Abstract
Introduction:
Physical activity guidelines recommend minimum thresholds. This study sought to identify evidence-based thresholds to maintain disability-free status over 4 years among adults with lower extremity joint symptoms.
Methods:
Prospective multisite Osteoarthritis Initiative accelerometer monitoring cohort data from September 2008 through December 2014 were analyzed. Adults (n=1,564) aged ≥49 years at elevated disability risk because of lower extremity joint symptoms were analyzed for biennial assessments of disability-free status from gait speed ≥1 meter/second (mobility disability free) and self-report of no limitations in activities of daily living (activities of daily living disability free). Classification tree analyses conducted in 2017–2018 identified optimal thresholds across candidate activity intensities (sedentary, light, moderate-vigorous, total light and moderate-vigorous activity, and moderate-vigorous accrued in bouts lasting ≥10 minutes).
Results:
Minimal thresholds of 56 and 55 moderate-vigorous minutes/week best predicted disability-free status over 4 years from mobility and activities of daily living disability, respectively across the candidate measures. Thresholds were consistent across sex, BMI, age, and knee osteoarthritis presence. Mobility disability onset was one eighth as frequent (3% vs 24%, RR=0.14, 95% CI=0.09, 0.20) and activities of daily living disability onset was almost half (12% vs 23%, RR= 0.55, 95% CI=0.44, 0.70) among people above versus below the minimum threshold.
Conclusions:
Attaining an evidence-based threshold of approximately 1-hour moderate-vigorous activity/week significantly increased the likelihood of maintaining disability-free status over 4 years. This minimum threshold tied to maintaining independent living abilities has value as an intermediate goal to motivate adults to take action towards the many health benefits of a physically active lifestyle.
INTRODUCTION
Disability is costly to society and to the individual. Older adults who lose independence in mobility or in ability to perform the necessary activities of daily living (ADL) are less likely to remain in the community and are at elevated risk of death.1–3 A leading cause of disability is knee and hip joint conditions, which is globally ranked as the 11th highest contributor4 to disability.
Physical activity is effective to prevent disability and improve health outcomes in adults, including those with joint conditions.5–8 International9 and government10 health agencies recommend at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity for adults throughout the week. Yet a large portion of adults fail to attain these aerobic recommendations. Approximately half of U.S. adults11 in the general population do less activity than recommended. But among adults with lower extremity joint conditions, a group at elevated risk for developing disability, as many as four in five do not attain recommended thresholds.12 The effectiveness of increasing physical activity to reduce disability onset risk is established from RCTs.6,13 Prospective studies also indicate greater time being sedentary increased the risk for disability onset.14 Physical activity intensities related to sedentary, moderate-vigorous (MV), light, and MV accrued in bouts lasting 10 minutes or more, have demonstrated relationships with ADL disability and mobility disability.14–16 Newer research finds health benefits from different amounts of activity.17,18 But not established from these studies is a minimum physical activity threshold (i.e., time and intensity) or maximum sedentary time related to maintaining independence in the community. This information is central to inform future physical activity recommendations.
The study objective is to systematically evaluate physical activity and sedentary time to identify the strongest evidence-based threshold related to maintaining disability-free status over 4 years. Separate thresholds are investigated related to mobility disability based on gait speed testing and disability ascertained from self-reported ADL limitations. For this purpose, a machine learning approach using classification decision trees was employed to systematically identify the optimal predictor and the optimal threshold of that measure to predict disability-free status. The question is examined among older adults with lower extremity joint symptoms because these people represent a large population at elevated risk for developing disability19,20 for whom evidence-based physical activity advice could positively alter their health trajectory.
METHODS
Study Population
Participants in this prospective multi-site cohort study of community-dwelling older adults were at elevated risk for disability due to lower extremity joint symptoms. Baseline occurred September 2008 to December 2010 with follow-up September 2010 to December 2014.
