Abstract
Introduction
Belimumab, an anti-B-lymphocyte-stimulator antibody, is approved for the treatment of active, autoantibody-positive systemic lupus erythematosus (SLE). Rituximab, a B cell-depleting anti-CD20 antibody, remains in the SLE treatment armamentarium despite failed trials in lupus nephritis and extrarenal lupus. These biologics, which operate through complementary mechanisms, might result in an enhanced depletion of circulating and tissue-resident autoreactive B lymphocytes when administered together. Thus, belimumab and rituximab combination may be a highly effective treatment of SLE. This study aims to evaluate and compare the efficacy, safety and tolerability of subcutaneous (SC) belimumab and a single cycle of rituximab in patients with SLE with belimumab alone.
Methods and analysis
BLISS-BELIEVE is a three-arm, randomised, double-blind, placebo-controlled, 104-week superiority study. Two hundred adults with SLE will be randomised 1:2:1 to arm A, belimumab SC 200 mg/week for 52 weeks plus placebo at weeks 4 and 6; arm B, belimumab SC 200 mg/week for 52 weeks plus rituximab 1000 mg at weeks 4 and 6; arm C, belimumab SC 200 mg/week plus standard of care for 104 weeks. The 52-week treatment period (arms A and B) is followed by a 52-week observational phase. The primary efficacy endpoint is the proportion of patients with disease control (SLE Disease Activity Index (SLEDAI)−2K≤2, without immunosuppressants and with a prednisone-equivalent dose of ≤5 mg/day) at week 52. Major secondary efficacy endpoints are the proportion of patients in clinical remission (defined as SLEDAI-2K=0, without immunosuppressants and corticosteroids) at week 64, and the proportion of patients with disease control at week 104. Safety endpoints include the incidence of adverse events (AEs), serious AEs and AEs of special interest.
Ethics and dissemination
Within 6 months of the study’s primary manuscript publication, anonymised individual participant data and study documents can be requested for further research from www.clinicalstudydatarequest.com.
Trial registration number
NCT03312907; Pre-results.
Keywords: clinical trials, rheumatology
Strengths and limitations of this study.
This study builds on the experience of randomised controlled trials of the biologics belimumab and rituximab used as single agents, as well as preclinical findings, case studies and open-label trials of belimumab and rituximab combination treatment.
The unique sequence of treatment administration and assessment of the clinically relevant outcomes of disease control and disease remission are novel features of this study.
BLISS-BELIEVE is the first randomised trial to carry out observations for 52 weeks after stopping belimumab treatment, allowing for the assessment of true disease remission and its durability.
BLISS-BELIEVE randomises patients to a third treatment arm of belimumab plus standard-of-care therapy to reflect current real-life practice.
The study is limited by a relatively small sample size, and thus has limited power to detect infrequent adverse events.
Introduction
Immune-mediated inflammatory diseases (IMIDs) share some common molecular pathways that lead to inflammation, which results from dysregulation of the normal immune response. Chronic inflammation in IMIDs is associated with progressive tissue damage as well as increased comorbidity and mortality. Systemic lupus erythematosus (SLE) and Sjögren’s syndrome are both prototypic antibody-dependent IMIDs.1 SLE is a chronic multisystem inflammatory autoimmune disease associated with impaired health-related quality of life.2 3 The ultimate goals of SLE treatment are disease remission, damage prevention (from both disease progression and prolonged use of medication) and normalisation of health-related quality of life.4 5 These goals are difficult to achieve in most patients owing to limitations in the efficacy of, and long-term toxicity associated with, conventional treatments for SLE, such as corticosteroids and immunosuppressants.6 7
Patients with SLE have elevated levels of circulating B-lymphocyte stimulator (BLyS), a member of the tumour necrosis factor ligand superfamily that promotes B cell activation and differentiation.8–10 Increased serum BLyS levels in patients with SLE are associated with disease activity, disease relapse and increased numbers of autoantibody-secreting plasma cells, linking BLyS to the pathogenesis of SLE.9 11 Belimumab, a recombinant immunoglobulin G1λ human monoclonal antibody, binds to and antagonises the biological activity of soluble BLyS.12 It has shown efficacy in patients with autoantibody-positive active SLE in multiple trials.13–16 Belimumab-treated patients also experienced fewer disease flares, and showed a reduction in steroid use and long-term organ damage accrual compared with patients receiving standard of care (SoC).13–17 While the efficacy of belimumab has been demonstrated in patients with SLE, a proportion of patients maintain a degree of disease activity despite belimumab treatment.13–16 Therefore, additional effective and well-tolerated treatment options are required to further improve overall disease control.
