Abstract
Thrombotic thrombocytopenic purpura (TTP) is a rare disease with a mortality rate of over 90% if left untreated. Therapeutic plasma exchange (PEX) is the mainstay of treatment of acquired TTP (aTTP), and with the introduction of PEX, the mortality rate declined dramatically below 20%. Although PEX together with corticosteroids are the backbone of the upfront management of patients with aTTP with successful outcomes, patients may remain refractory and/or relapse following an initial response to this treatment. There are some therapeutic options, which can be used among these patients, helping in improving outcomes of aTTP. Caplacizumab (formerly ALX-0081 or ALX-0681) is a humanized single-variable domain immunoglobulin that recognizes the human von Willebrand factor (vWF) A1 domain and inhibits the vWF–platelet glycoprotein 1b-alpha (GP1b-α) interaction. The drug was first developed for the prevention of thrombosis in high-risk patients with acute coronary syndrome undergoing percutaneous coronary intervention; however, drug development for this indication has been discontinued. Recently, caplacizumab received its first approval following Phase II TITAN and Phase III HERCULES trials in the European Union (EU) for the treatment of acute episode of aTTP in adult patients, in addition to PEX and immunosuppression. This review focuses on the use of caplacizumab as an emerging treatment option in patients with aTTP.
Keywords: acquired thrombotic thrombocytopenic purpura, ADAMTS13, aTTP, caplacizumab, ultra-large von Willebrand factor multimers
Introduction
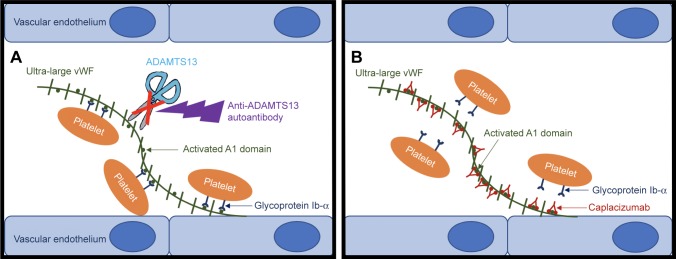
Thrombotic thrombocytopenic purpura (TTP) is a rare disease with a mortality rate of over 90% if left untreated.1 TTP is a prototype of the thrombotic microangiopathies (TMAs), and it is characterized by disseminated formation of platelet-rich thrombi in arterioles and capillaries resulting in microangiopathic hemolytic anemia (MAHA), thrombocytopenia, and potential end organ injury mainly involving the brain, heart, and kidneys leading to significant morbidity/mortality. TTP can either be hereditary or acquired, and the pathogenesis of the latter consists of autoimmune antibodies against the metalloproteinase “a disintegrin and metalloproteinase with a thrombospondin type 1 motif (ADAMTS13)”, and ADAMTS13 is responsible for the cleavage of ultra-large multimers of von Willebrand factor (vWF), which induces aggregation of platelets through glycoprotein 1b-alpha (GP1b-α) receptors and the activated A1 domain of the vWF multimers without a trigger-like endothelial damage or tissue factor (Figure 1A). Acquired TTP (aTTP) can be primary (idiopathic) or secondary to some underlying disorders.2 Therapeutic plasma exchange (PEX) is the mainstay of treatment of aTTP, and with the introduction of PEX, the mortality rate declined dramatically below 20%.1 The rationale of PEX is the replacement of ADAMTS13 and removal of ultra-large vWF and anti-ADAMTS13 antibodies.
Figure 1.
The mechanism of action of caplacizumab.
Notes: (A) The pathogenesis of aTTP; the presence of anti-ADAMTS13 autoantibodies inhibits the proteolytic cleavage of ultra-large vWF multimers by ADAMTS13, which results in the aggregation of platelets through GP1b-α receptors and the activated A1 domain of the vWF causing microvascular thrombosis and ischemic organ damage. (B) Caplacizumab blocks the platelet and ultra-large vWF interaction by binding to A1 domain of vWF.
Abbreviations: aTPP, acquired thrombotic thrombocytopenic purpura; GP1b-α, glycoprotein 1b-alpha; vWF, von Willebrand factor.
