Introduction
The prevalence of nephrolithiasis has increased rapidly over the last 20 years.1,2 The greatest increase in incidence has been observed among females and adolescents, and also African-Americans.1,3 Kidney stone recurrence in pediatric patients was previously thought to be lower than adults, but recent studies have demonstrated the risk of recurrence is up to 50% within 5 years of initial stone presentation.4,5 This high risk of recurrence is due, in part, to the finding of abnormal urine chemistries in approximately 50% of pediatric patients with nephrolithiasis.6, 7 The earlier age of onset and high prevalence of metabolic abnormalities suggests that kidney stone disease in childhood may represent a more severe phenotype.
Accordingly, the European Association of Urology guidelines recommend metabolic evaluation (including a 24-hour urine collection) of all high risk patients, which includes pediatric patients.11 This evaluation is designed to reduce the risk of recurrence of what historically was considered an adult disease.8, 9,10 Indeed, completion of 24-hour urine collections has been associated with a lower risk of recurrence among children and adolescents.5 However, completion of 24-hour urine collections is extremely low in both the pediatric and adult populations, with only 12% of pediatric patients obtaining 24-hour urine analyses within 6 months of an emergency department visit.12,13 Prior studies in adults have reported that patients with family history of nephrolithiasis have a higher probability of completing 24-hour urine collections whereas African-American race is associated with lower adherence to completion.14 However, factors associated with completion of 24-hour urine collections among pediatric patients with nephrolithiasis are unknown.
Therefore, the aim of this study was to identify patient characteristics associated with completing a 24-hour urine analysis. We hypothesized that, similar to adult stone formers, characteristics of pediatric patients such as family history of nephrolithiasis would be associated with adherence to completing a 24-hour urine collection.
Materials and Methods
Study Design and Patient Population
We performed a retrospective cohort study of all patients diagnosed with kidney stone disease between 3–18 years of age who were evaluated and treated from May 2012 to May 2017 at the Children’s Hospital of Philadelphia (CHOP). CHOP is a large pediatric healthcare system that serves a regional, national, and international patient population. Patients were identified by searching the Kidney Stone Registry, a prospective database of all patients with nephrolithiasis treated at our institution since 2012 and maintained in Research Electronic Data Capture (REDCap).15 All patients with kidney or ureteral stones confirmed with ultrasound or CT were prospectively included in the database. Patients were included regardless of symptoms on diagnosis. For this study, we identified patient demographics, kidney stone specific history, laboratory results, and radiology results. Cost information and reason for not completing 24- hour urine was not routinely documented in the chart and thus were not available for analysis. This study was approved by the CHOP Institutional Review Board.
To increase the generalizability of the results, the only exclusion criteria for the primary analysis was age. To examine a purely pediatric population that was likely toilet trained, we included patients between 3 to 18 years of age. Age was used as a proxy since toilet training status was not consistently documented.
Outcome
The outcome was completion of at least one 24-hour urine collection after initial presentation with nephrolithiasis. As part of the clinical pathway developed at our institution’s Kidney Stone Center, a metabolic evaluation is discussed and ordered for all patients at the first visit after stone passage, surgical intervention, or diagnosis of non-obstructive renal stones.16 The clinical care pathway was developed to improve quality of care and consistency among all pediatric urologists or pediatric nephrologists who treat children with nephrolithiasis. A single 24-hour urine analysis is ordered for patients who are toilet trained with instructions to complete the urine collection prior to their next appointment. The treating physician counseled the patient and caregivers about the determinants of kidney stone disease and the recommended evaluation. Counseling was provided through a medical interpreter if English was not the primary language of the patient and/or caregiver. Educational pamphlets on nephrolithiasis and an order for a 24-hour urine collection were provided to the patients. The laboratory preferred by the patient’s insurance was used. These laboratories were Litholink, Quest, and Labcorp for over 99% of patients.
