Abstract
The incidence of cardiac arrest in the intensive care unit (ICU-CA) has not been widely reported. We undertook a systematic review and meta-analysis of studies reporting the incidence of cardiac arrest in adult, general intensive care units. The review was prospectively registered with PROSPERO (CRD42017079717). The search identified 7550 records, which included 20 relevant studies for qualitative analysis and 16 of these were included for quantitative analyses. The reported incidence of ICU-CA was 22.7 per 1000 admissions (95% CI: 17.4–29.6) with survival to hospital discharge of 17% (95% CI: 9.5–28.5%). We estimate that at least 5446 patients in the UK have a cardiac arrest after ICU admission. There are limited data and significant variation in the incidence of ICU-CA and efforts to synthesise these are limited by inconsistent reporting. Further prospective studies with standardised process and incidence measures are required to define this important patient group.
Keywords: Heart arrest, cardiopulmonary resuscitation, critical care, critical care outcomes, intensive care units
Introduction
Out-of-hospital cardiac arrest is usually considered separately from in-hospital cardiac arrest as there are clinically important differences in population, medical response and outcome.1,2 Some special circumstances (e.g. trauma, pregnancy) are further distinguished on the basis of clinical factors and treatment recommendations.3
Within a hospital, such distinctions are not drawn, yet it is the case that the patients within the intensive care unit (ICU) are different to those on the wards. There is a quantitative difference in severity of illness if not a qualitative difference in provision of organ support. Further, as a consequence of continuous monitoring, higher nurse and doctor staffing and supportive therapies, the medical response is also necessarily different to that on the ward.4 Finally, our previous work suggests that patients who did and did not suffer cardiac arrest in the ICU represent distinct groups with different outcomes.5
In the United Kingdom, the prospective multi-centre National Cardiac Arrest Audit (NCAA) excludes patients with a cardiac arrest in the ICU if they are not attended by the hospital based resuscitation team in response to a 2222-call, and the Intensive Care National Audit and Research Centre Case Mix Programme (ICNARC CMP) does not collect information on cardiac arrest occurring in ICU.6 This is not unique to the UK: the Australia and New Zealand Intensive Care Society (ANZICS) CORE database also does not capture this information. A previous systematic review of the topic covering 1990–2012 concluded that data on ICU cardiac arrest (ICU-CA) was “limited” and of “moderate” quality.7
The search strategy used in this previous review can be improved by using free-text terms as well as thesaurus subject terms, by including all relevant thesaurus subject terms and by searching in an additional bibliographic database (EMBASE) unrestricted by date (as recommended in the Cochrane Handbook).8 Updating and extending the search strategy enabled us to address these issues and to identify studies published since 2012. We have also performed a meta-analysis to give a pooled estimate of incidence and to provide crude estimates of the numbers of patients who have a cardiac arrest within ICUs in the United Kingdom.
Methods
Aim and objectives
The primary aim of this systematic review was to describe the incidence of cardiac arrest in adults after admission to a non-cardiac intensive care unit. Objectives were to update a previous review of the incidence of ICU-CA, to compare incidence in all studies with that in contemporary (defined as 2014 to present) and UK practice and to provide an estimate of the absolute number of ICU-CA in the non-cardiac adult intensive care population in the UK.
Protocol and registration
The review was prospectively registered with PROSPERO (CRD42017079717). The protocol is available at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=79717.
Eligibility
The inclusion criteria were as follows:
Population: adult patients in an intensive care unit suffering a cardiac arrest (defined as receiving chest compressions and/or defibrillation) after admission.
Study types: all studies reporting the primary outcome measure were eligible.
Outcome measure: incidence of cardiac arrest, as defined above, reported as % of admissions or rate per 1000 admissions or both.
There was no date restriction. The exclusion criteria were as follows:
Specialist cardiac or paediatric ICU.
Patients under 18 years old.
Primary outcome (incidence) not reported.
Palliative care admissions to ICU.
Non-English language studies.
Sources and search strategy
We searched the following electronic bibliographic databases using the search strategy in Box 1: Medline via HDAS (1946 to present), Cochrane Central Register of Controlled Trials via Wiley, Embase via Ovid (1974 to present) and CINAHL via HDAS (1981 to present) on 17 October 2017. Manual searching was used to identify additional results. Study authors were not contacted.
Box 1.
Medline search strategy.
