Abstract
Background:
Rural women are at risk for health consequences (such as HIV) associated with substance misuse, but targeted interventions are limited for this population. Jails provide an underutilized opportunity for outreach to high-risk women in rural Appalachian communities.
Method:
Rural women were randomized to either the NIDA Standard education intervention (n = 201) or the NIDA Standard plus motivational interviewing (MI-HIV; n = 199) while in jail. Outcomes focused on HIV risk behaviors 3 months post-release from jail.
Results:
Decreases in HIV risk behaviors were observed at follow-up across conditions. Although participants in the MI-HIV group showed reductions in outcomes compared to the NIDA Standard group (OR = 0.82–0.93), these estimates did not reach significance (p values > .57).
Conclusions:
HIV education interventions can be associated with risk-reduction behaviors. These findings support the need for increased access to prevention education in criminal justice venues, particularly in rural communities.
Keywords: rural women, drug use, incarceration, HIV prevention, intervention
INTRODUCTION
Opioid misuse and infectious disease risk in rural Appalachia
The opioid epidemic is associated with significant public health consequences including the rising rates of infectious diseases, which has had a tremendous impact on rural Appalachian communities. While health disparities in Appalachia are often attributed to economic challenges, poverty, and limitations in health care access, these disparities are exacerbated by opioid misuse (1). Improvements of monitoring systems and pill reformulation during the last decade to deter illicit use have made little difference in the regional prevalence of rural Appalachian’s misuse of opioids.
The opioid epidemic is also associated with increased rates of injection drug use (IDU) in rural areas of Appalachian, particularly in Kentucky (2), as well as alarming trends in infectious disease transmission [such as Hepatitis C (HCV)] (3, 4, 5, 6). In fact, Kentucky (KY) had the highest proportionate rate of new HCV infections in the nation from 2008–2015 (3) and an overall prevalence rate nearly seven times higher than the national average (6). The high rate of HCV has been linked to injection drug use and needle sharing, high-risk behaviors that also significantly increase the vulnerability of persons who use drugs for contracting human immunodeficiency virus (HIV) infections. In fact, a recent Centers for Disease Control (CDC) report examined the indicator variables associated with IDU as a way of identifying U.S. counties most vulnerable to the rapid spread of HIV (7). In this report, rural Appalachian Kentucky counties were disproportionately represented in the list of 220 counties identified as most vulnerable, including about half of the counties in the top 50. Thus, while the overall HIV+ prevalence is relatively low in KY (7.6 per 100,000 [3]), individuals in rural Appalachian eastern KY are highly vulnerable for the rapid spread of HIV with limited access to effective interventions.
Rural Appalachian women at heightened risk
Rural Appalachian women are at heightened risk for health consequences associated with opioid and other substance misuse. Research indicates that women who use drugs, in general, are more likely to have injecting intimate partners, and with fewer economic resources to buy drugs, they are more likely to engage in sex exchange to obtain drugs (8). In addition, women have a faster trajectory from recreational use to substance use disorder than men (9, 10, 11).
These risk factors are even more pronounced in rural Appalachia where women face economic challenges, poverty, and limited health care access. In addition, adherence to or acceptance of traditional gender roles may also contribute to how rural Appalachian women define themselves in the context of relationships and how that identity relates to their drug use (12). Rural women who use drugs have been shown to have extensive injection histories (75%) and high rates of HCV (60%), with most (80%) meeting criteria for substance use disorder (13). In addition, the susceptibility for contracting infectious diseases is heightened among rural Appalachian women due to close knit drug-using networks involved in injection drug use and sharing practices (14). These risks are further complicated by apathy about contracting infectious diseases among rural women who use drugs. This apathy is illustrated by comments describing HCV as “common as a bad cold around here” and “it’s really not that big of a deal, everybody’s got it” (5). These factors bolster the need for targeted HIV risk-reduction interventions among rural Appalachian women.
Jail-based prevention
Despite the risks identified among rural Appalachians, there are currently no targeted HIV prevention interventions for rural women. In general, studies with rural women can be challenging due to limited formal treatment opportunities for recruitment, travel distances to study sites, and the general protective nature of rural social networks (15). Therefore, there is a need for HIV prevention interventions in settings where rural women who use drugs can be identified – such as jails. Conducting research in rural jails as places or venues to outreach to high-risk drug users is critical – not only because jails typically house a high volume of individuals who use drugs (16), but also because many of these women will never be identified as drug misusers, be assessed for HIV, or be engaged in risk-reduction interventions. Jails are different than prisons because they typically house individuals for a short period of time in local facilities and often have fewer resources for health and behavioral health services. Thus, it is feasible that jails provide an underutilized opportunity to outreach to disadvantaged, drug-using rural women at high-risk for HIV in understudied rural communities of Appalachia.
Study interventions
While there are no specific HIV prevention interventions tailored for rural women, one evidence-based approach to HIV risk reduction is the NIDA Standard. The NIDA Standard was developed through large, multisite NIDA funded cooperative agreement trials in the late 1980s (National AIDS Demonstration Research – NADR) and 1990s (Cooperative Agreement for AIDS Community-Based Outreach/Intervention Research), which were funded to educate high-risk injectors and encourage adoption of HIV prevention practices (e.g., 17). The NIDA Standard focuses on risk reduction education such as needle cleaning strategies, safe sex practices including the latex condom, and the importance of drug treatment. Through a series of randomized, controlled, experimental trials, the NIDA Standard decreased high-risk drug and/or sexual practices among high-risk drug using women (18, 19), noninjectors (20), out-of-treatment injectors (21), offenders at community re-entry (22), and ethnic minority drug users (23).