The patient completed the 24-hour urine collection at home with collection materials provided to the patient from the collection laboratories. After completion, the patient mailed the collection back to the laboratory. For first time stone formers regardless of symptoms upon diagnosis, 24-hour urine collections were obtained every six months for at least 2 years and then yearly until 24-hour urine if no recurrences developed. For recurrent stone formers, 24-hour urine collection was repeated every 6 months if abnormal urine chemistries persisted and then yearly for at least 3 years. All pediatric patients are seen in the clinic every 6 months with a renal bladder ultrasound and are accompanied by at least one adult family member or caregiver.
Covariates
Patient characteristics obtained from the Kidney Stone Registry included age at stone presentation, sex, race, body mass index (BMI) percentile, neurogenic bladder, medical comorbidities, and payer status. Stone-specific characteristics including symptomatic presentation (defined as abdominal pain, flank pain, and/or nausea/vomiting), history of spontaneous passage, prior surgical intervention, family history of nephrolithiasis, and length of follow up are recorded in the Registry and were also included in the analysis. Length of follow-up was defined as the date of initial evaluation to last follow up in Urology, Nephrology, or the Comprehensive Pediatric Kidney Stone Center. BMI percentile was determined using Centers for Disease Control and Prevention growth curves. Payer status was categorized into self-pay (without any form of insurance), public/government assistance (defined as any form of governmental insurance assistance such as Medicaid, Medicare, state assistance program, or Children’s Health Insurance Programs) and private insurance. Neurogenic bladder was defined as any condition that resulted in neurologic condition that resulted in abnormal bladder function (e.g. myelomeningocele).
Statistical Analysis
Differences in patient characteristics between patients who did and did not complete 24-hour urine collections were assessed by t-tests, Mann-Whitney U-tests, or chi-square tests as appropriate for the distribution and nature of the data. Cox proportional hazard regression models were fit to estimate the association between patient characteristics and completion of a 24-hour urine analysis. Patients were censored at completion of a 24-hour urine or last Urology or Nephrology follow-up. Regression models were built using manual backwards selection of covariates. Covariates assessed for inclusion in the models were age, sex, race, family history of nephrolithiasis, payer status, prior stone surgery, prior stone passage, multiple stone occurrences, and neurogenic bladder. We included in the final models all covariates with face validity (sex, age) and those that were associated with completion of 24-hour analyses on univariate analyses at a p-value <0.1.
The following sensitivity analyses were performed: 1) inclusion of the entire pediatric population, including those that were not toilet trained (newborn to 18 years of age); 2) inclusion of all patients (including both those <3 years of age and > 18 years of age) to reflect the entire population presented to our institution with nephrolithiasis; 3) exclusion of those with neurogenic bladder. Statistical analyses were performed using Stata version 13 (StataCorp, College Station, Texas). All tests were two-sided and a p-value < 0.05 was the threshold for statistical significance.
Results
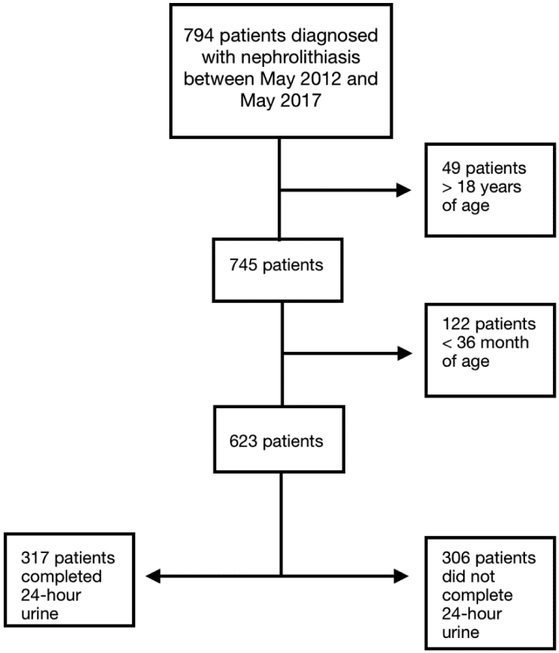
A total of 794 patients with a diagnosis of nephrolithiasis were identified, of which 49 patients >18 years old and 122 patients < 3 years old were excluded. This resulted in 623 patients in our primary analysis. Of these, 317 (50.9%) completed at least one 24-hr urine (Figure 1). The median age of the overall population was 14.4 years (IQR 10.5, 16.3). Patient characteristics and demographics are summarized in Table 1. The median follow-up was 153 days.
