Abstract
The original description of the LaPrade technique for anatomic posterolateral corner reconstruction addresses the 3 main stabilizing structures: the fibular collateral ligament, the popliteus, and the popliteofibular ligament. The use of two separate grafts (originally described with a tendo-Achilles allograft) may restrict the utility of the technique when sources of allograft may be limited and autografts must be used, particularly in the context of multiligament reconstruction. We present a modification of the technique, in which an adjustable cortical button is used for tibial fixation, which allows for the use of a single graft while maintaining the ability to independently tension the popliteus, popliteofibular ligament, and fibular collateral ligament limbs of the graft.
The understanding of the anatomy and biomechanics of the posterolateral corner (PLC) of the knee has evolved over the past 3 to 4 decades. The 3 key functional structures—the fibular collateral ligament (FCL), the popliteus, and the popliteofibular ligament (PFL)—play an important role in controlling both valgus and external rotation of the tibia.1, 2, 3, 4 Injury to the posterolateral structures is commonly associated with injury to 1 or both cruciate ligaments.4, 5 Failure to recognize and address concomitant PLC laxity during cruciate reconstruction may lead to persistent symptoms of instability, pain and ultimately increased risk of graft failure.1, 4
Many techniques, both anatomic and nonanatomic, have been described to address posterolateral rotatory laxity. These include biceps tenodesis procedures,6, 7 bone block advancements,8 and reconstruction techniques based off the fibular head, using 19 or 2 femoral tunnels.10 In 2004, LaPrade at al.11 published a technique for an anatomic reconstruction, attempting to recreate the FCL, PFL, and popliteus based on their native attachment sites.12 This has been shown to both biomechanically improve varus and rotatory laxity of the knee and produce good medium- to long-term clinical results.13 The reconstruction includes 2 separate grafts for the FCL and PFL/popliteus limbs and was originally described with the use of a split tendo-Achilles allograft.11 Modifications of the technique, in which 2 separate autografts are used, have been described.14 However, given that PLC lesions commonly occur in association with other ligament injuries, this may limit graft options.
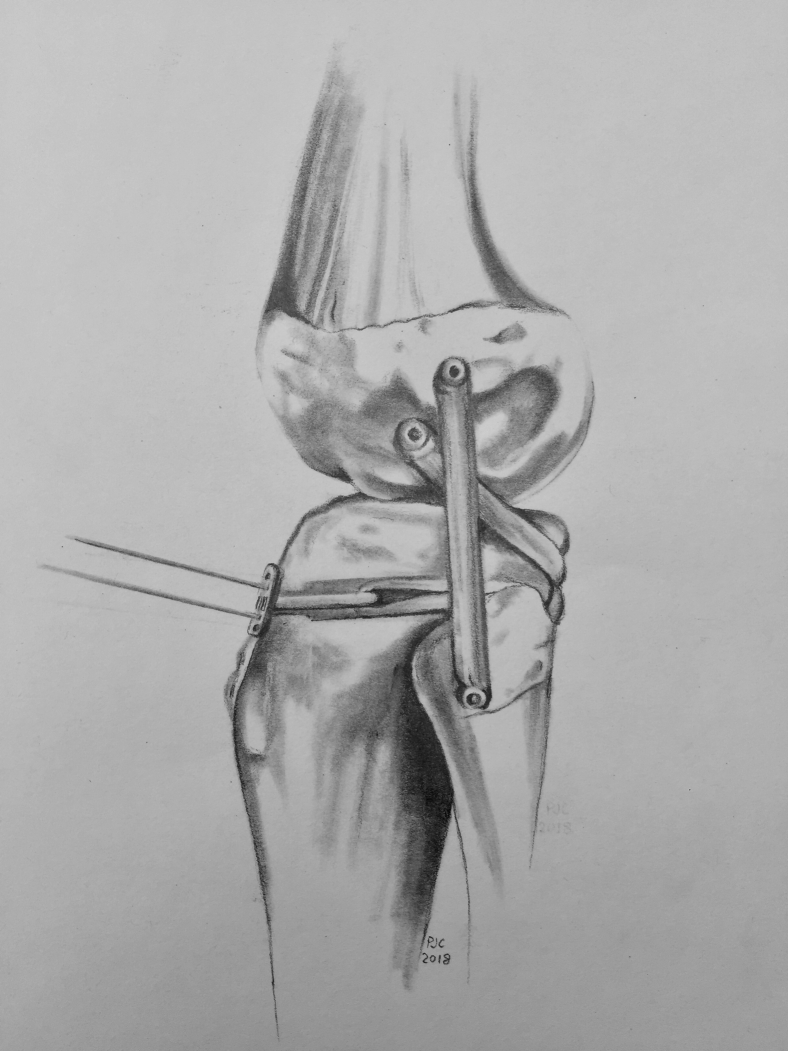
This report describes a modification of the LaPrade anatomic PLC reconstruction11 with the use of a single semitendinosus tendon and adjustable-length loop suspensory tibial fixation (summarized in Table 1), as well as pearls and pitfalls associated with the technique (Table 2). In our modification (Fig 1), only a single semitendinosus autograft is used, and the ability to cycle and retension the individual limbs of the graft is preserved because of the use of the adjustable- loop fixation device. This technique modification may be beneficial to surgeons who wish to undertake anatomic PLC reconstruction without using allograft either on grounds of cost or availability, in addition to reducing the morbidity associated with multiple autograft harvest sites, often involving the contralateral limb, particularly if autograft is the preferred option for multiligament reconstruction.
