Abstract
Los Angeles County (LAC) low-income communities of color experience uneven asthma rates, evidenced by asthma emergency department visits (AEDV). This has partly been attributed to inequitable exposure to diesel particulate matter (DPM). Promisingly, public parks and open space (PPOS) contribute to DPM mitigation. However, low-income communities of color with limited access to PPOS may be deprived of associated public health benefits. Therefore, this novel study investigates the AEDV, DPM, PPOS nexus to address this public health dilemma and inform public policy in at-risk communities. Optimized Hotspot Analysis was used to examine geographic clustering of AEDVs, DPM, and PPOS at the census tract unit of analysis in LAC. Ordinary Least Squares (OLS) regression analysis was used to examine the extent to which DPM and PPOS predict AEDVs. Finally, Geographic Weighted Regression (GWR) was employed to account for spatial dependence in the global OLS model. Optimized Hotspot Analysis confirmed significant clustering of elevated AEDVs and DPM in census tracts with reduced PPOS. After controlling for pertinent demographic characteristics (poverty, children, race/ethnicity), regression analysis confirmed that DPM was significantly positively associated with AEDVs, whereas PPOS was significantly negatively associated with AEDVs. Furthermore, GWR revealed that 71.5% of LACs census tracts would benefit from DPM reductions and 79.4% would benefit from PPOS increases toward redressing AEDVs. This is the first study to identify AEDV reductions in census tracts with higher concentrations of PPOS. Thus, reducing DPM and increasing PPOS may serve to improve asthma outcomes, particularly in low-income communities of color.
Keywords: Public parks, Open space, Greenspace, Diesel particulate matter, Communities of color, Asthma, Health disparities, Ecological determinants
1. Introduction
Asthma is a concerning chronic disease that disproportionately impacts low-income communities of color, especially African American communities (Akinbami et al., 2012; Aligne et al., 2000; Carr et al., 1992; Marder et al., 1992). A wealth of literature has focused on the relationship between asthma and individual- and household-level factors such as socioeconomic status and indoor air quality, thus attributing poor respiratory health outcomes to individual behavior and living conditions (Gelber et al., 1993; Huss et al., 2001; Schwartz et al., 1990; Warner et al., 1996). For example, research has emphasized the relationship between increased exposure to indoor allergens and asthma (Finkelstein et al., 2002; Gelber et al., 1993; Kanchongkittiphon et al., 2015; Pomés et al., 2016; Salo et al., 2008). However, evidence suggests that aside from potential susceptibility genes, exposure to proximal and distal environmental factors (e.g., indoor and outdoor air pollution) may be associated with asthma prevalence among a range of ethnocultural groups (Holgate, 1999; Torgerson et al., 2011; Wiesch et al., 1999). More specifically, indoor and outdoor air pollutants, as well as exposure to environmental tobacco smoke and pollen allergens, have been linked to disease inception and long-term severity and progression (Brunekreef, 2004; Holgate et al., 2007).
More recently, research has explored the nexus of asthma and traffic-related air pollution (Clark et al., 2010), with particular emphasis on negative respiratory and cardiovascular health impacts of diesel particulate matter (DPM) (Mar et al., 2010; McEntee and Ogneva-Himmelberger, 2008; Ristovski et al., 2012; Valavanidis et al., 2008). Diesel powered vehicles, including school buses and trucks, are considered viable public and private transportation solutions, yet 90% of primary particles emitted from diesel engines are less than 2.0 μm, which is less than the 2.5 μm size range of concern regarding National Ambient Air Quality Standards (Hodan and Bernard, 2017; Ristovski et al., 2012). Furthermore, in the Southern California context, DPM accounts for over 70% of the concomitant air pollution cancer risk (South Coast Air Quality Management District, 2016). This is particularly concerning from a public health disparities perspective, as low-income communities of color tend to experience unequal proximal and distal exposure to DPM (Gonzalez et al., 2011; Houston et al., 2014; Los Angeles Collaborative for Environmental Health and Justice, 2010; McEntee and Ogneva-Himmelberger, 2008; Morello-Frosch et al., 2001; Morello-Frosch et al., 2002).
Related research has also shifted to consider the nexus of greenspace (e.g., public parks and open space) and community health (Dadvand et al., 2014; Sbihi et al., 2015). For example, current research suggests that public parks and open spaces (PPOS) are important behavior settings for promoting health and wellness activities in the urban context (Cohen et al., 2013; Douglas et al., 2018; Kaczynski et al., 2014; Wolch et al., 2014). Furthermore, ecosystem services (e.g., health benefits derived from natural environments) associated with PPOS (e.g. urban trees) have been shown to mitigate air pollution, providing a medium for improving air quality and related respiratory health outcomes in urban communities experiencing high air pollution burdens (Cohen et al., 2014; Manes et al., 2016; Selmi et al., 2016; Yang et al., 2005). Urban trees have been estimated to reduce acute respiratory symptoms by 670,000 cases annually in the U.S. (Nowak et al., 2014). In the Los Angeles context, recent research estimates PM2.5 removal by urban trees amounting to 0.13 g m−2 yr−1, resulting in reduced morbidity and mortality, as well as decreased cost of illness associated with acute respiratory symptoms (Nowak et al., 2013).
Ecosystem services such as these have promisingly been linked with improved health outcomes in low-income communities of color (Jennings et al., 2012; Mitchell and Popham, 2007). However, it is important to note that socioeconomically disadvantaged communities often do not receive such benefits. For example, although extant research regarding disparities in residential proximity to PPOS remains inconclusive, Los Angeles' low-income communities of color experience marked inequities in public park acres and quality compared to more affluent White communities (García et al., 2016; Rigolon, 2016; Wolch et al., 2002). From a public health perspective, this is particularly problematic given the potential protective benefits of PPOS, as well as higher asthma rates, in low-income and ethnocultural minority communities.
While the available literature posits the detriments of air pollution and potential benefits of PPOS in the context of community health, only limited research connects these seemingly related variables (Baró et al., 2014; Carlsten and Rider, 2017; Derkzen et al., 2015; Van Dillen et al., 2011). One study explored associations between heavy traffic and child asthma, providing supportive evidence that greenspace may have a potential buffering effect against air pollution. However, the study used proxy indicators of air pollution via surveys of perceived traffic volume in Australia (Feng and Astell-Burt, 2017). To date, no other study has objectively investigated the distributional impacts of exposure to DPM and access to PPOS concerning AEDV prevalence. We seek to address this gap by investigating the geographical relationship between AEDVs, DPM, and PPOS in Los Angeles County.
1.1. Study aims
The current study had two objectives: 1) identify potential geographic clustering of asthma emergency department visits (AEDV), diesel particulate matter (DPM), and acres of public parks and open space (PPOS) in Los Angeles County by applying geographic information systems (GIS) hotspot analysis, and 2) in case of significant clustering of these variables, conducting an ensuing GIS regression analysis to diagnose spatial associations between these variables, while adjusting for sensitive population indicators including poverty, children, and race/ethnicity.
