Abstract
Background
Nature exposures may be associated with reduced risk of heart disease. The present study examines the relationship between objective measures of neighborhood greenness (vegetative presence) and 4 heart disease diagnoses (acute myocardial infarction, ischemic heart disease, heart failure, and atrial fibrillation) in a population‐based sample of Medicare beneficiaries.
Methods and Results
The sample included 249 405 Medicare beneficiaries aged 65 years and older whose location (ZIP+4) in Miami‐Dade County, Florida, did not change from 2010 to 2011. Analyses examined relationships between greenness, measured by mean block‐level normalized difference vegetation index from satellite imagery, and 4 heart disease diagnoses. Hierarchical regression analyses, in a multilevel framework, assessed the relationship of greenness to each heart disease diagnosis, adjusting successively for individual sociodemographics, neighborhood income, and biological risk factors (diabetes mellitus, hypertension, and hyperlipidemia). Higher greenness was associated with reduced heart disease risk, adjusting for individual sociodemographics and neighborhood income. Compared with the lowest tertile of greenness, the highest tertile of greenness was associated with reduced odds of acute myocardial infarction by 25% (odds ratio, 0.75; 95% CI, 0.63–0.90), ischemic heart disease by 20% (odds ratio, 0.80; 95% CI, 0.77–0.83), heart failure by 16% (odds ratio, 0.84; 95% CI, 0.80–0.88), and atrial fibrillation by 6% (odds ratio, 0.94; 95% CI, 0.87–1.00). Associations were attenuated after adjusting for biological risk factors, suggesting that cardiometabolic risk factors may partly mediate the greenness to heart disease relationships.
Conclusions
Neighborhood greenness may be associated with reduced heart disease risk. Strategies to increase area greenness may be a future means of reducing heart disease at the population level.
Keywords: cardiovascular disease, greenness, heart disease, Medicare beneficiaries, natural environment, neighborhood environment, population health
Subject Categories: Cardiovascular Disease, Epidemiology, Risk Factors, Aging
Short abstract
See Editorial by Balmes
Clinical Perspective
What Is New?
This is the first study to document the relationship between neighborhood greenness and heart disease among Medicare beneficiaries using objective measures of heart disease and greenness at the block level.
Because this method uses nationally available data from the Centers for Medicare & Medicaid Services to determine heart disease diagnoses and National Aeronautics and Space Administration satellite imagery to determine greenness at the block level, the study can be replicated/repeated in any neighborhood in the United States.
What Are the Clinical Implications?
This study identifies a potential new protective factor, block‐level greenness, that may reduce heart disease at the population level.
Strategies to increase greenness, such as tree planting, may reduce the risk for heart disease, perhaps by increasing physical activity opportunities.
Cardiovascular diseases (CVDs) including heart disease continue to be the leading cause of death both in the United States and worldwide.1, 2 Currently, there are well‐established guidelines for preventing CVD—including lifestyle factors such as physical activity, diet, nonsmoking, and body mass index, and biomedical indicators such as blood pressure, cholesterol, and blood glucose.3 At the same time, there is a growing awareness that environmental factors, such as air pollution,4 and characteristics of the built and social environment5, 6, 7 may also be important modifiable risk and/or protective factors for preventing CVD.
Neighborhood greenness or vegetative presence is an emerging risk and/or protective factor for health outcomes,8, 9, 10, 11, 12, 13, 14, 15, 16 including CVD.17, 18, 19, 20 It has been theorized that greenness including tree canopy and green spaces may promote cardiovascular health by increasing physical activity, social interaction, air quality, heat regulation, restoration from mental fatigue, and/or stress reduction.8, 9, 21, 22, 23, 24, 25, 26, 27, 28, 29 Indeed, recent findings suggest that greenness may be related to increased levels of physical activity,21, 22, 23, 24, 25, 26, 27, 28, 29, 30 reduced body mass index and risk for overweight/obesity,26, 31, 32, 33 reduced exposure to air pollution,25 and reduced stress symptoms,28, 29 and a reduced risk of cardiometabolic conditions such as diabetes mellitus, hypertension, and hyperlipidemia,11, 34 as well as CVD.17, 18, 19
The current study examines whether mean block‐level greenness (measured by the normalized difference vegetation index [NDVI] from satellite imagery)35, 36 is related to odds of CVD diagnoses37 in a population‐based sample of US Medicare beneficiaries aged 65 years and older.11 Prior studies in this area have been limited,17, 18, 19 and this is the first study to examine the relationship of block‐level greenness (NDVI) and specific heart disease diagnoses.37
Methods
Study Design
A cross‐sectional study was conducted to investigate the relationship between neighborhood greenness (mean NDVI at the Census block level) and the odds of each of 4 types of CVD (acute myocardial infarction [AMI], ischemic heart disease [IHD], heart failure [HF], and atrial fibrillation [AF]) among Medicare beneficiaries aged 65 years and older in Miami‐Dade County, Florida, whose location did not change from 2010 to 2011.11 Additionally, the analyses examined the relationship between neighborhood greenness and overall odds of any form of heart disease, defined as having any of the 4 types of CVD described above. Descriptive analyses were used to find the pattern of CVD rates across different levels of neighborhood greenness, followed by 3 rigorous sets of hierarchical regression models examining the relationship between CVDs and neighborhood greenness, before and after successive addition of covariates in the model (unadjusted, individual sociodemographics, and neighborhood income). A fourth, final model further adjusted for biological risk factors (diabetes mellitus, hypertension, and hyperlipidemia).
