Abstract
Objective:
To observe the venous leakage of penile veins through cavernosometry and cavernosography, using CT combined with three-dimensional volume rendering.
Methods:
186 consecutive erectile dysfunction patients (20–40 years old) with suspected venous leakage diagnosed by clinicians were enrolled. All patients underwent intracavernous injection of vasoactive agents combined with Doppler ultrasound to identify venous leakage.
Results:
Taking intracavernous injection combined with Doppler ultrasound as the “gold-standard”, 47/186 (25.3%) patients had negative venous leakage, and 139/186 (74.7%) patients had positive venous leakage. CT cavernosography showed that 22/139 (15.8%) cases were isolated deep dorsal vein or crural vein leakage, and 117/139 (84.2%) cases were complex venous leakage. Three types of deep dorsal vein were seen: single-branch 42/139 (30.2.%), double-branch 45/139 (32.4%), and complex 31/139 (22.3%). Three types of prostatic venous plexus were seen: single-branch 26/139 (18.7%), multiple-branch 36/139 (25.9%), and plexus 39/139 (28.1%). A total of 166 crural veins were revealed in 129 patients. Crural veins had three origins: medial dorsal side (112/166, 67.5%), lateral ventral side (30/166, 18.1%) and the curs tip (24/166, 14.4%).
Conclusion:
To achieve the expected success rate of ligation surgery or endovascular embolization, candidates for the procedures should be carefully selected through CT cavernosography, which can provide elaborate images and information about the venous leakage.
Advances in knowledge:
A modified evaluation method was used in this study to monitor the intracavernous pressure during examination. New classifications of the deep dorsal vein, prostatic venous plexus and crural vein are described in this study.
Introduction
Vasculogenic pathology, also known as venous leakage, is accepted as the main cause of organic ED.1 Because of their ability to reveal large regions of veins, cavernosometry and cavernosography have been adapted to evaluate venous leakage and are the only diagnostic procedures. The main reported treatment for venous leakage of penile veins is surgical ligation and endovascular embolization.2–4 Unfortunately, the reported success rate, especially the long-term satisfaction, varies among patients. As a result, the 2013 guidelines did not recommend the vascular surgery, stating that the criteria for patient selection were still unknown.
According to the reported successful results of vascular surgery, the patients enrolled have had highly selected isolated venous leakage,2–6 with a satisfaction time around 12 months. Although this satisfaction time is still short, it can be accepted by most patients under our national conditions. Many Chinese families have long wanted to have a child. If the procedure is successful, it can solve practical issues for many families.
Cavernosometry and CT cavernosography images combined with the volume rendering (VR) technique can provide elaborate details of venous leakage. This combined technique shows all the branches of penile veins and locates the origin of the crural vein, which will be ligated in the vascular surgery or an endovascular procedure. CT cavernosography can be used to select patients who would benefit from surgical or endovascular management.
methods and Materials
All patients were given adequate explanations of the details of the procedure to mitigate any anxiety or fear during the procedure. Written informed consent was obtained from all patients for the publication of this study and accompanying photographs under the guidelines of the Medical Ethics Committee of the Huazhong University Graduate School and Faculty. Two radiologists independently assessed the CT images.
Patients selection
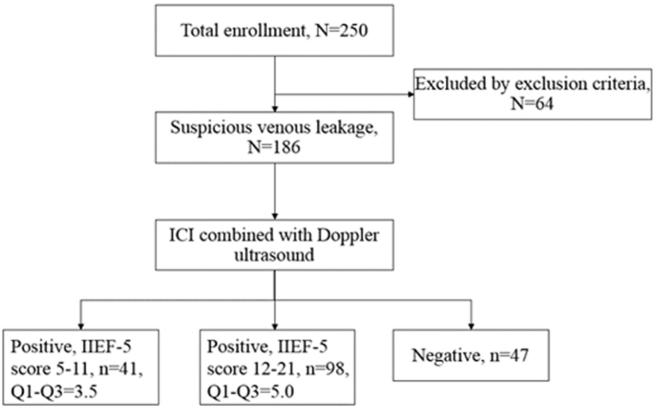
In total, 186 consecutive erectile dysfunction (ED) patients (20–40 years old) with suspected leakage of penile veins were enrolled (Figure 1). The International Index of Erectile Function (IIEF-5) questionnaire was conducted in all the patients to classify the severity of the disease.7 Patients were diagnosed with ED when the score of IIEF-5 was less than 22. Nocturnal penile tumescence and rigidity testing was used to differentiate organic ED from psychogenic.8 Intracavernous injection (ICI) of vasoactive agents combined with Doppler ultrasound was used to categorize the type of vasculogenic impotence. According to the criteria proposed by Quam et al9 and Lue et al10 patients who underwent ICI combined with Doppler ultrasound were divided as follows: (1) normal (with no vasculogenic pathology): cavernosal artery peak systolic velocity (PSV) >25 cm s−1, cavernosal artery end-diastolic velocity (EDV) <5 cm s−1, and restrictive indices (RI) > 0.8; (2) inflow insufficiency: PSV <25 cm s−1, EDV <5 cm s−1, RI > 0.8; (3) venous leakage: PSV > 25 cm s−1, EDV > 5 cm s−1, RI < 0.8; and (4) mixed pathology: PSV < 25 cm s−1, EDV > 5 cm s−1, RI < 0.8.
Figure 1.
Flow chart of patient enrollment process. ICI, intracavernous injection; IIEF-5, International Index of Erectile Function.