In newly diagnosed patients with aTTP, PEX and corticosteroids are usually started upfront together.3 However, a subset of patients may remain refractory to this treatment or have an initial response but relapse after the discontinuation of PEX during the follow-up. There is limited information or consensus available on the management of relapsed/refractory aTTP. While managing PEX refractory patients, PEX may be intensified to 1.5 plasma volume (PV), and even twice-daily PEX can be used.4 In cases who remain refractory to PEX plus corticosteroids, the administration of high-dose methylprednisolone 1 g per day for 3 days can be the choice of treatment.5 Other treatment options in patients with relapsed/refractory TTP may include rituximab, vincristine, cyclophosphamide, cyclosporine A, and splenectomy.6–11 Rituximab was shown to be effective as a second-line therapy,12 as well as in the upfront setting as an adjunct to PEX and corticosteroids.13–15 In addition to these indications, rituximab can be used in the setting of ongoing high anti-ADAMTS13 antibody titers and/or low ADAMTS13 activity without laboratory and clinical features resembling recurrence of aTTP.16
There are emerging therapies that can be used in patients with aTTP, including N-acetylcysteine (NAC), bortezomib, and recombinant ADAMTS13 (rADAMTS13). NAC can be used in the salvage setting as it inhibits platelet adherence to endothelial cell-anchored soluble ultra-large vWF multimers by reducing their size.17 Bortezomib was shown to be beneficial in patients with relapsed/refractory aTTP; however, the number of cases in the literature treated with bortezomib is limited.18 rADAMTS13 has shown some questionable activity among patients with aTTP, and its main indication will most likely be hereditary TTP, where it will substitute the lacking enzyme and replace regular plasma infusions. The main problem concerning rADAMTS13 is the allergic reactions, which would most probably prevent it from being widely used.19
Recently, caplacizumab was introduced, and the drug received its first approval in the European Union (EU) for the treatment of adult patients with aTTP, in addition to PEX and immunosuppression.20 This study mainly focuses on the use of caplacizumab as an emerging treatment option in patients with aTTP.
General information about caplacizumab
Caplacizumab (formerly ALX-0081 or ALX-0681) is a humanized single-variable domain immunoglobulin that recognizes the human vWF A1 domain and inhibits the vWF–platelet GP1b-α interaction.21 It consists of two identical humanized building blocks that are genetically linked by a three-alanine linker.20 In preclinical models, by targeting the A1 domain of the ultra-large vWF, it inhibits the interaction between vWF and platelets, and as a result, prevents platelet adhesion and thus microvascular thrombosis and enables normalization of the platelet count (Figure 1B).21,22 Caplacizumab was first developed for the prevention of thrombosis in high-risk patients with acute coronary syndrome undergoing percutaneous coronary intervention; however, drug development for this indication has been discontinued.23
Caplacizumab can be used either intravenously or subcutaneously. In healthy individuals, following intravenous administration, the drug displays a nonlinear pharmacokinetics and follows a two-compartment model, characteristic of target-mediated drug disposition.20 Following administration of subcutaneous caplacizumab 10 mg once daily in healthy volunteers, maximum serum concentration (Cmax) was reached 6–7 h post-dose, with steady state reached following the first administration. The drug is rapidly and almost completely absorbed in the systemic circulation following subcutaneous administration, with a central volume of distribution of 6.33 L in patients with aTTP. The elimination half-life of caplacizumab is concentration- and target-level dependent; the level of vWF antigen present determines the level of caplacizumab target complex retained in the circulation. Target-bound caplacizumab is thought to be catabolized hepatically, whereas unbound caplacizumab is thought to undergo renal clearance.20,23
Caplacizumab in aTTP
The clinical efficacy of caplacizumab in patients with aTTP was tested in the TITAN and HERCULES trials, which are going to be evaluated in detail.24–26 These studies are summarized in Table 1.
Table 1.