Rituximab is a B cell-depleting, anti-CD20 monoclonal antibody that showed promise in several open-label clinical studies,18–22 but failed to demonstrate efficacy in two randomised trials in SLE and lupus nephritis.23 24 In autoimmune diseases, rituximab treatment results in rapid and near-complete depletion of circulating CD20+ B cells; however, relatively high numbers of B cells persist in tissues, such as bone marrow, kidneys, synovium and salivary glands.25–29 In SLE, an increase in BLyS levels after rituximab treatment may contribute to survival and rebound of autoreactive B cells and subsequent disease flares,30 31 as demonstrated in several cohort studies.32–34 Consistent with these observations, reduced maturation of autoreactive B cells during B cell reconstitution was observed in mice treated with an agent that blocked B cell activating factor.35
Combining belimumab with rituximab therefore has a strong immunological rationale, as the drugs operate through complementary and perhaps synergistic mechanisms.36 Belimumab treatment results in the mobilisation of memory B cells from tissues despite an overall decrease in peripheral B cell levels.37 This phenomenon will render tissue-resident B cells more susceptible to depletion by rituximab. In addition, blocking the effects of high serum BLyS levels might have favourable quantitative and qualitative effects on B cell reconstitution after depletion.31 Synergistic or additive effects of such a combination have indeed been demonstrated in preclinical studies in lupus-prone mice. Improved tissue B cell subset depletion, a decrease in the levels of autoantibodies, reduced proteinuria and improved survival were observed with combination therapy compared with either treatment alone.38–40
This hypothesis is further supported by case reports in patients with SLE, lupus nephritis and Sjögren’s syndrome,41–45 and prompted the SynBioSe study, which showed significant clinical and immunological improvements from baseline in patients with refractory SLE who received rituximab and belimumab.46 Several clinical trials are currently investigating belimumab and rituximab combination therapy in primary Sjögren’s syndrome (NCT02631538), lupus nephritis (CALIBRATE; NCT02260934) and SLE (BEAT Lupus; ISRCTN47873003).
We hypothesised that durable low disease activity might be achieved in patients with active SLE by resetting the autoreactive humoral immune system. Therefore, we have designed the BLISS-BELIEVE study to examine whether combination treatment with belimumab and rituximab could induce a pre-defined state of disease control or disease remission, allowing the tapering of conventional SLE therapies. This study will employ a novel sequence of belimumab and rituximab combination therapy and investigate novel study endpoints, which could potentially shift the current paradigm of SLE treatment.
The objective of this study is to evaluate the efficacy, safety and tolerability of subcutaneous (SC) belimumab and a single cycle of rituximab administered in a combination regimen in adult patients with SLE compared with belimumab alone.
Methods and analysis
Study design
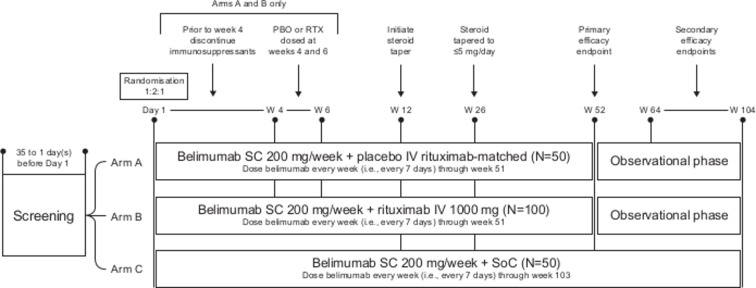
This is a phase III, multicentre, three-arm, randomised, double-blind, placebo-controlled, 104-week superiority study (BEL205646; NCT03312907). There will be a 52-week double-blind treatment period followed by a 52-week double-blind observational treatment-free follow-up period in arms A and B (to week 104) (figure 1). The study began recruitment in March 2018, with an estimated final completion in June 2021.
Figure 1.
Study design. IV, intravenous; PBO, placebo; RTX, rituximab; SC, subcutaneous; SoC, standard of care; W, week.
Study population
Detailed inclusion and exclusion criteria are listed in box 1. Briefly, patients must be ≥18 years of age, with a clinical diagnosis of SLE according to the American College of Rheumatology criteria, and an SLE Disease Activity Index (SLEDAI)-2K score ≥6 at screening. Patients with severe lupus nephritis or severe active central nervous system lupus will be excluded. Informed consent will be obtained from patients prior to the initiation of any study procedures or study-specific data collection.
Box 1. Patient inclusion and exclusion criteria.
Inclusion criteria
≥18 years of age
Clinical diagnosis of SLE according to the ACR criteria
Minimum screening SLEDAI-2K score ≥6
Unequivocally positive ANA and/or anti-dsDNA test results from two independent time points
Stable SLE treatment regimen
Female patients who are not pregnant, not breastfeeding, not of childbearing potential or follow contraceptive guidance
Exclusion criteria
Symptomatic herpes zoster within 3 months prior to screening
Active or latent TB, confirmed by medical history and examination, chest X-rays and TB testing: either a positive TST (defined as a skin induration ≥5 mm at 48–72 hours, regardless of BCG or other vaccination history), or a positive QuantiFERON-TB Gold test
Allergies to humanised monoclonal antibodies
Clinically significant multiple or severe drug allergies and/or history of hypersensitivity to belimumab and/or rituximab
Lymphoma, leukaemia, or any malignancy within the past 5 years
ALT >2 x ULN
Bilirubin >1.5 x ULN
IgA <10 mg/dL
IgG <250 mg/dL
Neutrophils <1.5×109
Unstable liver or biliary disease
Severe heart failure
QTc>450 msec or>480 ms in patients with bundle branch block
History of a major organ transplant
Clinical evidence of significant unstable or uncontrolled acute or chronic diseases not due to SLE
Acute or chronic infection requiring management
Severe lupus kidney disease
Severe active central nervous system lupus
Planned surgical procedure, laboratory abnormality or condition that makes the patient unsuitable for the study
Evidence of serious suicide risk
History of an anaphylaxis reaction to parenteral administration of contrast agents, human/murine protein, or monoclonal antibodies
Live vaccine(s) within 1 month prior to screening
Within 364 days of day 1, received certain biologics (belimumab, rituximab, abatacept, a B cell-targeted therapy, a biological investigational agent other than B cell-targeted therapy), or required three or more courses of systemic corticosteroids
Within 90 days of day 1, received anti-TNF therapy, interleukin-1 receptor antagonist, intravenous immunoglobulin, high-dose prednisone or equivalent, or plasmapheresis
Within 60 days of day 1, received a non-biological investigational agent, intravenous cyclophosphamide, a steroid injection
Positive HIV antibody test
Positive serology for hepatitis B or hepatitis C
Current or history (within 364 days of day 1) of drug/alcohol dependence
Sensitivity to any of the study treatments or components
Unable to administer belimumab by SC injection
ACR, American College of Rheumatology; ALT, alanine aminotransferase; ANA, anti-nuclear antibodies; BCG, Bacillus Calmette-Guerin; HIV, human immunodeficiency virus; IgA, immunoglobulin A; IgG, immunoglobulin G; QTc, corrected QT; SC, subcutaneous; SLE, systemic lupus erythematosus; SLEDAI-2K, SLE Disease Activity Index; TB, tuberculosis; TNF, tumour necrosis factor; TST, tuberculin skin test; ULN, upper limit of normal.
