Abstract
Background
Cardiovascular intensive care units (CICUs) have evolved from coronary care wards into distinct units for critically ill patients with primary cardiac diseases, often suffering from illnesses that cross multiple disciplines. Mounting evidence has demonstrated improved survival with the incorporation of dedicated CICU providers with expertise in critical care medicine (CCM). This is the first study to systematically survey dual certified physicians in order to assess the relevance of CCM training to contemporary CICU care.
Methods and Results
Utilizing American Board of Internal Medicine data through 2014, 397 eligible physicians had obtained initial certification in both cardiovascular disease and CCM. A survey to delineate the role of critical care training in the CICU was provided to these physicians. Among those surveyed, 120 physicians (30%) responded. Dual certified physicians reported frequent use of their CCM skills in the CICU, highlighting ventilator management, multiorgan dysfunction management, end‐of‐life care, and airway management. The majority (85%) cited these skills as the reason CCM training should be prioritized by future CICU providers. Few (17%) agreed that general cardiology fellowship alone is currently sufficient to care for patients in the modern CICU. Furthermore, there was a consensus that there is an unmet need for cardiologists trained in CCM (70%) and that CICUs should adopt a level system similar to trauma centers (61%).
Conclusions
Citing specific skills acquired during CCM training, dual certified critical care cardiologists reported that their additional critical care experience was necessary in their practice to effectively deliver care in the modern CICU.
Keywords: American Board of Internal Medicine survey, cardiology training , cardiovascular intensive care units, critical care cardiology
Subject Categories: Quality and Outcomes, Health Services
Clinical Perspective
What Is New?
This is the first study to systematically survey known dual certified physicians in both cardiovascular disease and critical care medicine.
Dual certified physicians outlined which critical care skills were most relevant to cardiovascular intensive care unit patient care, including ventilator management, multiorgan dysfunction management, and end‐of‐life care.
Dual certified physicians agreed that general cardiology fellowship alone is currently insufficient to practice effectively in the modern cardiovascular intensive care units.
What Are the Clinical Implications?
This study has important implications regarding training guidelines and standards for future cardiovascular intensive care unit providers.
Forthcoming iterations of training guidelines should incorporate the specific skills that dual certified physicians have identified as relevant to cardiovascular intensive care unit care.
Many of the highlighted areas are not currently adequately covered in general cardiology fellowships and will be important educational milestones to include in all future critical care cardiology training paradigms.
Introduction
There is growing evidence that cardiac intensive care units (CICUs) have evolved from coronary care observation wards into units that comprehensively care for critically ill patients with primary cardiac problems and complex multisystem illnesses. The American Heart Association released a scientific statement in 2012 detailing the need for CICUs with dedicated critical care cardiologists as well as potential shifts in training strategies for aspiring CICU physicians.1 The American Heart Association statement outlines the existing Accreditation Council for Graduate Medical Education training paradigm, which includes 4 years of fellowship with a minimum of 30 months of clinical training, 6 of which must be dedicated to critical care medicine (CCM). The American College of Cardiology Core Cardiovascular Training Statement Task Force has also recognized the need for advanced training opportunities, describing 3 levels of critical care cardiology proficiency.2 The Task Force specifies that level I should be obtained during a general cardiology fellowship and should be sufficient to care for the majority of CICU patients. Level II can be achieved with an extra 3 to 6 months of critical care time and level III with an extra 12 months of critical care time. The Task Force only highlights endotracheal intubation and intra‐aortic balloon pump placement as patient care milestones and no evaluation processes are specified, indicating that competencies for the practice of advanced critical care cardiology need to be further delineated.
There have been numerous publications, aiming to characterize the added value of critical care cardiology training. CICU providers are exposed to an increasing amount of noncardiac pathology, including sepsis, renal failure, and respiratory failure requiring prolonged mechanical ventilation.3, 4, 5, 6, 7, 8 Moreover, patients with these noncardiac complications have longer CICU lengths of stay and a higher risk of mortality.6 Transitioning to a high‐intensity staffing model, which incorporates dedicated critical care cardiologists or regular consultation with CICU‐based noncardiology critical care physicians may be associated with reduced mortality, length of stay, and costs.9, 10 However, dual trained critical care cardiologists remain few in number, with a recent survey identifying only 8.7% of hospitals utilizing them as unit leaders and only 14.7% of hospitals with at least 1 critical care cardiology attending.11 Similarly, an investigation of the Doximity physician database reported that only 0.47% of CICU admissions were treated by dual certified physicians and that only 3.4% of the identified dual certified physicians were female.12 Despite these data, the perceived priority of fostering critical care trained cardiologists remains a topic of debate, prompting numerous letters and editorials.13, 14, 15
Though numerous studies have described the current organizational structure and staffing of modern‐day CICUs, no previous study has systematically surveyed practitioners with American Board of Internal Medicine certification in both cardiovascular disease (CVD) and CCM. Thus, we sought to better understand how these American Board of Internal Medicine dual certified critical care cardiologists have utilized their training, and how they fit into the evolving critical care landscape.