The data, analytic methods, and study materials will not be made available by the authors to other researchers for purposes of reproducing the results or replicating the procedures, because of the Data Privacy Board requirements of the US Centers for Medicare & Medicaid Services (CMS), which limit data sharing. However, these CMS data may be requested directly from CMS’ Research Data Assistance Center at https://www.resdac.org/. The satellite imagery used in this study may be requested at https://asterweb.jpl.nasa.gov/.
Data
Data were obtained for this retrospective cohort study from the CMS’ Master Beneficiary Summary File, which provided for each beneficiary annual data on each of the 4 cardiovascular health outcomes, age, sex, race/ethnicity, and location for the calendar years 2010–2011 (available at https://www.resdac.org). The CMS Master Beneficiary Summary File Chronic Conditions Segment provides indications of 27 chronic conditions, using CMS’ chronic conditions algorithms,37 based on Medicare claims of all types for each beneficiary in a calendar year. The present study assessed the relationship between neighborhood greenness (NDVI) and each of 4 types of CVD in 2011—AMI, IHD, HF, and AF—as well as the overall likelihood of having any of these 4 types of CVD.
US National Aeronautics and Space Administration Advanced Spaceborne Thermal Emission and Reflection Radiometer satellite imagery at a 15×15‐meter spatial resolution was used to calculate greenness or vegetative presence by NDVI, a validated measure of neighborhood greenness.35, 36, 38 Mean NDVI at the block level was assessed, with continuous measurements that ranged from −1 to +1, with higher values indicating more greenness.35, 36 Mean NDVI was derived for each of the 36 563 Miami‐Dade County Census blocks for 2011 and was categorized into 3 levels to create meaningful exposure categories based on tertiles of block‐level greenness: low NDVI (−0.40 to −0.06, the lowest third), middle NDVI (−0.06 to 0.006), and high NDVI (0.006–0.429).11
US Census Bureau 2011 data provided neighborhood median household income at the level of the Census block group. For analytic purposes, neighborhood median household income was a continuously measured variable (measured in thousands of dollars).
The final study sample (Figure) was derived in stages, as described elsewhere.11 Starting with the 2011 CMS Master Beneficiary Summary File for Miami‐Dade County, of 407 296 unique Medicare beneficiaries, the following exclusions were made. First, beneficiaries who lived outside of Miami‐Dade County were excluded (n=11 507), as were those who died (n=14 296), had end‐stage renal disease as the reason for enrollment (n=3572), were younger than 65 years or born before 1900 (n=64 109), could not be matched to a specific ZIP code+4 location associated with a Census block (n=14 401), and were members of an ethnic/racial group comprising <1% of the Miami‐Dade County senior population (n=12 132). Finally, beneficiaries whose location changed from 2010 to 2011 were excluded (n=34 584), as well as those with nursing home claims, who may have been in a nursing home for all or part of the year, in which case their location may have been a billing address rather than an actual residence (n=3650). This resulted in a final cohort of 249 405 Medicare beneficiaries, aged 65 years and older who had the same location (based on ZIP code+4‐digit locator) across 2 calendar years (2010–2011). ZIP+4 data from CMS data were linked to a Census block for each beneficiary, using GeoLytics ZIP+4 software (GeoLytics, Inc), which provides the area centroid of the ZIP+4 with latitude and longitude coordinates, and assigns the corresponding 2010 Census block, block group, and tract identification numbers.39 This study was approved by the University of Miami's institutional review board and CMS’ privacy board.
Figure 1.
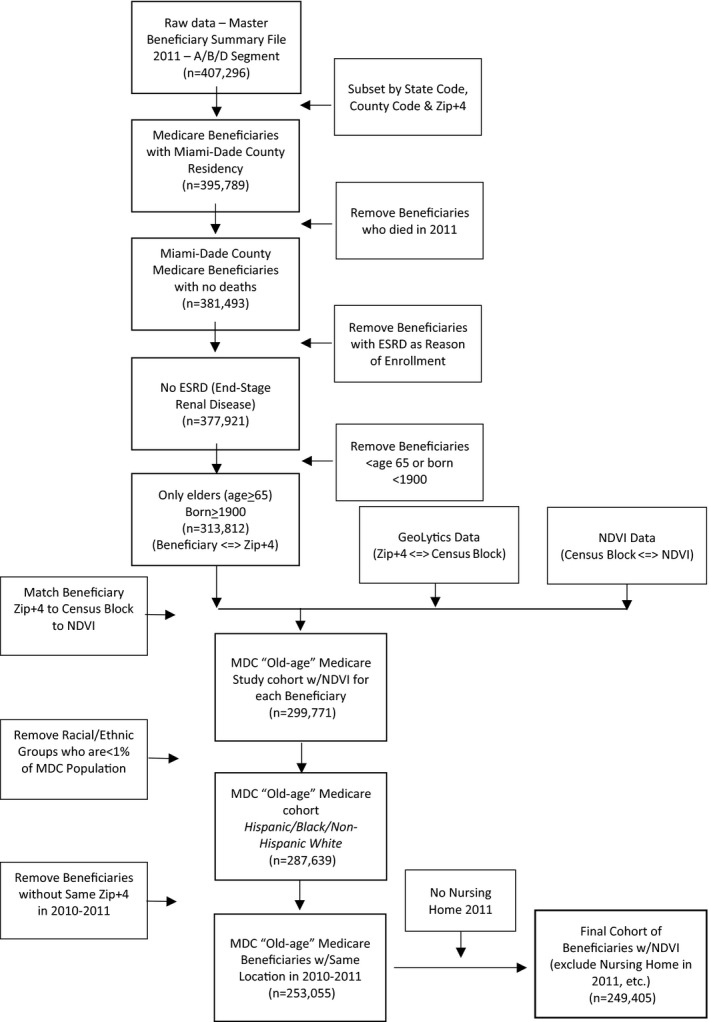
Flow diagram for deriving final cohort of 249 405 Medicare beneficiaries aged 65 years and older with the same location in Miami‐Dade County, Florida, in 2010–2011. ESRD indicates end‐stage renal disease; MDC, Miami‐Dade County; NDVI, normalized difference vegetation index. Reproduced in part from Brown et al11 with permission. Copyright ©2016, Elsevier.
