Abstract
BACKGROUND
There is a high risk for sudden cardiac death (SCD) in certain patient groups that would not meet criteria for implantable cardioverter defibrillator (ICD) therapy. In conditions such as hypertrophic cardiomyopathy (HCM) there are clear risk scores that help define patients who are high risk for SCD and would benefit from ICD therapy. There are however many areas of uncertainty such as certain patients post myocardial infarction (MI). These patients are high risk for SCD but there is no clear tool for risk stratifying such patients.
AIM
To assess risk factors for sudden cardiac death in major cardiac disorders and to help select patients who might benefit from Wearable cardiac defibrillators (WCD).
METHODS
A literature search was performed looking for risk factors for SCD in patients post-MI, patients with left ventricular systolic dysfunction (LVSD), HCM, long QT syndrome (LQTS). There were 41 studies included and risk factors and the relative risks for SCD were compiled in table form.
RESULTS
We extracted data on relative risk for SCD of specific variables such as age, gender, ejection fraction. The greatest risk factors for SCD in post MI patients was the presence of diabetes [Hazard ratio (HR) 1.90-3.80], in patient with LVSD was ventricular tachycardia (Relative risk 3.50), in LQTS was a prolonged QTc (HR 36.53) and in patients with HCM was LVH greater than 20 mm (HR 3.10). A proportion of patients currently not suitable for ICD might benefit from a WCD
CONCLUSION
There is a very high risk of SCD post MI, in patients with LVSD, HCM and LQTS even in those who do not meet criteria for ICD implantation. These patients may be candidates for a WCD. The development of more sensitive risk calculators to predict SCD is necessary in these patients to help guide treatment.
Keywords: Sudden cardiac death, Wearable cardiac defibrillators, Myocardial infarction, Hypertrophic cardiomyopathy, Left ventricular systolic dysfunction
Core tip: This article looks at the risk factors for sudden cardiac death (SCD) in patients post myocardial infarction, patients with left ventricular systolic dysfunction, patients with hypertrophic cardiomyopathy, patients with long QT syndrome and the relative risk for sudden cardiac death of these risk factors. This is compared to the absolute risk of SCD for these conditions. We reviewed the recommendations from current guidelines and we outline where patients are at high risk for SCD but are not eligible for implantable cardioverter defibrillator implantation. The risk factors identified in this study can be used to select patients who may benefit from Wearable cardiac defibrillators therapy.
INTRODUCTION
Sudden cardiac death (SCD) is a major global health problem estimated to account for 15%-20% of death[1]. The mechanism of SCD has changed substantially over the last decade with ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT) accounting for between 23%-36% of out-of-hospital cardiac arrests[2,3]. This compares to 75% of cases of SCD in the 1980’s and early 1990’s[4,5]. The decline in SCD due to VT/VF is partly due to improved medical care such as the use of beta blockers and implantable cardioverter defibrillators (ICD)[6,7]. Thus VF and pulseless VT are potentially treatable heart rhythms particularly if patients are given an early DC shock with return of an organised rhythm in up to 70% of cases after a single biphasic shock[8]. This has led to the development of multiple measures such as automated external defibrillators in public places, ICD therapy and wearable cardioverter defibrillators (WCD) to reduce the rate of preventable death from VF/VT.
History of defibrillation
The first successful closed chest direct current cardioversion of ventricular fibrillation was performed by Paul Zoll in the 1950’s[9]. This was initially a monophasic shock but more recently biphasic shocks are used. Biphasic waveforms have superior efficacy to monophasic pulses[8] and the European resuscitation council recommend a first shock at 150-200 J with subsequent shocks at a higher energy level if the device allows and the arrhythmia remains uncorrected[10]. Return of sinus rhythm and spontaneous circulation after administration of biphasic shocks occurs in up to 70% in patients with VF or VT[8]. This highlights the high efficacy of this relatively simple treatment.
The first ICD was implanted in a patient in 1980 by Mirowski et al[11]. There have since been multiple studies proving the benefit of ICDs in preventing SCD and reducing all-cause mortality. These include primary prevention studies which show a reduction in mortality from SCD of between 23%-54%[12-16](Table 1) and secondary prevention studies which show a reduction in mortality from SCD of between 20%-28%[17-19](Table 2). Current guidelines based on the results of these and other studies recommend the insertion of ICD in patients more than 40 d post myocardial infarction (MI) with severe LVSD (ejection fraction less than 35%), patients with severe LVSD and in several other situations such as high risk hypertrophic cardiomyopathy (HCM) patients, patients with long QT syndrome (LQTS) with a history of cardiac arrest. These guidelines advise against inserting an ICD for patients who survive sustained VT or VF within the first 48 h of an MI unless they have pre-existing LV impairment and are on optimal medical therapy already or they have incomplete revascularisation, as it is felt that tachyarrhythmia within this period is most likely due to the acute coronary obstruction and cardiac injury[20].
Table 1.
Primary prevention implantable cardioverter defibrillator studies
| Study | Intervention/control group | Inclusion criteria | Risk reduction of SCD with ICD |
| Multicenter Automatic Defibrillator Implantation Trial[12] | ICD vs antiarrhythmic drug | Previous MI; EF ≤ 35%; nsVT; positive findings on EPS | 54% (P = 0.001) |
| Multicenter Unsustained Tachycardia Trial[13] | EP-guided therapy vs placebo | Coronary disease; EF ≤ 40%; Non-sustained VT; inducible VT at EPS | 51% (P = 0.001) |
| Multicenter Automatic Defibrillator Implantation Trial 2[14] | ICD vs optimal pharmacological treatment | Prior MI EF ≤ 30% | 31% (P = 0.02) |
| Sudden Cardiac Death in Heart Failure Trial[15] | ICD vs optimal pharmacological therapy vs optimal pharmacological therapy + amiodarone | Ischaemic and non-ischaemic cardiomyopathy; EF ≤ 35% | 23% (P = 0.007) |
| Defibrillator implantation in patients with nonischemic systolic heart failure[16] | ICD vs optimal pharmacological therapy | Non-ischaemic cardiomyopathy; EF ≤ 35% | 50% (P = 0.005) |
SCD: Sudden cardiac death; ICD: Implantable cardioverter defibrillator; EF: Ejection fraction; EP: Electrophysiology; MI: Myocardial infarction; EPS: Electrophysiology studies; VT: Ventricular tachycardia.
Table 2.
Secondary prevention implantable cardioverter defibrillator studies
| Study | Intervention/control group | Inclusion criteria | Risk reduction with ICD |
| Antiarrhythmics Versus Implantable Defibrillators study[17] | ICD vs antiarrhythmic drugs | Resuscitated from near-fatal VF or post-cardioversion from sustained VT | 28% (P = 0.02) |
| Canadian Implantable Defibrillator Study[18] | ICD vs amiodarone | Resuscitated VF or VT or with unmonitored syncope | 20% (P = 0.14) |
| Cardiac Arrest Study Hamburg[19] | ICD vs amiodarone vs metoprolol | Survivors of cardiac arrest secondary to documented ventricular arrhythmias | 23% (P = 0.08) |
ICD: Implantable cardioverter defibrillator; VF: Ventricular fibrillation; VT: Ventricular tachycardia.
In other patients an ICD may not be possible due to infection or lack of vascular access or patient preference. Thus, some high risk patients who would warrant an ICD do not have one. In order to address this, the WCD was developed. The WCD has been in development since 1986 and had been tested for 17 years prior to it receiving the Food and Drug Administration approval in 2002[21]. The WCD is a device contained within a vest worn under a patient’s clothes which records a patient’s rhythm and delivers a shock if a shockable rhythm occurs[22]. This has provided a much lower risk solution to ICD implantation in selected patients. Current guidelines recommend considering a WCD or ICD post MI within 40 d of their MI in patients with incomplete revascularisation, VT or VF > 48 h post MI or pre-existing LVSD[23]. Additional groups of patients that could benefit from a WCD include patients with channelopathies such as LQTS who have not suffered a VT or VF event but have high risk features, patients with HCM who have intermediate risk features but not yet achieving criteria for ICD implantation, and also patients with infected ICDs could be offered a WCD once their ICD has been removed and they are awaiting ICD re-implantation. WCD do however come with a risk of inappropriate shocks and their efficacy can be reduced due to a lack of patient compliance.
The aim of this review is to use existing literature to identify risk factors for SCD that may help identify patients who may benefit from a WCD and to discuss the potential role that WCDs could play in reducing the risk of SCD in selected patient groups who do not currently meet guidelines for ICD implantation.
MATERIALS AND METHODS
Study design
This review included available data on risk factors for SCD in predefined patient groups. All odds ratio (OR), relative risk (RR), Exp(b) and hazard ratio (HR) were rounded to 2 decimal places for consistency. OR is a statistic defined as the ratio of the odds of variable A in the presence of variable B and the odds of variable A without the presence of variable B. RR is the ratio of the probability of an outcome in an exposed group to the probability of an outcome in an unexposed group. The HR is an expression of the hazard or chance of events occurring in the treatment arm as a ratio of the hazard of the events occurring in the control arm
Inclusion and exclusion criteria
All studies that reported risk factors for SCD in patients with LVSD, LQTS, HCM or post MI. There was no restriction on age, gender, geographical area or date of publication. Studies reported in English. Any studies where the risk of SCD was not quantified by either a HR, OR or RR were excluded.