Table 1.
Abbreviated Surgical Plan
| Surgical Step | Details |
|---|---|
| Setup | Supine positioning with a lateral post and footrest with the knee at 90°; Pneumatic tourniquet applied to upper thigh. |
| Examination under anesthesia | Assessment of lateral joint opening with varus stress and posterolateral rotatory laxity at 30° and 90°; examination of both cruciate ligaments for concomitant injury. |
| Graft harvest | Ipsilateral semitendinosus autograft preferred; length measured at minimum 25 cm. |
| Lateral approach | Curvilinear skin incision from proximal to lateral epicondyle to Gerdy's tubercle; full-thickness subcutaneous skin flaps raised anterior and posterior. |
| Neurolysis | Identification, neurolysis, and release of the common peroneal nerve. |
| Posterolateral dissection | Window created anterior to lateral head of gastrocnemius; FCL remnant tagged within biceps bursa. |
| Drilling of fibular head tunnel | Dissection of fibular head; drilling of oblique, anteromedial to posterolateral tunnel using freehand technique; placement of passing suture. |
| Drilling of tibial tunnel | Tunnel emerges at posterolateral tibia at the musculotendinous junction of popliteus muscle to accommodate a double loop of graft; passing wire placed with loop posteriorly. |
| Drilling of femoral tunnels | ITB split and L-shaped capsulotomy created; PT and FCL attachment sites identified and drilled; passing sutures placed |
| Sequential graft fixation |
|
FCL, fibular collateral ligament; ITB, iliotibial band; PFL, popliteofibular ligament; PT, patellar tendon.
Table 2.
Pearls and Pitfalls of the Technique
| Step | Pearl | Pitfall |
|---|---|---|
| Preoperative decision making | Use of varus stress radiography to quantify the extent of the FCL injury. | Positive Dial test results may be produced by anteromedial as well as posterolateral corner laxity. |
| Skin incision | Ensure more anterior placement of the incision; the posterior skin flap will naturally fall away, allowing access to common peroneal nerve and posterolateral tibia. | Incision placed too posteriorly can make harvesting B-PT-B or quads autograft (for combined ACL/PCL reconstruction) through the same incision difficult. |
| Concomitant ACL reconstruction | Drill ACL femoral tunnel before drilling FCL and popliteus tunnels. Drill femoral FCL/PT tunnels 35° proximal and anterior. Arthroscopic visualization within the ACL femoral tunnel confirms that FCL and popliteus tunnel guide pins do not breech the tunnel and allow for repositioning before socket drilling. |
Coalition of tunnels can prevent adequate fixation. |
| Concomitant PCL reconstruction | Ensure PCL graft is passed and fixed before PLC to allow correct restoration of tibial step-off. | Fixing the PLC reconstruction before the PCL may result in malreduction of the knee. |
| Passage of Ultrabutton/loop of graft | Mark graft 2 cm from the aperture of the fibula tunnel. This will aid in gauging the amount of graft docked into the tibial tunnel. | Initial docking of a too-large loop will not allow sufficient graft length to reconstruct the FCL portion. |
ACL, anterior cruciate ligament; B-PT-B, bone–patellar tendon–bone autograft; FCL, fibular collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner; PT, patellar tendon.
Fig 1.
Artist's impression of the single-graft anatomic posterolateral corner reconstruction in which an adjustable-loop tibial fixation is done.
Surgical Technique
A full procedural demonstration may be found in Video 1. After induction of general anesthesia, the patient is positioned supine with a lateral thigh post and 1 or 2 footrests, depending on whether concomitant anterior cruciate ligament (ACL) reconstruction will be done. Using 2 footrests allows the knee to be maintained at the 2 most commonly needed flexion angles during a combined procedure, 70° to 90° and >120°, eliminating the need for an assistant to hold the leg. A padded pneumatic tourniquet is placed around the proximal thigh of the operative leg and may be inflated during the procedure as required.
Examination is performed with the patient under anesthesia, confirming the preoperative diagnosis. Particular attention is given to the presence of varus opening at 30° of flexion and in extension, the result of the Dial test, reverse pivot-shift, and presence of additional anterolateral laxity. It is important to note that the Dial test is a sign of external rotation laxity and therefore may be associated with anteromedial patholaxity. It is therefore important to differentiate between them.
