Abstract
Purpose
To perform a narrative review of the literature regarding the discharge of patients directly to home (DDH) from the intensive care unit, and to identify patient characteristics and clinical outcomes associated with this practice.
Methods
We searched MEDLINE and EMBASE from 1946 to present. We also manually searched the references of relevant articles. A two-step review process with three independent reviewers was used to identify relevant articles based on predetermined inclusion/exclusion criteria.
Results
Four studies were included in the final review. Two studies were retrospective and two studies were prospective that shared data from the same patient cohort. All were single center studies. Two of the four studies outlined clinical outcomes associated with DDH.
Conclusions
This study highlights the relative dearth in the literature regarding the increasingly common practice of DDH, underscores the importance of further studies in this area, and identifies future important foci of research.
Keywords: Discharge, home, intensive care unit
Introduction
Traditionally, patients discharged from the intensive care unit (ICU) have been transferred to either an intermediate care unit or directly to the ward. This traditional transition of care model is under pressure, largely due to hospital ward capacity pressures, causing the critical care community to increase their number of discharges directly to home (DDH) from the ICU.1 There may be a risk of adverse events associated with DDH if it is not executed carefully. ICUs are not typically equipped with the personnel, resources, follow-up clinics, and discharge protocols that have been in place on the wards for decades. In addition, ICU survivors have prolonged recovery times that sometimes extend beyond hospital discharge and are clearly some of the sickest, most complex cases in the hospital. Conversely, if DDH is performed safely, it can shorten a patient’s length of stay and subsequently abrogate untoward iatrogenic morbidity, improve healthcare resource allocation and utilization, and reduce costs in an already strained healthcare system. Beyond these benefits, a recently published study has also demonstrated high patient satisfaction associated with this practice.2
There are reports of chronically ventilated and palliative patients being discharged directly home from the ICU.3–6 These populations differ from the traditional ICU patients recovering from a critical illness that are the focus of our narrative review.
The expanding prevalence of DDH has yet to be matched by a well circumscribed body of literature supporting its safety and efficacy. Furthermore, DDH is not rigorously defined, with wide variations in definitions and practices existing in the critical care community.
We present a narrative review of the literature reporting patient discharges to home from ICUs or high dependency units. We go on to describe the process of direct discharge to home: highlighting its benefits, its potential risks, and shedding light on areas that merit further research.
Materials and methods
Search question, population, inclusion, and exclusion criteria
The objective of our narrative review was: “To identify the existing literature describing the practice of DDH, with respect to the patient populations and/or outcomes associated with this practice.”
Our inclusion criteria encompassed all prospective and retrospective studies in critically ill adults. Scoping reviews, systematic reviews, and meta-analyses were included. Eligible articles evaluated the transition of critically ill patients from an ICU or high dependency unit to home. ICU was defined as a distinct unit in the hospital that provided invasive monitoring, invasive and non-invasive mechanical ventilation, and administration of vasoactive agents to critically ill patients. A critically ill patient was defined as any patient admitted either electively or non-electively, requiring invasive monitoring, invasive and non-invasive mechanical ventilation, or administration of vasoactive agents. We classified high dependency units or step-down units as ICUs. Home was defined as any place of residence that was a non-healthcare facility or a facility that did not routinely have healthcare personnel available to care for residents (e.g. complex care, rehabilitation facility, nursing home). In this context, patients discharged to home from the ICU in conjunction with additional healthcare services were included.
We excluded all experimental/animal and pediatric studies. Studies pertaining to patients on chronic mechanical ventilation as well as patients discharged directly to home for palliation were excluded. Non-research and conference abstracts were excluded.