The efficacy and safety data of both Phase II TITAN and Phase III HERCULES trials
| Phase II TITAN trial24
|
Phase III HERCULES trial26
|
|||
|---|---|---|---|---|
| Study arm | Placebo arm | Study arm | Placebo arm | |
|
| ||||
| Number of patients, n | 36 | 39 | 73 | 72 |
|
| ||||
| Primary outcome (platelet normalization, days) | 2.97 (p=0.005)* | 4.79 | 2.95 (p=0.01)* | 4.5 |
| Key secondary outcomes | ||||
| CR, n (%) | 29 (81) | 18 (46) | NA | NA |
| Exacerbation, n (%) | 3 (8) | 11 (28) | 3 (4) | 28 (38) |
| TTP-related death, n (%) | 0 | 2 (5) | 0 | 3 (4) |
| MTE during study period, n (%) | 1 (2) | 6 (15) | 6 (8) | 6 (8) |
| Recurrence after double-blind treatment period, n (%) | NA | NA | 6 (8) | 0 |
| Recurrence after 1 month of follow-up, n (%) | 8 (22) | 0 | NA | NA |
| Recurrence after 12 months of follow-up, n (%) | 11 (31) | 3 (8) | NA | NA |
| Refractory TTP, n | 0 | 4 (10) | 0 | 3 |
| Median time to normalization of end organ parameters, days | 3 | 4 | 2.86 | 3.36 |
|
| ||||
| Other secondary outcomes | ||||
| Mean PEX, days | 5.9 | 7.9 | 5 | 7 |
| Mean PV, L | 19.9 | 28.3 | 18.1 | 26.9 |
| Hospital stay, days | NA | NA | 9 | 12 |
| Patients followed in ICU, n | NA | NA | 28 | 27 |
| Number of days in ICU | NA | NA | 3 | 5 |
|
| ||||
| AEs | ||||
| Therapy-related AEs, n (%) | 6 (17) | 4 (11) | 41 (57.7) | 32 (43.8) |
| Possibly related AEs, n (%) | 19 (54) | 3 (8) | NA | NA |
| Serious TEAEs, n (%) | 13 (37) | 12 (32) | 29 (39.4) | 39 (53.4) |
| Therapy-related serious AEs, n (%) | NA | NA | 10 (14.1) | 4 (5.5) |
| Drug discontinuation, n (%) | 4 (11) | 2 (5) | 5 (7) | 9 (12.3) |
| Bleeding, n (%) | 19 (54) | 14 (38) | 49 (65) | 35 (48) |
| Serious bleeding, n (%) | 2 (5) | 2 (5) | 8 (10) | 1 (1) |
|
| ||||
| Post hoc analysis (TITAN+HERCULES trials)31 | ||||
|
| ||||
| Patients receiving caplacizumab (n=109) | Patients receiving placebo (n=111) | |||
|
| ||||
| TTP-related death, n (%) | 0 | 4 (3.6) | ||
|
| ||||
| MTEs, n (%) | 8 (7.4) | 14 (12.4) | ||
|
| ||||
| Exacerbation, n (%) | 6 (5.6) | 39 (34.8) | ||
|
| ||||
| Recurrence (whole study period), n (%) | 17 (15) | 3 (2) | ||
|
| ||||
| Refractoriness, n (%) | 0 | 7 (6.8) | ||
|
| ||||
| Death, n (%) | 1 (3.9) | 5 (4.5) | ||
Note:
These p-values indicate the differences between the study arms and the placebo arms of each study.
Abbreviations: AE, adverse event; CR, complete remission; ICU, intensive care unit; MTE, major thromboembolic event; NA, not available; PEX, plasma exchange; PV, plasma volume; TEAE, treatment-emergent adverse event; TTP, thrombotic thrombocytopenic purpura.
TITAN study
Study design
TITAN study (ClinicalTrials.gov Identifier: NCT01151423) is a single-blind, parallel-design, randomized, placebo-controlled multinational Phase II trial, in which adult patients with an acute episode of aTTP were recruited if they had a platelet count of <100 × 109/L, without active bleeding and required PEX.24 Seventy-five patients were assigned in a 1:1 ratio to caplacizumab (n=36) or placebo (n=39), in addition to daily PEX and immunosuppressive therapy, which is the standard-of-care treatment for aTTP. Patients received an intravenous loading dose of caplacizumab (10 mg) or placebo prior to the start of the first PEX. Throughout the PEX period, the study drug was administered subcutaneously 10 mg daily within 30 minutes after the end of each exchange. Once-daily subcutaneous administration of the study drug (10 mg) was continued for 30 days after the last PEX. The maximum duration of study drug administration was 90 days (Table 1).24
Evaluation of efficacy
The primary end point was the time to confirmed normalization of the platelet count, which was defined as a platelet count that was ≥150 × 109/L and a lactate dehydrogenase (LDH) level that was not higher than twice the upper limit of normal, and caplacizumab 10 mg significantly reduced the time to confirmed normalization of the platelet count by 39% compared with placebo (median 2.97 vs 4.79 days; p=0.005).24 As indicated by faster platelet count normalization, caplacizumab prevented further consumption of platelets into microthrombi and the consequent tissue ischemia, which led to a more rapid resolution of TTP episodes.