Another HIV risk-reduction approach that has been identified as a CDC evidence-based, best practice for high-risk criminal justice involved women with positive results is the Motivational Interviewing-based HIV Risk Reduction [MI-HIV] (24). Motivational interviewing is an individualized, targeted approach that has been shown to increase HIV knowledge and increase communication with partners (25), as well as to reduce the number of sexual partners (26), the number of unprotected sexual encounters (27), and disease transmission to sexual partners (28). The MI-HIV intervention demonstrated positive outcomes for safe sexual practices and reduced drug use in a randomized controlled trial with criminal justice-involved urban women (24).
Considering the effectiveness of HIV prevention interventions like the NIDA Standard and MIHIV, these interventions should be tailored for new contexts and underserved, high-risk populations. The effectiveness of HIV risk reduction interventions depends on whether or not high-risk individuals have access to those interventions (29, 30, 31). Thus, the current study examines the delivery of a prevention education-focused HIV risk reduction intervention (NIDA Standard) and an enhanced, individualized intervention for risk reduction (MI-HIV) in rural jails to target high-risk rural women who use drugs. Specifically, the study examines short-term outcomes at 3 months post-release from jail for high-risk rural women randomized to receive the NIDA Standard education intervention compared to women randomized to the NIDA Standard plus an enhanced risk-reduction intervention using motivational interviewing to reduce high-risk behaviors (MI-HIV). It is hypothesized that significant reductions in risk behavior will be observed for both conditions during the 3-month re-entry period compared to baseline (prior to incarceration). It is also expected that those who receive the enhanced intervention (MI-HIV) will report greater reductions in high-risk drug use and risky sexual practices due to the individualized and tailored approach using motivational interviewing.
METHOD
Participants
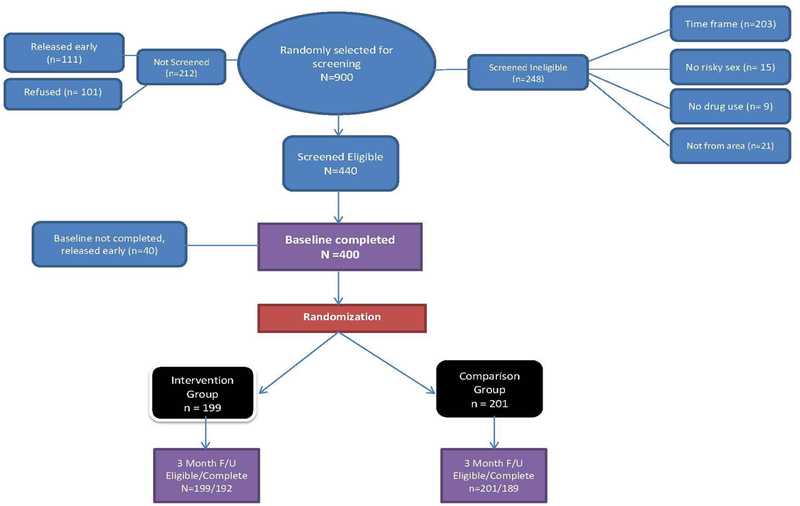
Study participants were high-risk, rural women randomly selected from three rural county jails in the Appalachian region of eastern Kentucky. Randomly selected women were screened for drug use and risky sexual practices using standardized criteria which included: 1) moderate need for substance misuse intervention based on the NIDA-modified Alcohol, Smoking and Substance Involvement Screening Test (NM-ASSIST) score of 4+ for any drug (32); 2) self-reported sexual risk behavior in the 3 months before incarceration (i.e., unprotected sex, sex while high); 3) residing in a designated Appalachian county before incarceration; and 4) willingness to participate. Participant enrollment is described in the study CONSORT (See Figure 1; see also [2]). During the study recruitment phase between December 2012 and August 2015, 900 women were randomly selected, 688 (76.4%) participated in the study screening sessions in the jails, 440 (64%) met study criteria for study enrollment, and 400 completed a baseline interview.
Figure 1.
Study CONSORT
Note. All participants in both intervention conditions completed the NIDA Standard. Of those in the Intervention group, 144 completed at least 3 of the 4 additional MI-HIV sessions (76%), 28 completed 1–2 MI-HIV sessions (15%), and 27 did not complete any of the sessions (14%).
Measures
Demographics –
Demographic variables included age (a continuous measure of self-reported age at the time of the baseline), education (a continuous measure of total number of years of formal education), race (self-reported racial group, coded as “white” and “other ethnicities”), marital status (categorically coded as married or living with someone as married vs. other), sexual orientation (self-reported and coded as “heterosexual” vs “other”), and employment (percentage of women reporting any employment including full-time or part-time prior to incarceration vs. not working). The Appalachian county of jail-based recruitment was also coded as the location of the rural jail (Perry, Leslie, or Laurel) in order to assess potential site differences. In addition, HCV status was coded as “seropositive” vs “seronegative” based on the initial baseline screening using ORAQUICK® rapid antibody test (described in Procedures).
Intervention groups –
Participants were randomly assigned to one of two intervention conditions: 1) a motivational interviewing plus NIDA standard intervention (MI-HIV + NIDA Standard; n = 199) or 2) NIDA standard alone (NIDA Standard; n = 201).