Search strategy
Unrestricted searches in MEDLINE and EMBASE were performed from 1946 to present to identify relevant articles. A combination of the following terms was used: ICU, critical care, patient discharge, home. A health information specialist performed the search with appropriate wildcards to take into account plurals and variations in spelling. The references of retrieved articles were screened for additional relevant articles. The full search strategy is available in online Appendix 1. We restricted our search studies to adults (defined as age 18 or older) and to those published in English. The searches encompassed both conference abstracts and non-research articles, which included editorials, correspondence letters, and textbook excerpts. Reference lists of relevant articles were manually searched to identify additional relevant articles.
Study selection and data extraction
Covidence® software was used to facilitate the review. Articles were assessed through a two-stage process to determine inclusion. In the first stage, two reviewers independently reviewed the titles and abstracts and relevant articles were selected for full text review (JB and JL). A third reviewer resolved disagreements (VL). In the second stage, conference abstracts or non-research studies were excluded. Two reviewers independently reviewed the full texts of the articles selected in the first stage (JB and JL). Disagreements between reviewers were discussed in conjunction with a third reviewer (VL) in order to reach agreement. Reviewers were not blinded to the author nor to the journal that the article was published in. In situations where it was unclear if the patient population was discharged from the ICU to home for any given study, the corresponding authors were contacted for further clarification.
Two reviewers independently extracted data in duplicate through a standardized form. We included study design, number of patients, ICU type (medical, surgical, etc.), patient demographics, ICU and hospital characteristics, and outcomes.
Results
Description of the articles
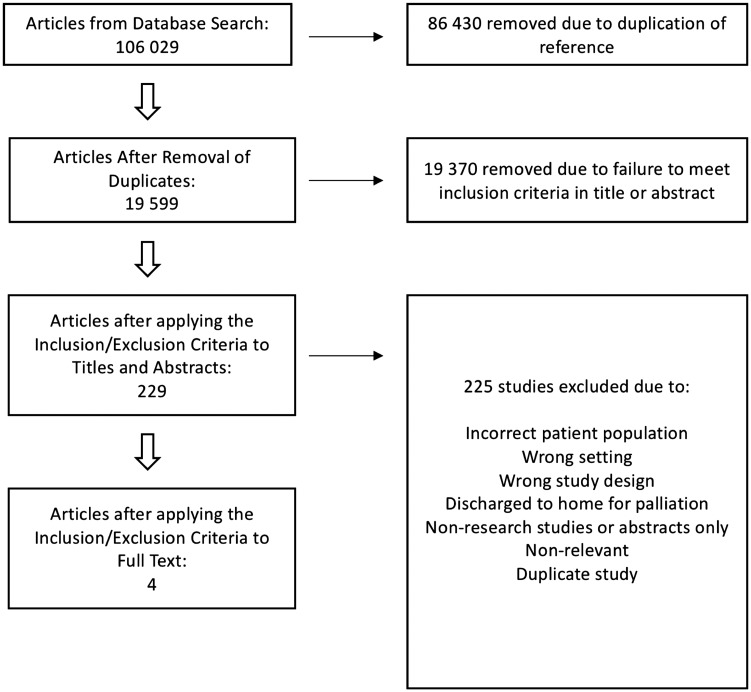
Our search strategy identified 106,029 studies. From these, 86,430 duplicates were removed by Covidence®, leaving 19,599 studies for review. A review of the titles and abstracts yielded 229 full text articles in English. The full texts of these studies were fully reviewed and 225 citations were excluded (Figure 1). The major reasons for exclusions included incorrect patient population, non-relevant articles, and non-research studies.
Figure 1.
PRISMA flow diagram. PRISMA indicates preferred reporting items for systematic reviews and meta-analyses.
