Abstract
The use of medication to support patients and optimise outcomes is a fundamental strand of care. Pharmacists provide a key role managing medication within the complexity of various routes of administration, severe and rapidly shifting pharmacokinetic and dynamic parameters, and extremes of physiology in critical illness. Pharmacists intercept and resolve medication errors, optimise medication therapy and undertake broader professional activities within the job role that contribute to the smooth running of ICU. These activities are associated with improved quality, reduced mortality and reduced costs.
Keywords: Critical care, intensive care, job role, pharmacist
Introduction
The use of medication to support patients and optimise outcomes is a fundamental strand of care. The complexities posed by altered routes of administration, severe and rapidly shifting pharmacokinetic and dynamic parameters, combined with extremes of physiology in critical illness demand close scrutiny and careful management of drug therapy. Pharmacists provide a key role within the critical care multi-professional team in managing this aspect of therapy.
Training
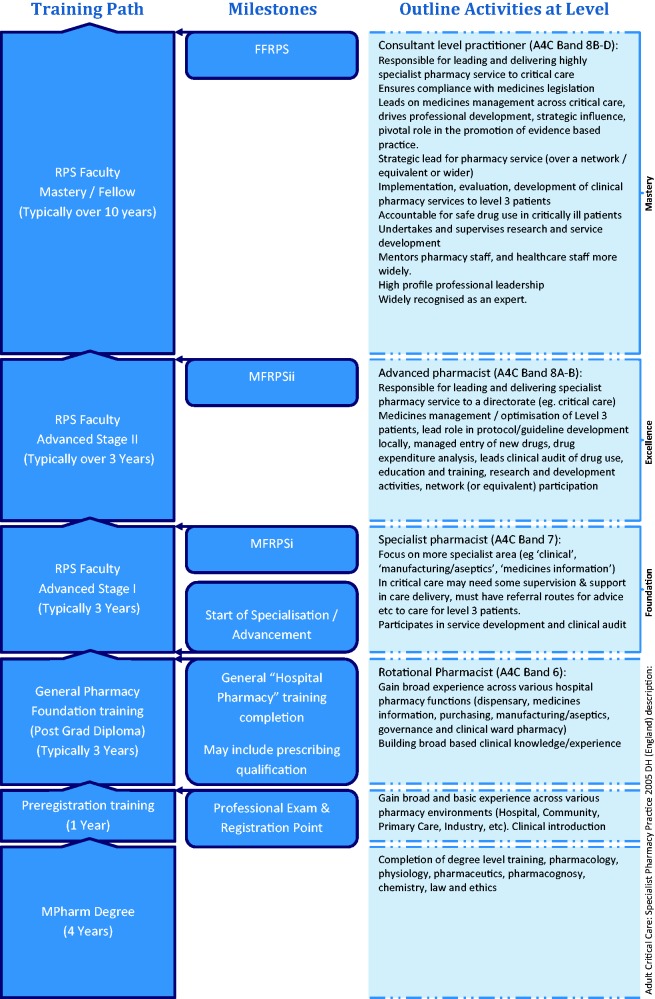
An overview of the training path in the United Kingdom (UK) is shown in Figure 1.1–3 Newly qualified pharmacists receive five years of training before examination and registration with the General Pharmaceutical Council, the majority enter community pharmacy with only 10–15% opting to go into hospital. Several years of foundation training are required to acquire experience across a broad range of pharmacy activities including fundamental clinical training, manufacturing (parenteral nutrition, chemotherapy, etc.), medicines information services, governance, medicines law, supply chain handling, formulary and patient services (dispensary, patient information hotlines, etc.). Hospital pharmacists then begin to major in specific aspects of practice with many concentrating on ward pharmacy over other activities such as aseptics or medicines information.
Figure 1.
An overview of pharmacists training path, milestones and professional activities at each level.