Randomisation
Patients will be randomised 1:2:1 to one of three treatment arms: belimumab plus placebo (arm A, control), belimumab plus rituximab (arm B, combination) or belimumab plus SoC (arm C, reference). At randomisation, patients will be stratified by their screening SLEDAI-2K score (≤9 vs ≥10), immunosuppressant use (immunosuppressant use vs no use) and corticosteroid dose (prednisone equivalent ≤10 mg/day vs >10 mg/day). Randomisation, and the first dose of belimumab, should be completed within 35 days of the initiation of screening.
Blinding
The study is double-blind with regards to whether participants are randomised to arm A or arm B. Randomisation to arm C will not be blinded. To minimise bias given that arm C is open-label, independent assessors blinded to treatment group will conduct the SLEDAI-2K assessments at selected visits for the primary and major secondary efficacy endpoints. Unblinded safety data will be reviewed regularly by an independent data monitoring committee.
Study treatments
Patients randomised to arm A (control) will receive belimumab SC 200 mg/week for 52 weeks with a cycle of intravenous placebo (rituximab-matched; dose 1 at week 4 and dose 2 at week 6). Patients randomised to arm B (combination) will receive belimumab SC 200 mg/week for 52 weeks with a cycle of rituximab intravenously (1000 mg doses given at week 4 and week 6). Patients randomised to arm C (reference) will receive belimumab SC 200 mg/week plus SoC, including immunosuppressants, for 104 weeks. Patients in arms A and B will be administered a premedication regimen 30 min before each placebo or rituximab infusion, consisting of methylprednisolone intravenously 100 mg or equivalent, an oral antihistamine and acetaminophen or equivalent (table 1).
Table 1.
Study treatment arms
| Treatment | Arm A (control) | Arm B (combination) | Arm C (reference) |
| Belimumab | Belimumab SC 200 mg/week for 52 weeks |
Belimumab SC 200 mg/week for 52 weeks |
Belimumab SC 200 mg/week plus SoC for 104 weeks |
| Rituximab or matched placebo | One cycle of placebo intravenously (rituximab-matched) at week 4 and week 6 | One cycle of rituximab intravenously 1000 mg at week 4 and week 6 | None |
| Premedication (30 min before each placebo or rituximab infusion) | Methylprednisolone intravenously 100 mg or equivalent, oral antihistamine, acetaminophen or equivalent | Methylprednisolone intravenously 100 mg or equivalent, oral antihistamine, acetaminophen or equivalent | None |
| Post week 52 therapy | Antimalarials, NSAIDs and/or corticosteroids with a prednisone equivalent dose of ≤5 mg/day |
Antimalarials, NSAIDs and/or corticosteroids with a prednisone equivalent dose of ≤5 mg/day |
Continue belimumab SC 200 mg/week plus SoC* |
*Patients in arm C are allowed to receive rescue therapy if, in the opinion of the investigator, they require additional treatment. This can include corticosteroids at >5 mg/day prednisone equivalent.
NSAIDs, non-steroidal anti-inflammatory drugs; SC, subcutaneous; SoC, standard of care.
After completing week 52, patients in arms A and B will enter into the 52-week treatment-free (defined as no active treatment with belimumab and/or rituximab), observational phase of the study (weeks 53 through 104). Patients in arm C will continue to receive belimumab SC and stable immunosuppressants during this phase. In addition, treatment with antimalarials, non-steroidal anti-inflammatory drugs and corticosteroids (prednisone equivalent ≤5 mg/day) is allowed in the observational phase in all three arms.
Patients considered treatment failures (patients in arm A or B who fail to respond adequately to study treatment, who do not meet the corticosteroid taper rules or tolerate immunosuppressant withdrawal at week 4, or who require additional therapy) will be encouraged to remain in the study to receive all safety and efficacy assessments through week 104. During this time (weeks 53–104), additional treatment may be given, if deemed of benefit by the investigator, to patients with responses that do not reach the predefined study criteria for disease control (as defined in the study endpoints), or subsequently experience increased disease activity. This treatment can include belimumab, corticosteroids, and/or immunosuppressants; additional treatment with rituximab will be permitted, but not encouraged.
Concomitant medications
Patients randomised to arms A and B who enter the study on immunosuppressants will discontinue immunosuppressants at or prior to the week 4 visit. Patients in arm C who enter the study on stable immunosuppressants may continue to receive them throughout the study. After the initial 12 weeks of study treatment, a protocol-specified corticosteroid taper will be initiated for all three arms (carried out under the direction of the investigator), with a target of reaching a prednisone equivalent dose of ≤5 mg/day by week 26. After week 26, if a patient’s average daily corticosteroid dose exceeds 5 mg/day prednisone equivalent, the patient will be declared a treatment failure. Antimalarials and non-steroidal anti-inflammatory drugs may be used throughout the study for all treatment arms.