Search strategy
A literature search was performed in 4 main groups of patients: Search terms included: (risk of SCD* or risk factors for SCD* or SCD* or female gender and outcome* or mortality in patients* or mortality in women* or risk stratification for SCD* or risk of cardiac arrest* or atrial fibrillation and mortality* or echocardiographic predictors of outcome* or risk of death* or COPD and mortality* or prognosis of heart failure* or risk of death in patients*) and (post myocardial infarction* or after myocardial infarction* or after acute st elevation myocardial infarction* or after ST elevation myocardial infarction* or with inferior myocardial infarction* or following myocardial infarction* or after myocardial infarction* or myocardial scarring* or electrocardiographic abnormalities* or patients with hypertrophic cardiomyopathy* or heart failure* or patients with heart failure* or left ventricular dysfunction* or after hospitalization for heart failure* or in the community* or new diagnosis of heart failure* or LQTS*).
The risk factor in each group that was associated with SCD, was then tabulated along with the relevant studies that supported this finding.
RESULTS
Results of literature search
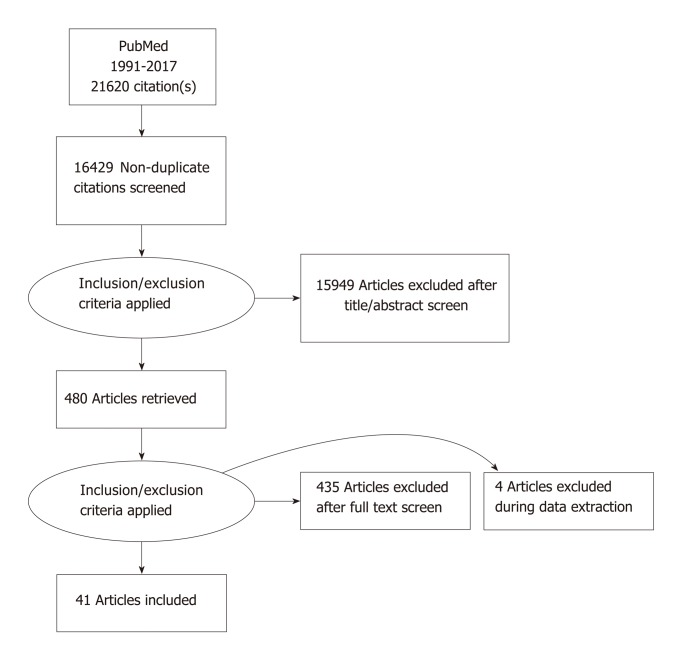
The initial search strategy produced 21620 articles. Removal of duplicates and screening of the papers reduced the number to 480 articles. A further 435 papers were removed after reading of the full text. During data extraction an additional 4 papers were removed as a result of not having the prerequisite data available in the correct form. Forty one papers were included in the final data analysis (Figure 1)
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Risk of sudden cardiac death post myocardial infarction
In patients post MI, 16 studies were identified involving a total of 250766 patients[24-39](Table 3). The absolute risk of SCD in these studies varied from around 4.9%-8%[24,26,30,33]. The absolute risk of SCD was 4.9% in the first month post-MI and decreased thereafter[24]. Another study showed a cumulative risk of SCD at 1 year to be 5.3%[26]. One study showed a risk of SCD of 7% at 30 d and 11% at 2 years[30]. Another study showed a risk of SCD at 4% in those with EF > 35% and 8% in those with EF < 35% at one year[33].
Table 3.
Risk factors for sudden cardiac death post myocardial infarction
| Risk factor studied | Relative risk of SCD | P value | Absolute SCD risk in cohort | Study size | Year | Country |
| Age | ||||||
| Rao et al[24] | OR 1.03 (1.00-1.05) (Increasing age) | 0.0163 | 4.9% in the 1st month post MI | 929 | 2012 | India |
| Mehta et al[25] | OR 0.12; Standard error = 0.02 (Age per 1 year increase) | 0.0001 | 2948 | 2001 | North America | |
| Abildstrom et al[26] | OR 1.56 (1.43–1.70) (Age per 10 years) | < 0.0001 | 5.3% at 1 year | 5983 | 2002 | Denmark |
| Female gender | ||||||
| Rao et al[24] | OR 1.78 (1.02-2.85) | 0.0042 | 4.9% in the 1st month post MI | 929 | 2012 | India |
| Greenland et al[27] | OR 1.72 (1.45-2.04) | < 0.0005 | 5839 | 1991 | Israel | |
| Greenland et al[27] | OR 1.32 (1.05-1.66) (Death at 1 year) | < 0.03 | 5839 | 1991 | Israel | |
| Ghaffari et al[28] | OR 1.76 (1.22–2.54) (univariate analysis) | 0.002 | 1017 | 2017 | Iran | |
| Ghaffari et al[28] | OR 1.19 (0.77–1.8) (multivariate analysis) | 0.407 | 1017 | 2017 | Iran | |
| Macintyre et al[29] | OR 1.09 (1.06 to 1.13) (Death at 1 year) | < 0.00001 | 201114 | 2001 | UK | |
| Male gender | ||||||
| Abildstrom et al[26] | OR 1.34 (1.11–1.63) | < 0.005 | 5.3% at 1 year | 5983 | 2002 | Denmark |
| LV dysfunction | ||||||
| Rao et al[24] | OR 2.35 (1.09-5.03) (Severe LV dysfunction ≤ 30%) | 0.0292 | 4.9% in the 1st month post MI | 929 | 2012 | India |
| Solomon et al[30] | HR 1.21 (1.10 to 1.30) (LV depression by each 5 percentage points) | 7% at 1 month post MI; 11% at 2 years post MI | 14609 | 2005 | North America, Europe and New Zealand | |
| Klem et al[31] | HR 6.30 (1.40-28.00) (LVEF > 30% and significant scarring > 5% on CMRI compared to no scarring) | 0.02 | 137 | 2012 | USA | |
| Klem et al[31] | HR 3.90 (1.20-13.10) (LVEF ≤ 30% and those with scar > 5% on CMRI compared to those with scarring) | 0.03 | 137 | 2012 | USA | |
| Yeung et al[32] | HR 3.60 (1.46–8.75) (LVEF ≤ 30%) | < 0.01 | 610 | 2012 | China | |
| Chitnis et al[33] | OR 4.51 (2.20–9.24) (LVEF ≤ 35%) | < 0.0001 | 4% in those with EF > 35% at 1 year post MI; 8% in those with EF≤ 35% at 1 year post MI | 929 | 2014 | India |
| Adabag et al[34] | HR 3.64 (1.71-7.75) (presence of heart failure based on the framingham criteria) | < 0.001 | 693 | 2008 | USA | |
| Right ventricular involvement | ||||||
| Mehta et al[25] | OR 3.20 (2.40-4.10) | < 0.00001 | 2948 | 2001 | Canada | |
| Diabetes | ||||||
| Yeung et al[32] | HR 1.90 (1.04–3.40) | 0.04 | 610 | 2012 | China | |
| Junttila et al[35] | HR 3.80 (2.40–5.80) | < 0.001 | 3276 | 2010 | Finland | |
| Ventricular arrythmia | ||||||
| Maggioni et al[36] | RR 2.24 (1.22-4.08) (more than 10 premature ventricular beats per hour) | 0.002 | 8676 | 1993 | Italy | |
| Maggioni et al[36] | RR 1.20 (0.80-1.79) (NSVT) | 8676 | 1993 | Italy | ||
| Mäkikallio et al[37] | HR 2.40 (1.30–4.40) (Ventricular premature complexes 10/h) | 0.0049 | 2130 | 2005 | Finland | |
| Mäkikallio et al[37] | HR 3.30 (1.70–6.50) (NSVT) | < 0.0005 | 2130 | 2005 | Finland | |
| ECG features | ||||||
| Mäkikallio et al[37] | HR 3.30 (1.70–6.50) (QRS ≥ 120 ms) | 0.0004 | 2130 | 2005 | Finland | |
| Zimetbaum et al[38] | HR 1.44 (1.11-1.88) (Non-specific intraventricular conduction delay) | 0.0069 | 1638 | 2004 | USA | |
| Zimetbaum et al[38] | HR 1.49 (1.02-2.17) (LBBB) | 0.0400 | 1638 | 2004 | USA | |
| Zimetbaum et al[38] | HR 1.35 (1.08-1.69) (LVH) | 0.0082 | 1638 | 2004 | USA | |
| Siscovick et al[39] | OR 1.40 (1.00-2.00) (LVH) | 0.02 | 688 | 1996 | USA | |
SCD: Sudden cardiac death; MI: Myocardial infarction; HR: Hazard ratio; OR: Odds ratio; LV: Left ventricular; EF: Ejection fraction.