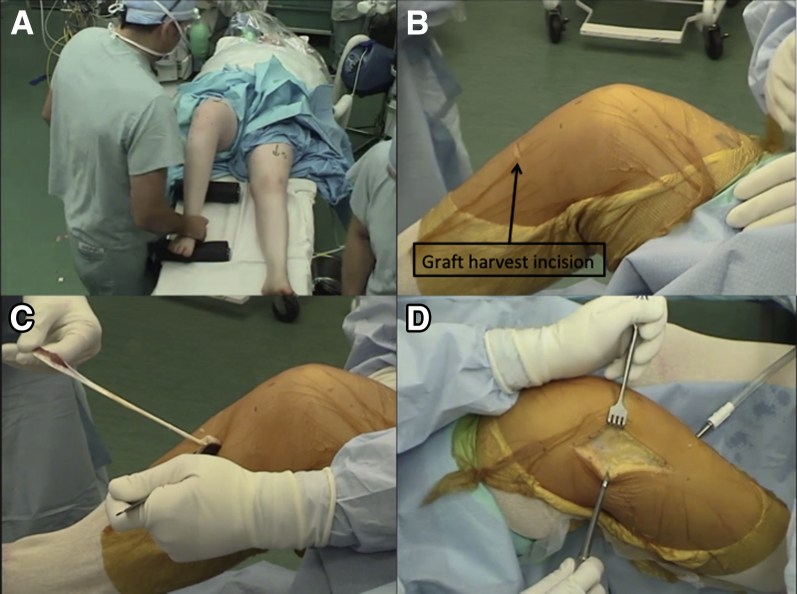
An arthroscopic examination can be undertaken first, but our preference is to perform the open surgical dissection of the lateral structures and graft harvest first (Fig 2). This prevents fluid extravasation into the soft tissues, which can distort tissue planes. Any doubts as to the underlying diagnosis would warrant initial arthroscopy before these steps are taken.
Fig 2.
Right leg, anterior cruciate ligament/posterolateral corner deficient knee. (A) The patient is positioned supine with a lateral thigh post and 1 or 2 footrests, depending on whether a concomitant ACL reconstruction will be done. Using 2 footrests allows the knee to be maintained at the 2 most commonly needed flexion angles during a combined procedure, 70° to 90° and >120°, eliminating the need for an assistant to hold the leg. A padded pneumatic tourniquet is placed around the proximal thigh of the operative leg and may be inflated during the procedure as required. (B and C) Semitendinosus graft harvest via a 1.5- to 2-cm longitudinal/oblique incision, made 2 cm medial to the tibial tuberosity 4 fingerbreadths distal to the medial joint line. (D) A lateral approach is used, and a curvilinear skin incision is made over the lateral side of the knee from the proximal to the lateral epicondyle toward Gerdy's tubercle on the anterolateral tibia.
With the knee positioned at 90° of flexion a 1.5- to 2-cm longitudinal/oblique incision is made 2 cm medial to the tibial tuberosity and 4 fingerbreadths distal to the medial joint line. The sartorius fascia is incised a few millimeters proximal to the superior border of the gracilis tendon. It is important to clearly distinguish the gracilis tendons from the semitendinosus tendons. The accessory bands running from the gracilis to the semitendinosus tendon are released with dissection along the inferior border of the gracilis tendon. Once the accessory bands have been clearly identified and freed, isolated semitendinosus harvest is performed. The harvested tendon is whipstitched for 25 mm at either end with No. 2 Vicryl sutures (Ethicon, Somerville, NJ) to tubularize the graft for easy passage into tunnels.
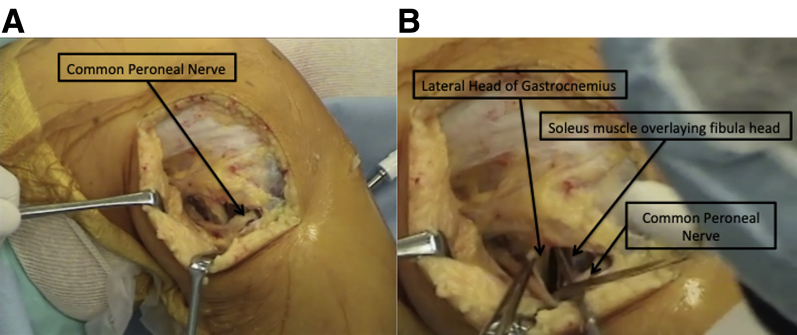
A curvilinear skin incision is made over the lateral side of the knee from the proximal to the lateral epicondyle toward Gerdy's tubercle on the anterolateral tibia. The same skin incision may be used to harvest a bone–patellar tendon–bone or quadriceps tendon autograft if required for combined ACL/posterior cruciate ligament reconstruction. Full-thickness subcutaneous skin flaps are then developed down to the level of the fibula neck. The common peroneal nerve is identified, released, and decompressed into the peroneus muscle belly (Fig 3). The peroneus fascia is incised, and a window is created just anterior to the lateral head of the gastrocnemius, allowing access to the posterolateral aspect of the tibial plateau. A horizontal incision is made in the distal biceps to enter the biceps bursa. The remnants of the FCL can be identified and tagged with traction sutures, allowing for easier identification of both femoral and fibula attachment sites.
Fig 3.
Right knee, lateral side, 90° of flexion. (A) Common peroneal nerve neurolysis. (B) The peroneus fascia is incised, and a window is created just anterior to the lateral head of gastrocnemius, allowing access to the posterolateral aspect of the tibial plateau.