| 1 | (“intensive care”).ti,ab |
| 2 | (“critical care”).ti,ab |
| 3 | (“intensive treatment unit*”).ti,ab |
| 4 | (“intensive therapy unit*”).ti,ab |
| 5 | (ICU).ti,ab |
| 6 | (ITU).ti,ab |
| 7 | "INTENSIVE CARE UNITS"/ |
| 8 | "CRITICAL CARE"/ |
| 9 | "CRITICAL CARE NURSING"/ |
| 10 | (1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9) |
| 11 | (“cardiac arrest*”).ti,ab |
| 12 | (“heart arrest*”).ti,ab |
| 13 | (“heart attack*”).ti,ab |
| 14 | (“cardiopulmonary resuscitation”).ti,ab |
| 15 | (“chest compression*”).ti,ab |
| 16 | (ALS OR BLS OR “advanced life support” OR “basic life support”).ti,ab |
| 17 | "DEATH, SUDDEN, CARDIAC"/ |
| 18 | "HEART ARREST"/ |
| 19 | "CARDIOPULMONARY RESUSCITATION"/ |
| 20 | "ADVANCED CARDIAC LIFE SUPPORT"/ |
| 21 | (11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20) |
| 22 | (incidence OR prevalence OR occur* OR frequenc* OR proportion* OR rate OR number* OR percent*).ti,ab |
| 23 | INCIDENCE/ |
| 24 | PREVALENCE/ |
| 25 | "SURVIVAL RATE"/ OR REGISTRIES/ |
| 26 | (22 OR 23 OR 24 OR 25) |
| 27 | (10 AND 21 AND 26) |
| 28 | (exp CHILD/ OR exp INFANT/) NOT (exp ADOLESCENT/ OR exp ADULT/) |
| 29 | 27 NOT 28 |
| 30 | 29 [Languages English] |
Note: The strategy was adapted for Embase, CINAHL and Cochrane Central.
Data items
Screening of titles and/or abstracts was undertaken using Rayyan (Qatar Computing Research Institute, 2016). All articles were screened independently by two review authors to identify studies that potentially met the inclusion criteria outlined above. The full text of potentially eligible studies was retrieved and independently assessed for eligibility by two review team members. Any disagreement over the eligibility of particular studies was resolved by discussion with a third reviewer.
The pre-specified primary outcome was incidence of cardiac arrest. Other data items extracted using a standardised pre-defined template were:
Patient demographic data, including co-morbidities.
Study setting and design, including information for risk of bias assessment.
Survival (using time points reported in source study).
Neurological outcome (using measures in source study).
Aetiology and type of cardiac arrest.
Risk of bias (quality) assessment
A modified version of the Newcastle-Ottawa Scale9 was used to assess the quality of included studies. The assessment domains and scoring are shown in Table 1: high scores identify studies at lower risk of bias. We performed sensitivity analysis excluding studies at risk of selection bias (i.e. score of 1 or 2 on selection domain of the Newcastle-Ottawa Scale). We performed a post hoc sensitivity analysis excluding outliers identified on clinical grounds. We did not assess publication bias.
Table 1.
Modified Newcastle-Ottawa Scale.
| Selection (maximum three points) | |
| Representativeness of exposed cohort | (a) Truly representative of the average intensive care unit* |
| (b) Somewhat representative of the average intensive care unit* | |
| (c) Selected group of patients (e.g. cardiac, surgical) | |
| (d) No description | |
| Selection of non-exposed cohort | (a) Drawn from the same community as the exposed cohort and numbers given* |
| (b) Drawn from a different source or numbers not given | |
| (c) No description of the non-exposed cohort (i.e. numbers not given) | |
| Demonstration that outcome of interest was not present at start of study | (a) Yes* |
| (b) No | |
| Comparability (maximum two points) | |
| Comparability of exposed and non-exposed on the basis of patient demographics | (a) Study reports patient demographics in exposed and non-exposed groups* |
| (b) Not reported | |
| Comparability of exposed and non-exposed on the basis of clinical details | (a) Study reports clinical information in exposed and non-exposed groups* |
| (b) Not reported | |
| Outcome (maximum three points) | |
| Assessment of outcome | (a) Record linkage, method reported* |
| (b) No description | |
| Follow-up to survival outcomes | (a) Yes* |
| (b) No | |
| Adequacy of follow-up of cohorts | (a) Complete follow-up to discharge, all subjects accounted for* |
| (b) Low follow-up rate and no description of those lost | |
| (c) No statement | |
Items marked with an asterisk score one point with maximum one point for each criterion.
Subgroup analysis
We performed subgroup analysis by date to define changes in incidence of ICU-CA over time. Three groups were specified: pre-2005, 2005–2013 and 2014 to present.
Synthesis of results
Meta-analysis was conducted using RStudio (RStudio, Inc.; Version 1.0.143, 2016). An inverse variance random effects model was used for all analyses. Between-study heterogeneity was assessed with I2-test using p < 0.1 as the threshold for statistical significance. Results are presented as percentages and/or rates per 1000 admissions with associated 95% confidence interval, p-values and forest plots. Analyses were performed for all eligible studies and pre-specified subgroups according to unit type.
Results
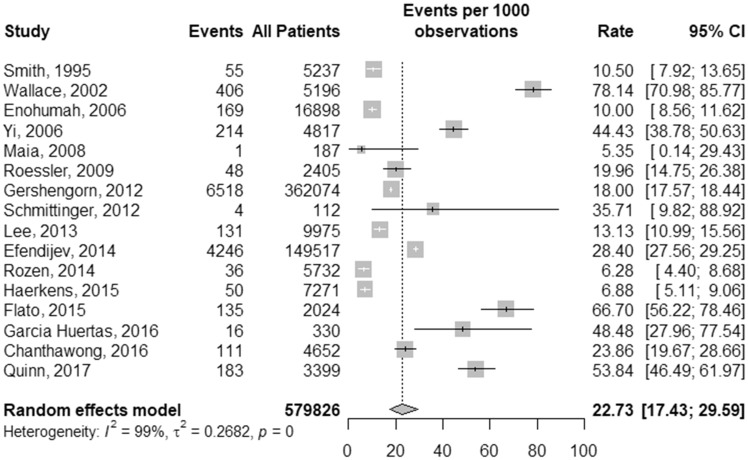
A total of 7550 records were identified in the initial search. After removal of duplicates and screening for eligibility based on the inclusion and exclusion criteria, 20 articles remained for inclusion in the review, 2 of which were identified by manual searching5,10 (Figure 1).
