Abstract
Objectives:
Describe trends in diagnosis of ankyloglossia and use of lingual frenotomy, and analyze patient and hospital-level factors compared to the total pediatric discharge population.
Study Design:
Retrospective analysis
Methods:
We reviewed available data from years 1997 to 2012 using the Kidś Inpatient Database (KID), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality. All weighted pediatric discharges with ankyloglossia, newborn feeding difficulty, or lingual frenotomy were analyzed for variables of sex, payer, zip code median income, hospital ownership, location/teaching status, bed size, region, and children’s hospital status. Chi2 analysis with 95% confidence intervals and Odds Ratio were used to identify differences between the study group and the total database discharge population.
Results:
Diagnosis of ankyloglossia increased each year with N of 3934, 5430, 7785, 11397, 19459, and 32837 children respectively, with the largest increase in the last 6 years. Similarly, frenotomy increased with N of 1279, 1633, 2538, 3988, 6900, and 12406 procedures. Compared to the total discharge population, children with ankyloglossia or frenotomy, respectively, were more often male (63.6% ankyloglossia, 65.3% frenotomy vs 51.2%), privately insured (60.1%, 62.1% vs 43.6%), from higher income zip code (78.1%, 78.2% vs 68.6%), and lived in Midwest region (29.3%, 32.3% vs 21.7%).
Conclusion:
These pilot data show increases in diagnoses of ankyloglossia and use of frenotomy. There is a preponderance of children who are male, privately-insured, or Midwest residents being diagnosed and treated for ankyloglossia. This broad variation may reflect local practice patterns, or imply cultural and socioeconomic bias.
Keywords: Ankylogossia, tongue tie, frenotomy, frenulectomy, lingual, pediatric, infant, feeding difficulty
Introduction
Clinical practice experience suggests that the diagnosis of ankyloglossia and use of lingual frenotomy may be increasing. Recently, this has been demonstrated in a large population study from British Columbia.1 However, the recent comparative effectiveness review sponsored by the AHQR published in 2015 concluded that the body of evidence supporting frenotomy is small and insufficient.2,3
The incidence of ankyloglossia has been estimated to range from 0.02 to 10.7%.2,3,4,5 There is little consensus in either diagnostic criteria for ankyloglossia or the significance of ankyloglossia in breastfeeding difficulties.6 Surgical treatment can be performed in a variety of settings including the newborn nursery or outpatient clinic. The procedures are often performed by otolaryngologists, pediatric surgeons, dentists, oral surgeons, family physicians, pediatricians, and nurse practitioners. With early access to breastfeeding specialists, often these procedures are performed prior to initial discharge.
There have been significant advances in the promotion of breastfeeding and the factors that impact its success. Ankyloglossia is believed to be associated with breastfeeding difficulty.2 Unfortunately, there are few high-quality studies that have addressed lingual frenotomy outcomes in breastfeeding. While there does appear to be benefit in feeding outcomes and maternal discomfort, the understanding of how to distinguish infants with functionally significant ankyloglossia and those with other factors impacting breastfeeding success is limited. Identifying infant feeding difficulties often involves a multidisciplinary team of nurses, pediatricians, lactation consultants, speech therapists, obstetricians, and surgeons. It is estimated that 14–90% of infants with ankyloglossia may have latching difficulties.7 Identifying and managing ankyloglossia within this multidisciplinary context can be complex especially without standardized diagnostic criteria and treatment thresholds.