Patients who met the following criteria were included:(1) preliminarily diagnosed with organic ED by detailed inquiry of disease history, physical examination and laboratory tests; (2) patients considered to have vasculogenic ED, i.e. a rigid erectile response did not appear in 10 min after ICI or did not last for 30 min;11 and (3) patients who were diagnosed with venous leakage by ICI combined with Doppler ultrasound.
The exclusion criteria were as follows: (1) diagnosis of psychogenic, neurogenic or endocrine ED; (2) diagnosis of arterial inflow insufficiency or mixed pathology by ICI combined with Doppler ultrasound; (3) drug-induced ED; (4) secondary ED to other disease or trauma; (5) contrast agent hypersensitivity; and (6) severe hepatic or renal failure.
Examination procedure
Patients underwent cavernosometry and CT cavernosography 3 days after ICI combined with Doppler ultrasound. Patients were told to take the supine position on the examination bed. The examination environment was completely private, which means that patients and doctors were not disturbed during the whole process.
After local sterilization, 20 µg of prostaglandin E1 (Alprostadil Injection, Beijing Tide Pharmaceutical Co., LTD, Beijing) was injected into the corpus cavernosum. When the penis achieved erection, the operator inserted a 7# needle (intravenous needle for single use, Shandong Weigao group medical polymer Co., LTD, Shandong) at the dorsal side of the left corpora cavernosum and injected 30–60 ml of 30% saline-diluted ioversol (320 mg ml−1) (Ioversol Injection, Jiangsu Hengrui Medicine Co., LTD, Jiangsu) at an infusion velocity of 6–180 ml min−1 through the duct that was connected with the needle to induce erection to the expected hardness. The expected erection degree during examination was assessed according to the Erection Hardness Score (EHS).12, 13 When the status of the erection was assessed as 4 according to the EHS, i.e. it kept a stable flow-to-maintain velocity, patients were considered to be well prepared for CT examination. The infusion velocity and flow-to-maintain velocity during cavernosometry were recorded and used to assess the correlation with RI in the Doppler ultrasound examination.
CT examinations were performed on a Philips Ingenuity Core 128 CT (Philips Healthcare, Cleveland, OH). The scanning parameters were as follows: 64 × 0.625 mm collimation, gantry rotation time 0.75 s, time resolution 30 ms, pitch factor 0.984. The tube voltage was 80 kV, and the tube current-time was 51–90 mAs. iDose6 was used to reduce the radiation dose. The scanning range for all examinations extended from the upper brim of the true pelvis to the most distant level of the penis.
The data constructive section thickness was 1 mm; the reconstruction increment was 1 mm. All images were analysed with post-processing software (Philips IntelliSpace Portal Release v 6.0.5.03900, Netherlands). Image post-processing methods on the workstation included three-dimensional VR, multiplanar reconstruction, and maximum intensity projection.
Taking ICI combined with Doppler ultrasound as the gold standard,14 patients with normal ultrasound parameters were considered to have psychogenic ED. Even if CT cavernosography revealed veins, patients with normal ultrasound parameters were diagnosed with normal penile haemodynamics in this study.
The venous drainage of the penis can be divided into three groups: superficial veins, intermediate veins and deep veins.15 This was the classification used for general assessment in this study. The types of deep dorsal vein and prostatic venous plexus, as well as the origin positions of the crural veins, were assessed.
Statistical analysis
All of the data were analysed in IBM SPSS Statistics 20.0. Patients with venous leakage were divided into two groups according to IIEF-5 score: score 5–11 and score 12–21. Comparisons between the score 5–11 group and the score 12–21 group were performed by using the Χ2 test for categorical variables and the Wilcoxon test for ordinal variables. The test was two-sided and used α = 0.05. A receiver operating characteristic (ROC) curve was fitted to the velocities recorded in cavernosometry and CT cavernosography. The accuracy was defined by the area under the ROC curve (AUC) with asymptotic 95% confidence intervals.
Results
All of the patients underwent cavernosometry and CT cavernosography successfully. No severe foreskin haematoma or contrast media allergy event happened. The mean effective dose was 1.1 ± 0.3 mSv (range 0.7–2.2 mSv).
Visible veins
Penile drainage veins were described in three layers: superficial veins, intermediate veins and deep veins.15 Taking ICI combined with Doppler ultrasound as the gold standard, 47/186 (25.3%) patients had normal penile haemodynamics and 139/186 (74.7%) patients had venous leakage (Table 1). Compared with negative venous leakage patients who were diagnosed by ultrasound examination, positive patients had a higher visible rate of intermediate and deep-layer veins (p < 0.001), especially of the crural vein. The types of deep dorsal vein and prostatic venous plexus in positive venous leakage patients were more complicated than those in negative patients (Table 1).
Table 1.
