Abstract
Objective:
Skill mix has been established as one method of maintaining imaging service delivery, with vertical and horizontal substitution of roles and tasks. Assistant practitioners (APs) have been undertaking limited imaging practice for almost two decades, but there remains a paucity of evidence related to the impact of their roles.
Methods:
This article reports on an electronic survey of individual APs within the NHS in the UK to explore utilisation, role scope and aspirations.
Results:
Responses were analysed from APs (n = 193) employed in 97 different organisations across the UK. The majority work in general radiography or mammography, with very few responses from other imaging modalities. Training routes varied across modalities, with most achieving Band 4 under Agenda for Change on completion of education. Limitations on practice vary between organisations and modalities, with many reporting blurring of the radiographer-AP boundary. Many aspire to continue their training to achieve registrant radiographer status, although there were clear frustrations from respondents over the lack of overt career prospects.
Conclusion:
Integration of the role into imaging department practice does not appear to be universal or consistent and further research is required to examine the optimal skill mix composition.
Advances in knowledge:
Skill mix implementation is inconsistent across modalities and geography in the UK. Opportunities for further workforce utilisation and expansion are evident.
Introduction
Demand for health services, including diagnostic imaging, continue to grow across the developed world.1 Complex cross-sectional modalities such as CT and MRI have seen double digit percentage rises over the last few years, but expansion of breast screening programmes and maintenance of small rises in high volume general radiographs have created a perfect storm.2–4 Imaging workforce expansion has failed to respond to this increased clinical demand, resulting in delays related in both acquisition and reporting.2, 5 Collaborative service models have been introduced to manage workload, blurring professional boundaries and clinical tasks across the radiology and radiography professions.5, 6 Skill mix has become a part of the international health landscape, with vertical and horizontal substitution of roles common across health professions.7–10 In diagnostic imaging, the last two decades has seen incremental expansion of the radiographer role with individuals taking on activities previously performed by a medical radiologist.11–13 Vertical substitution also relates to tasks being delegated to others outside of the registered workforce with auxiliary staff training to acquire high-quality images and directly support service users through their diagnostic imaging journey. Examples include clinical support worker and assistant practitioner (AP) roles in the UK and limited X-ray machine operator (LXMO) in the USA.14, 15 To ensure that imaging services are safe, efficient, and ensure patient satisfaction, there is a need to grow the workforce and fully utilise skills at all levels of practice, however, it is currently unknown as to whether this is being achieved at the AP tier.
Within the UK, the AP role was introduced as part of the national skill mix strategy published in 2003, designed to invigorate a career structure, improve staffing levels and deliver high quality care.13 The AP is the first of the four-tiers, established to perform protocol-limited tasks under the direction and supervision of a state-registered practitioner. The NHS Career Framework16 set out a formal progression route to support the needs of local service demands and patients. This enables individuals to enter at any point on the framework appropriate to their level of qualification and experience and then through additional training and experiential learning develop their role.17 Task delegation to APs was importantly seen as a means of enabling registered radiographers to extend their scope of practice into advanced and consultant roles, releasing their time and capacity for additional responsibilities.17, 18 To date, the AP role remains unregulated but voluntary accreditation is provided by the professional body, the Society and College of Radiographers (SCoR).19
In the 15 years since the pilot projects initially tested the four-tier model, there remains a lack of research evidence of the impact of restructuring the career pathway,20–22 in particular confirmation of capacity creation. This article reports on a national survey examining the AP role in the context of UK imaging practice and follows on from one recently published regarding AP post holders in general radiography.23 The outcomes of this study will also have relevance to all countries with, or considering, such roles.
Methods and Materials
An electronic cross-sectional survey was developed to explore the utilisation of APs in UK diagnostic imaging departments, with a particular focus on consensus or variation in roles. Such surveys provide information about a specific population at a given point in time, particularly personal experience, beliefs, or opinions and have been used in healthcare to determine organisational characteristics such as structure, workforce and activity.24 Importantly, this survey was designed to be completed at the individual level rather than organisational level, so as to consider variation across imaging modalities.