Figure 1.
PRISMA flowchart.
Study characteristics (Table 2)
Table 2.
Summary of included studies.
| Study | Study type | Single/ multicentre | Setting | Timepoint | Patient group | All patients (n) | Incidence (n) | Incidence (%) |
|---|---|---|---|---|---|---|---|---|
| Smith et al.11 | Prospective | Single centre | University hospital, US | 1987–1993 | SICU | 5237 | 55/5237 | 1.1 |
| Wallace et al.22 | Retrospective | Single centre | University hospital, US | 1993–2000 | MICU in a Cancer centre | 5196 | 406/5196 | 7.8 |
| Enohumah et al.25 | Retrospective | Single centre | Tertiary hospital, Germany | 1999–2003 | Mixed | 16,898 | 169/16,898 | 1.0 |
| Yi et al.10 | Retrospective | Single centre | Tertiary university hospital, South Korea | 1992–2002 | NICU | 4817 | 214/4817 | 4.4 |
| Galhotra et al.23 | Retrospective | Single centre | Tertiary centre, US | 2005 | Mixed | NR | 30 (4.02/1000 admissions) | 4.0 |
| Maia et al.12 | Prospective | Single centre | Portugal | 2004–2005 | SICU | 187 | 1/187 | 0.5 |
| Roessler et al.13 | Prospective | Multicentre | Eight ICUs, Austria | 2007–2008 | Mixed | 2405a | 48/2405b | 2.0c |
| Gershengorn et al.26 | Retrospective | Multicentre | 6518 ICUs*, US | 2001–2008 | Mixed* | 362,074 | 6518/362,074 | 1.8 |
| Schmittinger et al.14 | Prospective | Single centre | Tertiary university hospital, Austria | 2009 | Mixed* | 112 | 4/112 | 3.5 |
| Lee et al.24 | Retrospective | Single centre | Tertiary hospital, South Korea | 2009–2010 | Mixed | 9975 | 131/9975** | 1.3 |
| Efendijev et al.15 | Prospective | Multicentre | 21 ICUs, Finland | 2003–2013 | Mixed* | 164,225 | 4717/164,225 | 2.9 |
| Rozen et al.16 | Prospective | Single centre | Tertiary centre, Australia | 2010–2012 | Mixed* | 5732 | 36/5732 | 0.6 |
| Haerkens et al.17*** | Prospective | Single centre | Tertiary centre, Holland | 2009–2012 | Mixed* | 7271 (2295; 2423; 2553) | 50/7271 (21/2295; 20/2423; 9/2553) | 0.7 (0.9; 0.8; 0.4) |
| Flato et al.18 | Prospective | Single centre | Tertiary centre, Brazil | 2013–2014 | NR | 2024 | 135/2024 | 6.7 |
| Garcia Huertas et al.19 | Prospective | Single centre | Spain | 2015 | Mixed | 330 | 16/330 | 4.8 |
| Chanthawong et al.20 | Prospective | Multicentre | Nine tertiary hospitals, Thailand | 2011–2013 | SICU | 4652 | 111/4652 | 2.4**** |
| Perman et al.27 | Retrospective | Multicentre | 445 hospitals, US | 2003–2010 | Mixed* | NR | 50,514***** | |
| Miana et al.21 | Prospective | Multicentre | Three hospitals, Brazil | 2011–2014 | Mixed* | NR | 75/1000 admissions | 7.5 |
| Cook and Thomas5 | Retrospective | Single centre | Tertiary centre, UK | 2015–2017 | Mixed | NR | 25/1000 admissions | 2.5 |
| Quinn et al.28 | Retrospective | Multicentre | Various settings, US | 2010–2014 | Mixed* | 3399 | 183/3399 | 5.4 |
Included CICU. **8.5/1000 admissions/year. ***Numbers shown are total and then for each of three years of the study period. ****Study reported rate of 226/4652 (4.9%) but including 115 patients with do-not attempt resuscitation (DNAR) decision *****Mean event rate 0.337 (±0.215) per 1000 patient-bed days.
(1805 SICU; 600 MICU). b(26/1805 SICU; 22/600 MICU). c(1.4 SICU; 3.7 MICU). SICU surgical ICU; MICU medical ICU; NICU neurosurgical ICU; NR not reported.
Eleven11–21 of the 20 studies were prospective and 135,10–12,14,16–19,22–24 were single centre. The settings include Europe (8),5,12–15,17,19,25 North America (6),11,22,23,26–28 Asia (3),10,20,24 South America (2)18,21 and Australia16 and study dates range from 1987 to 2017. The number of ICU admissions ranges from 112 to 362,074. The results of the quality assessment are shown in Table 3.
Table 3.
