Abstract
Objective:
This study assessed bladder and rectal dose based on Cartesian-coordinates in intracavitary brachytherapy and examined the variations resulting from use of tandem-ring (T-R) of different angles.
Methods:
Cartesian-co-ordinates of bladder and rectum points were derived on orthogonal-radiographs of 90 patients who had high-dose-rate brachytherapy for cervical cancer at the Department of Radiation Oncology, University College Hospital, Ibadan, Nigeria. The patients were classified in three groups of 30, based on T-R angles 30°, 45° and 60° used, bearing same lengths and diameters across sets. The measured co-ordinates and the related percentage doses to points of interest in the two organs were analysed using EViews and SPSS statistical softwares.
Results:
The mean rectal point dose (RPD) obtained was 68.97 ± 13.57 % of the prescribed doses as against 56.57 ± 11.83% for bladder point dose. While the maximums of the mean RPD were 95.7, 90.5 and 82.5% for T-R angles 30°, 45° and 60° respectively; corresponding values for the bladder point were 72.8, 87.8 and 62.3%.
Conclusion:
The baseline data obtained in this study served as guidelines for subsequently achieving acceptable values of bladder point dose and RPD at University College Hospital, Nigeria. Special attention should be paid to the application of 2 cm-tandems in relation to the RPD.
Advances in knowledge:
This is one of the few studies assessing the influence of T-R angles on organs-at-risk. The increase in RPD with the use of intrauterine tandem-2 cm is found to be most pronounced with T-R 300, and this trend reduced with larger angles.
Introduction
The success of brachytherapy in managing cancer of the cervix could engender morbidity of the related normal organs at risk (OARs) such as the bladder and the rectum when exposed to undue radiation. Radiograph-based dosimetry proposed by the International Commission on Radiological Units and Measurements (ICRU)1 has been in practice for two-dimensional (2D) evaluation of dose to such organs in intracavitary brachytherapy (ICBT). This is practicable when the Cartesian co-ordinates of the reference points (related to the normal organs) defined by the ICRU are known. The geometrical positions of these points from the brachytherapy applicator will determine the dose incurred by the OARs, otherwise known as critical organs. Distance is an established factor for enhancing radiation protection in the field of radiation medicine. The inverse square law which is pivotal to distance is of more significance in brachytherapy than external beam radiotherapy. This could be attributable to steep dose gradient which particularly exists in brachytherapy dosimetry. The farther a point is away from the applicator-carrying source, the lower the dose that will result at such point. OARs such as bladder and rectum in this case should be considered independently (separately) as maximising applicator distance from the anterior bladder cannot automatically reduce radiation dose to the posterior rectum. Although image-based (three-dimensional, 3D) brachytherapy has evolved and in practice for about a decade, many institutions across the world, particularly in low-income countries still perform the 2D technique requiring use of orthogonal radiographs. In ICBT, treatment planning without an absolute guidance from 3D images often pose a challenge to dose distribution around the OARs. The potential risk to OARs becomes higher in the high-dose-rate (HDR) technique, which involves a higher prescription dose per fraction. In radiograph-based dosimetry, the need is therefore indicated to find measures of minimizing doses at the related normal organs using the concept of distance. This study set out to assess the relevance of Cartesian co-ordinates in 2D brachytherapy for cervical cancer.