Those interested in progressing in critical care spend time in the area, link up with peers for support and advice, engage with the Royal Pharmaceutical Society’s (RPS) Faculty process and participate in education events such as those by the United Kingdom Clinical Pharmacy Association. A competency framework has been published,2 though the terminology used has recently changed with ‘Foundation level’ competencies now termed ‘Advanced Stage I’ within the RPS Faculty. This was to accommodate a new general pharmacy foundation framework for the first three years of practice, filling the gap between registration and commencement of advanced practice.
Several postgraduate general clinical pharmacy courses exist, but with variation in critical care components ranging from a few lectures to several-month clerkships/clinical attachments. Most advanced training is self-directed, with attainment of level of competence independently verified through the RPS Faculty system.1 Supporting systems such as face-to-face peer discussion, mentorship and work-based learning are practitioner development tools that need expansion and formalising to optimise the pharmacist’s skills.4 Some of this is required by the revalidation for pharmacy professionals process which formally starts in 2018.5
A high proportion of critical care pharmacists are also prescribers,6 and this is set to become a standard feature.7
Historical perspective
Pharmacists became involved in critical care in the USA starting in the 1960s followed by studies linking the role with improved outcomes and reduced costs.8 Sporadic involvement in the UK health system developed from ward pharmacy and PN/nutrition teams in the 1990s towards a more overt in-depth role formally described by the NHS Modernisation Agency in 2002.9 ‘Adult Critical Care: Specialist Pharmacy Practice’ was published by DH (England) in 2005 and very clearly articulated roles and responsibilities with a competency framework.2 The publication of ‘Core standards for intensive care units’ in 2013 and subsequent incorporation into ‘Guidelines for the Provision of Intensive Care Services’ in 2016 has further cemented this.10,11 Now clinical pharmacy services are expected to transform into 7/7 coverage for high-risk patients and have better integration into the multi-professional team.12 The Carter report in England 2016 called for more clinical pharmacists to be deployed on wards due to improved medicines optimisation and to serve the Getting-it-Right-First-Time agenda.7 Pharmacists can now be identified on 98.6% of critical care units across the United Kingdom.13
Current impact in critical care
Pharmacists see the entire casemix and so must manage the pharmaceutical care of an extreme range of health problems, as well as quickly assimilate information and management paths for conditions they may not have seen before. Frequently, this can mean making judgements about therapies where there is no evidence, where evidence is contradictory or where there are opposing therapeutic goals. Pharmacists are healthcare scientists and use their underpinning training to good effect in such circumstances.
Optimising medication is a central and key role expected of pharmacists in all clinical areas, not only in critical care.14 They intercept a large number of prescribing errors, the majority of which have potential for moderate to severe clinical impact. The error rate picked up in ICU runs at a slightly lower rate than in the wider hospital population (6.8% versus 7.5–8.9%), but in addition to this activity pharmacists provide high optimisation rates (8.3%).15–17 Clinical impact gradings of critical care pharmacist activity in terms of error intercepts and optimisation activity have been verified by a 30-strong multi-professional panel.18
Pharmacist’s activity can generally be grouped into three broad areas.13 First, the pharmacist’s independent review occurs when reviewing charts, clinical data, performing medicines reconciliation, etc. as a specific pharmacy activity that has grown out of the traditional ‘ward pharmacy’ model and undertaken in almost all UK ICUs.13
Second, there is active participation in the daily multidisciplinary team (MDT) round, where the pharmacist rounds with the team, the patients are reviewed and plans are drawn up for the day’s activities and for longer term planning. In a UK study, almost 60% of pharmacist’s contributions are made during the MDT round.16
The third main area is broadly grouped as ‘professional support activity’ and includes guideline development, formulary applications, governance and incident reviews, financial reporting and forecasting, teaching, audit and research. Many functions grouped under this unit wide activity are associated with reduced mortality in US hospitals and contribute to the smooth running of the ICU.19
The cost of employing a pharmacist at the recommended minimum staffing level is approximately £20 per patient per day. Several studies find that the role reduces overall expenditure through more efficient use of medicines and the avoidance of direct costs of iatrogenic harm, with additional savings made from avoiding payouts arising from damages claims.20–23 Recently, further cost reductions have been shown due to closer adherence to standardised care,24 and in the UK replacing an existing ‘ward pharmacy’ type service with embedded critical care trained pharmacists who attend the daily MDT round further reduced direct medicines costs by £17 per patient bed day (£175,275 per annum).25
Overall, pharmacists have been shown to improve the quality of critical care through medicines optimisation, medication error interception and greater regard to standardised therapy whilst reducing medication and care costs.