Other investigational agents (or co-enrolment into another study of a different investigational agent), antitumour necrosis factor therapy, other biologics with effects on the immune system, immunoglobulin intravenously, cyclophosphamide intravenously and plasmapheresis are prohibited throughout the study.
Study endpoints
The primary efficacy endpoint is the proportion of patients with disease control at week 52, defined as a SLEDAI-2K score of ≤2, achieved without immunosuppressants and with a prednisone equivalent dose of ≤5 mg/day. The major secondary efficacy endpoints are the proportion of patients in clinical remission at week 64 (defined as a clinical SLEDAI-2K score of 0, allowing for serologies of anti-dsDNA and hypocomplementaemia and achieved without immunosuppressants and corticosteroids), and the proportion of patients with disease control at week 104 (defined as a SLEDAI-2K score of ≤2, achieved without immunosuppressants and with a prednisone-equivalent dose of ≤5 mg/day). Patient-reported outcome measures include change from baseline in Patient Global Assessment (PtGA), LupusQoL domain summary scores and Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue score, and proportion of patients with an improvement in FACIT-Fatigue score exceeding the minimal clinically-important difference. Safety endpoints include the incidence of adverse events (AEs), including serious AEs (SAEs) and AEs of special interest (AESI). The endpoints will be assessed using the measures listed in box 2.
Box 2. Study assessments.
Efficacy assessment
SLEDAI-2K, a clinical index for measuring SLE disease activity in the previous 10 days, at screening/baseline and at weeks 52, 64 and 104.
Safety assessment
Full physical examination, ECG, clinical safety laboratory assessments, neurological assessment, and suicidal risk monitoring (assessed via C-SSRS) at screening. Symptom-driven physical examination, vital signs, clinical safety laboratory assessments, neurological assessment, and suicidal risk monitoring at scheduled and unscheduled visits.
Laboratory tests
Anti-dsDNA/ANA, complement C3/C4, serum immunoglobulin (IgG, IgA, IgM), urine testing (urinalysis, spot urine protein), haematology and blood chemistry, pregnancy test: performed at screening and at each assessment visit. Autoantibody levels, including aCL, beta-2-glycoprotein, lupus anticoagulant, and extractable nuclear antigens, will be measured at day 1 and weeks 8, 26, 52, 60, 80 and 104.
B cell analyses
Pharmacokinetics
aCL, anticardiolipin; ANA, antinuclear antibodies; C, complement; C-SSRS, Columbia-Suicide Severity Rating Scale; ECG, electrocardiogram; Ig, immunoglobulin; SLE, systemic lupus erythematosus; SLEDAI, SLE Disease Activity Index.
Sample size calculation
Approximately 400 patients will be screened, with a goal of randomising at least 200 patients (50% screen failure rate). A target of 50 patients will be randomised in arms A and C, and 100 patients in arm B. This sample size provides at least 95% power (for the comparison of arm B to arm A at week 52) at a 5% level of significance, assuming the underlying response in the control arm is 10%, and the true population effect is ≥25% with treatment arm B (assumed response rate of 35%). For the primary endpoint, patients who drop out from the study will be included in the analysis as non-responders; thus, the assumed responder rates for arms A and B already account for the rate of patient dropout. However, to ensure adequate safety exposure in arm B, the sample size may be increased up to 300 patients if the dropout rate reaches 10% at the scheduled time point for receiving both doses of placebo or rituximab.
Based on limited clinical data with therapies including both belimumab and rituximab, opinions from external experts, and the rarity of remission or disease control seen in published studies, a rate of 35% of patients in arm B achieving a state of disease control is considered to be highly clinically significant in SLE care. A response rate of 10% at week 52 was assumed for arm A (control), based on historical data from three belimumab phase III trials. Assuming a 10% control responder rate and 50 patients in arm A and 100 patients in arm B, the minimum detectable effect at p<0.05 is a 12% improvement (ie, an observed improvement of 12% or more in arm B would give a p<0.05). A sample size sensitivity analysis was conducted on the primary endpoint to investigate the impact on power if the assumed underlying control response rate deviates from 10% or the treatment difference deviates from 25%.
Statistical analyses
Unless otherwise stated, all analyses will be performed on the intent-to-treat population. The key analyses will compare belimumab with or without a single cycle of rituximab (arm A vs arm B). Descriptive statistics will be used to compare the combination of belimumab with a single cycle of rituximab (arm B) versus belimumab with SoC (arm C). The primary and major secondary endpoints will be compared using a logistic regression model. The independent variables will include treatment group, baseline SLEDAI-2K score (≤9 vs ≥10), immunosuppressant use at baseline (immunosuppressant use vs no use), and baseline corticosteroid dose (prednisone equivalent ≤10 mg/day vs >10 mg/day). If any factor fails to converge it will be removed from the logistic model. If the model fails to converge (eg, owing to a small number of responders), the endpoints will be analysed using a Fisher’s exact test. Missing data are accounted for in the primary efficacy endpoint, as all patients will be classified as either a non-responder (including premature study discontinuation or treatment failure prior to week 52) or responder. Sensitivity analyses will be used to explore the impact of missing data and treatment failure imputation. Descriptive statistics will be used to summarise AEs, SAEs, AESI, changes in laboratory parameters, and immunogenicity.
