seven articles on this subject showed that quality assessment, assimilators and sensing-intuitive learning style have positive correlations with preventing academic failure in preclinical medical students.
Personality traits
Bhagat (2016) found a significant correlation between academic achievement and negative emotionality (19), but Guntern (2017) showed that emotional stability predicts perceived pre-clinical academic achievement (25). One article showed no correlation (22) and two showed that conscientiousness style predicted pre‐clinical academic achievement (25,40), another cited agreeableness (30) and one cited extraversion (25). Seven articles found, according to the power of evidence, that emotional stability, conscientiousness and agreeable personality have correlation with academic achievement.
Motivation strategies
Five articles showed a correlation (23,28,29,72,83) and one article showed no correlation (42). Five articles showed significant but moderate relationships between academic performance and the motivation strategies subsumed within the categories of task value and self-efficacy for learning performance. The power of evidence of the six articles suggests that motivational strategies have a positive correlation with academic achievement.
Self-efficacy
Four articles showed a correlation (25,41,50,78) and one article showed no correlation (34). Based on the power of evidence, five articles showed a relationship between self-efficacy and academic performance. The results indicated positive a correlation between self-efficacy and academic achievement (r=0.19).
Quality of sleep
According to the power of evidence, all four articles about the effect of sleep on academic achievement confirm sleep deprivation is negatively associated with academic performance in medical students (14,15,17,97).
Effect of stress
According to the power of evidence, all four articles about the effect of stress on academic achievement confirmed that higher levels of stress were associated with poor academic performance (37,51,67,80). The result showed there was moderate negative (-0.3) and significant correlation between academic performance and stress.
Demographic factors
The three studies showed different results. Bastias (2000) and Mann (2010) found a significant correlation between academic failure and being native (18,70), but Malau-Aduli (2017) showed Indigenous status had strong risk factors associated with academic difficulty (69). One article indicated lower socioeconomic status and parental marital problems were important factors (20). Another one indicated being the first in the family (FIF) to go to university was important (69), two highlighted parental education had a positive correlation with academic failure (71,83), another found a significantly higher risk for dropout was in the students above 21 years of age at university (91) and one study showed that minorities had a positive correlation with academic success (82). According to the power of evidence, demographic factors such as parental education, FIF and being over 21 years of age correlated with dropping out by the preclinical medical students.
Physical activity
Two studies showed physical activity and recreation increased students’ focus and could help them to succeed academically (44,76). study indicated that a high body mass index in female medical students impaired academic performance (53). According to the power of evidence, physical activity had a positive correlation with academic performance.
Coping strategies
Schiller (2018) stated that coping strategies were unrelated to preclinical academic performance (46). One article addressed this subject, so it was not possible to determine a result about this subject. It requires more original research.
Class attendance
Two studies highlighted class attendance during teaching sessions as having a direct impact on examination results. Students with poor attendance were at risk of failure of examinations (35,43). This is in line with the power of evidence.
Study strategies
The power of evidence suggests from all four articles confirmed the effect of study strategies on academic achievement. Study strategies are positively associated with academic performance in medical students (56,58,67,73). The results showed time management had moderate correlation (0.3) with academic performance
Admission test
Of 13 articles indicating that the MCAT score was a strong predictor of medical school performance, two indicated the multifaceted selection process. They suggest that, in addition to measuring of academic variables, the measuring of ethical and interpersonal attributes might help in selection of applicants with the greatest potential to succeed in medical education (16,96). One article showed no correlation between admission test score and academic failure (61). Three articles indicated medical college admission tests or student undergraduate grade-point average or both could identify individual students who were academically at risk (21,45,77). According to the power of evidence, multifaceted selection procedure seemed to be predictive of academic achievement.
Learning environment
Wayne (2013) found that a positively perceived learning environment added to better academic performance (55). There was only one study in this regard; thus, no definite conclusion can be made about the positive perception of the learning environment and academic achievement.
Curriculum planning
Iputo (2005) showed that the adoption of PBL⁄CBE curriculum had a positive impact on the dropout rate (63). Another study indicated that extended course duration had a correlation with academic achievement (81). According to the power of evidence, attention to curriculum planning can reduce the attrition rate
Discussion
This was the first systematic review to examine the causes of academic failure in preclinical medical students. This systematic review identified 89 studies and several conclusions could be drawn from the results. The framework for problem learners indicates that when teachers first suspect a challenge, they should ask themselves three questions in order to confirm their suspicions: What's the problem? Whose problem is it? Is it a problem that can be changed (2).