Figure 1.
- Flow chart of patient population
Table 1.
Patient Characteristics
| Patient characteristics | Obtained 24-hour urine (n=317) | Did not obtain 24-hour urine (n=306) |
|---|---|---|
| Median age in years (IQR) | 14.4 (11.0, 16.3) | 14.4 (10.5, 16.3) |
| BMI (SD) | 22.1 (6.7) | 20.9 (4.9) |
| Sex | ||
| Female | 161 (50.8%) | 157 (51.3%) |
| Male | 156 (49.2%) | 149 (48.7%) |
| Insurance | ||
| Medicaid/Medicare | 46 (14.5%) | 76 (24.8%) |
| Private | 240 (75.7%) | 165 (53.9%) |
| Self-pay/Unknown | 31 (9.8%) | 65 (21.2%) |
| Race | ||
| African-American | 19 (6.0%) | 47 (15.4%) |
| Caucasian | 245 (77.3%) | 190 (62.1%) |
| Other | 30 (9.5%) | 34 (11.1%) |
| Unknown | 33 (10.4%) | 35 (11.4%) |
| Family history of stones | ||
| Yes | 171 (53.9%) | 103 (33.7%) |
| No | 132 (41.6%) | 178 (58.2%) |
| Unknown | 14 (4.4%) | 25 (8.2%) |
| Stone history | ||
| Recurrent stone former | 104 (32.8%) | 33 (10.8%) |
| Medical Comorbidities | ||
| Yes | 115 (36.3%) | 157 (51.3%) |
Multivariable Cox models demonstrated that age at diagnosis (hazard ratio [HR] 1.03; 95% confidence interval [CI] 1.01–1.07), renal colic on presentation (HR 1.72; 95% CI 1.15–2.58), and family history of nephrolithiasis (HR 1.50; 95% CI 1.17–1.93) were associated with an increased likelihood of completion of a 24-hour urine. Public/government assistance insurance was associated with decreased likelihood of completing a 24-hour urine ((HR 0.68; 95% CI 0.48–0.96; Table 2).
Table 2.
Association between Patient Characteristics and Completion of 24-Hour Urine Analysis
| Patient Characteristics | Hazard Ratio | 95% Confidence Interval |
|---|---|---|
| Age (years) | 1.04 | 1.01–1.07 |
| Family history | 1.50 | 1.17–1.93 |
| Prior Passage of Nephrolithiasis | 1.07 | 0.84–1.37 |
| Renal Colic | 1.72 | 1.15–2.58 |
| Neurogenic bladder | 0.56 | 0.30–1.03 |
| Race (Caucasian Referent) | ||
| Asian | 1.42 | 0.51–3.93 |
| Hispanic | 1.42 | 0.91–2.20 |
| African American | 0.75 | 0.46–1.21 |
| Other/unknown | 1.25 | 0.86–1.81 |
| Insurance (Private Insurance Referent) | ||
| Medicaid/Medical Assistance | 0.68 | 0.48–0.96 |
| Self Pay | 1.04 | 0.33–3.32 |
| Unknown | 0.78 | 0.52–1.16 |
The results were similar in sensitivity analyses that included patients < 3 to 18 years old, with neurogenic bladder now associated with decreased likelihood of completing a 24-hour urine (HR 0.04; 95% CI 0.30–0.97; (Table 3). Inclusion of patients of all ages (<3 and >18 years of age; n=749) and excluding those with neurogenic bladder (n=538) yielded similar results (Table 3).
Table 3.
