Abstract
Investigating the prescribing trend is important to improve rational prescribing. This study aimed at assessing the cardiovascular drug use, pattern, and its impact on clinical outcome. A cross‐sectional study was employed in the outpatient department of chronic illness clinic of Gondar University specialized hospital, Ethiopia from 15 January 2017 to 15 March 2017. The independent variables were sociodemographic, medication, and other clinical information while cardiovascular disease improvement is the outcome variable. Binary logistic regression was used to test the association between the independent variables and the outcome variable. Kaplan Meier curve was used to analyze the clinical improvement while the Log‐rank test was employed to compare the clinical outcome with the number of medications. Eight hundred thirty‐three cardiovascular patient medical records were included in the final analysis. The majority (62.5%) of patients were females and more than 61% were above 50 years of age. Diuretics monotherapy accounted for a third (33.6%) of cardiovascular drug use, followed by combination therapy of angiotensin convertase enzyme inhibitors with Diuretics (21.8%) and calcium channel blockers with diuretics (8.3%). Cardiovascular patients followed for 72 months found to have a good level of clinical improvement on combination medication (Log Rank of 28.9, P = 0.000). In this study, diuretics monotherapy or in combination with angiotensin convertase enzyme inhibitors were found to be the frequently prescribed drugs in cardiovascular patients. Combination therapy has an implication for good cardiovascular improvement on long term follow‐up. It seems clinicians were restricted to certain cardiovascular medications while plenty of choices are available from the diverse classes of cardiovascular drugs.
Keywords: cardiovascular disease, clinical outcome, drug use, ethiopia, prescribing pattern
Abbreviations
- CI
confidence interval
- CVD
cardiovascular disease
- GUSH
Gondar university Specialized hospital
- SPSS
Statistical Package for Social Sciences
1. INTRODUCTION
Cardiovascular disease (CVD) is a major health problem throughout the world and a common cause of early morbidity and mortality. In 2015, estimated 422.7 million CVD cases and 17.92 million CVD deaths have been occurred globally. In sub‐Saharan Africa more than 1 million deaths per year and nearly half million deaths per year have been predicted in eastern Africa.1 CVDs have emerged as the leading cause of mortality in developing countries accounting for 80% of cardiovascular deaths and responsible for the significant number of medical admissions in hospitals.2, 3, 4 Ethiopia is in the state of epidemiological transition from communicable to noncommunicable diseases, and the recent surge in cardiovascular disorders is one that requires a rapid and adequate public health response.5 Cardiovascular patients are taking a single medication or combination therapies to control and slowdown the progression of their illness. Cardiovascular drugs are among the most complicated groups of drugs due to overlapping indication, equivalent therapeutic effectiveness and side effects.6 Wide ranges of cardiovascular medications have been used to manage CVDs including, antihypertensives, lipid‐lowering agents, and drugs that ameliorate heart failure.3
Appropriate drug selection and use are crucial to achieving the desired treatment outcomes in various disease state management including CVD. Rational drug use is described by WHO as “Patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and their community”. Therefore, prescribers, dispensers, and users themselves should ensure proper drug use that meets the patient need correctly.7, 8, 9, 10 Irrational prescribing is one of the malpractices observed during the treatment of cardiovascular disorders. This had been expressed in terms of unjustified drug selection, inappropriate dose, duration, and frequency. Patients faced additional expenditures from unnecessary drug therapy, improper drug selection or adverse drug events of medication with the wrong indication apart from the direct costs.11, 12
There is quiet controversy on multiple drug therapy indication in cardiovascular patients. The ongoing suggestion is to use multiple drug combination therapy to manage CVDs and for the prevention of cardiovascular events in high‐risk groups.13 In contrary, others argue the combination drug therapy is disregarding the lifestyle modifications for CVDs and still believing in prioritizing lifestyle modification as optimal CVD management and risk prevention.14, 15
It is proven that both cardiovascular drug therapy and lifestyle modifications are important measures to reduce CVD progression and mortality.3 Inappropriate use of drugs is the most critical problem in developing countries either at the setting of relatively better health facilities like teaching hospitals or resource‐limited health facilities such as general hospitals and health centres where health professionals are scarce. Low economic statuses, illiteracy, lack of skilled clinical experts, and unavailability of drugs have been associated with poor medication selection and utilization.9 The trend of prescribing practices and pattern of drug utilization in CVD patients is partly based on physicians own perception, perspective, prior experience, and attitude towards a certain class of medication.16 The reported reasons for irrational prescribing in the Ethiopian context were acquired habits of physicians, patients demand, lack of drug information, and peer norms.17 Patients had their own medication preference based on their previous experience and associating efficacy with a certain brand of medicine.18, 19, 20 Besides these, patients also fail to clearly inform their medical condition and medication experience in developing countries which have their own contribution to inappropriate drug use. This is attributed to some cultural and social taboos that prohibit transparency and disclosure to clinicians. These clinicians’ traditional trend should be replaced by the clinical guideline recommendations to change the prescribing practice for better patient outcomes since guideline recommendations are better supported by clinical evidence and superior to individual preferences.20, 21
Different studies conducted in various countries revealed that the pattern of cardiovascular drugs used was identified as erratic and varies across the countries. The variability and inconsistency among those studies might be reasonable due to variation in geographical location, disease pattern, patient preferences, and drug selection. Nonetheless, it can be an indicator to arbitrary and irregular use of the cardiovascular drugs.8, 22, 23, 24, 25, 26, 27 Appropriate prescribing, proper medication selection and use have a positive implication on medication adherence and CVD improvement. There is a paucity of data on the prescribing practice, selection, and utilization of cardiovascular drugs in Ethiopia. This study was intended to provide information on prescribing trend and drug use pattern of cardiovascular patients in a tertiary care teaching hospital of Ethiopia. We aimed at assessing the drug use pattern and medication effect on cardiovascular outcomes in outpatient chronic illness clinic of Gondar University specialized hospital, Northwestern Ethiopia.