The majority of non-relevant studies in the full text review reported on ICU discharge outcomes of patients discharged to the ward first. A few studies noted their experience with discharging ICU patients to home. Two of these studies7,8 were excluded as the discharges were all against medical advice. One citation was excluded based on discharge of chronically ill respiratory patients requiring home mechanical ventilation.3 Two studies were excluded because they described the discharge of critically ill patients to home for palliation.9,10 One other study reported about ICU discharge of chronic critically ill patients in a very small cohort (2 patients in a cohort of 16)11 but despite contacting the corresponding authors, we could not determine whether or not they were DDH from the ICU. Ultimately, four studies were selected for data extraction based on our pre-established inclusion and exclusion criteria.1,2,12,13 Among these, two studies utilized the same cohort of patients. Manual review of the references of these studies did not yield additional articles for consideration. The results of our search strategy are summarized in Figure 1.
Patient and ICU demographics and study design
The selected studies were all of single center, two of which drew upon a cohort of patients enrolled prospectively while the other two were retrospective in nature. A summary of the study designs and primary endpoints and outcomes can be seen in Table 1.
Table 1.
Study design and primary endpoints/outcomes.
| Study | Number of patients | Study design | Primary end points/outcomes |
|---|---|---|---|
| Chawla et al. | 95 | Retrospective cohort study in a 20-bed closed medical/surgical ICU in a tertiary care cancer center | 31.6% of discharged patients were admitted within 30 days. The unplanned readmission rate was 23.2% |
| Lau et al. (retrospective) | 642 | Retrospective cohort study in a 26-bed closed medical-surgical-trauma ICU in a tertiary care center | DDH patients are young, have fewer comorbidities on admission, and few discharge diagnoses |
| Lam et al.a | 137 | Prospective cohort study in a tertiary care center encompassing a 30-bed closed medical-surgical-trauma ICU and a 25-bed medical surgical ICU | Patients and family members are satisfied with practice of DDH from ICU, although ICU physician satisfaction is more variable |
| Lau et al.b (prospective) | 137 | Prospective cohort study in a tertiary care center encompassing a 30-bed closed medical-surgical-trauma ICU and a 25-bed medical surgical ICU | DDH patients experienced no mortality. The unplanned readmission rate was 7.8% |
ICU: intensive care unit.
Both studies drew upon the same cohort of prospectively enrolled patients.
Variations in patient demographics and clinical characteristics were noted between the selected studies. When compared with Lau et al.’s and Lam et al.’s cohorts, Chawla et al. described a patient population that was older, with a higher predicted in-hospital mortality and unplanned readmission rates, and with a longer ICU length of stay. The patient demographics and clinical characteristics are summarized in Table 2.
Table 2.
Patient demographics and clinical characteristics.
| Characteristic | Chawla et al. | Lau et al. (retrospective) | Lam et al. and Lau et al (prospective) |
|---|---|---|---|
| Age (years) | 61.1 | 49 | 45.75 |
| Male (%) | 60 | 54.9 | 66.4 |
| ICU length of stay, days | 4.5 (3–7) | 3 (1.6–5.7) | 1.8 (0.98–3.18) |
| Predicted in-hospital mortality at ICU admission (%) | 31.4a | 7b | 7b |
| Primary diagnoses | Respiratory failure Sepsis Cardiac syndromes Gastrointestinal Bleeding | Overdose Pneumonia Seizures Diabetic Ketoacidosis | Overdose Upper airway compromise Trauma Pulmonary Embolism Seizures |
| Time elapsed from planned transfer to discharge home (days) | 1.7 ± 1.4 | 2.6 ± 2.1 | – |
| Unplanned readmission rate (%) | 23.2 | – | 7.8 |
| Mortality post discharge (%) | 3.2c | – | 0 |
ICU: intensive care unit.
Extrapolated from MPM0II score.
Extrapolated from Multiple Organ Dysfunction Score.
Adjusted for predictable hospice deaths.
There were differences identified between the ICU and hospital characteristics where the studies took place. When compared with Lau et al.’s and Lam et al.’s cohort, Chawla et al.’s study took place in an ICU with a lower annual rate of home discharge, and a lower ICU and ward occupancy. A summary of the ICUs and hospital occupancy statistics is summarized in Table 3.
Table 3.
