Abstract
Disorders of the long head biceps tendon are among the most challenging of shoulder problems to diagnose and manage. In this Technical Note, we introduce an arthroscopic technique for proximal biceps tenodesis high in the groove at the articular margin of the humeral head using a single anchor and 2 self-cinching loops followed by 5 alternating half-hitches to secure the construct. This method is simple and enables stable fixation of the biceps tendon.
Anatomically, the long head biceps tendon (LHBT) originates from the supraglenoid tubercle and the superior glenoid labrum and travels across the glenohumeral joint to enter the bicipital groove distally.1 The overall length of the biceps tendon from its origin to the articular margin of the humeral head is equal between men and women (approximately 25 mm).2 A recent cadaveric study has defined the fibro-osseous boundaries of the bicipital tunnel, which extend from the articular margin of the humeral head to the subpectoral space.3
The functional role of the LHBT in the shoulder has long been debated. Despite this ongoing debate, there is little controversy as to whether the LHBT is a source of shoulder pain (i.e., a pain generator).1, 4 The LHBT may be a source of shoulder pain for several reasons including (1) lesions of the biceps-labral complex (e.g., SLAP lesions), (2) tenosynovitis or tendinopathy, (3) instability (e.g., subluxation, dislocation, or pulley lesions),5, 6 and (4) tendon tears (partial or complete).1, 4 Such lesions of the LHBT are frequently associated with partial or complete rotator cuff tears. In cases of reparable and irreparable rotator cuff tears, both biceps tenotomy and tenodesis procedures seem equally effective in reducing shoulder symptoms when biceps pathology is observed intraoperatively7, 8; however, a more recent study has demonstrated better shoulder function and strength when a tenodesis is performed as compared with tenotomy.9
The purpose of this Technical Note is to present our technique for arthroscopic proximal biceps tenodesis high in the groove (i.e., at the articular margin of the humeral head) for the treatment of patients with symptomatic biceps pathology. This technique is simple, reproducible, and cost-effective.
Surgical Technique
Preoperative Evaluation
A thorough patient history is obtained, and clinical examination of both the LHBT and biceps-labral complex is performed, with attention given to common concomitant pathologies (e.g., torn rotator cuff).10, 11 Advanced imaging studies (i.e., magnetic resonance imaging) currently remain an unreliable and insensitive modality for ruling out biceps-labrum complex lesions including instability of the LHBT and cases in which the bicipital tunnel is affected.12, 13 These findings stress the importance of performing a complete physical examination and maintaining a high level of clinical suspicion during management of commonly associated pathologic conditions (e.g., anterosuperior rotator cuff tears).
Anesthesia and Patient Positioning
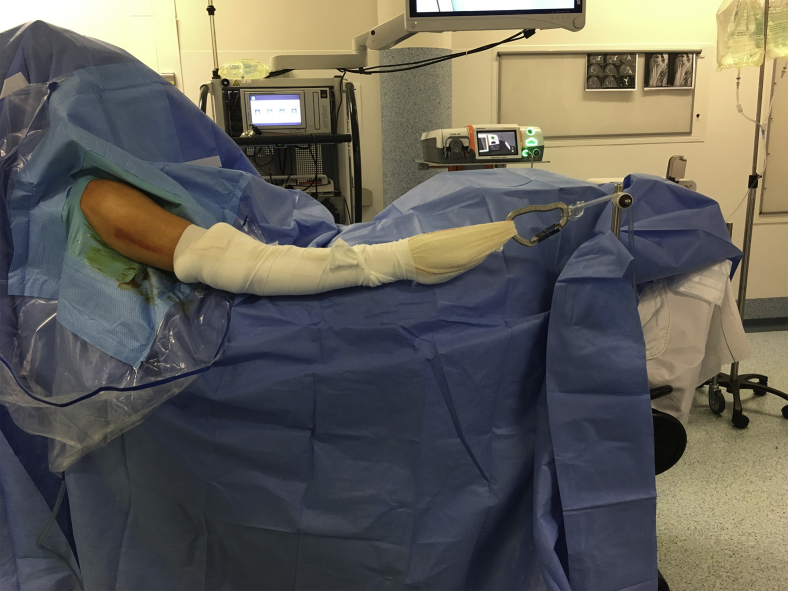
After induction of general anesthesia, the patient is positioned in the beach chair position with the head of bed at 60° to 70° of elevation. The affected arm is flexed 30° to 40° and placed in neutral rotation. Longitudinal traction (4 kg) is used to aid in distension of the subacromial and subdeltoid “working spaces” (Fig 1).
Fig 1.
Beach chair position with the head of bed in 60° to 70° of elevation and the shoulder in 30° to 40° of flexion with longitudinal traction (right shoulder).
Portal Placement
Surface landmarks are outlined, and a standard posterior viewing portal is created with a blunt trocar. An anterior rotator interval portal is developed by using an “outside-in technique” (i.e., with a spinal needle) to inspect the intra-articular LHBT. The arthroscope is then removed from the glenohumeral joint and placed in the subacromial (SA) space (i.e., through the same skin incision). While viewing posteriorly within the SA space, a lateral SA portal is established in line with the posterior aspect of the clavicle (i.e., the superior soft spot) and parallel to the undersurface of the acromion. Next, an anterosuperolateral portal (referred to as the anterolateral portal) is established 2 cm lateral to the anterolateral corner of the acromion, just anterior to the leading edge of the supraspinatus tendon and in line with the LHBT (Fig 2). While viewing from the posterior portal, a radiofrequency ablation device is introduced through the anterolateral portal into the SA space, and the deltoid fascia is released and then excised to obtain a panoramic view of the SA and subdeltoid spaces.14
Fig 2.