2. Methods
2.1. Research context
Los Angeles County (LAC) has a population of 10,038,388 people and a population density of 2419.6 people per square mile. It is an ethnoculturally diverse area that is approximately 8.0% African American/Black, 48.2% Latina/o, 26.9% White, 14% Asian, 0.2% American Indian/Alaska Native, and 0.2% Native Hawaiian/Pacific Islander (U.S. Census Bureau, 2015). With over 1.2 Million of its residents diagnosed with asthma, LAC has one of the highest asthma rates in California. Furthermore, LAC experiences 52.2 asthma related emergency department visits (AEDV) per 10,000 people of the population. In this context, significant AEDV escalations have been found in LACs ethnocultural minority communities—133.5 Black, 43.7 Latina/o, 27.2 White, 16.3 Asian/Pacific Islander—illustrating a public health disparity (Think Health LA, 2017). Compounding this, several of LACs census tracts, particularly those in socioeconomically deprived areas, are home to some of the highest pollution burdens (e.g. DPM) and population sensitivities (e.g., children under the age of 10 and poverty) in the state of California (Houston et al., 2004). It is critical to note that mobile sources of pollution (e.g. heavy-duty diesel trucks, off-road equipment, and ships and commercial boats), which are often geographically proximal to low-income communities of color, are the largest contributors to air pollution in Southern California (Houston et al., 2004). Furthermore, Los Angeles communities with a high density of ethnocultural minorities have fewer acres of greenspace per 1000 people of the population—e.g., 0.6 acres for Latina/os and 1.7 acres for African Americans—compared to 31.8 acres in White communities (Wolch et al., 2002).
2.2. Design
This study emerged to address a gap in the literature regarding the potential distributional impacts of health-promoting environmental resources, such as public parks and open space. As such, we examined associations between Asthma Emergency Department Visits (AEDV), Diesel Particulate Matter (DPM), and acres of public parks and open space (PPOS) across 2347 census tracts in LAC. Given the developing body of research identifying associations between air pollutants and AEDVs (Fan et al., 2016; Mar and Koenig, 2009; Norris et al., 1999; Sharma et al., 2016; Slaughter et al., 2005; Wang et al., 2010), as well as availability of asthma data for Los Angeles County (OEHHA, 2016), we identified AEDV records as a viable indicator of asthma prevalence.
2.3. Data
This study employed the California Communities Environmental Health Screening Tool CalEnviroScreen 3.0 dataset, which classifies 20 indicators covering pollution burdens and population characteristics of California's approximately 8000 census tracts (OEHHA, 2016). CalEnviroScreen 3.0, released in September 2016, was developed by the Office of Environmental Health Hazard Assessment (OEHHA), and uses a numerical score to indicate environmental, health, and socioeconomic information by census tract across the state. The included 2012 DPM data characterizes emissions and potential exposures where people live.
All data employed in the current study were located at the census tract unit of analysis, as regional or metropolitan scales potentially mask effects of community-level environmental indicators (Cagney and Browning, 2004). The utilized data included (1) age adjusted AEDVs per 10,000 persons of the population for 2011–2013, which were calculated for ZIP Codes and reapportioned to census tract rates (CEHTP, 2014); (2) spatial distribution of gridded DPM for a summer day in July 2012 calculated via EMFAC2013 on-road emissions models and CEPAM emissions forecasting system for off-road emissions estimates, wherein weighted averages were allocated to census tracts (CARB, 2013) and subsequently min-max normalized; (3) percent population living below two times the federal poverty level between 2011 and 2015, obtained from the U.S. Census Bureau (2015); and (4) percent population under the age of 10, also obtained from the U.S. Census Bureau (2010). Specific methods of compiling data for census tracts are discussed elsewhere (OEHHA, 2016).
In addition, census tract level race/ethnic population numbers—African American/Black, Latina/o, White, Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, Other—were gleaned from the U.S. Census Bureau (2010), and normalized per square mile. To measure impacts of public parks and open space, acres of PPOS were obtained from the Los Angeles County Department of Parks and Recreation (Department of Parks and Recreation, 2017) and min-max normalized. The dataset contains PPOS data for the entire County of Los Angeles, also at the census tract level.
2.4. Statistical analyses
2.4.1. Optimized hotspot analysis
The Optimized Hotspot Analysis (OHA) tool, using Getis-Ord Gi* statistic in ArcMap 10.2, was applied to analyze statistically significant hot and cold spots of AEDVs, DPM, and PPOS at the census tract unit of analysis. Thus, OHA provided a method for identifying spatial clustering of AEDVs, DPM, and PPOS across LAC's 2347 census tracts. A geospatial overlay of OHA maps was completed to visually compare geographic locations of AEDV, DPM, and PPOS hot and cold spots. The overlay was generated by combining the intersecting hot spot values of AEDV and DPM with inverse values of PPOS.
2.4.2. Ordinary least squares regression
We investigated associations across LAC census tracts by developing an ordinary least squares (OLS) regression model in ArcMap 10.2, with AEDVs as the dependent variable and DPM and PPOS as the main independent variables. The model also controlled for percentage of residents living two times below the federal poverty line, percentage of residents under the age of 10, and number of African American/Black, Latina/o, White, Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, and Other residents per square mile. This model uniformly summarized the relationships between variables across LAC. However, OLS models do not provide adequate explanatory power when spatial dependence is exhibited among variables, as OLS models are calculated for the total geographic area rather than individual census tracts, for example (Anselin, 2002). Accordingly, Moran's Index revealed spatial dependence in the current model.
2.4.3. Geographic weighted regression
Spatial dependence was accounted for via ArcMap 10.2 geographically weighted regression (GWR), which extends linear regression models by accounting for spatial effect at the local scale for each geographic location in the data (Brunsdon et al., 1996; Fotheringham et al., 1998; Matthews and Yang, 2012). With a large sample size, such as that included in the current study, GWR is advantageous because it is robust to remarkably high levels of multicollinearity and local coefficients that may display strong spatial autocorrelation (Oshan and Fotheringham, 2016). Thus, GWR was utilized to apply our regression model to each census tract within LAC. Furthermore, GWR afforded exploration of regional variation among AEDVs, DPM, and PPOS.