Methods
This research activity was designated exempt from institutional review board review by the Office for Human Research Protections at the National Institutes of Health. The original survey is available within Data S1. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Through 2014, the American Board of Internal Medicine granted initial certification in both CVD and CCM to 563 physicians. After excluding 5 deceased physicians, 4 physicians under disciplinary action, 21 physicians retired or without valid medical licenses, and 136 physicians without registered e‐mails, the analysis sample of 397 physicians remained (Figure 1). A questionnaire to delineate the role of additional critical care training in the setting of cardiology training was provided to these dual certified physicians by e‐mail invitation, using REDCap (Research Electronic Data Capture) data capture tools hosted at University of California San Francisco.16 REDCap is a secure, web‐based application designed to support data capture for research studies, incorporating data entry, auditing, and import/export procedures.
Figure 1.
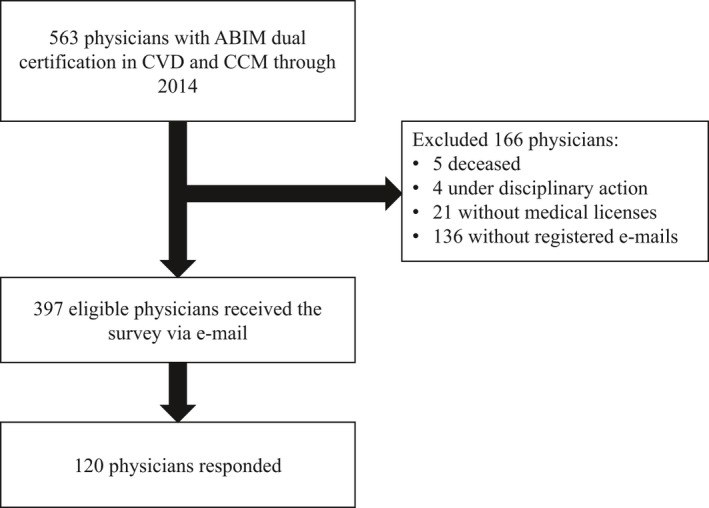
Flow diagram demonstrating formation of the analysis sample. A total of 563 physicians had achieved ABIM initial certification in both CCM and CVD by 2014. Five physicians were deceased, 4 were excluded for ongoing disciplinary action, 21 were excluded for not having current medical licenses, and 136 could not be reached by e‐mail communication. A total of 397 physicians remained in the analysis sample, with 120 responding to the survey. ABIM indicates American Board of Internal Medicine; CCM, critical care medicine; CVD, cardiovascular disease.
Survey data were augmented with key American Board of Internal Medicine administrative data. Variables derived from the administrative data included practice location, age, gender, an indicator variable for passing both CVD and CCM initial certification exams on the first attempt, and an indicator variable for obtaining CCM certification through the practice pathway. CCM certification through the practice pathway was possible during the first 3 years of exam administration: 1987, 1989, and 1991. No fellowship training in critical care medicine was required as long as applicants documented that they were currently providing critical care, and they had previously certified in internal medicine. Because these practice pathway physicians and those having completed fellowship training in CCM potentially represent distinct groups with divergent training and unique insight, they were separated for a subgroup analysis. We used chi‐square tests to examine whether responders differed from nonresponders in regard to demographic variables (Table 1). To adjust for possible nonresponse bias, we used propensity score weighting with poststratification.17 Subjects were assigned a poststratification weight after being divided into quintiles based on estimated propensity scores. Estimated propensity scores were computed with a logistic regression model containing an indicator variable for survey response as the outcome, along with practice location, age, gender, an indicator variable for passing both CVD and CCM initial certification exams on the first attempt, and an indicator variable for obtaining CCM certification through the practice pathway as predictors. Descriptive statistics of survey results were reported based on the calculated propensity score weights. Analyses were conducted using SAS software (version 9.4; SAS Institute Inc, Cary, NC).
Table 1.
Demographic Data of Survey Responders Compared to Non‐Responders
| Characteristics | Nonresponder (N=277) | Responder (N=120) | P Value (Responder vs Nonresponder) |
|---|---|---|---|
| Certified CCM through practice pathway, N (%)a | 196 (70.8) | 77 (64.2) | 0.193 |
| Age (y), N (%)a | 0.030 | ||
| <50 | 17 (6.1) | 17 (14.2) | |
| 50 to 59 | 41 (14.8) | 20 (16.7) | |
| 60 to 69 | 180 (65.0) | 73 (60.8) | |
| 70 or greater | 39 (14.1) | 10 (8.3) | |
| Female, N (%)a , b | 7 (2.5) | 6 (5.0) | 0.204 |
| Region, N (%)a , b | 0.139 | ||
| West | 37 (13.4) | 21 (17.5) | |
| Midwest | 63 (22.7) | 15 (12.5) | |
| South | 73 (26.4) | 40 (33.3) | |
| Northeast | 101 (36.5) | 43 (35.8) | |
| Canada/other | 3 (1.1) | 1 (0.8) | |
| Passed CVD/CCM on first attempt, N (%)a | 210 (75.8) | 105 (87.5) | 0.008 |
CCM indicates critical care medicine; CVD, cardiovascular disease.