2. MATERIALS AND METHODS
2.1. Study setting and design
The study setting is located 737 km, northwest from the capital city of Addis Ababa, Ethiopia, which is the largest hospital in the region. The hospital is selected since it is convenient for data collection and the only hospital in northwestern Ethiopia having the chronic illness clinic of CVDs and other noncommunicable diseases. It is a teaching hospital staffed with diverse expertise from senior specialists in internal medicine, general practitioners to nurses, and other health professionals.28
An institution‐based retrospective cross‐sectional study was employed to evaluate the use and prescribing trend of cardiovascular drugs. It was conducted in Gondar university Specialized hospital (GUSH), North West Ethiopia during 15 January 2017 to 15 March 2017. Eligible Patient medical cards based on the inclusion criteria were reviewed for drug classes, generic name, indication, frequency, duration, and follow‐up period.
2.2. Study population
All patients diagnosed to have CVDs and visited Gondar University Specialized Hospital from January 2011 to December 2016 were the source population. Those patients whose medical records were available were the study population.
2.3. Inclusion and exclusion criteria
The study included all patients diagnosed with CVDs and had the follow‐up from January 2011 to December 2016. Patient medical records with incomplete information, patient age below 20 years and lost patient medical records were excluded from the study.
2.4. Data collection, quality control, and management
Data were collected retrospectively from patient medical records by trained 4 data collectors (4 pharmacists). The patient medical records were traced back using their card number from a cardiovascular patient's registration book. The data collection form contains socio‐demographics of the patient (age, sex, residence), year of registration, patient diagnosis, name and class of medication, dose frequency, duration, and the clinical status of the patient on the last follow‐up. The data collectors were getting 1 training regarding the data extraction procedures, keeping the best data quality and what components to extract from the medical records during data collection. The data collection checklist was pretested prior to the actual data collection in 50 patient medical records to check for the validity of consisting of adequate data abstraction formats for drug use and prescription patterns of CVDs. The principal investigator was supervising regularly to check the completeness of each data collection checklist. The collected data were checked for validity and consistency difference among data collectors. Data collection checklists with incomplete and unreliable data were discarded from the final analysis.
2.5. Data analysis
Data were entered and analyzed using Statistical Package for Social Sciences (SPSS) version 20 for analysis. Descriptive statistics were used to describe the sociodemographic characteristics of the patients; medical diagnosis, drug use patterns, durations, and clinical status on the last follow‐up. Binary logistic regression was employed to test the association between the independent variables and the outcome variable. Kaplan Meier curve was used to analyze the clinical improvement of CVDs. Log‐rank test was used to compare the clinical improvement with the number of medications. P value less than 0.05 and 95% confidence interval (CI) were used as cutoff points for determining the statistical significance of associations among different variables.
2.6. Operational definitions
Cardiovascular diseases: is a general category of diseases that affect the heart and circulatory system. It includes hypertension, heart failure, stroke, ischemic heart disease, rheumatic heart disease, hypertensive heart disease, arrhythmia, dyslipidemia, congenital and degenerative heart diseases.
Patients’ clinical status on last follow‐up will be classified as improved or not improved (poor) based on the following definitions.
Improved: patients had better prognosis by the physician assessment described as good or fair both clinically and in laboratory parameters (signs and symptoms resolved, and other diagnostic parameters improvement or better than initial diagnosis and the previous follow‐up),
Poor (not improved): there was poor or no prognosis at all or patient clinical conditions might have become worse.