3. Results
3.1. Geospatial distribution of asthma emergency department visits, diesel particulate matter, and public parks and open space
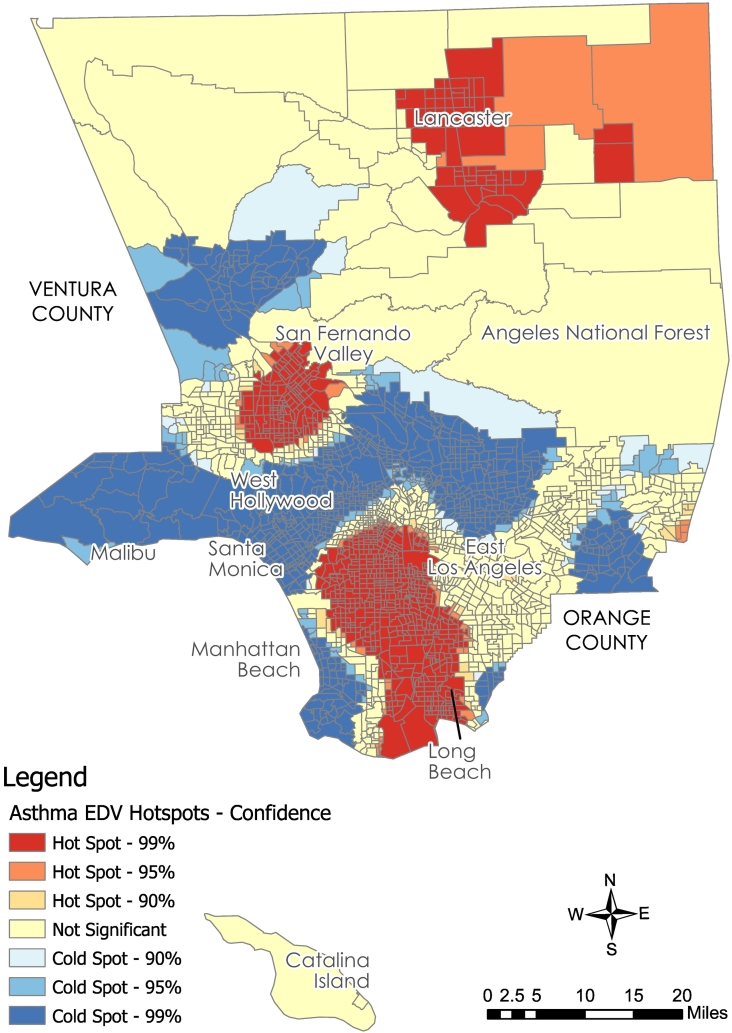
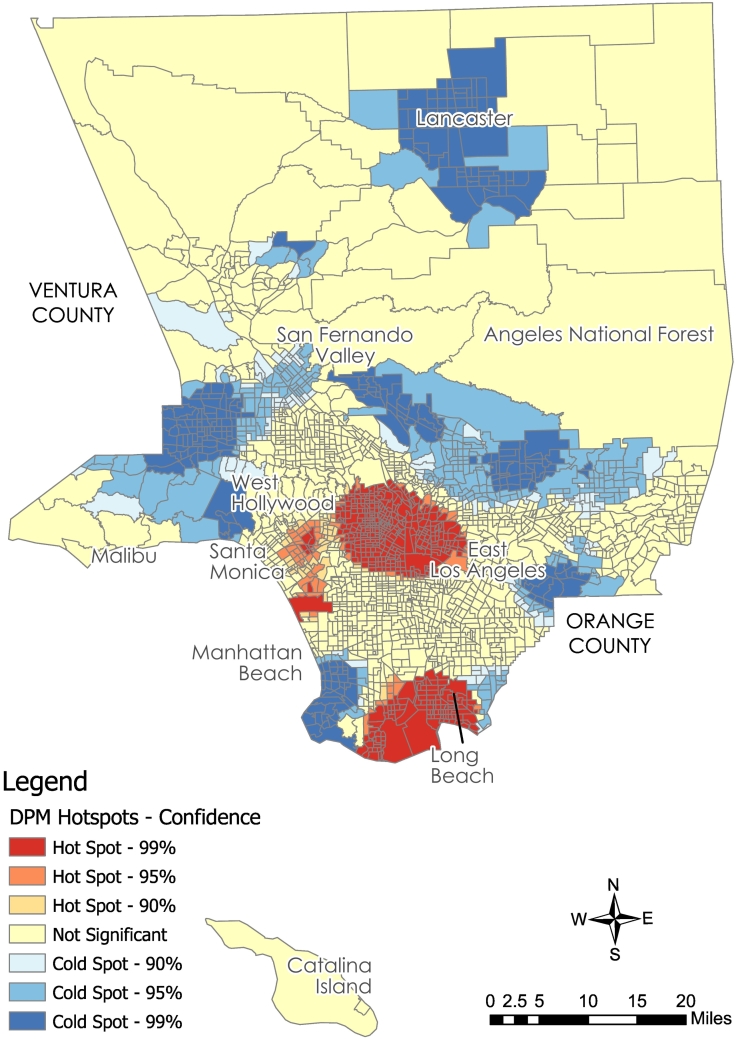
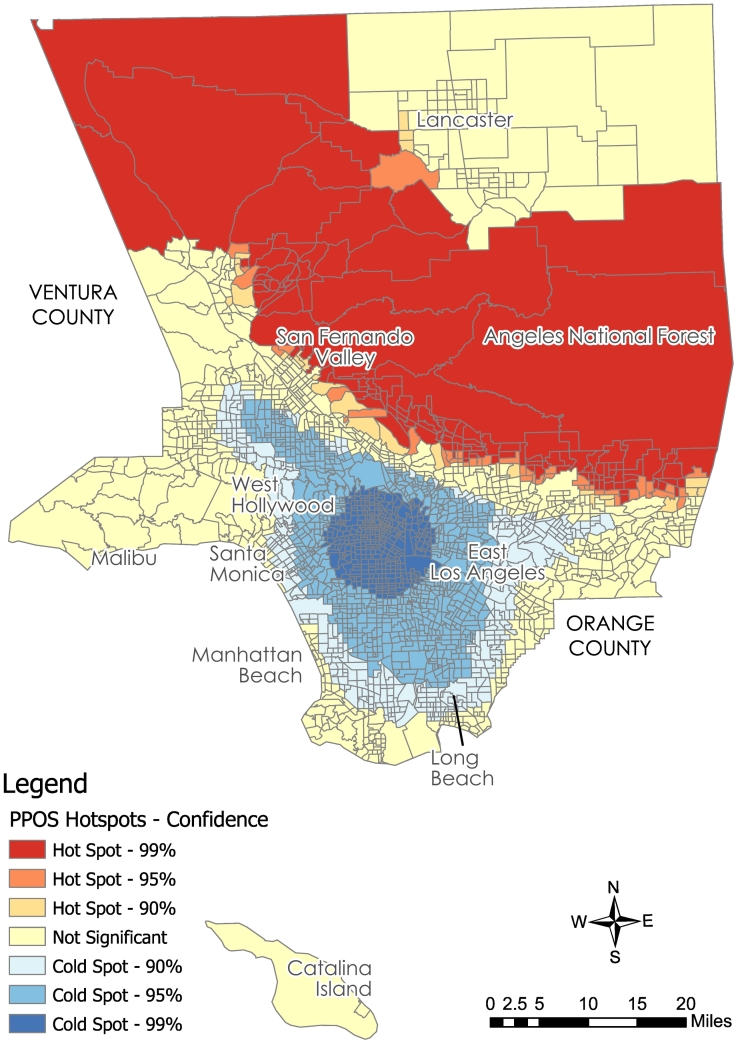
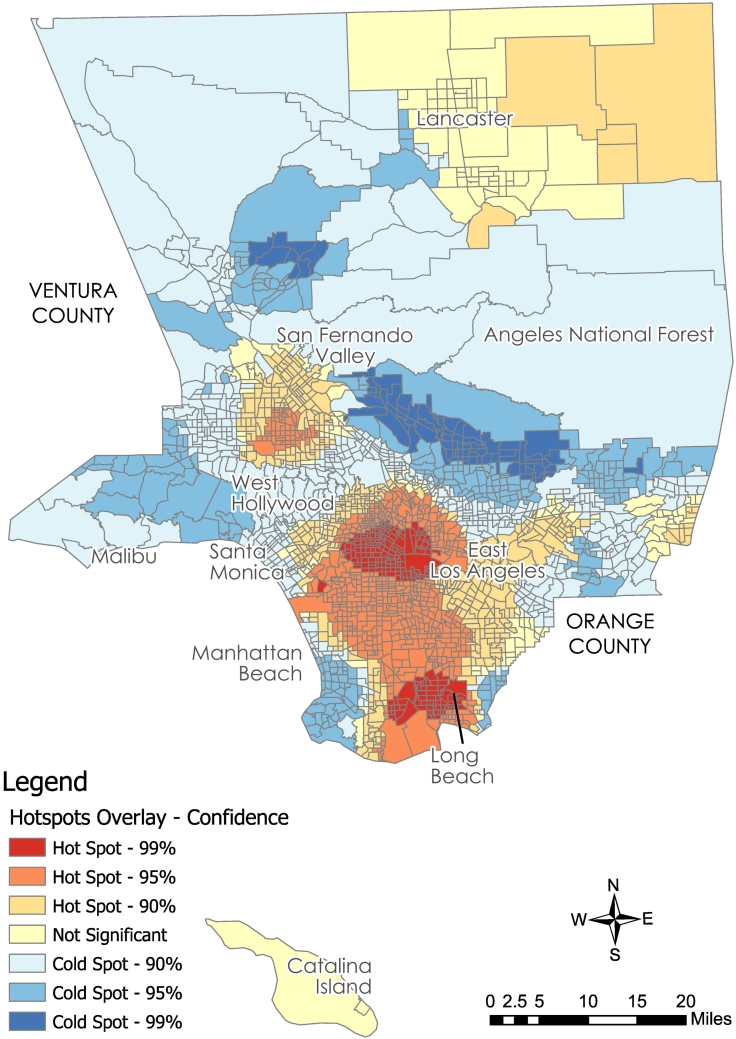
Hotspot analysis revealed statistically significant clustering of AEDVs, DPM, and PPOS in LAC when analyzed independently (Fig. 1, Fig. 2, Fig. 3). Visual inspection of these three discrete variables revealed several common hotspot locations between AEDVs and DPM, with PPOS coldspots overlapping these areas. An ensuing geospatial overlay of AEDV, DPM, and PPOS maps confirmed considerable overlap of elevated AEDVs and DPM located in areas with reduced PPOS (Fig. 4). This analysis provided the impetus for proceeding with OLS regression analysis.