Results
Statistical Analysis
Univariate descriptive analyses were conducted to observe the pattern of individual sociodemographics (age, sex, and race/ethnicity), neighborhood median household income, the CVD outcomes, and biological risk factors (diabetes mellitus, hypertension, and hyperlipidemia) in the overall study sample, as well as across tertiles of NDVI.
To fit the hierarchical structure of data, multilevel logistics regressions were run using SAS version 9.3 software (SAS Institute) with dichotomous variables presence/absence of cardiovascular conditions as outcomes and NDVI tertiles (low NDVI, the lowest tertile as reference) as predictors. A generalized estimating equation model with the assumption of compound symmetric working correlation structure was used to specify the hierarchical models. Specifically, neighborhood median household income was included in the model at the Census block‐group level (consisting of multiple Census blocks, and the smallest geographic scale at which this variable is available from the US Census Bureau); mean NDVI was included in the model at the Census block level (ie, for a single block, nested within the block‐group level, above); and age, sex, race, and ethnicity were included at the individual level (ie, nested within block). To test the hypotheses that block‐level greenness (measured by NDVI) is related to each of the CVD outcomes, 4 multilevel logistics regression analyses were run, one for each of AMI, IHD, HF, and AF, adjusting for potential explanatory factors. Model 1 was unadjusted, model 2 was adjusted for individual‐level sociodemographics as covariates (age, sex, and race/ethnicity), and model 3 was additionally adjusted for a block‐group level covariate (neighborhood median household income). In addition, to assess for possible attenuation of greenness impact on CVD outcomes, a fourth model (model 4) further added biological risk factors of diabetes mellitus, hypertension, and hyperlipidemia.
Of the 249 405 Miami‐Dade Medicare beneficiaries, we found that the race/ethnicity composition in each tertile of NDVI well represents the sociodemographic pattern of Miami‐Dade county—a multiracial metropolitan area with a large Hispanic population—and such distributions of NDVI across racial/ethnic levels correlated with median household incomes in each NDVI tertile. There were significantly more Hispanics in low‐NDVI neighborhoods (80.3%) compared with high‐NDVI neighborhoods (47.7%, P<0.0001). Average median household incomes were lowest in low‐NDVI neighborhoods and highest in high‐NDVI neighborhoods ($40 100 versus $65 800, P<0.0001). Additionally, rates of all biological risk factors and cardiovascular outcomes were generally lower with progressively higher tertiles of NDVI (P<0.001) (Table 1).
Table 1.