2.7. Ethical approval
Ethical clearance was obtained from the ethical review committee of the college of medicine and health sciences, University of Gondar. Permission letter was requested from the clinical director of Gondar University Specialized Hospital and the head of internal medicine was informed before data collection. In addition to these, individual patient data were kept anonymous and confidential by ensuring data taken from medical records were not including any personal identifiers and used only for the purpose of this study.
3. RESULT
3.1. Sociodemographic characteristics
Of 1091 cardiovascular patient medical records, 833 were included in the final analysis with the remaining removed due to incomplete availability of data. 62.5% of patients were females and more than 61% were above 50 years of age. Most of the patients had 3 years (25%), 2 years (29.9%), and 1 year (22.5%) follow‐up in the clinic. The majority (41.1%) of patients had a 2‐month appointment for the next follow‐up (Table 1).
Table 1.
Sociodemographic characteristics of cardiovascular patients of GUSH, 2017 (N = 833)
| Variables | N (%) | |
|---|---|---|
| Age | 21‐30 | 90 (10.8) |
| 31‐40 | 108 (13) | |
| 41‐50 | 126 (15.1) | |
| 51‐60 | 200 (24) | |
| 61‐70 | 179 (21.5) | |
| Above 70 | 130 (15.6) | |
| Sex | Male | 312 (37.5) |
| Female | 521 (62.5) | |
| Year of registration | 2011 | 145 (17.4) |
| 2012 | 151 (18.1) | |
| 2013 | 68 (8.2) | |
| 2014 | 138 (16.6) | |
| 2015 | 144 (17.3) | |
| 2016 | 187 (22.4) | |
| Follow‐up period | 1 year | 188 (22.5) |
| 2 years | 249 (29.9) | |
| 3 years | 208 (25) | |
| 4 years | 67 (8.1) | |
| 5 years | 74 (8.8) | |
| 6 years | 47 (5.6) | |
| Duration of appointment | Below 1 month | 65 (7.8) |
| 1 month | 293 (35.1) | |
| 2 months | 342 (41.1) | |
| 3 months | 133 (16) | |
3.2. Cardiovascular disease distribution and improvement
Two‐thirds of cardiovascular patients are hypertensive, followed by heart failure and rheumatic valvular heart disease 9.7% and 7.3%, respectively. Most of the patients (86.6%) had good improvement in the last follow‐up as assessed by their physicians. (Table 2).
Table 2.
Cardiovascular disease pattern of patients by diagnosis, GUSH, 2017. (N = 833)
| Diagnosis | Frequency n (%) |
|---|---|
| Hypertension | 544 (65.3) |
| Heart failure | 81 (9.7) |
| CRVHD | 61 (7.3) |
| Ischemic heart disease | 18 (2.2) |
| Stroke | 11 (1.3) |
| Arrhythmia | 26 (3.1) |
| Dyslipidemia | 4 (0.4) |
| DVHD | 16 (1.9) |
| Cor‐Pulmonale | 13 (1.6) |
| Heart failure + Ischemic heart disease | 5 (0.6) |
| CRVHD + heart failure | 14 (1.7) |
| DVHD + heart failure | 11 (1.3) |
| Heart failure + Dilated cardiomyopathy | 21 (2.5) |
| Arrhythmia + CRVHD | 8 (1) |
| Outcome | |
| Improved | 721 (86.6) |
| Not improved | 112 (13.4) |
Abbreviations: CRVHD, chronic rheumatic valvular heart disease; DVHD, degenerative valvular heart disease.
3.3. Pattern of cardiovascular drug use
Diuretics monotherapy accounted for a third (33.6%) of cardiovascular drug use, followed by combination therapy of angiotensin convertase enzyme inhibitors and diuretics (21.8%) and calcium channel blockers with diuretics (8.3%) (Table 3).
Table 3.
Distribution of cardiovascular drugs pattern by pharmacologic class in GUSH, 2017 (N = 833)
| Class of drugs | Frequency n (%) |
|---|---|
| Diuretics | 280 (33.6) |
| ACEI | 53 (6.4) |
| CCBs | 50 (6) |
| B‐blocker | 5 (0.6) |
| ACEI + Diuretics | 182 (21.8) |
| ACEI + CCBs | 17 (2) |
| Diuretics + B‐Blockers | 33 (4) |
| CCB + Diuretics | 68 (8.2) |
| Digoxin + Diuretics | 15 (1.8) |
| Statin + Diuretics | 7 (0.8) |
| CCB + B‐blocker + Diuretics | 15 (1.8) |
| Digoxin + Diuretics +ACEI | 12 (1.4) |
| ACEI + Diuretics + B‐Blocker | 10 (1.2) |
| Aspirin + Digoxin + Diuretics | 20 (2.4) |
| Warfarin + Digoxin + B‐blocker | 10 (1.2) |
| Warfarin + Statin + Diuretics + B‐blocker | 39 (4.7) |
| CCB + Aspirin + ACEI + Statin | 8 (1) |
| ACEI + B‐blocker + Statin + Diuretics + Aspirin | 9 (1.1) |
Abbreviations: ACEI, Angiotensin convertase enzyme inhibitors; CCB, Calcium channel blocker.