Risk of bias (quality) assessment.
| Study | Selection (maximum 3 points) | Comparability (maximum 2 points) | Outcome (maximum 3 points) |
|---|---|---|---|
| Smith et al.11 | 2 | 2 | |
| Wallace et al.22 | 2 | 2 | 3 |
| Enohumah et al.25 | 3 | 2 | 3 |
| Yi et al.10 | 2 | 2 | 3 |
| Galhotra et al.23 | 2 | 3 | |
| Maia et al.12 | 2 | 1 | |
| Roessler et al.13 | 3 | 2 | |
| Gershengorn et al.26 | 3 | 1 | 3 |
| Schmittinger et al.14 | 2 | 2 | |
| Lee et al.24 | 3 | 1 | 2 |
| Efendijev et al.15 | 3 | 2 | 3 |
| Rozen et al.16 | 3 | 2 | 3 |
| Haerkens et al.17 | 3 | 2 | |
| Flato et al.18 | 2 | 1 | |
| Garcia Huertas et al.19 | 3 | 1 | |
| Chanthawong et al.20 | 2 | 2 | 3 |
| Perman et al.27 | 2 | 2 | 2 |
| Miana et al.21 | 2 | 1 | 3 |
| Cook and Thomas5 | 2 | 1 | 2 |
| Quinn et al.28 | 2 | 1 |
Incidence of cardiac arrest (Table 2)
Ten studies reported the definition of cardiac arrest used. The number of cardiac arrests reported varied from 1 to 50,514. Seventeen studies reported both the number of events and the overall number of eligible admissions, three reported rates per 1000 admissions5,21,23 and the remaining study reported mean event rate per 1000 patient-bed days and was not included in pooled analyses.27
The prevalence of ICU-CA varied from 0.5 to 7.8% with incidence rates of 5–78 per 1000 admissions.
Patient demographics
Eleven studies reported demographic data. Average age ranged from 54 to 68.8 years with a male preponderance (51.6–68.5%). Seven studies reported data on patient comorbidities. Cardiac and respiratory co-morbidities were the most prevalent, with up to 100% of patients having one such chronic condition. One study reported the number of patients with any comorbidity at 80.6%, with a median number per patient of 1.5.16
Types of intensive care unit (Table 2)
Most studies (14) reported a mixture of medical and surgical ICUs or patients, of which eight included some cardiac surgery. Ten studies reported case mix data. Emergency admissions ranged from 69.6% to 92.9%. Surgical admissions accounted for 22.8–100% of patients in mixed unit reports. The most common causes of medical admission were respiratory or haemodynamic compromise with sepsis or severe sepsis reported in 10.7–43%. Seven studies reported on severity of illness using seven different models and a total of 10 scores. Further information is available in the online supplementary appendix (Tables A and B).
Cardiac arrest aetiology and outcome
Non-shockable rhythms were more common in eight of nine studies reporting initial rhythm with the proportion of non-shockable rhythms ranging from 61.5 to 89.7%. The presumed aetiology of cardiac arrest was reported in four studies21,24,25,27 with cardiac and respiratory causes accounting for 24.4–78.5% and 13.3–39.7% of arrests, respectively.
The rate of return of spontaneous circulation (ROSC; 10 studies) and of survival (14 studies) are given in Table 4.
Table 4.
Outcomes reported (ROSC and survival).
| Study | ROSC |
Survival |
||||||
|---|---|---|---|---|---|---|---|---|
| 24 h |
ICU |
Hospital |
||||||
| N | % | N | % | N | % | N | % | |
| Smith et al.11 | 23/55 | 41.8 | 7/55 | 12.7 | ||||
| Wallace et al.22 | 150/406 | 36.9 | 111/406 | 27.3 | 9/406 | 2.2 | 7/406 | 1.7 |
| Enohumah et al.25 | 136/169 | 80.5 | 84/169 | 49.7 | 80/169 | 47.3 | ||
| Yi et al.10 | 105/214 | 49.1 | 74/214 | 34.6 | 19/214 | 8.9 | ||
| Galhotra et al.23 | 25/30 | 83.3 | 14/30 | 46.7 | 7/30 | 23.3 | ||
| Roessler et al.13 | 21/48 | 43.8 | ||||||
| Gershengorn et al.26 | 1025/6518 | 15.7% | ||||||
| Schmittinger et al.14 | 4/4 | 100.0 | ||||||
| Lee et al.24 | 96/131 | 73.3 | 57/131 | 43.5 | ||||
| Efendijev et al.15 | 1891/4246 | 44.5 | ||||||
| Rozen et al.16 | 29/36 | 80.6 | 24/36 | 66.7 | 19/36 | 52.8 | 16/36 | 44.4 |
| Haerkens et al.17 | 21/50 | 42.0 | ||||||
| Chanthawong et al.20 | 42/111 | 37.8 | 28/111 | 25.2 | 20/111 | 18.0 | 19/111 | 17.1 |
| Perman et al.27 | NR | 16.2 | ||||||
| Miana et al.21 | 59/242 | 24.4 | 12/213 | 5.6 | ||||
| Cook and Thomas5 | 17/56 | 30.4 | ||||||
ROSC: rate of return of spontaneous circulation; ICU: intensive care unit.