Fig. 1.
Hotspot analysis of asthma emergency department visits (AEDV).
Fig. 2.
Hotspot analysis of diesel particulate matter (DPM).
Fig. 3.
Hotspot analysis of public parks and open space (PPOS).
Fig. 4.
Geospatial overlay of asthma emergency department visits (AEDV), diesel particulate matter (DPM), and public parks and open space (PPOS).
3.2. Associations between asthma emergency department visits, diesel particulate matter, and public parks and open space across Los Angeles County
The OLS AEDV model utilized DPM and PPOS as the primary predictor variables and percent of residents living two times below the federal poverty level, percent of residents under the age of 10, and number of African American/Black, Asian, Latina/o, White, American Indian/Alaska Native, Native Hawaiian/Pacific Islander, and Other residents per square mile as control variables (Table 1). Model diagnostics revealed that there was no multicollinearity in the model, wherein all Variance Inflation Factors were less than 2.53. However, spatial autocorrelation was detected (Moran's I).
Table 1.
Census tract level descriptive statistics.
| Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|
| AEDV | 0 | 154.14 | 51.59 | 25.47 |
| DPM | 0.000072 | 1 | 0.12 | 0.09 |
| PPOS | 0 | 1 | 0.02 | 0.14 |
| Children | 0 | 40.6 | 12.75 | 4.25 |
| Poverty | 0 | 94.9 | 25.31 | 127.85 |
| White | 0 | 51,339.49 | 2749.27 | 3857.95 |
| Black | 0 | 19,198.00 | 1106.70 | 2015.94 |
| Latina/o | 0 | 78,201.84 | 7154.93 | 8416.45 |
| AIAN | 0 | 415.60 | 23.10 | 28.66 |
| Asian | 0 | 45,486.61 | 1721.16 | 3239.61 |
| NHPI | 0 | 988.45 | 27.00 | 67.00 |
| Other | 0 | 675.85 | 36.10 | 47.19 |
The final OLS AEDV model accounted for 43% of the total variance in LAC AEDVs, with DPM (p = .001), poverty (p = .05), residents under age 10 (p = .001), African American/Black (p = .001), American Indian and Alaska Native (AIAN) (p = .05), and Native Hawaiian and Pacific Islander (NHPI) (p = .001) significantly positively associating with AEDVs at the census tract level. In addition, acres of PPOS (p = .001), along with the White and Asian race/ethnicity variables (p = .001), were significantly negatively associated with AEDVs. The Latina/o and Other race/ethnicity categories did not reveal any significant associations (Table 2). As noted above, model residuals were spatially autocorrelated (Moran's Index = 0.08, Z = 57.80, p = .001). Thus, we proceeded with GWR to correct for spatial autocorrelation and explore regional variation of the significant DPM and PPOS relationships identified in the OLS model.
Table 2.
Ordinary least squares regression results for associations between diesel particulate matter and public parks and open space with asthma emergency department visits in Los Angeles County.
| OLS model | |
|---|---|
| R2 | 0.44 |
| Adjusted R2 | 0.43 |
| AIC | 20,498.62 |
| Estimate | SE | t value | |
|---|---|---|---|
| Intercept | 22.07 | 2.68 | 8.24⁎⁎⁎ |
| DPM | 29.78 | 5.96 | 5.00⁎⁎⁎ |
| PPOS | −8.05 | 2.55 | −3.15⁎⁎⁎ |
| Children | 1.90 | 0.21 | 8.86⁎⁎⁎ |
| Poverty | 0.01 | 0.005 | 2.20⁎ |
| White | −0.0009 | 0.0001 | −6.48⁎⁎⁎ |
| Black | 0.005 | 0.0004 | 12.24⁎⁎⁎ |
| Latina/o | −0.00008 | 0.00009 | −0.84 |
| AIAN | 0.05 | 0.02 | 2.09⁎ |
| Asian | −0.0009 | 0.0001 | −7.90⁎⁎⁎ |
| NHPI | 0.02 | 0.005 | 3.51⁎⁎⁎ |
| Other | −0.007 | 0.01 | −0.54 |
p < .05.
p < .001.
3.3. Geospatial dependence between asthma emergency department visits, diesel particulate matter, and public parks and open space across Los Angeles County census tracts
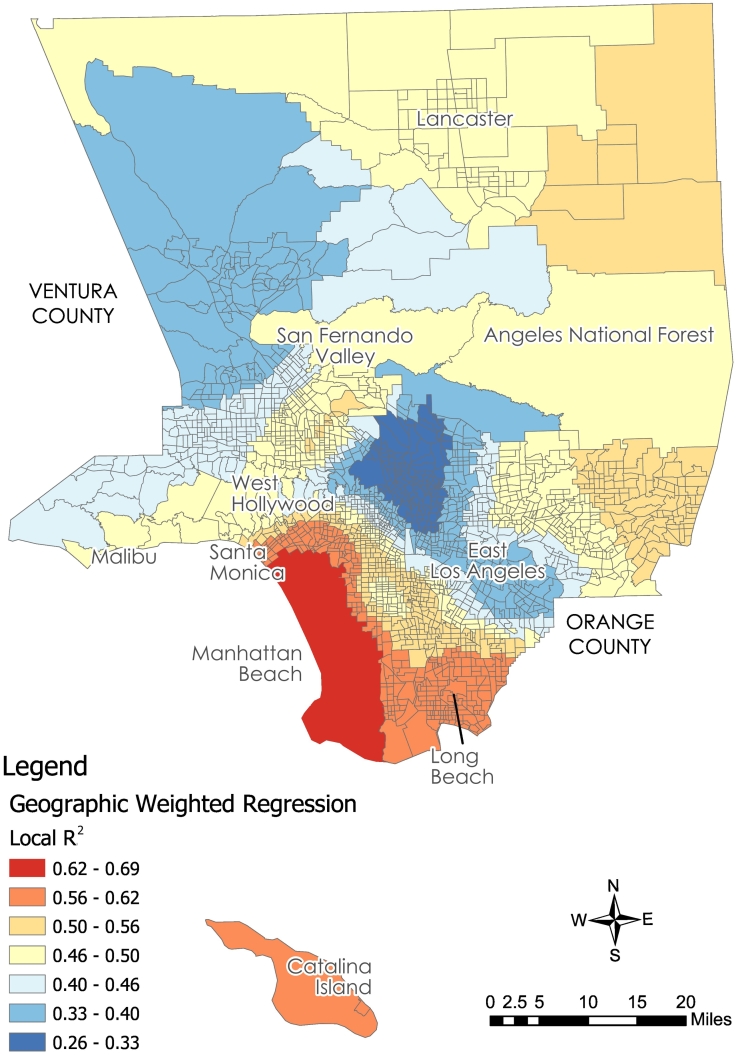
GWR estimates of the AEDV model yielded an adaptive bandwidth of 726 neighbors, an R2 of 0.66, and an adjusted R2 of 0.64, improving upon the OLS R2 of 0.43. The GWR model also produced a reduced AICc value of 19,459 compared to the OLS model AICc value of 20,499. As such, the local GWR model, with smaller AICc, yielded more explanatory power than the global OLS model by accounting for regional variation. In addition, as local R2 values ranged from 0.26 to 0.69, the GWR model predicted a range of AEDV instances in all census tracts (Fig. 5).
