Abstract
Purpose
Numerous surgical techniques and fixation methods have been described in medial patellofemoral ligament (MPFL) reconstruction such as choice of graft, graft fixation method of patella/femur and initial tension. We describe short term clinical results of MPFL reconstruction by using soft suture anchor and adjustable cortical fixation system.
Methods
Twenty-four patients who underwent isolated MPFL reconstruction by using soft suture anchor and adjustable cortical fixation system were included in this study. All patients were followed up for at least 2 years, and pre-operative and 2 years post-operative Kujala score, IKDC score and Knee Injury and Osteoarthritis Outcome Score were used to assess clinical outcome. Radiographic evaluation included the Q angle, congruence angle and patellar tilt angle. Pre- and post-operative changes were evaluated by Mann–Whitney U test.
Results
There were no complications including re-dislocation, patella fracture, infection, and joint contracture. The apprehension test was positive in 4.2% post-operatively. A statistically significant improvement in clinical scores and radiographic evaluation were evident after surgery.
Conclusions
Isolated MPFL Reconstruction using soft suture anchor and adjustable cortical fixation system led good restoration of patellar stability and significant improvement of knee function in short-term results. This surgical technique can reduce complications such as patella fractures, and can be done safely.
Clinical relevance
This technique may be a treatment option with little associated complications in the treatment for patellar instability.
Level of Evidence
Case series, Level IV.
Keywords: Isolated Medial Patellofemoral Ligament Reconstruction, Patellar dislocation, Suture anchor
1. Introduction
The medial patellofemoral ligament (MPFL) is the main stabilizer of the lateral patellar translation and is a structure that is frequently damaged by lateral patellar dislocation.1, 2, 3 Numerous surgical techniques and fixation methods have been described in MPFL reconstruction4, 5, 6, 7 such as choice of graft, graft fixation method of patella/femur and initial tension. Since non-anatomical restoration of footprint or over-constraint due to over-tensioned graft will result not only in recurrence of patellar instability but also cartilage injury and osteoarthritis of the patellofemoral joint, anatomical MPFL reconstruction is important.8, 9, 10, 11 During the past few years, MPFL reconstruction using a soft tissue graft has become a focus of interest and has shown good clinical results. The MPFL is one of the main restrictor against dislocation of the patella. It contributes 50%–60% of medial constraint.12, 13, 14 Multiple techniques for fixation of the graft at the patella are clinically applied. Some studies are described by using suture anchors or interference screws for fixation of the graft at the patella, others are described by creating two bone tunnels or a bone bridge on the medial margin of the patella holding the graft.4, 5, 6, 7 There are advantages and disadvantages to all surgical techniques of the graft fixation. The bone tunnel across the patella is at risk of patellar fracture.15, 16, 17 Moreover, the bone tunnels are created in a non-anatomical position to avoid fracture. In the graft fixation on the femoral side, there are reports using cortical buttons, interference screws, and suspension devices.4,5,7,15,18,19
The purpose of the present study is to prove good restoration of patellar stability and significant improvement of knee function compared to other surgical procedures of previous study without causing patellar fracture by using soft suture anchor to fix into the patella. The hypothesis is that MPFL reconstruction by using soft suture anchor and adjustable cortical fixation system is good with short term results.
2. Materials and methods
From 2014 to 2016, 25 patients underwent MPFL reconstruction using gracilis tendon autograft to treat patellar dislocation. All surgeries were performed by the senior author. All patients underwent X-ray and CT or MRI preoperatively. Trochlear dysplasia, patellar height and tibial tubercle-trochlear groove (TT-TG) distance were measured as the factors of instability (Table 1). Trochlear dysplasia was evaluated using DeJour classification20 and patellar height was evaluated using Caton-Deschamps index.21
Table 1.
Patient characteristics.
| Number of patient | 24 |
| Age, mean | 25.4 ± 9.3 |
| Sex (male/female) | 6/18 |
| TT-TG distance | 15.8 ± 3.6 |
| Caton-Deschamps index | 1.1 ± 0.13 |
| Sulcus angle | 145.2 ± 2.9 |
| Trochlear dysplasia DeJour | |
| Type A | 4 |
| Type B | 2 |
| Type C | 0 |
| Type D | 0 |
The inclusion criteria were as follows: (1) growth plate was closed; (2) apprehension sign was positive; (3) first time traumatic patellar dislocation and recurrent dislocation; (4) lateral patellar instability with MPFL injury. The exclusion criteria were as follows: (1) history of previous knee surgery; (2) a tibial tuberosity-trochlear groove distance of >20 mm; (3) concomitant cruciate ligament or collateral ligament injury. Based on these criteria, 24 patients were included in this study.