HIV Risk behaviors –
High-risk drug use during the community re-entry phase (3 months post-release from jail) was assessed using the GAIN (Global Appraisal of Individual Needs [33]). Specific measures included dichotomous codes (yes/no) for the following variables at both baseline (prior to incarceration) and at community re-entry (3 months post-release from jail): 1) illicit drug use in the past month, 2) use of drugs prior to the most recent sexual activity with a main or casual male sexual partner, 3) past month injection drug use (IDU), 4) shared needle use, and 5) shared injection equipment (works) use. Past month IDU, shared needle use, and shared works were only analyzed for participants with injection drug use in the year prior to isolate effects on active persons who inject drugs (PWID).
Covariates –
In order to assess the effects of the interventions during incarceration, factors associated with criminal justice involvement were treated as covariates including if this was the participants first incarceration, recidivism during the 3-month re-entry period, and community supervision (probation or parole) during the 3-month re-entry period. Additionally, whether a participant reported injecting illicit drugs in their lifetime (i.e., “Ever IDU”; ever injected versus never injected in lifetime) was included as a covariate for the illicit drug use in past month and the use of drugs prior to the most recent sexual activity outcomes given that Ever IDU was a potential indicator of severity of substance use.
Procedure
Random selection, screening, and interviewing procedures are described in detail elsewhere (2). In summary, this study used a random sampling approach to recruit hard-to-reach, out-of-treatment, rural drug-using women in three Appalachian area jails. Potential participants were selected based on simple random selection from the daily jail census report, indicating that each person on site on the screening day had an equal chance of being selected if their release dates were within 2 weeks to 3 months. Potential participants were screened for study eligibility in a group setting, and interviewed in the jail. Participants were paid $25 for the baseline interview, and all study screening and data collection procedures were approved by the university IRB and protected under a federal Certificate of Confidentiality.
Following the baseline interview, research staff presented cue cards from the NIDA Standard to educate all participants about the risks associated with contracting HIV through drug injection and risky sexual practices. The NIDA Standard was selected because it is a structured, evidence-based intervention with content consistent with CDC guidelines for core prevention information including education on the transmission of HIV/HCV, identifying risk behaviors, information on the reduction of risk behaviors, and the importance of referrals to treatment (34). Study research staff were trained and certified as HIV counselors by the State Department of Public Health.
At the conclusion of the NIDA Standard, participants were given the opportunity to be HIV and HCV tested using the OraQUICK ADVANCE® Rapid HIV-1/2 and OraQUICK ADVANCE® Rapid HCV Antibody Test kits, which have demonstrated sensitivity and specificity in clinical performance equivalent to current laboratory-based EIA (35, 36). Testing took place in a private office in each jail. Test results were available within 20 minutes, and participants received post-test counseling which included an explanation of the test result, referrals to resources either in the jail or in the community, and information about how to remain safe in the community. Regardless of test result, all women were retained in the study.
Randomization to intervention conditions was done at the individual level following the baseline and testing procedures using Research Randomizer (www.randomizer.org). Participants were informed about the intervention random assignment during the consent process, and they understood that they had a 50/50 chance of being included in one of the intervention conditions. Participants were either assigned to the 1) NIDA Standard intervention alone or 2) the NIDA Standard + MI-HIV. Participants in the NIDA Standard intervention alone did not receive any additional services during the remainder of their jail sentence. Participants in the MI-HIV had the opportunity to participate in up to 4 sessions of motivational interviewing with the study interventionist prior to their release from jail.
During the study, the same interventionist delivered all of the MI-HIV sessions with 199 participants in private rooms in each of the three jails. The interventionist was from rural Appalachia, and she was a certified social worker. Consistent with Weir and colleagues (24), core components of MI-HIV were delivered across four sessions which included: 1) identifying individual risky sexual behavior and risky drug use (including needle use) using an assessment tool, 2) discussing with the woman her perception of the risks associated with those behaviors, 3) determining her readiness to address those risks, and 4) engaging in stage-based discussions to target behavior change. Consistent with the overall approach of MI, the intervention allowed the woman’s individual level of commitment to change to guide the therapy sessions, and allowed for an individualized approach to each person’s unique situation and stressors, as well as her own risk behaviors and service utilization barriers. Thus, the intervention was targeted to each individual’s unique risk behaviors.
Participant files were monitored closely by research staff, and release dates were recorded in a study database. All study participants were followed 3 months post-release from jail to examine the changes in risky drug use and sexual practices. Of the 400 participants who completed a baseline interview, 398 were released to the community during the study window. Of those, 5 refused to complete a follow-up interview and 1 was deceased. Of the 392 remaining, 3-month follow-up interviews were completed with 381 women (97% follow-up rate). Follow-up rates did not significantly differ by intervention condition. Participant locating and tracking methods included phone calls, flyer mailings, internet searches, and social media outlets like Facebook (37). The follow-up interview was conducted face-to-face, and participants were paid $25.
Data Analysis
Univariate statistics initially examined the overall sample and intervention groups on demographic and drug use variables. Two study participants were excluded from analysis because of missing data on at least one primary outcome variable which included: 1) past month illicit drug use, 2) using drugs prior to the most recent sexual activity with a main or casual male sexual partner, 3) past month injection drug use (IDU), 4) shared needle use during the follow-up period, and 5) shared injection equipment (works) use during the follow-up period. For the IDU outcomes, only participants with injection drug use in the year prior to incarceration were included. Additionally, only 382 participants at baseline and 259 participants at the 3-month follow-up reported a recent sexual encounter with a male sexual partner. Preliminary analysis indicated that coding participants without a recent sexual encounter as either not available (missing) or as not engaging in the risk behavior revealed similar outcomes; therefore, the results reported are those in which the data were treated as missing to provide the closest continuity to the observed behavior (i.e., only measuring participants reporting sexual activity during the follow-up period).