Several risk factors for SCD were identified post MI in order of decreasing magnitude: diabetes (HR 1.90-3.80), LVSD (HR 1.21 to 3.64), NSVT (HR 3.30), right ventricular involvement (OR 3.20), premature ventricular complexes occurring at a frequency of 10 or more per hour (HR 2.40), female gender (OR 1.09-1.76), older age (OR 1.03-1.56), LBBB (HR 1.49), non-specific intraventricular conduction delay (HR 1.44) and LVH (OR 1.40)[24-39].
Risk factors for sudden cardiac death in heart failure
In patients with heart failure, 15 studies were identified involving a total of 65182 patients[40-54](Table 4). The absolute risk of SCD in these studies varied from 8.8%-23.7%[49,50]. Doval et al[49] showed that in patients with NSVT the risk of SCD at 2 year was 23.7% compared to 8.8% in those who do not have NSVT at 2 years. Teerlink et al[50] showed that the risk of SCD was 13% at 2 years.
Table 4.
Risk factors for sudden cardiac death in heart failure
| Risk factor studies | Relative risk of SCD | P value | Absolute SCD risk in cohort | Study size | Year | Country |
| Age | ||||||
| Lee et al[40] | OR 1.70 (1.45-1.99) (Age per 10 unit increase) | < 0.001 | 4031 | 2003 | Canada | |
| Cowie et al[41] | HR 1.26 (1.01 to 1.57) (Age per 10 year increase) | 0.04 | 220 | 2000 | UK | |
| Taylor et al[42] | HR 1.10 CI 1.09–1.10 (Increasing age) | 6162 | 2012 | UK | ||
| Male gender | ||||||
| Taylor et al[42] | HR 1.50 (1.36–1.66) | 6162 | 2012 | UK | ||
| Vaartjes et al[43] | HR 1.21 (1.14-1.28) at 28 d; HR 1.26 (1.21-1.31) at 1 year; HR 1.28 (1.24-1.31) at year 5 | 29053 | 2010 | Netherlands | ||
| Comorbidities | ||||||
| Lee et al[40] | OR 1.43 (1.03-1.98) 30-day mortality (Cerebrovascular disease) | 0.03 | 4031 | 2003 | Canada | |
| Lee et al[40] | OR 1.66 (1.22-2.27) (COPD) | 0.002 | 4031 | 2003 | Canada | |
| Lee et al[40] | OR, 3.22 (1.08-9.65) (Cirrhosis) | 0.04 | 4031 | 2003 | Canada | |
| Lee et al[40] | OR 2.54 (1.77-3.65) (Dementia) | < 0.001 | 4031 | 2003 | Canada | |
| Lee et al[40] | OR 1.86 (1.28-2.70) (Cancer) | 0.001 | 4031 | 2003 | Canada | |
| Yoshihisa et al[44] | HR 3.01 (1.11–8.63) (COPD) | 0.038 | 378 | 2014 | Japan | |
| Fisher et al[45] | RR 1.10 (1.06-1.14) Death at 1 year; RR 1.40 (1.28-1.52) death at 5 years (COPD) | 9748 | 2015 | USA | ||
| Atrial fibrillation | ||||||
| Taylor et al[44] | HR 1.55 (1.26–1.92) | 6162 | 2012 | UK | ||
| Ahmed et al[46] | HR 1.41 (1.08-1.83) | 944 | 2005 | USA | ||
| Corell et al[47] | HR 1.38 (1.07-1.78) | 0.01 | 1019 | 2007 | Denmark | |
| Middlekauff et al[48] | HR 0.89 (0.55-1.23) | 0.013 | 390 | 1991 | USA | |
| Ventricular arrythmia | ||||||
| Doval et al[49] | RR 2.77 (1.78-4.44) (NSVT) | < 0.001 | 23.7% at 2 years in those with NSVT; 8.8% at 2 years in those without NSVT | 516 | 1996 | Argentina |
| Doval et al[49] | RR 3.37 (1.57-7.25) (Couplets) | < 0.0005 | 23.7% at 2 years in those with NSVT; 8.8% at 2 years in those without NSVT | 516 | 1996 | Argentina |
| Teerlink et al[50] | RR 1.16 (1.09–1.24) (NSVT) | 0.001 | 13% at 2 years | 1080 | 2000 | USA |
| Szabó et al[51] | RR 3.50 (1.54-7.98) (VT) | 0.003 | 211 | 1994 | Netherlands | |
| Szabó et al[51] | RR 2.68 (1.11-6.48) (Freq. VT > 144 beats/min) | 0.029 | 211 | 1994 | Netherlands | |
| Szabó et al[51] | RR 3.89 (1.61-9.43) (Length VT > 2s) | 0.003 | 211 | 1994 | Netherlands | |
| Echocardiographic variables | ||||||
| Taylor et al[42] | HR 1.80 (1.55–2.10) (EF < 40% vs > 50%) | 6162 | 2012 | UK | ||
| Taylor et al[42] | HR 1.29 (1.11–1.50) (EF 40%–50% vs > 50%) | 6162 | 2012 | UK | ||
| Shadman et al[52] | OR 1.15 (EF per 10% decrease) | 0.005 | 9885 | 2015 | USA | |
| Quiñones et al[53] | RR 2.75 (1.62-4.66) (1-SD difference in LV Mass) | 0.0002 | 1209 | 2000 | USA | |
| Quiñones et al[53] | RR 1.84 (1.08-3.15) (1-SD difference in LA Diameter) | 0.03 | 1209 | 2000 | USA | |
| Quiñones et al[53] | RR 2.73 (1.43-5.20) (1-SD difference in lv end systolic dimension) | 0.003 | 1209 | 2000 | USA | |
| Grayburn et al[54] | HR 1.01 (1.00–1.01) (LV end-diastolic volume index) | 0.0012 | 336 | 2005 | USA | |
| Deranged kidney function | ||||||
| Grayburn et al[54] | HR 2.023 (1.24–3.32) | 0.0052 | 336 | 2005 | USA | |
| Cowie et al[41] | HR 2.64 (1.87-3.74) | < 0.001 | 220 | 2000 | UK | |
SCD: Sudden cardiac death; HR: Hazard ratio; OR: Odds ratio; LV: Left ventricular; EF: Ejection fraction.
Several features increasing the risk of SCD were identified in order of decreasing magnitude: VT (RR 3.50), NSVT (RR 2.77-3.89), couplets (RR 3.37), cirrhosis (OR 3.22), 1-SD difference in LV Mass (RR 2.75), a 1-SD difference in LV end systolic dimension (RR 2.73), deranged kidney function (HR 2.02-2.64), dementia (OR 2.54), cancer (OR 1.86), the degree of left ventricular impairment(less than 40%) (HR 1.29-1.80), older age (OR 1.70), COPD (OR 1.66), atrial fibrillation (HR 0.89-1.55), male gender (HR 1.21-1.50) and cerebrovascular disease (OR 1.43)[40-54].
Risk of sudden cardiac death in the long QT syndrome
In patients with LQTS, 5 studies were identified with a total of 9758 patients[55-59](Table 5). The absolute risk of SCD in these studies varied from 4.9%-13%[55,57]. Sauer et al[55] showed that the risk of SCD from the age of 18 until follow-up at the age of 40 was 4.9% in LQTS1, 8.0% in LQTS2 and 4.9% in LQTS3. Priori et al[57] showed that the risk of SCD was 13% over 28 years of follow-up before the age of 40.
Table 5.
