Abstract
Background:
As health care reform continues within the United States, navigators may play increasingly diverse and vital roles across the health care continuum. The growing interest in patient navigation programs for underserved populations calls for detailed descriptions of intervention components to facilitate implementation and dissemination efforts.
Methods:
In Chicago’s Chinatown, Chinese immigrant women face language, cultural, and access barriers in obtaining breast and cervical cancer screening and follow-up. These barriers spurred the research partnership between Northwestern University, the Chinese American Service League, Mercy Hospital & Medical Center, and Rush University Medical Center to formalize the Chinatown Patient Navigation Collaborative for adapting and implementing previously developed patient navigation models.
Results:
In this report, we describe the adaptation of patient navigation to build the Chinatown Patient Navigation Collaborative’s community-based patient navigation program for breast and cervical cancer. We offer insights into the roles of community patient navigators in safety net hospital and underserved Chinese immigrant communities, and describe implications for patient navigation initiatives to maximize community benefits by improving access to health care for vulnerable populations.
Conclusions:
Our adaptation and implementation of a patient navigation intervention in Chicago’s Chinatown illustrates promising approaches for future navigator research.
Keywords: Chinese, Asian American, implementation science, patient navigation, breast cancer, cervical cancer
Background
Among Chinese-American women, cancer is the leading cause of death, with breast and cervical cancer among the most frequently diagnosed cancers.1,2 A myriad of linguistic, cultural, access, and health care system barriers contribute to poor cancer outcomes among this population.3,4 These forces are evident in the low utilization rates of preventive care and cancer screening in Chicago’s Chinatown, one of the largest communities of low-income, working-class Chinese immigrants.5 As an example, according to population-based survey of Chinese older adults in Chicago’s Chinatown, the percent of women reporting ever having a mammogram is 59% and reporting ever having a Papanicolaou (Pap) test is 41%. In 2012, as part of a long-standing community-based participatory research partnership, researchers and leaders from Northwestern University, the Chinese American Service League (CASL), Mercy Hospital & Medical Center, and Rush University Medical Center launched Chicago’s Chinatown Patient Navigation Collaborative. This partnership was founded to address community leaders’ concerns about the ability of Chinatown immigrant women to obtain breast and cervical cancer screening and follow-up on abnormal results. Particular concerns revolved around barriers such as language and access encountered by non-English proficient, uninsured, and underinsured Chinese immigrants that may put them at higher risk for underscreening and delayed follow-up. To tackle barriers, the partnership sought to adapt and implement previously tested patient navigation models for cancer.6-8
Patient navigation—defined broadly as support and guidance offered to patients to overcome barriers to health care6—has demonstrated efficacy in improving breast and cervical cancer outcomes, such as reducing delays to diagnostic resolution and initiation of treatment.9-11 A growing body of literature suggests that patient navigation has greatest impact in low-resource settings and among populations most at risk for delayed follow-up.10 But gaps remain in the science of dissemination and implementation of patient navigation. For example, few studies have explored adaptation, implementation, and dissemination of cancer-related patient navigation programs in immigrant communities.9,11,12 None have targeted Chinese immigrant populations. Moreover, few detailed descriptions of navigation programs have been published that contextualize navigator roles.7 This dearth of detail is at odds with calls to improve intervention reporting and the dissemination and implementation of health interventions within context, or the set of circumstances or unique factors, that surround the intervention.13,14
Thus, our goal in this article is to describe the adaptation and implementation of the Chinatown Patient Navigation Collaborative’s community-level patient navigation intervention for breast and cervical cancer. We underscore elements of the intervention’s cultural, organizational, and community contexts to advance knowledge about operationalizing patient navigation programs in culturally isolated, immigrant communities. Outcomes from the patient navigation implementation hybrid trial will be reported separately.
Methods
The setting for partnership development
Chicago’s Chinatown has a history stretching back to the early 1900s. One of the Chicago’s most culturally rich neighborhoods, it is home to 42 060 Chinese immigrants and their descendants from mainland China, Hong Kong, and Taiwan.15 Despite Chinese immigrants being widely viewed as better educated and more well off than the general US population, Chinatown ethnic enclaves belie these popular beliefs. Among all Chinese living in Chicago and its surrounding suburbs, those with the lowest socioeconomic position reside in Chinatown. Nearly 50% of households have income less than US$25 000.15 Among Chinese older adults aged 65 years and over in Chinatown, over 40% have less than high school education, 9 out of 10 live below the poverty line, and over three-quarters do not speak or read English.16
Chicago’s Chinatown has long been underrepresented in health research, and investigators at Northwestern University Feinberg School of Medicine and Rush University Medical Center have sought to forge research infrastructures that would cultivate community-engaged research addressing needs in the Chicago Chinatown community. When an opportunity in 2012 arose to apply for National Cancer Institute (NCI) grant funding to address barriers to breast and cervical cancer screening and follow-up, we formalized the Chinatown Patient Navigation Collaborative as a community-engaged research partnership among investigators at Northwestern and Rush, community leaders at CASL, and leadership at Mercy Hospital & Medical Center (Mercy).
