Abstract
Background
As adolescents gain autonomy, it remains important for parents to be involved with diabetes management to avoid deterioration in glycemic control. Technologies for self-monitoring of blood glucose (SMBG) allow for remote monitoring in real-time by parents. This research compared three strategies for improving SMBG and diabetes self-care in the short-term. These strategies were: (1) health information technology (HIT)-enhanced blood glucose meter that shared blood glucose data among patients, their parent, and care providers, and allowed for text messaging; (2) family-centered goal setting; and (3) a combination of (1) and (2).
Methods
One hundred twenty-eight participants enrolled; 97 adolescent-parent pairs attended clinic at 3-month intervals during the 6-month intervention. Differences between treatment groups were evaluated using ANOVAs for continuous variables and chi-squared tests for frequencies. Within patient changes were evaluated using paired t-tests.
Results
Participants in the HIT-enhanced SMBG group had no change in mean HbA1c. Participants assigned to family-centered goal setting had a non-significant decrease in HbA1c of −0.3% (p = 0.26) from baseline to 6-months. Participants in the combined approach had a significant decrease in HbA1c of −0.6% (p = 0.02) from baseline to 3-months, but the decrease of −0.4% at 6-months was non-significant (p = 0.51). The change in HbA1c from baseline to 3-months was greater for the combined approach than for the HIT-enhanced SMBG (p = 0.05) or family-centered goal setting (p = 0.01).
Conclusions
Our data suggest that utilizing the family-centered goal setting strategy when implementing HIT-enhanced diabetes technology deserves further study.
Keywords: Type 1 Diabetes Mellitus, Patient-Centered Care, Self-Care, Blood Glucose Self-Monitoring, Adherence
Introduction
Technologies for managing type 1 diabetes (T1D) continue to evolve, yet the majority of adolescent youth with T1D have glycosylated hemoglobin (HbA1c) values above the recommended range.(1) A principal challenge of intensive diabetes self-care is maintaining frequent self-monitoring of blood glucose (SMBG). Health information technology (HIT) currently allows real-time sharing of SMBG between patient and parents, and messaging between patient, parents, and health care providers. This has the potential to improve reactive and proactive blood glucose management, provide real-time adherence support, and promote intensification of treatment. However, whether this technology will improve clinical outcomes among adolescents is unclear. Moreover, interventions that focus on improving clinical outcomes via increasing SMBG in adolescents, but ignore family-centered goals and conflict are less likely to succeed.(2–4) Few interventions have addressed both HIT-enhanced SMBG and family-centered goals.
We designed an intervention that combines mobile HIT-enhanced SMBG, messaging, and a clinic-based family-centered goal setting strategy to address patient-centered diabetes self-care and family-centered goals simultaneously. The objective of this research was to compare three strategies for improving SMBG and diabetes self-care in the short-term (6-months). These strategies were: (1) a HIT-enhanced blood glucose meter that both shared blood glucose data among patients, their parent, and health care providers, and allowed for text messaging; (2) family-centered goal setting; and (3) a combination of (1) and (2). We hypothesized that the combination therapy would lead to superior outcomes.
Methods
The study was performed at a tertiary care academic medical center, was approved by the University’s Institutional Review Board, and all participants signed informed consent/assent prior to engaging in study procedures. Inclusion criteria required age 12–18 years for youth, T1D diagnosed for at least 6 months, and a parent or guardian who agreed to participate. Exclusion criteria included diagnoses of other chronic diseases except controlled asthma, treated thyroid disease, or depression treated with a stable dose of medication. Participants also could not be using continuous glucose monitoring systems.