Position of arthroscopic portals (right shoulder). Portal 1, standard posterior portal; portal 2, lateral subacromial portal; portal 3, anterosuperolateral portal; portal 4, anterior (rotator interval) portal.
Tenodesis Technique
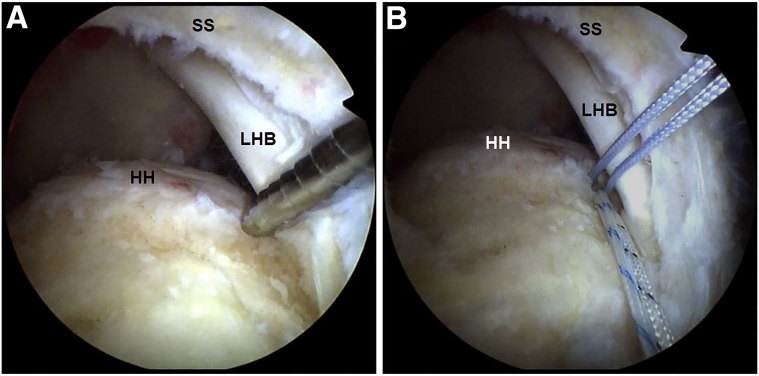
The procedure is performed with a 30° arthroscope after the intra-articular assessment of the LHBT has been completed. The rotator cuff footprint is first prepared while viewing within the glenohumeral joint and working through the anterolateral portal in an effort to protect the articular cartilage of the humeral head. Next, while viewing through the lateral SA portal, an anchor is placed next to the articular margin of the humeral head, in line with the LHBT (Y-Knot RC all-suture anchor; ConMed, Largo, FL) (Fig 3A, Video 1). Of note, most rotator cuff suture anchors can be used for this technique. Only 1 of the sutures loaded within the anchor is used for the tenodesis technique; the other sutures can be temporarily “docked” through the posterior portal (or exteriorized from the lateral cannula) and later used for the anterior supraspinatus tendon repair after the tenodesis procedure is performed (Fig 3B).
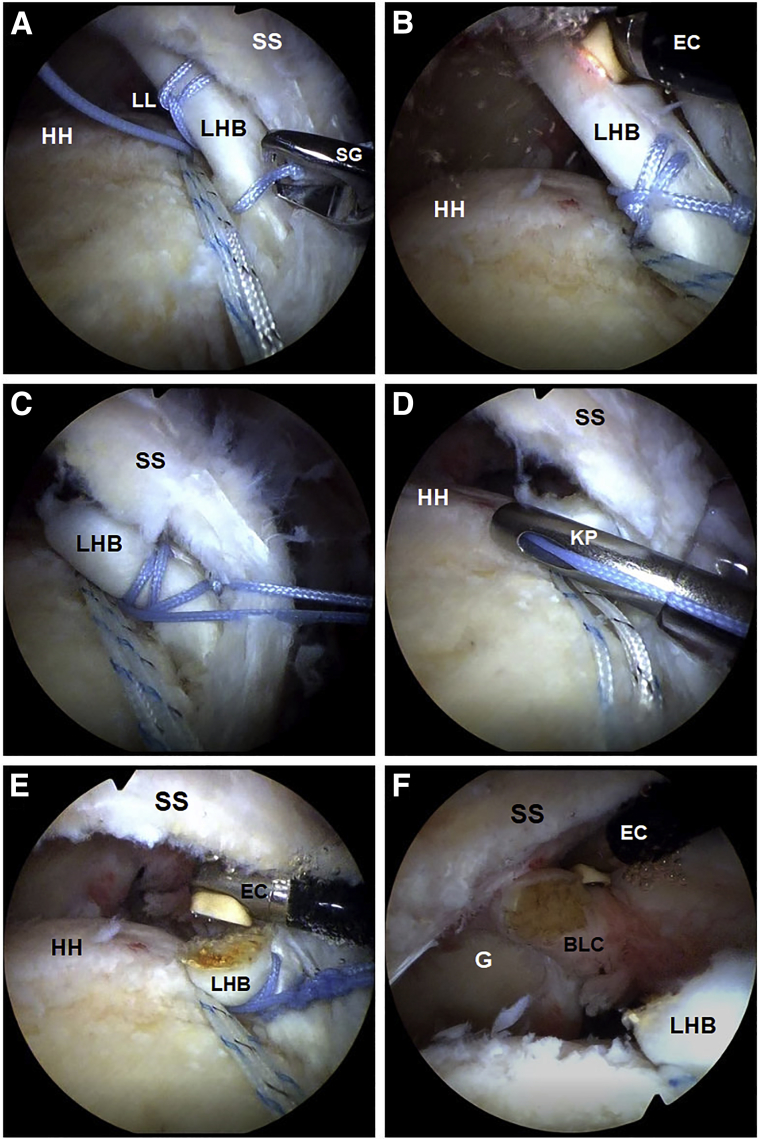
Fig 3.