Inspection of the data revealed a clear bimodal distribution when primary outcomes were treated as continuous (e.g., days past month drug use). Therefore, all outcome variables were dichotomously coded and logistic regression was used to avoid violating distributional assumptions. First, analyses focused on observed reductions in engagement in primary risk behaviors from baseline (prior to incarceration) and follow-up (3 months post-release from jail) across both study groups. McNemar’s test for paired nominal data was used to test for significant reductions in these dichotomous outcomes. Adjusted comparisons were then computed controlling for incarceration, incarceration history, probation & parole status, Ever IDU (as above) using generalized linear mixed-effects models with the glmer function in the lme4 package of R (38).
Second, unadjusted comparisons evaluating differences by study condition were computed. Adjusted comparisons were conducted controlling for incarceration during follow-up, incarceration history (first incarceration versus not first incarceration), probation & parole status, Ever IDU, and baseline risk behavior (e.g., controlling for baseline past month drug use for the past month drug use outcome). These covariates were included to control for exposure to risk behaviors during follow-up. Results of unadjusted odds ratios (OR) and adjusted odds ratios (AOR) are reported. Descriptive analyses and logistic regression were conducted using SPSS. Sample sizes for analyses are indicated in the text and tables. All analyses used two-tailed tests and an alpha rate of 0.05.
RESULTS
Sample Characteristics
Overall, the sample was white (99%), which is highly consistent with the overall racial make-up of the targeted counties – Perry County (97% white), Leslie County (98% white), and Laurel County (97% white) (www.census.gov). Participants were a mean age of 32.8 and had 11.1 years of education (See Table I). A majority of women reported unemployment in the six months before incarceration (68.8%) and most indicated this was not their first incarceration (90.7%). Approximately 75% of women reported a history of IDU (i.e., ever injected illicit drugs) and a majority of women in the total sample reported IDU in the year prior to incarceration (59.8%). More than half (59%) screened positive for HCV antibodies, but no women screened positive for HIV.
Table I.
Sample Descriptive and Intervention Outcome Information
| Overall (N = 400) | MI + NIDA Standard (n = 199) | NIDA Standard (n = 201) | |
|---|---|---|---|
| Baseline Demographics (n=400) | |||
| Age | 32.8 (8.2) | 33.1 (8.1) | 32.6 (8.4) |
| Years Education | 11.1 (2.3) | 11.2 (2.2) | 11.0 (2.4) |
| White | 99.0% | 99.0% | 99.0% |
| Married | 36.8% | 35.7% | 37.8% |
| Heterosexual | 79.3% | 76.9% | 81.6% |
| Unemployed | 68.8% | 69.3% | 68.2% |
| HCV Seropositivea | 59.0% | 59.8% | 58.1% |
| First Incarceration | 9.3% | 6.1% | 12.6%* |
| County | |||
| Perry | 31.0% | 31.7% | 30.3% |
| Leslie | 30.2% | 31.1% | 29.4% |
| Laurel | 38.8% | 37.2% | 40.3% |
| Ever IDU | 75.5% | 76.4% | 74.6% |
| Past Year IDU | 59.8% | 58.8% | 60.7% |
| Primary outcomes: Baseline (prior to incarceration) | |||
| Past Month Drug Use | 92.3% | 94.0% | 90.5% |
| Use Drugs Before Last Sexual Act | 84.6% | 85.3% | 83.8% |
| Past Month IDUb | 84.9% | 84.6% | 85.2% |
| Used Shared Needleb | 81.9% | 84.6% | 79.3% |
| Used Shared Worksb | 74.8% | 74.4% | 75.2% |
| Primary outcomes: Follow-up (3 months post jail release, n = 381) | |||
| Past Month Drug Use | 34.3% | 33.5% | 35.1% |
| Use Drugs Before Last Sexual Actc | 33.2% | 31.7% | 34.6% |
| Past Month IDUb | 19.5% | 18.6% | 20.3% |
| Used Shared Needleb | 19.0% | 18.6% | 19.5% |
| Used Shared Worksb | 16.5% | 15.0% | 17.8% |
Note. Married = married or living as married [dichotomous]; Employment = employed in the 6 months prior to incarceration; HCV= hepatitis C; First Incarceration = the current incarceration is the participant’s first incarceration [dichotomous]; IDU = injection drug use.
Significant difference between MI + NIDA Standard and NIDA Standard groups χ2 = 4.90; p = .03
37 participants refused an HCV test (tested n = 363)
only participants reporting IDU in the year before incarceration (n = 239)
only participants reporting a male sexual encounter in the 3 months post release (n = 259)
At the time of study randomization, most women reported past month drug use prior to incarceration (92.3%) and most indicated drug use prior to their last sexual encounter (84.6%). Among IDUs in the year before incarceration, a majority reported injecting in the month before incarceration (84.9%) as well as self-reporting using a shared needle (81.6%) or shared works (74.8%) during the year prior to incarceration. Intervention groups did not differ on baseline characteristics, except participants in the NIDA Standard group were significantly more likely to be incarcerated for the first time (12.4% versus 6.0%) (χ2 = 4.90; p = .03). Baseline drug use characteristics also did not differ by intervention group (See Table I).
Intervention engagement
Of the 400 women who completed a baseline interview, 201 were randomized to the NIDA Standard condition and 199 were randomized to the NIDA Standard + MI-HIV conditions. Of the MIHIV participants, 130 participants (65.3%) completed all 4 sessions, 14 (7.0%) completed 3 sessions, 28 (14.0%) completed 1–2 sessions, and 27 (13.6%) did not engage in any sessions. Reasons for not engaging in any sessions included no longer being interested, being transferred to a different facility, or being released to the community early. The mean number of sessions attended was 3.1 (SD = 1.5) of the 4 possible sessions.