methods and materials
In this retrospective study, 90 patients booked for HDR brachytherapy of the cervix using tandem-ring (T-R) applicators between 2011 and 2012 were enrolled in this study. This has been the primary applicator of choice at the Department of Radiation Oncology, University College Hospital (UCH), Ibadan which pioneered HDR BT in Nigeria and West Africa. T-R HDR-BT has been gaining wider utilization secondary to increased patient comfort, ease of insertion, interfractional consistency, and applicability in patient with narrow vagina.2 Other related equipment include Gynesource (60Co) Afterloader and HDR-Basic treatment planning system (TPS) (Bebig, Germany). The patients were classified into three groups according to the T-R angles utilized. They fitted in groups I, II and III treated with T-R sets 30°, 45° and 60° respectively. Based on manufacturer’s information given in Figure 1, the 30° tandem is the most angled. This was earlier stated by Busselberg et al3 who examined the effect of tandem dimensions on normal organs dose of patients treated with brachytherapy. The groups of 30 patients each shared a common feature in that ICBT was carried out using same dimensions [lengths of the intrauterine tandem (IUT) and diameters of the ring (R)] of ring applicators. This implies that for every patient enlisted in Group I who had BT application with a 30° T-R set, there was a corresponding patient each in the other groups treated with same applicator size. Each study group comprised six combinations of T-R applicators which include IUT 20mm-Ring 30mm, IUT 40mm-Ring 25mm, IUT 40mm-Ring 30mm, IUT 40mm-Ring 35mm, IUT 60mm-Ring 25mm and IUT 60mm-Ring 30mm. These applicators’ sizes are illustrated in Figure 2. Prior to this study, ethical approval was obtained from the institutional review board. The practice of HDR brachytherapy at UCH, Nigeria has been described previously.4 Dose prescriptions to the reference point A at the institution normally ranged from 15to21Gy delivered (weekly) in 3 fractions in addition to external beam dose of 45Gy in 12 fractions. The tandem and ring were weighted in a standard loading pattern as presented in Table 1 in which the posterior dwell positions were not activated inside the ring in order to limit their contribution to the rectal dose. The ICBT applications involved the use of a Foley's catheter inflated with 7 cm3 of radio-opaque contrast, urografin. Due to the lack of 3D imaging facilities at our institution (UCH, Nigeria), we utilized a fluoroscopic C-Arm X-ray machine for implant verification and generation of orthogonal radiographs prior to treatment delivery. The bladder reference point (BRP) was identified and marked on the radiographs according to the ICRU guidelines.1 Despite our institution’s busy schedule, medical physicists often evaluate doses related to the two OARs provided the orthogonal radiographs have clarity that is adequate for use. This however was often carried out post-treatment delivery of the BT fractional dose. Prior to the period under review, it was particularly challenging to identify the rectal reference point (RRP) on the sagittal patient’s radiograph. This was attributable to the difficulty in visualizing the posterior vaginal wall on the lateral film of the implant due to the fatty pelvic tissues in most of the patients. Besides, Bebig ring applicators available at our institution were not designed to accommodate the use of a rectal retractor (RR). In lieu of this device, the use of a re-usable rectal marker (RM), shown in Figure 3, was adopted. It was fabricated upon request in 2011 at Groote Schuur Hospital, Cape Town, South Africa. The traditional method of determining the rectal dose employs a wire marker inserted into the rectum and relies on its visualization in orthogonal pelvic radiographs.5 The image of the RM lies above the posterior surface of the vaginal cavity which is opacified by the sterile gauze used for intracavitary packing. In this study, Cartesian co-ordinates x,y,z for the BRP (a) and y,z for the RRPs (b, c, d) of the first brachytherapy insertions measured as shown in Figure 4 were only considered. Three points at intervals of 1 cm along the RM (around the T-R intersection) were identified on lateral radiographs in order to enhance the precision of the dose representative of the ICRU rectum point. While the BRP (a) has its x-co-ordinate on the frontal radiograph, the y and z values are obtainable on the lateral image. The RRPs (b, c, d) could be identified and described by the y and z co-ordinates according to the co-ordinate system obtainable on Bebig’s HDR Basic planning system. Assessment of radiation doses to the points of interest (POI) at the OARs was accomplished by replicating the measured co-ordinates (corrected for magnification) on the TPS. Dose to the RRP in this study was evaluated as the mean of the doses obtained from the three sets of co-ordinates y 1, z 1; y 2, z 2; y 3, z 3 based on the use of the RM. While the marker may not accurately be positioned at the anterior rectal wall, it is fairly reproducible from one insertion to another in an individual patient. A sample of three sets of orthogonal radiographs portraying this is shown in Figure 4. Regression analysis was carried out using EViews 10 statistical software while analysis of variance (ANOVA) was performed with SPSS (v. 20). The mathematical relationships obtained were subsequently used to deduce possible dose outcomes in all cases and compared with TPS dosimetry values.
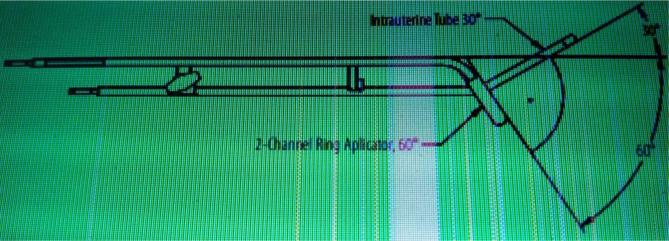
Figure 1.
Illustration of the angle relation between the intrauterine tube (tandem) and the ring applicator.