Descriptive Statistics for the Overall Sample and by Neighborhood Greenness Level (ie, Lowest, Middle, and Highest Tertiles on Block‐Level NDVI)
| Variable | Overall Sample (−0.40 to 0.429) (All NDVI) | Low NDVI (−0.40 to −0.06) (Lowest Tertile on NDVI) | Medium NDVI (−0.06 to 0.006) (Middle Tertile on NDVI) | High NDVI (0.006–0.429) (Highest Tertile on NDVI) | F (χ2) Test | P Value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. (%) | Mean (SD) | No. (%) | Mean (SD) | No. (%) | Mean (SD) | No. (%) | Mean (SD) | |||
| No. (beneficiaries) | 249 405 (100.00) | ··· | 82 790 (33.20) | ··· | 83 314 (33.41) | ··· | 83 301 (33.40) | ··· | ··· | ··· |
| Main predictor: NDVIa | ··· | −0.02 (0.09) | ··· | −0.11 (0.04) | ··· | −0.03 (0.02) | ··· | 0.07 (0.06) | 376 387a | <0.0001 |
| Neighborhood median household incomeb | ··· | 51.4 (30.7) | ··· | 40.1 (21.9) | ··· | 48.4 (23.8) | ··· | 65.8 (37.9) | 17 167.3a | <0.0001 |
| Individual sociodemographics | ||||||||||
| Age | ··· | 76.33 (7.50) | ··· | 76.71 (7.55) | ··· | 76.30 (7.43) | ··· | 75.98 (7.51) | 196.40a | <0.0001 |
| Female sex | 58.33 | ··· | 58.79 | ··· | 58.66 | ··· | 57.53 | (32.9a) | <0.0001 | |
| Race/ethnicity (RTI)c | (21 963.2a) | <0.0001 | ||||||||
| Hispanic, % | 65.56 | ··· | 80.29 | ··· | 68.77 | ··· | 47.71 | ··· | ||
| Non‐Hispanic white, % | 23.29 | ··· | 16.25 | ··· | 18.21 | ··· | 35.35 | ··· | ||
| Black, % | 11.15 | ··· | 3.45 | ··· | 13.02 | ··· | 16.94 | ··· | ||
| Biological risk factorsd | ||||||||||
| Diabetes mellitus diagnosis, % | 15.55 | ··· | 18.12 | ··· | 14.42 | ··· | 14.14 | ··· | (623.3a) | <0.0001 |
| Hypertension diagnosis, % | 27.88 | ··· | 31.21 | ··· | 25.72 | ··· | 26.74 | ··· | (703.1a) | <0.0001 |
| Hyperlipidemia diagnosis, % | 22.72 | ··· | 25.23 | ··· | 20.51 | ··· | 22.43 | ··· | (533.2a) | <0.0001 |
| Outcome variablese | ||||||||||
| AMI, % | 0.29 | 0.36 | 0.25 | 0.26 | (21.4a) | <0.0001 | ||||
| IHD, % | 20.68 | 23.92 | 18.92 | 19.22 | (793.0a) | <0.0001 | ||||
| HF, % | 7.56 | 9.06 | 7.05 | 6.58 | (412.4a) | <0.0001 | ||||
| AF, % | 2.61 | 2.37 | 1.89 | 3.02 | (90.3a) | <0.0001 | ||||
| Any heart disease, %e | 22.41 | 25.58 | 20.55 | 21.12 | (721.6a) | <0.0001 | ||||
RTI, Research Triangle Institute race code.
Mean normalized difference vegetation index (NDVI) was used to assess greenness/vegetative presence/absence at the Census block level (possible theoretical range of −1 to +1).
Neighborhood median household income is reported in thousands of dollars at the Census block‐group level using 2011 US Census data.
Race and ethnicity was assessed by US Centers for Medicare & Medicaid Services (CMS) for each beneficiary.
Biological risk factors and outcome variables were identified for each Medicare beneficiary, using CMS Beneficiary Summary File, Chronic Conditions segment.
Any heart disease refers to having any of the 4 forms of heart disease in the CMS Chronic Conditions Segment (acute myocardial infarction [AMI], ischemic heart disease [IHD], heart failure [HF], and atrial fibrillation [AF]).
We observed that the higher level of greenery as indicated by upper tertiles of mean NDVI measurements was generally associated with a notable reduction in the odds of all 4 types of cardiovascular‐related chronic conditions (Table 2).
Table 2.
NDVI Relationships to Health Outcomes in Unadjusted and Adjusted Models Adjusting for Individual Sociodemographics, Neighborhood Income, and/or Biological Risk Factors
| Health Outcome Variables (Models) | Model 1 (No Adjustment) | Model 2 (Individual Sociodemographic Covariates)a | Model 3 (Individual Sociodemographic Covariates, Plus Neighborhood‐Level Income)b | Model 4 (Individual Sociodemographic Covariates, Neighborhood‐Level Income, Plus Biological Risk Factors)c | ||||
|---|---|---|---|---|---|---|---|---|
| OR and (95% CI) | P Value | OR and (95% CI) | P Value | OR and (95% CI) | P Value | OR and (95% CI) | P Value | |
| AMI | ||||||||
| Low NDVI | 1 | 1 | 1 | 1 | ||||
| Medium NDVI | 0.97 (0.80–1.17) | 0.7459 | 0.97 (0.80–1.17) | 0.7163 | 0.94 (0.77–1.14) | 0.5231 | 0.96 (0.79–1.17) | 0.7086 |
| High NDVI | 0.70 (0.58–0.83)d | <0.0001d | 0.74 (0.62–0.88)d | 0.0008d | 0.75 (0.63–0.90)d | 0.0018d | 0.87 (0.73–1.04) | 0.1357 |
| P value linear trendse | 0.0003d | 0.0035d | 0.0231d | 0.2909 | ||||
| IHD | ||||||||
| Low NDVI | 1 | 1 | 1 | 1 | ||||