In terms of secondary end points, complete remission was more frequently observed in the caplacizumab arm (81% vs 46%). Three patients (8.3%) receiving caplacizumab had exacerbations, whereas 11 patients (28.2%) in the placebo arm had experienced an exacerbation. During the 1-month follow-up period, after cessation of treatment, eight patients in the caplacizumab arm had relapsed (seven of them within 10 days) with no relapse observed among patients receiving placebo treatment.24 In the seven patients who experienced a relapse within 10 days after the study drug had been stopped, ADAMTS13 activity was <10% shortly before the end of treatment. The mean number of PEX days and the mean volume of plasma administered were lower in the caplacizumab arm (5.9 vs 7.9 days and 19.9 vs 28.3 L, respectively) during the overall treatment period, including exacerbations (7.7 vs 11.7 days and 25.8 vs 41.8 L, respectively) than those of the placebo arm. Also, biomarkers reflecting ischemic organ damage tended to normalize more rapidly in patients receiving caplacizumab than those receiving placebo (Table 1).
Supporting the fact that caplacizumab does not address the underlying autoimmune pathophysiology in aTTP, there was a high rate of relapse after stopping caplacizumab 30 days after the last PEX session. These results might indicate that, as the relapsing patients had low ADAMTS13 activity (<10%), ADAMTS13 activity could potentially guide decisions about the duration and timing of caplacizumab and immunosuppressive treatment. These results also support the use of ADAMTS13 activity as a predictive marker to identify patients at risk for relapse. ADAMTS13 assays help to confirm the diagnosis and monitor the course of the disease and possible need for additional treatments. It was shown that a reduction in the enzyme level (<10%) is a marker to consider elective rituximab treatment, which results in normalization of ADAMTS13 activity and prevents an acute episode.24 Also, patients with ADAMTS13 activity <10% or an anti-ADAMTS13 autoantibody detected during remission had a threefold increase in relapse over 1 year.27 In another study, if ADAMTS13 was <5% in remission, relapse occurred in 38.5%, but if ADAMTS13 activity was >15%, only 5% relapsed.28 Sometimes, patients may require and benefit from long-term monitoring of ADAMTS13 activity and anti-ADAMTS13 autoantibody.1 Maybe, it can be concluded that the drug should better not be stopped until ADAMTS13 levels increase (eg, ≥10%), similar to that done in the HERCULES trial,25,26 or continuing caplacizumab until a response to a second-line treatment (eg, rituximab) is achieved (not only clinical response but also an increase in the ADAMTS13 levels) can be reasonable therapeutic maneuver.24,29
Adverse events
In the TITAN study, treatment-emergent adverse events (TEAEs) were reported in six patients (17%) receiving caplacizumab and four patients (11%) receiving placebo, and events that were possibly related to the study drug were reported in 19 (54%) and three patients (8%) in the caplacizumab and placebo arms, respectively.24 Serious TEAEs were reported in 13 patients (37%) in the caplacizumab group and 12 patients (32%) in the placebo group. Bleeding-related TEAEs, most of which were mild to moderate in severity, were more common in the caplacizumab group than in the placebo group (54% – 19 patients vs 38% – 14 patients).24 Eighty-four (83%) of the 101 bleeding-related TEAEs were reported as mild, 14 (14%) as moderate, and three events (3%) as severe. Serious bleeding-related adverse events (AEs) were reported in two patients in each study group: subarachnoid and retinal hemorrhage and metrorrhagia in the caplacizumab arm and cerebral hemorrhage and hematuria in the placebo arm. No patient received factor VIII or vWF for a bleeding event. Drug discontinuation due to the therapy was reported in four and two patients in the caplacizumab and placebo groups, respectively (Table 1). Immune-related TEAEs were reported in 17 patients (49%) in the caplacizumab arm and 12 patients (32%) receiving placebo had an immune-related AE. One caplacizumab-treated patient had a moderate allergic dermatitis that was reported as a serious AE.
Post hoc analysis of TITAN study
The clinical benefit of caplacizumab was further investigated in a post hoc analysis of the incidence of major thromboembolic events (MTEs) and exacerbations during the study drug treatment period and TTP-related death during the study.30 Four events (one pulmonary embolism and three TTP exacerbations) were reported in four patients receiving caplacizumab, and 14 patients in the placebo arm had experienced 20 events (two acute myocardial infarctions, one ischemic stroke, one hemorrhagic stroke, one pulmonary embolism, one deep vein thrombosis, one venous thrombosis, and 13 TTP exacerbations). Two patients in the placebo arm died from TTP during the study. In total, 11.4% of the caplacizumab-treated patients and 43.2% of the placebo-treated patients experienced one or more MTEs, experienced an exacerbation, or died, which underlines the potential for caplacizumab to reduce the risk of MTEs and mortality associated with aTTP.