Arthroscopic visualization of the right shoulder from the lateral subacromial portal with the patient in the beach chair position reveals a full-thickness, crescent-shaped supraspinatus tendon tear. (A) Position of the anchor adjacent to the articular margin of the humeral head in line with the long head biceps tendon. (B) After the anchor is inserted, 2 sutures are exteriorized outside the lateral cannula to be used after the tenodesis to repair the supraspinatus tendon tear. (HH, humeral head; LHB, long head biceps; SS, supraspinatus.)
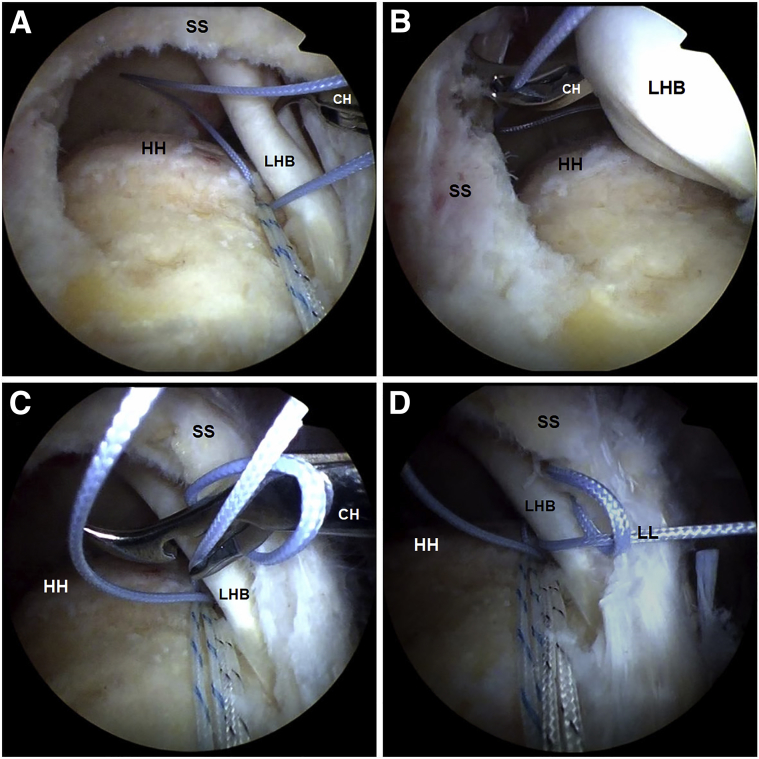
The first suture loop created within the LHBT is referred to as the “lasso-loop” stitch.15 A curved soft-tissue penetrator device, such as a 30° Cleverhook (DePuy Synthes, Raynham, MA), is used to create the lasso-loop stitch (curve to the right is used for the right shoulder and curve to the left for the left shoulder) (Fig 4). While viewing from the lateral portal, the surgeon uses an arthroscopic looped grasper, through the anterolateral cannula, to shuttle 1 of the 2 suture limbs into the glenohumeral joint (Fig 5A). The Cleverhook is then passed through the anterolateral cannula and through the center of the LHBT (i.e., from superior to inferior) just medial to the site of rotator cuff anchor insertion (Fig 5A). Using the Cleverhook, the surgeon grasps the midportion of the suture limb that was previously positioned within the joint and pulls the suture back through the LHBT, but not completely through, leaving a loop of suture exiting the superior surface of the tendon (Fig 5B). The tip of the Cleverhook is then passed through the loop so the surgeon can grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tensioned (Fig 5 C and D, Video 1).
Fig 4.
Cleverhook instrument (DePuy Synthes). (A) Right and left 30° curved configurations with a slim profile to pass down small (6-mm) cannulas. The Cleverhook's unique tip facilitates ease of penetration through the long head biceps tendon. (B) The spring-handle design maintains jaws in a closed position (located on posterior side of instrument) to enable easy retrieval of sutures.
Fig 5.
Arthroscopic visualization of the right shoulder from the lateral subacromial portal with the patient in the beach chair position revealing a full-thickness, crescent-shaped supraspinatus tendon tear and exposed humeral head. The anterolateral portal serves as the working portal through which to create the first self-cinching suture loop (i.e., lasso-loop). (A) After 1 suture limb has been shuttled into the joint, the tip of the Cleverhook (DePuy Synthes) is passed through the midportion of the long head biceps tendon. (B) The previously shuttled suture is grasped by using the jaw of the Cleverhook grasper. The suture is pulled back through the long head biceps tendon, but not completely through, leaving a loop of suture exiting the superior surface of the tendon. (C, D) The tip of the Cleverhook is then passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tightened to create the lasso-loop. (CH, Cleverhook; HH, humeral head; LHB, long head biceps; LL, lasso-loop; SS, supraspinatus.)