Sensitivity Analyses of Association between Patient Characteristics and Completion of 24-Hour Urine Analysis
| Patient Characteristics | Including Patients <3 and >18 Years of Age (n=794) | Excluding Those >18 Years of Age (n=745) | Excluding Those with Neurogenic Bladder (n=538) |
|---|---|---|---|
| Age (years) | 1.06 (1.03–1.09) | 1.06 (1.03–1.09) | 1.04 (1.00–1.07) |
| Family history | 1.54 (1.21–1.96) | 1.55 (1.21–1.98) | 1.47 (1.14–1.89) |
| Prior Passage of Nephrolithiasis | 1.54 (1.21–1.96) | 1.08 (0.84–1.37) | 1.08 (0.84–1.39) |
| Renal Colic | 1.82 (1.24–2.68) | 1.78 (1.19–2.65) | 1.69 (1.10–2.58) |
| Neurogenic bladder | 0.47 (0.26–0.83) | 0.54 (0.30–0.97) | --- |
| Race (Caucasian Referent) | |||
| Asian | 1.10 (0.40–3.01) | 1.14 (0.42–3.14) | 1.33 (0.48–3.69) |
| Hispanic | 1.40 (0.91–2.15) | 1.42 (0.92–2.19) | 1.27 (0.78–2.07) |
| African American | 0.67 (0.41–1.07) | 0.73 (0.46–1.17) | 0.77 (0.48–1.26) |
| Other/unknown | 1.21 (0.85–1.73) | 1.20 (0.83–1.73) | 1.27 (0.87–1.85) |
| Insurance (Private Insurance Referent) | |||
| Medicaid/Medical Assistance | 0.76 (0.55–1.05) | 0.75 (0.54–1.04) | 0.72 (0.51–1.03) |
| Self Pay | 1.25 (0.45–3.46) | 1.23 (0.44–3.39) | 1.33 (0.42–4.28) |
| Unknown | 0.87 (0.61–1.25) | 0.80 (0.54–1.17) | 0.76 (0.50–1.15) |
Discussion
In this study, we identified characteristics associated with completion of 24-hour urine analyses among nearly 800 pediatric patients evaluated and treated for nephrolithiasis over 5 years. Approximately 50% of our study population obtained a 24-hour urine, which is markedly higher than adherence reported previously in the United States, but far lower than ideal considering that completion of 24-hour urine collections has been associated with a lower risk of recurrence.12,13 Adjusting for length of follow up, we found that age on presentation, renal colic on presentation, and those with family history of stones were associated with increased probability of completion of 24-hour urine analyses. On the other hand, public/government assistance was associated with decreased probability of completing a 24-hour urine. These results suggest that patients who have had a painful experience (e.g. renal colic) or those with better understanding of the disease (family history, older age) might be more likely to adhere to completing a metabolic evaluation. Urine collections in younger patients could also be more challenging and difficult, which could contribute to the lower completion rate in younger patients. Conversely, we also found that those with governmental insurance may be vulnerable populations who could potentially benefit from strategies designed to improve adherence.
The clinical care pathway for outpatient management of nephrolithiasis at our institution is based on European Association of Urology guidelines, which recommend obtaining a metabolic workup for all pediatric stone formers.11, 16 To the best of our knowledge, this study is the first to report characteristics associated with completion of 24-hour urine analyses in a pediatric population. Ellison et al. found that that only 12% of commercially insured pediatric patients completed a metabolic work-up within 6 months of presenting to the emergency department.12 However, this prior study could not identify factors associated with adherence due to the nature of the claims data. In this study, we identified factors that were associated with completing 24-hour urine studies.
We found that patients who had renal colic was more likely to complete a 24-hour urine analysis than those who had asymptomatic, non-obstructive stones that may have been detected incidentally. This finding is important because regardless of symptoms, kidney stone disease is associated with an increased risk of fracture among children and adults, and an increased risk of hypertension, chronic kidney disease, and heart disease among adults.17,18,19,20 In addition, asymptomatic stones can grow and new stones can form, which represents a metabolically active disease. We also found that those with public/government insurance were less likely to adhere to ordered evaluations. These results are consistent with studies of other pediatric diseases such as asthma that have reported that patients with public/government assistance have lower adherence to therapy.21 This could be a result of various barriers to care often confronted by this population, such as cost or literacy. Patients who are economically disadvantaged, from different racial or ethnic minorities, or who have chronic comorbidities may represent vulnerable populations at risk for healthcare disparities that result in poor health outcomes.22,23 Consequently, our results suggest that efforts to increase adherence to completing 24 hour urine collections among patients with asymptomatic stones and vulnerable populations is particularly important in order to identify the primary modifiable determinants of the disease, slow progression, and reduce the risk of recurrence.