Participants from the Osteoarthritis Initiative (OAI) enrolled in an accelerometer substudy (2008 to 2010) included 2,127 individuals.12 The parent OAI prospective study enrolled 4,796 participants aged 45–79 years with or at high risk for developing knee osteoarthritis (OA), a major disability risk factor. Included were adults with radiographic knee OA in one or both knees or at high risk based on frequent knee symptoms without radiographic OA, or two or more eligibility risk factors (e.g., age, high BMI, prior knee injury, knee surgery, family history of total knee replacement for OA, Heberden’s nodes, and repetitive knee bending).21 OAI enrollment (2004 to 2006) and biennial follow-up visits occurred at four clinical sites (Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island). OAI eligibility criteria are described in detail elsewhere.22 Each participant provided written informed consent.
This study examined the 1,862 participants from the OAI accelerometer monitoring study reporting lower extremity (hip, knee, ankle, foot) joint symptoms (pain, aching, or stiffness) who were free at baseline of mobility and ADL disability.12 Ankle, foot, and knee questions solicited symptoms over the past 30 days; hip questions solicited symptoms over the past 12 months. The analysis sample was limited to 1,700 participants with valid baseline accelerometer monitoring (i.e., ≥4 days showing evidence >10 hours accelerometer wear). Loss to follow-up was minimal; >92% (1,564/1,700) of this cohort participated in a 4-year follow-up clinic visit (2012–2014) providing subsequent disability status from 1,370 people free of baseline mobility disability and 1,460 people free of ADL baseline disability (Appendix Figure 1).
Measures
Disability-free status between baseline and 4-year follow-up was ascertained from biennial assessments. Mobility disability-free status was identified by gait speed ≥1 meter/second23,24 from a 20-meter walk test. ADL disability-free status was identified from the report of no limitations in performing basic ADL tasks: walking across a room, dressing, bathing, eating, using the toilet, and bed transfer.25 If a specific ADL task response was missing (2%, n=35), information was imputed from a parallel item from the Western Ontario questionnaire.26 Sensitivity assessments omitting inferred task limitations yielded almost identical results.
Physical activity was monitored using a uniaxial accelerometer.27 Trained research personnel gave uniform instructions to wear the accelerometer for 7 consecutive days on a belt at the natural waistline in line with the right axilla upon rising in the morning until retiring for sleep, except during water activities. Daily logged data on water and cycling activities, which may not be fully captured by accelerometers, showed such activity was negligible (IQR, 0 to 0 minutes/week).
Accelerometer data were analytically filtered using validated methodology.28 National Cancer Institute thresholds were applied to identify sedentary (<100 counts/minute), non-sedentary (≥100 counts/minute) activity, light (100–2,019 counts/minute), and MV (≥2,020 counts/minute) activity.29 Weekly activity minutes were determined for sedentary, light, total MV activity (sum of all MV minutes), MV activity accumulated in bouts lasting ≥10 minutes (MV-bout), and total physical activity (sum of all light and MV minutes); for individuals with 4 to 6 valid days of monitoring, weekly activity minutes were estimated as seven times their average daily average.
Demographic factors included age and sex. BMI was calculated from measured height and weight (weight /height2 [kg/m2]). If baseline BMI was missing (0.1%, n=2), the most recent annual assessment was used as a proxy. Knee OA was identified by a Kellgren–Lawrence grade of two or greater for at least one knee assessed from “fixed-flexion” knee radiography images.30
Statistical Analysis
The area under the receiver operating characteristic curve (AUC) to predict disability-free status was calculated for each candidate physical activity/sedentary measure. A receiver operating curve is graphically represented by the fraction of true positives (sensitivity) of the measure plotted against the fraction of false positives (i.e., 1–specificity) in relation to the outcome.31 AUC values of the measures were compared using Delong, Delong, and Clarke–Pearson testing.32
Optimal thresholds to predict disability-free status were identified using classification and regression tree (CART) methodology.33 Optimal thresholds were separately investigated to predict mobility disability-free and ADL disability-free outcomes. All physical activity/sedentary measures were entered as predictors. Classification tree analysis identified the predictor and threshold of the selected predictor with the strongest relationship to disability-free status using minimum classification error criterion33 from cross-validation models pruned within one standard prediction error.34 Analyses used Salford Predictive Modeler software, version 8.0.35 Recognizing systematic differences between people with and without follow-up outcomes could influence these findings and weighted sensitivity analyses were conducted.36 Identical thresholds to unweighted analyses resulted. Sensitivity analyses evaluated the stability of thresholds across age, sex, BMI, and knee OA presence. Each factor was entered into a classification tree analysis in addition to physical activity/sedentary measures to predict disability-free status. RRs and associated CIs were estimated as unadjusted and adjusted (controlling for age, sex, BMI, presence of knee OA) using SAS software, version 9.4. Statistical testing was conducted at two-sided 5% significance level. Statistical analyses were conducted in 2017–2018.