In this systematic review, the causes of academic failure were distinguished and categorized for the learner, teacher and system. The causes for the learner are personal, the causes for the teacher are factors relevant to instructional design and the causes for the system are admission tests, learning environment, curriculum planning and pre-matriculation program.
Teacher issues
Teachers may label a medical student as a problem because he/she cannot fulfill the role that should be fulfilled (1). Teachers also enter medical school with specific expectations and experiences, all of which can lead to problems. Teachers should try to carefully assess to what extent they are contributing to the identified problem. One item related to the teacher is teaching strategies. If a teacher fails to use active teaching or a student-centered method, it may not be possible to identify gaps in student knowledge that will affect academic achievement. Formative evaluation in the form of daily quizzes was associated with better academic.
Success in the medical courses affects student success in the first two years of medical school by fostering critical thinking through effective teaching and evaluation. Limited use of problem solving methods, class discussions, questions and answers, and other methods of fostering thinking skill as well as the lack of encouragement of students to seek solutions by themselves prevent the growth of critical thinking in medical students. The use of evaluation methods based on memorization of a large amount of theoretical information is inapplicable and leads to learning without thinking and reasoning. This may cause academic failure.
Blended learning and flipped classrooms improve student learning and the lack of it may cause academic failure. Predictive courses indicate that students who scored high grades in biology, chemistry and physics were less likely to drop out of medical school. Those for whom prior achievement are likely to experience a downwardly biased indicator of future potential. This is a warning for teachers for early identification of a problem learner. Only one article on structure showed no correlation, but this cannot be confirmed with such a small sample size. More original articles are required. If medical teachers pay more attention to such variables as teaching strategies, student evaluation and curriculum planning, they are more likely to prevent academic failure.
Learner issues
In addition to gaps in knowledge, attitudes or skills, learner problems can include learning style, personality traits, lack of motivation and self-efficacy, quality of sleep, stress, demographic factors, physical activity, coping strategy, class attendance and study strategy. In consequence, students should be encouraged to be flexible in their own learning styles in order to be able to engage successfully in varying teaching methods across the curriculum. Teachers also should be motivated to provide a variety of teaching materials and resources to suit different learning styles. Faculty members must pay attention to differences in personality traits among students and use teaching methods that address the individual differences of students. They should guide these students to study based on their personal differences and try to coordinate these styles.
Student motivation may be an important determinant of academic achievement. Students must be taught how to regulate their learning behavior, receive sufficient instruction and obtain support from teachers. There is need for curricular/extracurricular education and counseling about healthy sleep patterns, effective stress management, and increased level of social literacy about problems related to the social status of families. Counseling and guidance services can help to prevent and identify problem learners and can encourage physical activity, monitor attendance in class and participation in the learning process and organize study skills.
System issues
System problems are often difficult to identify and can include admission tests, learning environment, curriculum planning and pre-matriculation program. Multifaceted selection procedures seem to be predictive of academic achievement. The sole use of test scores without interviews (non-academic performance) increase dropout rates. The perceived learning environment can improve academic performance, but the lack of enough articles requires additional primary research.
PBL curriculum has a positive impact on students from disadvantaged educational backgrounds to reduce attrition rates. Longer medical curriculum, and block/modular subject structure were associated with better academic outcomes and lower attrition; thus, curriculum planning can reduce the attrition rate. Grades on examinations in pre-matriculation programs have the potential to help identify students who are at risk of failing.
The results of this systematic review should be taken in the context of a specific cultural and educational environment. In American universities, the emphasis is more student-centered. In Iran, the teaching method is teacher-centered and the result is a lack of creativity and inventiveness by the students. The infrastructure (e.g. educational facilities) should be improved. Textbooks and educational content should be dynamic, collaborative and low-volume, instead of a large number of students in the classroom with a non-cooperative and heavy educational content. In Iran, student acceptance is based on quotas (konkoor), but universities in America and the West consider skills such as intelligence and talent and how to communicate and interact with friends when they enter the university. There is a cultural difference between Iranian and foreign students.
Conclusion
Medical teachers often cannot identify a problem learner and the causes of academic failure. The goal of this systematic review was to determine the reason behind the failure of a problem learner. The results suggested that managers, policymakers, instructors and counselors can monitor student academic achievement with careful planning for instructional design, educational environment, the use of active teaching methods and continuous assessment of students and consideration of personal factors.
Strengths and weaknesses
One limitation of the study was the lack of meta-analysis; however, a meta-analysis was not possible because of the different study designs, measurement tools and the nature of the results reported. But there was strength in our review because there was no language limitation and a checklist of 22 quality indices.