Calculated using registration data from full analysis sample (N=397).
Fisher's exact P value reported.
Results
Among the 397 eligible physicians, 120 (30%) responded to the survey. As seen in Table 1, responders were more likely to be aged <60 years than were nonresponders (30.9% versus 20.9%; P=0.03). They were also more likely to pass both CVD and CCM initial certification exams on the first attempt (87.5% versus 75.8%; P=0.01). Though the 2 groups were otherwise comparable, there was a notably small number of female dual certified physicians, making up only 3.3% of the analysis sample.
The majority of the critical care cardiologists in the analysis sample obtained CCM certification through the practice pathway (n=273; 68.8%), with substantially fewer completing CCM fellowships (n=124; 31.2%). Compared with physicians with CCM fellowship training, the practice pathway physicians were more likely to be aged >60 (93.4% versus 37.9%; P<0.001) and more likely to pass both CVD and CCM certification exams on their first attempt (83.5% versus 70.2%; P=0.002; Table 2). There were no significant differences between the practice pathway and CCM fellowship trained groups concerning type of hospital affiliation or number of weeks spent each year treating patients in an intensive care unit (ICU; Table 3). There was a trend toward increased clinical practice in the South and Northeast United States, but the hospitals represented were extremely diverse with only a single pair of respondents hailing from the same institution. Furthermore, 63% of practice pathway physicians and 39.2% of CCM fellowship trained physicians reported working at non‐university‐affiliated and community hospitals.
Table 2.
Demographic Data of Surveyed Practitioners (Responders and Nonresponders) According to Training Pathway
| Characteristics | Practice Pathway (N=273) | Fellowship (N=124) | P Value (Pathway vs Fellowship) |
|---|---|---|---|
| Age (y), N (%)a | <0.001 | ||
| <50 | 0 (0) | 34 (27.4) | |
| 50 to 59 | 18 (6.6) | 43 (34.7) | |
| 60 to 69 | 218 (79.9) | 35 (28.2) | |
| ≥70 | 37 (13.6) | 12 (9.7) | |
| Female, N (%)a | 7 (2.6) | 6 (4.8) | 0.238 |
| Region, N (%)a , b | 0.100 | ||
| West | 41 (15.0) | 17 (13.7) | |
| Midwest | 52 (19.1) | 26 (21.0) | |
| South | 69 (25.3) | 44 (35.5) | |
| Northeast | 109 (39.9) | 35 (28.2) | |
| Canada/other | 2 (0.7) | 2 (1.6) | |
| Passed CVD/CCM on first attempt, N (%)a | 228 (83.5) | 87 (70.2) | 0.002 |
CCM indicates critical care medicine; CVD, cardiovascular disease.
Calculated using registration data from full analysis sample (N=397).
Fisher's exact P value reported.
Table 3.
Self‐Reported Practice Characteristics of Survey Responders According to Training Pathway
| Survey Question | Practice Pathway (N=77) | Fellowship Trained (N=43) |
|---|---|---|
| What best describes the institution you are primarily affiliated with?a , b, % (95% CI) | ||
| University medical center | 23.9 (12.4, 35.4) | 36.0 (20.2, 51.7) |
| Non‐university‐affiliated hospitalc | 40.7 (28.7, 52.7) | 24.5 (10.9, 38.2) |
| University‐affiliated community/county hospital | 22.3 (11.9, 32.7) | 14.7 (3.9, 25.5) |
| Office‐based/outpatient clinic+hospital | 3.2 (0.0, 6.8) | 14.4 (3.1, 25.7) |
| Office‐based/outpatient clinic | 4.8 (0.0, 11.0) | 5.5 (0.0, 16.2) |
| Otherd | 5.1 (0.6, 9.6) | 5.0 (0.0, 12.1) |
| How many weeks each year do you manage patients in an intensive care unit?e , f, % (95% CI) | ||
| 0 to 10 | 40.1 (27.4, 52.8) | 45.6 (29.1, 62.2) |
| 11 to 20 | 18.6 (6.7, 30.6) | 19.5 (7.1, 31.8) |
| 21+ | 41.3 (28.5, 54.0) | 34.9 (18.5, 51.3) |
The original question choices were regrouped into meaningful categories.