The electronic survey was developed using the Bristol Online Survey tool (Bristol Online Survey®, Bristol, UK) and included a combination of closed and open-ended questions, which provided respondents the opportunity to provide a greater depth of information where appropriate and reduced the potential for researcher bias. Designed to be completed by qualified or trainee APs, questionnaire content was developed by a mixed role team and intentionally comprised questions relating to the scope of practice (including caveats and boundaries), as well as supplementary responsibilities of the AP workforce providing diagnostic imaging services. The initial survey tool was piloted using APs and modality specialist radiographers to ensure accuracy of comprehension, ease of completion and question relevance. This resulted in minor refinement of question phrasing.
There is no known current knowledge of UK AP roles or formal database of numbers in practice, beyond the voluntary register. To capture as many APs as possible, a snowball approach to sampling was applied. A letter of invitation to participate, including a short paragraph on ethical considerations; eligibility criteria; study team contacts and a link to the electronic survey, was distributed to all UK NHS Trusts and Health Boards identified from national hospitals databases. The initial hard copy invitation was posted for the attention of the radiology manager at the primary hospital site for each Trust. They were informed of the purpose of the survey and requested to share the study participant information sheet with all AP colleagues across their organisation. Participation in the survey was voluntary and consent was implied by completion of the online survey. Completion of the UK Health Research Authority checklist confirmed that ethical approval was not required in this case.
The survey requested the name of the Trust to be provided to enable geographical analysis, otherwise all data were collected anonymously. Although there are a number of independent sector providers of imaging services and these were excluded from this survey which focussed on NHS skills mix. To minimise response bias and avoid unnecessary correspondence, sites that did not employ APs were asked to email the lead author.
The survey ran from August to October 2017, to maximise responses a reminder letter was distributed specifically addressed to APs at the lead hospital site of each organisation (excluding those who had notified the researchers that they did not employ APs) and also to breast screening units, as these may operate outside of traditional hospital structures. To facilitate engagement, the survey was also promoted by the SCoR through their website, magazine and social media. Following survey closure, the site response data were anonymised and no identifiable information is reported. To ensure accuracy of results responses from therapy and nurse APs have been omitted from the analysis during data validation, with only those undertaking diagnostic imaging included. The response data were downloaded into Microsoft Excel (Microsoft vCorporation, Redmond, WA) for analysis and presentation of descriptive and free text findings. Further statistical analysis was undertaken using the freely available online Social Science Statistics calculator (www.socscistatistics.com).
Non-response bias in survey research can result in misleading or inaccurate findings and identification of variables that predict bias is encouraged to understand the representativeness of findings.24–26 Response bias was assessed through analysis of early (within the first week) and late (within the last week) responders answers to key questions on geography (England compared to other home countries); gender; modality; and aspirations to develop as to Health and Care Professions Council (HCPC) registered radiographer status. These characteristics were considered potentially influential in response motivation. For this, χ2 tests were used and a p-value < 0.05 was considered statistically significant.
Results
A total of 197 responses were received within the timeframe, of which 4 were subsequently excluded as they represented practice outside the scope of the survey, leaving 193 for further analysis. In addition, nine NHS Trusts responded to state they did not employ APs in diagnostic imaging, although they were employed by two local breast screening units, which was operationally managed by one of these Trusts.
Analysis of the early (n = 35) and late (n = 27) responses demonstrated non-response bias only in relation to modality with a greater proportion of general radiography respondents in the early wave compared to mammography in the late group (general radiography 80.0 vs 25.9%; mammography 8.6 vs 63.0%; p ≤ 0.001). There was no significant difference in responses to questions on geography (England 74.3 vs 92.6%; p = 0.061), gender (female 82.6 vs 96.3%; p = 0.973) or aspiration to progress as a radiographer (48.6 vs 44.4%; p = 0.747).
Geography
There were responses from all four UK home countries, although the number of respondents, and organisations, varied geographically (Table 1). Subanalysis by English regions also demonstrated disparity in response numbers.
Table 1.