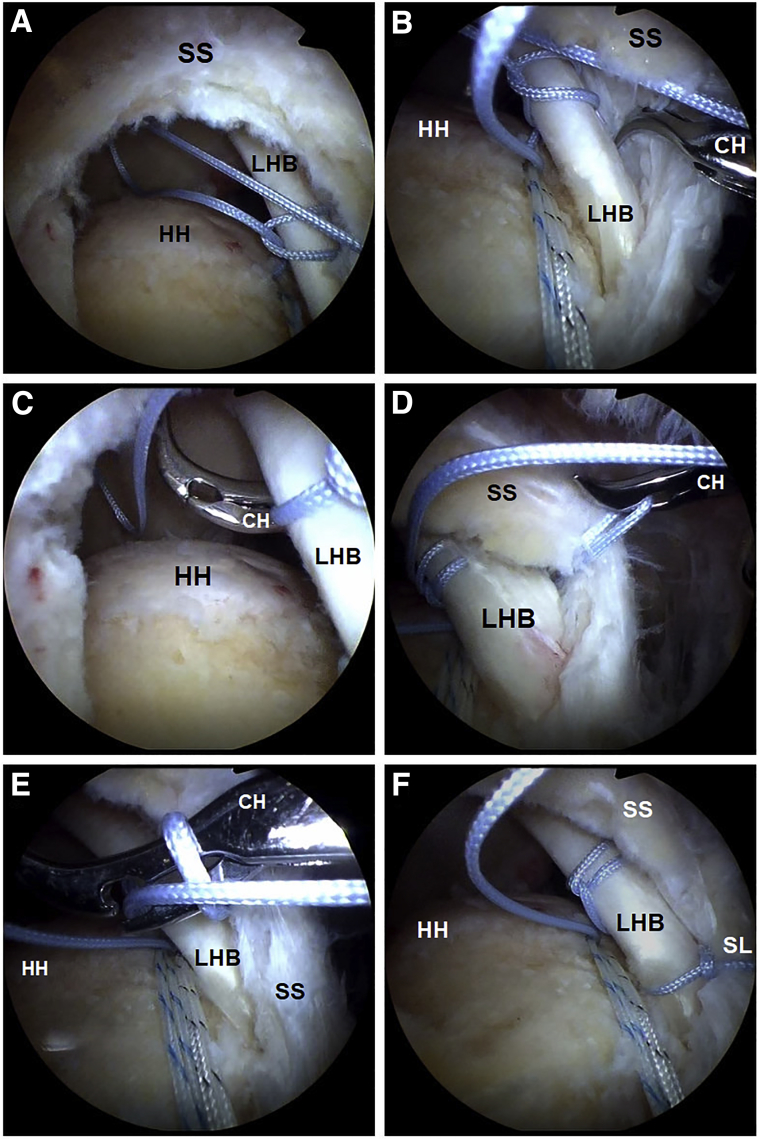
The surgeon starts the next suture loop, which is created to further secure the LHBT, by using a looped suture grasper to shuttle the same suture limb that was used to create the first loop back into the glenohumeral joint (Fig 6A). Next, the Cleverhook is placed around the anterior aspect of the tendon (from superior to inferior) (Fig 6B), continued under the tendon, and directed into the glenohumeral joint. The midportion of the suture limb that was previously positioned within the joint is grasped and pulled in the reverse direction back around the anterior aspect of the LHBT, leaving a loop of suture (Fig 6 C and D). The tip of the Cleverhook is similarly passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and out the anterolateral cannula to tighten the loop (Fig 6 E and F, Video 1). This second loop represents the modification of the “lasso-loop” tenodesis technique,15 which was originally described by 1 of the senior authors (C.L.D.); the end construct provides circumferential stabilization of the LHBT with 1 self-cinching lasso-loop on each side of the tendon (Fig 6F).
Fig 6.
Arthroscopic visualization of the right shoulder from the lateral subacromial portal with the patient in the beach chair position revealing a full-thickness, crescent-shaped supraspinatus tendon tear and exposed humeral head. The anterolateral portal serves as the working portal through which to create the second self-cinching suture loop. (A) A looped grasper is used to shuttle the same suture limb that was used to create the first loop into the joint. (B) The Cleverhook (DePuy Synthes) is passed around the anterior aspect and under the long head biceps tendon. (C, D) The midportion of the suture limb that was previously positioned within the joint is grasped and pulled in the reverse direction, leaving a loop of suture. (E, F) The tip of the Cleverhook is passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tightened to create the second self-cinching suture loop. (CH, Cleverhook; HH, humeral head; LHB, long head biceps; SL, suture loop; SS, supraspinatus.)
Before the tenodesis is secured, both suture limbs used for the tenodesis are retrieved into the anterolateral cannula. A looped suture grasper is used to reposition the second loop (i.e., lateral) in close proximity to the medially placed lasso-loop (Fig 7A). Next, an electrocautery device (or a pair of arthroscopic scissors) is used to perform the biceps tenotomy, medial to the previously placed suture loops (Fig 7B). While the suture end that does not pass through the LHBT (i.e., the post) is being pulled, the tendon is mobilized and reduced to the suture anchor (Fig 7C). Because of the configuration of the suture loops, sliding knots cannot be used. Half-hitch locking knots (i.e., reverse half-hitches or alternating posts) are used to secure the construct (Fig 7D). The electrocautery device is then used to remove residual medial LHBT tissue, adjacent to both the tenodesis construct and superior labrum (Fig 7 E and F, Video 1). Sufficient residual tissue proximal to the secured construct is removed such that this excess biceps tendon tissue does not cover the prepared rotator cuff footprint found just posterior to the biceps tenodesis. The previously docked sutures not used for the tenodesis can now be used to address associated lesions (e.g., an anterior supraspinatus tendon tear). A summary of the tenodesis technique described in this Technical Note is illustrated in Figures 8 and 9.