There is no statistical difference between the 2 training pathways (χ2=7.6; P=0.177).
Includes VA and nongovernment VA hospitals.
Other includes Industry settings.
There were 8 missing values for the practice pathway group and 1 missing value for the fellowship trained group.
There is no statistical difference between the 2 training pathways (χ2=2.6; P=0.272).
Critical care cardiologists commonly completed additional cardiology subspecialty training, particularly interventional cardiology (32%; 95% CI, 22.7–41.2%) and imaging (31.2%; 95% CI, 22.4.0–39.9%; Figure 2). A similar pattern for additional subspecialty training was observed in both those with CCM fellowship training and those certifying through the practice pathway, with a trend toward increased subspecialization in the CCM fellowship trained group.
Figure 2.
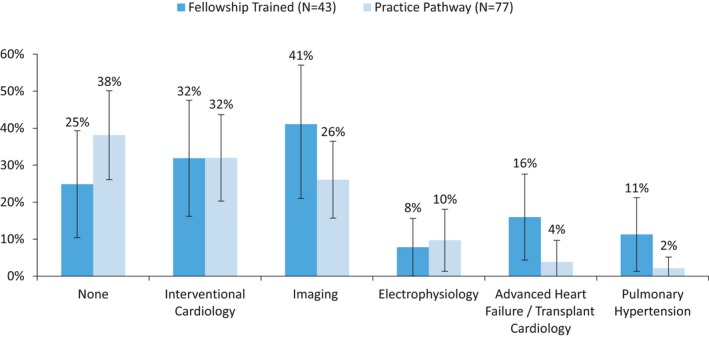
Subspecialties other than critical care grouped by training experience of respondents. Percentage of responders indicating additional cardiac subspecialization. Physicians completing CCM fellowship training are represented in dark blue and physicians certifying by the practice pathway in light blue. Multiple selections were allowed. Error bars represent 95% CIs. There was no statistical difference between groups. CCM indicates critical care medicine.
A total of 64.9% agreed that they would train in both cardiology and CCM again if granted the opportunity to do so (95% CI, 55.6–74.1%). Interestingly, this sentiment was far more robust among CCM fellowship trained physicians than those having completed the practice pathway (91.5% versus 50.9%; P<0.001). As a whole, the survey group supported this position by reporting that they used their CCM training on a regular basis. Sixty‐one percent responded that they used CCM training either “regularly” or “all the time” in their current practice (95% CI, 51.6–71.1%). The CCM fellowship trained group had a higher proportion reporting regular use of their skills than the practice pathway group (78.8% versus 52.2%; P=0.01; Figure 3).
Figure 3.
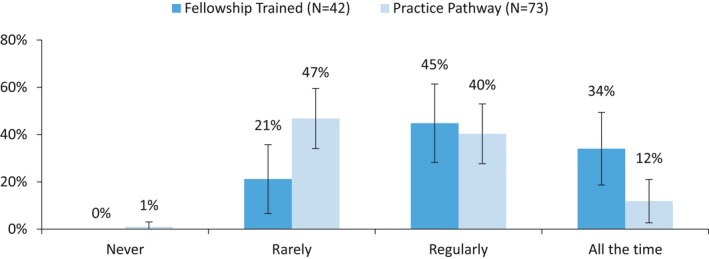
Responder utilization of CCM‐acquired skills grouped by training experience of respondents. Percentage of responders indicating their use of skills acquired during CCM training. Physicians completing CCM fellowship training are represented in dark blue and physicians certifying by the practice pathway in light blue. Error bars indicate 95% CIs. Five responders did not answer this survey question: 4 from the practice pathway group and 1 from the CCM fellowship trained group. Percentage of responders indicating use of CCM skills regularly or all the time was 52.2% and 78.8% in the practice pathway and CCM fellowship training groups, respectively; P=0.006. CCM indicates critical care medicine.
Critical care cardiologists were further asked to identify the specific CCM skills most essential to the effective management of CICU patients. They highlighted ventilator management (55%), multiorgan failure management (50%), end‐of‐life care (43%), and airway management (41%). ICU sedation, infection management, and ICU nutrition were also frequently selected as relevant clinical areas (Figure 4). The relative hierarchy of importance regarding these skills was similar between the CCM fellowship trained and practice pathway groups (r spearman=0.92; P<0.001); however, the CCM fellowship trained physicians selected a higher number of skills, on average (8.3 versus 3.7; P<0.001), which likely accounts for much of the intergroup differences observed in Figure 4.
Figure 4.