Hydrochlorothiazide is the single most commonly prescribed monotherapy followed by Enalapril and Nifedipine, 18.1%, 6.4% and 4.8%, respectively. Hydrochlorothiazide with enalapril (16.2%) and furosemide with spironolactone (11.9%) were the frequently used combined therapies in cardiovascular patients. 8.2% of patients have more than four drugs in their treatment regimens. (Table 4).
Table 4.
Cardiovascular drug use pattern at the outpatient department of GUSH, 2017 (N = 833)
| Name of the drug | Frequency (%) |
|---|---|
| Hydrochlorothiazide (HCT) | 151 (18.1) |
| Furosemide | 30 (3.6) |
| Enalapril | 53 (6.4) |
| Nifedipine | 40 (4.8) |
| Amlodipine | 10 (1.2) |
| Atenolol | 5 (0.6) |
| Atorvastatin + HCT | 7 (0.8) |
| Furosemide + Spironolactone | 99 (11.9) |
| HCT + Enalapril | 135 (16.2) |
| Furosemide + Enalapril | 47 (5.6) |
| HCT + Nifedipine | 68 (8.2) |
| HCT + atenolol | 15 (1.8) |
| Enalapril + Nifedipine | 17 (2) |
| Nifedipine + Atenolol + HCT | 15 (1.8) |
| Digoxin + Furosemide | 15 (1.8) |
| Furosemide + Spironolactone + Atenolol | 18 (2.2) |
| HCT+ Enalapril + Atenolol | 10 (1.2) |
| Enalapril + Furosemide + Digoxin | 12 (1.4) |
| Warfarin + Atenolol + Digoxin | 10 (1.2) |
| Aspirin + Digoxin + Furosemide + Spironolactone | 20 (2.4) |
| Simvastatin + Warfarin + Spironolactone + Atenolol | 39 (4.7) |
| Amlodipine + Aspirin + Simvastatin + Enalapril | 8 (1) |
| Atenolol + Enalapril + Simvastatin + Aspirin + Spironolactone | 9 (1.1) |
3.4. Factors associated with cardiovascular diseases improvement
Being in the age group of 51‐60 years was found to be associated with good CVD improvement (the improvement is nearly 2.4 times of the age group of 21‐30 years) in 95% confidence interval with an adjusted odds ratio of (2.374 [1.148‐4.912]). Two‐month appointment period for follow‐up was found to reduce CVD improvement by 56.6% in 95% confidence interval with an adjusted odds ratio of 0.434 [0.225‐0.837] (P‐value = 0.013) (Table 5).
Table 5.
Binary logistic regression test for predictors of CVDs improvement at GUSH, 2017
| Variable | CVD improvement | Crude OR | P‐value | Adjusted OR | P‐value | |
|---|---|---|---|---|---|---|
| Good (%) | Poor (%) | |||||
| Sex | 0.343 | |||||
| Male | 267 | 45 | 1 | 0.522 | 1 | |
| Female | 454 | 67 | 1.142 (0.760‐1.715) | 1.232 (0.800‐1.898) | 0.343 | |
| Age | 0.015 | 0.035 | ||||
| 21‐30 | 71 (78.8) | 19 (21.2%) | 1 | 1 | ||
| 31‐40 | 97 (89.8) | 11 (10.2) | 2.360 (1.057‐5.269) | 0.036 | 2.170 (0.937‐5.024) | 0.071 |
| 41‐50 | 100 (79.4) | 26 (21.6) | 1.029 (0.529‐2.002) | 0.932 | 0.933 (0.459‐1.897) | 0.849 |
| 51‐60 | 181 (90.5) | 19 (9.5) | 2.549 (1.275‐5.096) | 0.008 | 2.374 (1.148‐4.912) | 0.020 a |
| 61‐70 | 159 (88.8) | 20 (11.2) | 2.127 (1.070‐4.231) | 0.031 | 1.851 (0.894‐3.831) | 0.097 |
| Above 70 | 113 (86.9) | 17 (13.1) | 1.779 (0.867‐3.649) | 0.116 | 1.581 (0.745‐3.353) | 0.233 |
| Follow‐up period | 0.18 | 0.21 | ||||
| 1 year | 164 (87.2) | 24 (12.8) | 1 | 1 | ||
| 2 years | 230 (92.4) | 19 (7.6) | 1.771 (0.702‐2.910) | 0.5 | 1.052 (0.502‐2.205) | 0.893 |
| 3 years | 177 (85.1) | 31 (14.9) | 0.835 (0.305‐1.106) | 0.324 | 0.447 (0.228‐0.876) | 0.29 |
| 4 years | 50 (74.6) | 17 (25.4) | 0.430 (0.134‐0.589) | 0.098 | 0.262 (0.122‐0.563) | 0.1 |
| 5 years | 63 (85.1) | 11 (14.9) | 0.838 (0.412‐2.739) | 0.3 | 0.815 (0.308‐2.154) | 0.680 |
| 6 years | 37 (78.7) | 10 (21.3) | 0.541 (0.298‐2.564) | 0.899 | 0.743 (0.248‐2.226) | 0.596 |
| Duration of appointment | 0.001 | 0.003 | ||||
| Below 1 month | 55 (84.6) | 10 (15.4) | 0.595 (0.465‐4.777) | 0.503 | 0.751 (0.370‐4.037) | 0.741 |
| 1 month | 271 (92.5) | 22 (7.5) | 1.334 (0.525‐2.095) | 0.893 | 0.916 (0.449‐1.869) | 0.810 |
| 2 months | 275 (80.4) | 67 (19.6) | 0.445 (0.236‐0.836) | 0.012 | 0.434 (0.225‐0.837) | 0.013 |
| 3 months | 120 (90.2) | 13 (9.8) | 1 | 1 | ||
OR, Odds ratio.
P‐value < 0.05
When cardiovascular patients were followed for 72 months, patients on combination medication found to have a good level of clinical improvement with Log Rank of 28.9, P = 0.000. (Figure 1).