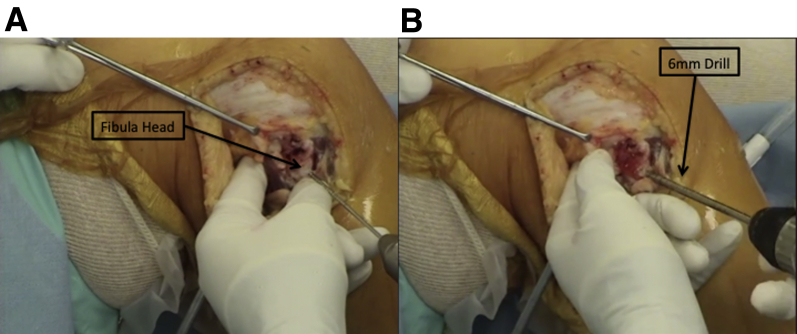
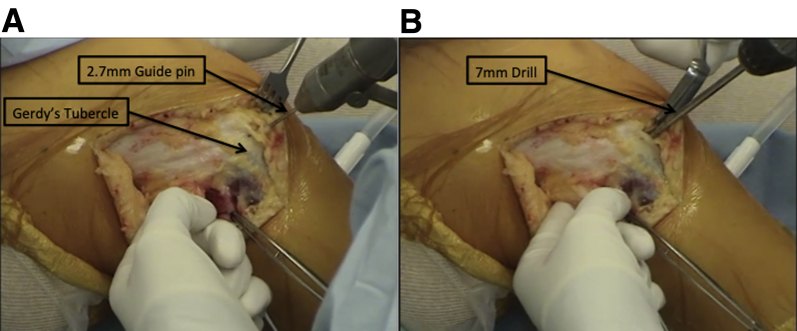
The distal attachment of the FCL on the fibula head is identified; it is located approximately 8 mm posterior to the anterior margin of the fibular head and 28 mm distal to the fibular styloid tip.3, 15 A 2.7-mm drill-tipped passing pin is drilled through the fibular head, in an anterolateral to posteromedial direction, from the FCL attachment site to the attachment site of the posterior division of the PFL on the posteromedial aspect of the fibular styloid process (Fig 4).
Fig 4.
Right knee, lateral side, 90° of flexion. (A) A 2.7-mm drill-tipped passing pin is drilled through the fibular head in an anterolateral to posteromedial direction, from the fibular collateral ligament (FCL) attachment site to the attachment site of the posterior division of the popliteofibular ligament on the posteromedial aspect of the fibular styloid process. (Note that in this case there is an avulsion of FCL off the fibula head.) (B) This is overdrilled with a 6-mm drill, and a passing suture is applied.
Our preference is to perform this freehand, drilling toward the tip of a finger placed at the back of the fibular head. This can then be overdrilled to a diameter to suit passage of a single limb of the graft of choice, typically 6 mm. The tunnel should be sized to allow easy passage of the graft, but care should be taken if a tunnel of larger diameter is being drilled because of the subsequent risk of fibula head fracture. A passing suture can then be passed through the tunnel and secured for future use.
The flat spot on the anterior tibia, just distal and medial to Gerdy's tubercle, is identified; and a 2.7-mm drill-tipped passing pin is drilled through the proximal tibia, in an anterior to posterior direction, aiming toward the musculotendinous junction of popliteus(Fig 5). This point is approximately 1 cm proximal and 1 cm medial to the fibular tunnel. Again, our preference is to drill freehand toward the tip of a finger, but a tibial aiming guide or proprietary posterolateral corner reconstruction aiming guide can be used for this step. The tunnel is then dilated to allow easy passage of the doubled loop of semitendinosus graft; typically, this is to a diameter of 6 to 8 mm, depending on the diameter of the doubled loop of the semitendinosus. A retrograde drilling technique can be used for this step to allow the suspensory fixation device to be deployed on the anterior tibia. Alternatively, the tunnel may be over-reamed from anterior to posterior, necessitating the use of a larger cortical fixation device (ExtendoButton, Smith & Nephew, London, UK) in conjunction with the Ultrabutton (Smith & Nephew). A loop of suture material is then passed from anterior to posterior through the tunnel and is retrieved at the posterior tibia and out through the lateral skin incision, while ensuring that the common peroneal nerve is free.
Fig 5.
Right knee, lateral side, 90° of flexion. (A) A 2.7-mm drill-tipped passing pin is drilled through the proximal tibia, starting at the flat spot medial to Gerdy's tubercle, in an anterior to posterior direction, aiming toward the musculotendinous junction of the popliteus. This tends to be 1 cm medial and proximal to the exit point of the fibula head tunnel. (B) The tunnel is then dilated to allow easy passage of the doubled loop of semitendinosus graft; typically, this is to a diameter of 6 to 8 mm, depending on the diameter of the doubled loop of the semitendinosus. A retractor or finger is kept posteriorly to protect the neurovascular structures.