Responder‐reported CCM‐acquired skills useful for practice in the CICU grouped by training experience of respondents. Percentage of responders who marked in the affirmative that a specific skill acquired in CCM training was useful in the CICU. Physicians completing CCM fellowship training are represented in dark blue and physicians certifying by the practice pathway in light blue. The vertical axis of the figure is organized according to the skill importance ranking (indicated next to the percentage; 1=most frequently selected skill) as designated by CCM fellowship trained physicians. Multiple selections were allowed. Error bars indicate 95% CIs. The CCM fellowship trained group marked a greater number of skills, on average, compared with the practice pathway group (8.3 vs 3.7; P<0.001). Rankings were similar between the CCM fellowship training group and the practice pathway physicians (r spearman=0.92, P<0.001). CCM indicates critical care medicine; CICU, cardiovascular intensive care unit; ICU, intensive care unit.
The majority of physicians indicated that additional CCM training is needed to practice in the CICU effectively. They most often identified completion of level III Core Cardiovascular Training Statement training (54.6%; 95% CI, 44.8–64.3%) and separate CCM training with board certification (47.1%; 95% CI, 37.3–56.9%) as adequate pathways to achieve this experience. Only 17.1% believed that a standard 3‐year general cardiology fellowship alone was sufficient (95% CI, 10.4–23.8%). When dichotomized by CCM training experience, the responses remained similar, though CCM fellowship trained physicians most frequently chose fellowship training (68%) and practice pathway physicians most frequently chose Core Cardiovascular Training Statement qualification (58%; Figure 5). Regardless of training experience, critical care cardiologists agreed that a general cardiology fellowship was insufficient.
Figure 5.
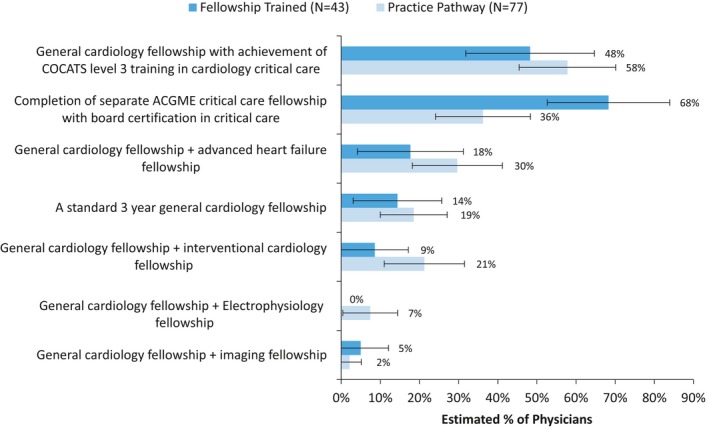
Potential critical care cardiology training paradigms grouped by training experience of respondents. Percentage of responders indicating agreement that the above training paradigms are adequate to practice in the CICU at their home institution. Physicians completing CCM fellowship training are represented in dark blue and physicians certifying by the practice pathway in light blue. Multiple selections allowed. Error bars indicate 95% CIs. Only 14% of CCM fellowship trained and 19% of practice pathway physicians selected general cardiology fellowship alone as an adequate training regimen. ACGME indicates Accreditation Council for Graduate Medical Education; CCM, critical care medicine; CICU, cardiovascular intensive care unit; COCATS, Core Cardiovascular Training Statement.
Seventy percent of responders believed there to be an unmet need for cardiologists with adequate CCM experience (95% CI, 61.5–80.1%). Regardless of training method, respondents (85%) primarily cited improved clinical skills and patient outcomes as the reason to prioritize critical care training (Figure 6). Lastly, the majority of dual certified critical care cardiologists supported the adoption of a trauma‐center–like level system for CICUs. We found that 61.2% were in favor of adoption (95% CI, 50.9–71.6%), 13.2% were against (95% CI, 6.2–20.1%), and 25.6% were neutral (95% CI, 15.9–35.2%). Those fellowship trained in CCM were more likely to agree with the transition to a CICU‐level system than were those who certified through the practice pathway (76.7% versus 52.8%; P=0.01; Figure 7).
Figure 6.
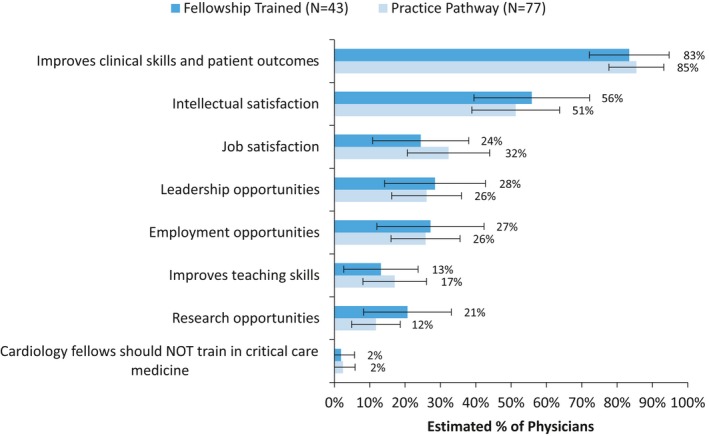
Responder‐reported reasons for additional training in CCM grouped by training experience of respondents. Percentage of responders indicating why they believed current cardiology fellows should pursue additional training in CCM. Physicians completing CCM fellowship training are represented in dark blue and physicians certifying by the practice pathway in light blue. Multiple selections allowed. Error bars indicate 95% CIs. CCM indicates critical care medicine.