Future perspectives
Whilst pharmacists are increasingly embedded into critical care MDTs, significant challenges to the routine delivery of this proven resource exist. Many ICUs do not have pharmacists with the right experience level or who have the minimum required job time resulting in a poor or absent weekend pharmacy service, lack of attendance at ward round and impaired provision of good governance, guidelines, understanding of budgets and prescribing patterns.13 A national training programme is required to ensure we can meet the demand for advanced-level critical care pharmacists.26 Staffing models for delivery of true seven day services need further strategic development.
With greater availability comes an enhanced training capability around medicines accessible to all healthcare staff, be that for existing roles such as in medicine, nursing, physiotherapy, etc., or in evolving roles such as advanced critical care practitioners.
Pharmacy technicians (a regulated pharmacy profession) and assistants could be added to the critical care workforce. They will manage aspects of the medicines supply chain, logistics and provision of various kits (intubation, transfer bags, resus trolleys, etc.) and in so doing release nursing time back to doing actual critical care nursing. There are already pilots of pharmacy technicians preparing and administering medicines underway to reduce delayed and omitted doses, they may release nurse time back to other care activities.27,28 This could be extended to critical care where nursing time is at a premium and where high-risk medication preparation occurring at bed sides is common.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.The Royal Pharmaceutical Society. The RPS roadmap to advanced practice. London: Royal Pharmaceutical Society, 2016, pp.1–43.
- 2.Department of Health (England). Adult critical care specialist pharmacy practice. London: Department of Health (England), 2005.
- 3.Agenda for change: National profiles for pharmacy, http://www.nhsemployers.org/∼/media/Employers/Documents/Payandreward/Pharmacy.pdf (accessed 22 February 2018).
- 4.Warin RE, Bourne RS, Borthwick M, et al. Advanced level practice education: UK critical care pharmacists’ opinions in 2015. Pharmacy 2015; 4: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GPhC Council gives green light to implementation of revalidation in a ‘step-change’ for pharmacy professionals | General Pharmaceutical Council. General Pharmaceutical Council, https://www.pharmacyregulation.org/news/gphc-council-gives-green-light-implementation-revalidation-step-change-pharmacy-professionals (2017, accessed 22 February 2018).
- 6.Bourne RS, Whiting P, Brown LS, et al. Pharmacist independent prescribing in critical care: results of a national questionnaire to establish the 2014 UK position. Int J Pharm Pract 2016; 24: 104–113. [DOI] [PubMed] [Google Scholar]
- 7.Lord Carter of Coles. Operational productivity and performance in English NHS acute hospitals: unwarranted variations. London: Department of Health (England), 2016.
- 8.Chant C, Dewhurst NF, Friedrich JO. Do we need a pharmacist in the ICU? Intensive Care Med 2015; 41: 1314–1320. [DOI] [PubMed] [Google Scholar]
- 9.NHS Modernisation Agency. Critical care programme: AHP and HCS Advisory Group. The role of healthcare professionals within critical care services. London: NHS Modernisation Agency, 2002.
- 10.Faculty of Intensive Care Medicine & Intensive Care Society. Core standards for intensive care units. London: Faculty of Intensive Care Medicine/ Intensive Care Society, 2013.
- 11.Faculty of Intensive Care Medicine & Intensive Care Society. Guidelines for the provision of intensive care services Ed1.1. London: Faculty of Intensive Care Medicine / Intensive Care Society, 2016.