The results were generally unchanged in sensitivity analyses, demonstrating the robustness of the findings to different age groups and functional status. However, neurogenic bladder were associated with a lower likelihood of obtaining a 24-hour urine collection when patients from birth to 18 years were included. It is likely that coordination of the various components of medical care, such as obtaining 24-hour urine collections, pose a greater challenge in younger patients and greater dependence on caregivers. Consequently, because of the potential increased complexity and higher incidence of nephrolithiasis secondary to various physiologic changes and urinary stasis, we performed a sub-analysis excluding patients with neurogenic bladder.24,25 The results were similar to our primary analysis. These results support efforts to increase adherence to obtaining 24-hour urine among patients with neurogenic bladder, who are at particularly high risk for stone recurrence.24
This study should be interpreted with respect to its limitations. Our study included data from a single pediatric healthcare system, which may not be generalizable to other healthcare systems. However, our institution cares for a patient population of 1.45 million patients drawn from a large geographic region and also national and international referrals, and reflects the typical population of pediatric patients with nephrolithiasis. Future comparisons of prospectively collected data from different regions and different practice settings would validate these results and potentially identify other unique characteristics associated with adherence. Second, the validity of our study relied heavily on the accuracy and reliability of clinical documentation by providers. Misclassification of patient characteristics is possible, but unlikely, due to the utilization of structured data fields in the electronic health record for patients with stones. Third, we were not able to analyze the cost of 24-hour urines as these data were not available. Multiple factors would affect cost such as patient co-pays, deductibles and the preferred laboratory for various types of insurance. In addition, each insurance company administers numerous plans, each of which have different co-pays and deductibles. Each component could have an impact on patient’s completion of 24-hour urine and many of these could not be ascertained without detailed family-level information on health care expenditures. For instance, a patient who has not met their deductible may look at the test very differently from someone who has met the deductible. Future studies that account for cost would build upon our findings. Finally, as an observational study, causality cannot be inferred.
Conclusions
We identified various facilitators and barriers to obtaining a 24-hour urine. Understanding these factors can aid in the development of strategies to increase adherence to pathways aimed to reduce stone recurrence.
Acknowledgement:
Dr. Diana Bowen is currently an Attending Physician of Pediatric Urology at Ann and Robert H. Lurie Children’s Hospital of Chicago and an Assistant Professor of Urology at Northwestern University Feinberg School of Medicine, however, all work pertaining to this project was completed while she was a Pediatric Urology Fellow at Children’s Hospital of Philadelphia.