Figure 7.
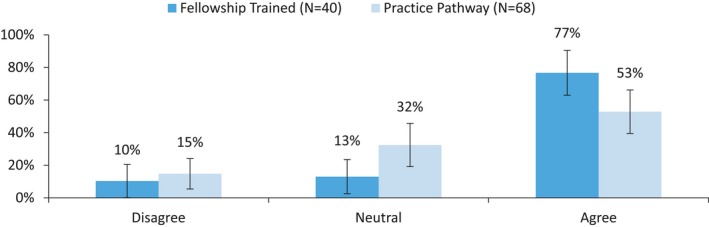
Responder agreement that CICUs should adopt a level system similar to trauma centers grouped by training experience of respondents. Percentage of responders indicating their agreement that CICUs should adopt a level system similar to trauma centers. Physicians completing CCM fellowship training are represented in dark blue and physicians certifying by the practice pathway in light blue. Error bars indicate 95% CIs. Twelve responders did not answer this survey question: 9 from the practice pathway group and 3 from the CCM fellowship trained group. Percentage of responders that agreed with adoption of a level system similar to trauma centers was 52.8% and 76.7% in practice pathway and CCM fellowship trained groups, respectively; P=0.012. CCM indicates critical care medicine; CICU, cardiovascular intensive care unit.
Discussion
The present study surveyed physicians with dual certification in both CVD and CCM with the aim of better understanding their collective perspectives and experiences. These cardiologists have unique insight into the importance of additional critical care training and its relevance to CICU patient care in their practice. Current critical care cardiologists, both CCM fellowship trained and practice pathway certified, described using the skills that they obtained by critical care training regularly, albeit the fellowship trained physicians had a higher proportion using those skills on a regular basis. Furthermore, they highlighted the specific CCM skills that are most fundamental to patient care in contemporary CICUs. Greater than 40% of responders selected ventilator management, multisystem organ failure management, airway management, and end‐of‐life care—topics that are not adequately emphasized in general cardiology fellowships.
The applicability of these CCM skills to CICU daily workflow is a potential driver of the improved patient outcomes that have been observed in recent studies.9, 10 The most intriguing study, by Na et al,9 described patient outcomes before and after the CICU was converted to a comanaged unit with the primary providers being critical care cardiologists. There was an absolute decrease in mortality of nearly 5% between the 2 time periods with an adjusted odds ratio of 0.43 (P<0.001). With the increasing complexity of CICU patients, it is possible that the majority of this benefit was derived from expertise in management of noncardiac complications as well as management of difficult cardiac cases requiring a combination of mechanical ventilator support, antimicrobial regimens, hemodynamic tailoring, and renal replacement therapies. Additionally, critical care cardiologists highlighted the importance of end‐of‐life care. Improved provider comfort with end‐of‐life care may foster timely goals‐of‐care discussions, which are associated with appropriate implementation of care limitations and withdrawal of life‐sustaining therapies as well as lower healthcare costs.18, 19 These multiple areas are not sufficiently emphasized in general cardiology fellowships, and the majority of survey respondents agreed that a general cardiology fellowship alone is insufficient to manage patients effectively in the CICU.
Looking forward, as the American Heart Association, American College of Cardiology, and corresponding international organizations move to set requirements for critical care cardiology training, it will be crucial to ensure that clinical competencies in a range of CCM skills are emphasized.1, 2, 20 For example, the document published by the Core Cardiovascular Training Statement Task Force only designated intra‐aortic balloon pump placement and endotracheal intubation as level III patient care milestones.2 The skills outlined in this article may serve as a guide for proficiency standards in future iterations. This survey also provides additional experiential support for a CICU organizational shift to a collaborative, multidisciplinary care team structure, especially in hospitals with level I– and level II–type CICUs.1 Although previously described as “closed” units, we believe this term to be imprecise and prefer the term collaboratively managed multidisciplinary units to more accurately reflect the situation in which there is a dedicated CICU attending trained in critical care who manages patients with input from the patient's primary, longitudinal provider.