Acknowledgement
This study is the result of a PhD thesis at Shahid Beheshti University of Medical Sciences by the second author.
Conflict of Interest:The authors declare no conflicts of interest.
References
- 1.Steinert Y, Levitt C. Working with the ‘‘problem’’ resident: Guidelines for definition and intervention. Fam Med. 1993; 25(10):627–32. [PubMed] [Google Scholar]
- 2.Steinert Y. The ‘‘problem’’ learner: Whose problem is it? AMEE Guide No. 76. Med Teach. 2013; 35:e1035–e1045. doi: 10.3109/0142159X.2013.774082. [DOI] [PubMed] [Google Scholar]
- 3.Vaughn LM, Baker RC, DeWitt TG. The problem learner. Teach Learn Med. 1998; 10(4):217–22. [Google Scholar]
- 4.Steinert Y. The ‘problem’ junior: Whose problem is it? BMJ. BMJ. 2008;336(7636):150–3. doi: 10.1136/bmj.39308.610081.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roback HB, Crowder MK. Psychiatric resident dismissal: A national survey of training programs. Am J Psychiatry. 1989; 146(1):96–8. doi: 10.1176/ajp.146.1.96. [DOI] [PubMed] [Google Scholar]
- 6.Yao DC, Wright SM. National survey of internal medicine residency program directors regarding problem residents. JAMA. 2000; 284(9):1099–104. doi: 10.1001/jama.284.9.1099. [DOI] [PubMed] [Google Scholar]
- 7.Reamy BV, Harman JH. Residents in trouble: An in-depth assessment of the 25-year experience of a single Family Medicine residency. Fam Med. 2006; 38(4):252–7. [PubMed] [Google Scholar]
- 8.Hays RB, Lawson M, Gray C. Problems presented by medical students seeking support: A possible intervention framework. Med Teach. 2011; 33(2):161–4. doi: 10.3109/0142159X.2010.509415. [DOI] [PubMed] [Google Scholar]
- 9.Arulampalam W, Naylor RA, Smith JP. Dropping out of medical school in the UK: explaining the changes over ten years. Med Edu. 2007;41(4): 385–94. doi: 10.1111/j.1365-2929.2007.02710.x. [DOI] [PubMed] [Google Scholar]
- 10.Adoukonou T, Tognon-Tchegnonsi F, Mensah E, Allode A, Adovoekpe JM, Gandaho P, et al. Predictors of success among first-year medical students at the University of Parakou. Pan Afr Med J. 2016;23(1): 1–7. doi: 10.11604/pamj.2016.23.87.8527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 12.Haynes RB, Mulrow CD, Huth EJ, Altman DG, Gardner MJ. More informative abstracts revisited. Ann Intern Med. 1990;113:69–76. doi: 10.7326/0003-4819-113-1-69. [DOI] [PubMed] [Google Scholar]
- 13.Ogut E, Senol Y, Yildirim FB. Do learning styles affect study duration and academic success? European Journal of anatomy. 2017;21(3):235–40. [Google Scholar]
- 14.Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AM, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34(1): S37–41. doi: 10.3109/0142159X.2012.656749. [DOI] [PubMed] [Google Scholar]
- 15.Alfakhri L, Sarraj J, Kherallah S, Kuhail K, Obeidat A, Abu-Zaid A. Perceptions of pre-clerkship medical students and academic advisors about sleep deprivation and its relationship to academic performance: A cross-sectional perspective from Saudi Arabia Medical Education. BMC Research Notes. 2015;8(1): 1–7. doi: 10.1186/s13104-015-1755-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alnasir FA, Jaradat AA. The effectiveness of AGU-MCAT in predicting medical student performance in year one of the College of Medicine of the Arabian Gulf University. Educ Health (Abingdon) . 2011;24(2):447. [PubMed] [Google Scholar]
- 17.BaHammam AS, Alaseem AM, Alzakri AA, Almeneessier AS, Sharif MM. The relationship between sleep and wake habits and academic performance in medical students: a cross-sectional study. BMC Medical Education. 2012; 12: 61. doi: 10.1186/1472-6920-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bastias G, Villarroel L, Zuniga D, Marshall G, Velasco N, Mena B. Academic performance of medical students: a predictable result? . Rev Med Chil. 2000;128(6):671–8. [PubMed] [Google Scholar]