| Medium NDVI | 0.94 (0.91–0.97)d | 0.0003d | 0.92 (0.89–0.96)d | <0.0001d | 0.97 (0.94–1.01) | 0.0961 | 1.03 (0.99–1.07) | 0.1809 |
| High NDVI | 0.75 (0.72–0.78)d | <0.0001d | 0.81 (0.79–0.84)d | <0.0001d | 0.80 (0.77–0.83)d | <0.0001d | 0.86 (0.83–0.90)d | <0.0001d |
| P value linear trendse | <0.0001d | <0.0001d | <0.0001d | <0.0001d | ||||
| HF | ||||||||
| Low NDVI | 1 | 1 | 1 | 1 | ||||
| Medium NDVI | 1.09 (1.04–1.14)d | 0.0003d | 1.03 (0.99–1.08) | 0.1559 | 1.02 (0.97–1.07) | 0.4930 | 1.03 (0.98–1.08) | 0.2277 |
| High NDVI | 0.77 (0.74–0.81)d | <0.0001d | 0.83 (0.79–0.87)d | <0.0001d | 0.84 (0.80–0.88)d | <0.0001d | 0.95 (0.91–1.00)d | 0.0318d |
| P value linear trendse | <0.0001d | <0.0001d | <0.0001d | 0.0015d | ||||
| AF | ||||||||
| Low NDVI | 1 | 1 | 1 | 1 | ||||
| Medium NDVI | 0.73 (0.68–0.78)d | <0.0001d | 0.82 (0.77–0.88)d | <0.0001d | 0.91 (0.84–0.97)d | 0.0062d | 0.92 (0.86–0.98)d | 0.0133d |
| High NDVI | 0.93 (0.86–1.00) | 0.0603 | 0.98 (0.91–1.05) | 0.5053 | 0.94 (0.87–1.00) | 0.0674 | 1.07 (1.00–1.14) | 0.0634 |
| P value linear trendse | <0.0001d | <0.0001d | 0.3435 | <0.0001d | ||||
| Any heart disease | ||||||||
| Low NDVI | 1 | 1 | 1 | 1 | ||||
| Medium NDVI | 0.93 (0.90–0.96)d | <0.0001d | 0.92 (0.89–0.95)d | <0.0001d | 0.97 (0.94–1.01) | 0.1177 | 1.03 (0.99–1.07) | 0.1676 |
| High NDVI | 0.76 (0.74–0.79)d | <0.0001d | 0.83 (0.80–0.86)d | <0.0001d | 0.81 (0.78–0.84)d | <0.0001d | 0.88 (0.84–0.91)d | <0.0001d |
| P value linear trendse | <0.0001d | <0.0001d | <0.0001d | <0.0001d | ||||
Tertiles for mean greenness: low (reference level), medium, and high normalized difference vegetation index (NDVI; see Table 1). AF indicates atrial fibrillation; AMI, acute myocardial infarction; HF, heart failure; IHD, ischemic heart disease; OR, odds ratio.
Individual sociodemographics: age, sex, and race/ethnicity.
Neighborhood‐level income: neighborhood median household income.
Biological risk factors: diabetes mellitus, hypertension, and hyperlipidemia.
Statistically significant results (P<0.05).
P value for linear trends reported across the 3 tertiles of greenness.
The unadjusted models (model 1) show that, compared with low NDVI, high NDVI is associated with lower odds of AMI (odds ratio [OR], 0.70; 95% CI, 0.58–0.83), IHD (OR, 0.75; 95% CI, 0.72–0.78), and HF (OR, 0.77; 95% CI, 0.74–0.81)—as well as any form of heart disease (OR, 0.76; 95% CI, 0.74–0.79). In addition, compared with low NDVI, medium NDVI is associated with lower odds of AF (OR, 0.73; 95% CI, 0.68–0.78), as well as any form of heart disease (OR, 0.93; 95% CI, 0.90–0.96).
In the models adjusting for individual‐level sociodemographics (model 2), the results of the analyses for all cardiovascular outcomes are consistent with the unadjusted models (model 1, reported above).
Of greatest interest for the present analyses are the results for the main model (model 3), which adjusted for individual sociodemographics and neighborhood income. These main analyses showed that compared with low NDVI, high NDVI was associated with statistically significantly (P<0.01) lower odds of AMI (OR, 0.75; 95% CI, 0.63–0.90), IHD (OR, 0.80; 95% CI, 0.77–0.83), HF (OR, 0.84; 95% CI, 0.80–0.88), and any form of heart disease (OR, 0.81; 95% CI, 0.78–0.84), as well as a marginally significantly lower odds of AF (OR, 0.94; 95% CI, 0.87–1.00 [P=0.067]). Additionally, compared with low NDVI, medium NDVI was associated with lower odds of AF (OR, 0.91; 95% CI, 0.84–0.97 [P<0.01]).
To test for potential attenuation of the impact of greenness on each of the 4 CVDs, when adjusting for biological risk factors (model 4), consistent results were observed in IHD, HF, and AF models, although the magnitude of these relationships were attenuated compared with the main model (model 3). However, high NDVI was no longer associated with lower odds of AMI.
The adjusted linear trends test—which includes the 3‐category NDVI variable as a continuous variable for each model—supports the linear trends hypotheses. The odds of having CVDs generally decrease across progressively higher tertiles of greenness in the main analyses (model 3; Table 2). There is a clear linear dose or gradient of relationship of greenness to odds of disease for every outcome except for AF. Otherwise, we observed significant linear trends statistics in all 4 models for the 4 types of CVD, except for the biological model (model 4) for AMI.