Fig. 5.
Geographically weighted regression R2 values indicating associations between asthma emergency department visits, diesel particulate matter, and public parks and open space.
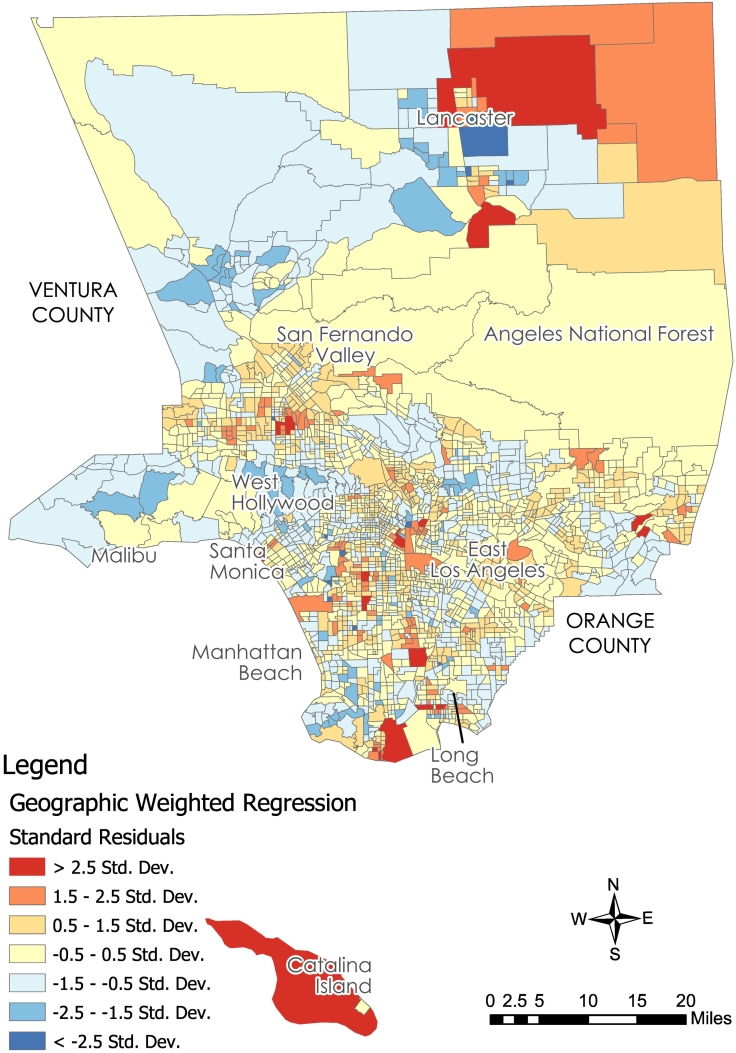
While the OLS model was significant across LAC, the GWR model revealed regional variation across census tracts, with DPM coefficients fluctuating from −256.06 to 82.10 and PPOS coefficients fluctuating from −39,737.40 to 4,357.92, illustrating negative to positive fluctuations in the study area. With respect to DPM, there were 669 census tracts that had negative associations with AEDVs, indicating that more DPM in these census tracts may have associated with reduced AEDVs in 28.5% of LACs census tracts. However, the majority of LACs census tracts (71.5%) experienced positive associations between DPM and AEDVs, indicating that more DPM associated with increased AEDVs. Furthermore, 483 census tracts (20.6%) exhibited positive associations between PPOS and AEDVs, indicating that more acres of PPOS may associate with increased AEDVs in these areas. Yet, the majority of LACs census tracts (79.4%) exhibited negative associations, wherein more PPOS was associated with AEDV reductions (Fig. 6).
Fig. 6.
Geographically weighted regression standard residuals of asthma emergency department visits, diesel particulate matter, and public parks and open space.
4. Discussion
The current study expanded research concerning the relationship between DPM and AEDVs by examining the extent to which PPOS may serve to mitigate AEDVs at the census tract unit of analysis. In agreement with the available literature, significant clustering of DPM and AEDVs revealed several hotspots, indicating a concerning spatial relationship between these variables (Mar et al., 2010; McEntee and Ogneva-Himmelberger, 2008). Furthermore, PPOS hotspot analysis and ensuing geospatial overlay of DPM and AEDV hotspots revealed PPOS disparities in census tracts that intersect those with DPM and AEDV hotspots.
The available literature also aligns with our results indicating that there are: 1) significant spatial associations between DPM and AEDVs, and 2) these associations tend to be stronger among ethnocultural minority communities, with significant AEDV escalations in African American, AIAN, and NHPI communities (Gonzalez et al., 2011; Houston et al., 2004; Los Angeles Collaborative for Environmental Health and Justice, 2010; Mar et al., 2010; McEntee and Ogneva-Himmelberger, 2008; Morello-Frosch et al., 2001; Morello-Frosch et al., 2002; Ristovski et al., 2012; Valavanidis et al., 2008). These findings suggest that ethnocultural minority communities, particularly African American, American Indian/Alaska Native, and Native Hawaiian/Pacific Islander communities, would benefit from 1) ongoing DPM and broader air quality monitoring at the census tract level, 2) DPM reduction programs that limit heavy-truck traffic in ethnocultural minority communities with high concentrations of AEDVs, and 3) local health clinics specializing in community asthma treatment and prevention.
Promisingly, when controlling for poverty, children below the age of 10, and race/ethnicity, PPOS generally predicted AEDV reductions, confirming the potential public health benefits of PPOS. Therefore, public parks and open space in the LAC context may, in part, serve to mitigate poor asthma outcomes. This is the first study to identify AEDV reductions in census tracts where there are higher concentrations of PPOS. Thus, in addition to reducing DPM and improving access to public health clinics, community members living in census tracts with high concentrations of DPM and AEDVs may benefit from improved access to public parks and open space, as 79% of the census tracts in the current study revealed negative associations between AEDVs and PPOS. Thus, associated public health improvements concerning community asthma outcomes may be achieved by improving access to health-promoting ecosystem services that tend to improve air quality, such as features of the natural environment (e.g., treetop canopy cover) concomitant with PPOS (Baró et al., 2014; Carlsten and Rider, 2017; Derkzen et al., 2015; Van Dillen et al., 2011).