Figure 1.
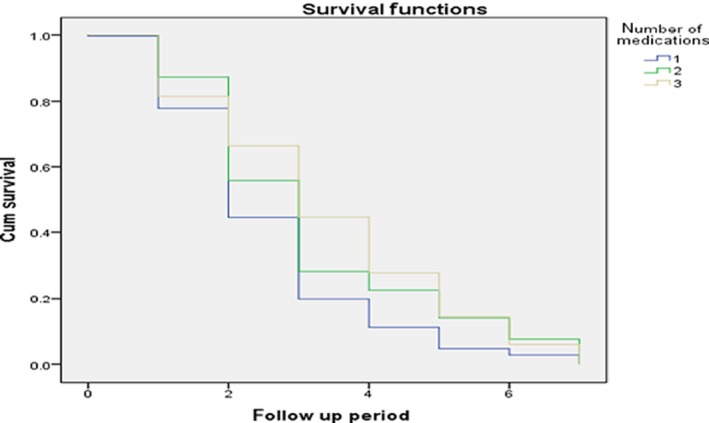
Kaplan Meier curve of clinical outcome of CV disorders over a mean follow‐up period of 72 months
4. DISCUSSION
This study presented the retrospective evaluation of the prescribing practices and patterns of cardiovascular drug use in the outpatient department of a University hospital in Ethiopia. Majority of the patients with CVDs in this study were females. Similarly, other studies in Ethiopia showed the proportion of females was higher in CVDs.5, 8, 26 More than 61% of the patients with CVDs are above 50 years of age, indicating that older age is associated with an increasing occurrence of CVDs. This is due to particularly cardiovascular risk factors rises in a parallel manner with age and age by itself is the nonmodifiable risk factor for CVDs. Modifiable risk factors and lifestyle changes to CVDs are compromised as age increment since aging is an irreversible physiologic process.29
More than three‐fourths of patients had at least 1‐3 years of follow‐up in the chronic illness clinic. Among those, nearly half of the patients had 1 month or less duration of appointment for follow‐up. Hypertension is the most common cardiovascular disorder followed by heart failure and rheumatic heart disease. This is similar to the pattern of CVDs in previous studies conducted in the same setting and other parts of Ethiopia.5, 30, 31, 32, 33 Proportionally highest numbers of patients are on diuretics monotherapy or diuretics‐based combination therapy. This showed that the majority of cardiovascular patients’ treatment relied on diuretics therapy. Hydrochlorothiazide is the most frequently used among diuretics class. This is plausibly acceptable as the Eighth Joint National Committee (JNC 8) recommendation since diuretics‐based treatment is the preferred first‐line treatment regimen for the black hypertensive patient in which Ethiopia belongs to.34 A study conducted to identify the recommended heart failure medications revealed that 56% of patients had diuretics in their prescription.18 The second commonly utilized diuretic in CVDs particularly in heart failure patients is Furosemide as other studies in the Netherlands showed that 80% of congestive heart failure patients were on loop diuretics.19
In this study hydrochlorothiazide monotherapy is commonly prescribed in nearly a fifth of patients followed by enalapril and nifedipine which is similar to previous studies conducted in Ethiopia and as per Ethiopian standard treatment guideline recommendations but different from the studies in India in which ACE inhibitor and calcium channel blocker monotherapy were the leading monotherapies while calcium channel blockers were the most frequently used drug classes followed by Angiotensin receptor blockers (ARBs) in China. This might attribute to patient differences in geographical location, physician, and patient preferences and Guideline recommendations.8, 16, 22, 24, 25, 26 Enalapril and hydrochlorothiazide take the foremost share of dual therapy followed by furosemide with spironolactone combination therapy. One Chinese study to determine the prescribing patterns in hypertension patients reported that ARBs and diuretics were frequent combinations while ARBs were not found to be used in Ethiopian patients 24, 35 Among triple therapies, no significant pattern use and difference were found in cardiovascular patients. Patients who are in more than four medicines were found to be on antiplatelet, anticoagulant, and lipid‐lowering agents. These patients are prone to drug interactions, adverse drug reactions, and complications. These polypharmacy prescriptions were found in elderly patients since the CVD incidence and complications rise as age increases.29