Re-entry risk behaviors
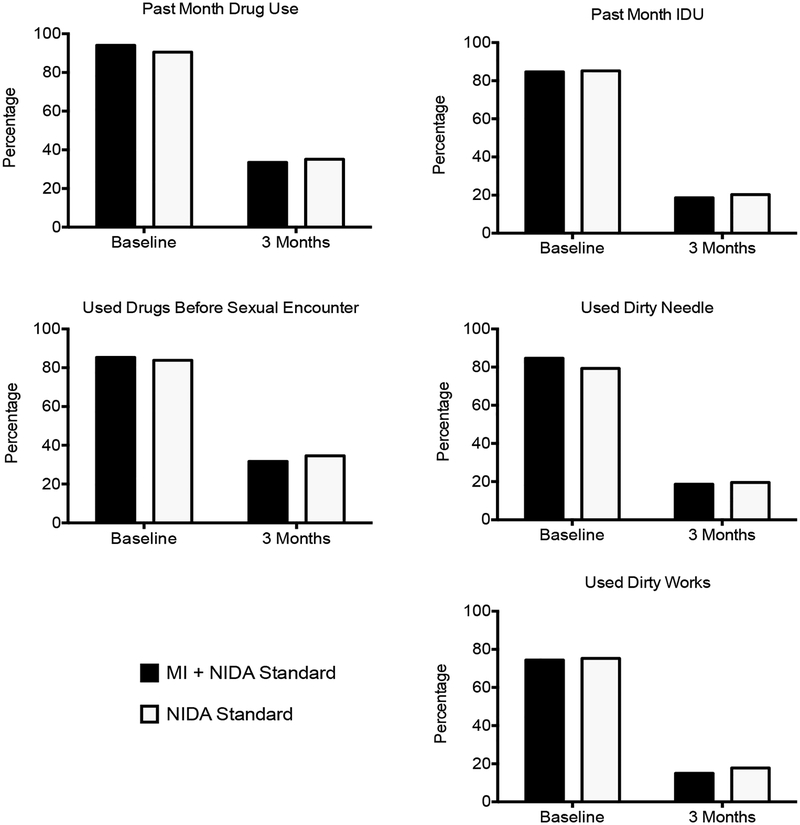
Overall, robust decreases in the number of participants reporting each HIV risk behavior were observed at the 3-month follow-up (Figure 2). Unadjusted comparisons using McNemar’s test for paired nominal data supported these robust reductions collapsing across intervention groups (χ2 = 120 to 202; p values < .001) and within individual groups (χ2 = 55 to 109; p values < .001). These reductions remained significant and robust after controlling for criminal justice variables (incarceration history, reincarceration during community re-entry, and probation/parole status) and Ever IDU using generalized linear mixed-effect models (OR 0.01–0.02; p values < .001). Inclusion of group by time (baseline to follow-up) interactions did not indicate significant main effects or interactions with intervention group (OR = 0.42–2.12; p values > .13), consistent with the intention-to-treat intervention analysis described below.
Figure 2.
Reductions in drug and injection drug use at 3-month follow-up. Participants were randomized to a motivational interviewing plus NIDA standard intervention (black bars; MI + NIDA Standard; n = 199) or NIDA standard alone (white bars; NIDA Standard; n = 201). Plotted are the percentages of participants reporting drug use, injection drug use, or risky behaviors in the month prior to incarceration and during the 3-month follow-up period. Reductions at the 3-month period were significant in unadjusted and adjusted analyses for all measures.
Group Effects: Intention-to-Treat Analysis
Table II presents unadjusted and adjusted estimates for the effect of intervention group on the five primary study outcomes at the 3-month follow-up (past month drug use, drug use prior to sex, past month injection drug use, shared needle use, shared works). Although participants in the NIDA Standard + MIHIV group showed reductions in the reported outcomes compared to the NIDA Standard group (OR = 0.82–0.93), these unadjusted estimates did not reach statistical significance (p values > .57). Similar results were observed after adjusting for reincarceration, incarceration history, probation & parole status, Ever IDU, and baseline risk behavior (AOR = 0.69–1.05; p values > .34). Consistent outcomes were also observed when analyzing by individual drug types as dependent variables (i.e., cannabis, cocaine, prescription opioids, and heroin, data not shown).
Table II.