Fig 7.
Arthroscopic visualization of the right shoulder from the lateral subacromial portal with the patient in the beach chair position revealing a full-thickness, supraspinatus tendon tear and exposed humeral head. The anterolateral portal serves as the working portal. (A) A looped suture grasper is used to reposition the second (i.e., lateral) suture loop in close proximity to the medially placed lasso-loop along the length of the long head biceps tendon. (B) An electrocautery device is used to perform the biceps tenotomy, medial to the previously placed suture loops. (C) While the surgeon pulls on the suture end that does not pass through the long head biceps tendon (i.e., the post), the tendon is reduced to the suture anchor. (D) Half-hitch locking knots (i.e., reverse half-hitches or alternating posts) are used to secure the construct with a standard knot pusher. (E+F) The electrocautery device is then used to remove residual medial long head biceps tendon tissue, adjacent to both the tenodesis construct and superior biceps labrum complex. (BLC, biceps labrum complex; EC, electrocautery device; HH, humeral head; KP, knot pusher; LHB, long head biceps; LL, lasso-loop; SG, suture grasper; SS, supraspinatus.)
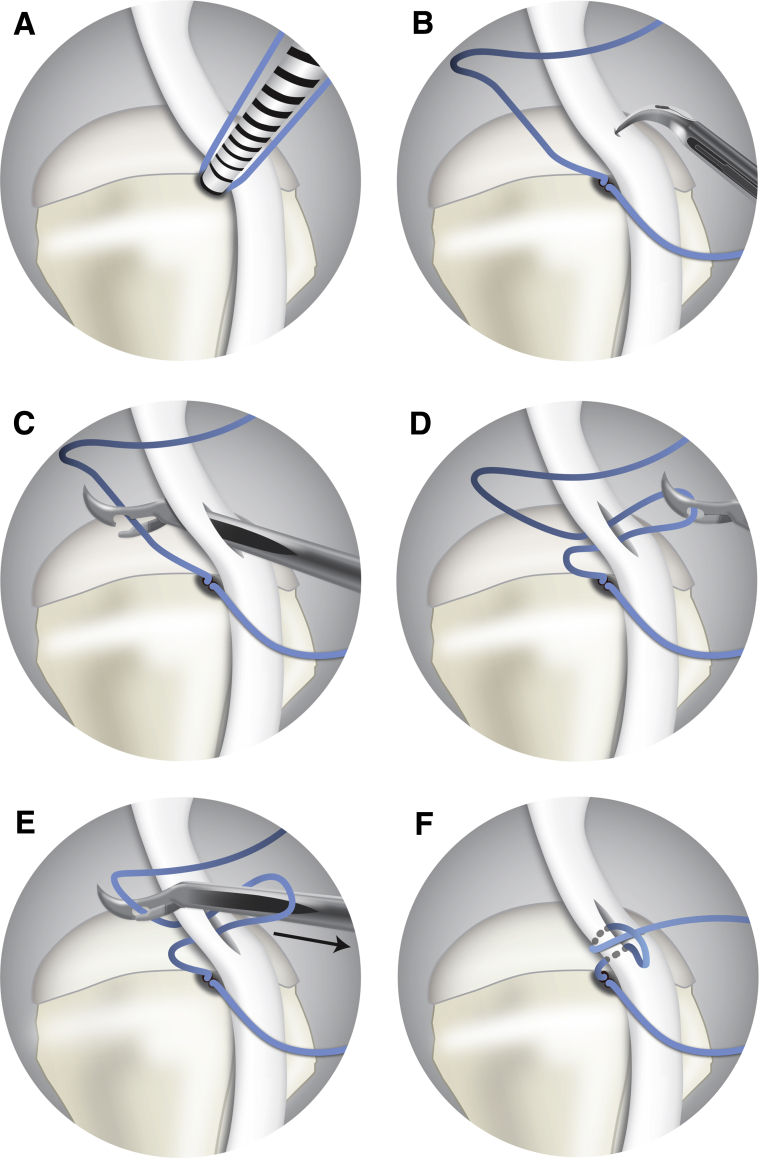
Fig 8.
Illustrations summarizing the steps required to create the first lasso-loop.