Although not the primary intent of the survey, this study identified that only 3.3% of dual certified critical care cardiologists were women. This finding is in line with a previous investigation, which found that only 3.4% of physicians dual certified in CCM and CVD were female.12 Interestingly, this gender gap far exceeds that of cardiology and critical care medicine in general, which only have 14.1% and 26.1% active women physicians, respectively.21 A gender disparity of this magnitude is comparable with that of interventional cardiology and should trigger a call for cardiology leaders to better understand why so few women have chosen to pursue these specialties.22 The issue is multifactorial, with potential contributors including compensation inequality and under‐representation of women in leadership roles.23, 24 Improved mentorship for women considering critical care cardiology and ongoing diversity task force implementation will hopefully aide in closing the gender gap.25
Study Limitations
The limitations of this study include its survey‐based design with associated recall bias and a low response rate. The group of providers surveyed represent a highly specialized group with the potential for implicit bias in favor of their own training paradigm. Additionally, the majority of respondents completed their CCM training by the practice pathway, which is no longer an available avenue to CCM certification. Thus, the surveyed population may not accurately represent the attitudes of more recently graduated and future dual trained and certified critical care cardiologists. This is also potentially highlighted by the following dichotomy: The younger, CCM fellowship trained cardiologists reported working at university medical centers more than any other care setting, whereas the majority of practice pathway physicians reported working at nonacademic centers. This indicates that a higher proportion of practice pathway physicians may have transitioned into private practice. Lastly, although certification pathway was accounted for in nonresponse weighting adjustments, comparison between these two training groups was not predefined for stratified sampling.
Conclusion
Based on the clinical and professional experience of dual certified critical care cardiologists, CCM‐acquired skills are likely a crucial component of patient care in the modern CICU. These areas should be emphasized in the development of integrated critical care cardiology training programs and high‐intensity CICU staffing models. Although formal CCM fellowship training may not be required for all providers, general cardiology fellowship programs should consider new curriculum and pathways to prepare trainees to provide optimal care in the modern CICU. Critical care training has long been standard in medical and surgical ICUs and has recently gained acceptance in neurological ICUs. Critical care cardiology training for the CICU should also be prioritized.
Sources of Funding
This research was supported, in part, by the Intramural Research Program of the National Institutes of Health Clinical Center.
Disclosures
Dr Morrow reports grants to the TIMI Study Group from Abbott Laboratories, Amgen, AstraZeneca, BRAHMS, Eisai, GlaxoSmithKline, Medicines Co, Merck, Novartis, Pfizer, Roche Diagnostics, Quark, and Takeda and consultant fees from Abbott Laboratories, Aralez, AstraZeneca, Bayer Pharma, InCardia, Pfizer, and Roche Diagnostics. The remaining authors have no disclosures to report.
Supporting information
Data S1. Original survey.
Acknowledgments
The authors acknowledge Kelly Byrne for help in formatting and submitting the manuscript.
(J Am Heart Assoc. 2019;8:e011721 DOI: 10.1161/JAHA.118.011721.)
References
- 1. Morrow DA, Fang JC, Fintel DJ, Granger CB, Katz JN, Kushner FG, Kuvin JT, Lopez‐Sendon J, McAreavey D, Nallamothu B, Page RL II, Parrillo JE, Peterson PN, Winkelman C; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Council on Quality of Care and Outcomes Research . Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. 2012;126:1408–1428. [DOI] [PubMed] [Google Scholar]
- 2. O'Gara PT, Adams JE III, Drazner MH, Indik JH, Kirtane AJ, Klarich KW, Newby LK, Scirica BM, Sundt TM III. COCATS 4 Task Force 13: training in critical care cardiology. J Am Coll Cardiol. 2015;65:1877–1886. [DOI] [PubMed] [Google Scholar]
- 3. Katz JN, Shah BR, Volz EM, Horton JR, Shaw LK, Newby LK, Granger CB, Mark DB, Califf RM, Becker RC. Evolution of the coronary care unit: clinical characteristics and temporal trends in healthcare delivery and outcomes. Crit Care Med. 2010;38:375–381. [DOI] [PubMed] [Google Scholar]
- 4. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 5. Goldfarb M, van Diepen S, Liszkowski M, Jentzer JC, Pedraza I, Cercek B. Noncardiovascular disease and critical care delivery in a contemporary cardiac and medical intensive care unit. J Intensive Care Med. 2017. DOI: 10.1177/0885066617741873. [DOI] [PubMed] [Google Scholar]