Geographical distribution of survey responses
| Country (and English region) | Individual responses n (%) | Unique Trusts/Health Boards n (%) |
| England | 153 (79.3) | 75 (77.3) |
| East Midlands | 9 | 5 |
| East of England | 10 | 7 |
| London | 8 | 7 |
| North East | 17 | 3 |
| North West | 22 | 13 |
| South East | 17 | 10 |
| South West | 20 | 11 |
| West Midlands | 18 | 8 |
| Yorkshire & Humber | 32 | 11 |
| Northern Ireland | 8 (4.1) | 4 (4.1) |
| Scotland | 19 (9.8) | 11 (11.3) |
| Wales | 13 (6.7) | 7 (7.2) |
| Total | 193 | 97 |
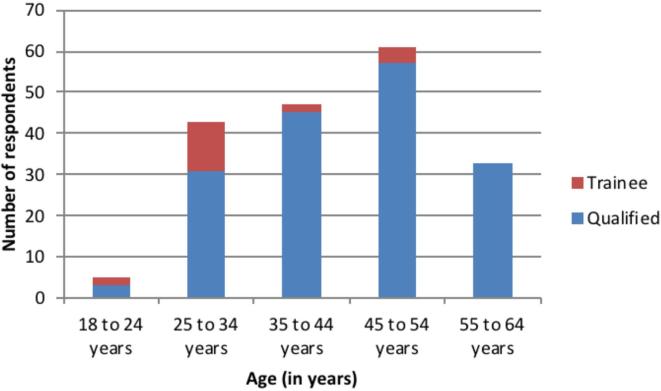
APs are predominately female (87.5%; n = 168/192), with the majority working full time (60.6%; n = 117/193). Two respondents confirmed they were employed as an AP part-time whilst undertaking a full-time degree in radiography. The age range was broad (Figure 1), with trainees comprising just 11.4% of the respondents.
Figure 1.
Age of respondent trainee and qualified assistant radiographer practitioners.
Qualification, modality of practice and pay banding
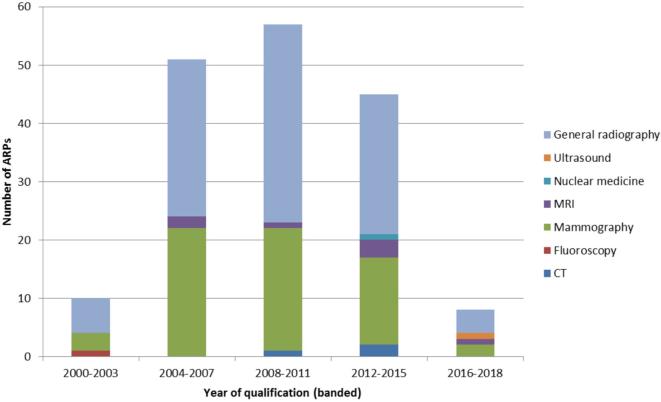
From those who responded, the workforce numbers saw greatest growth between 2008 and 2011 (Figure 2), with the majority of APs qualifying in 2009 (n = 20).
Figure 2.
Year of qualification of respondent assistant practitioners. ARP,assistant radiographer practitioners.
The practice bases represented were related to the typical imaging modalities. Over 90% of respondents are primarily employed in the general radiography or mammography settings (Table 2), with few training in other modalities over the last two decades (Figure 2). Of the 108 based in general radiography, 27 also stated they worked as an AP in another area, most commonly in fluoroscopy (n = 12) or bone densitometry (n = 12), although others across the modalities confirmed that they provide cover in different clinical areas as a support worker, as required.
Table 2.
Assistant practitioner modality or speciality base
| Speciality | Trainee | Qualified | Total (%) |
| CT | – | 3 | 3 (1.6) |
| Fluoroscopy | – | 1 | 1 (0.5) |
| Mammography | 8 | 63 | 71 (36.8) |
| MRI | 1 | 7 | 8 (4.1) |
| Nuclear medicine | – | 1 | 1 (0.5) |
| Ultrasound | – | 1 | 1 (0.5) |
| General radiography | 13 | 95 | 108 (56.0) |
| Total | 22 | 171 | 193 |
Almost all qualified APs were employed at Agenda for Change (AfC) Band 4 (95.9%; n = 164/171). The remaining seven work within mammography at five different NHS Trusts/organisations and are either paid at, or are under consideration for progression to, Band 5. In relation to APs in training, most are employed at AfC Band 3 (45.4%; n = 10/22), with equal numbers paid Band 2 or Band 4 (22.7%; n = 5/22), the remaining two described Annex U arrangements under AfC.
Training
No single education programme was evident, although the Foundation Degree and Certificate of Higher Education were the most commonly reported (Table 3). The other examples cited included in-house training supported by academic attendance (but specific course not detailed) and Postgraduate Diploma (nuclear medicine).