- 19.Bhagat V, Haque M, Bin Simbak N, Jaalam K. Study on personality dimension negative emotionality affecting academic achievement among Malaysian medical students studying in Malaysia and overseas. Advances in Medical Education and Practice. 2016; 7(1): 341–6. doi: 10.2147/AMEP.S108477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biggs JSG, Najman JM, Schulz EB, Williams G. Parental problems influencing the academic-achievement of medical-students - a prospective-study. Med Educ. 1991;25(5): 374–82. doi: 10.1111/j.1365-2923.1991.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 21.Burns ER, Garrett J. Student failures on first-year medical basic science courses and the USMLE step 1: A retrospective study over a 20-year period. Anatomical Sciences Education. 2015;8(2): 120–5. doi: 10.1002/ase.1462. [DOI] [PubMed] [Google Scholar]
- 22.Davoudi F, Esmaeeli S, Ahmadzad Asl M, Nojomi M. Academic performance in Iranian medical students during the pre-clinical stage. Medical Journal of the Islamic Republic of Iran. 2017; 31(1): 1–7. doi: 10.18869/mjiri.31.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feri R, Soemantri D, Jusuf A. The relationship between autonomous motivation and autonomy support in medical students' academic achievement. Int J Med Educ. 2016;7(1): 417–23. doi: 10.5116/ijme.5843.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gautam AP, Paudel BH, Agrawal CS, Niraula SR, Dalen JV. Examination of relationship of scores obtained in grades 10 and 12 with the entry and success in undergraduate medical education. Kathmandu Univ Med J (KUMJ) 2012; 10(37): 66–71. doi: 10.3126/kumj.v10i1.6918. [DOI] [PubMed] [Google Scholar]
- 25.Guntern S, Korpershoek H, Van der Werf G. Benefits of personality characteristics and self-efficacy in the perceived academic achievement of medical students. Educational Psychology. 2017; 37(6): 733–44. [Google Scholar]
- 26.Gurpinar E, Alimoglu MK, Mamakli S, Aktekin M. Can learning style predict student satisfaction with different instruction methods and academic achievement in medical education? . Adv Physiol Educ. 2010;34(4):192–6. doi: 10.1152/advan.00075.2010. [DOI] [PubMed] [Google Scholar]
- 27.Haidinger G, Frischenschlager O, Mitterauer L. Prediction of success in the first-year exam in the study of medicine--a prospective survey. Wien Klin Wochenschr. 2005;117(23): 827–32. doi: 10.1007/s00508-005-0477-x. [DOI] [PubMed] [Google Scholar]
- 28.Hamid S, Singaram VS. Motivated strategies for learning and their association with academic performance of a diverse group of 1st-year medical students. African Journal of Health Professions Education. 2016;8(1): 104–7. [Google Scholar]
- 29.Hamid S, Singaram VS. Exploring the relationship between demographic factors, performance and fortitude in a group of diverse 1st-year medical students. African Journal of Health Professions Education. 2016; 8(1): 99–103. [Google Scholar]
- 30.Hemyari C, Zomorodian K, Ahrari I, Tavana S, Parva M, Pakshir K, et al. The mutual impact of personality traits on seating preference and educational achievement. European Journal of Psychology of Education. 2013; 28(3): 863–77. [Google Scholar]
- 31.Hernandez-Torrano D, Ali S, Chan CK. First year medical students' learning style preferences and their correlation with performance in different subjects within the medical course. BMC Medical Education. 2017; 17(1): 1–7. doi: 10.1186/s12909-017-0965-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jiraporncharoen W, Angkurawaranon C, Chockjamsai M, Deesomchok A, Euathrongchit J. Learning styles and academic achievement among undergraduate medical students in Thailand. J Educ Eval Health Prof. 2015; 12(1): 1–7. doi: 10.3352/jeehp.2015.12.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joshi SV, Srivastava K, Raychaudhuri A. A Descriptive Study of Emotional Intelligence and Academic Performance of MBBS Students. International Conference on Education & Educational Psychology. 2012; 69(1): 2061–7. [Google Scholar]
- 34.Khan HU, Khattak AM, Mahsud IU, Munir A, Ali S, Khan MH, et al. Impact of class attendance upon examination results of students in basic medical sciences. J Ayub Med Coll Abbottabad. 2003; 15(2): 56–8. [PubMed] [Google Scholar]