Reported rates of ROSC varied from 24.4 to 100%. The most commonly reported time point for survival assessment was at hospital discharge (11 studies) with rates from 1.7 to 47.3%.
Long-term follow-up was variable with four studies reporting survival outcomes beyond hospital discharge and six reporting neurological outcomes. Time points and performance scales varied. Further information is available in the supplementary appendix (supplementary appendix, Table C).
Three studies compared survival outcomes in patients who did and did not suffer ICU-CA.5,15,20 ICU mortality was higher in ICU-CA patients with reported rates of 69.6% versus 10.5% in a study from a mixed ICU5 and 91.2% versus 6.4% in one SICU study.20 The same study also reported higher hospital mortality at 91.6% versus 7.8%,20 with rates of 55.5% versus 11.4% in a multicentre European study.15
Meta-analysis
Studies that reported only a rate of incidence for ICU-CA and did not report an overall number of observations5,21,23,27 were excluded from quantitative analyses. Similarly for analysis of outcomes, those with only a rate rather than numeric values were excluded.27
Incidence of cardiac arrest
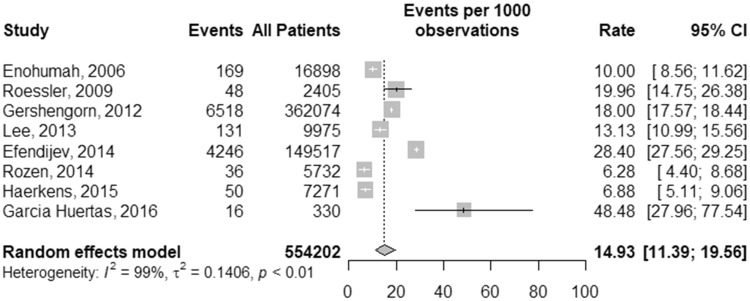
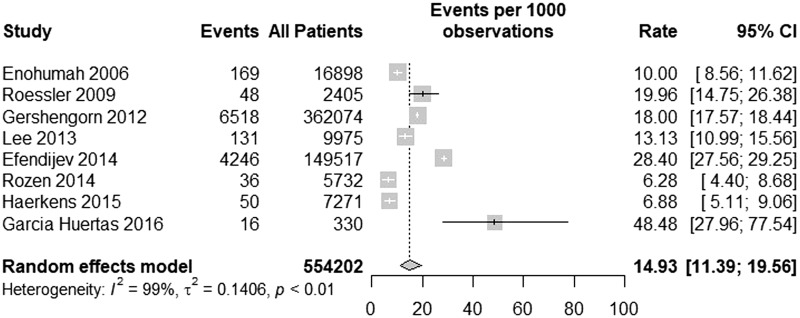
The incidence of cardiac arrest across all studies was 22.7 per 1000 admissions (95% CI: 17.4–29.6, I2 = 99%; Figure 2). For those studies reporting only surgical ICUs (SICUs) or surgical patients, the rate was 22.4 per 1000 admissions (95% CI: 10.5–47.2, I2 = 97%). In studies reporting only mixed medical and surgical ICUs (excluding two studies with only surgical patients in mixed units), the rate was 14.9 (95% CI: 11.4–19.6, I2 = 99%) per 1000 admissions (Figure 3).
Figure 2.
Meta-analysis of incidence for all studies.
Figure 3.
Meta-analysis of incidence for mixed medical and surgical intensive care units.
Incidence of cardiac arrest over time
The pooled rate of ICU-CA in the predefined subgroups is given in Table 5. Further information is available in the supplementary appendix.
Table 5.
Incidence of ICU-CA over time.
| Subgroup | Number of studies | Pooled Incidence (per 1000 admissions) | Pooled incidence 95% confidence interval (per 1000 admissions) |
|---|---|---|---|
| Pre-2005 | 2 | 29.2 | 3.9–187 |
| 2006–2013 | 7 | 18.7 | 12.6–27.8 |
| 2014–present | 7 | 24.7 | 15.6–38.9 |
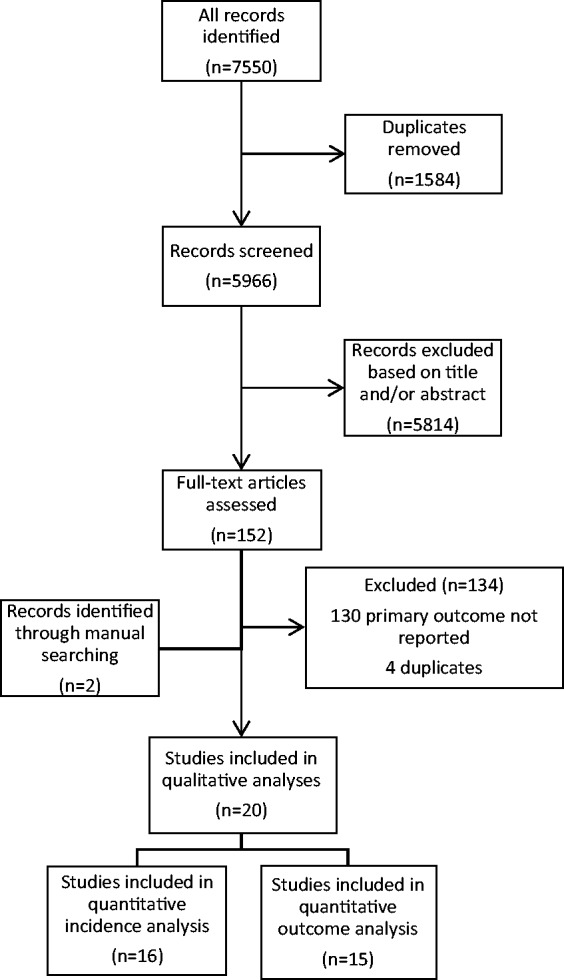
Sensitivity analysis
Excluding those studies at higher risk of selection bias, the pooled incidence of ICU-CA based on eight studies is 14.9 per 1000 admissions (95% CI: 11.4–19.6, I2 = 99%; Figure 4).