Ethical considerations
This study will be conducted in accordance with consensus ethical principles derived from international guidelines, including the Declaration of Helsinki and Council for International Organisations of Medical Sciences International Ethical Guidelines, applicable International Conference on Harmonisation Good Clinical Practice Guidelines and applicable laws and regulations. SAEs will be reported by the investigator to the sponsor immediately, and no later than within 24 hours. Written informed consent will be obtained from all patients, who will be assigned a unique identifier; all patient records and data transferred to the sponsor will contain the identifier only.
Dissemination
Study information will be publicly available at www.clinicaltrials.gov, and the results of this trial (positive and negative) will be submitted for publication in relevant peer-reviewed publications and the key findings presented at national and international conferences. Within 6 months of the publication of the primary manuscript for this study, anonymised individual participant data, the annotated case report form, protocol, reporting and analysis plan, data set specifications, raw data set, analysis-ready data set and clinical study report will be available for research proposals approved by an independent review committee. Proposals should be submitted to www.clinicalstudydatarequest.com. A data access agreement will be required. This paper complies with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) recommendations for protocol reporting.47
Patient and public involvement
Patients and/or public were not involved in the development of this study.
Discussion
This study aims to explore the potential for synergy and to demonstrate greater efficacy of combination treatment with belimumab and rituximab compared with belimumab monotherapy in achieving low disease activity, disease remission, or clinical quiescence in patients with SLE. Although to date, combination biologics have not been widely used in other diseases, we think there is a strong immunological rationale to study belimumab and rituximab combination therapy in the context of SLE. The residual disease activity that many patients with SLE experience despite current therapies further justifies the exploration of this novel combination treatment. If this study confirms our hypothesis that combined belimumab and rituximab treatment has additional efficacy over standard belimumab care, then this may transform the current treatment paradigm, allowing patients with SLE to discontinue conventional, often toxic medications.
The unique sequence of administering belimumab and rituximab (which we believe will enhance B cell depletion), the use of belimumab SC and a larger sample size, differentiate the BLISS-BELIEVE study from BEAT Lupus (ISRCTN47873003),48 a similar belimumab and rituximab combination therapy, phase II trial in SLE that is currently recruiting patients in the UK. The sequence of treatment administration also differs from that used in the CALIBRATE trial in lupus nephritis (NCT02260934).49 In addition, BLISS-BELIEVE is one of the first trials of belimumab to carry out assessments for 52 weeks after stopping treatment, and investigate ambitious, clinically relevant outcomes of low disease activity or disease remission. The 52-week observational, treatment-free phase provides an opportunity to observe if a true disease remission occurs, and allows for the assessment of the durability of any such remission or low disease activity. In the treatment of SLE, it is important to balance clinical efficacy and therapy-related toxicity. The unique design of BLISS-BELIEVE will ensure this is assessed through the use of rigorous endpoints (such as clinical remission), and by enabling the termination of belimumab if toxicity is an issue.
The unique treatment schedules were selected according to a rationale based on the current evidence. In the 52-week treatment phase, belimumab SC 200 mg will be administered weekly as per the treatment regimen in the phase III study of belimumab SC, which demonstrated its safety and efficacy in patients with SLE.15 Rituximab is not approved for the treatment of patients with SLE, and no standard dosing regimen has been established. Based on previous trials of rituximab that showed a lack of efficacy, we deemed that a rituximab-only arm would fail to meet standards of equipoise. In the current study, rituximab dosing will follow one cycle of the approved dosing recommendation for rheumatoid arthritis, which is two doses of 1000 mg intravenously given 2 weeks apart. In a phase II/III trial, this rituximab regimen demonstrated rapid depletion of CD19-positive cells (<5 cells/µL) in the majority of patients with SLE.23 It is also the dosing regimen recommended in NHS England’s Interim Clinical Commissioning Policy Statement for rituximab use in patients with refractory SLE.50 Furthermore, belimumab and rituximab combination treatment has previously shown acceptable safety and significant clinical responses in patients with severe, refractory SLE.46
Separating the administration of belimumab and rituximab may allow for observation of safety events attributable to each treatment; however, owing to the relatively small sample size, the study will have limited power to detect less common AEs. With the consecutive administration regimen, the study allows investigation of the hypothesis that belimumab mobilises additional CD20+ B cells into the circulation, making them available for anti-CD20 treatment with rituximab. Therefore, we will be able to further establish whether more efficient depletion of autoreactive B cells, otherwise protected from cell death in the tissue niches, is achieved.37 We anticipate that there will be fewer autoreactive B cells appearing in the memory B cell compartment during the early phase of B cell reconstitution. However, we are aware that the controls for this analysis are historical, owing to the ethical considerations discussed above. B cell mobilisation will be evaluated by comparing baseline, pre-belimumab B cell levels with autoreactive B cells appearing in peripheral blood after belimumab treatment. The possible reappearance of autoreactive B cells following rituximab treatment will then be established by comparing B cells levels between the belimumab-only and belimumab and rituximab arms.