Footnotes
Declaration of interest: None
References
- 1.Tasian GE, Ross ME, Song L, et al. Annual Incidence of Nephrolithiasis among Children and Adults in South Carolina from 1997 to 2012. Clin J Am Soc Nephrol. 2016;11(3):488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Routh JC, Graham DA, Nelson CP. Epidemiological trends in pediatric urolithiasis at United States freestanding pediatric hospitals. J Urol. 2010;184(3):1100. [DOI] [PubMed] [Google Scholar]
- 3.Dwyer ME, Krambeck AE, Bergstralh EJ. Temporal Trends in Incidence of Kidney Stone AMong Children: A 25-Year Population Based Study. J Urol. 2012; 188 (1): 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lao M, Kogan BA, White MD, et al. High recurrence rate at 5-year follow up in children after upper urinary tract stone surgery. J Urol. 2014;191(2):440. [DOI] [PubMed] [Google Scholar]
- 5.Tasian GE, Kabarriti AE, Kalmus A, et al. Kidney Stone Recurrence amodng Children and Adolescents. J Urol. 2017;197(1):246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Milliner DS, Murphy ME Urolithiasis in pediatric patients. Mayo Clin Proc. 1993;68:241. [DOI] [PubMed] [Google Scholar]
- 7.Coward RJ, Peters CJ, Duffy PG Epidemiology of paediatric renal stone disease in the UK. Arch Dis Child. 2003;88(11):962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bush NC, Xu L, Brown BJ, Holzer MS, et al. Hospitalizations for pediatric stone disease in United States, 2002–2007. J Urol. 2010;183(3):1151. [DOI] [PubMed] [Google Scholar]
- 9.VanDervoort K, Wiesen J, Frank R, et al. Urolithiasis in pediatric patients: A single center study of incidence, clinical presentation and outcome. J Urol. 2007;177:2300. [DOI] [PubMed] [Google Scholar]
- 10.Dangle P, Ayyash O, Shaikh H, et al. Predicting Spontaneous Stone Passage in Prepubertal Children: A Single Institution Cohort. J Endourol. 2016;30(9):945. [DOI] [PubMed] [Google Scholar]
- 11.Turk C, Petrik A, Sarica K. EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. Eur Urol. 2016; 69(3):468. [DOI] [PubMed] [Google Scholar]
- 12.Ellison JS, Kaufman SR, Kraft KH, et al. Underuse of 24-hour urine collection among children with incident urinary stones: a quality-of-care concern?. Urology. 2014;84(2):457. [DOI] [PubMed] [Google Scholar]
- 13.Milose JC, Kaufman SR, Hollenbeck BK, et al. Prevalence of 24-hour urine collection in high risk stone formers. J Urol. 2014;191(2):376. [DOI] [PubMed] [Google Scholar]
- 14.Ghiraldi EM, Reddy M, Li T, et al. Factors Associated with Compliance in Submitting 24-Hour Urine Collections in an Underserved Community. J Endourol. 2017;31(S1):S64. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform. 2009;42(2):377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tasian G, Copelovitch L, Plachter N, et al. (12 Aug. 2014) “Nephrolithiasis Clinical Pathway - Outpatient Specialty Care.”, Retrieved on April 30 2018 fromThe Children’s Hospital of Philadelphia website, http://www.chop.edu/clinical-pathway/nephrolithiasis-outpatient-specialty-care-clinical-pathway.
- 17.Denburg MR, Leonard MB, Haynes K, et al. Risk of fracture in urolithiasis: a population-based cohort study using the health improvement network. Clin J Am Soc Nephrol. 2014;9(12):2133–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Denburg MR, Jemielita TO, Tasian GE, et al. Assessing the risk of incident hypertension and chronic kidney disease after exposure to shock wave lithotripsy and ureteroscopy. Kidney Int. 2016;89(1):185–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alexander RT, Hemmelgarn BR, Wiebe N, et al. Kidney stones and cardiovascular events: a cohort study. Clin J Am Soc Nephrol. 2014;9(3):506–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferraro PM, Taylor EN, Eisner BH, et al. History of kidney stones and the risk of coronary heart disease. JAMA. 2013;310(4):408–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang J, Freed GL, Prosser LA, et al. Comparisons of health care utilization outcomes in children with asthma enrolled in private insurance plans versus medicaid. J Pediatr Health Care. 2014;28(1):71. [DOI] [PubMed] [Google Scholar]
- 22.Aday L Health Status of Vulnerable Populations. Annu. Rev. Public Health 1994; 15:487. [DOI] [PubMed] [Google Scholar]
- 23.Shi L, Stevens G. Vulnerability and Unmet Health Care Needs: The Influence of Multiple Risk Factors. J Gen Intern Med. 2005; 20(2): 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raj GV, Bennett RT, Preminger GM, et al. The incidence of nephrolithiasis in patients with spinal neural tube defects. J Urol. 1999;162(3 Pt 2):1238. [DOI] [PubMed] [Google Scholar]
- 25.Welk B, Fuller A, Razvi H, Denstedt J. Renal stone disease in spinal-cord-injured patients. J Endourol. 2012;26(8):954–9. [DOI] [PubMed] [Google Scholar]