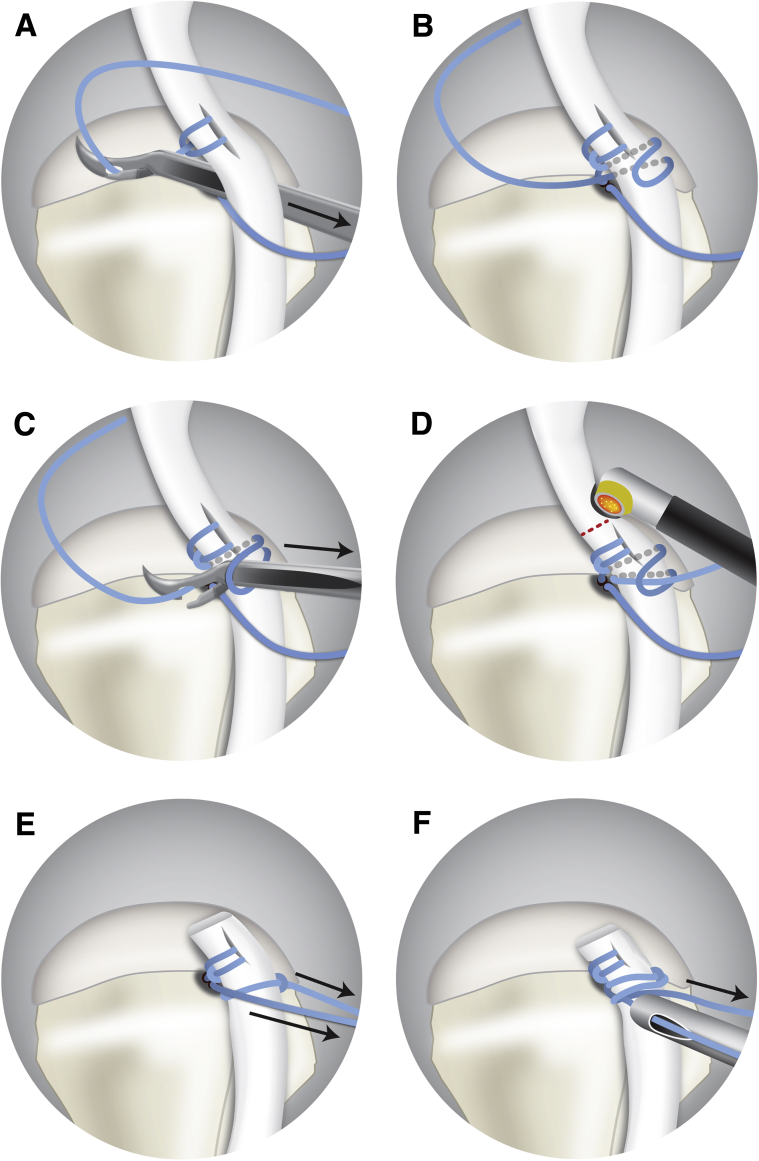
Fig 9.
Illustrations summarizing the steps required to create the second lasso-loop.
Technique Variations
In cases of a symptomatic LHBT lesion without an associated supraspinatus tendon tear (e.g., a “concealed” LHBT lesion), the same tenodesis technique can be performed within or below the biceps groove, just above the pectoralis major tendon. These latter 2 tenodesis positions are preferred by some surgeons, regardless of the status of the supraspinatus tendon.
Postoperative Rehabilitation
The postoperative rehabilitation protocol follows general recommendations for rotator cuff repairs. For the first 6 weeks, the shoulder is immobilized in a sling; early passive stretching exercises of the shoulder are initiated, and resisted elbow flexion is avoided during this time.
Discussion
The optimal treatment for patients with a symptomatic LHBT is controversial; both biceps tenotomy and tenodesis remain effective options. When clinically indicated, 1 advantage of performing a biceps tenodesis compared with a tenotomy is maintenance of the biceps muscle length tension relationship.2 As a result, improvements in cosmesis (e.g., lower rate of Popeye deformity), decreased rates of discomfort (e.g., less biceps muscle cramping), and preservation of muscle strength (i.e., forearm supination) can be observed.16, 17
In cases in which a tenodesis is selected, the method and location of fixation of the LHBT are largely dependent on the surgeon's experience and preference. The long head biceps tenodesis technique described in this Technical Note includes use of a standard rotator cuff anchor and 2 self-cinching suture loops on each side of the tendon, followed by locking half-hitches to secure the construct. The single “lasso-loop” tenodesis technique was first described in 2006 by Lafosse et al.15 We have modified this technique by adding a second suture loop to permit circumferential fixation of the LHBT. Biomechanical testing has demonstrated that self-cinching stitches lead to superior tissue-holding strength at the tissue-suture interface compared with non–self-cinching stitches.18 Other investigators have performed biomechanical testing on modifications of the lasso-loop stitch and have found equivalent tendon fixation compared with that achieved with interference screws.19
In early reports of arthroscopic biceps tenodesis, suture anchors and interference screws were used for fixation. Arthroscopic tenodesis techniques performed “high in the groove” (i.e., at the articular margin of the humeral head) have been previously described.20 Recently, Brady et al.21 reported the clinical outcomes of this technique for 1,083 patients at an average of 2.6 years of follow-up; the overall revision rate for tenodesis-related issues was only 0.4% (4 cases).20, 21
The potential limitations of this procedure are similar to those seen with other tenodesis techniques that are performed high in the bicipital groove. In cases in which there is concern that patients may have persistent “bicipital groove pain” due to a portion of diseased biceps being left within the groove, the procedure can be performed low in the groove or below the groove rather than adjacent to the articular margin of the humeral head. Another potential limitation of this procedure could occur if sufficient residual biceps tissue is not removed such that this excess tissue covers the prepared rotator cuff footprint and interferes with healing of the repaired supraspinatus tendon. Time should be taken to carefully remove biceps tendon tissue found proximal to the secured construct to mitigate this potential problem.