This study has some limitations. Because rituximab is not approved for the treatment of patients with SLE, a rituximab-only arm could not be included in the protocol. Therefore, some clinical and serological outcomes attributable to rituximab treatment will not be assessed. However, this study aims to explore whether belimumab treatment can be optimised by sequential treatment with rituximab, for which a rituximab-only arm is not required. Another limitation of the study design is that direct measurements of B cell depletion in tissue niches will not be performed. However, this measurement and a rituximab-only arm are being explored in a clinical trial of belimumab and rituximab combination therapy in primary Sjögren’s syndrome (NCT02631538), which follows a similar administration regimen. Another concern is that patients in study arms A and B will discontinue immunosuppressants from week 4, which might result in a higher than predicted treatment failure rate, due to flares occurring before belimumab and rituximab achieve therapeutic efficacy at week 12. However, the risk of disease flares to patients will be mitigated by methylprednisolone pretreatment and the option for investigators to adjust concomitant corticosteroid treatment as clinically necessary up to week 26. Although substantially different from previous belimumab trials, such as BLISS-76, in which more than half the patients continued on background immunosuppressive agents,12 this regimen will allow investigation of whether belimumab and rituximab combination therapy could result in an immunologically more favourable condition in some patients, thus enabling the tapering of conventional immunosuppressive drugs and possibly an immunosuppressant-free honeymoon. A positive outcome of BLISS-BELIEVE would further support the rationale to test this therapeutic strategy in Sjögren’s syndrome and other autoantibody-dependent IMIDs.
In conclusion, the BLISS-BELIEVE study is supported by strong scientific rationale from preclinical studies, case reports and open-label trials. Its pioneering and unique design will allow for a long-term observation of true clinical remission, assessment of the durability of such a remission state and assessment of any potential safety issues. The results of this study may support the rationale for combination therapy in other autoimmune conditions. BLISS-BELIEVE began recruitment in March 2018, with estimated study completion in June 2021.
Supplementary Material
Footnotes
Contributors: PPT initiated this study and has been involved in its design. YKOT, INB, RAF, RFvV, DG, JG, RBH, MO and PPT were involved in the development of the study protocol, preparation of the manuscript and its subsequent revisions and provided final approval of the version published. BD was involved in the preparation of the manuscript and its subsequent revisions, and provided final approval of the version published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This study (205646; NCT03312907) is being conducted and funded by GSK. Medical writing assistance was provided by Gosia Carless, PhD, of Fishawack Indicia Ltd, UK, funded by GSK.
Disclaimer: The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Competing interests: YKOT’s work is funded by the Netherlands Scientific Organisation and the Dutch Kidney Foundation (KJPB12.028 & 17OKG04). INB is a National Institute for Health Research (NIHR) Senior Investigator and is funded by Arthritis Research UK and the NIHR Manchester Biomedical Research Centre. INB has also received speaker’s bureau and advisory board grants from UCB, has participated in advisory boards and steering committees for AstraZeneca, is a member of Independent Data Safety Boards for Medimmune and Merck Serono, has received grants from Genzyme Sanofi and has participated in advisory boards for Eli Lilly. BD is an investigator on the CALIBRATE study, which is sponsored by National Institute of Allergy and Infectious Diseases. RAF has received grants and is a consultant for GSK and Genentech/Roche. RFvV has received grants and is a consultant for AbbVie, BMS, GSK, Pfizer and UCB, and is a consultant for Celgene, Biotest, Janssen, Lilly and Novartis. DG was an employee of GSK at the time of protocol development and holds shares in BMS. JG, RBH, MO (and her husband) and PPT are employees of GSK and hold shares in the company. RBH has a patent pending (patent number WO 2017050833 A1) related to this work.
Ethics approval: The protocol has been reviewed and approved by institutional review boards (IRB)/independent ethics committees (IEC). The sponsor will comply with country-specific regulatory requirements relating to safety reporting to the regulatory authority, IRB/IEC, and investigators.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Dörner T, Kinnman N, Tak PP. Targeting B cells in immune-mediated inflammatory disease: a comprehensive review of mechanisms of action and identification of biomarkers. Pharmacol Ther 2010;125:464–75. 10.1016/j.pharmthera.2010.01.001 [DOI] [PubMed] [Google Scholar]
- 2. D’Cruz DP, Khamashta MA, Hughes GRV. Systemic lupus erythematosus. The Lancet 2007;369:587–96. 10.1016/S0140-6736(07)60279-7 [DOI] [PubMed] [Google Scholar]
- 3. Lau CS, Mak A. The socioeconomic burden of SLE. Nat Rev Rheumatol 2009;5:400–4 https://www.nature.com/articles/nrrheum.2009.106#supplementary-information 10.1038/nrrheum.2009.106 [DOI] [PubMed] [Google Scholar]
- 4. Wilhelm TR, Magder LS, Petri M. Remission in systemic lupus erythematosus: durable remission is rare. Ann Rheum Dis 2017;76:547–53. 10.1136/annrheumdis-2016-209489 [DOI] [PubMed] [Google Scholar]