CASL, at the heart of Chicago’s Chinatown community, is the largest social service agency in Chinatown. Chinese American Service League offers resources and programs in youth education and development, family counseling and social services, adult employment and training, elder services, housing, financial literacy, and citizenship and immigration. Mercy Hospital & Medical Center is the nearest medical center, located within the Greater Chinatown area. Mercy is a long-standing safety net hospital. Mercy is also the largest provider of screening mammograms and Pap tests for the state-funded Illinois Breast & Cervical Cancer Program (IBCCP) that provides eligible uninsured and underinsured women with free mammograms, Pap tests, and follow-up diagnostic screenings and services. Women eligible for the IBCCP program are Illinois residents aged 35 to 64 years, and without health insurance.17
Ours was a partnership of synergistic goals. We expected the Chinatown Patient Navigation Collaborative’s intervention (referred hereafter as the Chinatown Patient Navigation Program) would expand opportunities for community outreach and health education for CASL clients. We also anticipated that the Chinatown Patient Navigation Program would increase linguistic and cultural appropriateness as well as quality and continuity of care for Mercy’s Chinese patient population.
Overview of intervention design and description
Funded through the NCI as a hybrid type 1 implementation research study, the Chinatown Patient Navigation Program was an adaptation and implementation of the cancer patient navigation interventions developed by the national Patient Navigation Research Program (PNRP) and our prior scaling of the PNRP intervention to the county-level in DuPage County, IL.6,8 In the first phase of the study, we adapted a patient navigation intervention for Chinatown. In the second phase, we implemented and evaluated the program. This article focuses on describing intervention adaptation and implementation. The Institutional Review Boards at Northwestern University Feinberg School of Medicine and at Mercy Hospital & Medical Center approved all study protocols.
Conceptual framework
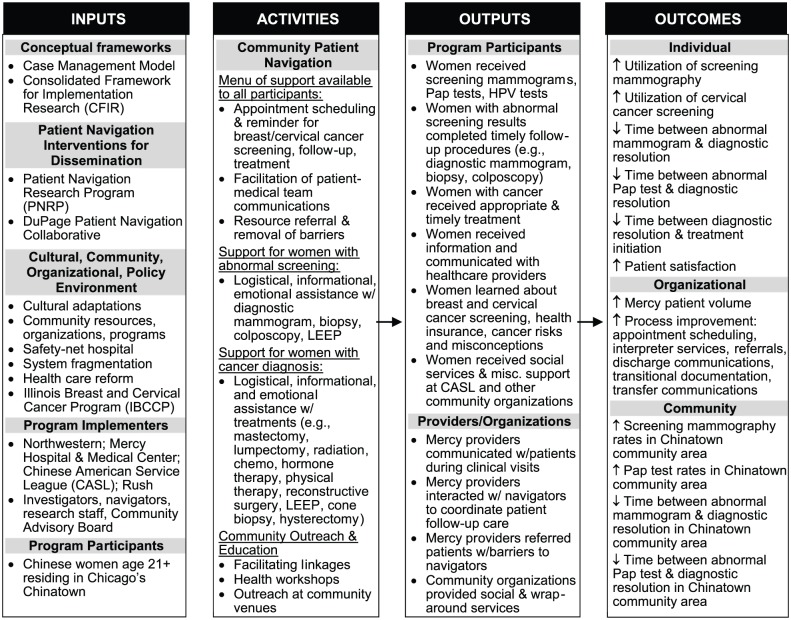
Our conceptual framework integrates the Case Management Model from the PNRP and the Consolidated Framework for Implementation Research (CFIR). The Case Management Model informs 4 components of a patient navigator’s role: (1) identifying cases, (2) identifying individual barriers to care, (3) designing and implementing a care plan addressing those barriers, and (4) tracking through completion of all services.6 While the Case Management Model provides a framework for core elements of a navigation program, CFIR guides adaptation and implementation processes with salient constructs across multiple domains: (1) characteristics of an intervention, (2) inner organizational setting, (3) outer setting, (4) characteristics of those implementing an intervention, and (5) processes for implementation.14 These constructs underscore attention to specific facets of an intervention, including characteristics of an intervention’s internal and external context as shapers of intervention success. See Logic Model in Figure 1.