Intensive care unit and hospital characteristics.
| Characteristic | Chawla et al. | Lau et al. (retrospective) | Lam et al. and Lau et al. (prospective) |
|---|---|---|---|
| ICU model of care | Closed unit | Closed unit | Closed unit |
| ICU capacity (beds) | 20 | 26 | 45a |
| Hospital capacity | 470 | 507 | 952a |
| Hospital services rendered | Academic, tertiary care referral cancer center | Academic, tertiary care referral center | Academic, tertiary care referral center |
| Annual rate of ICU to home discharge (%) | 4.6b | 9.85c | 8.5c |
| ICU occupancy (%) | 76.3d | 92.3 | 92 |
| Ward occupancy (%) | 87e | 103.3 | 104 |
ICU:intensive care unit.
Pooled number between two sites.
Adjusted for planned discharges to hospice.
Calculated average over 14 years.
Calculated average over 3 years.
Reported as total hospital occupancy.
Discussion
We initially sought to perform a systematic review, but only four studies were identified that described the patient demographics and/or outcomes associated with DDH: all of which were single center and two of which were retrospective studies. While the cohorts shared some similarities such as a low acuity of illness and shorter length of stay, there were stark differences in the demographics of the patient population and in the interplay between occupancy rates of the ICU and the ward. The heterogeneity among the studies makes it challenging to draw definitive conclusions but highlights the importance of further prospective research in this area.
Proponents of DDH claim that its value lies in curtailing the volume of ward transfers, yielding both patient centered and system centered benefits. Patients who await ward transfer and experience transfer delays out of the ICU have the potential to suffer iatrogenic morbidity, including disturbances in sleep and delirium14,15 and increased risk of nosocomial infections.16 A recent multicenter study demonstrated that patients experiencing an ICU discharge delay of more than 6 h had longer hospital length of stay and were more likely to be discharged after hours.17 This increase in hospital length of stay may be the result of ward teams needing time to familiarize themselves with patients prior to hospital discharge. When faced with delays in ward transfer due to census issues, patients who could otherwise be discharged directly home from the ICU may be transferred to the wards after-hours. After-hours transfers from the ICU are well known to be associated with higher in-hospital mortality.18,19
Handover is known to be a high-risk period of patient care with the potential to cause adverse events.20,21 The transition of care from the ICU to the ward requires handover of a patient with a complex course from one care team to another. In some cases, opting to discharge a patient to home instead of conforming to historical transition-to-ward models can reduce the number of handovers and spare the patient undue morbidity.22,23 Based on Lau et al’s prospective study, ICU patients discharged directly to home had less unplanned return visits and readmission rates than those who were transferred to the ward and subsequently discharged within 24 h. A future trial randomizing ICU patient expected to need short ward stays to either DDH or ward transfer is required to definitively answer the question of which course is better for patient outcomes.
The practice of DDH can be a valuable tool in the management of ICU census and capacity. Several studies have shown a positive association between mortality and ICU occupancy rate.24–26 This phenomenon can be independent of patient acuity, as demonstrated by one study which showed that peak occupancy and the ratio of occupied to appropriately staffed beds were most strongly associated with mortality, even after controlling for acuity.27 These data suggest that DDH candidates awaiting ward beds can adversely affect the management of other ICU patients.
Chawla et al.’s study reported a 23.2% unplanned readmission rate, while Lau et al.’s study reported a 7.8% unplanned readmission rate in. The glaring difference in outcomes between these studies is a testament to the tremendous potential for DDH. These two studies highlight two contrasting cohorts: one is older, with an established diagnosis of malignancy, higher predicted mortality at ICU admission, and longer ICU length of stay; while the other is younger, with a lower predicted mortality at ICU admission, and a shorter ICU length of stay. We feel that the stark contrast in unplanned readmission rates between the two major studies demands further work in this area, in the form of a multi-center, randomized trial, and the derivation and validation of a prediction model to guide clinicians in their selection of patients that may be safely discharged directly home.