We hypothesize that there is an increasing trend in the diagnosis of ankyloglossia and use of lingual frenotomy within the hospital setting. We aimed to evaluate national trends in diagnosis of ankyloglossia and feeding difficulty and frenotomy procedures performed during hospitalization, and evaluate factors associated with these diagnosis and procedure.2,3
Methods
We performed a Johns Hopkins Medicine IRB approved retrospective review of the data from the Kidś Inpatient Database (KID), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.8 We utilized the online HCUPnet to analyze trends of pediatric discharges related to ankyloglossia. 9
The HCUP KIDS database contains discharge level inpatient data on children (age 0–17 years) from a representative sample of nationwide hospitals weighted from 3 million pediatric discharges, 44 states, and more than 4,100 hospitals in 2012 to estimate approximately 7 million hospitalizations. The weighted sample includes both normal newborn as well as other pediatric discharges in order to be representative of the United States geographic distribution. The KID data is published every three years from 1997 to 2012. HCUPnet is a free, online query tool that allows online access to HCUP data and produces aggregate data for analysis. Weighted aggregate data was obtained from the HCUPnet KIDS database from years 1997, 2000, 2003, 2006, 2009, and 2012. All pediatric patient discharges for children aged 0 to 17 with ankyloglossia (ICD-9 750.0) and newborn feeding difficulty (ICD-9 783.3) from each year were tabulated. Additionally, procedure code lingual frenotomy (ICD-9 25.91) for each year was tabulated.
Total births data for each corresponding year were obtained from CDC National Vital Statistics System. The 2012 HCUPnet KIDS was then queried for variables of age, sex, payer, median income for zip code, patient residence, hospital ownership, location/teaching hospital status, bed size, region, and children’s hospital status. Median income of zip code was used as a proxy for socioeconomic status.
Chi2 analyses were performed with HCUPnet aggregate data at an alpha level of 0.01, to assess differences in demographics between the total discharged population and children with ankyloglossia, frenotomy, and feeding difficulty. Odds Ratio was calculated for effect size of comparisons with significant differences (p<0.01). Statistically significant comparisons with 95% CIs that did not overlap were deemed clinically meaningful and statistically significant on post-hoc analysis. Analysis was performed with Stata version 14.10
Results
From 1997 to 2012, diagnosis of ankyloglossia (ICD-9 750.0) increased each database year with N of 3934, 5430, 7785, 11397, 19459, and 32837 children diagnosed respectively, with the largest increase noted in the last 6 years. Frenotomy procedures (ICD-9 25.91) increased by N of 1279, 1633, 2538, 3988, 6900, and 12406 procedures. Diagnosis of feeding difficulty (ICD-9 783.3) increased by N of 8845, 10724, 15173, 20222, 29004, and 36720. These exponential increases in the diagnosis of feeding difficulty, ankyloglossia, and frenotomy procedure are shown in Figure 1. The total pediatric discharges remained stable with N of 6348537, 6351345, 6468925, 6578069, 6393803, and 5850184. Additionally, the number of births, as identified by CDC data, has remained stable with N of 3882000, 4058814, 4089950, 4265555, 4131019, and 3952841 [Figure 2]. There was an 834% increase in the reported diagnosis of ankyloglossia and an 866% increase in the reported frenulum procedures from the 1997 data to the 2012 data.