Figure 1.
Logic Model for the Chinatown Patient Navigation Program.
Results
Formative research
Between June and August 2014, we conducted focus groups among a convenience sample of Chicago Chinatown women, exploring their experiences with the US health care system and culturally appropriate strategies for participant engagement. Detailed findings are published elsewhere, but briefly, focus groups identified cultural and contextual barriers and facilitators to inform intervention adaptation.18,19 Findings confirmed Chinatown women’s barriers to care, such as transportation, language, lack of Chinese-speaking providers, and perceived stigma. Findings also illuminated preferences among women to limit their family dependency with respect to health care, and elevated physician recommendation and informational and logistical support as facilitators to cancer screening.
Community Advisory Board
In recognition of the vital role of community expertise and engagement in all study components, we engaged a Community Advisory Board (CAB) of long-standing community advocates, cancer survivors, and representatives from health and social service organizations serving Chicago’s Chinatown. Our CAB convened on a quarterly basis to vocalize community needs and ensure cultural appropriateness of research questions and intervention programming.
Adaptation process
The core of the Chinatown Patient Navigation Program was derived from the PNRP and DuPage navigation interventions, including navigator roles of identifying and mitigating patient barriers, facilitating communications between patients and care teams, enhancing referral systems, documenting/reviewing medical records and navigation logs, conducting research activities, and performing community outreach and education.7,20 We adapted the prior navigation interventions with attention to CFIR domains, CAB input, and formative research findings. These adaptations included cultural adaptations to tailor the PNRP and DuPage navigation interventions to Chinese women and process adaptations to situate the intervention within a safety net hospital and urban Chinatown community.
It has been posited that cultural relevance—alignment to beliefs, values, traditions—to a cultural group increases intervention effectiveness and that the greater the cultural adaptations, the better the outcomes.21 Cultural adaptation involves not just surface structure adaptations of observable aspects, but deep structure adaptations addressing social, historical, and psychological factors.22 Thus, we addressed beliefs such as fatalism, hiding one’s illness to “save face” and avoid bad luck, and traditional gender and family roles identified from our formative research and prior work.18,23 From these beliefs and traditions, we developed intervention messages and strategies. For example, to highlight family values and counter tendencies to neglect self-care, we encouraged women to undergo cancer screenings as an aspect of taking care of their family. To counter stigmas, we leveraged case studies of Chinese celebrities and prominent Chinatown community leaders who have been diagnosed with cancer and who have since become advocates of cancer screening.
Motivated by CFIR inner setting domains as key drivers in implementation, we placed emphasis on developing strategies to align the navigation intervention with the organizational and community settings where navigators would spend most of their time. For example, to leverage existing organizational structures and processes of breast and cervical screening, follow-up, and treatment, we elected for navigators to work alongside Mercy’s IBCCP office. To enhance Mercy’s readiness for implementation, we integrated navigators as core members of the medical care team, with access to hospital networks and systems. To embed navigators in clinical teams, navigators formed strong working relationships through open communications and were involved in quality assurance efforts. We considered the social realities in which Chinese immigrant women lived and worked, and opted to deploy navigators that moved freely among multiple Chinatown settings to provide health education and outreach—orienting the intervention toward community patient navigation.
Community patient navigators
We recruited and hired navigators through CASL, Mercy, Northwestern, and Rush, as supported by NCI grant funding. Preferred qualifications included tri-lingual proficiency (English and 2 Chinese dialects: Mandarin and Cantonese) and high school graduate. The collaborative research team interviewed applicants, and the CASL co-investigator conducted language proficiency testing. Between April 2013 and July 2017, we hired 9 individuals to the navigator positions, with salaries commensurate with community health workers in the Chicago, IL, area. The navigation team ranged from 1 to 5 navigators at any given point. Aligned with the targeted sex-specific cancers of interest, all navigators were women. All 9 had some college/college degree and 5 had master’s degrees in social work, public health, or a related scientific field. All 9 were fluent or conversationally proficient in Mandarin, 6 were fluent in Cantonese, and 3 were fluent in Toishanese. Navigators who left the project did so to pursue graduate study or career advancement opportunities.
Navigator training and supervision
Navigators underwent extensive training at Mercy, including on-the-job resource and administrative training, clinical shadowing, and onboarding as Mercy employees/affiliates with access to electronic medical records and appointment scheduling systems. Navigators also learned alongside the training of resident physicians, in the form of case studies, review of films, reports, and medical histories. Navigators attended Mercy’s biweekly breast conferences, weekly tumor boards, and quarterly cancer committees for ongoing training to improve medical knowledge and proficiency with hospital resources and procedures. In addition to training at Mercy, navigators received research training at Northwestern regarding study protocols, recruitment and enrollment, protection of human subjects, survey administration, and process tracking. Through CASL, navigators were introduced to community and social service referral resources in the Chicago Chinatown area.