This study was approved by the Ethics Committee of Toho University Ohashi medical Center (No.H17037).
3. Surgical technique
The patient is placed in a supine position under general anesthesia. We do not use the air tourniquet. The gracilis tendon is harvested through 3 cm incision over the pes anserinus and released with a tendon stripper. After trimming the graft, pre-tension is applied and the length is measured. This technique is possible if the graft length is 20 cm or more. Arthroscopy is performed next. Additional procedures perform loose body removal and synovectomy and microfracture of osteochondral lesions, as well as repair or meniscectomy for meniscal injury.
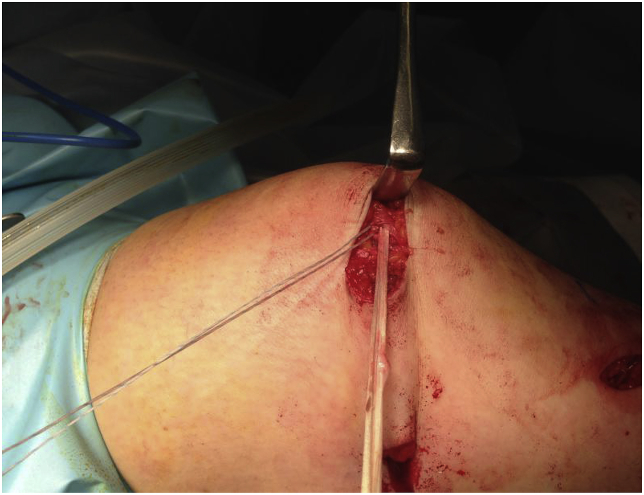
Then 3 cm longitudinal incision is made on the medial border of patella and the upper half to two-thirds of the medial patellar facet is exposed to surface of the joint capsule. A 1.7 mm suture anchor (SUTURFIX ULTRA®; Smith&Nephew, Andover, MA) is inserted horizontally from center of patella. One of the anchor sutures is sutured to about 1.5 cm of the stump side with the periosteum of the gracilis tendon using the modified baseball suture (Fig. 1). The graft is sutured drawing the stump into the anchor hole of the patellar (Fig. 2).
Fig. 1.

Demonstrates the modified baseball suture.
Fig. 2.
The gracilis tendon graft is sutured into bone tunnel of suture anchor.
A 2 cm incision is made on adductor tubercle of the medial femur. The femoral bone tunnels are prepared with reference to the femoral attachment according to the method reported by Nomura et al.22 2.4 mm passing pin is drilled throughout from the femoral attachment. The diameter of the two-fold gracilis tendon is measured beforehand. Using a drill of that diameter size, drill about 30 mm from the inside, then a socket-like bone tunnel is prepared by creating a through tunnel to the outside with end button drill of a 4.5 mm diameter. The adjustable cortical fixation system (TightRope®; Arthrex, Naples, FL) is flipped through the bone tunnel. The sutured gracilis tendon is guided to the second layer on the outer side of the joint capsule and the gracilis tendon is passed through the loop of the TightRope and again passed through the second layer to the patella side. If the gracilis tendon is too long, it is cut off at this stage and the other stump of the gracilis tendon is sewn through the medial retinaculum of the medial upper edge of the patella. This is because we thought that inserting another anchor at the upper edge of patella increased the risk of patellar fracture. Moreover, it is difficult to insert the anchor into the anatomical position when trying to insert the anchor in a place where it can be inserted. Tight rope is pulled up from outside with tension applied to the graft with an elevation at 30° knee flexion position. Because of the characteristics of TightRope, it cannot be loosened, so arthroscopic view of PF joint, extension and flexion of the knee, and lateral shift of the patella must be carefully observed. Since this technique cannot quantify tension on the graft, it is necessary to confirm that the patella does not dislocate by applying lateral stress to the patella at 30°, 60° and 90°, and to not excessively pull up TightRope by checking the tension of the graft. We do not include lateral retinacular release in our standard procedure (Fig. 3, Fig. 4).