Figure 1 –
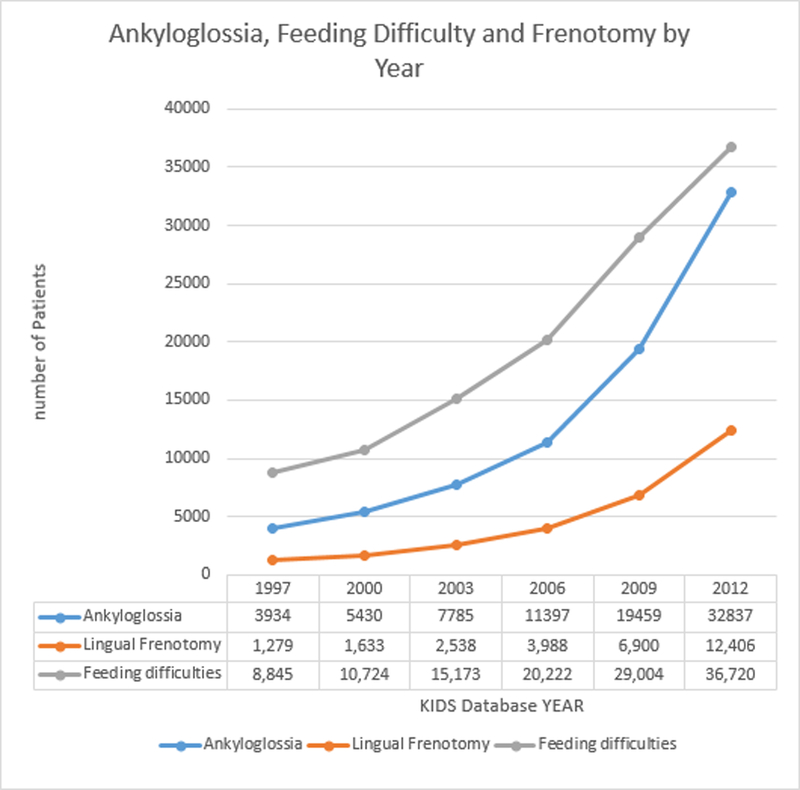
Diagnosis of Ankyloglossia, Frenotomy, and Feeding Difficulty Trends by Year
Figure 2 –
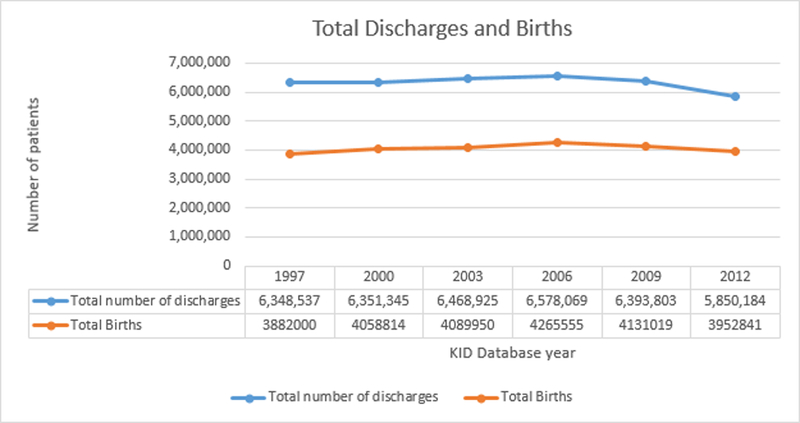
Total Discharges and Births Trend by Year
The demographic comparison of children diagnosed with ankyloglossia from the 2012 HCUPnet KIDS database to the discharge population is shown in Table 1.
Table 1 –
Ankyloglossia Group
| Tongue Tie (ICD-9 750.0) | All Discharges | ||||||
|---|---|---|---|---|---|---|---|
| N | % [95% CI] | N | % [95% CI] | OR | P value | ||
| All discharges | 32,837 | 5850184 | |||||
| Age group | <1 year | 32,458 | 98.8% [91.1,106.6] | 4269984 | 73.0% [70.7,75.3] | ||
| Sex | Male** | 20,872 | 63.6% [58.6,68.5] | 2993781 | 51.2% [49.3,53.1] | 1.67 | <0.0001 |
| Female | 11,944 | 36.4% [33.4,39.3] | 2854141 | 48.8% [47.1,50.5] | - | - | |
| Payer | Medicare | 113 | 0.3% [0.2,0.5] | 20659 | 0.4% [0.3,0.5] | 0.97 | 0.783 |
| Medicaid** | 10806 | 32.9% [29.6,36.3] | 2845288 | 48.6% [46.6,50.7] | 0.52 | <0.0001 | |
| Private insurance** | 19749 | 60.1% [54.8,65.5] | 2550281 | 43.6% [41.7,45.5] | 1.96 | <0.0001 | |
| Uninsured | 948 | 2.9% [2.4,3.4] | 207468 | 3.5% [3.3,3.8] | 0.81 | <0.0001 | |
| Other | 1176 | 3.6% [3.0,4.2] | 211478 | 3.6% [3.2,4.0] | 0.99 | 0.744 | |
| Missing | 46 | 0.1% * | 15010 | 0.3% [0.2,0.4] | 0.54 | <0.0001 | |
| Median income for zipcode | Low** | 6806 | 20.7% [18.0,23.5] | 1723887 | 29.5% [28.0,31.0] | 0.62 | <0.0001 |
| Not low** | 25653 | 78.1% [71.8,84.4] | 4014292 | 68.6% [65.7,71.5] | 1.64 | <0.0001 | |
| Missing | 378 | 1.2% [0.9,1.4] | 112005 | 1.9% [1.6,2.2] | 0.6 | <0.0001 | |
| Owner | Government | 4031 | 12.3% [9.8,14.8] | 763782 | 13.1% [12.0,14.1] | 0.93 | <0.0001 |
| Private, not-for-profit | 26448 | 80.5% [73.3,87.8] | 4316055 | 73.8% [70.5,77.1] | 1.47 | <0.0001 | |
| Private, for-profit** | 2359 | 7.2% [5.7,8.7] | 770347 | 13.2% [11.9,14.5] | 0.51 | <0.0001 | |
| Location/ Teaching status | Rural | 3407 | 10.4% [9.1,11.6] | 604476 | 10.3% [9.8,10.8] | 0.97 | 0.798 |
| Urban nonteaching | 10705 | 32.6% [29.3,35.9] | 1838613 | 31.4% [29.8,33.0] | 1.06 | <0.0001 | |