The visible veins and types in CT cavernosography, both in positive and negative venous leakage patients
| Positive (N = 139) | N | N % | Negative (N = 47) | N % | Statistics | p-value | |
| Visible veins | Superficial layer veins | 50 | 36.0% | 11 | 23.4% | 2.517 | 0.113 |
| Intermediate layer veins | 125 | 89.9% | 30 | 63.8% | 17.225 | <0.001 | |
| Deep layer veins | 131 | 94.2% | 30 | 63.8% | 27.927 | <0.001 | |
| Deep dorsal vein | 118 | 84.9% | 29 | 61.7% | 11.398 | 0.001 | |
| Prostatic venous plexus | 101 | 72.7% | 24 | 51.1% | 7.434 | 0.006 | |
| Crural vein | 129 | 92.8% | 29 | 61.7% | 26.573 | <0.001 | |
| Types of deep dorsal vein | −3.211 | 0.001 | |||||
| Single branch | 42 | 30.2% | 11 | 23.4% | |||
| Double branches | 45 | 32.4% | 13 | 27.7% | |||
| Complex type | 31 | 22.3% | 5 | 10.6% | |||
| Unrevealed | 21 | 15.1% | 18 | 38.3% | |||
| Types of prostatic venous plexus | −3.393 | 0.001 | |||||
| Single branch | 26 | 18.7% | 13 | 27.7% | |||
| Multiple branches | 36 | 25.9% | 6 | 12.8% | |||
| Plexus | 39 | 28.1% | 5 | 10.6% | |||
| Unrevealed | 38 | 27.3% | 23 | 48.9% |
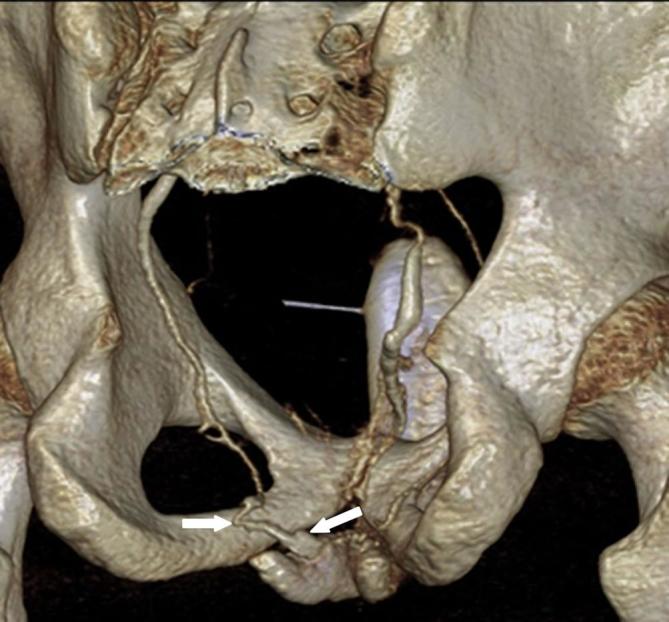
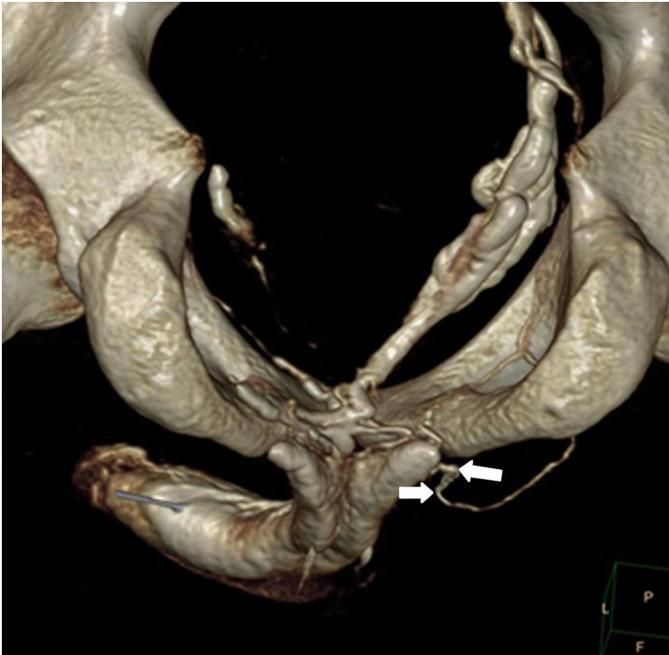
Deep dorsal veins were divided into three categories: single-branch, double-branch and complex (Figures 2–4). The prostatic venous plexus was also divided into three categories: single-branch, multiple-branch, and plexus (Figures 5–7).
Figure 2.
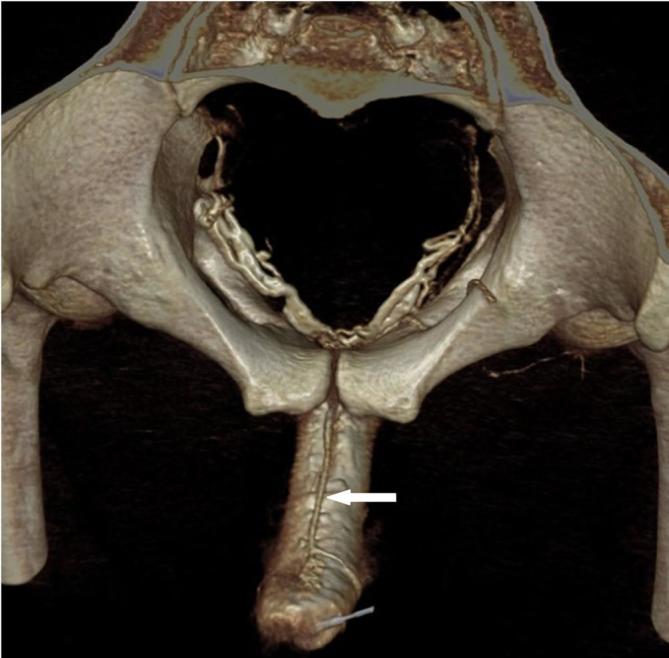
Single-branch type of the deep dorsal vein. Male, 32 years old, suffering from ED for 6 years.
Figure 3.

Double-branch type of the deep dorsal vein. Male, 27 years old, suffering from ED for 3 years. ED,erectile dysfunction.