Summary of Intervention Outcome Models
| Past Month Drug Usea | Sex After Drug Useb | |||||
|---|---|---|---|---|---|---|
| OR | AOR | OR | AOR | |||
| Back In Jail | 2.15 (1.19, 3.90)* | 7.56 (3.10, 18.40)*** | ||||
| First incarceration | 0.37 (0.14, 0.99)* | 0.94 (0.29, 3.00) | ||||
| P&P | 0.61 (0.38, 0.96)* | 0.84 (0.46, 1.55) | ||||
| Ever IDU | 1.17 (0.67, 2.05) | 3.00 (1.20, 7.53)* | ||||
| Baseline | 1.47 (0.54, 4.02) | 9.09 (2.40, 34.35)** | ||||
| Group | 0.93 (0.61, 1.42) | 0.94 (0.60, 1.48) | 0.88 (0.52, 1.48) | 1.05 (0.57, 1.92) | ||
| Model R2 | <.01 | .06 | <.01 | .26 | ||
| Past Month IDUc | Shared Needle Usec | Shared Works Usec | ||||
| OR | AOR | OR | AOR | OR | AOR | |
| Back In Jail | 5.48 (2.42, 12.38)*** | 4.26 (1.91, 9.51)*** | 3.88 (1.62, 9.32)** | |||
| First incarceration | 0.32 (0.04, 2.52) | 0.31 (0.04, 2.45) | 0.34 (0.04, 2.76) | |||
| P&P | 0.60 (0.28, 1.31) | 0.87 (0.41, 1.85) | 0.86 (0.39, 1.89) | |||
| Baseline | 1.40 (0.48, 4.15) | 1.88 (0.66, 5.38) | 8.29 (1.85, 37.10)** | |||
| Group | 0.89 (0.47, 1.72) | 0.86 (0.42, 1.78) | 0.94 (0.49, 1.82) | 0.90 (0.44, 1.85) | 0.82 (0.41, 1.65) | 0.69 (0.32, 1.48) |
| Model R2 | <.01 | .14 | <.01 | .11 | <.01 | .17 |
Note. IDU = injection drug use; Back in Jail = participants reported return to jail in 3-month follow-up [dichotomous; First Incarceration = participants first time incarcerated [dichotomous]; P&P = on parole or probation at the 3-month follow-up [dichotomous]; Baseline = reported behavior at baseline assessment. Model R2 = Nagelkerke Pseudo R2
Only participants with complete 3 month follow up data (n = 360)
Only participants with complete 3 month follow up data and reported sexual experience in the 3 month follow up period (n = 243)
Only participants with complete 3 month follow up data and past year injection drug use at baseline (n = 221)
p < .05;
p < .01;
p < .001
DISCUSSION
Despite risk behaviors among rural Appalachian women who use drugs, research is limited on HIV risk reduction interventions. This study provides an innovative examination of risk reduction interventions in rural jails to target HIV prevention education (NIDA Standard), as well as examining the additive effects of an individualized, tailored HIV risk reduction intervention (MI-HIV) for this vulnerable, underserved group of women.
During the year before entering jail, the majority of women in this study reported injecting drugs, sharing needles and other drug injection equipment, and engaging in drug use prior to sexual activity. Research has shown that women who engage in more HIV risk behaviors, such as injection drug use and risky sexual practices, are also more likely to cycle in and out of the criminal justice system (39). Studies have also shown that the community re-entry period following incarceration is a time of heightened risk for women to relapse to high-risk drug use, including IDU and casual sexual practices (40). Thus, consistent with the findings from the current study, the jail provides both an ideal venue and a critical opportunity to identify and intervene with women who are highest risk for HIV infection.
Considering limited health and behavioral health resources available in county jails, it was hypothesized that there would be significant reductions in community re-entry risky behaviors in both intervention conditions. This hypothesis was supported by significant reductions between baseline (behaviors before entering jail) and the 3-month community follow-up for each of the primary outcomes of interest including drug use, injection drug use, shared needles and drug injection equipment, and the use of drugs prior to or during sexual activity. These findings are consistent with other research on reduced risk behavior associated with HIV prevention interventions for women re-entering urban communities from prison (41, 42), jails (43), and community custody (24). With limited availability and access to critical prevention services in rural Appalachian communities, these findings support the importance of criminal justice settings for HIV prevention and education interventions.
The importance of HIV prevention in rural jails is further supported by intervention engagement. As an indicator of feasibility, more than 72% of participants randomized to MI-HIV attended at least 3 sessions, which is a completion rate similar to other motivational interventions (e.g., 44). In addition, the majority of women (91%) volunteered for testing, and of these women, about a third (37%) learned for the first time they were positive for the presence of HCV antibodies, suggesting that risk reduction could also be associated with testing. Although, in a preliminary analysis (not presented), there were no differences in primary outcome variables based on test results by intervention condition. This finding further underscores the importance of educating high-risk women during critical windows of opportunity like incarceration.
It was also expected that women who received the enhanced intervention (MI-HIV) would report greater reductions in high-risk drug use and risky sexual practices. Despite overall decreases, the MI-HIV intervention did not add significantly to the reduction of risk behaviors compared to the NIDA Standard alone. This finding differs from earlier research on the effectiveness of MI-HIV to reduce high-risk needle sharing (24), as well as other studies which have reported on the effectiveness of motivational interviewing in reducing HIV related risk behaviors (e.g., 25, 26). However, most of these studies examined motivational interviewing interventions compared to treatment as usual or a no treatment control group. In the current study, MI-HIV was examined as an enhancement to the NIDA Standard HIV educational intervention. Other studies have also reported a lack of differences between the NIDA Standard and an enhanced intervention (e.g., 21, 23). Taking into account the degree of risk of the women in the study and the limited amount of information they received about HIV, it is possible that the NIDA Standard was a robust comparison group, making it difficult to detect possible differences in the MI-HIV condition, which is an important consideration for future research.
This study has some limitations. Women were randomly selected and recruited for the study from three purposefully selected rural Appalachian area jails, which may limit generalizability to other substance-using women involved in the criminal justice system in urban areas. Also, findings may not be generalizable to other rural women since the target recruitment sites were in rural Appalachia. It is possible that women were concerned about confidentiality in the jail environment and it is not clear how this may have influenced self-report responses or intervention engagement. Baseline interviews and intervention sessions were completed face-to-face in private rooms in the three jails with no correctional officers or others present, and a Certificate of Confidentiality was obtained to increase protections. Finally, with regard to the intervention, it is noted that the lack of a true comparison group may lead to questions about the role of incarceration in reducing risk behaviors during community re-entry. However, the risk behaviors of rural women identified in previous work (e.g., 45) suggest that a no treatment/no education comparison group would raise ethical concerns for these highly vulnerable and underserved women.