Most of the patients had good improvement on the last follow‐up of the appointment with their physician. This showed that patients responded to most of the dosage regimens selected for their disease indications. The cardiovascular drug use pattern of this study is more or less similar as per JNC 8 and Ethiopian treatment guideline recommendations and might be explanatory to the improvement of most patients. Patients in age group of 51‐60 were associated with good cardiovascular improvement as compared with patients in the age group between 21 and 30 years. This might be in the youngest age groups of developing countries like Ethiopia the frequent cardiovascular disorders are rheumatic heart diseases and valvular heart diseases which have a poor prognosis and less responsive to medications in the late young ages unless surgically intervened.36, 37, 38 Appointments for next follow‐up with 2‐month duration were related to the poor cardiovascular outcome. This could be justified as closer follow‐up with physicians (1 month and less) might result good assessment of patient compliance and disease prognosis while long appointment for follow‐up of the disease may fasten the progression of disease since they are prone to be lost and away from physicians’ follow‐up.5
In the present study, combination therapy found to have a good cardiovascular outcome on longer follow‐up as compared with single medication therapy. This can be elucidated as combination therapy can optimally control CVDs and prevent further risk of cardiovascular events. The working group on a summit on the combination therapy for CVD publicized that combination drug therapy along with appropriate lifestyle changes can bring an estimated reduction in CVD (70%‐80%).13 Therefore, combination therapy might benefit many individuals and suggested along with other preventive measures.39, 40, 41, 42
4.1. Limitation of the study
Even though it is showing the prescribing trends and cardiovascular drug use which can serve as a foundation for further researches, this was retrospective that could not consider the regimen changes, prognosis throughout the follow‐up period of patients and only reflected on the cardiovascular outcome of patients on the last follow‐up by their physician assessment. The outcome relied on physician assessment (secondary data) which is prone to interpersonal variability as it depends on physicians’ experience, the guideline he/she uses, work experience, expert lever (GP, senior). Moreover, this study used all cardiovascular drugs used as general and was not tried to relate factors explicitly with separate disease entities. Prospective researches on cardiovascular drug use and patterns peculiar to each CVD is warranted to further understand the implications and to evaluate the appropriateness of drug selection with the existing recommended clinical guidelines.
5. CONCLUSION
Diuretics monotherapy or in combination with angiotensin convertase enzyme inhibitors and diuretics combination therapy were the frequently used drugs in cardiovascular patients. Combination therapy found to have an implication for the good cardiovascular outcome on long term follow‐up. The prescribing practices to cardiovascular patients were only limited to specific drugs from Diuretics, ACEIs, and Calcium channel blockers and rarely to B‐blockers. It seems clinicians opt out to consider the diverse class of cardiovascular medications; the prescribing choice should not be limited to few pharmacological classes of cardiovascular drugs. Studying the prospective use of cardiovascular drugs with each CVD entity along with treatment guideline adherence will have paramount importance in the better understanding of compliance to clinical recommendations.
CONFLICT OF INTEREST
All authors declared no conflict of interest in this research.
AUTHOR CONTRIBUTIONS
YGT supervised and conceived the study, participating in the analysis and interpretations of the findings, drafting the manuscript and write up. TMA and TBA participated in data collection and analysis, ABM and MSK participated in data collection and interpretation of the findings. TMA edited the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the help of physicians, medical director, and the staffs in the medical record office of Gondar University specialized Hospital for facilitating access to the records of the patients.