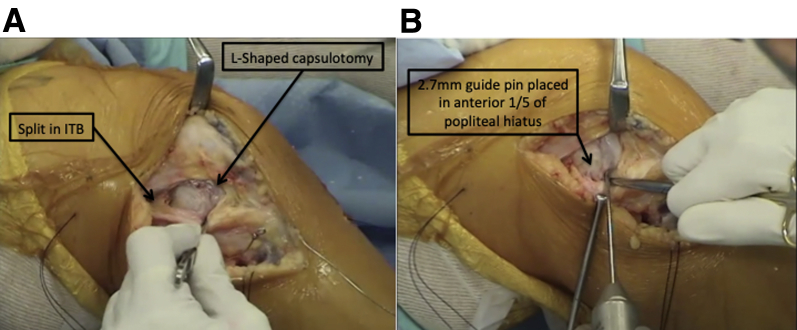
The proximal attachment of the FCL and the insertion of the politeus tendon on the lateral femur are now identified. The iliotibial band is split at the level of the lateral epicondyle (Fig 6). An L-shaped capsulotomy is made at the articular margin of the anterior and distal femur to allow visualization of the popliteal sulcus and the insertion of the popliteus tendon. Remnants of the native popliteus tendon can be identified and whipstitched at this point for incorporation into the repair, if preferred. The popliteus inserts into the anterior fifth of the popliteal sulcus. A 2.7-mm drill-tipped pin is positioned at this point. With combined ACL and PLC reconstruction, it is recommended to aim 35° anteriorly16 and 30° proximally17 to avoid tunnel collision with the femoral tunnel of an anatomic ACL reconstruction or entry into the intercondylar notch. A socket with a depth of 25 mm and a diameter of 6 mm is then created with the drill.
Fig 6.
Right knee, lateral side, 90° of flexion. (A) The ITB is split at the level of the lateral epicondyle, and an L-shaped capsulotomy is made at the articular margin of the anterior and distal femur to allow visualization of the popliteal sulcus and insertion of the popliteus tendon. (B) A 2.7-mm drill-tipped pin is positioned into the anterior fifth of the popliteal sulcus. With combined anterior cruciate ligament and posterolateral corner reconstruction, it is recommended to aim 35° anteriorly16 and 30° proximally17 to avoid tunnel collision with the femoral tunnel of an anatomic ACL reconstruction or entry into the intercondylar notch. A 25-mm deep, 6-mm diameter socket is then drilled. (ITB, iliotibial band.)
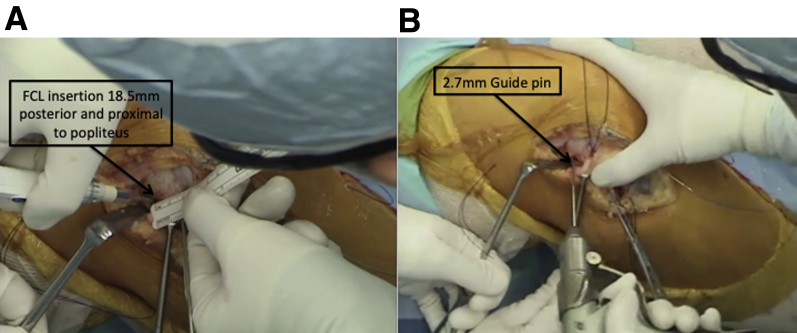
The FCL attachment is located just proximal and posterior to the lateral epicondyle, approximately 18.5 mm proximal to the popliteus tendon insertion (Fig 7). Tugging on the traction suture in the proximal FCL remnant helps identify this position. A 2.7-mm drill-tipped pin is positioned at this point and drilled parallel to the popliteus tunnel guide pin through the medial femoral cortex. This tunnel is reamed to 6 mm up to the medial cortex. Passing sutures are placed in both the FCL and popliteus femoral tunnels (Fig 8).
Fig 7.
Right knee, lateral side, 90° of flexion. (A) The FCL attachment is located just proximal and posterior to the lateral epicondyle, approximately 18.5 mm proximal to the popliteus tendon insertion. (B) A 2.7-mm drill-tipped pin is positioned at this point and drilled parallel to the popliteus tunnel guide pin through the medial femoral cortex. This tunnel is reamed to 6-mm up to the medial cortex. (FCL, fibular collateral ligament.)
Fig 8.
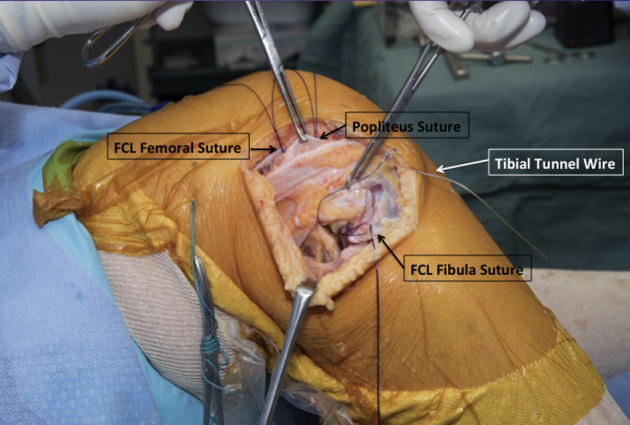
Right knee, lateral side, 90° of flexion. Passage of sutures in femoral and fibula tunnels and passage of wire loop in tibial tunnel. (FCL, fibular collateral ligament.)
With combined ACL and PLC reconstruction, we recommend that the ACL femoral tunnel be drilled before the femoral posterior cruciate ligament and popliteus tunnels. This allows arthroscopic visualization within the femoral ACL tunnel to ensure that the positions of the drill-tipped pins for the FCL and popliteus tunnel are satisfactory and that there has been no collision with the ACL femoral tunnel.