Fig. 3.

Arthroscopic view of the right knee with post-MPFL reconstruction.
Fig. 4.

Schematic drawing of isolated Medial Patellofemoral Ligament Reconstruction by using Soft Suture Anchor and adjustable cortical fixation system.
4. Post-operative physiotherapy
A knee brace with 0° was used for first week, with full weight bearing on straight knee. From 1 week, range of motion of 0°–90° was started. After 8 weeks, range of motion of full range was allowed. Jogging after 4 months and contact sports after 6 months were allowed.
5. Clinical evaluation
All patients were followed up for at least 2 years, and clinical outcome assessments were performed using pre-operative and 2 years post-operative Kujala score, International Knee Documentation Committee (IKDC) score and Knee Injury and Osteoarthritis Outcome Score (KOOS). Radiographic evaluation included the Q angle (QA), congruence angle (CA) and patellar tilt angle (PTA) and patellar height. Q angle was defined as the angle created by two lines, both starting at the anterior center of the patella using lower limbs full-length X ray. One line extended to the anterior-superior iliac spine (ASIS) and the other extended to the tibial tuberosity. Congruence angle was defined as the angle between the bisect of the femoral trochlea and a line from the apex of the femoral trochlea through the apex of the patella. Patellar tilt angle was defined as follows: (1) Draw the first line parallel to the posterior femoral condyles. (2) Draw the second line parallel to the first at the patellar apex. (3) The angle between the lateral patellar facet and trochlea. Moreover, complications were analyzed about infection, re-dislocation, patella fracture and joint contracture.
6. Statistical analysis
All statistical analyses were performed using SPSS (version 24.0; IBM Corp., Armonk, NY, USA). Pre- and post-operative changes were evaluated by Mann–Whitney U test. A P value < 0.05 was considered statistically significant. A post hoc power analysis was performed to determine whether the sample size had sufficient power to detect significant differences. The power was between 0.81 and 0.95 for a sample with 24 cases in each evaluation. The α-level was 0.05.
7. Result
The mean age at the time of surgery was 25.4 years (±9.3 years). Mean follow-up was 33.6 months (±3.1 months). About the additional procedures during operation, loose body removal was performed five cases, microfracture of osteochondral lesions was performed four cases, meniscal repair was performed two cases. At 2 years post-operation, no complications including re-dislocation, patella fracture, infection, joint contracture had occurred. Apprehension test was negative in 23 (95.8%) cases. The apprehension test was positive in 1 of the 24 (4.2%) cases post-operation. A statistically significant improvement in clinical scores (Kujala score, IKDC score and KOOS) were evident after surgery. Radiographic evaluation (Q angle, congruence angle and patellar tilt angle) also showed clear improvement after surgery (Table 2).
Table 2.
Clinical outcome of pre- and post-operatively.
| Pre-operative | Post-operative | P value | |
|---|---|---|---|
| Kujala score | 50.9 ± 23.7 | 93.7 ± 4.2 | 0.001 |
| IKDC score | 43.2 ± 8.4 | 91.1 ± 2.9 | 0.001 |
| KOOS | |||
| Symptom | 66.0 ± 14.8 | 93.5 ± 6.8 | 0.001 |
| Pain | 75.7 ± 9.8 | 95.4 ± 2.9 | 0.001 |
| ADL | 80.8 ± 13.1 | 97.7 ± 3.1 | 0.001 |
| Sports | 59.0 ± 16.9 | 92.0 ± 4.6 | 0.001 |
| QOL | 47.9 ± 13.3 | 91.5 ± 5.2 | 0.001 |
| Q angle | 12.9 ± 2.4 | 10.5 ± 1.6 | 0.003 |
| Congruence angle | 15.9 ± 4.0 | −0.81 ± 6.4 | 0.001 |
| Patellar tilt angle | 10.4 ± 2.1 | 3.5 ± 0.78 | 0.001 |
∗ IKDC: International Knee Documentation Committee.
∗ KOOS: Knee Injury and Osteoarthritis Outcome Score.