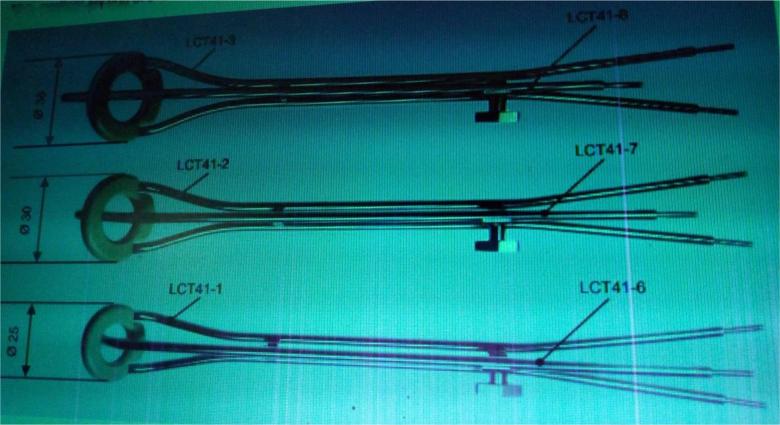
Figure 2.
Illustrations of the different dimensions of Bebig ring (LCT 41–1, 41–2 and 41–3) and tandem (LCT 41–6, 41–7 and 41–8) according to manufacturer’s information.
Table 1.
Applicators and source loading pattern used at University College Hospital, Ibadan, Nigeria
| Applicator type | Dimensions | Source dwell positions | |
| Intrauterine tandem | Length (cm) | No. available | No. activated |
| Long | 6.0 | 12 | 12 |
| Medium | 4.0 | 8 | 8 |
| Short | 2.0 | 4 | 4 |
| Ring applicator | Diameter (cm) | ||
| Large | 3.5 | 7 | 6 |
| Medium | 3.0 | 6 | 5 |
| Small | 2.5 | 5 | 4 |
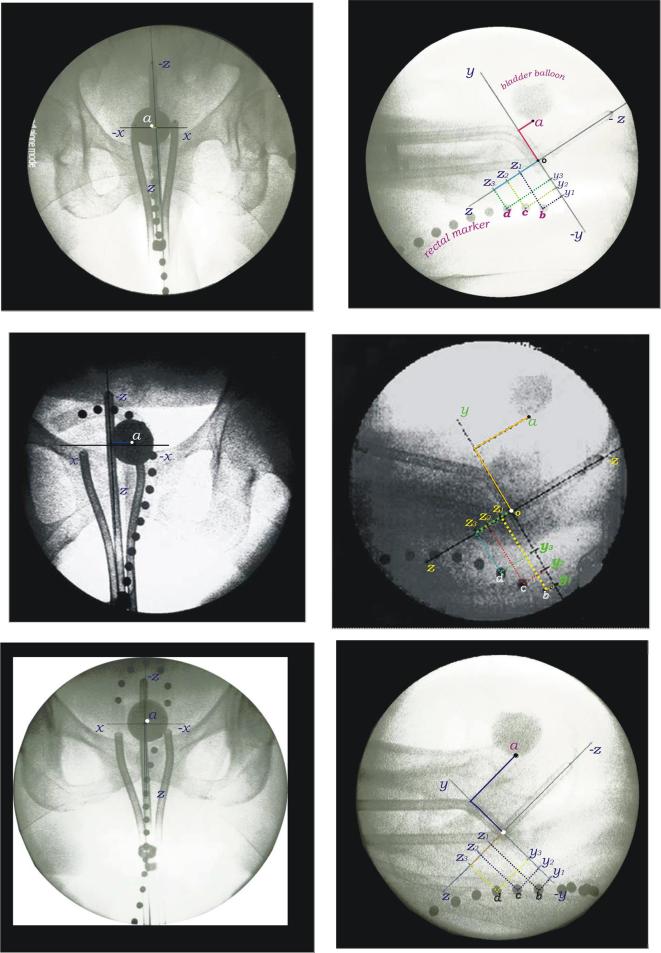
Figure 3.
Rectal marker with 1 cm-spaced ball bearings used for intracavitary brachytherapy at UCH, Nigeria. UCH, University College Hospital.
Figure 4.
Frontal (left) and lateral (right) views of ICBT implants showing the points of interest for the bladder (a), the rectum (b, c, d), the origin of the axes (o) and the related positional coordinates. The three sets of orthogonal radiographs portray the degree of reproducibility of the rectal marker positioning achievable in the same patient with multiple insertions.
Results
In Table 2, bladder point doses (BPDs) and rectum point doses (RPDs) are presented for the three T-R applicators’ angles used at UCH, Nigeria. The data are presented in increasing order of the applicator dimensions (IUT lengths 20–60 mm, ring diameters 25–35 mm). In view of the variation in prescription doses to patients, point doses are presented as percentages of the prescription doses. Table 3 presents the combined results of regression analysis using ordinary least squares method for the two dependent variables, BPD and RPD. It shows the relevant statistics that help deduce the association between the independent and the dependent variables. The mathematical relationships for the BPD resulting from Table 3 could be expressed as:
Table 2.