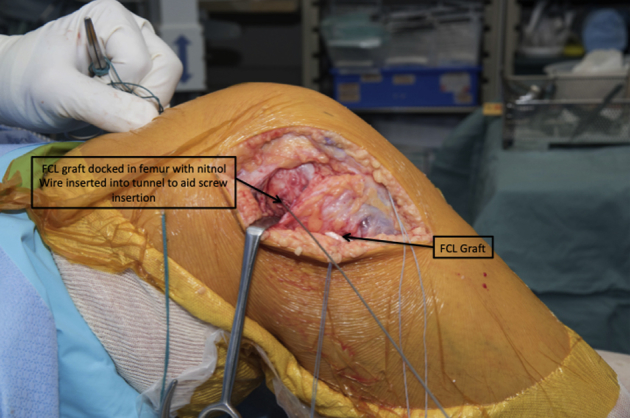
Passage of the semitendinosus graft and sequential fixation can now take place. One end of the graft is passed into the popliteus femoral socket, docked, and secured with a 7 × 25-mm Biosure PEEK (polyether ether ketone) interference screw (Smith & Nephew). The graft is then passed distally through the popliteal hiatus toward the posterolateral aspect of the tibia, exiting between the lateral heads of the gastrocnemius and soleus muscles (Fig 9). The graft is then passed through the loop of an Ultrabutton adjustable-loop fixation device. The graft is then passed through the fibula tunnel, after which the Ultrabutton is shuttled into the tibial tunnel using the traction sutures, from posterior to anterior, and flipped to engage on the anterior tibial cortex. With tension applied to the free end of the graft, the adjustable loop is shortened until the graft sits at the aperture of the tibial tunnel. A 3-cm mark is then placed on the graft from the anterolateral aperture of the fibula tunnel. The Ultrabutton is then tensioned, while a loop of graft is pulled into the tibial tunnel. Once the mark on the graft reaches the aperture of the fibula tunnel, it can be assumed that a 1.5-cm long loop of tendon has been secured in the tibial tunnel, thereby allowing the length of the FCL graft to be preserved.
Fig 9.
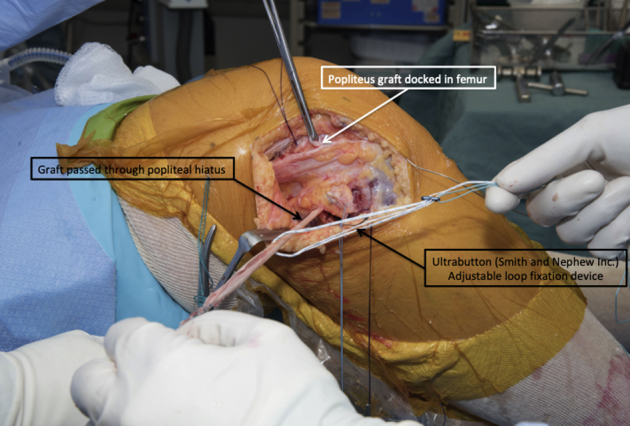
Right knee, lateral side, 90° of flexion. One end of graft is docked and fixed in the popliteus femoral tunnel and then passed through the popliteal hiatus exiting posterolateral to the fibula head. The graft is passed through the adjustable-loop device (Ultrabutton, Smith & Nephew).
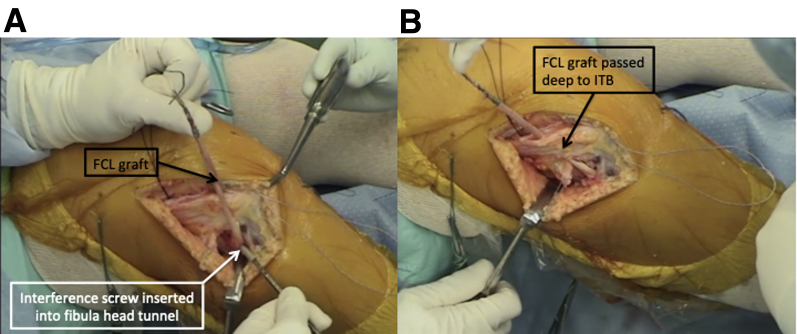
The graft is then tunneled deep to the superficial iliotibial band (but remaining superficial to the popliteus limb of the graft) and passed anteriorly and proximally toward the femoral FCL tunnel. Depending on the remaining length, further graft may be drawn into the tibial tunnel or the end can be rewhipstitched and cut to allow 25 to 30 mm of graft for docking and fixation within the FCL tunnel. The graft is then fixed in the fibula head with a 6 × 20-mm Biosure PEEK interference screw with the knee held at 70° of flexion and neutral tibial rotation (Fig 10). The free end of the graft is then passed into the FCL tunnel where tension is applied and the knee is cycled through a range of motion. Then, with the knee held at 30o of flexion with a valgus force applied, femoral fixation of the FCL graft is performed with a 7 × 25-mm Biosure PEEK interference screw (Fig 11). The popliteus and PFL limbs of the graft are then retensioned by using the Ultrabutton; slack in the graft is taken up into the tibial tunnel. Final tensioning of the popliteus and PFL elements of the graft is performed with the knee at 70o of flexion, ensuring neutral tibial rotation (Fig 12). Range of motion and stability are then checked to ensure that there has been no overconstraint. After final tensioning with the Ultrabutton has been done, the tensioning loop is cut and tied over the button.
Fig 10.