After enrollment, participants entered a three-month run-in period of routine diabetes care in an adolescent diabetes clinic without being assigned to a specific intervention strategy to establish baseline characteristics. A single diabetes care provider (a board certified pediatric endocrinologist) and a certified diabetes educator/nurse practitioner (CDE, CNP) provided American Diabetes Association endorsed care recommendations during the 3-month run-in period. Participants were randomized using block randomization, stratifying by sex, in a 1:1:1 ratio to one of three treatment strategies. This study design allowed for the measurement of longitudinal change in outcomes in individuals by treatment (patients serving as their own controls) and between treatment groups.
Interventions
HIT-enhanced SMBG strategy –
Adolescents and their parents were oriented to the Telcare System (Concord, MA, https://telcare.com) for SMBG, and received a meter and testing supplies for the duration of the study. The Telcare System allows real-time SMBG data monitoring for the patient, their parents, and their healthcare provider by automatically transmitting SMBG data to a secure, online, HIPPA-compliant web portal via cellular data networks. Both pre-set and free-text alerts can be sent to any cell phone in real time when SMBG is performed. Participants randomized to this strategy were encouraged to use the Telcare blood glucose meter for the duration of the study, regardless of their mode of insulin delivery. The study CDE, CNP reviewed all SMBG data weekly. Participants were sent messages by phone or by direct messaging via the Telcare system with care recommendations. If possible, telephone or text message contact was made directly with the adolescent participant.
Family-centered goal setting strategy –
Adolescent-parent pairs randomized to this approach met with a health educator, in addition to a CDE, and a board certified pediatric endocrinologist at the randomization visit and the 3 month follow-up visit for approximately 30 minutes. Family-centered goals were discussed and ultimately chosen utilizing motivational interviewing techniques taking into account the child’s age, maturity level, and desires of both the adolescent and the parent. We utilized a goal-setting tool specifically designed for this study (Appendix). Suggested categories of goals to address were: 1) frequency of SMBG, 2) giving bolus insulin according to diabetes care team recommendations, 3) self-adjustment of insulin, 4) parental nagging and oversight, and 5) frequency of contact with the diabetes care team.
Combined approach –
This intervention arm received both the HIT-enhanced SMBG strategy and the family-centered goal setting strategy.
Data Analysis
The sample size estimation for this pilot study was based on the primary outcome of interest, change in HbA1c at 6 months from baseline. The mean number of SMBG tests by treatment group at baseline, 3-month, and 6-month time points were secondary outcomes. For evaluation of the longitudinal change in outcomes measures in individuals by treatment we had over 90% power to detect a HbA1c difference of 0.5 ± 0.8% from baseline to 6 months among individuals (paired-T test, α=0.05). For evaluation of treatment group differences for the 3 treatment arms we had 80% power to detect a HbA1c difference of 0.5 ± 0.5% (one-way ANOVA, α=0.05). We modeled the longitudinal changes in HbA1c and frequency of SMBG at 6 months from baseline. Differences between treatment groups were evaluated using ANOVAs for continuous variables, and chi-squared tests for frequencies. Changes within patients over time were evaluated using paired t-tests.