Figure 4.
Meta-analysis of incidence for studies at lower risk of selection bias.
Excluding one study from a medical ICU in a cancer centre22 on clinical grounds (highest rate of ICU-CA with lowest rate of survival), the pooled incidence is 20.7 per 1000 admissions (95% CI: 16.4–26.2, I2 = 99%).
Cardiac arrest aetiology and outcome
Across all studies (n = 9), the pooled rate of non-shockable rhythm was 76.8% (95% CI: 69.9–82.4, I2 = 90%). The rate of ROSC across all studies (n = 10) was 58.2% (95% CI: 43.7–71.4%, I2 = 95%). Pooled survival to hospital discharge, the most commonly reported outcome measure (n = 10), was 17% (95% CI: 9.6–28.5%, I2 = 99%). ICU patients who suffered a cardiac arrest in critical care had higher ICU and hospital mortality, with a risk ratio of 7.6 (95% CI: 3.2–18.1) for hospital mortality across two studies. Further information is available in the supplementary appendix.
Intensive care unit cardiac arrest in the United Kingdom
The incidence of ICU-CA in the United Kingdom is estimated at 25 per 1000 admissions (one study).5 Combining data from ICNARC and the Scottish Intensive Care Society Audit Group gives an estimate of 217,820 admissions to ICU in 2016/2017.29,30 The absolute number of ICU-CA in that year may then be approximated as 5446. Using data from NHS Digital for the year 2016–2017, including 293,170 adult critical care records, results in a higher estimate of 7329 ICU-CA.31
Discussion
The reported incidence of cardiac arrest in the intensive care unit (ICU-CA) ranged from 5 to 78 per 1000 admissions with a pooled rate across all studies of 22.7 per 1000 admissions (95% CI: 17.4–29.6). In comparison, the studies selected by Efendijev et al.7 for reporting incidence of ICU-CA give a range of 5–78 per 1000 admissions and a pooled rate of 13.0 per 1000 admission (95% CI: 4.7–35.3). Our figure is based on 16 studies against 6 for the previous study, provides a narrower confidence interval, and represents the current best estimate across a range of unit characteristics. However, clinical and statistical heterogeneity precludes detailed quantitative analysis and it is not possible to determine how much of the variation in incidence and outcome is related to case mix and severity of illness and how much reflects variation in delivery of care.
Given the difference in search strategy and study selection criteria, it is not surprising that our review identifies a different group of articles to Efendijev et al.7 Importantly, updating the previous review of the topic meant that we identified seven studies reported since its publication in 2014. This is the ‘contemporary’ cohort that gives a pooled rate of 24.7 ICU-CA per 1000 admissions, which is very similar to that for current UK practice (25 per 1000 admissions) based on cardiac arrests in our ICU.
Comparing this figure to prior epochs suggests that there is no clear reduction in the overall incidence of ICU-CA with time. The division into three groups is pragmatic based on number of studies, the timing of the previous review and a recognition of the ‘modern era’ of cardiac arrest temperature management from late 2013.32
Again our analysis does not highlight a reason for this. One potential, and worrying, explanation is that the occurrence of ICU-CA is considered normal in the context of critical illness rather than a preventable event. Alternatively, an unchanged rate in the face of increased severity of illness and/or frailty would represent progress.
The sensitivity analysis reveals studies at lower risk of selection bias, taken together, report a lower incidence of ICU-CA than all studies. The magnitude of the difference between the high and low risk groups is comparable to the difference seen between SICUs and mixed ICUs and likely reflects the variability in the primary studies. Given their heterogeneous nature (see below), it is wise to reserve recommendations on changes to clinical practice, or on use of benchmarks from the literature, until sound data have been gathered.
Using a contemporary UK estimate of the incidence of ICU-CA suggests that between 5446 and 7329 cardiac arrests occur after ICU admission each year. For the same year, the NCAA records a total of 16,201 in-hospital cardiac arrests including only 1110 occurring in ICU, high dependency unit (HDU) or combined ICU/HDU.33 There is a need for caution, as the national case mix may not match that in a single, albeit large, ICU even if the incidence there is similar to the contemporary incidence more widely. Despite these caveats, our data suggest a hidden epidemic of cardiac arrest, associated with poorer outcomes (risk ratio for hospital mortality of 7.6) for the sickest patients in hospitals, that is currently under-recognised and under-reported.