RESULTS
This cohort of participants with lower extremity joint symptoms who were free of baseline disability (n=1,564) ranged in age from 49 to 83 years at baseline, were primarily female (56%), and a substantial percentage were obese (38%, BMI ≥30). The most common lower extremity symptoms reported were knee symptoms (93%, of whom 62% had radiographic disease) followed by hip (61%), foot (12%), and ankle symptoms (11%). Concomitant hip and knee symptoms were reported by 54% of this sample.
Table 1 shows this cohort spent almost twice the time each week being sedentary (median=69 hours) as in physical activity (median=35 hours). The vast majority of their physical activity time comprises light-intensity activity (median=32 hours). These patterns of physical activity and sedentary behavior held for both males and females (not shown).
Table 1.
Median Physical Activity/Sedentary Measures From Adults Having Lower Extremity Joint Symptoms by 4-Year Disability Status
| Overall (n=1,564a) | Mobility disability status over 4 years (n=1,370) | Activity of daily living (ADL) disability status over 4 years (n=1,460) | |||
|---|---|---|---|---|---|
| Physical activity/sedentary measures in minutes/week | Median (Q1,b Q3c) | Mobility disability (n=147) Median (Q1, Q3) | Mobility disability free (n=1,223) Median (Q1, Q3) | ADL disability (n=238) Median (Q1, Q3) | ADL free (n=1,222) Median (Q1, Q3) |
| Moderate-vigorous (MV) | 81 (30, 91) | 19 (7, 48) | 106 (44, 214) | 52 (18, 138) | 93 (33, 206) |
| MV activity accrued in bouts ≥10 minutes | 13 (0, 79) | 0 (0, 0) | 22 (0, 94) | 0 (0, 44) | 19 (0, 90) |
| Light physical activity | 1,949 (1,613, 2,317) | 1,686 (1,383, 2,050) | 1,984 (1,677, 2,361) | 1,818 (1,456, 2,160) | 1,966 (1,639, 2,331) |
| Total light + MV physical activity | 2,081 (1,724, 2,483) | 1,710 (1,402, 2,107) | 2,140 (1,814, 2,538) | 1,901 (1,528, 2,264) | 2,119 (1,762, 2,496) |
| Sedentary behavior | 4,131 (3,716, 4,543) | 4,250 (3,854, 4,721) | 4,120 (3,703, 4,519) | 4,181 (3,781, 4,635) | 4,121 (3,710, 4,527) |
Individuals free of mobility disability (n=1,370) or free of ADL disability (n=1,460) at baseline and followed over 4 years.
Q1=First quartile (25th percentile).
Q3= Third quartile (75th percentile).
The primary outcome was maintaining disability-free status. Over the subsequent 4 years, 89% (1,223/1,370) remained free of mobility disability and 84% (1,222/1,460) remained free of ADL disability. The baseline physical activity experience in Table 1 depicted by subsequent disability status shows the median time spent in baseline physical activity of all intensities is notably greater among adults who remained disability free compared with those who subsequently developed disability in ADL or mobility.
The AUC for each physical activity/sedentary measure is depicted for maintaining mobility disability-free status (Figure 1A) and for ADL disability-free status (Figure 1B) over 4 years. All measures performed better than a random coin flip (AUC=0.5) to predict subsequent disability-free status. Total MV time (AUC=0.80, 95% CI=0.76, 0.84) was a stronger and significantly better predictor of mobility disability-free status than other measures. Total MV time had greater AUC but was not statistically superior to other measures for predicting ADL disability-free status. Although sedentary time at baseline was related to remaining disability free over the 4-year period, it uniformly was the weakest predictor for both outcomes.
Figure 1.