Figure 4.

Complex type of the deep dorsal vein. Male, 25 years old, suffering from ED for 6 years. ED, erectile dysfunction.
Figure 5.

Single-branch type of the prostatic venous plexus. Male, 23 years old, suffering from ED for 4 years. ED, erectile dysfunction.
Figure 6.

Multiple-branch type of the prostatic venous plexus. Male, 36 years old, suffering from ED for 8 years. ED, erectile dysfunction.
Figure 7.

Plexus type of the prostatic venous plexus. Male, 30 years old, suffering from ED for 6 years. ED, erectile dysfunction.
A total of 166 crural veins were revealed in 129 positive venous leakage patients. The origin of the crural veins was divided into three places on each side: medial dorsal side, lateral ventral side and the crus tip (Figures 8–10). In total, 112/166 (67.5%) cases were derived from the medial dorsal side, 30/166 (18.1%) cases were derived from the lateral ventral side, and 24/166 (14.4%) cases were derived from the crus tip.
Figure 8.
Left crural vein derived from the medial dorsal side. Male, 23 years old, suffering from ED form 1 year. ED, erectile dysfunction.
Figure 9.
Right crural vein derived from the lateral ventral side. Male, 24 years old, suffering from ED for 1 year. ED, erectile dysfunction.
Figure 10.
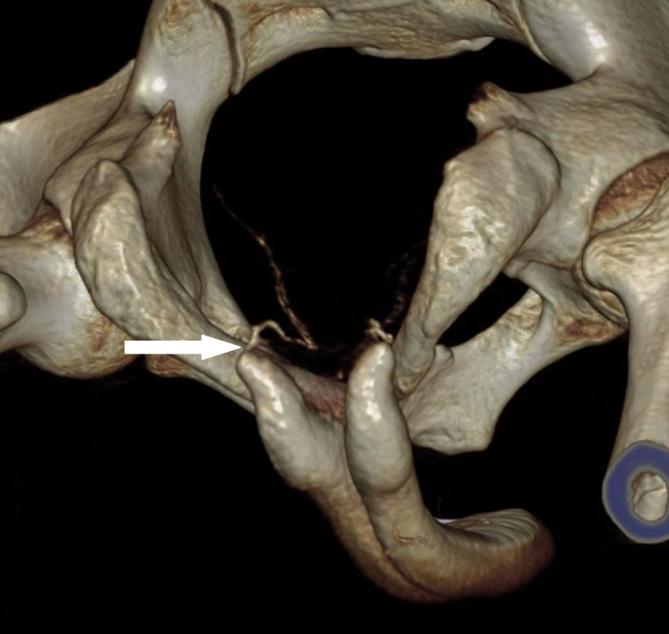
Left crural vein derived from the crus tip. Male, 26 years old, suffering from ED for 2 years. ED, erectile dysfunction.
Comparisons between the IIEF-5 score 5-11 group and score 12-21 group
The visible rates of superficial and intermediate veins in the score 5–11 group were higher than those in the score 12–21 group. The visible rates of the deep dorsal vein, prostatic venous plexus and crural vein in the score 5–11 group were higher than those in the score 12–21 group. The types of deep dorsal vein and prostatic venous plexus in the score 5–11 group were more complicated than those in the score 12–21 group. The details of the comparisons between the two groups are given in Table 2.
Table 2.
Comparisons between score 5–11 group and score 12–21 group of visible veins in positive venous leakage patients
| Visible veins | Score 5–11 group N (%) (n = 41) | Score 12–21 group N (%) (n = 98) | Statistics | p-value |
| Superficial layer veins | 27 (65.9%) | 23 (23.5%) | 22.546 | <0.001 |
| Intermediate layer veins | 41 (100%) | 84 (85.7%) | 6.513 | <0.001 |
| Deep layer veins | 41 (100%) | 90 (91.8%) | 3.551 | 0.105 |
| Deep dorsal vein | 41 (100%) | 77 (78.6%) | 10.349 | <0.001 |
| Prostatic venous plexus | 40 (97.6%) | 61 (62.2%) | 18.150 | <0.001 |
| Crural vein | 41 (100%) | 88 (89.8%) | 4.508 | 0.034 |
| Type of deep dorsal vein | −3.877 | <0.001 | ||
| Type of prostatic venous plexus | −6.821 | <0.001 |
Diagnostic accuracy of cavernosometry for venous leakage
Taking ICI combined with Doppler ultrasound as the gold-standard, the AUCs of infusion velocity and flow-to-maintain velocity in cavernosometry for the assessment of venous leakage were 0.814 and 0.916, respectively (Figures 11 and 12, Table 3). The corresponding sensitivity, specificity, positive-predictive value, negative-predictive value, cut-off and accuracy are listed in Table 3. The flow-to-maintain velocity had a higher diagnostic accuracy than infusion velocity. We proposed that when the flow-to-maintain velocity is >6 ml/min and the infusion velocity is >30 ml/min, a positive venous leakage will be diagnosed through CT cavernosography.
Figure 11.