Risk factors for sudden cardiac death in the long QT syndrome
| Risk factor studied | Relative risk of SCD | P value | Absolute SCD risk in cohort | Study size | Year | Country |
| Female gender | ||||||
| Sauer et al[55] | HR 2.68 (1.10–6.50) | < 0.05 | Risk between ages of 18-40: LQTS1 4.9%; LQTS2 8.0%; LQTS3 4.9% | 812 | 2007 | USA |
| QTc interval | ||||||
| Sauer et al[55] | HR 3.34 (1.49–7.49) (QTc 500–549 ms vs ≤ 499 ms) | < 0.01 | Risk between ages of 18-40: LQTS1 4.9%; LQTS2 8.0%; LQTS3 4.9% | 812 | 2007 | USA |
| Sauer et al[55] | HR 6.35 (2.82–14.32) (QTc ≥ 550 ms vs ≤ 499 ms) | < 0.01 | Risk between ages of 18-40: LQTS1 4.9%; LQTS2 8.0%; LQTS3 4.9% | 812 | 2007 | USA |
| Moss et al[56] | HR 1.05 (1.02-1.09) (QTc per 0.01 units) | < 0.01 | 1496 | 1991 | USA | |
| Priori et al[57] | RR 5.34 (2.82-10.13) [QTc in the third quartile (469 to 498 ms)] | Risk between ages 12-40 was 13% over 28 years | 580 | 2003 | Italy | |
| Priori et al[57] | RR 8.36 (2.53-27.21) [QTc in the highest quartile (more than 498 ms)] | Risk between ages 12-40 was 13% over 28 years | 580 | 2003 | Italy | |
| Goldenberg et al[58] | HR 36.53 (13.35–99.95) (LQTS with prolonged QTc interval vs unaffected family members) | < 0.001 | 3386 | 2012 | USA, Europe, Japan and Israel | |
| Goldenberg et al[58] | HR 10.25 (3.34–31.46) (LQTS with normal-range QTc interval vs unaffected family members) | < 0.001 | 3386 | 2012 | USA, Europe, Japan and Israel | |
| Previous history of cardiac events | ||||||
| Sauer et al[55] | HR 5.10 (2.50–10.39) (Interim time dependant syncope vs no interim syncope) | < 0.01 | Risk between ages of 18-40: LQTS1 4.9%; LQTS2 8.0%; LQTS3 4.9% | 812 | 2007 | USA |
| Moss et al[56] | HR 3.10 (1.30-7.20) (History of cardiac event) | < 0.01 | 1496 | 1991 | USA | |
| Genotype | ||||||
| LQTS 3 | ||||||
| Priori et al[57] | RR 2.76 (1.01-7.51) (Male sex) | Risk between ages 12-40 was 13% over 28 years | 580 | 2003 | Italy | |
| Priori et al[57] | RR of 1.80 (1.07-3.04) (mutation at the LQT3 locus) | Risk between ages 12-40 was 13% over 28 years | 580 | 2003 | Italy | |
| LQTS 2 | ||||||
| Priori et al[57] | RR 1.61 (1.16-2.25) (LQT2 locus) | Risk between ages 12-40 was 13% over 28 years | 580 | 2003 | Italy | |
| LQTS 1 | ||||||
| Goldenberg et al[58] | HR 9.88 (1.26–37.63) (LQTS 1 mutation and normal QTc) | 0.03 | 3386 | 2012 | USA, Europe, Japan and Israel | |
| Heart rate | ||||||
| Moss et al[56] | HR 1.02 (1.00-1.03) (Resting heart rate less than 60 beats/min) | 0.01 | 1496 | 1991 | USA | |
| Niemeijer et al[59] | Bazett: HR 2.23 (1.17-4.24) Fridericia: HR 6.67 (2.96-15.06) (Consistent Qtc interval prolongation) | 3484 | 2015 | Netherlands | ||
SCD: Sudden cardiac death; LQTS: Long QT syndrome; QTc: QT corrected interval; HR: Hazard ratio; OR: Odds ratio; LV: Left ventricular; EF: Ejection fraction.
Several risk factors for SCD were identified in order of decreasing magnitude including: LQTS with a prolonged QTc interval (HR 36.53), LQTS with a normal range QTc interval (HR 10.25), LQTS 1 (HR 9.88), length of QTc interval (RR 5.34-8.36), consistent QTc interval prolongation (HR 2.23-6.67), previous history of cardiac events (syncope or aborted SCA) (HR 3.10-5.10), LQTS 3 (RR 1.80-2.76), female gender (HR 2.68), LQTS 2 (RR 1.61) and bradycardia (HR 1.02)[55-59].
Risk of sudden cardiac death in patients with HCM
In HCM there were 5 studies involving a total of 25823 patients[60-64](Table 6). The risk of SCD in HCM was about 5% over 5 years[60].
Table 6.
Risk factors for sudden cardiac death in patients with hypertrophic cardiomyopathy
| Risk factor studied | Relative risk of SCD | P value | Absolute SCD risk in cohort | Study size | Year | Country |
| Age | ||||||
| O’Mahony et al[60] | HR 0.99 (0.98-1.00) (Age 42 ± 15) | 0.007 | 5% at 5 years | 3675 | 2014 | Europe |
| Syncope | ||||||
| Liu et al[61] | HR 2.31 (1.22-4.38) | 12146 | 2017 | USA, China | ||
| O’Mahony et al[60] | HR 2.33 (1.69-3.19) | < 0.001 | 5% at 5 years | 3675 | 2014 | Europe |
| Christiaans et al[62] | HR 2.68 (0.97–4.38) | 9357 | 2010 | Netherlands, UK | ||
| Family history of SCD | ||||||
| Christiaans et al[62] | HR 1.27 (1.16–1.38) | 9357 | 2010 | Netherlands, UK | ||
| O’Mahony et al[60] | HR 1.76 (1.32-2.24) | <0.001 | 5% at 5 years | 3675 | 2014 | Europe |
| Liu et al[61] | HR 2.34 (1.46- 3.75) | 12146 | 2017 | USA, China | ||
| Abnormal blood pressure response during exercise | ||||||
| Liu et al[61] | HR 1.38 (0.65-2.89) (BP dropping on excersice) | 12146 | 2017 | USA, China | ||
| Christiaans et al[62] | HR 1.30 (0.64–1.96) (BP dropping on excersice) | 9357 | 2010 | Netherlands, UK | ||
| Non sustained ventricular tachycardia | ||||||
| Liu et al[61] | HR 2.92 (1.97-4.33) | 12146 | 2017 | USA, China | ||
| Sugrue et al[63] | HR 3.36 (1.00-11.35) | 0.05 | 52 | 2017 | USA | |
| O’Mahony et al[60] | HR 2.53 (1.85-3.47) | < 0.001 | 5% at 5 years | 3675 | 2014 | Europe |
| Christiaans et al[62] | HR 2.89 (2.21–3.58) | 9357 | 2010 | Netherlands, UK | ||
| Left ventricular wall thickness/hypertrophy | ||||||
| Liu et al[61] | HR 3.17 (1.64-6.12) (Maximum LV wall thickness ≥ 30 mm) | 12146 | 2017 | USA, China | ||
| Maeda et al[64] | HR 1.21 (1.04–1.39) (Maximum left ventricular wall thickness per 1-mm increase) | 0.011 | 593 | 2016 | Japan | |
| O’Mahony et al[60] | HR 1.05 (1.03-1.07) (Maximal LV wall thickness in mm 21.5 ± 6) | < 0.001 | 5% at 5 years | 3675 | 2014 | Europe |
| Christiaans et al[62] | HR 3.10 (1.81–4.40) (LVH ≥ 20 mm) | 9357 | 2010 | Netherlands, UK | ||
| Left ventricular outflow tract obstruction | ||||||
| Liu et al[61] | HR 2.41 (1.55-3.73) | 12146 | 2017 | USA, China | ||
| O’Mahony et al[60] | HR 1.01 (1.00-1.01) [LVOT Gradient mmHG 18 (6-58)] | 0.005 | 5% at 5 years | 3675 | 2014 | Europe |
| Left atrial diameter | ||||||
| O’Mahony et al[60] | HR 1.04 (1.02-1.05) (LA diameter in mm 46.2 ± 9) | < 0.001 | 5% at 5 years | 3675 | 2014 | Europe |
SCD: Sudden cardiac death; LVOT: Left ventricular outflow tract; HR: Hazard ratio; OR: Odds ratio; LV: Left ventricular; EF: Ejection fraction.
The following risk factors for SCD in order of decreasing magnitude were identified including: LVH (highest risk when greater than 20 mm) (HR 1.05-3.17), NSVT (HR 2.53-2.92), syncope (HR 2.31-2.68), left ventricular outflow tract obstruction (HR 1.01-2.41), family history of SCD (HR 1.27-2.34), abnormal blood pressure response during exercise (HR 1.30-1.38) and an enlarged left atrial diameter (HR 1.04)[60-64].
Wearable cardioverter defibrillator studies
There are currently only a few published outcome studies of WCDs. The WCD use in patients perceived to be at high risk, early post-MI study showed that 1.6% of patients received an appropriate shock for VT/VF and up to 67% of patients with VT/VF survived because of an appropriate shock[65]. Inappropriate shocks occurred in 1.1% of patients; none of the inappropriate shocks induced an arrhythmia.
“The aggregate national experience with the WCD vest: event rates, compliance and survival study” showed that 1.7% of patients received an appropriate shock for VT/VF. It also showed that 90% of patients survived because of an appropriate shock for VT/VF[66]. Inappropriate shocks occurred in 1.9% of patients[66].
The Vest Prevention of Early Sudden Death Trial compared WCD therapy to optimal medical therapy that was the control group. This trial showed that 0.6% of patients received an inappropriate shock. 1.4% of patients received an appropriate shock. The number of hours per day, the WCD was worn was 14.1 h. The risk of SCD was 1.6% in the WCD group compared to 2.4% in the control group (P = 0.18). All-cause mortality in the WCD group was 3.1% compared to 4.9% in the control group (P = 0.04)[67](Table 7).
Table 7.
Summary of wearable cardioverter defibrillator studies
| Study | General findings | Survival post shock |
| Wearable cardioverter-defibrillator use in patients perceived to be at high risk early post-myocardial infarction[65] | 99 out of 8453 patients received 114 inappropriate shocks. None of the inappropriate shocks induced arrhythmias. The inappropriate shock rate was 0.006 shocks per patient month of use. | 67% for those with VT/VF; 62% for those treated for PMVT/VF |
| Aggregate national experience with the wearable cardioverter defibrillator vest: event rates, compliance and survival[66] | Inappropriate shocks occurred in 67/3569 (1.9%) patients | 90% for VT/VF events; 73.6% for all events |
| Vest Prevention of Early Sudden Death Trial[67] | Inappropriate shocks: 0.6%; Appropriate shocks: 1.4%; Hours/day WCD worn: 14.1 | Risk of SCD (WCD vs Control): 1.6% vs 2.4%, P = 0.18. All-cause mortality (WCD vs Control): 3.1% vs 4.9%, P = 0.04 |
VT: Ventricular tachycardia; VF: Ventricular fibrillation; WCD: Wearable cardioverter defibrillator; SCD: Sudden cardiac death.