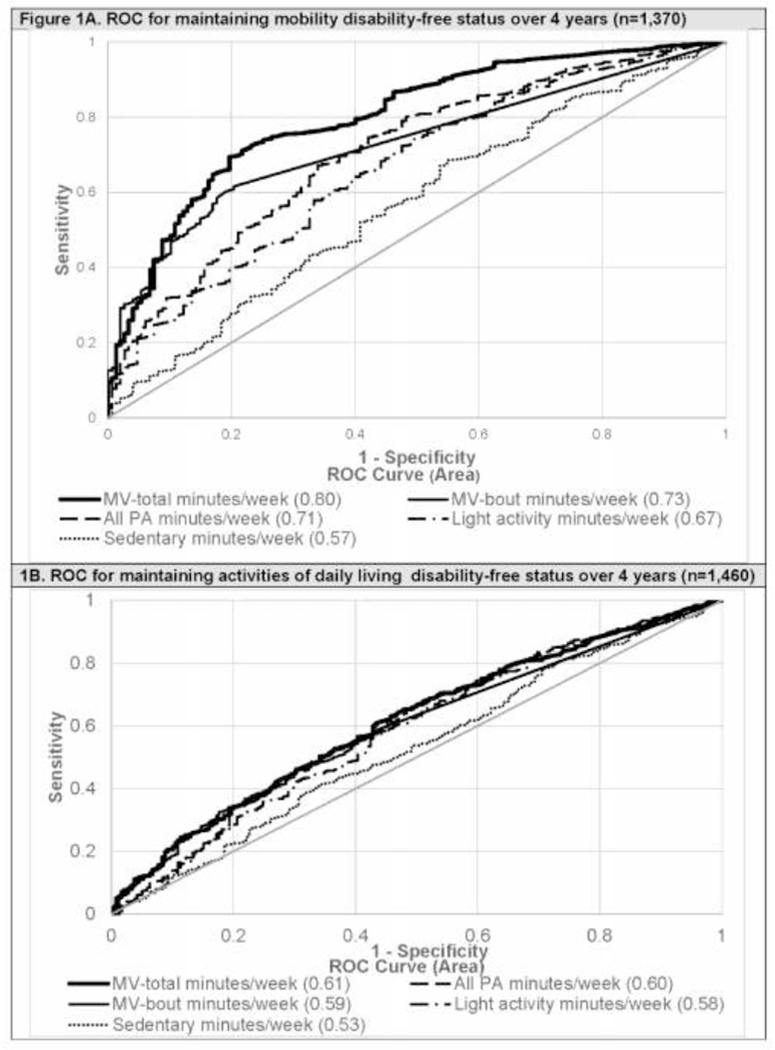
Receiver operating characteristic (ROC) curves for maintaining disability-free status over 4 years among adults with lower extremity joint symptom by physical activity/sedentary measures.
Notes: Moderate-vigorous (MV) activity, MV activity accrued in bouts lasting 10 minutes or more (MV-bout), light physical activity, total physical activity (PA) and sedentary behavior.
Classification tree analysis identified the optimal separately threshold to predict people who maintained disability-free status over 4 years for each separate outcome. All physical activity/sedentary measures were entered as classification tree predictors. The optimal classification trees in Figure 2 selected total MV per week as the best predictor of both outcomes. The optimal minimum threshold predicting disability-free status in mobility was total MV ≥56 minutes/week at baseline. The optimal minimum threshold predicting ADL disability-free status was total MV ≥55 minutes/week at baseline.
Figure 2.