Right knee, lateral side, 70° of flexion. (A) The graft is then fixed in the fibula head with a 6 × 20-mm Biosure PEEK (Smith & Nephew) interference screw with the knee held at 70o of flexion and neutral tibial rotation. (B) The graft is then passed deep to the ITB. (FCL, fibular collateral ligament; ITB, iliotibial band.)
Fig 11.
Right knee, lateral side, 30° of flexion. After anterior cruciate ligament tibial fixation, the free end of the graft is pulled into the femoral tunnel at the FCL insertion. With the knee held at 30° of flexion, neutral rotation is done and a valgus stress is applied; a 7 × 25-mm interference screw is passed (Biosure PEEK, Smith & Nephew). (FCL, fibular collateral ligament.)
Fig 12.
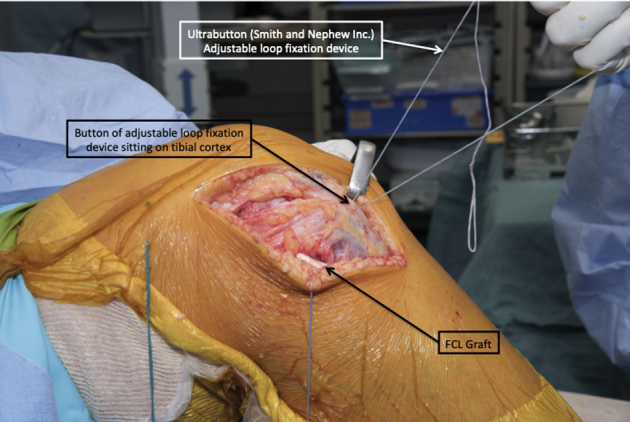
Right knee, lateral side, 70° of flexion. Final retensioning of the adjustable-loop device at 70° of flexion, neutral rotation, enabling differential tensioning on the FCL and popliteus/popliteofibular ligament limbs of the graft. (FCL, fibular collateral ligament.)
Wounds are then copiously irrigated and closed in the standard fashion. A postoperative hinged knee brace is applied while the patient is still under general anesthesia.
Postoperative Rehabilitation
The goals of rehabilitation are restoration of range of motion, management of swelling and pain, and early reactivation of muscles around the knee, without compromising the reconstruction. The patient is mobilized, with flat-foot-feather touch weight bearing allowed, during the first 2 weeks with the postoperative brace knee set to allow 0o to 90o of flexion. At 2 weeks after the operation, partial weight bearing in the hinged knee brace can start, and range of motion may be increased out of the brace with isometric quads activation and gluteal stimulation exercises. From 6 to 12 weeks after the operation, the patient may progress to full weight bearing with commencement of active muscle strengthening within the brace and unrestricted range of motion when resting. From 12 weeks after the operation, use of the brace is discontinued, and further rehabilitation is directed toward ongoing muscle conditioning, return to work, and then progressive return to sporting activities at the 6- to 9-month stage after formal functional assessment. Adjustments to this suggested protocol will need to be made depending on whether there were additional procedures required within the knee (e.g., meniscal root repair or concomitant ACL/posterior cruciate ligament reconstruction).
Discussion
Anatomic reconstruction of the PLC addresses the 3 key functional structures that restrain varus and external rotation laxity: the FCL, the popliteus, and the PFL. The original description of this technique by LaPrade et al.11 advocated the use of 2 allografts for the reconstruction. We present a modification of this technique, which allows for the use of a single semitendinosus autograft but still allows differential tensioning of the FCL and PFL/popliteus component of the reconstruction. This technique may be particularly advantageous for surgeons who have limited access to allograft and may decrease donor site morbidity, potentially sparing the involvement of the contralateral limb. It may also be beneficial in the context of multiligament reconstruction. It is important for the single graft to have enough length, and we recommend a minimum of 25 cm. The patient should be prepared, and consent for use of additional grafts should be obtained if a single graft cannot be used.
A similar modification of the technique, in which a fixed Endobutton device is used, has been described in the literature.14 When this method is used, all grafts must be tensioned and fixed with the knee in 1 position. The benefit of using an adjustable-loop device is that the PFL and popliteus grafts can be retensioned after initial fixation and cycling of the knee. This allows for the removal of creep from the system, potentially ensuring a more stable fixation. Additionally, the ability to tension the different limbs independently of the graft allows the knee to be optimally positioned for fixation of the FCL, popliteus, and PFL components.
The main limitation of this technique is the length of semitendinosus graft, which should be a minimum of 25 cm. If the tendon is found to be shorter, we recommend performing an anatomic reconstruction with 2 separate grafts as originally described by LaPrade et al.11 This can be performed with a second contralateral semitendinosus autograft if available, with the addition of 2 gracilis tendon autografts, or with allograft.
The main risks associated with the procedure are those pertaining to any PLC reconstruction including the following:
-
•
Common peroneal nerve palsy: This may be mitigated by first exploring, decompressing, and translating the nerve away from the surgical field.
-
•
Fibula head fracture: Care must be taken when drilling the fibula head tunnel to ensure that there is adequate bone posteriorly to avoid inadvertent breakthrough of the tunnel into the posterolateral cortex. Use of a small-diameter drill and a smaller interference screw (6 mm) also helps to reduce this risk.