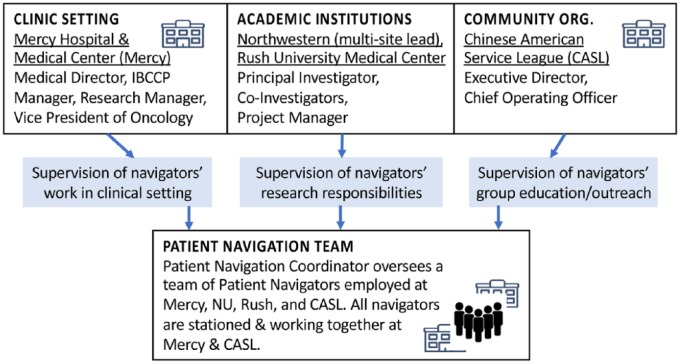
Although hired through different institutions, navigators were all based in the Chinatown community, with workstations at CASL and Mercy Hospital. The navigators worked together as a team and supervision of the Chinatown navigation team reflected the joint nature of the research partnership (Figure 2). The Northwestern investigator and a master’s-level project manager directly supervised the navigators’ research responsibilities, ensuring navigators’ fidelity to recruitment, intervention, and evaluation protocols. Navigators’ research responsibilities included participant recruitment and enrollment into the navigation program, as well as logging of patient barriers and navigation activities. A team at Mercy consisting of the Medical Director of Mercy’s Family Health Center, Mercy’s Vice President of Oncology, and the IBCCP Nurse Manager supervised the navigators’ work in the clinical setting, with a lead patient navigator coordinating the navigation workflow and supporting the recruitment, training, and supervision of other navigators. Chinese American Service League’s executive director supervised the navigators’ community health education and outreach, working with navigators to host health workshops and events at CASL and in the community. These community health education group events about breast and cervical cancer screening were adapted from Research-Tested Intervention Programs (RTIPs)24 and supported by Community Preventive Services Task Force recommendations for using group education to inform and motivate participants to seek cancer screenings.25 Educational content about accessing services was adapted from materials developed by IBCCP and Mercy. Monthly meetings brought together all project investigators, staff, and navigators to optimize available resources. Weekly project meetings involved discussing challenging cases, navigation strategies, and clinical and supportive care processes.
Figure 2.
Organizational support system for Patient Navigation Team.
Navigation participants
Women were eligible to participate in the Chinatown Patient Navigation Program research study if they self-identified as Chinese, were aged 21 years or older, resided in one of the 8 Chicago zip codes corresponding to Chinatown’s geographical boundaries, and were uninsured, had public insurance, or were newly insured via the Affordable Care Act (ACA). We took a multifaceted approach to recruitment. At Mercy, navigators recruited women through the IBCCP program and while in outpatient waiting rooms. Navigators also relied on referrals from hospital staff. Referrals came from the medical care team after a patient’s abnormal screening, and from medical providers in the oncology and infusion departments, social workers, and admissions staff when they encountered Chinese-speaking patients. In the community, navigators recruited women through CASL, print media, and by word of mouth at local senior housing, churches, schools, and businesses. To enroll participants into the research study, navigators conducted a brief eligibility screener, presented study information, obtained informed consent, and scheduled an appointment to administer an intake form and baseline health questionnaire. Women who did not meet the inclusion criteria (eg, lived outside the study’s 8 zip code areas) received standard of care at Mercy for breast and cervical cancer screenings, including referral to Mercy’s IBCCP. Participant enrollment occurred between January 2014 and December 2017.
Community patient navigation intervention
Between January 2014 and December 2017, we provided navigation services to 678 women. Salient demographic characteristics of the participants are shown in Table 1. Self-reported utilization of screening mammography and Pap tests was gathered in the baseline health questionnaire, and those results are displayed in Table 2. Our menu of navigation services for breast and cervical cancer early detection, diagnosis, and treatment offered navigation support through breast and cervical cancer screening for all enrollees, through diagnostic resolution for women with an abnormal cancer screening result, and through treatment completion for women diagnosed with cancer. Specifically, for all women, navigators offered assistance with appointment scheduling and sent reminders for mammography, Pap tests, and human papillomavirus (HPV) screening. For all women, navigators also facilitated patient communication with the health care team by accompanying patients to clinic visits, and reduced barriers (eg, cultural, transportation, and financial/insurance) with education, outreach, and referrals to community, local, and state resources.