Results
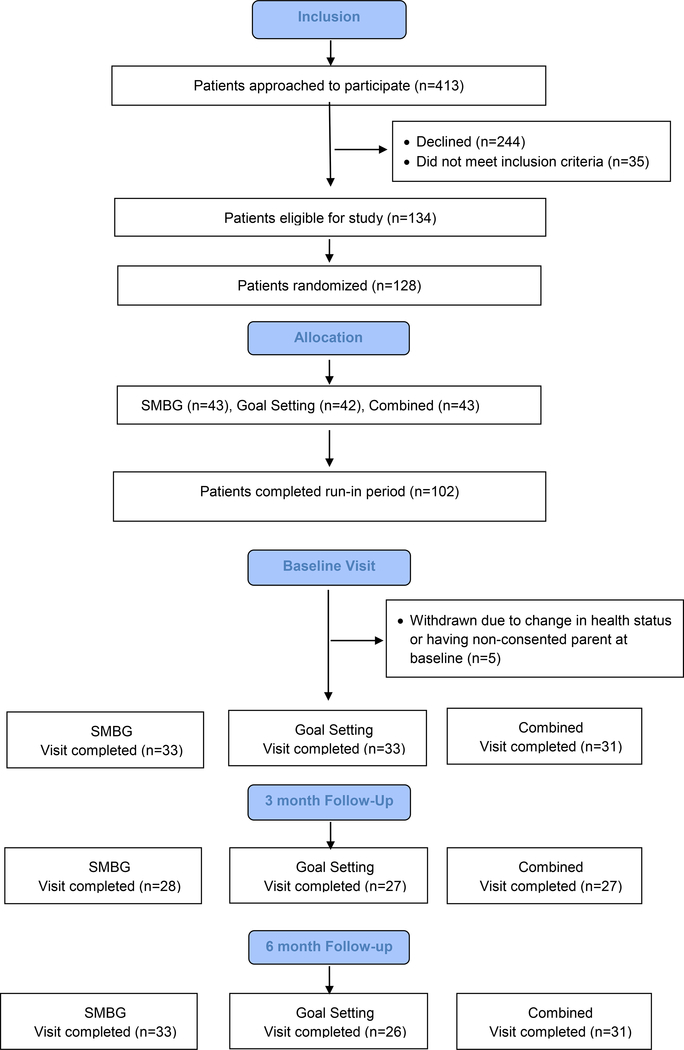
One hundred twenty-eight participants enrolled; 102 completed run-in and presented for randomization. Five participants were withdrawn at the baseline visit due to not having the consenting parent/guardian with them, or due to a change in health/treatment status. Ninety-seven participants completed the baseline visit following the 3-month run-in. Adolescents and parents attended clinic at 3-month intervals during the 6-month intervention (Figure 1).
Figure 1.
CONSORT Flow Diagram
Baseline characteristics of these participants are shown in Table 1. There were equal numbers of males and females; the study population was predominately white, non-Hispanic. Intervention groups were similar for age, sex, and race/ethnicity. Despite randomization, the mean HbA1c at baseline for the combined approach participants was higher than the other groups (10.1 ± 2.1% versus 9.0 ± 1.6% and 9.0 ± 1.9% in the HIT-enhanced SMBG and family-centered goal setting groups, p=0.03) even though the HbA1c was similar for all groups prior to run-in.
Table 1.
Participant Characteristics
| HIT-enhanced SMBG | Family-Centered Goal Setting | Combined Approach | p-value | |
|---|---|---|---|---|
| Participants, n (%) | 33 (34.0%) | 33 (34.0%) | 31 (32.0%) | |
| Age, years (SD) | 14.5 (1.7) | 14.7 (1.5) | 14.7 (2.0) | 0.69 |
| Sex | 0.96 | |||
| Female | 17 (51.5%) | 16 (48.5%) | 15 (48.4%) | |
| Male | 16 (48.5%) | 17 (51.5%) | 16 (51.6%) | |
| Race / Ethnicity | 0.65 | |||
| Asian | 0 (0%) | 1 (3.0%) | 0 (0%) | |
| Black | 3 (9.1%) | 2 (6.1%) | 3 (9.7%) | |
| White | 29 (87.9%) | 28 (84.9%) | 23 (74.2%) | |
| More than one race | 0 (0%) | 1 (3.0%) | 2 (6.4%) | |
| Hispanic or Latino | 1 (3.0%) | 1 (3.1%) | 3 (9.7%) | |
| HbA1c at Consent (beginning of run-in), % (SD) | 8.9 (1.9) | 9.0 (1.8) | 8.9 (1.5) | 0.96 |
| HbA1c at Baseline Visit, % (SD) | 9.0 (1.6) | 9.0 (1.9) | 10.1 (2.1) | 0.03 |
| Mode of Treatment - Pump | 11 (33.3%) | 12 (36.4%) | 8 (25.8%) | 0.65 |
| Time Since Diagnosis, years (SD) | 5.8 (3.8) | 5.0 (3.5) | 6.1 (4.2) | 0.77 |
| Time Since Diagnosis > 1 year | 32 (97.0%) | 32 (97.0%) | 29 (93.6%) | 0.69 |
The mean HbA1c by treatment group at baseline, 3-month, and 6-month time points are shown in Table 2. Participants in the group assigned to HIT-enhanced SMBG had no change in mean HbA1c over the course of the intervention. Participants in the group assigned to family-centered goal setting had a non-significant decrease in HbA1c of −0.3% (p = 0.26) from baseline to 6-months. Participants in the combined approach had a significant decrease in HbA1c of −0.6% (p = 0.02) from baseline to 3-months, but the decrease of −0.4% at 6-months was non-significant (p = 0.51).