HERCULES study
Study design
Caplacizumab was currently further evaluated in the HERCULES trial, which is a double-blind, placebo-controlled, multicenter Phase III study (ClinicalTrials.gov Identifier: NCT02553317), which was first presented at the 59th American Society of Hematology (ASH) meeting25 and then was published recently.26 One-hundred and forty-five patients with an acute episode of aTTP who had received one PEX treatment were randomized 1:1 to placebo (n=73) or 10 mg caplacizumab (n=72), in addition to daily PEX and corticosteroids. Similar to the TITAN trial, a single intravenous dose of caplacizumab was given before the first on-study PEX and a subcutaneous dose was given daily during the PEX period and 30 days thereafter. With the evidence gathered from the TITAN trial,24 in patients with low (<10%) ADAMTS13 activity at the end of this period, which was thought to be a possible sign of ongoing disease, investigators were encouraged to extend the blinded treatment for a maximum of 4 weeks together with optimization of immunosuppression (Table 1).25,26 Primary end point was time to platelet count response, defined as a platelet count of ≥150 × 109/L with stop of daily PEX within 5 days. There were four secondary end points; first one was a composite of aTTP-related death, aTTP recurrence, or MTE during the study drug treatment period, second one was recurrences during the entire study period, third one evaluated refractoriness to therapy, and the last one was the time to normalization of the following three organ damage markers: LDH, cardiac troponin I, and serum creatinine.
Evaluation of efficacy
During the study drug treatment period, caplacizumab therapy resulted in a 74% reduction in TTP-related death, recurrence of TTP, or an MTE (either one of these three outcomes occurred in nine patients [12%] in the caplacizumab group vs 36 [45%] in the placebo group [p<0.0001]).25,26 During the overall study period, 28 patients (38%) receiving placebo experienced a recurrence versus nine patients (12%) in the caplacizumab arm, showing a 67% reduction (p<0.001). In all six caplacizumab-treated patients who had a relapse during the follow-up period, ADAMTS13 activity was still <10% at the time of the discontinuation of the study drug, reflecting ongoing disease. A total of 31 patients experienced exacerbations in both arms, of which 28 had an ADAMTS13 activity below 10% measured after the last PEX. Nine out of the 29 patients with an ADAMTS13 activity <10% after drug/placebo discontinuation had a relapse. No caplacizumab-treated patients remained refractory, whereas three patients on placebo were (p=0.057). Treatment with caplacizumab was associated with a trend toward faster normalization of the three organ damage markers. Patients in the caplacizumab arm had fewer days on PEX, required less volume of plasma, and had shorter hospital stay (Table 1).
Adverse events
In the caplacizumab group, the most common TEAEs were epistaxis, gingival bleeding, and bruising. Treatment-related serious bleeding events were reported in eight patients with caplacizumab (11%) and three placebo-treated patients (4%). Mucocutaneous bleedings were more common in patients receiving caplacizumab than that of the placebo arm as expected (65% vs 48%). The frequency of at least one study drug-related AE was 57.7% for caplacizumab arm and 43.8% in patients receiving placebo, whereas the frequency of at least one drug-related AE leading to study drug discontinuation was 7% and 12.3% for the caplacizumab and placebo arms, respectively. At least one serious TEAE was reported in 39.4% of the caplacizumab and 53.4% of the placebo recipients, with at least 14% and 6%, respectively, considered possibly therapy-related. During the study drug treatment period, three patients on placebo died. One caplacizumab-treated patient died during the follow-up period, and it was thought not to be related to the study drug (Table 1).
ASH 2018 meeting abstracts
At the most recent ASH meeting, there were four abstracts regarding caplacizumab and aTTP.31–34 These abstracts were summarized as follows:
In this oral abstract (Abstract No: 373), the authors presented the results of the integrated efficacy analyses of both Phase II TITAN and Phase III HERCULES.31 The authors concluded that treatment with caplacizumab significantly reduced the time to platelet count response compared to treatment with placebo. In addition to that, caplacizumab treatment produced statistically significant reductions in 1) the percentage of patients with TTP-related death, a recurrence of TTP, or at least one treatment-emergent MTE; 2) the percentage of patients who died from TTP during the study drug treatment period; 3) the percentage of patients with a recurrence of TTP during treatment and overall; 4) the number of patients who remain refractory to therapy; and 5) the mean number of days of PEX (Table 1).31 The post hoc analysis of both TITAN and HERCULES trials, which were presented in this abstract, is summarized in Table 1.