8. Discussion
The most important findings of this study are that good restoration of patellar stability and significant improvement of knee function were achieved by this technique of MPFLR. Also, there are no complications that occurred including re-dislocation, patella fracture, infection, and joint contracture. Our hypothesis that MPFL reconstruction by using soft suture anchor and adjustable cortical fixation system is good with short term results. is confirmed.
Positive rate of apprehension test was 4.2% postoperatively. In a recent systematic review, recurrent instability rate was reported in 32.7% of patients who were treated with procedures including MPFL reconstruction, MPFL repair and lateral retinacular release.23 However, recurrent instability rate of isolated MPFL reconstruction was described between 1.1% and 12.5%.18,24, 25, 26, 27 This rate is significantly lower than a recent systematic review, and the rate of this study was within this range. Lateral retinacular release is often performed concomitantly with MPFL reconstruction, however, it can increase postoperative instability, particularly the risk of medial patellar subluxations.13,28,29 On the other hand, Niu et al. described that no statistically significant differences were noted between double-bundle anatomical MPFL reconstruction combined with lateral retinaculum plasty and isolated MPFL reconstruction alone.19 In the previous studies, there are also reports that medial patellar subluxations occur in 57–94% of cases after lateral retinacular release. Lateral patellofemoral ligament or lateral retincular lengthening has been increasingly considered for individuals with combined MPFL reconstruction; however, the criterion for utilizing a lengthening procedure is variable by provider. Therefore, we chose not to do lateral retinacular release in this study. The most important consideration is given to the location of femoral and patella tunnel. A non-anatomical surgical reconstruction can lead to aberrant restraining forces and patellofemoral contact pressures.30, 31, 32 In previous cadaveric study, there are many reports that say the femoral insertion of MPFL was between medial femoral epicondyle and adductor tubercle.33, 34, 35 The femoral tunnel was made with reference to these reports in this study. Regarding patella insertion, there are many reports of proximal half35, 36, 37 and proximal two thirds,22,33,38,39 and it is widely attached to the inside of the patella. Some studies are described using suture anchors or interference screws and creating two bone tunnels or a bone bridge for fixation of the graft at the patella.4, 5, 6, 7 Shah et al. have reported in two types of tunnel technique and suture technique tendon fixation of the patella side in Systematic Review.17 The complication rate was lower in suture technique (21.6%) than in tunnel technique (29.8%).17 The most serious complication is patella fracture, and it is reported that it often occurs when creating transverse patella tunnels or when using a thick drill such as 4.5 mm.4,17 It is considered that patella fracture did not occur in this study due to the fact that a 1.7 mm suture anchor was used and transverse patella tunnel was not created. Also, the suture anchor was inserted at the middle part of medial patella, and the upper part is sewn through the medial retinaculum without inserting suture anchor. Therefore, the attachment of graft can cover two thirds of proximal patella and an anatomical reconstruction is possible. The graft tension is determined on femoral side in this study. Stephen et al. described that Patellofemoral joint contact pressure and patella tracking restored when fixed at knee flexion 30° or 60° and tension of 2 N in anatomical MPFL reconstruction.40 Non-anatomical reconstruction and over-tensioning lead to increased contact pressure and osteoarthritis. In the technique used in this study, tightrope is pulled up at once at knee flexion 30 to determine tension. The characteristic of the tightrope is such that once pulled, it cannot be returned to the previous position, it is therefore most carefully pulled up. It also cannot quantify how tightly it is fixed with the graft tension. The technical aspect here is to apply lateral pressure as we proceed to confirm there are no dislocation or subluxation, at the same time ensuring that the graft is fixed with enough tension allowance without applying excessive tension to the Tightrope.
The main limitation of this study is that it was conducted on a small number of cases without a control group. A long term, comparative studies with large number of patients is required to corroborate our findings. Second, this method cannot quantify the fixed tension of the graft. However, recurrent dislocation of patella did not occur and the results were relatively good. The clinical relevance of the present study is that this technique may be a treatment option with little associated complications for the treatment for patellar instability.
9. Conclusion
Isolated Medial Patellofemoral Ligament Reconstruction by using Soft Suture Anchor and adjustable cortical fixation system led good restoration of patellar stability and significant improvement of knee function in short-term results. This surgical technique can reduce complications such as patella fractures, and can be done safely.