| Urban teaching | 18725 | 57.0% [50.1,64.0] | 3407094 | 58.2% [54.9,61.6] | 0.95 | 0.001 | |
| Bedsize | Small | 3562 | 10.8% [9.2,12.5] | 638027 | 10.9% [9.7,12.1] | 0.99 | 0.733 |
| Medium | 8473 | 25.8% [21.8,29.8] | 1442122 | 24.7% [22.7,26.7] | 1.06 | <0.0001 | |
| Large | 20802 | 63.3% [56.8,69.9] | 3770036 | 64.4% [61.1,67.8] | 0.95 | <0.0001 | |
| Region | Northeast | 6230 | 19.0% [15.6,22.3] | 995190 | 17.0% [15.2,18.9] | 1.14 | <0.0001 |
| Midwest** | 8482 | 25.8% [23.2,28.5] | 1266699 | 21.7% [19.9,23.5] | 1.26 | <0.0001 | |
| South** | 9625 | 29.3% [24.5,34.1] | 2227819 | 38.1% [35.5,40.7] | 0.67 | <0.0001 | |
| West | 8500 | 25.9% [21.4,30.3] | 1360476 | 23.3% [21.3,25.2] | 1.15 | <0.0001 | |
| Children’s hospital | Non-children’s | 25719 | 78.3% [72.3,84.4] | 4089846 | 69.9% [67.4,72.5] | 1.56 | <0.0001 |
| Children’s | 7119 | 21.7% [16.1,27.3] | 1760338 | 30.1% [26.4,33.8] | - | - | |
- too small for accuracy
- p<0.01 and non-overlapping CI
OR = Odds Ratio, CI = Confidence Interval
When considering the total discharge population, a higher proportion of children with ankyloglossia when compared to children without ankylogossia were observed in the variables of male sex at 63.6% with 95% CI [58.6, 68.5], OR 1.67 [1.63, 1.71] p<0.0001, private insurance 60.1% [54.8, 65.5], OR 1.96 [1.92, 2.00] p<0.0001, mid-level to high median income zip code 78.1% [71.8,84.4], OR 1.64 [1.59,1.68] p<0.0001, and Midwest region 25.8% [23.2,28.5], OR 1.26 [1.23, 1.29] p<0.0001. Lower observed proportions of children with ankyloglossia were found for Medicaid 32.9% [29.6,36.2], OR 0.52 [0.50, 0.53] p<0.0001, low income zip code 20.7% [18.0,23.5], OR 0.62 [0.61, 0.64] p<0.0001, private for profit hospital 7.2% [5.7,8.7], OR 0.51 [0.48, 0.53] p<0.0001, and South region 29.3% [24.5,34.1], OR 0.67 [0.66,0.69] p<0.0001. [Table 1]
The trends of ankyloglossia diagnosis by insurance payer for each year were compared and shown in Figure 3. Medicaid payer status from 1997 to 2012 was 1116, 1308, 2082, 3250, 6208, 10806. Private insurance payer status for the same period was 2493, 3762, 5081, 7266, 12019, 19749.