- 6. Holland EM, Moss TJ. Acute noncardiovascular illness in the cardiac intensive care unit. J Am Coll Cardiol. 2017;69:1999–2007. [DOI] [PubMed] [Google Scholar]
- 7. Sinha SS, Sjoding MW, Sukul D, Prescott HC, Iwashyna TJ, Gurm HS, Cooke CR, Nallamothu BK. Changes in primary noncardiac diagnoses over time among elderly cardiac intensive care unit patients in the United States. Circ Cardiovasc Qual Outcomes. 2017;10:e003616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Watson RA, Bohula EA, Gilliland TC, Sanchez PA, Berg DD, Morrow DA. Prospective registry of cardiac critical illness in a modern tertiary care Cardiac Intensive Care Unit. Eur Heart J Acute Cardiovasc Care. 2018. DOI: 10.1177/2048872618789053. [DOI] [PubMed] [Google Scholar]
- 9. Na SJ, Chung CR, Jeon K, Park CM, Suh GY, Ahn JH, Carriere KC, Song YB, Choi JO, Hahn JY, Choi JH, Choi SH, On YK, Gwon HC, Jeon ES, Kim DK, Yang JH. Association between presence of a cardiac intensivist and mortality in an adult cardiac care unit. J Am Coll Cardiol. 2016;68:2637–2648. [DOI] [PubMed] [Google Scholar]
- 10. Kapoor K, Verceles AC, Netzer G, Chaudhry A, Bolgiano M, Devabhakthuni S, Ludmir J, Pollock JS, Ramani GV, McCurdy MT. A collaborative cardiologist‐intensivist management model improves cardiac intensive care unit outcomes. J Am Coll Cardiol. 2017;70:1422–1423. [DOI] [PubMed] [Google Scholar]
- 11. van Diepen S, Fordyce CB, Wegermann ZK, Granger CB, Stebbins A, Morrow DA, Solomon MA, Soble J, Henry TD, Gilchrist IC, Katz JN, Cohen MG, Newby LK. Organizational structure, staffing, resources, and educational initiatives in cardiac intensive care units in the United States: an American Heart Association Acute Cardiac Care Committee and American College of Cardiology Critical Care Cardiology Working Group Cross‐Sectional Survey. Circ Cardiovasc Qual Outcomes. 2017;10:e003864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blumenthal DM, Mikhael B, Lawler PR, Yeh RW, Metlay JP, Dudzinski DM. Personal and professional characteristics of U.S. dual‐boarded critical care cardiologists in 2015. Crit Care Med. 2017;45:e1292–e1296. [DOI] [PubMed] [Google Scholar]
- 13. Fuster V. The (R)Evolution of the CICU: better for the patient, better for education. J Am Coll Cardiol. 2018;72:2269–2271. [DOI] [PubMed] [Google Scholar]
- 14. Katz JN, Minder M, Olenchock B, Price S, Goldfarb M, Washam JB, Barnett CF, Newby LK, van Diepen S. The genesis, maturation, and future of critical care cardiology. J Am Coll Cardiol. 2016;68:67–79. [DOI] [PubMed] [Google Scholar]
- 15. Geller BJ, Fleitman J, Sinha SS. Critical care cardiology: implementing a training paradigm. J Am Coll Cardiol. 2018;72:1171–1175. [DOI] [PubMed] [Google Scholar]
- 16. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–524. [Google Scholar]
- 18. Naib T, Lahewala S, Arora S, Gidwani U. Palliative care in the cardiac intensive care unit. Am J Cardiol. 2015;115:687–690. [DOI] [PubMed] [Google Scholar]
- 19. Khandelwal N, Benkeser D, Coe NB, Engelberg RA, Teno JM, Curtis JR. Patterns of cost for patients dying in the intensive care unit and implications for cost savings of palliative care interventions. J Palliat Med. 2016;19:1171–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Le May M, van Diepen S, Liszkowski M, Schnell G, Tanguay JF, Granger CB, Ainsworth C, Diodati JG, Fam N, Haichin R, Jassal D, Overgaard C, Tymchak W, Tyrrell B, Osborne C, Wong G. From coronary care units to cardiac intensive care units: recommendations for organizational, staffing, and educational transformation. Can J Cardiol. 2016;32:1204–1213. [DOI] [PubMed] [Google Scholar]
- 21. Association of American Medical Colleges . 2018 Physician specialty data report: number and percentage of active physicians by sex and specialty, 2017. Table 1.3. 2018. Available at: https://www.aamc.org/data/workforce/reports/492560/1-3-chart.html. Accessed January 10, 2019.
- 22. Abbott JD. Women in interventional cardiology: small numbers, big impact. Circ Cardiovasc Interv. 2016;9:e004323. [DOI] [PubMed] [Google Scholar]
- 23. Jagsi R, Biga C, Poppas A, Rodgers GP, Walsh MN, White PJ, McKendry C, Sasson J, Schulte PJ, Douglas PS. Work activities and compensation of male and female cardiologists. J Am Coll Cardiol. 2016;67:529–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Venkatesh B, Mehta S, Angus DC, Finfer S, Machado FR, Marshall J, Mitchell I, Peake S, Zimmerman JL. Women in Intensive Care study: a preliminary assessment of international data on female representation in the ICU physician workforce, leadership and academic positions. Crit Care. 2018;22:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Douglas PS, Williams KA Sr, Walsh MN. Diversity matters. J Am Coll Cardiol. 2017;70:1525–1529. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Original survey.