Conflicts of interest
The authors declare that they have no conflict of interest.
Footnotes
This study was approved by the Ethics Committee of Toho University Ohashi medical Center (No.H17037).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2019.03.016.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Amis A.A., Firer P., Mountney J., Senavongse W., Thomas N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. doi: 10.1016/s0968-0160(03)00006-1. https://www.ncbi.nlm.nih.gov/pubmed/12893142 [DOI] [PubMed] [Google Scholar]
- 2.Fithian D.C., Paxton E.W., Stone M.L. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 3.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christiansen S.E., Jacobsen B.W., Lund B., Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 5.Golant A., Quach T., Rosen J.E. Medial patellofemoral ligament reconstruction with a looped semitendinosus tendon, using knotless anchor fixation on patella and hybrid fixation on the femur. Arthrosc Tech. 2014;12(3):e211–216. doi: 10.1016/j.eats.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lenschow S., Schliemann B., Gestring J., Herbort M., Schulze M., Kösters C. Medial patellofemoral ligament reconstruction: fixation strength of 5 different techniques for graft fixation at the patella. Arthroscopy. 2013;29:766–773. doi: 10.1016/j.arthro.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Nakagawa S., Arai Y., Kan H. Medial patellofemoral ligament reconstruction procedure using a suspensory femoral fixation system. Arthrosc Tech. 2013;15(4):e491–495. doi: 10.1016/j.eats.2013.07.009. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bollier M., Fulkerson J., Cosgarea A., Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27(8):1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy M., Ridley T.J., Bollier M., Wolf B., Albright J., Amendola A. Femoral tunnel placement in medial patellofemoral ligament reconstruction. Iowa Orthop J. 2013;33:58–63. https://www.ncbi.nlm.nih.gov/pubmed/24027462 [PMC free article] [PubMed] [Google Scholar]
- 10.Schottle P., Schmeling A., Romero J., Weiler A. Anatomical reconstruction of the medial Patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009;129(3):305–309. doi: 10.1007/s00402-008-0712-9. [DOI] [PubMed] [Google Scholar]
- 11.Servien E., Fritsch B., Lustig S. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–139. doi: 10.1177/0363546510381362. [DOI] [PubMed] [Google Scholar]
- 12.Conlan T., Garth W.P., Jr., Lemons J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. https://www.ncbi.nlm.nih.gov/pubmed/?term=Evaluation+of+the+medial+soft-tissue+restraints+of+the+extensor+mechanism+of+the+knee [DOI] [PubMed] [Google Scholar]
- 13.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 14.Hautamaa P.V., Fithian D.C., Kaufman K.R., Daniel D.M., Pohlmeyer A.M. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. doi: 10.1097/00003086-199804000-00021. https://www.ncbi.nlm.nih.gov/pubmed/9584380 [DOI] [PubMed] [Google Scholar]
- 15.Mikashima Y., Kimura M., Kobayashi Y., Miyawaki M., Tomatsu T. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg. 2006;72(1):65–71. https://www.ncbi.nlm.nih.gov/pubmed/16570897 [PubMed] [Google Scholar]
- 16.Schiphouwer L., Rood A., Tigchelaar S., Koëter S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):245–250. doi: 10.1007/s00167-016-4245-4. [DOI] [PubMed] [Google Scholar]
- 17.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feller J.A., Richmond A.K., Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2470–2476. doi: 10.1007/s00167-014-3132-0. [DOI] [PubMed] [Google Scholar]
- 19.Niu Y., Wang X., Liu C. Double-bundle anatomical medial patellofemoral ligament reconstruction with lateral retinaculum plasty can lead to good outcomes in patients with patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2743–2749. doi: 10.1007/s00167-017-4720-6. [DOI] [PubMed] [Google Scholar]
- 20.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors off patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. https://www.ncbi.nlm.nih.gov/pubmed/?term=Factors+off+patellar+instability%3A+an+anatomic+radiographic+study [DOI] [PubMed] [Google Scholar]