Table 1.
Chinatown Patient Navigation Program participant self-reported characteristics at baseline (N = 678).
| Characteristic | N (%) |
|---|---|
| Age (years) | |
| 21-39 | 71 (11) |
| 40-49 | 205 (30) |
| ⩾50 | 400 (59) |
| Missing | 2 |
| Educational attainment | |
| ⩽Some high school | 312 (47) |
| High school graduate | 223 (34) |
| Some college | 77 (12) |
| College graduate | 53 (8) |
| Missing | 13 |
| Recent immigrant (<5 years in the United States) | |
| No | 596 (91) |
| Yes | 57 (9) |
| Missing | 25 |
| Lives alone | |
| No | 605 (90) |
| Yes | 67 (10) |
| Missing | 6 |
| Household income (in US$1000) | |
| <10 | 137 (21) |
| 10-15 | 102 (15) |
| 15-20 | 127 (19) |
| 20-35 | 202 (31) |
| 35-200 | 93 (14) |
| Missing | 0 |
| Preferred dialect/language | |
| Cantonese | 443 (65) |
| Mandarin | 161 (24) |
| Toishanese | 71 (10) |
| English | 3 (0.5) |
| Don’t know/Missing | 2 |
| Insurance type | |
| Medicare | 76 (11) |
| Medicaid | 269 (40) |
| Private | 103 (15) |
| Other insurance | 41 (6) |
| None/Don’t know/Missing | 189 (28) |
| Have a primary care provider (PCP) | |
| Yes | 366 (54) |
| No | 312 (46) |
Table 2.
Chinatown Patient Navigation Program participant self-reported utilization of screening mammography and Pap tests at baseline.
| Characteristic | N (%) |
|---|---|
| Screening mammography (aged 40+ years) (n = 605) | |
| 1 year ago or less | 271 (45) |
| More than 1, up to 2 years ago | 58 (10) |
| More than 2, up to 3 years ago | 62 (10) |
| More than 3, up to 5 years ago | 46 (8) |
| More than 5 years ago | 45 (7) |
| Never had a mammogram | 119 (20) |
| Missing | 4 |
| Most recent Pap test (aged 21-65 years) (n = 582) | |
| 1 year ago or less | 240 (42) |
| More than 1, up to 2 years ago | 54 (9) |
| More than 2, up to 3 years ago | 73 (13) |
| More than 3, up to 5 years ago | 59 (10) |
| More than 5 years ago | 49 (9) |
| Never had a Pap test | 99 (17) |
| Missing | 8 |
Abbreviation: Pap, Papanicolaou.
Navigators offered repeat screening reminders through the duration of the intervention period. Mammography screening reminders were in accordance with the American College of Radiology’s recommended annual screening mammography interval for women starting at age of 40 years with normal breast cancer screening results.26 Repeat cervical cancer screening reminders were based on US Preventive Services Task Force clinical recommendation of screening for women 21 to 65 years of age.27 Navigators tracked screening intervals using the navigation program’s administrative logs.
For women with abnormal mammography results, navigators provided guidance through diagnostic mammograms, ultrasounds, biopsies, and surgical consultations. For women with a breast cancer diagnosis, navigators provided logistical, informational, and emotional support through mastectomy, lumpectomy, radiation, chemotherapy, hormone therapy, physical therapy, and reconstructive surgery. Navigators guided women with abnormal cervical cancer screening results through colposcopy, loop electrosurgical excision procedure, and cone biopsy; and guided women diagnosed with cervical cancer through hysterectomy, chemoradiation, and other treatments. Navigation of breast or cervical cancer patients also included linkages to social workers/counseling, support groups, nutrition, and survivorship clinics in their preferred language.
Although most clinical navigation interactions took place at Mercy and its affiliated clinics, Chinatown patient navigators guided cancer patients through care received at other health care settings, such as Stroger Hospital of Cook County (public hospital) and cancer centers. In addition to responsibilities in clinical settings, navigators conducted community health education and outreach, disseminating information about breast and cervical cancer, HPV, and women’s health at CASL workshops, health fairs, schools, churches, and local businesses. Navigators also linked women with local health and social service organizations. For example, navigators referred women to local agencies for public transit cards and organizations offering hepatitis B and colorectal cancer screenings.