It is likely that a proportion of these deaths are related to a ‘failure to rescue’ after critical illness and as such represent an opportunity to intervene to improve patient outcomes. Prospective data collection would better define the scale and prognostic implications of these events. Further ahead, the rate and outcome of ICU-CA could be considered alongside the standardised mortality ratio as a quality indicator and comparison measure. Any prospective data collection should be done according to a standardised set of variables and outcome measures that follow the Utstein style.34,35 This would enhance the quality of published data and permit comparison across varied settings.
This would also address many of the limitations of our systematic review. The studies which comprise this review are largely single-centre reports, with almost half based on retrospective data and the majority at risk of selection bias. Different types of units, countries and healthcare systems are included. Furthermore, they span a period of 30 years, over which time the clinical caseload and interventions of critical care have changed significantly. Finally, there is substantial risk of bias given the low quality of some included studies and small numbers suitable for meta-analysis of key outcomes. It is also the case that, by restricting eligibility to studies reporting the incidence of ICU-CA, we have missed the opportunity to present more complete data on outcomes.
Nevertheless, in comparison to the previous systematic review on this topic, our search strategy proved more sensitive, included an additional bibliographic database, and reports several studies published after 2014 including the first UK data on the topic. We also report quantitative analyses to produce pooled estimates of incidence and outcome measures.
In conclusion, the wide variation in reported incidence of cardiac arrest in the ICU, the difficulty applying these findings to any one ICU or healthcare system, and potential for under-reporting, requires high quality prospective epidemiological studies to provide a sound footing for measures to improve outcomes in this most critical of critical care populations.
Supplemental Material
Supplemental material, Appendix for The incidence of cardiac arrest in the intensive care unit: A systematic review and meta-analysis by Richard A Armstrong, Caroline Kane, Fiona Oglesby, Katie Barnard, Jasmeet Soar and Matt Thomas in Journal of the Intensive Care Society
Authors’ contributions
RA: screening of abstracts, data extraction, analyses, co-author first and subsequent drafts. JS: co-author first and subsequent drafts. CK: screening of abstracts, review final manuscript. FO: screening of abstracts, data extraction, reviewed final version of the manuscript. KB: literature searching, reviewed version of the manuscript. MT: conceived the study, co-author first and subsequent drafts.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JS is paid an honorarium as an editor of Resuscitation, and member of the National Cardiac Arrest Audit Steering Group. The other authors declare that there is no conflict of interest.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Buanes EA, Heltne JK. Comparison of in-hospital and out-of-hospital cardiac arrest outcomes in a Scandinavian community. Acta Anaesthesiol Scand 2014; 58: 316–322. [DOI] [PubMed] [Google Scholar]
- 2.Fredriksson M, Aune S, Bång A, et al. Cardiac arrest outside and inside hospital in a community: mechanisms behind the differences in outcome and outcome in relation to time of arrest. Am Heart J 2010; 159: 749–756. [DOI] [PubMed] [Google Scholar]
- 3.Truhlář A, Deakin CD, Soar J, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation 2015; 95: 148–201. [DOI] [PubMed] [Google Scholar]
- 4.Myrianthefs P, Kalafati M, Lemonidou C, et al. Efficacy of CPR in a general, adult ICU. Resuscitation 2003; 57: 43–48. [DOI] [PubMed] [Google Scholar]
- 5.Cook J, Thomas M. Cardiac arrest in ICU. J Intensive Care Soc 2017; 18: 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Intensive Care National Audit and Research Centre. Response to Cardiac arrest in ICU (J Intensive Care Soc 2017; 18: 173). J Intensive Care Soc 2017; 18: 174. [DOI] [PMC free article] [PubMed]
- 7.Efendijev I, Nurmi J, Castrén M, et al. Incidence and outcome from adult cardiac arrest occurring in the intensive care unit: a systematic review of the literature. Resuscitation 2014; 85: 472–479. [DOI] [PubMed] [Google Scholar]
- 8.Higgins J and Green S (eds). Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011), www.cochrane-handbook.org (2011, accessed 6 Feburary 2018).
- 9.Wells G, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, www.ohri.ca/programs/clinical_epidemiology/oxford.htm (2008, accessed 16 January 2018).