Discussion
Higher levels of neighborhood greenness (ie, vegetative presence, measured by NDVI at the Census block level) were generally associated with lower odds of heart disease, adjusting for individual sociodemographics and neighborhood income. Specifically, higher greenness was associated with lower odds of 3 of 4 forms of CVD—AMI, IHD, and HF, respectively—as well as overall odds of heart disease. In further analyses adjusting for 3 common cardiometabolic conditions—diabetes mellitus, hypertension, and hyperlipidemia—which have also been linked to neighborhood greenness,11 the associations between greenness and the 4 types of heart disease were attenuated. This study builds on prior findings that higher levels of neighborhood greenness—measured by mean NDVI—are related to better health outcomes.11, 12, 13, 14, 15, 16, 18, 20, 26, 28, 31, 32, 33 Moreover, this is the first study of which we are aware, that has linked block‐level greenness to heart disease, in any population.
Results show a less consistently strong relationship between greenness and AF, as compared with AMI, IHD, and HF. It is possible that the less strong relationship of AF with greenness occurred because at least 1 form of AF—familial AF—may be less strongly impacted by environmental factors and more strongly related to genetics when compared with the other heart disease diagnoses.40, 41
Although the present findings are correlational in nature, they add to the literature suggesting that greenness or vegetative presence may be associated with reduced odds of CVD at the population level.17, 18, 19 In communities with subtropical climates, such as Miami‐Dade County, the presence of more tree canopies may increase the amount of shade and thus the attractiveness of walking and other outside activities. Thus, the increased canopy may increase the likelihood of residents engaging in physical activity and/or positive social interaction—all of which may be associated with reduced odds of CVD.21, 42, 43, 44 Additionally, evidence supports that greenness may also benefit health by restoring attention and/or reducing perceived stress,22, 23, 45 which, in turn, may lead to better cardiovascular health outcomes.46, 47 Moreover, neighborhood greenness may also mitigate impacts of air pollution25 and urban heat island effects,27 and hence reduce the odds of CVD outcomes.4, 18, 47, 48
Study Strengths
This is the first study to show that higher levels of block‐level greenness (mean NDVI) are associated with lower odds of heart disease. Moreover, it does so in a population‐based sample of older adults—specifically, those enrolled in Medicare for a single large county in the United States. Few prior studies have identified the relationship of the neighborhood built and/or natural environment with heart disease, which is the leading cause of morbidity and mortality in the United States, and may be impacted by changes in land use, such as greenness and destinations for walking and recreation—which may be an area for possible interventions. Changes in policy to promote the addition of vegetation and green spaces to increase opportunities for physical activity—and possibly reduce air pollution—may potentially reduce the risk of CVD at the population level. However, future work is needed to elucidate the specific mechanisms through which neighborhood greenness may impact cardiovascular health.
Study Limitations
The present study focused on a single large US county, so the present findings require replication in similar, and different, populations and locales, including those in other climates. Additionally, Medicare data did not provide moves or reasons for moves, although the sample was restricted to individuals who had the same location for 2 calendar years. The cross‐sectional nature of the present analyses limits assertions about causality, as does the lack of information about environmental exposures beyond the residential block. Self‐selection is a known issue in the built environment and health literature, and healthier individuals, or those who are physically active or prefer nature exposure, may have selected greener environments. Specific behavioral mechanisms through which greenness may impact CVD were not available, such as increased physical activity and social interaction, and decreases in attentional fatigue, perceived stress, and/or more restorative sleep. Similarly, other mediating or moderating factors by which greenness may impact health, such as safety or aesthetics, or smoking behavior or other cardiovascular risk factors, were not available. Other unmeasured variables such as potentially lower levels of air or noise pollution, reduced temperatures, or buffered noise exposure may account for the observed relationships between greenness and heart disease outcomes in the present study. A further limitation is that those individuals who could not be matched to a specific residential ZIP code, who had nursing home claims or moved to a nursing home, and/or those who moved within the 2 years were likely different than those included in the study. Future research is needed that assesses the health impacts of greenness in those who move as well as nursing home residents, which may be important for generalizability. Moreover, the specific measure of greenness in this study—NDVI—does not identify specific types of vegetation or greenery or whether the greenness was publicly accessible. Therefore, future work should examine specific types of vegetation and green spaces, as well as changes in individuals’ residence over time, in relation to cardiovascular outcomes, and thus further elucidate the nature of the relationships observed in this study.
Conclusions
Higher levels of greenness (measured by mean block‐level NDVI) were associated with reduced overall odds of any form of heart disease, as well as 3 specific forms of heart disease (AMI, IHD, and HF). These relationships were obtained in a population‐based sample of 249 405 Medicare beneficiaries aged 65 years and older, who represent a large and growing population at risk for CVD and associated healthcare utilization in the coming years. Prior work suggests that nature exposure, as well as increased opportunities for walking, socializing, and/or stress reduction—which may occur through increased vegetation or greenness—may promote the health of senior populations. This study suggests that adding greenness or vegetation at the block level—even a limited or small amount—may be a useful strategy for combatting CVD at the population level, and hence increase the quality and quantity of life for residents.
Sources of Funding
This project was supported in part by grants from the US Department of Housing & Urban Development (grant number HUD H‐21620‐RG; contact principal investigator: Brown), the Health Foundation of South Florida (principal investigator: Brown), the Parks Foundation of Miami‐Dade, and the Evelyn F. McKnight Brain Institute at the University of Miami.
Disclosures
No disclosures.
(J Am Heart Assoc. 2019;8:e010258 DOI: 10.1161/JAHA.118.010258.)