- 35.Khan AS, Cansever Z, Avsar UZ, Acemoglu H. Perceived Self-Efficacy and Academic Performance of Medical Students at Ataturk University, Turkey. Jcpsp-Journal of the College of Physicians and Surgeons Pakistan. 2013; 23(7): 495–8. [PubMed] [Google Scholar]
- 36.Kulac E, Sezik M, Asci H, Gurpinar E. Learning Styles, Academic Achievement, and Gender in a Medical School Setting. Journal of Clinical and Analytical Medicine. 2015; 6(5): 608–11. [Google Scholar]
- 37.Kumar M, Sharma S, Gupta S, Vaish S, Misra R. Effect of stress on academic performance in medical students: a cross sectional study. Indian J Physiol Pharmacol. 2014;58(1): 81–6. [PubMed] [Google Scholar]
- 38.Lee HJ, Park SB, Park SC, Park WS, Ryu SW, Yang JH, et al. Multiple mini-interviews as a predictor of academic achievements during the first 2 years of medical school. BMC Res Notes. 2016; 9(1): 93. doi: 10.1186/s13104-016-1866-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leiden LI, Crosby RD, Follmer H. Assessing learning-style inventories and how well they predict academic performance. Acad Med. 1990; 65(6): 395–401. doi: 10.1097/00001888-199006000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Lievens F, Coetsier P, De Fruyt F, De Maeseneer J. Medical students' personality characteristics and academic performance: a five-factor model perspective. Med Educ. 2002; 36(11): 1050–6. doi: 10.1046/j.1365-2923.2002.01328.x. [DOI] [PubMed] [Google Scholar]
- 41.Lucieer SM, Jonker L, Visscher C, Rikers RM, Themmen AP. Self-regulated learning and academic performance in medical education. Med Teach. 2016; 38(6): 585–93. doi: 10.3109/0142159X.2015.1073240. [DOI] [PubMed] [Google Scholar]
- 42.Luqman M. Relationship of Academic Success of Medical Students with Motivation and Pre-admission Grades. JCPSP, Journal of the College of Physicians and Surgeons Pakistan. 2013;23(1): 31–6. [PubMed] [Google Scholar]
- 43.Millis RM, Dyson S, Cannon D. Association of classroom participation and examination performance in a first-year medical school course. Adv Physiol Educ. 2009; 33(3): 139–43. doi: 10.1152/advan.00028.2009. [DOI] [PubMed] [Google Scholar]
- 44.Nayak SB, Miranda SA, Bin Fitzrol OJ, Anthony L, Gowrish SR, Aithal AP. The impact of physical activities on the academic performance of medical students. Online Journal of Health and Allied Sciences. 2016;15(2):1–5. [Google Scholar]
- 45.Poole P, Shulruf B, Rudland J, Wilkinson T. Comparison of UMAT scores and GPA in prediction of performance in medical school: a national study. Med Educ. 2012;46(2):163–71. doi: 10.1111/j.1365-2923.2011.04078.x. [DOI] [PubMed] [Google Scholar]
- 46.Schiller JH, Stansfield RB, Belmonte DC, Purkiss JA, Reddy RM, House JB, et al. Medical Students' Use of Different Coping Strategies and Relationship With Academic Performance in Preclinical and Clinical Years. Teaching and Learning in Medicine. 2018;30(1): 15–21. doi: 10.1080/10401334.2017.1347046. [DOI] [PubMed] [Google Scholar]
- 47.Schneid SD, Apperson A, Laiken N, Mandel J, Kelly CJ, Brandl K. A summer prematriculation program to help students succeed in medical school. Advances in Health Sciences Education. 2018; 1(3): 1–13. doi: 10.1007/s10459-017-9808-8. [DOI] [PubMed] [Google Scholar]
- 48.Scott JN, Markert RJ. Relationship between critical thinking skills and success in preclinical courses. Acad Med. 1994; 69(11): 920–4. doi: 10.1097/00001888-199411000-00015. [DOI] [PubMed] [Google Scholar]
- 49.Sitticharoon C, Srisuma S, Kanavitoon S, Summachiwakij S. Exploratory study of factors related to educational scores of first preclinical year medical students. Adv Physiol Educ. 2014;38(1):25–33. doi: 10.1152/advan.00162.2012. [DOI] [PubMed] [Google Scholar]
- 50.Sobral DT. Medical students' reflection in learning in relation to approaches to study and academic achievement. Med Teach. 2001; 23(5): 508–13. doi: 10.1080/01421590120042973. [DOI] [PubMed] [Google Scholar]
- 51.Sohail N. Stress and academic performance among medical students. J Coll Physicians Surg Pak. 2013;23(1): 67–71. [PubMed] [Google Scholar]