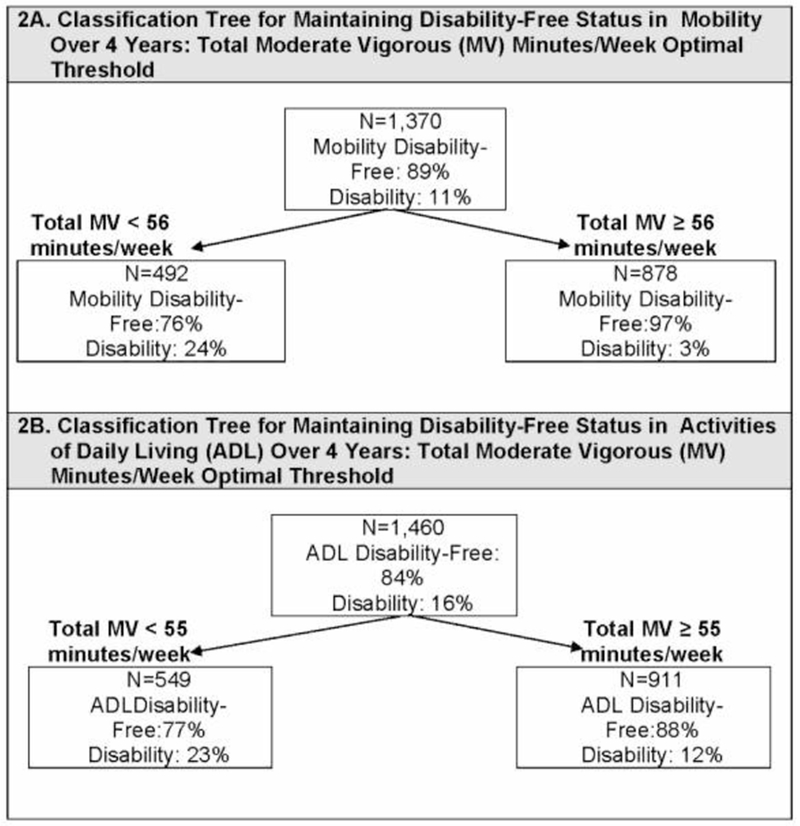
Classification trees selecting physical activity thresholds to predict disability free status over 4 years.
Sensitivity analyses investigated if these optimal thresholds were specific to age, sex, presence/absence of knee OA, or BMI. All sensitivity analysis classification trees selected the optimal total MV thresholds shown in Figure 2, demonstrating good stability of the MV-total thresholds.
Table 2 summarizes the ability of the identified physical activity thresholds to predict subsequent disability onset expressed as RRs. Observed disability onset rates over 4 years were 8 times greater (24% vs 3%) for developing mobility disability and almost double (23% vs 12%) for developing ADL disability among people engaged in total MV activity below versus above minimum threshold levels. People meeting the optimal mobility threshold (total MV ≥56 minutes/week) had 85% lower risk for developing mobility disability (RR=0.14, 95% CI=0.09, 0.20) compared with those doing less. People meeting the optimal MV threshold for ADL disability-free outcomes (MV total ≥55 minutes/week) had 45% lower RR for developing ADL disability (RR=0.55, 95% CI=0.44, 0.70) compared with those with less. These significant risk reductions held adjusting for age, sex, BMI, and the presence of knee OA.
Table 2.
RR for Developing Disability Among Adults With Baseline Lower Extremity Symptoms by Physical Activity Thresholds
| Physical activity in minutes/week | Mobility disability above vs below threshold N=1,370 | ADL disability above vs below threshold N=1,460 | ||
|---|---|---|---|---|
| Unadjusted RR (95% CI) | Adjusted RR (95% CI) | Unadjusted RR (95% CI) | Adjusted RR (95% CI) | |
| Optimal threshold | ||||
| MVa ≥55b | – | – | 0.55 (0.44, 0.70) | 0.60 (0.46, 0.78) |
| MVa ≥56c | 0.14 (0.09, 0.20) | 0.21 (0.14, 0.32) | – | – |
| Simple threshold | ||||
| MVa ≥60d | 0.15 (0.10, 0.22) | 0.23 (0.15, 0.35) | 0.56 (0.45, 0.71) | 0.61 (0.47, 0.80) |
Total minutes of moderate-to-vigorous (MV) physical activity.
Optimal threshold for maintaining ADL disability-free status over 4 years.
Optimal threshold for maintaining mobility disability-free status over 4 years.
Conceptually easy threshold for public health message.
ADL, activity of daily living.
Because a conceptually simple threshold has communication advantages, the predictive property of a 1-hour per week total MV activity threshold, which is slightly greater than the optimal thresholds was investigated. Table 2 further illustrates the RR of people meeting a simple total MV ≥60 minutes/week compared with the CART optimal mobility disability threshold of total MV ≥56 minutes/week (RR=0.14 vs RR=0.15) and the CART optimal ADL disability threshold, total MV≥55 minutes/week (RR=0.55 vs RR=0.56). These similar findings support a simple total MV ≥1-hour/week threshold to reduce the risk of developing disability.