Mean values of Cartesian co-ordinates measured, related treatment planning system point doses and their comparisons with model-based outcomes for the three tandem-ring angles
| Applicator sizes (mm) | x (cm) | y (cm) | z (cm) | TPS BPD (%) | Model BPD (%) | Diff. (%) | y (cm) | z (cm) | TPS RPD(%) | Model RPD (%) | Diff. (%) |
| 30° | |||||||||||
| T 20-R 30 | 0.2 | 1.9 | 2.4 | 67.8 | 64.0 | –5.6 | 1.3 | 1.8 | 95.7 | 62.2 | –30.0 |
| T 40-R 25 | 0.2 | 2.7 | 2.6 | 58.8 | 55.1 | –6.3 | 1.4 | 1.6 | 59.5 | 63.2 | 6.2 |
| T 40-R 30 | –0.2 | 3.3 | 2.7 | 46.8 | 46.0 | –1.7 | 1.4 | 1.5 | 58.3 | 64.3 | 10.3 |
| T 40-R 35 | –0.4 | 1.2 | 2.7 | 60.3 | 66.5 | 10.3 | 1.7 | 1.2 | 59.1 | 63.8 | 8.0 |
| T 60-R 25 | 0.2 | 2.0 | 1.7 | 60.2 | 65.2 | 8.3 | 1.4 | 1.2 | 61.7 | 67.8 | 9.9 |
| T 60-R 30 | 0.6 | 2.0 | 2.4 | 72.8 | 65.6 | –9.9 | 0.9 | 1.8 | 61.2 | 67.5 | 10.3 |
| Mean | 61.1 | 60.4 | 65.9 | 64.8 | |||||||
| Std. Dev. | 8.9 | 8.2 | 14.6 | 2.3 | |||||||
| 45° | |||||||||||
| T 20-R 30 | 0.6 | 3.0 | 1.0 | 55.1 | 59.1 | 7.3 | 1.7 | 1.3 | 90.5 | 76.2 | –15.8 |
| T 40-R 25 | 0.2 | 2.0 | 2.1 | 87.8 | 79.2 | –9.8 | 2.0 | 1.1 | 63.5 | 68.4 | 7.7 |
| T 40-R 30 | 0.3 | 3.5 | 2.6 | 35.6 | 36.8 | 3.4 | 1.7 | 1.1 | 80.5 | 80.8 | 0.4 |
| T 40-R 35 | 0.1 | 2.8 | 1.9 | 53.9 | 58.5 | 8.5 | 1.5 | 1.4 | 91.3 | 82.1 | –10.0 |
| T 60-R 25 | 0.0 | 2.9 | 0.9 | 54.8 | 60.3 | 10.0 | 1.8 | 1.4 | 63.2 | 69.7 | 10.3 |
| T 60-R 30 | –0.6 | 2.9 | 1.8 | 56.6 | 53.9 | –4.8 | 1.9 | 1.0 | 67.9 | 74.9 | 10.3 |
| Mean | 57.3 | 58.0 | 76.2 | 75.4 | |||||||
| Std. Dev. | 16.9 | 13.6 | 13.0 | 5.6 | |||||||
| 60° | |||||||||||
| T 20-R 30 | 0.2 | 2.7 | 1.2 | 62.3 | 59.8 | –4.0 | 1.9 | 1.4 | 82.5 | 70.6 | –14.4 |
| T 40-R 25 | 0.0 | 3.0 | 1.4 | 57.1 | 51.3 | –10.2 | 2.4 | 1.4 | 56.5 | 54.2 | –4.1 |
| T 40-R 30 | 0.2 | 3.0 | 1.8 | 53.6 | 49.6 | –7.5 | 1.6 | 1.1 | 77.0 | 83.0 | 7.8 |
| T 40-R 35 | -–0.1 | 3.7 | 1.3 | 33.8 | 34.3 | 1.5 | 1.9 | 1.3 | 68.5 | 71.4 | 4.2 |
| T 60-R 25 | 0.0 | 2.8 | 1.1 | 52.4 | 57.7 | 10.1 | 2.4 | 1.2 | 51.4 | 55.8 | 8.6 |
| T 60-R 30 | 0.2 | 3.2 | 0.4 | 48.6 | 51.0 | 4.9 | 2.5 | 0.8 | 53.1 | 55.7 | 4.9 |
| Mean | 51.3 | 50.6 | 64.8 | 65.1 | |||||||
| Std. Dev. | 9.7 | 9.0 | 13.1 | 11.7 | |||||||
BPD, bladderpoint dose; RPD, rectumpoint dose; TPS, treatmentplanning system.