Despite these limitations, this study presents an innovative approach to delivering HIV risk-reduction interventions for high-risk rural women drug users who may not have been be identified for services. Even with evidence on the effectiveness of interventions to reduce HIV risk among women, there has been limited effort to adapt these types of interventions in new contexts and underserved, high-risk populations (29, 30, 31). These study findings support the feasibility of delivering an education-focused HIV risk reduction intervention (NIDA Standard) and an enhanced, individualized intervention for risk reduction (MI-HIV) in rural jails to target high-risk rural women who use drugs. Although study findings did not support the additive value of a motivational enhancement to HIV prevention education and testing, study findings indicate that exposure to HIV risk reduction information and testing can be associated with reduction in high-risk injection drug use and needle sharing practices during community re-entry. Considering the public health implications of the opioid epidemic, particularly in rural communities, these findings support the need for increased access to treatment and prevention in criminal justice venues including community settings like probation and parole. Future research and policy initiatives should be targeted to expand these opportunities more broadly in real-world settings where high-risk drug users can be identified for intervention.
Funding:
This study was funded by the National Institute on Drug Abuse of the National Institutes of Health under Awards R01DA033866, K02DA035116, and T32DA035200 and the National Science Foundation under Award 1247392. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We would also like to recognize the cooperation and partnership with the Kentucky Department of Corrections and the local jails participating in this study.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Conflict of Interest: Dr. Staton declares that she has no conflict of interest. Mr. Strickland declares that he has no conflict of interest. Dr. Webster declares that he has no conflict of interest. Dr. Leukefeld declares that he has no conflict of interest. Dr. Oser declares that she has no conflict of interest. Dr. Pike declares that she has no conflict of interest.
Informed consent: Informed consent was obtained from all individual participants included in the study.
REFERENCES
- 1).Maxwell JC. The prescription drug epidemic in the United States: A perfect storm. Drug Alcohol Rev. 2011;30(3):264–270. [DOI] [PubMed] [Google Scholar]
- 2).Staton M, Ciciurkaite G, Havens JR, et al. Correlates of injection drug use among rural Appalachian women. J Rural Health. 2017;July 7:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Kentucky Department for Public Health (KDPH). State Health Assessment Report, 2017 Update. Frankfort, Kentucky: Cabinet for Health and Family Services, Kentucky Department for Public Health, 2017. [Google Scholar]
- 4).Strickland JC, Staton M, Leukefeld CG, Oser CB, Webster JM. Hepatitis C antibody reactivity among high-risk rural women: Opportunities for services and treatment in the criminal justice system. Int J Prison Health. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Staton-Tindall M, Webster JM, Oser CB, Havens JR, Leukefeld CG. Drug use, hepatitis C, and service availability: Perspectives of incarcerated rural women. Soc Work Public Health. 2015;30(4):385–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among person aged <30 years – Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. MMWR Morb Mortal Wkly Rep. 2015. May 8;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]
- 7).Van Handel M, Rose CE, Hallisey EJ, et al. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J Acquir Immune Defic Syndr. 2016;73(3):323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Frajzyngier V, Neaigus A, Gyarmathy VA, Miller M, Friedman SR. Gender differences in injection risk behaviors at the first injection episode. Drug Alcohol Depend. 2007;89(2–3):145–152. [DOI] [PubMed] [Google Scholar]
- 9).Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend. 2004;74(3):265–72. [DOI] [PubMed] [Google Scholar]
- 10).Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010;33(2):339–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Prithwish D, Cox J, Boivin J, Platt RW, Jolly AM. The importance of social networks in their association to drug equipment sharing among injection drug users: A review. Addiction. 2007;102(11):1730–1739. [DOI] [PubMed] [Google Scholar]
- 12).Staton M, Strickland JC, Tillson M, Leukefeld C, Webster M, Oser C. Partner relationships and high-risk practices among rural Appalachian women who inject. Womens Health Issues. 2017;September 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Staton M, Ciciurkaite G, Oser C, et al. Drug use and incarceration among rural Appalachian women: Findings from a jail sample. Subst Use Misuse. 2018;53(6):931–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Young AM, Havens JR. Transition from first illicit drug use to first injection drug use among rural Appalachian drug users: A cross sectional comparison and retrospective survival analysis. Addiction. 2012;107(3):587–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Friedman P Meeting the challenge of social service delivery in rural areas. Welfare Information Network. 2003. [cited July 31, 2017];7(2). Available from http://www.financeproject.org/publications/meetingthechallengeIN.htm. [Google Scholar]
- 16).Bronson J, Stroop J, Zimmer S, Berzofsky M. Drug use, dependence, and abuse among state prisoners and jail inmates, 2007–2009. US Department of Justice, Bureau of Justice Statistics; #NCJ250546. 2017. [cited September 28, 2017]. Available from https://www.bjs.gov/content/pub/pdf/dudaspji0709.pdf. [Google Scholar]
- 17).Coyle SL, Needle RH, Normand J. Outreach-Based HIV Prevention for Injecting Drug Users: A Review of Published Outcome Data. Public Health Rep. 1998;113(Suppl 1):19–30. [PMC free article] [PubMed] [Google Scholar]