Figure 3 –
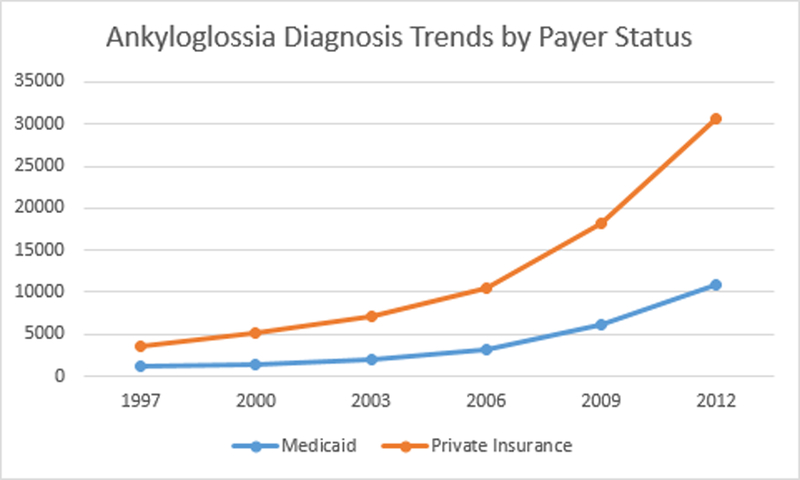
Ankyloglossia Diagnosis by Payer Status Trend
Variations similar to the ankyloglossia group were observed in children receiving a frenotomy procedure. There were higher observed percentages with non-overlapping 95% CIs for male 65.3% [57.5, 73.1], OR 1.80 [1.73, 1.87] p<0.0001, private insurance 62.1% [54.0, 70.2], OR 2.12 [2.04, 2.20] p<0.0001, and Midwest region 32.3% [27.3,37.3], OR 1.73 [1.66, 1.79] p<0.0001. Lower observed percentages were found for Medicaid 30.7% [25.6,35.7], OR 0.47 [0.45, 0.49] p<0.0001, low income zip code 20.7% [16.0,25.4], OR 0.62 [0.60, 0.65] p<0.0001, private for profit hospital 6.1% [4.1,8.2], OR 0.43 [0.40, 0.46] p<0.0001, and South region 26.1% [18.7,33.4], OR 0.57 [0.55, 0.60] p<0.0001.
It is also notable that in the feeding difficulty group, the above factors of sex, insurance, and location were not as significantly found. However, lower observed percentages with non-overlapping 95% CIs were found in uninsured patients 2.6% [2.3,2.9], OR 0.73 [0.71, 0.76] p<0.0001, and in rural location 6.8% [5.9,7.8], OR 0.63 [0.62, 0.65] p<0.0001.
Discussion
This study is the first to measure US national trends for the diagnosis and surgical treatment of ankyloglossia. We found large increases in the number of patients diagnosed and treated for ankyloglossia over the years 1997 to 2012. Clinically meaningful factors more commonly seen in children with ankyloglossia included male sex, private insurance, mid-level to high median income zip code, and Midwest location. Moreover, for children with ankyloglossia who underwent frenotomy procedure male sex, private insurance, and mid-level to high median income zip code were more commonly seen.