Table 3.
Training route taken by assistant radiographer practitioners
| Training route | CT | Fluoroscopy | Mammography | MRI | Nuclear medicine | Ultrasound | General radiography | Total (%) |
| Foundation Degree | 2 | – | 16 | 3 | – | 1 | 35 | 57 (29.5) |
| Certificate of Higher Education | 1 | – | 22 | 3 | – | – | 27 | 53 (27.5) |
| Diploma of Higher Education | – | 1 | 3 | 1 | – | – | 14 | 21 (10.9) |
| Completed part of undergraduate radiography course a | – | – | 1 | – | – | – | 16 | 17 (8.8) |
| Higher National Certificate (Scotland) | – | – | 3 | – | – | – | 11 | 14 (7.3) |
| In-house training only | – | – | 11 | – | – | – | 2 | 14 (7.3) |
| NVQ level 3 | – | – | 8 | – | – | – | – | 8 (4.1) |
| Btec Higher Diploma | – | – | 1 | – | – | – | 1 | 2 (1.0) |
| City and Guilds | – | – | 5 | – | – | – | – | 1 (0.5) |
| Other | – | – | 2 | – | 1 | – | 2 | 8 (4.1) |
| Total | 3 | 1 | 71 | 7 | 1 | 1 | 108 | 193 |
Educational level not stated but likely to be either Certificate or Diploma of Higher Education.
Scope of practice
The scope of practice varies across modalities and geography, and includes limitations based on patient age, referral groups and specialised or supplementary examinations (Table 4). Additional AP Trust roles included manual handling, fire safety, infection control, patient liaison and work as a freedom to speak champion. Many APs reported flexibility in their duties, describing undertaking imaging assistant, housekeeping, stock control and coordinator roles within their daily practice.
Table 4.
Reported scope of practice across modalities
| Modality | Common examination scope | Identified limitations on practice a | Other non-image acquisition activities |
| CT | |||
| Fluoroscopy | |||
| Mammography | |||
| MRI | |||
| NM | |||
| Ultrasound | |||
| General Radiography |
NM, nuclear medicine.
Self-reported and not universal or verified.
There was inconsistency in the level of supervision described by APs, most general radiography and mammography APs confirmed that a radiographer was always available for support and advice, although they were not necessarily in the same room. This was illustrated by one mammography AP who stated that having a radiographer in the room “would be pointless, the radiographer might as well do the exam herself”. In contrast, those working in cross-sectional modalities (CT and MRI) and nuclear medicine confirmed that a radiographer was always present in the control room. The process for justification of examinations was also seen to vary across modalities, with those in high radiation-dose areas (CT and nuclear medicine) always being reviewed by a registered radiographer prior to the examination commencing, though this was not standard in other areas. There also appears to be a lack of clarity across modalities regarding AP autonomy and clinical decision making processes. In MRI, responsibility for patient safety procedures has been delegated to some APs, with one confirming that their role included “going through safety questionnaire” whereas another stated that the “safety questionnaires [are] checked by radiographer.” The differences in practice between screening and symptomatic breast imaging were also highlighted by one individual: “A qualified radiographer has to justify, check and sign all symptomatic mammograms but not screening.”
There is evidence that APs are potentially undertaking activities outside of the legal framework of the unregistered practitioner role. The fluoroscopy AP and two (of the three) working in CT described dispensing oral contrast. Additionally, intravenous contrast is also being administered by APs in CT, but only when a radiographer is present. In comparison, none of the respondents working in MRI, mammography or nuclear medicine were administering medications. Further, one individual based in nuclear medicine, employed as an AP whilst undertaking postgraduate training stated “until my post grad diploma training is completed I am unable to dispense and inject radioisotope. I am unable to label white cells and administer medication under PGDs.”
Aspirations and frustrations
Just over half of the qualified APs confirmed membership of the Society of Radiographers (53.2%; n = 91/171), although only 45.0% indicated that they have voluntary accreditation (n = 77/171). The main reasons given related to a lack of perceived benefit, it not being compulsory and cost, for example “I have been [accredited] but found it to no advantage to my job” and “I was accredited but have not renewed as I feel very unmotivated as my CPD repeats every year with no professional development” (AP Mammography). Some suggested that they were considering application, although a small number were unaware of the option. One AP based in mammography did suggest that the “register should be mandatory and afforded the respect that registration entails.”