Table 3.
Combined results of regression analysis for the BPD and the RPD in the three groups of patients treated with tandem-ring sets 300, 450 and 600
| 30° | 45° | 60° | ||||
| BPD | RPD | BPD | RPD | BPD | RPD | |
| Constant | 90.063* (12.292) | 99.809* (23.508) | 142.893* (8.284) | 176.632* (16.077) | 132.688* (13.278) | 144.594* (10.539) |
| x | 6.414** (2.957) | 3.294 (2.244) | 0.337 (6.575) | |||
| y | –10.328* (2.567) | –13.125 (10.111) | -26.962* (2.344) | –41.296* (6.751) | –24.955* (3.839) | –32.973* (3.832) |
| z | –3.203 (4.782) | –11.405 (8.688) | –4.882** (1.883) | –23.275* (5.604) | –4.623 (2.123) | –8.083 (4.476) |
| R-sq. | 0.482 | 0.077 | 0.838 | 0.602 | 0.665 | 0.733 |
| R-sq(Adj) | 0.442 | 0.009 | 0.820 | 0.573 | 0.627 | 0.713 |
| Prob(F-statistic) | 0.000 | 0.339 | 0.000 | 0.000 | 0.000 | 0.000 |
| SE of reg. | 11.090 | 18.088 | 9.156 | 11.288 | 8.741 | 8.055 |
| Observations | 30 | 30 | 30 | 30 | 30 | 30 |
BPD, bladderpoint dose; RPD, rectumpoint dose; SE, standard error.
* and ** represent significance at 1 % and 5 % respectively.
for applicator sets 30°, 45° and 60° respectively.
In the case of RPD, the corresponding relationships obtained are:
In Table 4, the combined results of ANOVA are given. The mean doses across T-R combinations differ significantly from one another irrespective of the IUT angle.
Table 4.
Combined outcomes of ANOVA for BDP and RDP of the six combinations of tandem-ring sizes for the three applicator angles
| Source | Degree of freedom | Mean square bladder rectum |
F-stat bladder rectum |
p-value bladder rectum |
| Between groups IUT-ring 30° | 5 | 501.311 1374.334 | 3.284 13.537 | 0.021** 0.000* |
| Within groups | 24 | 152.670 101.521 | ||
| Between groups IUT-ring 45° | 5 | 1413.272 1065.488 | 5.285 7.690 | 0.002* 0.000* |
| Within groups | 24 | 267.419 138.562 | ||
| Between groups IUT-ring 60° | 5 | 540.363 860.513 | 4.295 9.121 | 0.006* 0.000* |
| Within groups | 24 | 125.815 94.348 |
ANOVA, analysisof variance; BPD, bladderpoint dose; RPD, rectumpoint dose; IUT, intrauterine tandem.
* and ** represent significance at 1% and 5% respectively.
Discussion
Cervical cancer is the most common cancer among females in subsaharan Africa.6, 7 However in Nigeria, it is the second most common after breast cancer.8 Many studies have revealed the significant role of brachytherapy in the management of cervical cancer.9–11 It is not feasible, however, to exclude the bladder and the rectum completely of radiation dose while irradiating the target volume, which is the cervix in this case. In each group of patients, the mean dose values were lower for the BRP than the RRP. This could be attributed to the constraints in maximizing the spatial distance between the rectum and the T-R at the time of the study. There was no availability of a RR at our brachytherapy centre. The available ring applicators could not be attached to a RR even if the latter was available. A number of studies12, 13 have considered the rectum as a more critical OAR in which a clinical correlation exists between its dose parameters and toxicity. In the present study (n = 90), the mean rectal dose according to Table 2 was 68.97 ± 13.57% as against 56.57 ± 11.83% for bladder. In a similar study (n = 38, fractions = 38) by Brahmacharimayum et al14 the results were 65 ± 15% and 61 ± 21%, respectively, of prescribed dose at Point A. This trend is again repeated in another study (n = 10, fractions = 55) with the values being 72 ± 6% and 67 ± 7%.15 The American Brachytherapy Society recommended keeping doses to bladder and rectal points below 80% of dose at Point A.16 From another perspective, the present study indicates that 70 and 90% patients received rectal and bladder doses below 80% of prescribed dose at Point A. Corresponding outcomes in a previous study14 mentioned above are 87 and 84% respectively. It is also noticeable in our institutional study that the maximum doses (82.5–95.7%) to the rectum points in each sub group (of five patients each) across the T-R angles occurred with the use of uterine tandem length 2 cm. This outcome is similar to the findings (RPD > 80 %) of Brahmacharimayum et al14 in their study involving the Fletcher-suit applicators. They affirmed that shorter intrauterine lengths (≤4 cm) have a tendency to increase rectal and bladder dose in Manchester system of defining dose at Point A. In a related study3 carried out with T-R applicators, the same trend was obtained. The study by Busselberg et. al.3 also revealed that the median doses (D0.1cm 3, D2cm 3) to the bladder were higher for the 30° applicators than the 45° while the converse is the case for the rectum. The mean dose values in relation to T-R angles presented in Table 2 