In this poster presentation (Abstract No: 1142), the authors presented the risk factors and manageability of the bleeding events observed in the HERCULES study.32 As a result, the authors concluded that the safety profile of caplacizumab was favorable. As expected, caplacizumab was associated with an increased risk of mucocutaneous bleeding. These events were generally mild to moderate, and the majority did not require therapeutic intervention. The authors also evaluated the bleeding events in relation to the use of concomitant antithrombotic therapy and direct oral anticoagulants (DOACs), and although the number of patients receiving DOACs was low, no increased risk for bleeding with antithrombotic therapy was observed.32
In this poster presentation (Abstract No: 3739), the authors overviewed the safety and tolerability data from Phase II and Phase III studies of caplacizumab,33 knowing the fact that the main expected safety risk of the drug is bleeding. The results showed that bleeding TEAEs, mainly epistaxis and gingival bleeding, were the most common TEAEs in patients treated with caplacizumab. No new safety signals were identified in the other populations studied, and the authors concluded that caplacizumab was well tolerated and had a favorable safety profile.33
In the last abstract regarding caplacizumab, the HERCULES study collaborators evaluated the trial data and performed a post hoc analysis of the safety results normalized to time of exposure during the double-blind treatment period (Abstract No: 3744).34 The results showed that the TEAEs, which occurred more frequently in the caplacizumab group were epistaxis and gingival bleeding, whereas TTP, hypokalemia, contusion, rash, insomnia, and hypertension occurred more frequently in the placebo arm. This post hoc analysis confirmed that caplacizumab was tolerated well, with the overall good tolerability for the treatment of aTTP with mucocutaneous bleeding being the most relevant risk.34
Conclusion
Although PEX together with corticosteroids are the backbone of the upfront management of patients with aTTP with successful outcomes, patients may remain refractory and/or relapse following an initial response to this treatment. There are some therapeutic options, which can be used among these patients and help in improving outcomes of aTTP. Caplacizumab has recently been approved in adult patients experiencing an episode of aTTP in the EU. The drug mainly has a protective effect in the acute phase aTTP; however, it does not modify the underlying immune pathophysiology of aTTP and patients still need to use it in combination with immunosuppression. Future studies are needed, which will focus on the risk factors for relapse including ADAMTS13 activity and anti-ADAMTS13 autoantibodies, which can stop caplacizumab activity and to evaluate whether these tests can be used to guide the duration of therapy, together with the potential role of caplacizumab in refractory aTTP.
Acknowledgments
The authors would like to thank Prof. Teoman Soysal for his continuous guidance and support.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Scully M, Hunt BJ, Benjamin S, et al. British committee for standards in haematology. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323–335. doi: 10.1111/j.1365-2141.2012.09167.x. [DOI] [PubMed] [Google Scholar]
- 2.Rizzo C, Rizzo S, Scirè E, et al. Thrombotic thrombocytopenic purpura: a review of the literature in the light of our experience with plasma exchange. Blood Transfus. 2012;10(4):521–532. doi: 10.2450/2012.013S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell WR, Braine HG, Ness PM, Kickler TS. Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 1991;325(6):398–403. doi: 10.1056/NEJM199108083250605. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen L, Li X, Duvall D, Terrell DR, Vesely SK, George JN. Twice-daily plasma exchange for patients with refractory thrombotic thrombocytopenic purpura: the experience of the Oklahoma Registry, 1989 through 2006. Transfusion. 2008;48(2):349–357. doi: 10.1111/j.1537-2995.2007.01530.x. [DOI] [PubMed] [Google Scholar]