Table 2.
HbA1c and Frequency of SMBG by treatment at baseline, 3-mo, and 6-mo time points*
| Treatment | HbA1c pre run-in (%) | HbA1c (%) Baseline | HbA1c (%) 3 mo | HbA1c (%) 6 mo |
| HIT-enhanced SMBG | 8.9 ± 1.9 (33) | 9.0 ± 1.6 (33) | 9.0 ± 1.6 (28) | 9.0 ± 2.0 (33) |
| Family-centered goal setting | 9.0 ± 1.8 (33) | 9.0 ± 1.9 (33) | 9.0 ± 1.9 (27) | 8.7 ± 1.8 (26) |
| Combined approach | 8.9 ± 1.5 (31) | 10.1 ± 2.1 (31) | 9.5 ± 1.8 (27)** | 9.7 ± 1.9 (31) |
| Treatment | Tests/day Baseline | Tests/day 3 mo | Tests/day 6 mo | |
| HIT-enhanced SMBG | 3.6 ± 1.9 (29) | 3.0 ± 1.3 (26) | 2.9 ± 1.3 (29) | |
| Family-centered goal setting | 4.0 ± 1.9 (31) | 3.5 ± 1.9 (23) | 4.1 ± 2.5 (21) | |
| Combined approach | 3.2 ± 1.8 (28) | 3.2 ± 1.7 (27) | 2.7 ± 1.3 (29) | |
Data are means ± SD (n)
p = 0.02 for change from baseline to 3 months
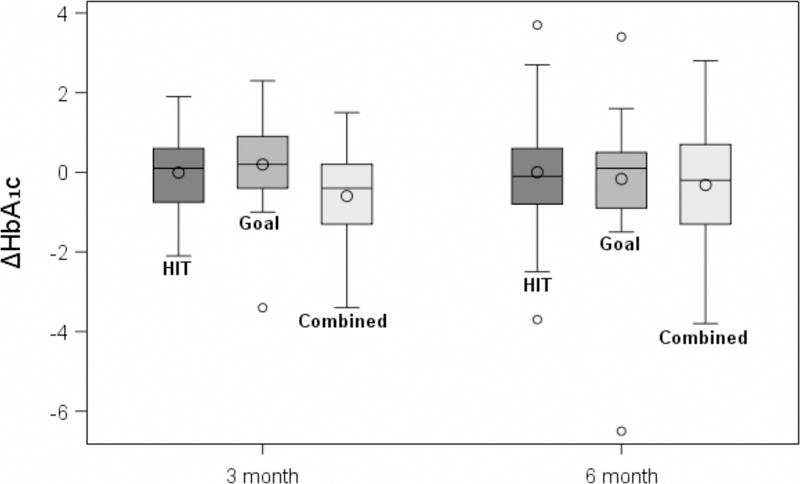
The change in HbA1c from baseline to 3-months was greater for the combined approach than for the HIT-enhanced SMBG (p = 0.05) or family-centered goal setting (p = 0.01) (Figure 2). However, when this was adjusted for baseline HbA1c, there was no significant difference in change in HbA1c between the groups at 3 months (combined approach versus HIT-enhanced SMBG, p = 0.26; combined approach versus family centered goal setting, p = 0.09). There were no significant group differences in change in HbA1c from baseline to 6 months (Figure 2).