- 21.Caton J., Deschamps G., Chambat P., Lerat J.L., Dejour H., infera Patella. A propos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. https://www.ncbi.nlm.nih.gov/pubmed/?term=Patella+infera.+Apropos+of+128+cases [PubMed] [Google Scholar]
- 22.Nomura E., Inoue M., Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):510–515. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 23.Erickson B.J., Mascarenhas R., Sayegh E.T. Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31(6):1207–1215. doi: 10.1016/j.arthro.2014.11.040. [DOI] [PubMed] [Google Scholar]
- 24.Csintalan R.P., Latt L.D., Fornalski S., Raiszadeh K., Inacio M.C., Fithian D.C. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27(2):139–146. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 25.Deie M., Ochi M., Adachi N., Shibuya H., Nakamae A. Medial patellofemoral ligament reconstruction fixed with a cylindrical bone plug and a grafted semitendinosus tendon at the original femoral site for recurrent patellar dislocation. Am J Sports Med. 2011;39(1):140–145. doi: 10.1177/0363546510377436. [DOI] [PubMed] [Google Scholar]
- 26.Fink C., Veselko M., Herbort M., Hoser C. MPFL reconstruction using a quadriceps tendon graft, part 2: operative technique and short term clinical results. Knee. 2014;21(6):1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Kang H.J., Cao J.H., Pan S., Wang X.J., Yu da H., Zheng Z.M. The horizontal Y-shaped graft with respective graft tension angles in anatomical two-bundle medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2445–2451. doi: 10.1007/s00167-014-3005-6. [DOI] [PubMed] [Google Scholar]
- 28.Christoforakis J., Bull A.M., Strachan R.K., Shymkiw R., Senavongse W., Amis A.A. Effects of lateral retinacular release on the lateral stability of the patella. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):273–277. doi: 10.1007/s00167-014-3005-6. [DOI] [PubMed] [Google Scholar]
- 29.McCarthy M.A., Bollier M.J. Medial patella subluxation: diagnosis and treatment. Iowa Orthop J. 2015;35:26–33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4492148/ [PMC free article] [PubMed] [Google Scholar]
- 30.Beck P., Brown N.A.T., Greis P.E., Burks R.T. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557–1563. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 31.DeVries Watson N., Duchman K.R., Bollier M.J., Grosland N.M. A finite element analysis of medial patellofemoral ligament reconstruction. Iowa Orthop J. 2015;35:13–19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4492131/ [PMC free article] [PubMed] [Google Scholar]
- 32.Elias J.J., Cosgarea A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 33.Baldwin J.L. The anatomy of the medial patellofemoral ligament. Am J Sports Med. 2009;37(12):2355–2361. doi: 10.1177/0363546509339909. [DOI] [PubMed] [Google Scholar]
- 34.Fujino K., Tajima G., Yan J. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):998–1003. doi: 10.1007/s00167-013-2797-0. [DOI] [PubMed] [Google Scholar]
- 35.Philippot R., Chouteau J., Wegrzyn J., Testa R., Fessy M.H., Moyen B. Medial patellofemoral ligament anatomy: implications for its surgical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):475–479. doi: 10.1007/s00167-009-0722-3. [DOI] [PubMed] [Google Scholar]
- 36.Jacobi M., Reischl N., Bergmann M., Bouaicha S., Djonov V., Magnussen R.A. Reconstruction of the medial Patellofemoral ligament using the adductor magnus tendon: an anatomic study. Arthroscopy. 2012;28(1):105–109. doi: 10.1016/j.arthro.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 37.Stephen J.M., Lumpaopong P., Deehan D.J., Kader D., Amis A.A. The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med. 2012;40(8):1871–1879. doi: 10.1177/0363546512449998. [DOI] [PubMed] [Google Scholar]
- 38.Andrikoula S., Tokis A., Vasiliadis H.S., Georgoulis A. The extensor mechanism of the knee joint: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):214–220. doi: 10.1007/s00167-005-0680-3. [DOI] [PubMed] [Google Scholar]
- 39.Tuxøe J.I., Teir M., Winge S., Nielsen P.L. The medial patellofemoral ligament: a dissection study. Knee Surg Sports Traumatol Arthrosc. 2002;10(3):138–140. doi: 10.1007/s00167-001-0261-z. [DOI] [PubMed] [Google Scholar]
- 40.Stephen J.M., Kaider D., Lumpaopong P., Deehan D.J., Amis A.A. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42(2):364–372. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.