DISCUSSION
The primary finding of this study is people who met an evidence-based threshold of approximately 1-hour total MV minutes per week had greater probability to remain disability free over 4 years than those below the threshold among adults with lower extremity joint symptoms. Time spent in MV each week was a stronger predictor of maintaining disability-free status than time spent in bouts of MV, less intensive physical activity, or sedentary time. Evidence-based thresholds to maintain disability-free status in mobility and ADL (56 and 55 minutes/week of total MV activity, respectively) are lower than the standard physical activity recommendation (MV-bout 150 minutes or more/week). A lower threshold that supports maintaining disability-free status provides an intermediate goal to motivate inactive older adults to begin their path towards a physically active lifestyle with the wide range of health benefits promoted by this lifestyle.
Traditional aerobic thresholds are embodied in international9 and government37 health agency aerobic recommendations (at least 150 MV minutes throughout the week or at least 75 minutes of vigorous-intensity physical activity throughout the week). In reality, a large portion of adults fail to attain these aerobic guidelines, particularly those adults with lower extremity joint conditions, who are at elevated risk for developing disability.12 It is likely levels of physical activity below the recommended aerobic threshold are beneficial based on demonstrated dose–response relationships between physical activity and health outcomes. A recent Physical Activity Guideline Advisory Committee reported dose–response relationships between physical activity and blood pressure, cardiovascular disease, lipids, blood glucose, and many others.17 Prospective data from more than 33,000 Norwegian adults found 1 to 2 hours of reported exercise each week nearly halved the long-term risk of depression.38 Longitudinal studies of 336,326 older Asians found self-reported physical activity below the current recommendation was related to lower all-cause mortality rates compared with inactive adults.39 Although these studies give valuable support to formulating intermediate physical activity goals, they are not designed to assess minimum thresholds.
To the authors’ knowledge, no systematic work has been conducted to identify minimum physical activity thresholds related to preventing disability outcomes in older adults. Recent work investigated minimum physical activity thresholds related to maintaining physical function.40 Optimal minimum thresholds to maintain function were 45–47 total MV minutes/week. Taken together with the present thresholds of 55–56 total MV minutes/week to improve the likelihood of remaining disability free over 4 years, these findings support an intermediate physical activity goal substantially below the 150 MV minutes/week recommendation.
Limitations
Strengths of this study included prospective data collection across multiple sites, the large sample size, and the objective assessment of physical activity from accelerometer monitoring. Study limitations need to be considered in interpreting results. The present sample was composed of adults with lower extremity joint symptoms from a cohort having or at high risk for developing knee OA. This sample may include a larger proportion of adults with symptomatic knees than the general joint symptom population, which may influence the generalizability of these results. However, physical activity thresholds held within subgroups with and without knee OA, supporting the robustness of these findings to disease status. Although a methodological strength is objective accelerometer measurement of physical activity, it is recognized the accelerometers used cannot capture water activities and may underestimate cycling activities. But time spent in these activities was negligible. Although less demanding physical activity thresholds may strengthen motivation to improve physical activity behavior, individuals with joint symptoms may need assistance to overcome additional barriers to maintain mobility (e.g., pain/weight management). Finally, causation cannot be inferred from these observational data. Physical activity at baseline could be a proxy for general health status. However, individuals with baseline disability were excluded by design, which partially mitigates this issue.
Recognizing simplicity is advantageous to public health communication, the predictive ability of a conceptually simple threshold based on 1-hour per week was investigated. If future work shows a 1-hour/week total MV threshold is beneficially related to other health outcomes, it provides advantages as an intermediate physical activity goal. A 1-hour/week goal is substantially less time than the traditional aerobic threshold. This finding is important from a public health perspective because time is a frequently cited as a barrier for not adopting a more physically active lifestyle.41 Also a threshold based on total MV activity in contrast to time in MV-bouts is valuable to increase activity levels in a symptomatic population, because symptoms often keep deconditioned people (like those with joint issues) from being able to sustain 10 minutes of MV. These findings are in harmony with the 2018 Physical Activity Guidelines for Americans which removed the MV-bout constraint from their updated recommendation.10 An intermediate target for inactive individuals, such as older adults dealing with joint symptoms, may motivate more people to increase physical activity.