- 5.Balduini CL, Gugliotta L, Luppi M, et al. Italian TTP study group. High versus standard dose methylprednisolone in the acute phase of idiopathic thrombotic thrombocytopenic purpura: a randomized study. Ann Hematol. 2010;89(6):591–596. doi: 10.1007/s00277-009-0877-5. [DOI] [PubMed] [Google Scholar]
- 6.Öngören S, Salihoğlu A, Apaydın T, et al. Vincristine as an adjunct to therapeutic plasma exchange for thrombotic thrombocytopenic purpura: a single-institution experience. Balkan Med J. 2018;35(6):417–421. doi: 10.4274/balkanmedj.2017.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ziman A, Mitri M, Klapper E, Pepkowitz SH, Goldfinger D. Combination vincristine and plasma exchange as initial therapy in patients with thrombotic thrombocytopenic purpura: one institution’s experience and review of the literature. Transfusion. 2005;45(1):41–49. doi: 10.1111/j.1537-2995.2005.03146.x. [DOI] [PubMed] [Google Scholar]
- 8.Beloncle F, Buffet M, Coindre J-P, et al. Thrombotic microangiopathies reference center. Splenectomy and/or cyclophosphamide as salvage therapies in thrombotic thrombocytopenic purpura: the French TMA reference center experience. Transfusion. 2012;52(11):2436–2444. doi: 10.1111/j.1537-2995.2012.03578.x. [DOI] [PubMed] [Google Scholar]
- 9.Yilmaz M, Eskazan AE, Unsal A, et al. Cyclosporin A therapy on idiopathic thrombotic thrombocytopenic purpura in the relapse setting: two case reports and a review of the literature. Transfusion. 2013;53(7):1586–1593. doi: 10.1111/j.1537-2995.2012.03944.x. [DOI] [PubMed] [Google Scholar]
- 10.Cataland SR, Jin M, Ferketich AK, et al. An evaluation of cyclosporin and corticosteroids individually as adjuncts to plasma exchange in the treatment of thrombotic thrombocytopenic purpura. Br J Haematol. 2007;136(1):146–149. doi: 10.1111/j.1365-2141.2006.06384.x. [DOI] [PubMed] [Google Scholar]
- 11.Kappers-Klunne MC, Wijermans P, Fijnheer R, et al. Splenectomy for the treatment of thrombotic thrombocytopenic purpura. Br J Haematol. 2005;130(5):768–776. doi: 10.1111/j.1365-2141.2005.05681.x. [DOI] [PubMed] [Google Scholar]
- 12.Lim W, Vesely SK, George JN. The role of rituximab in the management of patients with acquired thrombotic thrombocytopenic purpura. Blood. 2015;125(10):1526–1531. doi: 10.1182/blood-2014-10-559211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vazquez-Mellado A, Pequeño-Luévano M, Cantu-Rodriguez OG, et al. More about low-dose rituximab and plasma exchange as front-line therapy for patients with thrombotic thrombocytopenic purpura. Hematology. 2016;21(5):311–316. doi: 10.1080/10245332.2015.1133008. [DOI] [PubMed] [Google Scholar]
- 14.Scully M, McDonald V, Cavenagh J, et al. A phase 2 study of the safety and efficacy of rituximab with plasma exchange in acute acquired thrombotic thrombocytopenic purpura. Blood. 2011;118(7):1746–1753. doi: 10.1182/blood-2011-03-341131. [DOI] [PubMed] [Google Scholar]
- 15.Page EE, Kremer Hovinga JA, Terrell DR, Vesely SK, George JN. Rituximab reduces risk for relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2016;127(24):3092–3094. doi: 10.1182/blood-2016-03-703827. [DOI] [PubMed] [Google Scholar]
- 16.Hie M, Gay J, Galicier L, et al. French thrombotic microangiopathies reference centre. Preemptive rituximab infusions after remission efficiently prevent relapses in acquired thrombotic thrombocytopenic purpura. Blood. 2014;124(2):204–210. doi: 10.1182/blood-2014-01-550244. [DOI] [PubMed] [Google Scholar]
- 17.Rottenstreich A, Hochberg-Klein S, Rund D, Kalish Y. The role of N-acetylcysteine in the treatment of thrombotic thrombocytopenic purpura. J Thromb Thrombol. 2016;41(4):678–683. doi: 10.1007/s11239-015-1259-6. [DOI] [PubMed] [Google Scholar]
- 18.Eskazan AE. Bortezomib therapy in patients with relapsed/refractory acquired thrombotic thrombocytopenic purpura. Ann Hematol. 2016;95(11):1751–1756. doi: 10.1007/s00277-016-2804-x. [DOI] [PubMed] [Google Scholar]
- 19.Masias C, Cataland SR. Novel therapies in thrombotic thrombocytopenic purpura. Res Pract Thromb Haemost. 2017;2(1):19–26. doi: 10.1002/rth2.12066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.European Medicines Agency Cablivi (caplacizumab): summary of product characteristics. 2018. [Accessed October 8, 2018]. Available from: http://www.ema.europa.eu.