- 5. van Vollenhoven RF, Mosca M, Bertsias G, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis 2014;73:958–67. 10.1136/annrheumdis-2013-205139 [DOI] [PubMed] [Google Scholar]
- 6. Gladman DD, Urowitz MB, Rahman P, et al. Accrual of organ damage over time in patients with systemic lupus erythematosus. J Rheumatol 2003;30:1955–9. [PubMed] [Google Scholar]
- 7. Oglesby A, Shaul AJ, Pokora T, et al. Adverse event burden, resource use, and costs associated with immunosuppressant medications for the treatment of systemic lupus erythematosus: a systematic literature review. Int J Rheumatol 2013;2013:1–9. 10.1155/2013/347520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cheema GS, Roschke V, Hilbert DM, et al. Elevated serum B lymphocyte stimulator levels in patients with systemic immune-based rheumatic diseases. Arthritis Rheum 2001;44 1313–9. [DOI] [PubMed] [Google Scholar]
- 9. Petri M, Stohl W, Chatham W, et al. Association of plasma B lymphocyte stimulator levels and disease activity in systemic lupus erythematosus. Arthritis Rheum 2008;58:2453–9. 10.1002/art.23678 [DOI] [PubMed] [Google Scholar]
- 10. Zhang J, Roschke V, Baker KP, et al. Cutting edge: a role for B lymphocyte stimulator in systemic lupus erythematosus. J Immunol 2001;166:6–10. 10.4049/jimmunol.166.1.6 [DOI] [PubMed] [Google Scholar]
- 11. Roth DA, Thompson A, Tang Y, et al. Elevated BLyS levels in patients with systemic lupus erythematosus: Associated factors and responses to belimumab. Lupus 2016;25:346–54. 10.1177/0961203315604909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Baker KP, Edwards BM, Main SH, et al. Generation and characterization of LymphoStat-B, a human monoclonal antibody that antagonizes the bioactivities of B lymphocyte stimulator. Arthritis Rheum 2003;48:3253–65. 10.1002/art.11299 [DOI] [PubMed] [Google Scholar]
- 13. Furie R, Petri M, Zamani O, et al. A phase III, randomized, placebo-controlled study of belimumab, a monoclonal antibody that inhibits B lymphocyte stimulator, in patients with systemic lupus erythematosus. Arthritis Rheum 2011;63:3918–30. 10.1002/art.30613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Navarra SV, Guzmán RM, Gallacher AE, et al. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet 2011;377:721–31. 10.1016/S0140-6736(10)61354-2 [DOI] [PubMed] [Google Scholar]
- 15. Stohl W, Schwarting A, Okada M, et al. Efficacy and safety of subcutaneous belimumab in systemic lupus erythematosus: A fifty-two-week randomized, double-blind, placebo-controlled study. Arthritis Rheumatol 2017;69:1016–27. 10.1002/art.40049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang F, Bae SC, Bass D, et al. A pivotal phase III, randomised, placebo-controlled study of belimumab in patients with systemic lupus erythematosus located in China, Japan and South Korea. Ann Rheum Dis 2018;77:355–63. 10.1136/annrheumdis-2017-211631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bruce IN, Urowitz M, van Vollenhoven R, et al. Long-term organ damage accrual and safety in patients with SLE treated with belimumab plus standard of care. Lupus 2016;25:699–709. 10.1177/0961203315625119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Anolik JH, Barnard J, Cappione A, et al. Rituximab improves peripheral B cell abnormalities in human systemic lupus erythematosus. Arthritis Rheum 2004;50:3580–90. 10.1002/art.20592 [DOI] [PubMed] [Google Scholar]
- 19. Cambridge G, Leandro MJ, Teodorescu M, et al. B cell depletion therapy in systemic lupus erythematosus: effect on autoantibody and antimicrobial antibody profiles. Arthritis Rheum 2006;54:3612–22. 10.1002/art.22211 [DOI] [PubMed] [Google Scholar]
- 20. Leandro MJ, Cambridge G, Edwards JC, et al. B-cell depletion in the treatment of patients with systemic lupus erythematosus: a longitudinal analysis of 24 patients. Rheumatology 2005;44:1542–5. 10.1093/rheumatology/kei080 [DOI] [PubMed] [Google Scholar]
- 21. Looney RJ, Anolik JH, Campbell D, et al. B cell depletion as a novel treatment for systemic lupus erythematosus: a phase I/II dose-escalation trial of rituximab. Arthritis Rheum 2004;50:2580–9. 10.1002/art.20430 [DOI] [PubMed] [Google Scholar]
- 22. Smith KG, Jones RB, Burns SM, et al. Long-term comparison of rituximab treatment for refractory systemic lupus erythematosus and vasculitis: Remission, relapse, and re-treatment. Arthritis Rheum 2006;54:2970–82. 10.1002/art.22046 [DOI] [PubMed] [Google Scholar]
- 23. Merrill JT, Neuwelt CM, Wallace DJ, et al. Efficacy and safety of rituximab in moderately-to-severely active systemic lupus erythematosus: the randomized, double-blind, phase II/III systemic lupus erythematosus evaluation of rituximab trial. Arthritis Rheum 2010;62:222–33. 10.1002/art.27233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rovin BH, Furie R, Latinis K, et al. Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: the Lupus Nephritis Assessment with Rituximab study. Arthritis Rheum 2012;64:1215–26. 10.1002/art.34359 [DOI] [PubMed] [Google Scholar]
- 25. Pijpe J, Meijer JM, Bootsma H, et al. Clinical and histologic evidence of salivary gland restoration supports the efficacy of rituximab treatment in Sjögren’s syndrome. Arthritis Rheum 2009;60:3251–6. 10.1002/art.24903 [DOI] [PubMed] [Google Scholar]