- 18).Surratt HL, Inciardi JA. An Effective HIV Risk Reduction Protocol for Drug-Involved Women Sex Workers. J Prev Interv Community. 2010;38(2):118–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Wechsberg WM, Lam WKK, Zule WA, Bobashev G. Efficacy of a Woman-Focused Intervention to Reduce HIV Risk and Increase Self-Sufficiency among African American Crack Abusers. Am J Public Health. 2004;94(7):1165–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Cottler LB, Leukefeld CG, Hoffman J, et al. Effectiveness of HIV risk-reduction initiatives among out-of-treatment non-injection drug users. J Psychoactive Drugs. 1998;30(3):279–290. [DOI] [PubMed] [Google Scholar]
- 21).Booth R, Kwiatkowski C, Stephens R. Effectiveness of HIV/AIDS interventions on drug use and needle risk behaviors for out-of-treatment injection drug users. J Psychoactive Drugs. 1998;30(3):269–278. [DOI] [PubMed] [Google Scholar]
- 22).Martin SS, O’Connell DJ, Inciardi JA, Surratt HL, Beard RA. HIV/AIDS among probationers: An assessment of risk and results from a brief intervention. J Psychoactive Drugs. 2003;35(4):435–442. [DOI] [PubMed] [Google Scholar]
- 23).Dushay RA, Singer M, Weeks MR, Rohena L, Gruber R. Lowering HIV risk among ethnic minority drug users: Comparing culturally targeted intervention to a standard intervention. Am J Drug Alcohol Abuse. 2001;27(3):501–524. [DOI] [PubMed] [Google Scholar]
- 24).Weir BW, O’Brien K, Bard RS, et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: A randomized controlled trial of two motivational Interviewing-based interventions. AIDS Behav. 2009;13(3):509–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. J Consult Clinl Psychol. 1997;65(4): 531–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26).Jaworski BG, Carey MP. Effects of a brief, theory-based STD-prevention program for female college students. J Adolesc Health. 2001;29(6):417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).Carpenter KM, Stoner SA, Mikko AN, Dhanak LP, Parsons JT. Efficacy of a web-based intervention to reduce sexual risk in men who have sex with men. AIDS Behavior. 2010;14(3): 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28).Rutledge SE. Single-session motivational enhancement counseling to support change toward reduction of HIV transmission by HIV positive persons. Arch Sex Behav. 2007;36(2):313–319. [DOI] [PubMed] [Google Scholar]
- 29).McKleroy VS, Galbraith JS, Cummings B, et al. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18(4 Suppl A):59–73. [DOI] [PubMed] [Google Scholar]
- 30).Wenzel SL, Cederbaum JA, Song A, et al. Pilot test of an adapted, evidence-based HIV sexual risk reduction intervention for homeless women. Prev Sci. 2016;17(1):112–121. [DOI] [PubMed] [Google Scholar]
- 31).Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV Interventions. J Acquir Immune Defic Syndr. 2008;47(Suppl 1):S40–46. [DOI] [PubMed] [Google Scholar]
- 32).National Institute on Drug Abuse (NIDA). NIDA Modified-ASSIST. 2009. [cited August 20, 2017]. Available from http://www.drugabuse.gov/nidamed/screening/.
- 33).Dennis ML, Ives ML, White MK, Muck RD. The Strengthening Communities for Youth (SCY) initiative: a cluster analysis of the services received, their correlates and how they are associated with outcomes. J Psychoactive Drugs. 2008;40(1):3–16. [DOI] [PubMed] [Google Scholar]
- 34).Centers for Disease Control and Prevention (CDC). Recommendations for prevention and control of Hepatitis C virus (HCV) infection and HCV-related chronic disease. MMWR. 16 October 1998. [Google Scholar]
- 35).Lee SR, Yearwood GD, Guillon GB, et al. Evaluation of a rapid, point-of-care test device for the diagnosis of hepatitis C infection. J Clin Virol. 2010;48(1):15–17. [DOI] [PubMed] [Google Scholar]
- 36).Lee SR, Kardos KW, Schiff E, et al. Evaluation of a new, rapid test for detecting HCV infection, suitable for use with blood or oral fluid. J Virol Methods. 2011;172(1–2):27–31. [DOI] [PubMed] [Google Scholar]
- 37).Dickson MF, Staton-Tindall M, Smith KE, Leukefeld C, Webster JM, Oser CB. A Facebook follow-up strategy for rural drug-using women. J Rural Health. 2017;33(3):250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38).Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. [Google Scholar]
- 39).Herbst JH, Branscomb-Burgess O, Gelaude DJ, Seth P, Parker S, Fogel CI. Risk profiles of women experiencing initial and repeat incarcerations: Implications for prevention programs. AIDS Educ Prev. 2016;28(4):299–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40).Hearn LE, Whitehead NE, Khan MR, Latimer WW. Time since release from incarceration and HIV risk behaviors among women: the potential protective role of committed partners during re-entry. AIDS Behav. 2015;19(6):1070–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41).Knudsen HK, Staton-Tindall M, Oser CB, Havens JR, Leukefeld CG. Reducing risky relationships: a multi-site trial of a prison-based intervention for reducing HIV sexual risk behaviors among women with a history of drug use. AIDS Care. 2014;26(9):1071–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42).Leukefeld C, Havens J, Staton-Tindall M, et al. Risky relationships: targeting HIV prevention for women offenders. AIDS Educ Prev. 2012;24(4):339–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43).Scott CK, Dennis ML. The first 90 days following release from jail: findings from the Recovery Management Checkups for Women Offenders (RMCWO) experiment. Drug Alcohol Depend. 2012;125(1–2):110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44).Staton-Tindall M, Havens JR, Webster JM, Leukefeld C. METelemedicine: A pilot study with rural alcohol users on community supervision. Journal of Rural Health. 2014;30(4):422–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45).Staton-Tindall M, Duvall JL, Leukefeld C, Oser CB. Health, mental health, substance use, and service utilization among rural and urban incarcerated women. Womens Health Issues. 2007;17(4):183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]