-
•
Femoral tunnel coalition: Tunnel coalition may occur during femoral tunnel drilling, particularly with respect to the ACL femoral tunnel. To avoid coalition, the PLC femoral tunnels are drilled in a direction 35° anterior and 30° proximal to the coronal plane. The arthroscope may be introduced into the knee after pin insertion to verify that no coalition exists before full tunnel drilling is done.
In conclusion, this technique of anatomic PLC reconstruction enables the use of a single graft while allowing for differential tensioning of the FCL and popliteus/popliteofibular components of the reconstruction.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.G. receives research funding from ISAKOS and Smith and Nephew and is a consultant for Smith & Nephew. J.R. receives research funding from Smith and Nephew and is a consultant for Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video demonstrates a right knee combined anterior cruciate ligament reconstruction (bone–patellar tendon–bone autograft) with an anatomic posterolateral corner reconstruction utilizing a single semitendinosus autograft with adjustable-loop suspensory fixation in the tibial tunnel to enable differential tensioning of the popliteus and popliteofibular ligament grafts in relation to the fibular collateral ligament graft. The patient is placed in a supine position with a lateral thigh post and 2 footrests to allow stable flexion at 90° and 120°. A pneumatic tourniquet is applied and inflated throughout the procedure.
References
- 1.Amis A.A., Bull A.M.J., Gupte C.M., Hijazi I., Race A., Robinson J.R. Biomechanics of the PCL and related structures: Posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003;11:271–281. doi: 10.1007/s00167-003-0410-7. [DOI] [PubMed] [Google Scholar]
- 2.Gollehon D.L., Torzilli P.A., Warren R.F. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69:233–242. [PubMed] [Google Scholar]
- 3.LaPrade R.F., Ly T.V., Wentorf F.A., Engebretsen L. The posterolateral attachments of the knee. Am J Sports Med. 2003;31:854–860. doi: 10.1177/03635465030310062101. [DOI] [PubMed] [Google Scholar]
- 4.Chahla J., Moatshe G., Dean C.S., Laprade R.F. Posterolateral corner of the knee: Current concepts. Arch Bone Joint Surg. 2016;97:97–103. [PMC free article] [PubMed] [Google Scholar]
- 5.Djian P. Posterolateral knee reconstruction. Orthop Traumatol Surg Res. 2015;101:S159–S170. doi: 10.1016/j.otsr.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 6.Fanelli G.C., Giannotti B.F., Edson C.J. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy. 1996;12:521–530. doi: 10.1016/s0749-8063(96)90189-9. [DOI] [PubMed] [Google Scholar]
- 7.Clancy W.G.J., Shelbourne K.D., Zoellner G.B., Keene J.S., Reider B., Rosenberg T.D. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg Am. 1983;65:310–322. [PubMed] [Google Scholar]
- 8.Noyes F.R., Barber-Westin S.D. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med. 1996;24:415–426. doi: 10.1177/036354659602400404. [DOI] [PubMed] [Google Scholar]
- 9.Larson R.V. Isometry of the lateral collateral and popliteofibular ligaments and techniques for reconstruction using a free semitendinosus tendon graft. Oper Tech Sports Med. 2001;9:84–90. [Google Scholar]
- 10.Arciero R.A. Anatomic posterolateral corner knee reconstruction. Arthroscopy. 2005;21:1147.e1–1147.e5. doi: 10.1016/j.arthro.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 12.Serra Cruz R., Mitchell J.J., Dean C.S., Chahla J., Moatshe G., LaPrade R.F. Anatomic posterolateral corner Reconstruction. Arthrosc Tech. 2016;5:e563–e572. doi: 10.1016/j.eats.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geeslin A.G. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: A prospective case series and surgical Technique. J Bone Joint Surg. 2011;93:1672. doi: 10.2106/JBJS.J.01639. [DOI] [PubMed] [Google Scholar]
- 14.Franciozi C.E., Albertoni L.J.B., Gracitelli G.C. Anatomic posterolateral corner reconstruction with Autografts. Arthrosc Tech. 2018;7:e89–e95. doi: 10.1016/j.eats.2017.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.James E.W., LaPrade C.M., LaPrade R.F. Anatomy and biomechanics of the lateral side of the knee and surgical implications. Sports Med Arthrosc. 2015;23:2–9. doi: 10.1097/JSA.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 16.Moatshe G., Brady A.W., Slette E.L. Multiple ligament reconstruction femoral tunnels. Am J Sports Med. 2017;45:563–569. doi: 10.1177/0363546516673616. [DOI] [PubMed] [Google Scholar]
- 17.Gelber P.E., Erquicia J.I., Sosa G. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: Computed tomography evaluation in a cadaveric model. Arthroscopy. 2013;29:257–265. doi: 10.1016/j.arthro.2012.08.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video demonstrates a right knee combined anterior cruciate ligament reconstruction (bone–patellar tendon–bone autograft) with an anatomic posterolateral corner reconstruction utilizing a single semitendinosus autograft with adjustable-loop suspensory fixation in the tibial tunnel to enable differential tensioning of the popliteus and popliteofibular ligament grafts in relation to the fibular collateral ligament graft. The patient is placed in a supine position with a lateral thigh post and 2 footrests to allow stable flexion at 90° and 120°. A pneumatic tourniquet is applied and inflated throughout the procedure.