This study was presented as a poster at the American Heart Association Epidemiology and Prevention | Lifestyle and Cardiometabolic Health Scientific Sessions, March 5– 8, 2019 in Houston, TX.
References
- 1. Centers for Disease Control and Prevention (CDC) . Leading Causes of Death. Atlanta, GA: CDC; 2017. Available at: https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Accessed January 2, 2019. [Google Scholar]
- 2. World Health Organization (WHO) . Cardiovascular Diseases: Fact Sheet. Geneva, Switzerland: WHO; 2017, May 17. Available at: http://www.who.int/mediacentre/factsheets/fs317/en/. Accessed January 2, 2019. [Google Scholar]
- 3. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 4. Lee BJ, Kim B, Lee K. Air pollution exposure and cardiovascular disease. Toxicol Res. 2014;30:71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Malambo P, Kengne AP, De Villiers A, Lambert EV, Puoane T. Built environment, selected risk factors and major cardiovascular outcomes: a systematic review. PLoS One. 2016;11:e0166846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Diez Roux AV, Mujahid MS, Hirsch JA, Moore K, Moore LV. The impact of neighborhoods on cardiovascular risk: the MESA neighborhood study. Glob Heart. 2017;11:353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hartig T, Mitchell R, de Vries S, Frumkin H. Nature and health. Annu Rev Public Health. 2014;35:207–228. [DOI] [PubMed] [Google Scholar]
- 9. James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep. 2015;2:131–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124:1344–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brown SC, Lombard J, Wang K, Byrne MM, Toro M, Plater‐Zyberk E, Feaster DJ, Kardys J, Nardi MI, Perez‐Gomez G, Pantin HM, Szapocznik J. Neighborhood greenness and chronic health conditions in Medicare beneficiaries. Am J Prev Med. 2016;51:78–89. [DOI] [PubMed] [Google Scholar]
- 12. Brown SC, Perrino T, Lombard J, Wang K, Toro M, Rundek T, Marinovic Gutierrez C, Dong C, Plater‐Zyberk E, Nardi MI, Kardys J, Szapocznik J. Health disparities in the relationship of neighborhood greenness to mental health outcomes in 249,405 Medicare beneficiaries. Int J Environ Res Public Health. 2018;15:430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pun VC, Manjourides J, Suh HH. Association of neighborhood greenness with self‐perceived stress, depression and anxiety symptoms in older U.S adults. Environ Health. 2018;17:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Demoury C, Thierry B, Richard H, Sigler B, Kestens Y, Parent ME. Residential greenness and risk of prostate cancer: a case‐control study in Montreal, Canada. Environ Int. 2017;98:129–136. [DOI] [PubMed] [Google Scholar]
- 15. Dalton AM, Jones AP, Sharp SJ, Cooper AJ, Griffin S, Wareham NJ. Residential neighbourhood greenspace is associated with reduced risk of incident diabetes in older people: a prospective cohort study. BMC Public Health. 2016;16:1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. de Keijzer C, Tonne C, Basagaña X, Valentin A, Singh‐Manoux A, Alonso J, Anto JM, Nieuwenhuijsen MJ, Sunyer J, Dadvand P. Residential surrounding greenness and cognitive decline: a 10‐year follow‐up of the Whitehall II cohort. Environ Health Perspect. 2018;126:077003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Donovan GH, Michael YL, Gatziolis D, Prestemon JP, Whitsel EA. Is tree loss associated with cardiovascular‐disease risk in the Women's Health Initiative? A natural experiment. Health Place. 2015;36:1–7. [DOI] [PubMed] [Google Scholar]
- 18. Pereira G, Foster S, Martin K, Christian H, Boruff BJ, Knuiman M, Giles‐Corti B. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health. 2012;12:466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. Morbidity is related to a green living environment. J Epidemiol Community Health. 2009;63:967–973. [DOI] [PubMed] [Google Scholar]
- 20. Yitshak‐Sade M, Kloog I, Novack V. Do air pollution and neighborhood greenness exposures improve the predicted cardiovascular risk? Environ Int. 2017;107:147–153. [DOI] [PubMed] [Google Scholar]
- 21. Almanza E, Jerrett M, Dunton G, Seto E, Penz MA. A study of community design, greenness and physical activity in children using satellite, GPS and accelerometer data. Health Place. 2012;18:46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kaplan S. The restorative benefits of nature: toward an integrative framework. J Environ Psychol. 1995;15:169–182. [Google Scholar]
- 23. Kuo FE, Sullivan WC. Aggression and violence in the inner city: effects of environment via mental fatigue. Environ Behav. 2001;33:543–571. [Google Scholar]
- 24. Sullivan WC, Kuo FE, De Pooter SF. The fruit of urban nature: vital neighborhood spaces. Environ Behav. 2004;36:678–700. [Google Scholar]