Challenges to the AP role were evident, with a perceived change in professional body support quoted as the rationale for the cessation of activities “there is no place for assistant practitioners doing CT brain scans and we are no longer protected by the Society of Radiographers.” Additionally, a lack of radiographer support for the AP role was perceived as a block to opportunities: “used in the pool of assistants mainly, only certain members of staff will offer me the option to scan. Tried to push department to utilise our skills but will be moved into the main department pending consultation” (AP MRI).
A proportion of survey participants indicated they would like to progress in radiography (45.1%; n = 87/193). The main stumbling blocks were cited as funding and course availability. The potential for an apprenticeship route was identified by some, with many others describing the same principles, e.g.: “I am waiting for a way of qualifying without leaving work and going back to university” (AP general radiography), “If there was a way that it could be done within my workplace whilst still being employed” (AP mammography). However, the requirement to develop in the wider imaging setting also appears to be off-putting, with many suggesting that if there was the opportunity to remain working in their sub speciality (e.g. mammography or MRI), they may be interested.
“My interest and vast experience is within breast. I do not want to become a radiographer as I have no interest in general radiography.” (AP mammography)
“To become qualified currently I would need to undertake 4 further years study to do the same job I am doing now, however I wouldn't need to be supervised. If there was a 'bridge the gap' course to become a Radiographer in Mammography then yes I would be interested in doing it.” (AP mammography)
“if funded and for MRI only” (AP MRI)
The responses demonstrate inconsistency in the implementation of the remainder of the four-tier structure, with over two thirds of sites employing advanced practitioners in the relevant modality/speciality groups (68.0%; n = 102/150). A greater proportion of consultant practitioner roles were seen in mammography compared to general radiography (57.8% vs 22.7%; Z = 3.757; p ≤ 0.001).
Overall, many APs felt their role was appreciated by those around them, but the lack of career prospects was a major influence on their job satisfaction. The number of free text comments on completion of the survey (n = 100) appears to reflect the strength of feeling, and although some relished the role, progression was a major issue: “It is the best thing I did re training for this position love my job but do wish there was a chance for further development and to enhance my job satisfaction” (AP mammography).
Others failed to see how the role differs from that of a radiographer:
“I feel our role covers the same jobs as a radiographer within my department.” (AP mammography).
“I can consider myself as a qualified radiographer due to the nature of my role within our department. It's just a qualification I need to do so I can be part of HCPC. (AP CT)
Importantly, the lack of role clarity and absence of a career framework was seen as a major source of frustration:
“I feel that after 9 years of experience AP's have little or no chance of career progression, unless you side step into management, and I personally feel, under appreciated for what we do, also stuck we have nowhere to go!!!” (AP general radiography)
“The role of AP can be quite a lonely one. You are neither one thing or another. The title is misleading as you don't 'assist', you 'do'!” (AP mammography)
Discussion
Unlike state registered practitioners, there is currently no national record of APs working within UK imaging departments; therefore, the actual response rate for this survey of practice cannot be ascertained. The SCoR states there are 257 accredited APs on their register (personal communication, L Coleman), although accreditation is voluntary and is not sought by all APs, as reflected by the responses received in this study. Overall, there was no evidence of non-response bias, other than increasing mammography respondents by target mailing breast screening units during the reminder phase. Therefore, if the proportion of accredited APs remains similar it is feasible to suggest that there are in excess of 570 APs. Comparison with previous research is difficult as this survey was targeted at an individual level, but geographical expansion of the role is evident.27
This study has highlighted inconsistency in the development of AP roles across imaging modalities. This may be because the common pay grade for registrants to practice in some modalities is Band 6, although other factors, such as professional indemnity, education programme and local preferences also appear to be contributing. Although internationally, the registered radiographer role is similar,28, 29 training for the limited scope practitioner role varies. In the USA, education for the limited X-ray machine operator varies from 6 weeks to 9 months with the scope varying between states.14, 30 The role has evolved as nurses, assistants and office personnel have been trained to provide limited aspects of general radiography or bone densitometry primarily, but not exclusively, in clinics and physicians’ offices. Unlike the UK, these roles are both examined and certified by the regulatory body. In Australia, limited operators are registered healthcare professionals (predominantly nurses and doctors), who have restricted training in limited general radiography examinations for the remote and rural setting.31, 32 When these differences are considered the key appears to be that in the UK, the AP role exists across most modalities/specialities as the role is to work alongside rather than in replacement of a registered radiographer.32 This may now be the underlying cause of the problem, and frustrations, regarding implementation and career progression. It may, however serve as a lesson to the international radiography community in any future development of such roles.