The arthroscopic tenodesis technique described in this Technical Note has several advantages. This technique is easily taught and reproduced by surgeons, which is likely the result of optimal visualization and ease of steps required to complete the procedure. This technique can also be easily mastered by surgeons in training. In addition, this procedure is versatile. Furthermore, we consider this technique safe from neurovascular injury or humeral fracture, injuries that have been reported after biceps tenodesis in the subpectoral region.22, 23 Finally, we consider this a cost-effective technique for several reasons: (1) It is a time-efficient technique that takes less than 5 minutes to perform, saving operating room time; (2) “tenodesis-specific” anchors or implants are not required; and (3) sutures from the same anchor can be used to address associated pathology involving the anterior supraspinatus tendon (Table 1).
Table 1.
Advantages and Limitations
| Advantages | Limitations |
|---|---|
|
|
LHBT, long head biceps tendon.
Multiple techniques for long head biceps tenodesis have been described with variations in surgical approach (e.g., arthroscopic vs mini-open), method of fixation, and anatomic location of the tenodesis. Overall, this arthroscopic technique is safe, reproducible, versatile, and cost-effective and serves as another option for surgeons to consider for tenodesis of the LHBT.
Acknowledgments
The authors thank Sandy Cochrane, Illustrator, Cumming School of Medicine (University of Calgary), for providing the drawings in Figures 8 and 9.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical video of a right shoulder (patient placed in the beach chair position) demonstrating the “double lasso-loop” technique used for arthroscopic proximal biceps tenodesis. The anterolateral portal serves as the working portal through which to create the first self-cinching suture loop (i.e., lasso-loop). After 1 suture limb has been shuttled into the joint, the tip of the Cleverhook (DePuy Synthes) is passed through the midportion of the long head biceps tendon. The previously shuttled suture is grasped by using the jaw of the Cleverhook grasper. The suture is pulled back through the long head biceps tendon, but not completely through, leaving a loop of suture exiting the superior surface of the tendon. The tip of the Cleverhook is then passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tightened to create the lasso-loop. The anterolateral portal similarly serves as the working portal through which to create the second self-cinching suture loop. A looped grasper is used to shuttle the same suture limb that was used to create the first loop into the joint. The Cleverhook (DePuy Synthes) is passed around the anterior aspect and under the long head biceps tendon. The midportion of the suture limb that was previously positioned within the joint is grasped and pulled in the reverse direction, leaving a loop of suture. The tip of the Cleverhook is passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tightened to create the second self-cinching suture loop. To secure the construct, a looped suture grasper is used to reposition the second (i.e., lateral) suture loop in close proximity to the medially placed lasso-loop along the length of the long head biceps tendon. An electrocautery device is used to perform the biceps tenotomy, medial to the previously placed suture loops. While the surgeon pulls on the suture end that does not pass through the long head biceps tendon (i.e., the post), the tendon is reduced to the suture anchor. (D) Half-hitch locking knots (i.e., reverse half-hitches or alternating posts) are used to secure the construct with a standard knot pusher. The electrocautery device is then used to remove residual medial long head biceps tendon tissue, adjacent to both the tenodesis construct and superior biceps labrum complex.
References
- 1.Elser F., Braun S., Dewing C.B., Giphart J.E., Millett P.J. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581–592. doi: 10.1016/j.arthro.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 2.Denard P.J., Dai X., Hanypsiak B.T., Burkhart S.S. Anatomy of the biceps tendon: Implications for restoring physiological length tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28:1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 3.Taylor S.A., Fabricant P.D., Bansal M. The anatomy and histology of the bicipital tunnel of the shoulder. J Shoulder Elbow Surg. 2015;24:511–519. doi: 10.1016/j.jse.2014.09.026. [DOI] [PubMed] [Google Scholar]
- 4.Khazzam M., George M.S., Churchill R.S., Kuhn J.E. Disorders of the long head of biceps tendon. J Shoulder Elbow Surg. 2012;21:136–145. doi: 10.1016/j.jse.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 5.Braun S., Horan M.P., Elser F., Millett P.J. Lesions of the biceps pulley. Am J Sports Med. 2011;39:790–795. doi: 10.1177/0363546510393942. [DOI] [PubMed] [Google Scholar]
- 6.Hawi N., Liodakis E., Garving C., Habermeyer P., Tauber M. Pulley lesions in rotator cuff tears: Prevalence, etiology, and concomitant pathologies. Arch Orthop Trauma Surg. 2017;137:1097–1105. doi: 10.1007/s00402-017-2721-z. [DOI] [PubMed] [Google Scholar]
- 7.Boileau P., Baqué F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 8.Shang X., Chen J., Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PLoS One. 2017;12:1–14. doi: 10.1371/journal.pone.0185788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Godenèche A., Kempf J.F., Nové-Josserand L. Tenodesis renders better results than tenotomy in repairs of isolated supraspinatus tears with pathologic biceps. J Shoulder Elbow Surg. 2018;27:1939–1945. doi: 10.1016/j.jse.2018.03.030. [DOI] [PubMed] [Google Scholar]