To optimize navigation services around patient schedules and clinic workflows, we did not systematically assign patients to specific navigators. Other than navigator–patient concordance on preferred language/dialect, navigators worked as a team and coordinated their work with the support of administrative tracking logs, electronic health records, shared calendars, daily communications, and shared workspaces. Navigators’ communication to patients regarding appointment scheduling, follow-up, and health resources was multimodal depending on patient preference, including in-person, via telephone, and/or the mobile messaging app, WeChat, which is widely used among Chinese. When communicating with patients who preferred WeChat over other modes of communication, navigators optimized confidentiality using a WeChat account set up specifically for the navigation program through password-protected mobile devices designated for research study use only.
Expansion of navigation activities
Changes in policy and emerging needs presented opportunities to expand Chinatown patient navigation activities during the intervention period. In particular, a navigation response was needed with implementation of the ACA and the accompanying insurance marketplaces, changes to insurance plans, and networks of primary care providers (PCPs) in 2013. By January 2014 when ACA-driven health insurance coverage took effect, Chinatown patient navigators were navigating insurance- and PCP-related access barriers for breast and cervical cancer screening and care—including enrolling women for insurance, educating women on their insurance plans, informing women about patient rights, finding in-network PCPs, and facilitating screening referrals from PCPs. In addition to one-on-one interactions, navigators developed bilingual health insurance booklets and conducted group workshops to help patients navigate their health insurance. Navigators’ work ameliorating health-insurance-related barriers to cancer screening complemented the work of others at Mercy providing auxiliary support, such as financial counselors who experienced difficulty providing Chinese language support. To enable the Chinatown Patient Navigation Program to better address insurance barriers, we added a navigator to our team who was also an ACA-certified navigator. This navigator provided guidance and training to the other navigators, thus enhancing the program’s collective responsiveness to insurance-related cancer screening barriers.
For patients who remained uninsured and who did not qualify for IBCCP (which only offers free services up through a cancer diagnosis), navigators also connected patients with public financial assistance programs. One such program was Chicago Cook County’s CareLink, which helps cover the costs of health care services at public health care facilities for Cook County residents not eligible for other public insurance programs.28
Discussion
Concerns about the ability of Chinatown immigrant women to obtain breast and cervical cancer screening and follow-up on abnormal results due to myriad language, cultural, and access barriers spurred the establishment of the Chinatown Patient Navigation Collaborative in Chicago’s Chinatown. Our description of a community-based patient navigation intervention for breast and cervical cancer in Chicago’s Chinatown addresses the need to articulate navigation interventions and functions that would enhance understanding of navigation in different contexts and catalyze opportunities for replication, dissemination, and implementation.13,29 The Chinatown Patient Navigation Program described in this report has multiple implications for practitioners.
Collaborative partnerships have long brought people and organizations working together toward a common purpose.30 Our report detailing adaptation of navigation protocols and implementation with respect to culture, institutional and community environments, and health policy affirms the complex interplay of system-, organization-, provider-, and client-level intervention domains.14,31 Our report also lends support to intervention adaptations such as de-emphasis or emphasis, addition of components, language and cultural adaptations to make interventions suitable to settings where it would otherwise not fit.32,33 Although we proceeded with cultural adaptations to the PNRP and DuPage patient navigation interventions, our experience was that the bulk of intervention adaptation was iterative toward community, organizational, and external environments to align with community structures, clinic processes/work flows, emerging community needs, and changes in policy. Examples included ongoing relationship building with the health care team and increasing intensity of health-insurance-related work. Attention to iterative aspects of adaptation may optimize use of an intervention’s core components,34 but the mechanisms by which these adaptations enhance the efficacy of navigation interventions are not well documented and require further study.
Formidable challenges encountered by the Chinatown Patient Navigation Program included the navigation effort that went toward mitigating health insurance barriers. Chinatown patient navigators have temporarily filled a role carved by increasingly complex health care systems, but it was a strain on already limited resources. In response to challenging health care environments, intervention adaptability and navigators’ abilities to wear multiple hats as we have described may be crucial for implementation success. However, patient navigator role ambiguity also poses risks of overburden, lower service quality, undesirable work environments, and inefficiencies.35,36 Despite Chinatown Patient Navigation Program navigators being key to program implementation, turnover was high as many navigators left to pursue further educational study or career opportunities. Human resource issues of recruitment and high turnover may be inherent in patient navigation programs,37 so creating checklists and standard work38 (documented known best practices on how to execute specific processes of the program) and developing navigator leadership may be useful strategies for successful implementation of navigation programs.