DISCUSSION
The risk of SCD in various groups of patients has been well studied. This has led to the development of clear criteria for ICD implantation[23]. There is data on various subgroups of patients that quantifies the magnitude of known risk factors for SCD (post MI, LQTS, HCM and LVSD). There are clear guidelines on the use of ICD in these groups of patients but a lack of clear guidelines for WCD therapy. This study has identified risk factors for several groups of patients who may not qualify for an ICD (due to the risk associated with implantation) but could benefit from WCD. These risk factors may help select patient for WCD therapy.
In patients who have recently had an MI with severe LVSD, guidelines recommend primary prevention with an ICD should be delayed for 40 d as the degree of myocardial recovery is uncertain in the acute period. This leaves certain patients without the best possible treatment if they were to have a further episode of VT/VF or patients who develop VT/VF later as a result of left ventricular dysfunction resulting from an MI. Patients post-MI are at increased risk of SCD. Several factors are associated with this increased risk of SCD. These risk factors could be used to select patient who may benefit from WCD post MI and if there risk remains high, they could be offered an ICD at 40 d. In addition, the DINAMIT study looked at early ICD implantation within 6-40 d vs optimal medical therapy. The DINAMIT study showed a reduction in arrhythmic death with early ICD implantation but no effect on overall mortality[68]. These results do raise the question of whether there are device related deaths that may reduce the overall mortality benefit such as device infections, procedural complications etc. These risks would not be present with WCD as there are no procedural risks associated with these devices. Some studies have advocated differentiating ICD implantation in the setting of acute MI based on whether the VT/VF occurred within 48 h in which case it could be attributed to acute MI and the treatment was revascularisation or if it occurred after 48 h in the absence of recurrent ischemia then these patients needed ICD implantation on the basis of secondary prevention and the 40 d rule in guidelines shouldn’t apply[69]. These patients could also potentially be covered by using a WCD until the 40 d window has elapsed. In addition, the highest risk of SCD is within the first 30 d of an MI and so high-risk patients who have not yet suffered VT/VF may benefit from a WCD during this period[30]. The risk factors identified in this study could be used to help select such patients.
In patients with LVSD, guidelines only recommend an ICD if EF is less than 35 percent. This is the group of patients who are at the highest risk of SCD from LVSD. Studies of heart failure patients with an EF between 30% and 35% have shown that these patients also benefit from ICD therapy and have a lower mortality than the same group of patients without an ICD[70]. This would also lead one to believe that patients at higher EF with more high risk features may also benefit from having a defibrillator such patients could be offered a WCD as a lower risk option than ICD implantation. Similarly patients post-MI who develop severe LVSD are not offered a ICD and are sent home for a clinic review in 40 d to assess the degree of myocardial recovery during this period. This is potentially dangerous as the absolute risk of SCD during this period is about 4.9% which is similar to the risk of SCD in patients with HCM at which an ICD would be implanted these patients should probably all be offered a WCD during this time period[24,60]. It is important to note, however, the results of the recent VEST trial looking at the risk of SCD in WCD patient vs controls in the first 90 d post MI. It did not show a statistically significant reduction in SCD (1.6% vs 2.4%, P = 0.18) but there was a trend to lower risk of SCD in the WCD group. It did show a reduction in overall mortality (3.1% vs 4.9%, P = 0.04). These results are the opposite of the DINAMIT study this may be due to poor patient compliance with compliance decreasing with time during the study, which may have contributed to the lack of a significant reduction in SCD. It is important to note that at the time of SCD only 8 of 25 patients in the treatment group were wearing their WCD[67]. Another group of patient who may benefit from a WCD are those who are awaiting heart transplantation. These patients should be offered an ICD based on current guidelines pre-transplantation; however, a WCD could be used as an alternative in these patients while they await their heart transplant.
In patients with non-ischaemic cardiomyopathy, the risk for SCD appears to be lower than those with ischaemic cardiomyopathy. They also do not appear to benefit from ICD therapy in the same way as patients with ischaemic cardiomyopathy as was shown by the recent defibrillator implantation in patients with nonischemic systolic heart failure (DANISH) study. The DANISH study showed no significant reduction in all-cause mortality between the ICD therapy and standard care group (21.6% vs 23.4%, P = 0.28). It did show a reduction in sudden cardiac death in the ICD group when compared to the standard care group ((4.3% vs 8.2%, P = 0.005)[16]. This reinforces the need for a risk stratification tool to help determine individual risk factors that would make patients at higher risk for SCD. This study does help provide data that could be used to select not only patients for WCD but also patients who might benefit from an ICD in this patient group.
In patients with LQTS guidelines only recommend an ICD in these patients if they have survived an episode of VT/VF. This may be an unacceptable risk for some patients and a WCD could afford these patients with some protection until they meet criteria for a permanent ICD. One large study used 4 variables which included age, length of QTc, symptoms and the presence of cardiac arrest to determine the decision on whether patients were likely to benefit from therapy with an ICD in LQTS[71]. Such a risk score could also be used to offer patients a choice between an ICD or a WCD.
Patients with HCM who have 5 year risk of death of less than 6% could be offered a WCD if they find the risk of SCD unacceptable. The ESC HCM risk-SCD calculator has a cut off of > 6% at which an ICD should be implanted. There may be patients who do not want an ICD and these patients could also be offered a WCD as an alternative.
A large WCD registry showed that WCD usage in patients with HCM and LQTS was safe, effective and associated with a high rate of compliance[72]. A further large meta-analysis of WCD showed that WCD have a 95% success rate at terminating arrhythmias[73].The HCM risk-SCD calculator provides a very helpful measure of assessing a patient’s risk of SCD and making treatment decisions in patients with HCM. It would be useful to develop risk calculators for SCD in other conditions, which are more common and have a much larger impact on global mortality. This would provide patients and doctors with more information to make the best decision regarding their care.
The following groups of patients could also benefit from WCD therapy; patients who have an explanted ICD for infective endocarditis and must wait a certain time period before reinsertion, patients who have a risk of SCD but have a lower absolute risk such that the cost and risk of ICD insertion can’t be justified, patients in remote areas where there is no expertise for ICD insertion, patients with myocarditis, patients with takotsubo cardiomyopathy, patients with peripartum cardiomyopathy, patients with advanced stage chronic kidney disease and children and young adults with channelopathies. The risk factors compiled in this review article could be used to help risk stratify many of these patients. The risk factors for patients post MI could be extrapolated to patients with takotsubo cardiomyopathy and myocarditis as all these processes involve an acute myocardial injury and so could be expected to have similar risk factors for SCD. In addition, the risk factors for LVSD could be extrapolated to patients with peripartum cardiomyopathy and those awaiting heart transplantation to determine high risk patients who may benefit from a WCD. There is potentially large scope for the use of WCD in carefully selected patient populations. One of the key disadvantages to WCD is the dependence on patient compliance for successful therapy as patients may decide to not wear the WCD, which can be a key limiting factor in its success.
In conclusion, we have identified multiple risk factors for sudden cardiac death in various conditions that could be used to help select patients for WCD therapy. The WCD is a landmark development that provides patients and physicians an additional therapy for the treatment of SCD; however, it is underutilized due to a lack of clear guidelines governing its usage[74]. SCD remains a common cause of death and continued effort must be made to try and develop more targeted approaches to treatment for SCD.
ARTICLE HIGHLIGHTS
Research background
There are many groups of patients including those post myocardial infarction (MI), patients with hypertrophic cardiomyopathy (HCM), patients with left ventricular systolic dysfunction (LVSD) and patients with long QT syndrome (LQTS) who are at high risk of sudden cardiac death (SCD) that do not meet criteria for implantable cardioverter defibrillator (ICD) implantation. This study looked at risk factors for SCD in these patient groups, which could be used as a method for identifying patients at high risk for SCD. Patients at high risk for SCD but not meeting conventional indications for ICD therapy could be offered a WCD until an ICD was indicated.
Research motivation
There is a need for more refined risk calculators to determine the risk of SCD in various conditions as is already present for patients with HCM. There is a requisite for more refined risk calculators to determine the risk of SCD in various conditions such as patients post MI, patients with LVSD, patients with LQTS and other channelopathies, patients with post-partum cardiomyopathy, patients with takotsubo cardiomyopathy, patients with myocarditis and patients with advanced chronic renal failure. This would allow better selection of patients at high risk of SCD and allow physicians to offer their patients the best treatment for each specific patient based on their individual risk.
Research objectives
The main objectives of our study were to collate the risk factors for SCD in specific patient groups as mentioned previously. These risk factors were to be used as a guide to help in determining high-risk patients that may benefit from WCD therapy. This to the best of our knowledge is the first attempt made at collating risk factors for SCD for various conditions in one place. This should help future studies to build on this data and hopefully give rise to risk calculators for SCD in these and many more conditions.