Similar increases have been demonstrated in a British Columbia population study from 2004 to 2013.1 It is possible that this observed increase could be an artifact of a shift from outpatient diagnosis and management of ankyloglossia to early diagnosis and treatment of newborns before discharge. If this was the case, a representative decrease in outpatient procedures could be identified in an appropriate outpatient database sample. However, anecdotally in clinical practice experience there seems to be a corresponding increase in infants diagnosed and treated for ankyloglossia in outpatient settings as well, but we are not aware that this observation has been scientifically validated. The increase could also be due to higher numbers of premature births, with longer hospitalizations. However, this is also less likely in that the rate of premature births in the US has either remained stable or declined according to the CDC National Vital Statistics System.12 Therefore, a possible explanation for the identified increase could be due to national and global efforts on supporting breastfeeding, awareness of ankyloglossia, and its role in successful breastfeeding. For example, the Innocenti Declaration was published in 1990.13 The Academy of Breastfeeding Medicine was established in 1993. In 1998 the United States Breastfeeding Committee was established. In 2011, the Surgeon General published the breastfeeding call to action.11 These organizations, along with the World Alliance for Breastfeeding Action and many other national and international committees on breastfeeding have made great efforts to promote and advance the knowledge and research of breastfeeding. As part of this multidisciplinary focus, the issues of functional and anatomical barriers in the infant have played an increasing role.
It is reasonable to consider the association of factors such as private insurance, higher income zip codes, and private hospitals with increased access to breastfeeding support and resources. When comparing the diagnosis to the surgical treatment of ankyloglossia, differences in these statistically significant factors are similar, with the exception of zip code incomes, which are not as strongly demonstrated in surgically treated ankyloglossia. Additionally, the increasing trend of diagnosis of ankyloglossia is disproportionally seen in private insurance over Medicaid status when examined from 1997 to 2012.
The finding of 1.75:1 male to female ratio for ankyloglossia diagnosis is supported in other studies that demonstrate a higher incidence in male infants with a ratio of 1.5–2.6:1.14
A limitation of this study is that the KIDS database is a sample estimation of the total population. The HCUP KIDS database is a discharge level database that samples both birth and non-birth related discharges. The database does not capture procedures or diagnosis being made outside of the hospital admission. Conclusions of data can only be made for the population of children diagnosed and treated prior to their first discharge or who are readmitted and treated as an inpatient. Additionally, the data obtained from HCUPnet is aggregate data, individual level data for multivariate analysis was not utilized. Regarding the limitation of discharge level data, healthy newborn infants are typically discharged within 24–72 hours after birth. This leaves little time for determining if feeding difficulties are present and, more importantly, if ankyloglossia is playing a role in any difficulties. Breastfeeding difficulties can occur from factors that include maternal milk production problems, neonatal development factors, and limited access to breast feeding experts. Therefore, the identified trends of diagnosis and treatment are possibly of more import in light of those issues.
Overall, since initiation of worldwide initiatives in support and research for breastfeeding, there have been notable increases in awareness of, publications, diagnosis, and treatment for ankyloglossia and its related effects.14 Data on prevalence and trends prior to these initiatives is not available with current HCUP data. The role of global initiatives in the identified trends can only be speculated. Quality research studies are still lacking in many areas of the knowledge and management of breastfeeding and speech issues related to ankyloglossia. Gaps still remain between the increases in diagnosis and surgical treatment we demonstrate in this study and the available evidence. Further studies are needed to provide evidenced based guidance on standardized diagnosis of ankyloglossia as well as indications for treatment with surgery.