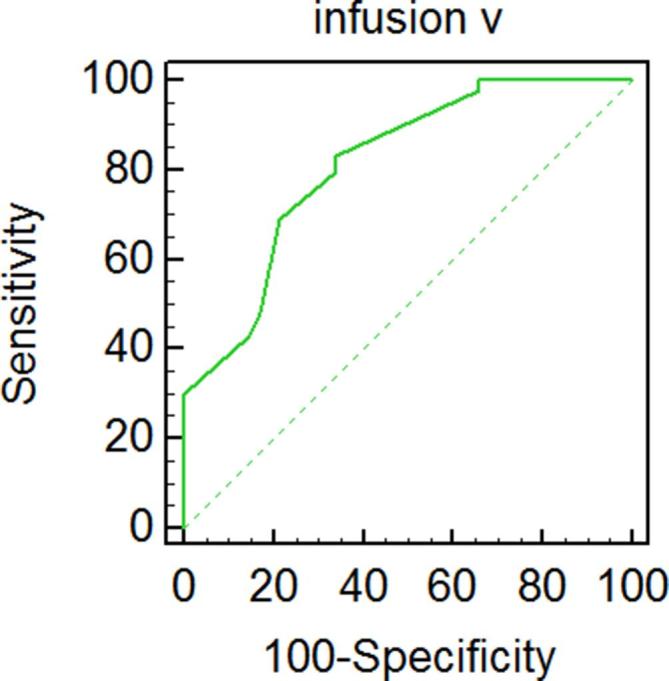
ROC curve and the AUC for infusion velocity of cavernosometry. AUC, area under the curve; ROC, receiver operating characteristic.
Figure 12.
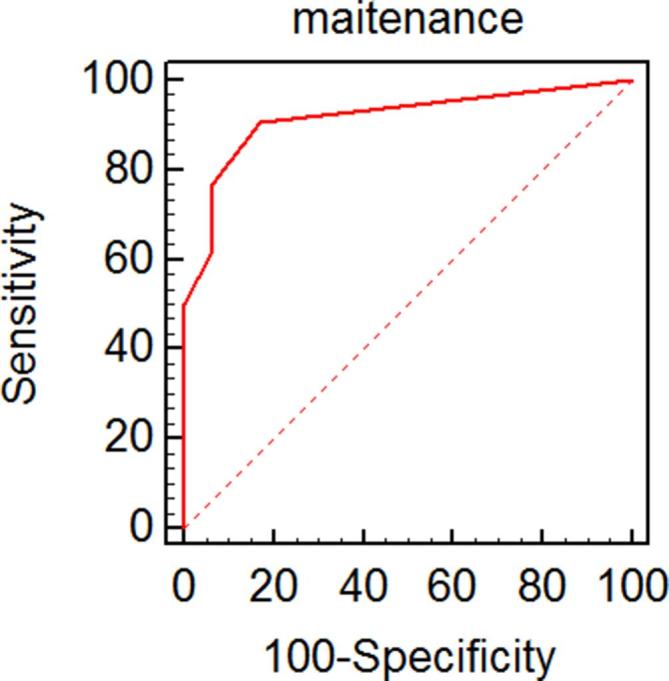
ROC and AUC for flow-to-maintain velocity of cavernosometry. AUC, area under the curve; ROC, receiver operating characteristic.
Table 3.
Cavernosometry accuracy and evaluation in diagnosing venous leakage
| Variable | AUC | AUC 95% CI | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Cut-off | Accuracy |
| Infusion V | 0.814 | 0.751–0.867 | 83.45 | 65.96 | 71.03 | 79.94 | 30 | 0.790 |
| Flow-to-maintain V | 0.916 | 0.866–0.952 | 90.65 | 82.98 | 84.19 | 89.87 | 6 | 0.887 |
AUC, area under the ROC curve; NPV, negative-predictive value; PPV, positive- predictive value.
Discussion
Penile erection requires a series of interdependent synergistic mechanisms: smooth muscle cell relaxation, increased arterial flow, and increased venous outflow restriction.15, 16 Reduced venous outflow and increased lacunar pressure of the cavernosa are the primary mechanism of penile rigidity. Impaired venous function is the most common cause of vasculogenic ED.1, 6,17
Diagnostic method
To evaluate the integrity of the vasculogenic function of ED, haemodynamic testing is necessary.18 ICI of vasoactive agents combined with Doppler ultrasound provides reliable and detailed information about penile haemodynamics and is used as an ED screening test. It can evaluate penile arterial and veno-occlusive function and can identify the type of vasculogenic pathology. Cavernosometry is used when there is a suspicion of venous leakage of penile drainage with normal arterial flow.19 Dynamic infusion of cavernosometry and cavernosography is widely used as a reference diagnostic technique for the evaluation of venous leakage of penile drainage.20 ICI combined with Doppler ultrasound and dynamic infusion of cavernosometry and cavernosography have been the most widely employed methods to evaluate the veno-occlusive function and the arterial flow to the corpus cavernosum. While ICI combined with Doppler ultrasound has had roughly the same diagnostic standard of vasculogenic ED in different reports9, 10,14,21 and has been used as the gold standard,14 the diagnostic standard of venous leakage in cavernosometry varies.3,19,22–26 The maximum normal flow-to-maintain velocity ranges from 3 to 20 ml/min, and the infusion velocity has been reported as 35 ml/min.
Cavernosometry and CT cavernosography procedure
In this study, we took ICI combined with Doppler ultrasound as the gold standard to calculate the diagnostic accuracy of cavernosometry used in our study. The ROC and AUC showed that the flow-to-maintain velocity had a good diagnostic accuracy and that the cut-off was 6 ml/min, which was commensurate with previous research.24, 25 The cut-off of infusion velocity we proposed was 30 ml/min, which was commensurate with one study,26 but the sensitivity and specificity were lower than that of the flow-to-maintain velocity.