Job satisfaction echoes the findings of Miller et al,33 although the major difference in current research is the increased numbers wanting to progress to radiographer status. AP training routes were seen to vary across imaging modalities, consistent with other reviews of AP curricula.15,33–36 Such variation appears to be inhibiting some from academic and career progression and this is likely to only be exacerbated by the development of Higher Level and Degree apprenticeships. Whether the new apprenticeships will have any influence on career progression opportunities for APs is as yet unclear.
The scope of practice and level of supervision appears to vary significantly depending on the modality and organisation in which they are employed. This is strikingly evident in the supply and administration of medicines, such as contrast agents, by APs, who may have a supporting role in venous cannulation and medication administration. Realistically, standards for medicines management are not always conducive to an efficient department at an organisational level. As a result, there is opportunity for local delegation, training, education and competencies to be established for APs undertaking these tasks.37–39 Assistants are not permitted by law to use patient group directives,18, 37 however, the reported restrictions to the performance of some imaging procedures is unfounded.
Internationally, health sector growth continues and the push for advanced (and consultant) practice to help meet this demand is supported in the UK by career development frameworks.7 Evidence of extended roles in radiography is strong,9, 40 however, to balance the workload and budgets, this requires a suitably qualified AP workforce with an appropriate level of training and expertise to backfill these roles and take on delegated tasks. When the skills mix project was introduced, there was a clear rationale for the need to reform career structures in response to a national shortage of staff and expansion of cancer services to meet population needs. The career pathways were envisaged as a way of recruiting and retaining highly-skilled and engaged staff and improving the quality and efficiency of diagnostic imaging provision within patient care pathways.13 This survey has demonstrated a potential disconnect between the aims and aspirations of the skills mix project and the real world. The tasks performed by radiographers and APs have become a “grey area” with boundaries blurring, exacerbated by locally increased scopes of practice of some APs. However, the counter argument has been presented that the performance of limited delegated tasks does not enable service flexibility and it may be preferential to recruit registered radiographers over APs.41
Similar to previous research many saw value in the AP role,33 but this study reinforces an underlying disquiet linked to overlapping professional and task boundaries and a lack of overt career opportunities. A number of APs are undertaking activities more aligned to operational management than clinical service delivery. Whether this is as an opportunity for personal development or driven by a need for flexibility in the service, it is not clear. The establishment of role scope does not appear to be a standardised process, evidenced by the geographical and modality variation found in this study. Delegation and role substitution may not be accepted uniformly, confirming previous work exploring theoretical models of professional practice boundaries8, 36,42 and the “negotiated compromise” of Spilsbury et al.43Further research is required to explore the optimal integration and ongoing management of skills mix within diagnostic imaging, but also current legislation, education and barriers to this.
Conclusion
The intention of workforce redesign and the introduction of the AP tier in the four-tier structure, was to ease the staff shortages faced within diagnostic imaging and facilitate efficient service delivery. It was also seen as a way of enabling staff progression and while registered staff have populated the higher tiers, this largely remains in general radiography and mammography. Importantly, APs do not perceive a clear connection from the first tier to higher level of the career framework through personal and professional development. This lack of overt pathways to radiographer status, and beyond, is leading to frustration amongst this important element of the workforce.