Conclusion
We show large increases in the diagnosis and treatment of ankyloglossia across U.S from 1997 to 2012, as demonstrated in a database of hospital pediatric discharges. Children who are male, privately insured, located in a mid to high income zip code, and Midwest location more likely to be diagnosed with ankyloglossia and treated with frenotomy. The paucity of high-quality evidence for the benefits of frenotomy raises concerns with regard to the demonstrated increases in diagnosis and treatment. There may also be factors of national initiatives for breastfeeding, local practice patterns, and cultural and socioeconomic bias which may be influencing national trends.
The disparity between the increasing trends, demographic and socioeconomic differences, and the available evidence emphasizes the need for objective diagnostic measures, and high-quality studies of ankylogossia’s role in infant feeding difficulties.
Footnotes
PRESENTED at the AAO-HNS Annual Meeting. September 2016. San Diego, CA.
REFERENCES
- 1.Joseph K, Kinniburgh B, Metcalfe A, Razaz N, Sabr Y, Lisonkova S. Temporal trends in ankyloglossia and frenotomy in British Columbia, Canada, 2004–2013: a population-based study. CMAJ Open 2016;4(1):E33–E40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Francis D, Krishnaswami S, McPheeters M. Treatment of Ankyloglossia and Breastfeeding Outcomes: A Systematic Review. Pediatrics 2015;135(6):e1458–e1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chinnadurai S, Francis D, Epstein R, Morad A, Kohanim S, McPheeters M. Treatment of Ankyloglossia for Reasons Other Than Breastfeeding: A Systematic Review. Pediatrics 2015;135(6):e1467–e1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webb A, Hao W, Hong P. The effect of tongue-tie division on breastfeeding and speech articulation: A systematic review. Int. J. Pediatr. Otorhinolaryngol 2013;77:635–646. [DOI] [PubMed] [Google Scholar]
- 5.Power R, Murphy J. Tongue-tie and frenotomy in infants with breastfeeding difficulties: achieving a balance. Arch Dis Child 2015;100:489–494. [DOI] [PubMed] [Google Scholar]
- 6.Messner A, Lalakea L. Ankyloglossia: controversies in management. Int. J. Pediatr. Otorhinolaryngol 2000:54 (123–131). [DOI] [PubMed] [Google Scholar]
- 7.Suter V, Bornstein M. Ankyloglossia: Facts and Myths in Diagnosis and Treatment. J Periodontol 2009;80:1204–1219. [DOI] [PubMed] [Google Scholar]
- 8.HCUP Kids’ Inpatient Database (KID). Healthcare Cost and Utilization Project (HCUP) 1997–2012. Agency for Healthcare Research and Quality, Rockville, MD: www.hcup-us.ahrq.gov/kidoverview.jsp [Google Scholar]
- 9.HCUPnet. Healthcare Cost and Utilization Project (HCUP) 1997–2012. Agency for Healthcare Research and Quality, Rockville, MD: http://hcupnet.ahrq.gov/ January 18, 2016. [PubMed] [Google Scholar]
- 10.StataCorp. 2015. Stata Statistical Software: Release 14 College Station, TX: StataCorp LP. [Google Scholar]
- 11.U.S. Department of Health and Human Services. Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; January 20, 2011. www.surgeongeneral.gov/libary/calls/breastfeeding September 7, 2016. [Google Scholar]
- 12.Martin J, Hamilton B, Osterman M, Curtin S, Mathews T. Births: Final Data for 2012. National Vital Statics Reports December 2013:62(9). http://www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_09.pdf September 27, 2016. [PubMed] [Google Scholar]
- 13.Innocenti Declaration. WHO/UNICEF meeting on “Breastfeeding in the 1990s: A Global Initiative” Spedale degli Innocenti, Florence, Italy: July 30, 1990. www.who.int/about/agenda/health_development/events/innocenti_declaration_1990.pdf November 7, 2016. [Google Scholar]
- 14.Ballard J, Auer C, Khoury J. Ankyloglossia: Assessment, Incidence, and Effect of Frenuloplasty on the Breastfeeding Dyad. Pediatrics 2002;110(5):e63. [DOI] [PubMed] [Google Scholar]