In this study, we used EHS to evaluate the intracavernous pressure during cavernosometry and CT cavernosography. When the status of the erection was assessed as 4 under sustained injection velocity, we considered it ready for the examination. Using EHS instead of a direct pressure recording device to evaluate the erection status can simplify the procedure by eliminating the need for a needle that would otherwise need to be inserted in the corpus cavernous to monitor the intracavernous pressure.
Using post-processing (including VR, multiplanar reconstruction, and maximum intensity projection), the venous drainage can be visualized accurately through any angle. Through various angles of rotation, the deep layer of the penile veins, mainly the crural veins, can be visualized clearly, including the venous leakage origin sites and distribution. However, the origin sites of intermediate- and superficial-layer penile veins can hardly be visualized. A large part of the reason is that the intermediate and superficial veins drain many small vein branches. Although the distant veins and the origin sites cannot be identified, the proximal veins can be revealed clearly, which is the most employed operation site. Besides, because the proximal region of penis would often be chosen as the ligation site of dorsal veins to guarantee the effect of the vascular surgery, the invisibility of the sites of leakage of dorsal veins usually won’t influence the validity of vascular surgery.
The penile drainage veins and treatment implication
The penis is drained by three groups of veins,27 including superficial, intermediate and deep. The superficial veins primarily drain penile skin, and they can communicate with the deep dorsal veins. The intermediate veins primarily consist of the deep dorsal vein and prostatic venous plexus. The venous drainage of the penis relies mainly on the deep dorsal vein under the fascia penis. Then, the deep dorsal vein drains to the prostatic venous plexus. The deep veins primarily consist of crural veins, draining the deep cavernous tissue.
Because of the reported low long-term surgical success rate, the 2013 guidelines relegated vascular surgery to a low recommendation status, stating that the criteria of patient selection and operative technique selection are controversial. It was concluded that vascular surgery should be offered in highly select candidates in order to achieve the expected surgical success.
The primary surgical options for venous leakage are ligation of the dorsal veins (both superficial and deep) and its collaterals.28 But the long-term success rate is no greater than 25%.20, 29 The reasons for the low success rate are thought to be the inability to ligate all the defective veins, as small vein branches cannot be observed during surgery and some proximal veins cannot be ligated due to the exposure problem. To correct the haemodynamic pathology more successfully, researchers20, 22,30 have resorted to endovascular embolization of deep dorsal veins and the periprostatic venous plexus6 for patients with isolated deep dorsal vein leakage. However, according to our results, isolated and focal venous leakage is rare in ED, so the candidates for endovascular embolization should be highly selected.
Crural ligation surgery has improved the long-term success rate through the application of strict candidate criteria.3, 4,31 Patients with isolated crural vein leakage can benefit from this surgery. In addition to isolated crural vein leakage, the origin site of the crural vein is also important. The perineal approach is useful only when the crural vein originates from the curs tip. However, the crural vein generally involves a long segment of the crus, and ligation of the crus tip may be inadequate.31
Still, there are reports of long-lasting efficacy in selected cases.5 The validity of the vascular surgery or the endovascular procedure depends on highly select candidates, well-designed procedure plan, and operation technique. According to our results, deep dorsal veins, which were categorized as single- and double-branched, can be ligated by surgery, and the complex type with many small vein branches can be embolized through an endovascular procedure. Considering the origin sites of the crural vein, crural ligation should be employed in patients with the crural vein originating from the crus tip, or else the long-lasting efficacy of crural ligation would be unsatisfactory. Theoretically, simultaneous ligation of dorsal veins and crural veins may lead to better outcomes for patients with mixed type of venous leakage. However, over estimating the potential collaterals between two-layer veins often lead to failure of surgery. CT cavernosography can help to identify the existing tiny collaterals, and reduce the risk of failure of surgery or embolization.
With the development of image technology, especially three-dimensional DSA image fusion technology,32, 33 embolization is now reconsidered as a minimally invasive treatment in our department. Through CT cavernosography and three-dimensional DSA image fusion, which can provide navigation images, penile veins embolization can be more accurate, and operation time can be shorten to reduce radiation dose.
Patients’ age
Most of the young patients in this study had a long course of disease or had a history of ED tracing back to their initial sexual experiences. Most had no trauma history, unsatisfactory erectile rigidity or insufficient sustaining capability. These patients were once considered to have primary ED3 resulting from venous leakage. However, several pathophysiological processes lead to venous leakage as a result of impaired cavernous tissue.34 The impairment or loss of the tunica albuginea veno-occlusive mechanism results from the degeneration and atrophy of collagen and elastic fibres in the tunica albuginea.34, 35
Conclusions
Using EHS to evaluate the intracavernous pressure during cavernosometry can simplify the procedure and eliminate the use of a needle that would otherwise be inserted into the other side of the corpora cavernosum. Through CT cavernosography and VR images, the types of deep dorsal vein and prostatic venous plexus can be distinguished, and the origin of the crural vein can be identified. To achieve a long satisfaction time, surgical ligation and endovascular embolization should be chosen for relatively simple types of penile veins, and crus ligation should be engaged only when the crural vein originates from the crus tip.
The validity of vascular surgery and embolization based on our theory and plan has not been validated yet. The validation has been carried out, and the result will be published in the future.
Footnotes
Acknowledgements: We wish to thank Dr Zhaohui Zhu for his illustration of this study, Ms Xi Yao for her preparation of the procedures.
Contributor Information
Tianhe Ye, Email: tianhe-ye@outlook.com.
Jun Li, Email: 1012784420@qq.com.
Lingli Li, Email: 18734896722@163.com.