- 26. Rehnberg M, Amu S, Tarkowski A, et al. Short- and long-term effects of anti-CD20 treatment on B cell ontogeny in bone marrow of patients with rheumatoid arthritis. Arthritis Res Ther 2009;11:R123 10.1186/ar2789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Teng YK, Levarht EW, Hashemi M, et al. Immunohistochemical analysis as a means to predict responsiveness to rituximab treatment. Arthritis Rheum 2007;56:3909–18. 10.1002/art.22967 [DOI] [PubMed] [Google Scholar]
- 28. Teng YK, Levarht EW, Toes RE, et al. Residual inflammation after rituximab treatment is associated with sustained synovial plasma cell infiltration and enhanced B cell repopulation. Ann Rheum Dis 2009;68:1011–6. 10.1136/ard.2008.092791 [DOI] [PubMed] [Google Scholar]
- 29. Thurlings RM, Vos K, Wijbrandts CA, et al. Synovial tissue response to rituximab: mechanism of action and identification of biomarkers of response. Ann Rheum Dis 2008;67:917–25. 10.1136/ard.2007.080960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cambridge G, Isenberg DA, Edwards JC, et al. B cell depletion therapy in systemic lupus erythematosus: relationships among serum B lymphocyte stimulator levels, autoantibody profile and clinical response. Ann Rheum Dis 2008;67:1011–6. 10.1136/ard.2007.079418 [DOI] [PubMed] [Google Scholar]
- 31. Carter LM, Isenberg DA, Ehrenstein MR. Elevated serum BAFF levels are associated with rising anti-double-stranded DNA antibody levels and disease flare following B cell depletion therapy in systemic lupus erythematosus. Arthritis Rheum 2013;65:2672–9. 10.1002/art.38074 [DOI] [PubMed] [Google Scholar]
- 32. Cambridge G, Stohl W, Leandro MJ, et al. Circulating levels of B lymphocyte stimulator in patients with rheumatoid arthritis following rituximab treatment: relationships with B cell depletion, circulating antibodies, and clinical relapse. Arthritis Rheum 2006;54:723–32. 10.1002/art.21650 [DOI] [PubMed] [Google Scholar]
- 33. Lavie F, Miceli-Richard C, Ittah M, et al. Increase of B cell-activating factor of the TNF family (BAFF) after rituximab treatment: insights into a new regulating system of BAFF production. Ann Rheum Dis 2007;66:700–2. 10.1136/ard.2006.060772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pollard RP, Abdulahad WH, Vissink A, et al. Serum levels of BAFF, but not APRIL, are increased after rituximab treatment in patients with primary Sjogren’s syndrome: data from a placebo-controlled clinical trial. Ann Rheum Dis 2013;72:146–8. 10.1136/annrheumdis-2012-202071 [DOI] [PubMed] [Google Scholar]
- 35. Kawabata D, Venkatesh J, Ramanujam M, et al. Enhanced selection of high affinity DNA-reactive B cells following cyclophosphamide treatment in mice. PLoS One 2010;5:e8418 10.1371/journal.pone.0008418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ehrenstein MR, Wing C. The BAFFling effects of rituximab in lupus: danger ahead? Nat Rev Rheumatol 2016;12:367–72. 10.1038/nrrheum.2016.18 [DOI] [PubMed] [Google Scholar]
- 37. Stohl W, Hiepe F, Latinis KM, et al. Belimumab reduces autoantibodies, normalizes low complement levels, and reduces select B cell populations in patients with systemic lupus erythematosus. Arthritis Rheum 2012;64:2328–37. 10.1002/art.34400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bekar KW, Owen T, Dunn R, et al. Prolonged effects of short-term anti-CD20 B cell depletion therapy in murine systemic lupus erythematosus. Arthritis Rheum 2010;62:2443–57. 10.1002/art.27515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gong Q, Ou Q, Ye S, et al. Importance of cellular microenvironment and circulatory dynamics in B cell immunotherapy. J Immunol 2005;174:817–26. 10.4049/jimmunol.174.2.817 [DOI] [PubMed] [Google Scholar]
- 40. Lin W, Seshasayee D, Lee WP, et al. Dual B cell immunotherapy is superior to individual anti-CD20 depletion or BAFF blockade in murine models of spontaneous or accelerated lupus. Arthritis Rheumatol 2015;67:215–24. 10.1002/art.38907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. De Vita S, Quartuccio L, Salvin S, et al. Sequential therapy with belimumab followed by rituximab in Sjögren’s syndrome associated with B-cell lymphoproliferation and overexpression of BAFF: evidence for long-term efficacy. Clin Exp Rheumatol 2014;32:490–4. [PubMed] [Google Scholar]
- 42. Gonzalez-Echavarri C, Ugarte A, Ruiz-Irastorza G. Rituximab-refractory lupus nephritis successfully treated with belimumab. Clin Exp Rheumatol 2016;34:355–6. [PubMed] [Google Scholar]
- 43. Gualtierotti R, Borghi MO, Gerosa M, et al. Successful sequential therapy with rituximab and belimumab in patients with active systemic lupus erythematosus: a case series. Clin Exp Rheumatol 2018;36. [PubMed] [Google Scholar]
- 44. Kraaij T, Huizinga TW, Rabelink TJ, et al. Belimumab after rituximab as maintenance therapy in lupus nephritis. Rheumatology 2014;53:2122–4. 10.1093/rheumatology/keu369 [DOI] [PubMed] [Google Scholar]
- 45. Simonetta F, Allali D, Roux-Lombard P, et al. Successful treatment of refractory lupus nephritis by the sequential use of rituximab and belimumab. Joint Bone Spine 2017;84:235–6. 10.1016/j.jbspin.2016.01.008 [DOI] [PubMed] [Google Scholar]
- 46. Kraaij TKS, de Rooij ENM, Daele PLV, et al. Synergetic B-Cell Immunomodulation with Rituximab and Belimumab Combination Treatment in Severe, Refractory SLE. Arthritis Rheumatol 2017;69. [Google Scholar]
- 47. Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. BEAT Lupus. https://beatlupusuk/.
- 49. CALIBRATE. About CALIBRATE. http://calibratestudy.org/about-calibrate#.Ww7HKbpFzDd
- 50. NHS. Interim clinical commissioning policy statement: Rituximab for the treatment of systemic lupus erythematosus in adults. 2013. https://wwwenglandnhsuk/wp-content/uploads/2013/10/a13-ps-apdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.