corroborate these outcomes in the earlier study. The bladder is closer to uterine tandem anteriorly. In principle, the uterine sources contribute more to bladder dose than the vaginal sources whether rings or ovoids are used. Similarly, the vaginal sources contribute more to the rectal dose. Prior to this study, we were of the opinion that the longer the uterine tandem (having more effective source strengths), the higher the bladder dose and the larger the ring diameter, the lesser the rectal dose due to distance factor. However, variations in these trends can happen due to the spatial anatomical positioning relative to the “hot” spots of the T-R combination. The rectal doses in this study are comparable at least, or less than the values obtained from other studies even though there was no availability of a RR at our institution. Over the years, rectal retractors have been found to contribute reasonably to rectal dose reduction. Their applications engender a good reproducibility with an adjustable fixing mechanism holding them and the applicators together. However, there are constraints in the use of RR as they could be difficult to apply in patients with narrow or fibrotic vaginal vaults.17 The present study indicates that the increase in rectal dose with the use of IUT length 2 cm is particularly more pronounced with T-R 30°, and this trend reduces with larger T-R angles. From the foregoing, efforts should be generally intensified in brachytherapy to keep the rectum dose very minimal from the first application, irrespective of the applicator type in use. Table 3 which presents inferential outputs of the regression analysis shows that a significant p-value (0.000) was obtained for the BPD across the applicator angles. This implies that x,y,z co-ordinates jointly have significant effect on the bladder dose. The same trend was obtained for the RPD except for the 30° tandem applicator (p = 0.339). The degree of this effect was examined by considering the adjusted R2 which depicts the proportion of variance in bladder or rectal dose that is jointly explained by the related co-ordinates. For T-R sets 45° (most commonly used at UCH) and 60°, the values of this parameter are 82 and 62.7% respectively for the bladder dose. However, the values of the adjusted R2 showed an increasing trend with the angles of IUT-R combination for the rectal dose. According to Table 3, the x-co-ordinate is a positive function of the BPD irrespective of the tandem angles. It is therefore needful to have the Foley balloon pulled down prior to imaging in every application. Consequently, it will be centrally placed on the anteroposterior radiograph and the x-co-ordinate of the BRP will be or approximately zero, to engender a reduced BPD. From the foregoing, the effect of this would be most pronounced in the 30° applicator sets where the coefficient of the x-co-ordinate is maximal. Conversely, y and z co-ordinates are a negative function of the BPD and the related factors are 10.33, 26.96 and 25.53% (y axis) and 3.20, 4.88 and 4.75% (z axis) for 30°, 45° and 60° T-R respectively. It could be inferred, therefore, that maximizing the distance of the rectal points from the applicator-carrying source on the y-co-ordinate (Figure 4) is fundamental. This is more crucial to engendering reduction in BPDs and RPDs in 2D-based brachytherapy. In Table 2, the dose outcomes of the mathematical equations resulting from the regression analysis and their comparisons with TPS values are also presented. The co-ordinates shown are the mean values of such data for five patients in each case. The resulting model-based data deviated positively and otherwise from TPS-related doses. A positive deviation (more noticeable for rectal doses) which implies that a predicted value is higher relative to TPS calculation would rather be to the advantage of the OAR. The model-based results generally agree with the TPS values within 10% except for rectal doses involving the application of the shortest (2 cm) tandems only. The results of ANOVA presented in Table 4 depict that there are significant differences (mostly at 99% confidence interval) in the mean rectal and bladder doses related to the six combinations of IUT and R sizes across the tandem angles. The outcomes of the ANOVA affirm that applicator sizes are crucial to dose distributions in bladder and rectum, particularly in 2D brachytherapy where image guidance is not applied. Based on our knowledge, this is the first study considering and comparing the effects of Cartesian-co-ordinates on bladder and rectum points’ doses in T-R sets of three different angles. At the moment, there are no published data of this nature with which certain outcomes of this study could be compared.