Current admission triage and discharge guidelines do not provide any recommendations on the practice of DDH,28 leaving clinicians to use their own judgment when planning the disposition of a critically ill patient. Discharge planning requires medication reconciliation, arrangement of home supports, and scheduling outpatient appointments as demonstrated in Chawla et al.’s study. We feel that the increasing rates of DDH should serve as a call to empower ICUs to develop the infrastructure required to discharge patients safely – which can include streamlining the discharge process for these complex individuals or to have pre-emptive ICU follow-up to mitigate bounce-backs. It also highlights that future research should evaluate the economic sequelae and the net effect this practice has on the healthcare system. Future direct discharge home guidelines would be well served by the incorporation of a randomized control trial, clinical prediction model, and economic analysis of DDH. This scientifically derived evidence could improve the confidence of ICUs who currently have much lower DDH rates than those in this review (9.9% over 12 years in Lau et al.’s study), empowering them to increase their DDH rates.
Conclusion
Our review identified four single center DDH studies, two of which drew upon the same prospectively enrolled cohort of patients. We confirm the scarcity of data describing the practice of DDH, describe benefits of the practice as well as some well-founded reservations, and suggest future avenues of research to better character should address clinical and economic outcomes associated with DDH in a prospective and multicenter fashion, as well as the development a clinical prediction model and clinical practice guidelines to better inform the safe practice of DDH.
Supplemental Material
Supplemental material for Lessons learned and new directions regarding Discharge Direct from Adult Intensive Care Units Sent Home (DISH): A narrative review by John Basmaji, Vincent Lau, Joyce Lam, Fran Priestap and Ian M Ball in Journal of the Intensive Care Society
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Lau VI, Priestap FA, Lam JN, et al. Factors associated with the increasing rates of discharges directly home from intensive care units – a direct from ICU sent home study. J Intensive Care Med 2018; 33: 121–127. [DOI] [PubMed] [Google Scholar]
- 2.Lam JNH, Lau VI, Priestap FA, et al. Patient, family and physician satisfaction with planning for direct discharge to home from intensive care units: direct from ICU sent home study. J Intensive Care Med. Epub ahead of print 1 January 2017. DOI: 10.1177/0885066617731263. [DOI] [PubMed]
- 3.Clini E, Vitacca M. From intermediate intensive care unit to home care. Monaldi Arch Chest Dis 1994; 49: 533–536. [PubMed] [Google Scholar]
- 4.Hayes N, Raine SF, Rushing P. Discharging ICU ventilator-dependent patients to home healthcare. Crit Care Nurse 1990; 10: 39–47. [PubMed] [Google Scholar]
- 5.Huang YC, Huang SJ, Ko WJ. Going home to die from surgical intensive care units. Intensive Care Med 2009; 35: 810–815. [DOI] [PubMed] [Google Scholar]
- 6.Ryder-Lewis M. Going home from ICU to die: a celebration of life. Nurs Crit Care 2005; 10: 116–121. [DOI] [PubMed] [Google Scholar]
- 7.Ba L, Zhang M, Su L, et al. Nine-year change of mortality and discharge against medical advice among major trauma patients in a Chinese intensive care unit. Eur J Trauma Emerg Surg 2016; 42: 47–53. [DOI] [PubMed] [Google Scholar]
- 8.Baptist AP, Warrier I, Arora R, et al. Hospitalized patients with asthma who leave against medical advice: characteristics, reasons and outcomes. J Allerg Clin Immunol 2007; 119: 924–929. [DOI] [PubMed] [Google Scholar]
- 9.Lusardi P, Jodka P, Stambovsky M, et al. The going home initiative: getting critical care patients home with hospice. Critical Care Nurse 2011; 31: 46–57. [DOI] [PubMed] [Google Scholar]