- 52.Strayhorn G. Participation in a premedical summer programme for underrepresented minority students as a predictor of academic performance in the first three years of medical school: two studies. Acad Med. 1999;74(4):435–47. doi: 10.1097/00001888-199904000-00043. [DOI] [PubMed] [Google Scholar]
- 53.Suraya F, Meo SA, Almubarak Z, Alqaseem YA. Effect of obesity on academic grades among Saudi female medical students at College of Medicine, King Saud University: Pilot study. Journal of the Pakistan Medical Association. 2017;67(8): 1266–9. [PubMed] [Google Scholar]
- 54.Urval RP, Kamath A, Ullal S, Shenoy AK, Shenoy N, Udupa LA. Assessment of learning styles of undergraduate medical students using the VARK questionnaire and the influence of sex and academic performance. Adv Physiol Educ. 2014; 38(3): 216–20. doi: 10.1152/advan.00024.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wayne SJ, Fortner SA, Kitzes JA, Timm C, Kalishman S. Cause or effect? The relationship between student perception of the medical school learning environment and academic performance on USMLE Step 1. Med Teach. 2013; 35(5): 376–80. doi: 10.3109/0142159X.2013.769678. [DOI] [PubMed] [Google Scholar]
- 56.West C, Sadoski M. Do study strategies predict academic performance in medical school? Med Educ. 2011;45(7): 696–703. doi: 10.1111/j.1365-2923.2011.03929.x. [DOI] [PubMed] [Google Scholar]
- 57.Bahri Yusoff MS, Abdul Rahim AF, Baba AA, Esa AR. Medical Student Selection Process and Its Pre-Admission Scores Association with the New Students' Academic Performance in Universiti Sains Malaysia. International Medical Journal. 2011;18(4): 329–33. [Google Scholar]
- 58.Zhou Y, Graham L, West C. The relationship between study strategies and academic performance. Int J Med Educ. 2016;7(1): 1219–26. doi: 10.5116/ijme.57dc.fe0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arulampalam W, Naylor R, Smith J. Factors affecting the probability of first year medical student dropout in the UK: a logistic analysis for the intake cohorts of 1980-92. Med Educ. 2004;38(5): 492–503. doi: 10.1046/j.1365-2929.2004.01815.x. [DOI] [PubMed] [Google Scholar]
- 60.Croen LG, Reichgott M, Spencer RK. A performancebased method for early identification of medicalstudents at risk of developing academic problems. Acad Med. 1991;66(8): 486–8. doi: 10.1097/00001888-199108000-00017. [DOI] [PubMed] [Google Scholar]
- 61.Farrokhi-Khajeh-Pasha Y, Nedjat S, Mohammadi A, Rad EM, Majdzadeh R, Monajemi F, et al. The validity of Iran's national university entrance examination (Konkoor) for predicting medical students' academic performance. BMC Medical Education. 2012;12(1): 1–8. doi: 10.1186/1472-6920-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Frischenschlager O, Haidinger G, Mitterauer L. Factors associated with academic success at Vienna Medical School: Prospective survey. Croatian Medical Journal. 2005;46(1): 58–65. [PubMed] [Google Scholar]
- 63.Iputo JE, Kwizera E. Problem-based learning improves the academic performance of medical students in South Africa. Med Educ. 2005; 39(4): 388–93. doi: 10.1111/j.1365-2929.2005.02106.x. [DOI] [PubMed] [Google Scholar]
- 64.James D, Chilvers C. Academic and non-academic predictors of success on the Nottingham undergraduate medical course 1970-1995. Med Edu. 2001;35(11): 1056–64. doi: 10.1046/j.1365-2923.2001.01042.x. [DOI] [PubMed] [Google Scholar]
- 65.James D, Yates J, Ferguson E. Can the 12-item General Health Questionnaire be used to identify medical students who might 'struggle' on the medical course? A prospective study on two cohorts. BMC Med Educ 2013;13(1): 1–8. doi: 10.1186/1472-6920-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jankovic SM, Tufegdzic BI, Vukovic MV, Folic M. Paying tuition and academic performance of students at Kragujevac University School of Medicine. Croatian Medical Journal. 2002;43(1): 63–6. [PubMed] [Google Scholar]
- 67.Kleijn WC, Van der Ploeg HM, Topman RM. Cognition, study habits, test anxiety, and academic performance. Psychol Rep. 1994;75(3): 1219–26. doi: 10.2466/pr0.1994.75.3.1219. [DOI] [PubMed] [Google Scholar]