- 12.Department of Health (England). Transformation of seven day clinical pharmacy services in acute hospitals. London: Department of Health (England), 2016.
- 13.Borthwick M, Barton G, Bourne RS, et al. Critical care pharmacy workforce: UK deployment and characteristics in 2015. Int J Pharm Pract. 2018; 26: 325–333. [DOI] [PubMed]
- 14.National Institute for Health and Care Excellence. Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes. London: NG5, 2015. [PubMed]
- 15.Dornan T, Ashcroft D, Heathfield H, et al. An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education: EQUIP study. London: General Medical Council, https://www.gmc-uk.org/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf (accessed 22 February 2018).
- 16.Shulman R, McKenzie CA, Landa J, et al. Pharmacist’s review and outcomes: treatment-enhancing contributions tallied, evaluated, and documented (PROTECTED-UK). J Crit Care 2015; 30: 808–813. [DOI] [PubMed] [Google Scholar]
- 17.Ryan C, Ross S, Davey, et al. Prevalence and causes of prescribing errors: the PRescribing Outcomes for Trainee Doctors Engaged in Clinical Training (PROTECT) study. PLoS One 2014; 9: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bourne RS, Shulman R, Tomlin M, et al. Reliability of clinical impact grading by healthcare professionals of common prescribing error and optimisation cases in critical care patients. Int J Qual Health Care 2017; 29: 250–255. [DOI] [PubMed] [Google Scholar]
- 19.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy 2007; 27: 481–493. [DOI] [PubMed] [Google Scholar]
- 20.Kopp BJ, Mrsan M, Erstad BL, et al. Cost implications of and potential adverse events prevented by interventions of a critical care pharmacist. Am J Health Syst Pharm 2007; 64: 2483–2487. [DOI] [PubMed] [Google Scholar]
- 21.Michalets E, Creger J, Shillinglaw WR. Outcomes of expanded use of clinical pharmacist practitioners in addition to team-based care in a community health system intensive care unit. Am J Health Syst Pharm 2015; 72: 47–53. [DOI] [PubMed] [Google Scholar]
- 22.MacLaren R, Bond CA, Martin SJ, et al. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infections. Crit Care Med 2008; 36: 3184–3189. [DOI] [PubMed] [Google Scholar]
- 23.Louzon P, Jennings H, Ali M, et al. Impact of pharmacist management of pain, agitation, and delirium in the intensive care unit through participation in multidisciplinary bundle rounds. Am J Health Syst Pharm 2017; 74: 253–262. [DOI] [PubMed] [Google Scholar]
- 24.Leguelinel-Blache G, et al. Impact of quality bundle enforcement by a critical care pharmacist on patient outcome and costs. Crit Care Med 2018; 46: 199–207. [DOI] [PubMed] [Google Scholar]
- 25.Parker J, Clymer M, Owen O, et al. Poster 15: inclusion of specialist critical care pharmacists to the multidisciplinary team on an adult cardiac critical care unit significantly reduces drug expenditure. In: Association of cardiothoracic anaesthesia and critical care annual scientific meeting, Birmingham, UK, 2017.
- 26.Seneviratne RE, Bradbury H and Bourne RS. How do pharmacists develop into advanced level practitioners? Learning from the experiences of critical care pharmacists. Pharmacy 2017; 5: 38. [DOI] [PMC free article] [PubMed]
- 27.Keers RN, Seston E, Kontopantelis E, et al. Evaluation of pharmacy TECHnician supported MEDication administration rounds (TECHMED) on reducing omitted doses: a pilot randomised controlled trial and process evaluation in a university teaching hospital, http://pharmacyresearchuk.org/wp-content/uploads/2017/01/CPRG2-TECHMED-final-report-v3.pdf (2017, accessed 22 February 2018).
- 28.Langham JM, Boggs KS. The effect of a ward-based pharmacy technician service. Pharm J 2000; 264: 961–963. [Google Scholar]