- 10.Coombs MA, Darlington AE, Long-Sutenhall T, et al. Transferring patients home to die: what is the potential population in UK critical care units? BMJ Support Palliat Care 2017; 7: 98–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipson AR, Kelley CG, Higgins PA, et al. ‘My mother’s leaving today?’: a pilot study on awareness of discharge date in the chronically critically ill. Medsurg Nurs 2006; 15: 8–12. [PMC free article] [PubMed] [Google Scholar]
- 12.Chawla S, D’Agostino RL, Pastores SM, et al. Homeward bound: an analysis of patients discharged home from an oncologic intensive care unit. J Crit Care 2012; 27: 681–687. [DOI] [PubMed] [Google Scholar]
- 13.Lau VI, Lam JNH, Basmaji J, et al. Survival and safety outcomes of ICU patients discharged directly home – a direct from ICU sent home study. Crit Care Med 2018. [DOI] [PubMed]
- 14.Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care 2008; 12: S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drouot X, Cabello B, d’Ortho MP, et al. Sleep in the intensive care unit. Sleep Med Rev 2008; 12: 391–403. [DOI] [PubMed] [Google Scholar]
- 16.Salgado CD, O’Grady N, Farr BM. Prevention and control of antimicrobial-resistant infections in intensive care patients. Crit Care Med 2005; 33: 2373–2382. [DOI] [PubMed] [Google Scholar]
- 17.Tirovoipati R, Botha J, Fletcher J, et al. Intensive care discharge delay is associated with increased hospital length of stay: a multicenter prospective observational study. PLoS One 2017; 12: e0181827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Priestap FA, Martin CM. Impact of intensive care unit discharge time on patient outcome. Crit Care Med 2006; 34: 2946–2951. [DOI] [PubMed] [Google Scholar]
- 19.Azevedo LC, de Souza IA, Zygun DA, et al. Association between nighttime discharge from the intensive care unit and hospital mortality: a multi-center retrospective cohort study. BMC Health Serv Res 2015; 15: 378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott M, Worrall-Carter L, Page K. Factors contributing to adverse events after ICU discharge: a survey of liaison nurses. Aust Crit Care 2013; 26: 76–80. [DOI] [PubMed] [Google Scholar]
- 21.Jones PB, Cherry RA, Allen BN, et al. Association between handover of anesthesia care and adverse postoperative outcomes among patients undergoing major surgery. JAMA 2018; 319: 143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peterson LA, Brennan TA, O’Neil AC, et al. Does house-staff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med 1994; 121: 866–872. [DOI] [PubMed] [Google Scholar]
- 23.Horwitz LI, Moin T, Krumholz HM, et al. Consequences of inadequate sign-out for patient care. Arch Intern Med 2008; 168: 1755–1760. [DOI] [PubMed] [Google Scholar]
- 24.Iapichino G, Gattinoni L, Radrizzani D, et al. Volume of activity and occupancy rate in intensive care units: association with mortality. Intensive Care Med 2004; 30: 290–297. [DOI] [PubMed] [Google Scholar]
- 25.Gabler NB, Ratcliffe SJ, Wager J, et al. Mortality among patients admitted to strained intensive care units. Am J Respir Crit Care Med 2013; 188: 800–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chrusch CA, Olafson KP, McMillan PM, et al. High occupancy increases the risk of early death or readmission after transfer from intensive care. Crit Care Med 2009; 37: 2753–2758. [DOI] [PubMed] [Google Scholar]
- 27.Tarnow-Mordi WO, Hau C, Warden A, et al. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet 2000; 356: 185–189. [DOI] [PubMed] [Google Scholar]
- 28.Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med 2016; 44: 1553–1602. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Lessons learned and new directions regarding Discharge Direct from Adult Intensive Care Units Sent Home (DISH): A narrative review by John Basmaji, Vincent Lau, Joyce Lam, Fran Priestap and Ian M Ball in Journal of the Intensive Care Society