- 25. Dadvand P, de Nazelle A, Triguero‐Mas M, Schembari A, Cirach M, Amoly E, Figueras F, Basagaña X, Ostro B, Neiuwenhuijsen MJ. Surrounding greenness and exposure to air pollution during pregnancy: an analysis of personal monitoring data. Environ Health Perspect. 2012;120:1286–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dadvand P, Villanueva CM, Font‐Ribera L, Martinez D, Basagaña X, Belmonte J, Vrijheid M, Gražulevičien≐ R, Kogevinas M, Nieuwenhuijsen MJ. Risks and benefits of green spaces for children: a cross‐sectional study of associations with sedentary behavior, obesity, asthma, and allergy. Environ Health Perspect. 2014;122:1329–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Weng Q, Lu D, Schubring J. Estimation of land surface temperature‐vegetation abundance relationship for urban heat island studies. Remote Sens Environ. 2004;89:467–483. [Google Scholar]
- 28. Beyer KM, Kaltenbach A, Szabo A, Bogar S, Javier Nieto F, Malecki KM. Exposure to neighborhood green space and mental health: evidence from the Survey of the Health of Wisconsin. Int J Environ Res Public Health. 2014;11:3453–3472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kondo MC, Jacoby SF, South EC. Does spending time outdoors reduce stress? A review of real‐time stress response to outdoor environments. Health Place. 2018;51:136–150. [DOI] [PubMed] [Google Scholar]
- 30. Astell‐Burt T, Feng X, Kolt GS. Mental health benefits of neighborhood green space are stronger among physically active adults in middle‐to‐older age: evidence from 260,061 Australians. Prev Med. 2013;57:601–606. [DOI] [PubMed] [Google Scholar]
- 31. Pereira G, Christian H, Foster S, Boruff BJ, Bull F, Knuiman M, Giles‐Corti B. The association between neighborhood greenness and weight status: an observational study in Perth, Western Australia. Environ Health. 2013;12:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bell JF, Wilson JS, Liu GC. Neighborhood greenness and 2‐year changes in body mass index of children and youth. Am J Prev Med. 2008;35:547–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tilt JH, Unfried TM, Roca B. Using objective and subjective measures of neighborhood greenness and accessible destinations for understanding walking trips and BMI in Seattle, Washington. Am J Health Promot. 2007;21:371–379. [DOI] [PubMed] [Google Scholar]
- 34. Astell‐Burt T, Feng X, Kolt GS. Is neighborhood green space associated with a lower risk of type 2 diabetes? Evidence from 267,072 Australians. Diabetes Care. 2014;37:197–201. [DOI] [PubMed] [Google Scholar]
- 35. NASA . MODIS Vegetation Index Products (NDVI & EVI). Washington, DC: NASA; 2015. Available at: https://modis.gsfc.nasa.gov/data/dataprod/dataproducts.php?MOD_NUMBER=13. Accessed January 2, 2019. [Google Scholar]
- 36. Weier J, Herring D. Measuring Vegetation (NDVI & EVI). Washington, DC: NASA Earth Observatory; 2000, August 30. Available at: https://earthobservatory.nasa.gov/Features/MeasuringVegetation/. Accessed January 2, 2019. [Google Scholar]
- 37. Chronic Conditions Data Warehouse (CCW) . Condition Categories. Baltimore, MD: Centers for Medicare and Medicaid Services (CMS) and HealthAPT; 2019. Available at: https://www.ccwdata.org/web/guest/condition-categories. Accessed January 2, 2019. [Google Scholar]
- 38. Rhew IC, Vander Stoep A, Kearney A, Smith NL, Dunbar MD. Validation of the normalized difference vegetation index as a measure of neighborhood greenness. Ann Epidemiol. 2011;21:946–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. GeoLytics . Zip+4. Somerville, NJ: GeoLytics, Inc; 2015. Available at: http://www.geolytics.com/USCensus,Zip4,Products.asp. Accessed January 2, 2019. [Google Scholar]
- 40. Lubitz SA, Yi BA, Ellinor PT. Genetics of atrial fibrillation. Heart Fail Clin. 2010;6:239–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Campuzano O, Perez‐Serra A, Iglesias A, Brugada R. Genetic basis of atrial fibrillation. Genes Dis. 2016;3:257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Maas J, van Dillen SME, Verheij RA, Groenewegen PP. Social contacts as a possible mechanism behind the relation between green space and health. Health Place. 2009;15:586–595. [DOI] [PubMed] [Google Scholar]
- 43. Li J, Siegrist J. Physical activity and risk of cardiovascular disease—a meta‐analysis of prospective cohort studies. Int J Environ Res Public Health. 2012;9:391–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Barth J, Schneider S, von Känel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta‐analysis. Psychosom Med. 2010;72:229–238. [DOI] [PubMed] [Google Scholar]
- 45. de Keijzer C, Gascon M, Neiuwenhuijsen MJ, Dadvand P. Long‐term green space exposure and cognition across the life course: a systematic review. Curr Environ Health Rep. 2016;3:468–477. [DOI] [PubMed] [Google Scholar]
- 46. Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51:1237–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mitchell R, Popham F. Effect of exposure to natural environment on health inequalities: an observational population study. Lancet. 2008;372:1655–1660. [DOI] [PubMed] [Google Scholar]
- 48. WHO Regional Office for Europe . Urban Green Spaces and Health. Copenhagen, Denmark: WHO Regional Office for Europe; 2016. Available at: http://www.euro.who.int/__data/assets/pdf_file/0005/321971/Urban-green-spaces-and-health-review-evidence.pdf?ua=1. Accessed January 2, 2019. [Google Scholar]