Public parks and open spaces have been associated with a number of additional public health outcomes—e.g., reduced risk of obesity and heart disease, and improved mental health and wellbeing—providing an evidence-base for improving public health outcomes in at-risk communities (Cohen et al., 2013; Douglas et al., 2018; Kaczynski et al., 2014; Wolch et al., 2014). Unfortunately, in the LAC context, ethnocultural minority communities are not receiving such benefits, as LAC's communities of color experience inequitable access to PPOS compared to predominantly affluent and White communities (García et al., 2016; Wolch et al., 2002). Such evidence provides a grounded argument for improving access to PPOS in ethnocultural minority communities experiencing a range of poor health outcomes associated with built, natural, and social environments.
There are several limitations to the current study. First, this study may have benefitted from multilevel analyses accounting for additional contextual conditions—e.g., access to health clinics and additional resources—as well as community exposure to additional air pollutants, such as NOx and Ozone. Second, an analysis of tree top canopy cover may provide additional understandings about the potential for greenspace to mitigate poor respiratory health outcomes. Third, the available DPM data does not account for neighborhood and local-scale emissions dispersion. Fourth, we recognize that emergency department visits at the census tract unit of analysis may not fully characterize asthma burdens, as some residents receive preventive and emergency services outside of their immediate locales. Fifth, large portions of PPOS in the current analysis included national parks that may not directly benefit community health. Sixth, data employed in the current study, while close in years, did not overlap in all cases. Results may be strengthened with data collected within the same timeframe. Seventh, by using tract-level census data, the current results assume resident proximal exposure to DPM, whereas prior studies indicate significance of distal exposure (Setton et al., 2011; Steinle et al., 2013). Eighth, the current study relied on cross-sectional rather than longitudinal data. Finally, significance levels were included in the OLS model only, as GWR data were intended to provide visual mapping of localized spatial relationships.
5. Conclusions
Findings from this novel study indicate that, when controlling for poverty, children, and race/ethnicity, DPM and acres of PPOS are associated with AEDVs. This suggests that reducing exposure to DPM and increasing acres of PPOS may serve to improve asthma outcomes, particularly in ethnocultural minority communities. Thus, it will behoove future public health research to explore the promotion and preservation of PPOS as a means for redressing asthma, in part, and improving community health more broadly. As such, the specific built and natural environment characteristics of PPOS—e.g., tree top canopy, hedges, open fields, etc.—that potentially contribute to asthma reductions warrant further investigation. Furthermore, research taking a multilevel, contextual approach concerning community access to public parks and open space may reveal additional social and environmental conditions that may encourage or encumber access to health promoting built and natural environments.
Conflicts of interest
None
Acknowledgements
We would like to thank the National Science Foundation funded Germinating Transformative Climate Change Research through Diversity program for creating a collaborative space for all authors included in this paper. Their efforts provided the impetus for the formation of our current research team.
References
- Akinbami L.J., Moorman J.E., Bailey C., Zahran H.S., King M., Johnson C.A., Liu X. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012;94:1–8. [PubMed] [Google Scholar]
- Aligne C., Auinger P., Byrd R.S., Weitzman M. Risk factors for pediatric asthma: contributions of poverty, race, and urban residence. Am. J. Respir. Crit. Care Med. 2000;162(3):873–877. doi: 10.1164/ajrccm.162.3.9908085. [DOI] [PubMed] [Google Scholar]
- Anselin L. Under the hood: issues in the specification and interpretation of spatial regression models. Agric. Econ. 2002;27(3):247–267. [Google Scholar]
- Baró F., Chaparro L., Gómez-Baggethun E., Langemeyer J., Nowak D.J., Terradas J. Contribution of ecosystem services to air quality and climate change mitigation policies: the case of urban forests in Barcelona, Spain. AMBIO. 2014;43(4):466–479. doi: 10.1007/s13280-014-0507-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunekreef B. The great indoors. Thorax. 2004;59(9):729–730. doi: 10.1136/thx.2004.024091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunsdon C., Fotheringham A.S., Charlton M.E. Geographically weighted regression: a method for exploring spatial nonstationarity. Geogr. Anal. 1996;28(4):281–298. [Google Scholar]
- Cagney K.A., Browning C.R. Exploring neighborhood-level variation in asthma and other respiratory diseases. J. Gen. Intern. Med. 2004;19(3):229–236. doi: 10.1111/j.1525-1497.2004.30359.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARB California air resources board mobile source emissions inventory. 2013. https://www.arb.ca.gov/msei/categories.htm
- Carlsten C., Rider C.F. Traffic-related air pollution and allergic disease: an update in the context of global urbanization. Curr. Opin. Allergy Clin. Immunol. 2017;17(2):85–89. doi: 10.1097/ACI.0000000000000351. [DOI] [PubMed] [Google Scholar]
- Carr W., Zeitel L., Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am. J. Public Health. 1992;82(1):59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CEHTP California environmental health tracking program asthma data. 2014. http://www.cehtp.org/page/asthma
- Clark N.A., Demers P.A., Karr C.J., Koehoorn M., Lencar C., Tamburic L., Brauer M. Effect of early life exposure to air pollution on development of childhood asthma. Environ. Health Perspect. 2010;118(2):284–290. doi: 10.1289/ehp.0900916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D.A., Lapham S., Evenson K.R., Williamson S., Golinelli D., Ward P.…McKenzie T.L. Use of neighbourhood parks: does socio-economic status matter? A four-city study. Public Health. 2013;127(4):325–332. doi: 10.1016/j.puhe.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P., Potchter O., Schnell I. The impact of an urban park on air pollution and noise levels in the Mediterranean city of Tel-Aviv, Israel. Environ. Pollut. 2014;195:73–83. doi: 10.1016/j.envpol.2014.08.015. [DOI] [PubMed] [Google Scholar]
- Dadvand P., Villanueva C.M., Font-Ribera L., Martinez D., Basagaña X., Belmonte J., Nieuwenhuijsen M.J. Risks and benefits of green spaces for children: a cross-sectional study of associations with sedentary behavior, obesity, asthma, and allergy. Environ. Health Perspect. 2014;122(12):1329–1335. doi: 10.1289/ehp.1308038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Parks and Recreation Countywide Parks and Open Space Los Angeles county GIS data portal. 2017. https://egis3.lacounty.gov/dataportal/2016/10/25/department-of-parks-and-recreation-county-parks-and-open-space/