To advance patient navigation sustainability, future directions could explore transition of patients from initial high-intensity navigator interaction to low-level interaction characterized by long-term peer support or self-management, as well as explore the scaling of community patient navigation. We have described how the Chinatown Patient Navigation intervention organically expanded beyond direct breast and cervical cancer to health care access broadly. Whereas navigation has primarily been disease specific with focus on specialty care,6 we envision that the infrastructure and processes in place for breast and cervical cancer patient navigation in Chicago’s Chinatown could segue into patient navigation for other prevalent health concerns and wellness. Example topics include women’s health, perinatal care, sexual health, mental health, and navigation targeting social determinants of health. In addition, the growing complexity of the health care delivery system may warrant even greater collaborative and integrative patient navigation programming in the future.
Limitations of this study should be noted. First, we do not know the degree to which our methods may be generalizable to other settings or population groups. However, our approach may shed light on adaptation and implementation processes for further consideration. Another limitation is that although our intervention description advances understanding of how navigators operate within existing community structures and resource-thin health care environments, our intervention description cannot speak to efficacy or cost-effectiveness. Formal program evaluation and cost-effectiveness analyses would be valuable for guiding future patient navigation initiatives and policy. Finally, another potential study limitation is that we illustrate intervention adaptation and implementation, but what happens with sustaining, or de-implementing navigation components are important areas of future research to advance dissemination and implementation science.
Conclusions
There is a great need to disseminate patient navigation programs for underserved populations. As health care reform continues within the United States, navigators may play increasingly diverse roles across the health care continuum. Detailed descriptions of program components should be made available to catalyze the work of researchers, health service providers, and policy-makers. Navigation interventions need to be responsive to their cultural, organizational, and community context, and our description of a community-based patient navigation intervention for breast and cervical cancer in Chicago’s Chinatown offers critical insights into the potential roles of navigators within underserved immigrant communities and safety net clinical settings.
Acknowledgments
The authors acknowledge the Chinese Health, Aging, and Policy Program; the Chinatown Community Advisory Board; and Catherine O’Brian, Marcie Kirschner, Shaneah Taylor, and Jen Cooper who have provided invaluable input.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (grant numbers R01CA163830, R34MH100393, and U54CA203000). In addition, this work was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences (grant number UL1TR000150). The sponsors did not participate in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript and the decision to submit the manuscript for publication.
Declaration of conflicting interests:The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.A.S. is a member of the United States Preventive Services Task Force (USPSTF). This article does not necessarily represent the views and policies of the USPSTF.
Author Contributions: M.A. Simon led the concept development, study design, interpretation of data, and the drafting and revision of the article. L.S. Tom and I. Leung contributed to the study design, interpretation of the data, and the drafting of this article. E. Wong, E. Knightly, D. Vicencio, and X. Dong contributed to the concept development, study design, and article revision. A. Yau and K. Ortigara contributed to the study design and article revision. All authors approved the final version of the article.
Research involving Human Participants and Informed consent: The Institutional Review Boards at Northwestern University Feinberg School of Medicine and at Mercy Hospital and Medical Center approved all study protocols. Written consent was obtained from all participants of the Chicago Chinatown Patient Navigation Program.
ORCID iD: Melissa A Simon  https://orcid.org/0000-0001-9021-7315
https://orcid.org/0000-0001-9021-7315
References
- 1. Gomez SL, Noone AM, Lichtensztajn DY, et al. Cancer incidence trends among Asian American populations in the United States, 1990-2008. J Natl Cancer Inst. 2013;105:1096–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hastings KG, Jose PO, Kapphahn KI, et al. Leading causes of death among Asian American subgroups (2003-2011). PLoS ONE. 2015;10:e0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guidry JJ, Torrence W, Herbelin S. Closing the divide: diverse populations and cancer survivorship. Cancer. 2005;104:2577–2583. [DOI] [PubMed] [Google Scholar]
- 4. Ngo-Metzger Q, Massagli MP, Clarridge BR, et al. Linguistic and cultural barriers to care. J Gene Int Med. 2003;18:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Simon MA, Li Y, Dong X. Preventive care service usage among Chinese older adults in the Greater Chicago area. J Gerontol A Biol Sci Med Sci. 2014;69:S7–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Freund KM, Battaglia TA, Calhoun E, et al. National cancer institute Patient Navigation Research program. Cancer. 2008;113:3391–3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Samaras AT, Murphy K, Nonzee NJ, et al. Community-campus partnership in action: lessons learned from the DuPage County Patient Navigation Collaborative. Prog Community Health Partnersh. 2014;8:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Simon MA, Tom LS, Nonzee NJ, et al. Evaluating a bilingual patient navigation program for uninsured women with abnormal screening tests for breast and cervical cancer: implications for future navigator research. Am J Public Health. 2015;105:e87–e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Freund KM, Battaglia TA, Calhoun E, et al. Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst. 2014;106:dju115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bensink ME, Ramsey SD, Battaglia T, et al. Costs and outcomes evaluation of patient navigation after abnormal cancer screening: evidence from the Patient Navigation Research Program. Cancer. 2014;120:570–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jojola C, Cheng H, Wong L, Paskett E, Freund K, Johnston F. Efficacy of patient navigation in cancer treatment: a systematic review. J Oncol Navig Surv. 2017;8:106–115. [Google Scholar]
- 12. Bush ML, Kaufman MR, Shackleford T. Adherence in the cancer care setting: a systematic review of patient navigation to traverse barriers. J Cancer Educ. 2018:33;1222–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
- 14. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chicago Metropolitan Agency for Planning. Chinatown community vision plan: existing conditions report. http://www.cct.org/wp-content/uploads/2015/05/ChinatownCommunityVisionPlan2013.pdf. Up-dated 2014. Accessed June 4, 2017.