REFERENCES
- 1. Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, et al. Evidence for overuse of medical services around the world. Lancet 2017; 390: 156–68. doi: 10.1016/S0140-6736(16)32585-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cake R, Cavanagh P, Gordon B. Horizon Scanning: An evaluation of imaging capacity across the NHS in England. Cancer Research UK; 2015. [Google Scholar]
- 3. Royal College of Radiologists. Radiology in the UK- the case for a new service model. London: The British Institute of Radiology.; 2014. [Google Scholar]
- 4. Smith-Bindman R, Miglioretti DL, Johnson E, Lee C, Feigelson HS, Flynn M, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA 2012; 307: 2400–9. doi: 10.1001/jama.2012.5960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maskell G. The demand for radiology services. British Journal of Healthcare Management 2015; 21: 110–1. doi: 10.12968/bjhc.2015.21.3.110 [DOI] [Google Scholar]
- 6. Royal College of Radiologists. Clinical radiology UK workforce census report 2016 report. London: The British Institute of Radiology.; 2017. [Google Scholar]
- 7. Health Education England. Multi-professional framework for advanced clinical practice in England. London: The British Institute of Radiology.; 2017. [Google Scholar]
- 8. Traynor M, Nissen N, Lincoln C, Buus N. Occupational closure in nursing work reconsidered: UK health care support workers and assistant practitioners: A focus group study. Soc Sci Med 2015; 136-137: 81–8. doi: 10.1016/j.socscimed.2015.05.020 [DOI] [PubMed] [Google Scholar]
- 9. Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Sociol Health Illn 2005; 27: 897–919. doi: 10.1111/j.1467-9566.2005.00463.x [DOI] [PubMed] [Google Scholar]
- 10. Buchan J, Dal Poz MR. Skill mix in the health care workforce: reviewing the evidence. Bull World Health Organ 2002; 80: 575–80. [PMC free article] [PubMed] [Google Scholar]
- 11. Ten Napel TL, Sanders VL, Wright DL. Radiologist assistant: best fit for medical imaging. Radiol Manage 2014; 36: 22–7. [PubMed] [Google Scholar]
- 12. Hardy M, Legg J, Smith T, Ween B, Williams I, Motto J. The concept of advanced radiographic practice: An international perspective. Radiography 2008; 14(Supp 1): e15–e19. doi: 10.1016/j.radi.2008.10.001 [DOI] [Google Scholar]
- 13. Department of Health. Radiography Skills Mix: A report on the four-tier service delivery model. London: The British Institute of Radiology.; 2003. [Google Scholar]
- 14. Long BW, Frank ED, Ehrlich RA. Radiography essentials for limited practice. Missouri: The British Institute of Radiology.; 2017. –p6. [Google Scholar]
- 15. Winnard Y, Kittle S. Assistant practitioners in radiography. British Journal of Healthcare Assistants 2008; 2: 42–4. doi: 10.12968/bjha.2008.2.1.28017 [DOI] [Google Scholar]
- 16. Skills for Health. Key elements of the Career Framework. London: The British Institute of Radiology.; 2010a. [Google Scholar]
- 17. Skills for Health. The role of assistant practitioners in the NHS: factors affecting evolution and development of the role. Skills for Health expert paper. London: The British Institute of Radiology.; 2011. [Google Scholar]
- 18. Society of Radiographers. Scope of Practice of Assistant Practitioners. London: The British Institute of Radiology.; 2012. [Google Scholar]
- 19. Society of Radiographers Assistant practitioner accreditation. 2018;.
- 20. Henderson I, Mathers SA, McConnell J. Advanced and extended scope practice of diagnostic radiographers in Scotland: Exploring strategic imaging service imperatives. Radiography 2017; 23: 181–6. doi: 10.1016/j.radi.2017.02.009 [DOI] [PubMed] [Google Scholar]
- 21. Hardy M, Johnson L, Sharples R, Boynes S, Irving D. Does radiography advanced practice improve patient outcomes and health service quality? A systematic review. Br J Radiol 2016; 89: 20151066. doi: 10.1259/bjr.20151066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Price R, Miller L, Hicks B, Higgs A. The introduction, deployment and impact of assistant practitioners in diagnostic radiography in Scotland. Radiography 2015; 21: 141–5. doi: 10.1016/j.radi.2014.08.003 [DOI] [Google Scholar]