- Derkzen M.L., Teeffelen A.J.A. van, Verburg P.H. Review: quantifying urban ecosystem services based on high-resolution data of urban green space: an assessment for Rotterdam, the Netherlands. J. Appl. Ecol. 2015;52(4):1020–1032. [Google Scholar]
- Douglas J.A., Briones M.D., Bauer E.Z., Trujillo M., Lopez M., Subica A.M. Social and environmental determinants of physical activity in urban parks: testing a neighborhood disorder model. Prev. Med. 2018;109:119–124. doi: 10.1016/j.ypmed.2018.01.013. [DOI] [PubMed] [Google Scholar]
- Fan J., Li S., Fan C., Bai Z., Yang K. The impact of PM2.5 on asthma emergency department visits: a systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2016;23(1):843–850. doi: 10.1007/s11356-015-5321-x. [DOI] [PubMed] [Google Scholar]
- Feng X., Astell-Burt T. Is neighborhood green space protective against associations between child asthma, neighborhood traffic volume and perceived lack of area safety? Multilevel analysis of 4447 Australian children. Int. J. Environ. Res. Public Health. 2017;14(6):543. doi: 10.3390/ijerph14050543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein J.A., Fuhlbrigge A., Lozano P., Grant E.N., Shulruff R., Arduino K.E., Weiss K.B. Parent-reported environmental exposures and environmental control measures for children with asthma. Archives of Pediatrics & Adolescent Medicine. 2002;156(3):258–264. doi: 10.1001/archpedi.156.3.258. [DOI] [PubMed] [Google Scholar]
- Fotheringham A.S., Charlton M.E., Brunsdon C. Geographically weighted regression: a natural evolution of the expansion method for spatial data analysis. Environment and Planning A: Economy and Space. 1998;30(11):1905–1927. [Google Scholar]
- García J.J., Gee G.C., Jones M. A critical race theory analysis of public park features in Latino immigrant neighborhoods. Du Bois Review: Social Science Research on Race. 2016;13(02):397–411. [Google Scholar]
- Gelber L.E., Seltzer L.H., Bouzoukis J.K., Pollart S.M., Chapman M.D., Platts-Mills T.A.E. Sensitization and exposure to indoor allergens as risk factors for asthma among patients presenting to hospital. Am. Rev. Respir. Dis. 1993;147(3):573–578. doi: 10.1164/ajrccm/147.3.573. [DOI] [PubMed] [Google Scholar]
- Gonzalez P.A., Minkler M., Garcia A.P., Gordon M., Garzón C., Palaniappan M., Beveridge B. Community-based participatory research and policy advocacy to reduce diesel exposure in West Oakland, California. Am. J. Public Health. 2011;101(S1):S166–S175. doi: 10.2105/AJPH.2010.196204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodan W.M., Bernard W.R. Evaluating the contribution of PM2.5 precursor gases and re-entrained road emissions to mobile source PM2.5 particulate matter emissions. 2017. https://www3.epa.gov/ttnchie1/conference/ei13/mobile/hodan.pdf
- Holgate S.T. Genetic and environmental interaction in allergy and asthma. J. Allergy Clin. Immunol. 1999;104(6):1139–1146. doi: 10.1016/S0091-6749(99)70005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holgate S.T., Davies D.E., Powell R.M., Howarth P.H., Haitchi H.M., Holloway J.W. Local genetic and environmental factors in asthma disease pathogenesis: chronicity and persistence mechanisms. Eur. Respir. J. 2007;29(4):793–803. doi: 10.1183/09031936.00087506. [DOI] [PubMed] [Google Scholar]
- Houston D., Wu J., Ong P., Winer A. Structural disparities of urban traffic in Southern California: implications for vehicle-related air pollution exposure in minority and high-poverty neighborhoods. J. Urban Aff. 2004;26(5):565–592. [Google Scholar]
- Houston D., Li W., Wu J. Disparities in exposure to automobile and truck traffic and vehicle emissions near the Los Angeles–Long Beach Port Complex. Am. J. Public Health. 2014;104(1):156–164. doi: 10.2105/AJPH.2012.301120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huss K., Adkinson N.F., Eggleston P.A., Dawson C., Natta M.L.V., Hamilton R.G. House dust mite and cockroach exposure are strong risk factors for positive allergy skin test responses in the Childhood Asthma Management Program. J. Allergy Clin. Immunol. 2001;107(1):48–54. doi: 10.1067/mai.2001.111146. [DOI] [PubMed] [Google Scholar]
- Jennings V., Johnson Gaither C., Gragg R.S. Promoting environmental justice through urban green space access: a synopsis. Environmental Justice. 2012;5(1):1–7. [Google Scholar]
- Kaczynski, A. T., Besenyi, G. M., Stanis, S. A. W., Koohsari, M. J., Oestman, K. B., Bergstrom, R., … Reis, R. S. (2014). Are park proximity and park features related to park use and park-based physical activity among adults? Variations by multiple socio-demographic characteristics. Int. J. Behav. Nutr. Phys. Act., 11(1), 146. doi: 10.1186/s12966-014-0146-4. [DOI] [PMC free article] [PubMed]
- Kanchongkittiphon Watcharoot, Mendell Mark J., Gaffin Jonathan M., Wang Grace, Phipatanakul Wanda. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ. Health Perspect. 2015;123(1):6–20. doi: 10.1289/ehp.1307922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Los Angeles Collaborative for Environmental Health and Justice . Liberty Hill Foundation; Santa Monica, CA: 2010. Hidden Hazards: A Call to Action for Healthy, Livable Communities.https://dornsife.usc.edu/assets/sites/242/docs/hidden-hazards-low-res-version.pdf Retrieved from. [Google Scholar]
- Manes F., Marando F., Capotorti G., Blasi C., Salvatori E., Fusaro L., Munafò M. Regulating ecosystem services of forests in ten Italian metropolitan cities: air quality improvement by PM10 and O3 removal. Ecol. Indic. 2016;67:425–440. [Google Scholar]
- Mar T.F., Koenig J.Q., Primomo J. Associations between asthma emergency visits and particulate matter sources, including diesel emissions from stationary generators in Tacoma, Washington. Inhal. Toxicol. 2010;(6):445. doi: 10.3109/08958370903575774. [DOI] [PubMed] [Google Scholar]
- Mar Therese F., Koenig J.Q. Relationship between visits to emergency departments for asthma and ozone exposure in greater Seattle, Washington. Ann. Allergy Asthma Immunol. 2009;103(6):474–479. doi: 10.1016/S1081-1206(10)60263-3. [DOI] [PubMed] [Google Scholar]
- Marder D., Targonski P., Orris P., Persky V., Addington W. Effect of racial and socioeconomic factors on asthma mortality in Chicago. CHEST. 1992;101(6):426s–429s. doi: 10.1378/chest.101.6_supplement.426s. [DOI] [PubMed] [Google Scholar]
- Matthews S.A., Yang T.C. Mapping the results of local statistics: using geographically weighted regression. Demogr. Res. 2012;26:151–166. doi: 10.4054/DemRes.2012.26.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEntee J.C., Ogneva-Himmelberger Y. Diesel particulate matter, lung cancer, and asthma incidences along major traffic corridors in MA, USA: a GIS analysis. Health & Place. 2008;14(4):817–828. doi: 10.1016/j.healthplace.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Mitchell R., Popham F. Greenspace, urbanity and health: relationships in England. J. Epidemiol. Community Health. 2007;61(8):681–683. doi: 10.1136/jech.2006.053553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R., Pastor M., Sadd J. Environmental justice and southern California's “riskscape”. Urban Aff. Rev. 2001;36(4):551–578. [Google Scholar]