- 16. Dong X. The Pine Report. Chicago, IL: Rush Institute for Health Aging, Rush University Medical Center; 2013. [Google Scholar]
- 17. Illinois Department of Public Health. IL Breast & Cervical Cancer Program (IBCCP). http://dph.illinois.gov/topics-services/life-stages-populations/womens-health-services/ibccp. Accessed February 28, 2019.
- 18. Simon MA, Tom LS, Leung I, et al. Chinese immigrant women’s attitudes and beliefs about family involvement in women’s health and healthcare: a qualitative study in Chicago’s Chinatown. Health Equity. 2018;2:182–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Simon MA, Tom LS, Taylor S, Leung I, Vicencio D. ‘There’s nothing you can do … it’s like that in Chinatown’: Chinese immigrant women’s perceptions of experiences in Chicago Chinatown healthcare settings. [published online ahead of print January 28, 2019]. Ethn Health. doi: 10.1080/13557858.2019.1573973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parker VA, Clark JA, Leyson J, et al. Patient navigation: development of a protocol for describing what navigators do. Health Serv Res. 2010;45:514–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barrera M, Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol. 2013;81:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. J Commun Psychol. 2000;28:271–290. [Google Scholar]
- 23. Simon MA, Tom LS, Dong X. Breast cancer screening beliefs among older Chinese women in Chicago’s Chinatown. J Gerontol A Biol Sci Med Sci. 2017;72:S32–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. National Cancer Institute. Research-tested interventions programs. rtips.cancer.gov/rtips. Accessed February 27, 2019.
- 25. Community Preventive Services Task Force (CPSTF). The community guide: cancer screening: group education for clients—breast cancer. https://www.thecommunityguide.org/findings/cancer-screening-group-education-clients-breast-cancer. Accessed February 26, 2019.
- 26. American College of Radiology. ACR position statement on screening mammography and health care coverage. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Screening-Mammography-and-Health-Care-Coverage. Up-dated 2016. Accessed February 26, 2019.
- 27. US Preventive Services Task Force. Published recommendations. https://www.uspreventiveservicestaskforce.org/BrowseRec/Index. Accessed June 30, 2017.
- 28. Cook County Health. Assistance programs: patient financial services. http://www.cookcountyhhs.org/patient-services/billing-financial-assistance/assistance-programs/. Accessed February 26, 2019.
- 29. Robinson-White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: a systematic review. Cancer Nurs. 2010;33:127–140. [DOI] [PubMed] [Google Scholar]
- 30. Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annu Rev Public Health. 2000;21:369–402. [DOI] [PubMed] [Google Scholar]
- 31. Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Quarter. 2004;82:581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aarons GA, Green AE, Palinkas LA, et al. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implement Sci. 2012;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clin Psychol Sci Prac. 2006;13:295–310. [Google Scholar]
- 34. Bowen DJ, Sorensen G, Weiner BJ, Campbell M, Emmons K, Melvin C. Dissemination research in cancer control: where are we and where should we go? Cancer Causes Control. 2009;20:473–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jaskiewicz W, Tulenko K. Increasing community health worker productivity and effectiveness: a review of the influence of the work environment. Hum Resour Health. 2012;10:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. O’Brien MJ, Squires AP, Bixby RA, Larson SC. Role development of community health workers: an examination of selection and training processes in the intervention literature. Am J Prev Med. 2009;37:S262–S269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bone L, Edington K, Rosenberg J, et al. Building a navigation system to reduce cancer disparities among urban black older adults. Prog Community Health Partnersh. 2013;7:209–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bicheno J. The Lean Toolbox for Service Systems. Johannesburg, South Africa: PICSIE Books; 2008. [Google Scholar]