Research methods
We performed a literature search on PubMed. The studies were then selected according to whether they met the inclusion criteria for our review article. The inclusion criteria were any study that reported risk factors for SCD in patients with LVSD, LQTS, HCM or post MI. There was no restriction on age, gender, geographical area or date of publication. Studies had to be reported in English. Any studies where the risk of SCD was not quantified by either a hazard ratio, odds ratio or relative risk were excluded. The relevant risk factors for SCD in the 4 main conditions were then collected and tabulated in table format.
Research results
We collected a large number of risk factors for SCD in all 4 patients groups. These risk factors provide a robust method of assessing a patients risk for SCD. The study also looked at several WCD studies which showed that WCD were effective at terminating VT/VF but were limited in their effectiveness by patient compliance.
Research conclusions
This review shows that there are many risk factors for SCD that to the best of our knowledge have never been compiled together in one place such as this study has done. We also show that WCD are effective therapies for ventricular tachycardia/ventricular fibrillation, but are limited by patient compliance.
This should help in the development of more precise risk calculators for sudden cardiac death such as the existing risk calculator for HCM. This should also help select patients who may benefit from WCD.
Research perspectives
This study demonstrates the wealth of data present that could be used to create precise risk calculators for SCD. These risk calculators could be used to determine patients at high risk for SCD. It could be used to select which patients need an ICD and which could benefit from a WCD. Further study should be in the form of a meta-analysis to allow this area of research to move forward.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Endocrinology and metabolism
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
Conflict-of-interest statement: The authors have no conflicts of interest to declare in relation to this manuscript.
Peer-review started: January 8, 2019
First decision: January 21, 2019
Article in press: March 16, 2019
P-Reviewer: Barik R, Petix NR, Ueda H S-Editor: Wang JL L-Editor: A E-Editor: Zhang YL
Contributor Information
Hilal Mohammed Khan, Cardiac Unit, Raigmore Hospital, Inverness IV2 3UJ, United Kingdom.
Stephen J Leslie, Cardiac Unit, Raigmore Hospital, Inverness IV2 3UJ, United Kingdom; Department of Diabetes and Cardiovascular Science, University of the Highlands and Islands, The Centre for Health Science, Old Perth Road, Inverness IV2 3JH, United Kingdom. stephen.leslie@nhs.net.
References
- 1.Myerburg RJ, Castellanos A. Philadelphia: Saunders Elsevier; 2009. Sudden cardiac death, Cardiac electrophysiology: From cell to bedside; p. 797–808. [Google Scholar]
- 2.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, Berg RA National Registry of Cardiopulmonary Resuscitation Investigators. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 3.Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38:101–108. doi: 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 4.Bayés de Luna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death: mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J. 1989;117:151–159. doi: 10.1016/0002-8703(89)90670-4. [DOI] [PubMed] [Google Scholar]
- 5.Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death. Structure, function, and time-dependence of risk. Circulation. 1992;85:I2–10. [PubMed] [Google Scholar]
- 6.Chadda K, Goldstein S, Byington R, Curb JD. Effect of propranolol after acute myocardial infarction in patients with congestive heart failure. Circulation. 1986;73:503–510. doi: 10.1161/01.CIR.73.3.503. [DOI] [PubMed] [Google Scholar]
- 7.Hulleman M, Berdowski J, de Groot JR, van Dessel PF, Borleffs CJ, Blom MT, Bardai A, de Cock CC, Tan HL, Tijssen JG, Koster RW. Implantable cardioverter-defibrillators have reduced the incidence of resuscitation for out-of-hospital cardiac arrest caused by lethal arrhythmias. Circulation. 2012;126:815–821. doi: 10.1161/CIRCULATIONAHA.111.089425. [DOI] [PubMed] [Google Scholar]
- 8.van Alem AP, Chapman FW, Lank P, Hart AA, Koster RW. A prospective, randomised and blinded comparison of first shock success of monophasic and biphasic waveforms in out-of-hospital cardiac arrest. Resuscitation. 2003;58:17–24. doi: 10.1016/S0300-9572(03)00106-0. [DOI] [PubMed] [Google Scholar]
- 9.Zoll PM, Linenthal AJ, Gibson W, Paul MH, Norman LR. Termination of ventricular fibrillation in man by externally applied electric countershock. N Engl J Med. 1956;254:727–732. doi: 10.1056/NEJM195604192541601. [DOI] [PubMed] [Google Scholar]
- 10.Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, Pellis T, Sandroni C, Skrifvars MB, Smith GB, Sunde K, Deakin CD Adult advanced life support section Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 11.Mirowski M, Reid PR, Mower MM, Watkins L, Gott VL, Schauble JF, Langer A, Heilman MS, Kolenik SA, Fischell RE, Weisfeldt ML. Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings. N Engl J Med. 1980;303:322–324. doi: 10.1056/NEJM198008073030607. [DOI] [PubMed] [Google Scholar]
- 12.Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, Brown MW, Heo M. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 13.Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341:1882–1890. doi: 10.1056/NEJM199912163412503. [DOI] [PubMed] [Google Scholar]
- 14.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 15.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 16.Køber L, Thune JJ, Nielsen JC, Haarbo J, Videbæk L, Korup E, Jensen G, Hildebrandt P, Steffensen FH, Bruun NE, Eiskjær H, Brandes A, Thøgersen AM, Gustafsson F, Egstrup K, Videbæk R, Hassager C, Svendsen JH, Høfsten DE, Torp-Pedersen C, Pehrson S DANISH Investigators. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. N Engl J Med. 2016;375:1221–1230. doi: 10.1056/NEJMoa1608029. [DOI] [PubMed] [Google Scholar]
- 17.Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med. 1997;337:1576–1583. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 18.Connolly SJ, Gent M, Roberts RS, Dorian P, Roy D, Sheldon RS, Mitchell LB, Green MS, Klein GJ, O'Brien B. Canadian implantable defibrillator study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000;101:1297–1302. doi: 10.1161/01.CIR.101.11.1297. [DOI] [PubMed] [Google Scholar]
- 19.Kuck KH, Cappato R, Siebels J, Rüppel R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg (CASH) Circulation. 2000;102:748–754. doi: 10.1161/01.CIR.102.7.748. [DOI] [PubMed] [Google Scholar]
- 20.Kusumoto FM, Calkins H, Boehmer J, Buxton AE, Chung MK, Gold MR, Hohnloser SH, Indik J, Lee R, Mehra MR, Menon V, Page RL, Shen WK, Slotwiner DJ, Stevenson LW, Varosy PD, Welikovitch L. HRS/ACC/AHA expert consensus statement on the use of implantable cardioverter-defibrillator therapy in patients who are not included or not well represented in clinical trials. Circulation. 2014;130:94–125. doi: 10.1161/CIR.0000000000000056. [DOI] [PubMed] [Google Scholar]
- 21.Food and Drug Administration. FDA Approves First Wearable Defibrillator. Available from: http://permanent.access.gpo.gov/lps1609/www.fda.gov/fdac/departs/2002/202_upd.html#defib.