- 68.Koles PG, Stolfi A, Borges NJ, Nelson S, Parmelee DX. The impact of team-based learning on medical students' academic performance. Acad Med. 2010; 85(11): 1739–45. doi: 10.1097/ACM.0b013e3181f52bed. [DOI] [PubMed] [Google Scholar]
- 69.Malau-Aduli BS, O'Connor T, Ray RA, Kerlen Y, Bellingan M, Teague PA. Risk factors associated with academic difficulty in an Australian regionally located medical school. BMC Medical Education. 2017;17(1): 1–9. doi: 10.1186/s12909-017-1095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mann C, Canny B, Lindley J, Rajan R. The influence of language family on academic performance in Year 1 and 2 MBBS students. Med Educ. 2010;44(8): 786–94. doi: 10.1111/j.1365-2923.2010.03711.x. [DOI] [PubMed] [Google Scholar]
- 71.Maslov Kruzicevic S, Barisic KJ, Banozic A, Esteban CD, Sapunar D, Puljak L. Predictors of attrition and academic success of medical students: a 30-year retrospective study. PLoS One. 2012; 7(6): e39144. doi: 10.1371/journal.pone.0039144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mavis B, Doig K. The value of noncognitive factors in predicting students' first-year academic probation. Acad Med. 1998;73(2): 201–3. doi: 10.1097/00001888-199802000-00021. [DOI] [PubMed] [Google Scholar]
- 73.Meleca CB. Traditional predictors of academic-performance in a medical-schools independent study program. Acad Med. 1995;70(1): 59–63. doi: 10.1097/00001888-199501000-00015. [DOI] [PubMed] [Google Scholar]
- 74.O’Neill LD, Morcke AM, Eika B. The validity of student tutors’ judgments in early detection of struggling in medical school. A prospective cohort study. Advances in Health Sciences Education . 2016;21(5): 1061–79. doi: 10.1007/s10459-016-9677-6. [DOI] [PubMed] [Google Scholar]
- 75.Shen HK, Comrey AL. Predicting medical students' academic performances by their cognitive abilities and personality characteristics. Acad Med. 1997; 72(9): 781–6. doi: 10.1097/00001888-199709000-00013. [DOI] [PubMed] [Google Scholar]
- 76.Slade AN, Kies SM. The relationship between academic performance and recreation use among first-year medical students. Med Educ Online. 2015;20(1): 25105. doi: 10.3402/meo.v20.25105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sladek RM, Bond MJ, Frost LK, Prior KN. Predicting success in medical school: a longitudinal study of common Australian student selection tools. BMC Med Educ. 2016;16(1): 187. doi: 10.1186/s12909-016-0692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stegers-Jager KM, Cohen-Schotanus J, Themmen AP. Motivation, learning strategies, participation and medical school performance. Med Educ. 2012; 46(7): 678–88. doi: 10.1111/j.1365-2923.2012.04284.x. [DOI] [PubMed] [Google Scholar]
- 79.Stegers-Jager KM, Themmen APN, Cohen-Schotanus J, Steyerberg EW. Predicting performance: Relative importance of students' background and past performance. Med Educ. 2015;49(9): 933–45. doi: 10.1111/medu.12779. [DOI] [PubMed] [Google Scholar]
- 80.Stewart SM, Lam TH, Betson CL, Wong CM, Wong AM. prospective analysis of stress and academic performance in the first two years of medical school. Med Educ. 1999;33(4): 243–50. doi: 10.1046/j.1365-2923.1999.00294.x. [DOI] [PubMed] [Google Scholar]
- 81.Tesija RA, Maslov Kruzicevic S, Banozic A, Esteban CD, Sapunar D, Puljak L. Impact of extended course duration and stricter study organization on attrition and academic performance of medical students. Croat Med J. 2013; 54(2): 192–7. doi: 10.3325/cmj.2013.54.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Veloski JJ, Callahan CA, Xu G, Hojat M, Nash DB. Prediction of students' performances on licensing examinations using age, race, sex, undergraduate GPAs, and MCAT scores. Acad Med. 2000;75(10): S28–30. doi: 10.1097/00001888-200010001-00009. [DOI] [PubMed] [Google Scholar]
- 83.Zhou YX, Ou CQ, Zhao ZT, Wan CS, Guo C, Li L, et al. The impact of self-concept and college involvement on the first-year success of medical students in China. Advances in Health Sciences Education. 2014; 20(1): 163–79. doi: 10.1007/s10459-014-9515-7. [DOI] [PubMed] [Google Scholar]