Previous studies in image-guided cervical brachytherapy showed that ICRU bladder and rectum points fail to correspond with the maximum doses to these structures.18, 19 This, therefore, informs the need to minimize point doses as much as possible. Bearing the dose estimates in Table 2 in mind, our subsequent institutional goal was to achieve ≤60% and 70% of the fractional Point A dose at the RRP and BRP respectively. This work (Table 2) presents some guidelines to help busy clinics with very limited resources achieve the expected dosimetry goals in relation to these OARs. It has been documented earlier that there is a variation in the application geometry with multiple HDR applications in cervical carcinoma.16, 20,21 This challenge could be addressed by ensuring proper selection of applicator size and angle at every instance of an individual’s BT applications, as well as vaginal packing. This study has therefore helped to formulate some guidelines for T-R applications. This is in response to concerns on how to keep the rectal and bladder doses within the acceptable limits in the practice of 2D brachytherapy. The application of a RM in this study might have engendered an underestimation of the rectal dose in some cases. However, the need for a satisfactory level of vaginal packing which will determine the Cartesian coordinates of the OARs with respect to the applicator is indicated. Our institution intends to replace the current sets of applicators with new ones that are usable with a RR in the near future. This rectal tool will definitely facilitate vaginal packing in the case of the rectum which is a more critical OAR. Gauze packing is one of the factors affecting the dose to rectum and bladder.22
CONCLUSIONs
This study reports a 2D dosimetric approach for limiting doses to bladder and rectum’s POI in intracavitary HDR brachytherapy. While the clinical workflow at UCH is dictated by the limited equipment and staffing, the outcomes presented here are practical and compelling. This work identifies what considerations should be given to the Cartesian co-ordinates to reach the desired OARs’ dose constraints, and also makes comparisons among the T-R sets of different angles. Acceptable levels of BPD and RPD using T-R applicators were subsequently achieved at UCH with the use of the baseline data obtained. Institutions not practicing image-guided (3D) brachytherapy should carry out similar studies with their applicators to promote QA in ICBT.
Footnotes
Acknowledegments: The authors acknowledge the International Atomic Energy Agency, Vienna, Austria for setting up the first HDR brachytherapy center in Nigeria at our institution. Also, we are grateful to Jan Hough and the engineering staff of the Department of Medical Physics, Groote Schuur Hospital, Cape Town, South Africa for producing the re-usable rectal markers used at University College Hospital, Ibadan, Nigeria.
REFERENCES
- 1. International commission on radiation units and measurements, dose and volume specification for reporting intracavitary therapy in gynecology. ICRU Report 38. Bethesda 1985. 1985.
- 2. Wolli M, Kagan A, Olch A. Comparison of the ring ap plicator and the Fletcher applicator for HDR gynaecological brachytherapy. Selectron Brach J 1991; 2: 25–7. [Google Scholar]
- 3. Busselberg C, Craciunescu O, Meltsner S, Steffey B, Chino J. The effect of tandem angle and tandem length on normal structure dose in cervical cancer patients treated with tandem and ring applicators. Brachytherapy 2014; 13: S87–S88. doi: 10.1016/j.brachy.2014.02.360 [DOI] [Google Scholar]
- 4. Ibhade OR, Oyeyemi OE, Idayat AB, Atara I N. Tandem-ring dwell time ratio in Nigeria: dose comparisons of two loading patterns in standard high-dose-rate brachytherapy planning for cervical cancer. J Contemp Brachytherapy 2015; 7: 161–70. doi: 10.5114/jcb.2015.50660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Serkies K, Badzio A, Jereczek-Fossa B, Tarnawska Z, Nowak R, Szewczyk P, et al. Rectal doses in intracavitary brachytherapy of gynecological malignancies: comparison of two dosimetric methods. Radiother Oncol 2001; 58: 37–41. doi: 10.1016/S0167-8140(00)00325-X [DOI] [PubMed] [Google Scholar]
- 6. Sitas F, Pacella-Norman R, Carrara H, Patel M, Ruff P, Sur R, et al. The spectrum of HIV-1 related cancers in South Africa. Int J Cancer 2000; 88: 489–92. doi: [DOI] [PubMed] [Google Scholar]