- 22.Francis J, Reek S. Wearable cardioverter defibrillator: a life vest till the life boat (ICD) arrives. Indian Heart J. 2014;66:68–72. doi: 10.1016/j.ihj.2013.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, Kirchhof P, Kjeldsen K, Kuck KH, Hernandez-Madrid A, Nikolaou N, Norekvål TM, Spaulding C, Van Veldhuisen DJ ESC Scientific Document Group. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC) Eur Heart J. 2015;36:2793–2867. doi: 10.1093/eurheartj/ehv316. [DOI] [PubMed] [Google Scholar]
- 24.Rao HB, Sastry BK, Korabathina R, Raju KP. Sudden cardiac death after acute ST elevation myocardial infarction: insight from a developing country. Heart Asia. 2012;4:83–89. doi: 10.1136/heartasia-2012-010114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mehta SR, Eikelboom JW, Natarajan MK, Diaz R, Yi C, Gibbons RJ, Yusuf S. Impact of right ventricular involvement on mortality and morbidity in patients with inferior myocardial infarction. J Am Coll Cardiol. 2001;37:37–43. doi: 10.1016/S0735-1097(00)01089-5. [DOI] [PubMed] [Google Scholar]
- 26.Abildstrom SZ, Rask-Madsen C, Ottesen MM, Andersen PK, Rosthøj S, Torp-Pedersen C, Køber L TRACE Study Group. Trandolapril cardiac evaluation. Impact of age and sex on sudden cardiovascular death following myocardial infarction. Heart. 2002;88:573–578. doi: 10.1136/heart.88.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenland P, Reicher-Reiss H, Goldbourt U, Behar S. In-hospital and 1-year mortality in 1,524 women after myocardial infarction. Comparison with 4,315 men. Circulation. 1991;83:484–491. doi: 10.1161/01.CIR.83.2.484. [DOI] [PubMed] [Google Scholar]
- 28.Ghaffari S, Pourafkari L, Tajlil A, Bahmani-Oskoui R, Nader ND. Is female gender associated with worse outcome after ST elevation myocardial infarction? Indian Heart J. 2017;69 Suppl 1:S28–S33. doi: 10.1016/j.ihj.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacIntyre K, Stewart S, Capewell S, Chalmers JW, Pell JP, Boyd J, Finlayson A, Redpath A, Gilmour H, McMurray JJ. Gender and survival: a population-based study of 201,114 men and women following a first acute myocardial infarction. J Am Coll Cardiol. 2001;38:729–735. doi: 10.1016/S0735-1097(01)01465-6. [DOI] [PubMed] [Google Scholar]
- 30.Solomon SD, Zelenkofske S, McMurray JJ, Finn PV, Velazquez E, Ertl G, Harsanyi A, Rouleau JL, Maggioni A, Kober L, White H, Van de Werf F, Pieper K, Califf RM, Pfeffer MA Valsartan in Acute Myocardial Infarction Trial (VALIANT) Investigators. Sudden death in patients with myocardial infarction and left ventricular dysfunction, heart failure, or both. N Engl J Med. 2005;352:2581–2588. doi: 10.1056/NEJMoa043938. [DOI] [PubMed] [Google Scholar]
- 31.Klem I, Weinsaft JW, Bahnson TD, Hegland D, Kim HW, Hayes B, Parker MA, Judd RM, Kim RJ. Assessment of myocardial scarring improves risk stratification in patients evaluated for cardiac defibrillator implantation. J Am Coll Cardiol. 2012;60:408–420. doi: 10.1016/j.jacc.2012.02.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yeung CY, Lam KS, Li SW, Lam KF, Tse HF, Siu CW. Sudden cardiac death after myocardial infarction in type 2 diabetic patients with no residual myocardial ischemia. Diabetes Care. 2012;35:2564–2569. doi: 10.2337/dc12-0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chitnis N, Vooturi S, Hygriv Rao B. Sudden cardiac death early after ST elevation myocardial infarction with and without severe left ventricular dysfunction. Indian Heart J. 2014;66:569–573. doi: 10.1016/j.ihj.2014.10.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adabag AS, Therneau TM, Gersh BJ, Weston SA, Roger VL. Sudden death after myocardial infarction. JAMA. 2008;300:2022–2029. doi: 10.1001/jama.2008.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Junttila MJ, Barthel P, Myerburg RJ, Mäkikallio TH, Bauer A, Ulm K, Kiviniemi A, Tulppo M, Perkiömäki JS, Schmidt G, Huikuri HV. Sudden cardiac death after myocardial infarction in patients with type 2 diabetes. Heart Rhythm. 2010;7:1396–1403. doi: 10.1016/j.hrthm.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 36.Maggioni AP, Zuanetti G, Franzosi MG, Rovelli F, Santoro E, Staszewsky L, Tavazzi L, Tognoni G. Prevalence and prognostic significance of ventricular arrhythmias after acute myocardial infarction in the fibrinolytic era. GISSI-2 results. Circulation. 1993;87:312–322. doi: 10.1161/01.CIR.87.2.312. [DOI] [PubMed] [Google Scholar]
- 37.Mäkikallio TH, Barthel P, Schneider R, Bauer A, Tapanainen JM, Tulppo MP, Schmidt G, Huikuri HV. Prediction of sudden cardiac death after acute myocardial infarction: role of Holter monitoring in the modern treatment era. Eur Heart J. 2005;26:762–769. doi: 10.1093/eurheartj/ehi188. [DOI] [PubMed] [Google Scholar]
- 38.Zimetbaum PJ, Buxton AE, Batsford W, Fisher JD, Hafley GE, Lee KL, O'Toole MF, Page RL, Reynolds M, Josephson ME. Electrocardiographic predictors of arrhythmic death and total mortality in the multicenter unsustained tachycardia trial. Circulation. 2004;110:766–769. doi: 10.1161/01.CIR.0000139311.32278.32. [DOI] [PubMed] [Google Scholar]
- 39.Siscovick DS, Raghunathan TE, Rautaharju P, Psaty BM, Cobb LA, Wagner EH. Clinically silent electrocardiographic abnormalities and risk of primary cardiac arrest among hypertensive patients. Circulation. 1996;94:1329–1333. doi: 10.1161/01.CIR.94.6.1329. [DOI] [PubMed] [Google Scholar]
- 40.Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV. Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA. 2003;290:2581–2587. doi: 10.1001/jama.290.19.2581. [DOI] [PubMed] [Google Scholar]
- 41.Cowie MR, Wood DA, Coats AJ, Thompson SG, Suresh V, Poole-Wilson PA, Sutton GC. Survival of patients with a new diagnosis of heart failure: a population based study. Heart. 2000;83:505–510. doi: 10.1136/heart.83.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taylor CJ, Roalfe AK, Iles R, Hobbs FD. Ten-year prognosis of heart failure in the community: follow-up data from the Echocardiographic Heart of England Screening (ECHOES) study. Eur J Heart Fail. 2012;14:176–184. doi: 10.1093/eurjhf/hfr170. [DOI] [PubMed] [Google Scholar]
- 43.Vaartjes I, Hoes AW, Reitsma JB, de Bruin A, Grobbee DE, Mosterd A, Bots MI. Age- and gender-specific risk of death after first hospitalization for heart failure. BMC Public Health. 2010;10:637. doi: 10.1186/1471-2458-10-637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yoshihisa A, Takiguchi M, Shimizu T, Nakamura Y, Yamauchi H, Iwaya S, Owada T, Miyata M, Abe S, Sato T, Suzuki S, Oikawa M, Kobayashi A, Yamaki T, Sugimoto K, Kunii H, Nakazato K, Suzuki H, Saitoh S, Takeishi Y. Cardiovascular function and prognosis of patients with heart failure coexistent with chronic obstructive pulmonary disease. J Cardiol. 2014;64:256–264. doi: 10.1016/j.jjcc.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 45.Fisher KA, Stefan MS, Darling C, Lessard D, Goldberg RJ. Impact of COPD on the mortality and treatment of patients hospitalized with acute decompensated heart failure: the Worcester Heart Failure Study. Chest. 2015;147:637–645. doi: 10.1378/chest.14-0607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ahmed A, Perry GJ. Incident atrial fibrillation and mortality in older adults with heart failure. Eur J Heart Fail. 2005;7:1118–1121. doi: 10.1016/j.ejheart.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 47.Corell P, Gustafsson F, Schou M, Markenvard J, Nielsen T, Hildebrandt P. Prevalence and prognostic significance of atrial fibrillation in outpatients with heart failure due to left ventricular systolic dysfunction. Eur J Heart Fail. 2007;9:258–265. doi: 10.1016/j.ejheart.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 48.Middlekauff HR, Stevenson WG, Stevenson LW. Prognostic significance of atrial fibrillation in advanced heart failure. A study of 390 patients. Circulation. 1991;84:40–48. doi: 10.1161/01.CIR.84.1.40. [DOI] [PubMed] [Google Scholar]
- 49.Doval HC, Nul DR, Grancelli HO, Varini SD, Soifer S, Corrado G, Dubner S, Scapin O, Perrone SV. Nonsustained ventricular tachycardia in severe heart failure. Independent marker of increased mortality due to sudden death. GESICA-GEMA Investigators. Circulation. 1996;94:3198–3203. doi: 10.1161/01.CIR.94.12.3198. [DOI] [PubMed] [Google Scholar]
- 50.Teerlink JR, Jalaluddin M, Anderson S, Kukin ML, Eichhorn EJ, Francis G, Packer M, Massie BM. Ambulatory ventricular arrhythmias in patients with heart failure do not specifically predict an increased risk of sudden death. PROMISE (Prospective Randomized Milrinone Survival Evaluation) Investigators. Circulation. 2000;101:40–46. doi: 10.1161/01.CIR.101.1.40. [DOI] [PubMed] [Google Scholar]