Lian Yang, Email: yanglian2003@163.com.
REFERENCES
- 1. Elhanbly S, Abdel-Gaber S, Fathy H, El-Bayoumi Y, Wald M, Niederberger CS. Erectile dysfunction in smokers: a penile dynamic and vascular study. J Androl 2004; 25: 991–5. doi: 10.1002/j.1939-4640.2004.tb03172.x [DOI] [PubMed] [Google Scholar]
- 2. Aschenbach R, Steiner T, Kerl MJ, Zangos S, Basche S, Vogl TJ. Endovascular embolisation therapy in men with erectile impotence due to veno-occlusive dysfunction. Eur J Radiol 2013; 82: 504–7. doi: 10.1016/j.ejrad.2012.10.030 [DOI] [PubMed] [Google Scholar]
- 3. Flores S, Tal R, O'Brien K, Mulhall JP. Outcomes of crural ligation surgery for isolated crural venous leak. J Sex Med 2011; 8: 3495–9. doi: 10.1111/j.1743-6109.2011.02315.x [DOI] [PubMed] [Google Scholar]
- 4. Cayan S. Primary penile venous leakage surgery with crural ligation in men with erectile dysfunction. J Urol 2008; 180: 1056–9. doi: 10.1016/j.juro.2008.05.024 [DOI] [PubMed] [Google Scholar]
- 5. Shaeer O, Shaeer K. Same-session dorsal vein ligation and testing by intracavernous injection prior to penile prosthesis implantation (DVL-ICI-PPI). J Sex Med 2014; 11: 2333–7. doi: 10.1111/jsm.12582 [DOI] [PubMed] [Google Scholar]
- 6. Rebonato A, Auci A, Sanguinetti F, Maiettini D, Rossi M, Brunese L, et al. Embolization of the periprostatic venous plexus for erectile dysfunction resulting from venous leakage. J Vasc Interv Radiol 2014; 25: 866–72. doi: 10.1016/j.jvir.2014.01.015 [DOI] [PubMed] [Google Scholar]
- 7. Rhoden EL, Telöken C, Sogari PR, Vargas Souto CA, Vargas SC. The use of the simplified International Index of Erectile Function (IIEF-5) as a diagnostic tool to study the prevalence of erectile dysfunction. Int J Impot Res 2002; 14: 245–50. doi: 10.1038/sj.ijir.3900859 [DOI] [PubMed] [Google Scholar]
- 8. Wasserman MD, Pollak CP, Spielman AJ, Weitzman ED. The differential diagnosis of impotence. The measurement of nocturnal penile tumescence. JAMA 1980; 243: 2038–42. [PubMed] [Google Scholar]
- 9. Quam JP, King BF, James EM, Lewis RW, Brakke DM, Ilstrup DM, et al. Duplex and color Doppler sonographic evaluation of vasculogenic impotence. AJR Am J Roentgenol 1989; 153: 1141–7. doi: 10.2214/ajr.153.6.1141 [DOI] [PubMed] [Google Scholar]
- 10. Lue TF, Hricak H, Marich KW, Tanagho EA. Vasculogenic impotence evaluated by high-resolution ultrasonography and pulsed Doppler spectrum analysis. Radiology 1985; 155: 777–81. doi: 10.1148/radiology.155.3.3890009 [DOI] [PubMed] [Google Scholar]
- 11. Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol 2010; 57: 804–14. doi: 10.1016/j.eururo.2010.02.020 [DOI] [PubMed] [Google Scholar]
- 12. Goldstein I, Mulhall JP, Bushmakin AG, Cappelleri JC, Hvidsten K, Symonds T. The erection hardness score and its relationship to successful sexual intercourse. J Sex Med 2008; 5: 2374–80. doi: 10.1111/j.1743-6109.2008.00910.x [DOI] [PubMed] [Google Scholar]
- 13. Mulhall JP, Goldstein I, Bushmakin AG, Cappelleri JC, Hvidsten K. Validation of the erection hardness score. J Sex Med 2007; 4: 1626–34. doi: 10.1111/j.1743-6109.2007.00600.x [DOI] [PubMed] [Google Scholar]
- 14. Arslan D, Esen AA, Seçil M, Aslan G, Celebi I, Dicle O. A new method for the evaluation of erectile dysfunction: sildenafil plus Doppler ultrasonography. J Urol 2001; 166: 181–4. doi: 10.1016/S0022-5347(05)66105-8 [DOI] [PubMed] [Google Scholar]
- 15. Gratzke C, Angulo J, Chitaley K, Dai YT, Kim NN, Paick JS, et al. Anatomy, physiology, and pathophysiology of erectile dysfunction. J Sex Med 2010; 7: 445–75. doi: 10.1111/j.1743-6109.2009.01624.x [DOI] [PubMed] [Google Scholar]
- 16. Kaminetsky J. Epidemiology and pathophysiology of male sexual dysfunction. Int J Impot Res 2008; 20(Suppl 1): S3–S10. doi: 10.1038/ijir.2008.16 [DOI] [PubMed] [Google Scholar]
- 17. Rajfer J, Rosciszewski A, Mehringer M. Prevalence of corporeal venous leakage in impotent men. J Urol 1988; 140: 69–71. doi: 10.1016/S0022-5347(17)41489-3 [DOI] [PubMed] [Google Scholar]
- 18. Wespes E, Amar E, Hatzichristou D, Hatzimouratidis K, Montorsi F, Pryor J, et al. EAU guidelines on erectile dysfunction: an update. Eur Urol 2006; 49: 806–15. doi: 10.1016/j.eururo.2006.01.028 [DOI] [PubMed] [Google Scholar]