- 7. Piras F, Piga M, De Montis A, Zannou AR, Minerba L, Perra MT, et al. Prevalence of human papillomavirus infection in women in Benin, West Africa. Virol J 2011; 8: 514. doi: 10.1186/1743-422X-8-514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127: 2893–917. doi: 10.1002/ijc.25516 [DOI] [PubMed] [Google Scholar]
- 9. Coia L, Won M, Lanciano R, Marcial VA, Martz K, Hanks G. The Patterns of care outcome study for cancer of the uterine cervix. Results of the second national practice survey. Cancer 1990; 66: 2451–6. doi: [DOI] [PubMed] [Google Scholar]
- 10. Lanciano RM, Won M, Coia LR, Hanks GE. Pretreatment and treatment factors associated with improved outcome in squamous cell carcinoma of the uterine cervix: a final report of the 1973 and 1978 patterns of care studies. Int J Radiat Oncol Biol Phys 1991; 20: 667–76. doi: 10.1016/0360-3016(91)90007-Q [DOI] [PubMed] [Google Scholar]
- 11. Logsdon MD, Eifel PJ. Figo IIIB squamous cell carcinoma of the cervix: an analysis of prognostic factors emphasizing the balance between external beam and intracavitary radiation therapy. Int J Radiat Oncol Biol Phys 1999; 43: 763–75. doi: 10.1016/S0360-3016(98)00482-9 [DOI] [PubMed] [Google Scholar]
- 12. Georg P, Kirisits C, Goldner G, Dörr W, Hammer J, Pötzi R, et al. Correlation of dose-volume parameters, endoscopic and clinical rectal side effects in cervix cancer patients treated with definitive radiotherapy including MRI-based brachytherapy. Radiother Oncol 2009; 91: 173–80. doi: 10.1016/j.radonc.2009.01.006 [DOI] [PubMed] [Google Scholar]
- 13. Koom WS, Sohn DK, Kim JY, Kim JW, Shin KH, Yoon SM, et al. Computed tomography-based high-dose-rate intracavitary brachytherapy for uterine cervical cancer: preliminary demonstration of correlation between dose-volume parameters and rectal mucosal changes observed by flexible sigmoidoscopy. Int J Radiat Oncol Biol Phys 2007; 68: 1446–54. doi: 10.1016/j.ijrobp.2007.02.009 [DOI] [PubMed] [Google Scholar]
- 14. Sharma BA, PhD T, Tomcha Singh MD. The rectum and bladder doses in intracavitary brachytherapy for cervical cancer. J Contemp Brachyther 2010; 2: 153–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tan YI, Choo BA, Lee KM. 2D to 3D evaluation of organs at Risk doses in intracavitary brachytherapy for cervical cancer. J Contemp Brachyther 2010; 2: 37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nag S, Erickson B, Thomadsen B, Orton C, Demanes JD, Petereit D, et al. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys 2000; 48: 201–11. doi: 10.1016/S0360-3016(00)00497-1 [DOI] [PubMed] [Google Scholar]
- 17. Lee KC, Kim TH, Choi JH, Choi MS, Kim CY, Kim JY. Use of the rectal retractor to reduce the rectal dose in high dose rate intracavitary brachytherapy for a carcinoma of the uterine cervix. Yonsei Med J 2004; 45: 113–22. doi: 10.3349/ymj.2004.45.1.113 [DOI] [PubMed] [Google Scholar]
- 18. Schoeppel SL, Fraass BA, Hopkins MP, La Vigne ML, Lichter AS, McShan DL, et al. A CT-compatible version of the fletcher system intracavitary applicator: clinical application and 3-dimensional treatment planning. Int J Radiat Oncol Biol Phys 1989; 17: 1103–9. doi: 10.1016/0360-3016(89)90164-8 [DOI] [PubMed] [Google Scholar]
- 19. Schoeppel SL, LaVigne ML, Martel MK, McShan DL, Fraass BA, Roberts JA. Three-dimensional treatment planning of intracavitary gynecologic implants: analysis of ten cases and implications for dose specification. Int J Radiat Oncol Biol Phys 1994; 28: 277–83. doi: 10.1016/0360-3016(94)90168-6 [DOI] [PubMed] [Google Scholar]
- 20. Grigsby PW, Georgiou A, Williamson JF, Perez CA. Anatomic variation of gynecologic brachytherapy prescription points. Int J Radiat Oncol Biol Phys 1993; 27: 725–9. doi: 10.1016/0360-3016(93)90402-H [DOI] [PubMed] [Google Scholar]
- 21. Kim RY, Meyer JT, Spencer SA, Meredith RF, Jennelle RL, Salter MM. Major geometric variations between intracavitary applications in carcinoma of the cervix: high dose rate vs. low dose rate. Int J Radiat Oncol Biol Phys 1996; 35: 1035–8. doi: 10.1016/0360-3016(96)00187-3 [DOI] [PubMed] [Google Scholar]
- 22. Garipağaoğlu M, Tunçel N, Dalmaz MG, Gülkesen H, Toy A, Kizildağ AU, et al. Changes in applicator positions and dose distribution between high dose rate brachytherapy fractions in cervix carcinoma patients receiving definitive radiotherapy. Br J Radiol 2006; 79: 504–9. doi: 10.1259/bjr/33762931 [DOI] [PubMed] [Google Scholar]