- Morello-Frosch R., Pastor M., Porras C., Sadd J. Environmental justice and regional inequality in southern California: implications for future research. Environ. Health Perspect. 2002;110(Suppl. 2):149–154. doi: 10.1289/ehp.02110s2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris G., Sharon N., Young P., Koenig J.Q., Larson T.V., Sheppard L., Stout J.W. An association between fine particles and asthma emergency department visits for children in Seattle. Environ. Health Perspect. 1999;(6):489. doi: 10.1289/ehp.99107489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak D.J., Hirabayashi S., Bodine A., Hoehn R. Modeled PM2.5 removal by trees in ten U.S. cities and associated health effects. Environ. Pollut. 2013;178:395–402. doi: 10.1016/j.envpol.2013.03.050. [DOI] [PubMed] [Google Scholar]
- Nowak D.J., Hirabayashi S., Bodine A., Greenfield E. Tree and forest effects on air quality and human health in the United States. Environ. Pollut. 2014;193:119–129. doi: 10.1016/j.envpol.2014.05.028. [DOI] [PubMed] [Google Scholar]
- Office of Environmetnal Health Hazard Assessment Draft California communities environmetnal health screening tool, version 2.0. 2016. https://oehha.ca.gov/calenviroscreen/report/calenviroscreen-version-20
- Oshan T., Fotheringham A. International Conference on GIScience Short Paper Proceedings. 2016. A closer examination of spatial-filter-based local models; p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomés A., Chapman M.D., Wünschmann S. Indoor allergens and allergic respiratory disease. Curr Allergy Asthma Rep. 2016;16(6):43. doi: 10.1007/s11882-016-0622-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigolon A. A complex landscape of inequity in access to urban parks: A literature review. Landsc. Urban Plan. 2016;153:160–169. [Google Scholar]
- Ristovski Z.D., Miljevic B., Surawski N.C., Morawska L., Fong K.M., Goh F., Yang I.A. Respiratory health effects of diesel particulate matter. Respirology. 2012;17(2):201–212. doi: 10.1111/j.1440-1843.2011.02109.x. [DOI] [PubMed] [Google Scholar]
- Salo P.M., Arbes S.J., Crockett P.W., Thorne P.S., Cohn R.D., Zeldin D.C. Exposure to multiple indoor allergens in US homes and its relationship to asthma. J. Allergy Clin. Immunol. 2008;121(3):678–684.e2. doi: 10.1016/j.jaci.2007.12.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sbihi H., Tamburic L., Koehoorn M., Brauer M. Greenness and incident childhood asthma: a 10-year follow-up in a population-based birth cohort. Am. J. Respir. Crit. Care Med. 2015;192(9):1131–1133. doi: 10.1164/rccm.201504-0707LE. [DOI] [PubMed] [Google Scholar]
- Schwartz J., Gold D., Dockery D.W., Weiss S.T., Speizer F.E. Predictors of asthma and persistent wheeze in a national sample of children in the United States: association with social class, perinatal events, and race. Am. Rev. Respir. Dis. 1990;142(3):555–562. doi: 10.1164/ajrccm/142.3.555. [DOI] [PubMed] [Google Scholar]
- Selmi W., Weber C., Rivière E., Blond N., Mehdi L., Nowak D. Air pollution removal by trees in public green spaces in Strasbourg city, France. Urban For. Urban Green. 2016;17:192–201. [Google Scholar]
- Setton E., Marshall J.D., Brauer M., Lundquist K.R., Hystad P., Keller P., Cloutier-Fisher D. The impact of daily mobility on exposure to traffic-related air pollution and health effect estimates. Journal of Exposure Science & Environmental Epidemiology. 2011;21(1):42–48. doi: 10.1038/jes.2010.14. [DOI] [PubMed] [Google Scholar]
- Sharma K.I., Toh J., Desai T., Shum M., Patel P., Rosenstreich D.L., Jariwala S.P. The association between pollutant levels and asthma-related emergency department visits in the Bronx after the World Trade Center attacks. J. Allergy Clin. Immunol. 2016;137(2, Supplement):AB6. doi: 10.1080/02770903.2018.1531989. [DOI] [PubMed] [Google Scholar]
- Slaughter J.C., Kim E., Sheppard L., Sullivan J.H., Larson T.V., Claiborn C. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. Journal of Exposure Analysis & Environmental Epidemiology. 2005;15(2):153–159. doi: 10.1038/sj.jea.7500382. [DOI] [PubMed] [Google Scholar]
- South Coast Air Quality Management District . 2016. Final 2016 Air Quality Management Plan. [Google Scholar]
- Steinle S., Reis S., Sabel C.E. Quantifying human exposure to air pollution—moving from static monitoring to spatio-temporally resolved personal exposure assessment. Sci. Total Environ. 2013;443:184–193. doi: 10.1016/j.scitotenv.2012.10.098. [DOI] [PubMed] [Google Scholar]
- Think Health LA (2017). Los Angeles age-adjusted ER rate due to asthma. http://www.thinkhealthla.org/index.php?module=indicators&controller=index&action=view&indicatorId=126&localeId=256. Published August 2017. Accessed January 5, 2018.
- Torgerson, D. G., Ampleford, E. J., Chiu, G. Y., Gauderman, W. J., Gignoux, C. R., Graves, P. E., … Nicolae, D. L. (2011). Meta-analysis of genome-wide association studies of asthma in ethnically diverse North American populations. Nat. Genet., 43(9), 887–892. doi: 10.1038/ng.888. [DOI] [PMC free article] [PubMed]
- U.S. Census Bureau American FactFinder - search. 2010. http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t Available from.
- U.S. Census Bureau . 2015. American FactFinder - Search.http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t Available from: [Google Scholar]
- Valavanidis A., Fiotakis K., Vlachogianni T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. Journal of Environmental Science and Health, Part C. 2008;26(4):339–362. doi: 10.1080/10590500802494538. [DOI] [PubMed] [Google Scholar]
- Van Dillen, S. M. E., Vries, S. de, Groenewegen, P. P., & Spreeuwenberg, P. (2011). Greenspace in urban neighbourhoods and residents' health: adding quality to quantity. J. Epidemiol. Community Health, jech.2009.104695. doi: 10.1136/jech.2009.104695. [DOI] [PubMed]
- Wang L., Koenig J.Q., Mar T.F., Primomo J. Associations between asthma emergency visits and particulate matter sources, including diesel emissions from stationary generators in Tacoma, Washington. Inhal. Toxicol. 2010;22(6):445–448. doi: 10.3109/08958370903575774. [DOI] [PubMed] [Google Scholar]
- Warner A.M., Bjbrksten B., Munir A.K.M., Möller C., Schou C., Kjellman N.-L.M. Childhood asthma and exposure to indoor allergens: lowmite levels are associated with sensitivity. Pediatr. Allergy Immunol. 1996;7(2):61–67. doi: 10.1111/j.1399-3038.1996.tb00108.x. [DOI] [PubMed] [Google Scholar]
- Wiesch D.G., Meyers D.A., Bleecker E.R. Genetics of asthma. J. Allergy Clin. Immunol. 1999;104(5):895–901. doi: 10.1016/s0091-6749(99)70065-5. [DOI] [PubMed] [Google Scholar]
- Wolch J., Wilson J.P., Fehrenbach J. Parks and park funding in Los Angeles: an equity-mapping analysis. Urban Geogr. 2002;26(1):4–35. [Google Scholar]
- Wolch J.R., Byrne J., Newell J.P. Urban green space, public health, and environmental justice: the challenge of making cities ‘just green enough’. Landsc. Urban Plan. 2014;125:234–244. [Google Scholar]
- Yang J., McBride J., Zhou J., Sun Z. The urban forest in Beijing and its role in air pollution reduction. Urban For. Urban Green. 2005;3(2):65–78. [Google Scholar]