Tefera YG, Abebe TB, Mekuria AB, Kelkay MS, Abegaz TM. Prescribing trend in cardiovascular patients at Ethiopian university hospital: The number of medications and implication on the clinical improvement. Pharmacol Res Perspect. 2019;e00474 10.1002/prp2.474
DATA AVAILABILITY
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
REFERENCES
- 1. Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization . Global status report on noncommunicable diseases World Health Organization. 2014.
- 3. Hommerson P, Nedeljkovic SI, Klungel OH, et al. Cardiovascular drug use and differences in the incidence of cardiovascular mortality in elderly Serbian men. Pharm World Sci. 2005;27:124‐128. [DOI] [PubMed] [Google Scholar]
- 4. Noor SK, Elmadhoun WM, Bushara SO, Ahmed MH. The changing pattern of hospital admission to medical wards: burden of non‐communicable diseases at a hospital in a developing country. Sultan Qaboos Univ Med J. 2015;15:e517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tefera YG, Abegaz TM, Abebe TB, Mekuria AB. The changing trend of cardiovascular disease and its clinical characteristics in Ethiopia: hospital‐based observational study. Vasc Health Risk Manag. 2017;13:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kesselheim AS, Misono AS, Lee JL, et al. Clinical equivalence of generic and brand‐name drugs used in cardiovascular disease: a systematic review and meta‐analysis. JAMA. 2008;300:2514‐2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shrank WH, Hoang T, Ettner SL, Glassman PA, Nair K, DeLapp D, et al. The implications of choice: prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med. 2006;166:332‐337. [DOI] [PubMed] [Google Scholar]
- 8. Abegaz TM, Tefera YG, Abebe TB. Antihypertensive drug prescription patterns and their impact on outcome of blood pressure in Ethiopia: a hospital‐based cross‐sectional study. Integr Pharm Res Pract. 2017;6:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mengistu A. Patterns of drug utilization in inpatients department, Jimma hospital south west Ethiopia. Ethiop J Health Sci. 2005;15:139‐145. [Google Scholar]
- 10. World Health Organization . Promoting rational use of medicines: core components. Geneva: World Health Organization; 2002. [Google Scholar]
- 11. Laing R, Hogerzeil H, Ross‐Degnan D. Ten recommendations to improve use of medicines in developing countries. Health Policy Plan. 2001;16:13‐20. [DOI] [PubMed] [Google Scholar]
- 12. Sisay M, Mengistu G, Molla B, Amare F, Gabriel T. Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: a cross sectional study. BMC Health Serv Res. 2017;17:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yusuf S, Attaran A, Bosch J, et al. Combination pharmacotherapy to prevent cardiovascular disease: present status and challenges. Eur Heart J. 2013;35:353‐364. [DOI] [PubMed] [Google Scholar]
- 14. Mulrow C, Kussmaul W. The middle‐aged and older American: wrong prototype for a preventive polypill? Ann Intern Med. 2005;142:467‐468. [DOI] [PubMed] [Google Scholar]
- 15. Trewby P, Trewby C. “Polypill” to fight cardiovascular disease: patients before populations. BMJ. 2003;327:807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Arief M, Harika B, Satyanarayana B, Pasha S, Paladugu N, Pashab S. Evaluation of prescribing pattern of antihypertensive drugs in a tertiary care hospital. Acta Chim Pharma Indica. 2013;3:172‐181. [Google Scholar]
- 17. Dilbato DD, Kuma ZG, Tekle‐Mariam S. A baseline survey on prescribing indicators and the underlying factors influencing prescribing in Southern Ethiopia. Ethiop J Health Dev. 1998;12:87‐94. [Google Scholar]
- 18. Koschack J, Jung H, Scherer M, Kochen M. Prescriptions of recommended heart failure medications can be correlated with patient and physician characteristics. Int J Clin Pract. 2009;63:226‐232. [DOI] [PubMed] [Google Scholar]
- 19. Bouvy ML, Heerdink ER, Leufkens HG, Hoes AW. Patterns of pharmacotherapy in patients hospitalised for congestive heart failure. Eur J Heart Fail. 2003;5:195‐200. [DOI] [PubMed] [Google Scholar]
- 20. Muhit MA, Rahman MO, Raihan SZ, et al. Cardiovascular disease prevalence and prescription patterns at a tertiary level hospital in Bangladesh. J Appl Pharm Sci. 2012;2:8. [Google Scholar]