- 51.Szabó BM, van Veldhuisen DJ, Crijns HJ, Wiesfeld AC, Hillege HL, Lie KI. Value of ambulatory electrocardiographic monitoring to identify increased risk of sudden death in patients with left ventricular dysfunction and heart failure. Eur Heart J. 1994;15:928–933. doi: 10.1093/oxfordjournals.eurheartj.a060612. [DOI] [PubMed] [Google Scholar]
- 52.Shadman R, Poole JE, Dardas TF, Mozaffarian D, Cleland JG, Swedberg K, Maggioni AP, Anand IS, Carson PE, Miller AB, Levy WC. A novel method to predict the proportional risk of sudden cardiac death in heart failure: Derivation of the Seattle Proportional Risk Model. Heart Rhythm. 2015;12:2069–2077. doi: 10.1016/j.hrthm.2015.06.039. [DOI] [PubMed] [Google Scholar]
- 53.Quiñones MA, Greenberg BH, Kopelen HA, Koilpillai C, Limacher MC, Shindler DM, Shelton BJ, Weiner DH. Echocardiographic predictors of clinical outcome in patients with left ventricular dysfunction enrolled in the SOLVD registry and trials: significance of left ventricular hypertrophy. Studies of Left Ventricular Dysfunction. J Am Coll Cardiol. 2000;35:1237–1244. doi: 10.1016/S0735-1097(00)00511-8. [DOI] [PubMed] [Google Scholar]
- 54.Grayburn PA, Appleton CP, DeMaria AN, Greenberg B, Lowes B, Oh J, Plehn JF, Rahko P, St John Sutton M, Eichhorn EJ BEST Trial Echocardiographic Substudy Investigators. Echocardiographic predictors of morbidity and mortality in patients with advanced heart failure: the Beta-blocker Evaluation of Survival Trial (BEST) J Am Coll Cardiol. 2005;45:1064–1071. doi: 10.1016/j.jacc.2004.12.069. [DOI] [PubMed] [Google Scholar]
- 55.Sauer AJ, Moss AJ, McNitt S, Peterson DR, Zareba W, Robinson JL, Qi M, Goldenberg I, Hobbs JB, Ackerman MJ, Benhorin J, Hall WJ, Kaufman ES, Locati EH, Napolitano C, Priori SG, Schwartz PJ, Towbin JA, Vincent GM, Zhang L. Long QT syndrome in adults. J Am Coll Cardiol. 2007;49:329–337. doi: 10.1016/j.jacc.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 56.Moss AJ, Schwartz PJ, Crampton RS, Tzivoni D, Locati EH, MacCluer J, Hall WJ, Weitkamp L, Vincent GM, Garson A., Jr The long QT syndrome. Prospective longitudinal study of 328 families. Circulation. 1991;84:1136–1144. doi: 10.1161/01.CIR.84.3.1136. [DOI] [PubMed] [Google Scholar]
- 57.Priori SG, Schwartz PJ, Napolitano C, Bloise R, Ronchetti E, Grillo M, Vicentini A, Spazzolini C, Nastoli J, Bottelli G, Folli R, Cappelletti D. Risk stratification in the long-QT syndrome. N Engl J Med. 2003;348:1866–1874. doi: 10.1056/NEJMoa022147. [DOI] [PubMed] [Google Scholar]
- 58.Goldenberg I, Horr S, Moss AJ, Lopes CM, Barsheshet A, McNitt S, Zareba W, Andrews ML, Robinson JL, Locati EH, Ackerman MJ, Benhorin J, Kaufman ES, Napolitano C, Platonov PG, Priori SG, Qi M, Schwartz PJ, Shimizu W, Towbin JA, Vincent GM, Wilde AA, Zhang L. Risk for life-threatening cardiac events in patients with genotype-confirmed long-QT syndrome and normal-range corrected QT intervals. J Am Coll Cardiol. 2011;57:51–59. doi: 10.1016/j.jacc.2010.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Niemeijer MN, van den Berg ME, Deckers JW, Franco OH, Hofman A, Kors JA, Stricker BH, Rijnbeek PR, Eijgelsheim M. Consistency of heart rate-QTc prolongation consistency and sudden cardiac death: The Rotterdam Study. Heart Rhythm. 2015;12:2078–2085. doi: 10.1016/j.hrthm.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 60.O'Mahony C, Jichi F, Pavlou M, Monserrat L, Anastasakis A, Rapezzi C, Biagini E, Gimeno JR, Limongelli G, McKenna WJ, Omar RZ, Elliott PM Hypertrophic Cardiomyopathy Outcomes Investigators. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD) Eur Heart J. 2014;35:2010–2020. doi: 10.1093/eurheartj/eht439. [DOI] [PubMed] [Google Scholar]
- 61.Liu Q, Li D, Berger AE, Johns RA, Gao L. Survival and prognostic factors in hypertrophic cardiomyopathy: a meta-analysis. Sci Rep. 2017;7:11957. doi: 10.1038/s41598-017-12289-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Christiaans I, van Engelen K, van Langen IM, Birnie E, Bonsel GJ, Elliott PM, Wilde AA. Risk stratification for sudden cardiac death in hypertrophic cardiomyopathy: systematic review of clinical risk markers. Europace. 2010;12:313–321. doi: 10.1093/europace/eup431. [DOI] [PubMed] [Google Scholar]
- 63.Sugrue A, Killu AM, DeSimone CV, Chahal AA, Vogt JC, Kremen V, Hai J, Hodge DO, Acker NG, Geske JB, Ackerman MJ, Ommen SR, Lin G, Noseworthy PA, Brady PA. Utility of T-wave amplitude as a non-invasive risk marker of sudden cardiac death in hypertrophic cardiomyopathy. Open Heart. 2017;4:e000561. doi: 10.1136/openhrt-2016-000561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maeda R, Minami Y, Haruki S, Kanbayashi K, Itani R, Suzuki A, Ejima K, Shiga T, Shoda M, Hagiwara N. Implantable cardioverter defibrillator therapy and sudden death risk stratification in hypertrophic cardiomyopathy patients with midventricular obstruction: A single-center experience. Int J Cardiol. 2016;214:419–422. doi: 10.1016/j.ijcard.2016.03.231. [DOI] [PubMed] [Google Scholar]
- 65.Epstein AE, Abraham WT, Bianco NR, Kern KB, Mirro M, Rao SV, Rhee EK, Solomon SD, Szymkiewicz SJ. Wearable cardioverter-defibrillator use in patients perceived to be at high risk early post-myocardial infarction. J Am Coll Cardiol. 2013;62:2000–2007. doi: 10.1016/j.jacc.2013.05.086. [DOI] [PubMed] [Google Scholar]
- 66.Chung MK, Szymkiewicz SJ, Shao M, Zishiri E, Niebauer MJ, Lindsay BD, Tchou PJ. Aggregate national experience with the wearable cardioverter-defibrillator: event rates, compliance, and survival. J Am Coll Cardiol. 2010;56:194–203. doi: 10.1016/j.jacc.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Olgin JE, Pletcher MJ, Vittinghoff E, Wranicz J, Malik R, Morin DP, Zweibel S, Buxton AE, Elayi CS, Chung EH, Rashba E, Borggrefe M, Hue TF, Maguire C, Lin F, Simon JA, Hulley S, Lee BK VEST Investigators. Wearable Cardioverter-Defibrillator after Myocardial Infarction. N Engl J Med. 2018;379:1205–1215. doi: 10.1056/NEJMoa1800781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hohnloser SH, Kuck KH, Dorian P, Roberts RS, Hampton JR, Hatala R, Fain E, Gent M, Connolly SJ DINAMIT Investigators. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med. 2004;351:2481–2488. doi: 10.1056/NEJMoa041489. [DOI] [PubMed] [Google Scholar]
- 69.Lim HS, Lip GY, Tse HF. Implantable cardioverter defibrillator following acute myocardial infarction: the '48-hour' and '40-day' rule. Europace. 2008;10:536–539. doi: 10.1093/europace/eun070. [DOI] [PubMed] [Google Scholar]
- 70.Al-Khatib SM, Hellkamp AS, Fonarow GC, Mark DB, Curtis LH, Hernandez AF, Anstrom KJ, Peterson ED, Sanders GD, Al-Khalidi HR, Hammill BG, Heidenreich PA, Hammill SC. Association between prophylactic implantable cardioverter-defibrillators and survival in patients with left ventricular ejection fraction between 30% and 35% JAMA. 2014;311:2209–2215. doi: 10.1001/jama.2014.5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schwartz PJ, Spazzolini C, Priori SG, Crotti L, Vicentini A, Landolina M, Gasparini M, Wilde AA, Knops RE, Denjoy I, Toivonen L, Mönnig G, Al-Fayyadh M, Jordaens L, Borggrefe M, Holmgren C, Brugada P, De Roy L, Hohnloser SH, Brink PA. Who are the long-QT syndrome patients who receive an implantable cardioverter-defibrillator and what happens to them?: data from the European Long-QT Syndrome Implantable Cardioverter-Defibrillator (LQTS ICD) Registry. Circulation. 2010;122:1272–1282. doi: 10.1161/CIRCULATIONAHA.110.950147. [DOI] [PubMed] [Google Scholar]
- 72.Kutyifa V, Moss AJ, Klein H, Biton Y, McNitt S, MacKecknie B, Zareba W, Goldenberg I. Use of the wearable cardioverter defibrillator in high-risk cardiac patients: data from the Prospective Registry of Patients Using the Wearable Cardioverter Defibrillator (WEARIT-II Registry) Circulation. 2015;132:1613–1619. doi: 10.1161/CIRCULATIONAHA.115.015677. [DOI] [PubMed] [Google Scholar]
- 73.Nguyen E. Wearable Cardioverter-defibrillators for the Prevention of Sudden Cardiac Death: A Meta-analysis. J Innov Card Rhythm Manag. 2018 doi: 10.19102/icrm.2018.090506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pillarisetti J, Emert M, Biria M, Chotia R, Guda R, Bommana S, Pimentel R, Vacek J, Dendi R, Berenbom L, Dawn B, Lakkireddy D. Under-Utilization of Implantable Cardioverter Defibrillators in Patients with Heart Failure - The Current State of Sudden Cardiac Death Prophylaxis. Indian Pacing Electrophysiol J. 2016;15:20–29. doi: 10.1016/S0972-6292(16)30838-5. [DOI] [PMC free article] [PubMed] [Google Scholar]