- 10.Yi HJ, Kim YS, Ko Y, et al. Factors associated with survival and neurological outcome after cardiopulmonary resuscitation of neurosurgical intensive care unit patients. Neurosurgery 2006; 59: 838–845. discussion 845–836. [DOI] [PubMed] [Google Scholar]
- 11.Smith DL, Kim K, Cairns BA, et al. Prospective analysis of outcome after cardiopulmonary resuscitation in critically ill surgical patients. J Am Coll Surg 1995; 180: 394–401. [PubMed] [Google Scholar]
- 12.Maia PC, Abelha FJ. Predictors of major postoperative cardiac complications in a surgical ICU. Rev Port Cardiol 2008; 27: 321–328. [PubMed] [Google Scholar]
- 13.Roessler B, Stefaniak J, Krychtiuk K, et al. Outcome after cardiopulmonary resuscitation in intensive care units – preliminary results. Intensive Care Med 2009; 35: S299. [Google Scholar]
- 14.Schmittinger CA, Torgersen C, Luckner G, et al. Adverse cardiac events during catecholamine vasopressor therapy: a prospective observational study. Intensive Care Med 2012; 38: 950–958. [DOI] [PubMed] [Google Scholar]
- 15.Efendijev I, Raj R, Reinikainen M, et al. Temporal trends in cardiac arrest incidence and outcome in Finnish intensive care units from 2003 to 2013. Intensive Care Med 2014; 40: 1853–1861. [DOI] [PubMed] [Google Scholar]
- 16.Rozen TH, Mullane S, Kaufman M, et al. Antecedents to cardiac arrests in a teaching hospital intensive care unit. Resuscitation 2014; 85: 411–417. [DOI] [PubMed] [Google Scholar]
- 17.Haerkens MHTM, Kox M, Lemson J, et al. Crew resource management in the intensive care unit: a prospective 3-year cohort study. Acta Anaesthes Scand 2015; 59: 1319–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flato UAP, Paiva EF, Carballo MT, et al. Echocardiography for prognostication during the resuscitation of intensive care unit patients with non-shockable rhythm cardiac arrest. Resuscitation 2015; 92: 1–6. [DOI] [PubMed] [Google Scholar]
- 19.Garcia Huertas D, Manzano F, Villagran-Ramirez F, et al. Incidence of adverse events in adult intensive care unit patients. Intensive Care Med Exp 2016; 4: A374. [Google Scholar]
- 20.Chanthawong S, Chau-In W, Pipanmekaporn T, et al. Incidence of cardiac arrest and related factors in a multi-center thai university-based surgical intensive care units study (THAI-SICU study). Chotmaihet thangphaet (J Med Assoc Thailand) 2016; 99: S91–S99. [PubMed] [Google Scholar]
- 21.Miana LA, Moraes MM, Moraes BM, et al. Cardiopulmonary resuscitation in an average Brazilian intensive care unit: should we perform less or better? Braz J Cardiovasc Surg 2017; 32: 177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wallace SK, Ewer MS, Price KJ, et al. Outcome and cost implications of cardiopulmonary resuscitation in the medical intensive care unit of a comprehensive cancer center. Support Care Cancer 2002; 10: 425–429. [DOI] [PubMed] [Google Scholar]
- 23.Galhotra S, DeVita MA, Simmons RL, et al. Mature rapid response system and potentially avoidable cardiopulmonary arrests in hospital. Qual Saf Health Care 2007; 16: 260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee HK, Lee H, No JM, et al. Factors influencing outcome in patients with cardiac arrest in the ICU. Acta Anaesthesiol Scand 2013; 57: 784–792. [DOI] [PubMed] [Google Scholar]
- 25.Enohumah KO, Moerer O, Kirmse C, et al. Outcome of cardiopulmonary resuscitation in intensive care units in a university hospital. Resuscitation 2006; 71: 161–170. [DOI] [PubMed] [Google Scholar]
- 26.Gershengorn HB, Li G, Kramer A, et al. Survival and functional outcomes after cardiopulmonary resuscitation in the intensive care unit. J Crit Care 2012; 27: 421.e9–421.e17. [DOI] [PubMed] [Google Scholar]
- 27.Perman SM, Stanton E, Soar J, et al. Location of in-hospital cardiac arrest in the United States-variability in event rate and outcomes. J Am Heart Assoc 2016; 5: e003638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quinn TD, Gabriel RA, Dutton RP, et al. Analysis of unplanned postoperative admissions to the intensive care unit. J Intensive Care Med 2017; 32: 436–443. [DOI] [PubMed] [Google Scholar]
- 29.Intensive Care National Audit and Research Centre. Annual Quality Report 2016/17 for adult critical care, https://onlinereports.icnarc.org/Reports/2017/12/annual-quality-report-201617-for-adult-critical-care# (2017, accessed 28 January 2018).
- 30.Scottish Intensive Care Society Audit Group. Audit of critical care in Scotland 2017: reporting on 2016, www.sicsag.scot.nhs.uk/docs/2017/2017-08-08-SICSAG-Report.pdf?24 (2017, accessed 28 January 2018).
- 31.NHS Digital. Hospital admitted patient care activity 2016–17, https://digital.nhs.uk/catalogue/PUB30098 (accessed 29 March 2018).
- 32.Nielsen N, Wetterslav J, Cronberg T, et al. for the TTM Trial Investigators. Targeted temperature management at 33℃ versus 36℃ after cardiac arrest. N Engl J Med 2013; 369: 2197–2206. [DOI] [PubMed] [Google Scholar]
- 33.Intensive Care National Audit and Research Centre. Key statistics from the National Cardiac Arrest Audit 2016–17, www.icnarc.org/Our-Audit/Audits/Ncaa/Reports/Key-Statistics (2017, accessed 27 January 2018).
- 34.Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation 2015; 96: 328–340. [DOI] [PubMed] [Google Scholar]
- 35.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style'. A statement for healthcare professionals from the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, the Australian Resuscitation Council, and the Resuscitation Councils of Southern Africa. Resuscitation 1997; 34: 151–183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix for The incidence of cardiac arrest in the intensive care unit: A systematic review and meta-analysis by Richard A Armstrong, Caroline Kane, Fiona Oglesby, Katie Barnard, Jasmeet Soar and Matt Thomas in Journal of the Intensive Care Society