- 23. Palmer D, Snaith B, Harris MA. Assistant radiographer practitioners: Creating capacity or challenging professional boundaries? Radiography 2018; 24: 247–251. doi: 10.1016/j.radi.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 24. Lewis EF, Hardy M, Snaith B. Estimating the effect of nonresponse bias in a survey of hospital organizations. Eval Health Prof 2013; 36: 330–51. doi: 10.1177/0163278713496565 [DOI] [PubMed] [Google Scholar]
- 25. Rashidian A, van der Meulen J, Russell I. Differences in the contents of two randomized surveys of GPs’ prescribing intentions affected response rates. J Clin Epidemiol 2008; 61: 718–21. doi: 10.1016/j.jclinepi.2007.10.019 [DOI] [PubMed] [Google Scholar]
- 26. Young J. Mail surveys of general practice physicians; response rates and non-response bias. Swiss Med Weekly 2005; 135: 187–8. [DOI] [PubMed] [Google Scholar]
- 27. Price RC, Le Masurier SB. Longitudinal changes in extended roles in radiography: A new perspective. Radiography 2007; 13: 18–29. doi: 10.1016/j.radi.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 28. McNulty JP, Rainford L, Bezzina P, Henner A, Kukkes T, Pronk-Larive D, et al. A picture of radiography education across Europe. Radiography 2016; 22: 5–11. doi: 10.1016/j.radi.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 29. Cowling C. Global review of radiography. Radiography 2013; 19: 90–1. doi: 10.1016/j.radi.2013.01.001 [DOI] [Google Scholar]
- 30. Campeau F, Fleitz J. Limited Radiography. Fourth Edition Boston: The British Institute of Radiology.; 2016. [Google Scholar]
- 31. Australian Institute of Radiography. Discussion paper on Limited Licence Remote X-ray Operator Radiography in Australia. Melbourne: The British Institute of Radiology.; 2011. http://www.asmirt.org/cms_files/00_Homepage/00_LatestNews/rxo_air_discussion_sept2011.pdf. [Google Scholar]
- 32. Smith T, Fisher K. Self-reported competency and continuing education needs of limited licence remote X-ray operators in New South Wales, Australia. Rural Remote Health 2011; 11: 1560. [PubMed] [Google Scholar]
- 33. Miller L, Price R, Hicks B, Higgs T. Second phase evaluation of the introduction of Radiography Assistant Practitioners in Imaging Services in Scotland. Brighton: The British Institute of Radiology.; 2011. [Google Scholar]
- 34. Baker D. Designing a curriculum for the assistant practitioner of the future: Ensuring interprofessional care aspects and other stakeholder requirements are met. Radiography 2016; 22: 161–5. doi: 10.1016/j.radi.2015.10.004 [DOI] [Google Scholar]
- 35. Stewart-Lord A. Training and development of the Assistant Practitioners (APs) in radiography. Radiography 2014; 20: 36–41. doi: 10.1016/j.radi.2013.08.003 [DOI] [Google Scholar]
- 36. Miller L, Williams J, Marvell R, Tassinari A. Assistant Practitioners in the NHS in England. Bristol: The British Institute of Radiology.; 2013. [Google Scholar]
- 37. Nursing and Midwifery Council. Standards for medicines management. London: The British Institute of Radiology.; 2010. [Google Scholar]
- 38. Skills for Health. CHS2 Assist in the administration of medication. London: The British Institute of Radiology.; 2010b. [Google Scholar]
- 39. Skills for Health. CHS3 Administer medication to individuals. London: The British Institute of Radiology.; 2010c. [Google Scholar]
- 40. Society of Radiographers. Diagnostic Radiography: A Survey of the Scope of Radiographic Practice 2015. London: The British Institute of Radiology.; 2017. https://www.sor.org/sites/default/files/document-versions/2017-05-17_diagnostic_scope_of_practice_2015_-_final.pdf. [Google Scholar]
- 41. Royal College of Radiologists. The breast imaging and diagnostic workforce in the United Kingdom. London: The British Institute of Radiology.; 2016. P34. [Google Scholar]
- 42. Drennan VM, Gabe J, Halter M, de Lusignan S, Levenson R. Physician associates in primary health care in England: A challenge to professional boundaries? Soc Sci Med 2017; 181: 9–16. doi: 10.1016/j.socscimed.2017.03.045 [DOI] [PubMed] [Google Scholar]
- 43. Spilsbury K, Adamson J, Atkin K, Bloor K, Carr-Hill R, McCaughan D, et al. Challenges and opportunities associated with the introduction of assistant practitioners supporting the work of registered nurses in NHS acute hospital trusts in England. J Health Serv Res Policy 2011; 16(Supp 1): 50–6. doi: 10.1258/jhsrp.2011.010106 [DOI] [PubMed] [Google Scholar]