- 21.Ulrichts H, Silence K, Schoolmeester A, et al. Antithrombotic drug candidate ALX-0081 shows superior preclinical efficacy and safety compared with currently marketed antiplatelet drugs. Blood. 2011;118(3):757–765. doi: 10.1182/blood-2010-11-317859. [DOI] [PubMed] [Google Scholar]
- 22.Callewaert F, Roodt J, Ulrichts H, et al. Evaluation of efficacy and safety of the anti-VWF nanobody ALX-0681 in a preclinical baboon model of acquired thrombotic thrombocytopenic purpura. Blood. 2012;120(17):3603–3610. doi: 10.1182/blood-2012-04-420943. [DOI] [PubMed] [Google Scholar]
- 23.Duggan S. Caplacizumab: first global approval. Drugs. 2018;78(15):1639–1642. doi: 10.1007/s40265-018-0989-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peyvandi F, Scully M, Kremer Hovinga JA, et al. TITAN investigators. caplacizumab for acquired thrombotic thrombocytopenic purpura. N Engl J Med. 2016;374(6):511–522. doi: 10.1056/NEJMoa1505533. [DOI] [PubMed] [Google Scholar]
- 25.Scully M, Cataland SR, Peyvandi F, et al. Results of the randomized, double-blind, placebo-controlled, phase 3 HERCULES study of caplacizumab in patients with acquired thrombotic thrombocytopenic purpura [abstract no. LBA-1 plus presentation] Blood. 2017;130:1. [Google Scholar]
- 26.Scully M, Cataland SR, Peyvandi F, et al. HERCULES investigators. caplacizumab treatment for acquired thrombotic thrombocyto-penic purpura. N Engl J Med. 2019;380(4):335–346. doi: 10.1056/NEJMoa1806311. [DOI] [PubMed] [Google Scholar]
- 27.Westwood JP, Webster H, McGuckin S, McDonald V, Machin SJ, Scully M. Rituximab for thrombotic thrombocytopenic purpura: benefit of early administration during acute episodes and use of prophylaxis to prevent relapse. J Thromb Haemost. 2013;11(3):481–490. doi: 10.1111/jth.12114. [DOI] [PubMed] [Google Scholar]
- 28.Peyvandi F, Lavoretano S, Palla R, et al. ADAMTS13 and anti-ADAMTS13 antibodies as markers for recurrence of acquired thrombotic thrombocytopenic purpura during remission. Haematologica. 2008;93(2):232–239. doi: 10.3324/haematol.11739. [DOI] [PubMed] [Google Scholar]
- 29.Ferrari S, Scheiflinger F, Rieger M, et al. French clinical and biological network on adult thrombotic microangiopathies. Prognostic value of anti-ADAMTS 13 antibody features (ig isotype, titer, and inhibitory effect) in a cohort of 35 adult French patients undergoing a first episode of thrombotic microangiopathy with undetectable ADAMTS 13 activity. Blood. 2007;109(7):2815–2822. doi: 10.1182/blood-2006-02-006064. [DOI] [PubMed] [Google Scholar]
- 30.Peyvandi F, Scully M, Kremer Hovinga JA, et al. Caplacizumab reduces the frequency of major thromboembolic events, exacerbations and death in patients with acquired thrombotic thrombocytopenic purpura. J Thromb Haemost. 2017;15(7):1448–1452. doi: 10.1111/jth.13716. [DOI] [PubMed] [Google Scholar]
- 31.Peyvandi F, Cataland SR, Scully M, et al. Integrated efficacy results from the phase II and phase III studies with caplacizumab in patients with acquired thrombotic thrombocytopenic purpura. Blood. 2018;132:373. abstract. [Google Scholar]
- 32.Cataland SR, Scully M, Peyvandi F, et al. Risk factors and manageability of the mainly mild mucocutaneous bleeding profile observed in aTTP patients treated with caplacizumab during the phase III hercules study. Blood. 2018;132:1142. abstract. [Google Scholar]
- 33.Knöbl P, Scully M, Cataland SR, et al. Integrated safety results from the phase II and phase III studies with caplacizumab in patients with acquired thrombotic thrombocytopenic purpura. Blood. 2018;132:3739. abstract. [Google Scholar]
- 34.Kremer Hovinga JA, Scully M, Cataland SR, et al. Safety of caplacizumab for the treatment of patients with acquired thrombotic thrombocytopenic purpura – results normalized to time of exposure in a double-blind, placebo-controlled, phase 3 hercules study. Blood. 2018;132:3744. abstract. [Google Scholar]