CONCLUSIONS
Meeting an evidence-based threshold of 1-hour MV each week increased the likelihood of remaining free of disability among adults having lower extremity joint symptoms. This physical activity benchmark is lower than the traditionally recommended aerobic threshold. As an intermediate goal, this evidence-based 1-hour threshold supports future disability-free status and may help motivate adults with joint symptoms to take action towards the many health benefits of a physically active lifestyle.
Supplementary Material
ACKNOWLEDGMENTS
Research reported in this publication was supported in part by National Institute of Arthritis and Musculoskeletal Diseases under award numbers: R01-AR054155, P30-AR072579, and P60-AR48098, and the Falk Medical Trust. The publically released Osteoarthritis Initiative data were funded through a public-private partnership comprising five contracts (N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, N01-AR-2-2262) awarded by NIH, a branch of HHS. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation; GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the Osteoarthritis Initiative is managed by the Foundation for the NIH. The content of this report is solely the responsibility of the authors and does not necessarily represent the official views of NIH, the private funding partners, or the Centers for Disease Control and Prevention.
C. Kent Kwoh reported receiving consulting fees from EMD Serono, Astrellas, Thusane, Express Scripts, Regulus, GSK, Regeneron, and grant funding from Pfizer and AbbVie. No other financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hardy SE, Kang Y, Studenski SA, Degenholtz HB. Ability to walk 1/4 mile predicts subsequent disability, mortality, and health care costs. J Gen Intern Med. 2011;26(2):130–135. 10.1007/s11606-010-1543-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161(21):2602–2607. 10.1001/archinte.161.21.2602. [DOI] [PubMed] [Google Scholar]
- 3.Luppa M, Luck T, Weyerer S, Konig HH, Brahler E, Riedel-Heller SG. Prediction of institutionalization in the elderly: a systematic review. Age Ageing. 2010;39(1):31–38. 10.1093/ageing/afp202. [DOI] [PubMed] [Google Scholar]
- 4.Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 5.Gill TM, Guralnik JM, Pahor M, et al. Effect of structured physical activity on overall burden and transitions between states of major mobility disability in older persons: secondary analysis of a randomized trial. Ann Intern Med. 2016;165(12):833–840. 10.7326/M16-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311(23):2387–2396. 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hidalgo-Santamaria M, Fernandez-Montero A, Martinez-Gonzalez MA, et al. Exercise intensity and incidence of metabolic syndrome: the SUN Project. Am J Prev Med. 2017;52(4):e95–e101. 10.1016/j.amepre.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 8.Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. 2013;45(5):649–657. 10.1016/j.amepre.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 9.WHO. Global recommendations on physical activity for health Geneva, Switzerland: WHO Press; 2010:15–35. [Google Scholar]
- 10.HHS. Physical Activity Guidelines for Americans, 2nd edition HHS; 2018. [Google Scholar]
- 11.Clarke T, Norris T, Schiller J. Early release of selected estimates based on data from 2016 National Health Interview Survey. National Center for Health Statistics; 2017. [Google Scholar]
- 12.Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the osteoarthritis initiative: are guidelines being met? Arthritis Rheum. 2011;63(11):3372–3382. 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ettinger WH Jr., Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: the Fitness Arthritis and Seniors Trial (FAST). JAMA. 1997;277(1):25–31. 10.1001/jama.1997.03540250033028. [DOI] [PubMed] [Google Scholar]
- 14.DiPietro L, Jin Y, Talegawkar S, Matthews CE. The joint associations of sedentary time and physical activity with mobility disability in older people: the NIH-AARP Diet and Health Study. J Gerontol A Biol Sci Med Sci. 2018;73(4):532–538. 10.1093/gerona/glx122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dunlop DD, Song J, Semanik PA, et al. Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: prospective cohort study. BMJ. 2014;348:g2472 10.1136/bmj.g2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song J, Gilbert AL, Chang RW, et al. Do inactive older adults who increase physical activity experience less disability: evidence from the osteoarthritis initiative. J Clin Rheumatol. 2017;23(1):26–32. 10.1097/RHU.0000000000000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Scientific Report. Washington DC: HHS; 2018. [Google Scholar]
- 18.Stamatakis E, Kelly P, Strain T, Murtagh EM, Ding D, Murphy MH. Self-rated walking pace and all-cause, cardiovascular disease and cancer mortality: individual participant pooled analysis of 50 225 walkers from 11 population British cohorts. Br J Sports Med. 2018;52(12):761–768. 10.1136/bjsports-2017-098677. [DOI] [PubMed] [Google Scholar]
- 19.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. 10.1093/gerona/55.4.M221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA. Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among U.S. adults, 2015–2040. Arthritis Rheumatol. 2016;68(7):1582–1587. 10.1002/art.39692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nevitt M, Felson D, Lester G. The Osteoarthritis Initiative Protocol for the Cohort Study. https://oai.epi-ucsf.org/datarelease/docs/studydesignprotocol.pdf. Published 2006. Accessed December 20, 2018.