- 19. Glina S, Ghanem H. SOP: corpus cavernosum assessment (cavernosography/cavernosometry). J Sex Med 2013; 10: 111–4. doi: 10.1111/j.1743-6109.2012.02795.x [DOI] [PubMed] [Google Scholar]
- 20. Aschenbach R, Steiner T, Kerl MJ, Zangos S, Basche S, Vogl TJ. Endovascular embolisation therapy in men with erectile impotence due to veno-occlusive dysfunction. Eur J Radiol 2013; 82: 504–7. doi: 10.1016/j.ejrad.2012.10.030 [DOI] [PubMed] [Google Scholar]
- 21. Cohen SD. The challenge of erectile dysfunction management in the young man. Curr Urol Rep 2015; 16: 84. doi: 10.1007/s11934-015-0553-3 [DOI] [PubMed] [Google Scholar]
- 22. Miwa Y, Shioyama R, Itou Y, Kanamaru H, Okada K. Pelvic venoablation with ethanol for the treatment of erectile dysfunction due to veno-occlusive dysfunction. Urology 2001; 58: 76–9. doi: 10.1016/S0090-4295(01)01013-5 [DOI] [PubMed] [Google Scholar]
- 23. Kawanishi Y, Izumi K, Muguruma H, Mashima T, Komori M, Yamanaka M, et al. Three-dimensional CT cavernosography: reconsidering venous ligation surgery on the basis of the modern technology. BJU Int 2011; 107: 1442–6. doi: 10.1111/j.1464-410X.2010.09644.x [DOI] [PubMed] [Google Scholar]
- 24. Spiliopoulos S, Shaida N, Katsanos K, Krokidis M. The role of interventional radiology in the diagnosis and management of male impotence. Cardiovasc Intervent Radiol 2013; 36: 1204–12. doi: 10.1007/s00270-012-0520-z [DOI] [PubMed] [Google Scholar]
- 25. Kaufman JM, Borges FD, Fitch WP, Geller RA, Gruber MB, Hubbard JG, et al. Evaluation of erectile dysfunction by dynamic infusion cavernosometry and cavernosography (DICC). Multi-institutional study. Urology 1993; 41: 445–51. doi: 10.1016/0090-4295(93)90505-5 [DOI] [PubMed] [Google Scholar]
- 26. Kurbatov DG, Kuznetsky YY, Kitaev SV, Brusensky VA. Magnetic resonance imaging as a potential tool for objective visualization of venous leakage in patients with veno-occlusive erectile dysfunction. Int J Impot Res 2008; 20: 192–8. doi: 10.1038/sj.ijir.3901607 [DOI] [PubMed] [Google Scholar]
- 27. Hsu GL. Hypothesis of human penile anatomy, erection hemodynamics and their clinical applications. Asian J Androl 2006; 8: 225–34. doi: 10.1111/j.1745-7262.2006.00108.x [DOI] [PubMed] [Google Scholar]
- 28. Katzenwadel A, Popken G, Wetterauer U. Penile venous surgery for cavernosal venous leakage: long-term results and retrospective studies. Urol Int 1993; 50: 71–6. doi: 10.1159/000282455 [DOI] [PubMed] [Google Scholar]
- 29. Da Ros CT, Telöken C, Antonini CC, Sogari PR, Souto CA. Long-term results of penile vein ligation for erectile dysfunction due to cavernovenous disease. Tech Urol 2000; 6: 172–4. [PubMed] [Google Scholar]
- 30. Peşkircioğlu L, Tekin I, Boyvat F, Karabulut A, Ozkardeş H. Embolization of the deep dorsal vein for the treatment of erectile impotence due to veno-occlusive dysfunction. J Urol 2000; 163: 472–5. doi: 10.1016/S0022-5347(05)67904-9 [DOI] [PubMed] [Google Scholar]
- 31. Rahman NU, Dean RC, Carrion R, Bochinski D, Lue TF. Crural ligation for primary erectile dysfunction: a case series. J Urol 2005; 173: 2064–6. doi: 10.1097/01.ju.0000158447.12163.f5 [DOI] [PubMed] [Google Scholar]
- 32. Koutouzi G, Sandström C, Roos H, Henrikson O, Leonhardt H, Falkenberg M. Orthogonal rings, fiducial markers, and overlay accuracy when image fusion is used for EVAR guidance. Eur J Vasc Endovasc Surg 2016; 52: 604–11. doi: 10.1016/j.ejvs.2016.07.024 [DOI] [PubMed] [Google Scholar]
- 33. Zhang Q, Zhang Z, Yang J, Sun Q, Luo Y, Shan T, et al. CBCT-based 3D MRA and angiographic image fusion and MRA image navigation for neuro interventions. Medicine 2016; 95: e4358. doi: 10.1097/MD.0000000000004358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. El-Sibai O, Shafik AA, Shafik IA. Tunica albuginea reefing: a novel technique for the treatment of erectile dysfunction. J Invest Surg 2011; 24: 44–8. doi: 10.3109/08941939.2010.526682 [DOI] [PubMed] [Google Scholar]
- 35. Shafik A, Shafik I, El Sibai O, Shafik AA. Tunica albuginea overlapping: a novel technique for the treatment of erectile dysfunction. Andrologia 2005; 37: 180–4. doi: 10.1111/j.1439-0272.2005.00678.x [DOI] [PubMed] [Google Scholar]