- 21. Abegaz TM, Tefera YG, Befekadu Abebe T. Target organ damage and the long term effect of nonadherence to clinical practice guidelines in patients with hypertension: a retrospective cohort study. Int J Hypertens. 2017;2017:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. George J, Devi P, Kamath DY, Anthony N, Kunnoor NS, Sanil SS. Patterns and determinants of cardiovascular drug utilization in coronary care unit patients of a tertiary care hospital. J Cardiovasc Dis Res. 2013;4:214‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Khalid Labu Z, Sultana R, Bake A, Sikder K, Jahan K. Surveillance on prescribed cardiovascular drugs by generic names in Dhaka city of Bangladesh. Int J Pharm Life Sci. 2013;4:2511‐2520. [Google Scholar]
- 24. Cheng H. Prescribing pattern of antihypertensive drugs in a general hospital in central China. Int J Clin Pharm. 2011;33:215‐220. [DOI] [PubMed] [Google Scholar]
- 25. Dhanaraj E, Raval A, Yadav R, Bhansali A, Tiwari P. Prescription pattern of antihypertensive agents in T2DM patients visiting tertiary care centre in North India. Int J Hypertens. 2012;2012:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shukrala F, Gabriel T. Assessment of prescribing, dispensing, and patient use pattern of antihypertensive drugs for patients attending outpatient department of Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia. Drug Des Devel Ther. 2015;9:519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beg MA, Dutta S, Varma A, et al. A study on drug prescribing pattern in hypertensive patients in a tertiary care teaching hospital at Dehradun, Uttarakhand. Int J Med Sci Public Health. 2014;3:922‐927. [Google Scholar]
- 28. Gondar Univeristy Specialized hospital Statistics and Information Office. Annual Report on Health Services and Employees. 2017.
- 29. Silwer L. Public Health Aspects of Pharmaceutical Prescription Patterns: Exemplified by treatments for prevention of cardiovascular disease: Nordic School of Public Health NHV Göteborg, Sweden; 2007.
- 30. Habte B, Alemseged F, Tesfaye D. The pattern of cardiac diseases at the cardiac clinic of Jimma University specialised hospital, south West Ethiopia. Ethiop J Health Sci. 2010;20:99‐105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hodes RM. Pattern of heart disease in Ethiopia as seen in a cardiology referral clinic. Cardiology. 1988;75:458‐464. [DOI] [PubMed] [Google Scholar]
- 32. Mengistu MD. Pattern of blood pressure distribution and prevalence of hypertension and prehypertension among adults in Northern Ethiopia: disclosing the hidden burden. BMC Cardiovasc Disord. 2014;14:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Maru M. The changing pattern of cardiovascular diseases in Ethiopia. East Afr Med J. 1993;70:772‐776. [PubMed] [Google Scholar]
- 34. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507‐520. [DOI] [PubMed] [Google Scholar]
- 35. Authority FMHCAaC . Standard Treatment Guidelines for General Hospitals in Ethiopia. Addis Ababa, Ethiopia.: Ministry of Health; FMHACA; 2014.
- 36. Ntusi NB, Mayosi BM. Epidemiology of heart failure in sub‐Saharan Africa. Expert Rev Cardiovasc Ther. 2009;7:169‐180. [DOI] [PubMed] [Google Scholar]
- 37. Essop MR, Nkomo VT. Rheumatic and nonrheumatic valvular heart disease: epidemiology, management, and prevention in Africa. Circulation. 2005;112:3584‐3591. [DOI] [PubMed] [Google Scholar]
- 38. Kang D‐H, Kim JH, Rim JH, et al. Comparison of early surgery versus conventional treatment in asymptomatic severe mitral regurgitation. Circulation. 2009;119:797. [DOI] [PubMed] [Google Scholar]
- 39. Dehghan M, Mente A, Teo K, et al. Ongoing Telmisartan Alone and in Combination With Ramipril Global End Point Trial (ONTARGET)/Telmisartan Randomized Assessment Study in ACEI Intolerant Subjects With Cardiovascular Disease (TRANSCEND) Trial Investigators . Relationship between healthy diet and risk of cardiovascular disease among patients on drug therapies for secondary prevention: a prospective cohort study of 31 546 high‐risk individuals from 40 countries. Circulation. 2012;126:2705‐2712. [DOI] [PubMed] [Google Scholar]
- 40. Joshi R, Chow CK, Raju PK, et al. The rural Andhra Pradesh cardiovascular prevention study (RAPCAPS): a cluster randomized trial. J Am Coll Cardiol. 2012;59:1188‐1196. [DOI] [PubMed] [Google Scholar]
- 41. Critchley JA, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA. 2003;290:86‐97. [DOI] [PubMed] [Google Scholar]
- 42. Viera AJ, Sheridan SL, Edwards T, Soliman EZ, Harris R, Furberg CD. Acceptance of a polypill approach to prevent cardiovascular disease among a sample of US physicians. Prev Med. 2011;52:10‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.