- 22.Eckstein F, Wirth W, Nevitt MC. Recent advances in osteoarthritis imaging--the osteoarthritis initiative. Nat Rev Rheumatol. 2012;8(10):622–630. 10.1038/nrrheum.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perera S, Patel KV, Rosano C, et al. Gait speed predicts incident disability: a pooled analysis. J Gerontol A Biol Sci Med Sci. 2016;71(1):63–71. 10.1093/gerona/glv126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Montero-Odasso M, Schapira M, Soriano ER, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60(10):1304–1309. 10.1093/gerona/60.10.1304. [DOI] [PubMed] [Google Scholar]
- 25.Rodgers W, Miller B. A comparative analysis of ADL questions in surveys of older people J Gerontol B Psychol Sci Soc Sci. 1997;52B(Special Issue):21–36. 10.1093/geronb/52B.Special_Issue.21. [DOI] [PubMed] [Google Scholar]
- 26.Jette AM, Haley SM, Coster WJ, et al. Late life function and disability instrument: I. development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M209–M216. 10.1093/gerona/57.4.M209. [DOI] [PubMed] [Google Scholar]
- 27.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34(8):1376–1381. 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 28.Song J, Semanik P, Sharma L, et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2010;62(12):1724–1732. 10.1002/acr.20305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 30.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32(3):128–132. 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 31.Pepe MS. The receiver operating curve for continuous tests In: The Statistical Evaluation of Medical Tests of Classification and Prediction. New York: Oxford University Press; 2004:66–76. [Google Scholar]
- 32.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–845. 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 33.Breiman L, Friedman JH, Oshen RA, Stone CJ. Classification and Regression Trees. Monterey, CA: Wadsworth & Brooks; 1984. [Google Scholar]
- 34.Esposito F, Malerva D, Semeraro G. Decision tree pruning as a search in the state space In: Lecture Notes in Computer Science . London: Springer-Verlag; 1993:165–184. [Google Scholar]
- 35.Salford Systems. CART. 7.0 ed San Diego, CA: Salford Systems; 2008. [Google Scholar]
- 36.Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat Med. 2004;23(9):1455–1497. 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- 37.HHS. 2008 Physical Activity Guidelines for Americans. Washington DC: HHS; 2008. [Google Scholar]
- 38.Harvey SB, Overland S, Hatch SL, Wessely S, Mykletun A, Hotopf M. Exercise and the prevention of depression: results of the HUNT Cohort Study. Am J Psychiatry. 2018;175(1):28–36. 10.1176/appi.ajp.2017.16111223. [DOI] [PubMed] [Google Scholar]
- 39.Jeong HG, Kim DY, Kang DW, et al. Physical activity frequency and the risk of stroke: a nationwide cohort study in Korea. J Am Heart Assoc. 2017;6(9). 10.1161/JAHA.117.005671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dunlop DD, Song J, Lee J, et al. Physical activity minimum threshold predicting improved function in adults with lower-extremity symptoms. Arthritis Care Res (Hoboken). 2017;69(4):475–483. 10.1002/acr.23181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sallis JF, Hovell MF, Hofstetter CR. Predictors of adoption and maintenance of vigorous physical activity in men and women. Prev Med. 1992;21(2):237–251. 10.1016/0091-7435(92)90022-A. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