- 84.Cho KK, Marjadi B, Langendyk V, Hu W. The self-regulated learning of medical students in the clinical environment: a scoping review. BMC Medical Education. 2017; 17: 112. doi: 10.1186/s12909-017-0956-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Migliaretti G, Bozzaro S, Siliquini R, Stura I, Costa G, Cavallo F. Is the admission test for a course in medicine a good predictor of academic performance? A case-control experience at the school of medicine of Turin. BMJ Open. 2017;7(11): 1–7. doi: 10.1136/bmjopen-2017-017417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Peng R, Khaw HH, Edariah AB. Personality and performance of preclinical medical students. Med Educ. 1995; 24(4): 283–8. doi: 10.1111/j.1365-2923.1995.tb02850.x. [DOI] [PubMed] [Google Scholar]
- 87.Poljicanin A, Caric A, Vilovic K, Kosta V, Marinovic Guic M, Aljinovic J, et al. Daily mini quizzes as means for improving student performance in anatomy course. Croat Med J. 2009;50(1): 55–60. doi: 10.3325/cmj.2009.50.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Popovic N, Popovic T, Dragovic IR, Cmiljanic O. A Moodle-based blended learning solution for physiology education in Montenegro: a case study. Advances in Physiology Education. 2018;42(1): 111–7. doi: 10.1152/advan.00155.2017. [DOI] [PubMed] [Google Scholar]
- 89.Pratten MK, Merrick D, Burr SA. Group in-course assessment promotes cooperative learning and increases performance. Anat Sci Educ. 2014;7(3): 224–33. doi: 10.1002/ase.1397. [DOI] [PubMed] [Google Scholar]
- 90.Rashid-Doubell F, Doubell T, O’Sullivan R, Elmusharaf K. To click or not to click: Introducing audience response system during undergraduate teaching to improve academic performance. Bahrain Medical Bulletin. 2014; 36(4): 232–4. [Google Scholar]
- 91.Reibnegger G, Caluba HC, Ithaler D, Manhal S, Neges HM, Smolle J. Progress of medical students after open admission or admission based on knowledge tests. Med Educ. 2010;44(2): 205–14. doi: 10.1111/j.1365-2923.2009.03576.x. [DOI] [PubMed] [Google Scholar]
- 92.Reibnegger G, Caluba HC, Ithaler D, Manhal S, Neges HM, Smolle J. Dropout rates in medical students at one school before and after the installation of admission tests in Austria. Acad Med. 2011;86(8): 1040–8. doi: 10.1097/ACM.0b013e3182223a1b. [DOI] [PubMed] [Google Scholar]
- 93.Romanov K, Nevgi A. Do medical students watch video clips in eLearning and do these facilitate learning? Med Teach. 2007;29(5):484–8. doi: 10.1080/01421590701542119. [DOI] [PubMed] [Google Scholar]
- 94.Sajid MR, Laheji AF, Abothenain F, Salam Y, AlJayar D, Obeidat A. Can blended learning and the flipped classroom improve student learning and satisfaction in Saudi Arabia? . Int J Med Educ. 2016;7(1):281–5. doi: 10.5116/ijme.57a7.83d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Salopek D, Lovric J, Hren D, Marusic A. Temporal Structure of First-year Courses and Success at Course Exams: Comparison of Traditional Continual and Block Delivery of Anatomy and Chemistry Courses. Croatian Medical Journal. 2009; 50(1): 61–8. doi: 10.3325/cmj.2009.50.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schripsema NR, Van Trigt AM, Borleffs JC, Cohen-Schotanus J. Selection and study performance: comparing three admission processes within one medical school. Med Educ. 2014;48(12): 1201–10. doi: 10.1111/medu.12537. [DOI] [PubMed] [Google Scholar]
- 97.Shantakumar SR, Kumar N, Adnan FS, Yacob FNM, Ismai FN, Samsuddin H, et al. Effect of light exposure during sleep on the curricular and extracurricular activities of medical students. Bangladesh Journal of Medical Science. 2017; 16(4): 541–4. [Google Scholar]
- 98.Tucker RP. Performance in a prematriculation gross anatomy course as a predictor of performance in medical school. Anat Sci Educ. 2008; 1(5): 224–7. doi: 10.1002/ase.48. [DOI] [PubMed] [Google Scholar]
- 99.Williams MT. Pre-matriculation program at the University of South Florida College of Medicine. Acad Med. 1999; 74(4): 397–9. doi: 10.1097/00001888-199904000-00035. [DOI] [PubMed] [Google Scholar]