- 10.Taylor S.A., Newman A.M., Dawson C. The “3-pack” examination is critical for comprehensive evaluation of the biceps-labrum complex and the bicipital tunnel: A prospective study. Arthroscopy. 2017;33:28–38. doi: 10.1016/j.arthro.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Rosas S., Krill M.K., Amoo-Achampong K., Kwon K., Nwachukwu B.U., McCormick F. A practical, evidence-based, comprehensive (PEC) physical examination for diagnosing pathology of the long head of the biceps. J Shoulder Elbow Surg. 2017;26:1484–1492. doi: 10.1016/j.jse.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malavolta E.A., Assuncao J.H., Guglielmetti C.L., de Souza F.F., Gracitelli M.E., Ferreira Neto A.A. Accuracy of preoperative MRI in the diagnosis of disorders of the long head of the biceps tendon. Eur J Radiol. 2015;84:2250–2254. doi: 10.1016/j.ejrad.2015.07.031. [DOI] [PubMed] [Google Scholar]
- 13.Taylor S.A., Newman A.M., Nguyen J. Magnetic resonance imaging currently fails to fully evaluate the biceps-labrum complex and bicipital tunnel. Arthroscopy. 2016;32:238–244. doi: 10.1016/j.arthro.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Yalizis M., Kruse K., II, Godenèche A. Arthroscopic “panorama” view of the subacromial space via deltoid fascia release. Arthrosc Tech. 2016;5:e935–e939. doi: 10.1016/j.eats.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: “The lasso-loop stitch”. Arthroscopy. 2006;22:1246.e1–1246.e3. doi: 10.1016/j.arthro.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 16.Oh J.H., Lee Y.H., Kim S.H. Comparison of treatments for superior labrum-biceps complex lesions with concomitant rotator cuff repair: A prospective, randomized, comparative analysis of debridement, biceps tenotomy, and biceps tenodesis. Arthroscopy. 2016;32:958–967. doi: 10.1016/j.arthro.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 17.Lee H.J., Jeong J.Y., Kim C.K., Kim Y.S. Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: A prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg. 2016;25:1107–1114. doi: 10.1016/j.jse.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Ponce B.A., Hosemann C.D., Raghava P., Tate J.P., Eberhardt A.W., Lafosse L. Biomechanical evaluation of 3 arthroscopic self-cinching stitches for shoulder arthroscopy: The lasso-loop, lasso-mattress, and double-cinch stitches. Am J Sports Med. 2011;39:188–194. doi: 10.1177/0363546510383394. [DOI] [PubMed] [Google Scholar]
- 19.Patzer T., Rundic J.M., Bobrowitsch E., Olender G.D., Hurschler C., Schofer M.D. Biomechanical comparison of arthroscopically performable techniques for suprapectoral biceps tenodesis. Arthroscopy. 2011;27:1036–1047. doi: 10.1016/j.arthro.2011.03.082. [DOI] [PubMed] [Google Scholar]
- 20.Lo I.K., Burkhart S.S. Arthroscopic biceps tenodesis using a bioabsorbable interference screw. Arthroscopy. 2004;20:85–95. doi: 10.1016/j.arthro.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 21.Brady P.C., Narbona P., Adams C.R. Arthroscopic proximal biceps tenodesis at the articular margin: Evaluation of outcomes, complications, and revision rate. Arthroscopy. 2015;31:470–476. doi: 10.1016/j.arthro.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 22.Sears B.W., Spencer E.E., Getz C.L. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7–e11. doi: 10.1016/j.jse.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 23.Hohmann E. Editorial commentary: Shoulder subpectoral biceps tenodesis significantly increases the humeral fracture risk – is this a reason to look for alternatives? Arthroscopy. 2018;34:814–815. doi: 10.1016/j.arthro.2017.10.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical video of a right shoulder (patient placed in the beach chair position) demonstrating the “double lasso-loop” technique used for arthroscopic proximal biceps tenodesis. The anterolateral portal serves as the working portal through which to create the first self-cinching suture loop (i.e., lasso-loop). After 1 suture limb has been shuttled into the joint, the tip of the Cleverhook (DePuy Synthes) is passed through the midportion of the long head biceps tendon. The previously shuttled suture is grasped by using the jaw of the Cleverhook grasper. The suture is pulled back through the long head biceps tendon, but not completely through, leaving a loop of suture exiting the superior surface of the tendon. The tip of the Cleverhook is then passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tightened to create the lasso-loop. The anterolateral portal similarly serves as the working portal through which to create the second self-cinching suture loop. A looped grasper is used to shuttle the same suture limb that was used to create the first loop into the joint. The Cleverhook (DePuy Synthes) is passed around the anterior aspect and under the long head biceps tendon. The midportion of the suture limb that was previously positioned within the joint is grasped and pulled in the reverse direction, leaving a loop of suture. The tip of the Cleverhook is passed through the loop to grasp the free end of the suture (i.e., the same limb used to create the loop), which is pulled through the loop and tightened to create the second self-cinching suture loop. To secure the construct, a looped suture grasper is used to reposition the second (i.e., lateral) suture loop in close proximity to the medially placed lasso-loop along the length of the long head biceps tendon. An electrocautery device is used to perform the biceps tenotomy, medial to the previously placed suture loops. While the surgeon pulls on the suture end that does not pass through the long head biceps tendon (i.e., the post), the tendon is reduced to the suture anchor. (D) Half-hitch locking knots (i.e., reverse half-hitches or alternating posts) are used to secure the construct with a standard knot pusher. The electrocautery device is then used to remove residual medial long head biceps tendon tissue, adjacent to both the tenodesis construct and superior biceps labrum complex.