Figure 2.
Change in HbA1c from baseline to three months and six months for the three arms.
The mean number of SMBG tests by treatment group at baseline, 3-month, and 6-month time points are shown in Table 2. There was no significant change in the mean number of SMBG tests during the intervention in any of the groups, and no group differences in change in SMBG over time. Participants verbally endorsed not having the meter charged at all times, and loss of cellular signal in some areas that interrupted data sharing.
Characteristics of participants with an HbA1c decrease of at least 0.5%, compared with those with no improvement, are shown in Table 3. Higher levels of HbA1c prior to beginning run-in and at the baseline visit were associated with an improvement in HbA1c at the 6-month time point.
Table 3.
Characteristics of Participants with Improved HbA1c* at 6-months
| Did Not Improve | Improved | p-value | |
|---|---|---|---|
| Participants, n (%) | 57 (63.3%) | 33 (36.7%) | |
| Treatment | |||
| HIT-enhanced SMBG | 22 (38.6%) | 11 (33.3%) | |
| Family-Centered Goal Setting | 16 (28.1%) | 10 (30.3%) | |
| Combined Approach | 19 (33.3%) | 12 (36.4%) | 0.88 |
| Age, years (SD) | 14.6 (1.8) | 14.5 (1.7) | 0.79 |
| Sex | 0.54 | ||
| Female | 28 (49.1%) | 14 (42.4%) | |
| Male | 29 (50.9%) | 19 (57.6%) | |
| Race / Ethnicity | 0.42 | ||
| Asian | 1 (1.8%) | 0 (0%) | |
| Black | 6 (10.5%) | 1 (3.0%) | |
| White | 46 (80.7%) | 29 (87.9%) | |
| More than one race | 2 (3.5%) | 0 (0%) | |
| Hispanic or Latino | 2 (3.5%) | 3 (9.1%) | |
| HbA1c at Consent (beginning of run-in), % (SD) | 8.6 (1.7) | 9.4 (1.6) | 0.04 |
| HbA1c at Baseline Visit, % (SD) | 8.9 (1.6) | 10.1 (2.3) | 0.003 |
| Mode of Treatment - Pump | 21 (36.8%) | 9 (27.3%) | 0.35 |
| Time Since Diagnosis, years (SD) | 5.8 (4.0) | 5.2 (3.6) | 0.50 |
| Time Since Diagnosis > 1 year | 54 (94.7%) | 32 (97.0%) | 1.0 |
HbA1c decreased by at least 0.5%
Discussion
In this study, we compared three pragmatic strategies for improving SMBG in adolescents: a) an HIT-enhanced SMBG strategy that utilized shared blood glucose records among patients, their parent, and health care providers and provided feedback via text messaging; b) a family-centered goal setting strategy; and c) a combination of both strategies. We found that assigning the use of HIT-enhanced SMBG alone resulted in no change in HbA1c over time at 3 or 6 months. Combining HIT-enhanced SMBG with family-centered goal setting led to superior 3-month outcomes. However, this was complicated by the fact that participants in this arm had higher HbA1cs to begin with and so regression to the mean may have played a role in reducing the HbA1c. Nevertheless, we included a 3-month run-in period to account for this potential. We anticipated that HbA1cs might improve in patients who agreed to participate in a clinical trial, even without a specific intervention, and all three groups were therefore exposed to a 3-month run-in.
Some prospective cohort studies using HIT-enhanced SMBG and text messaging (5) or multimedia and text messaging alone (6) have shown improvement in glycemic control in adolescent youth. However, other prospective cohort studies using mobile applications with mobile health technology +/− text messaging have shown no significant improvement in glycemic control.(7–10) There have been few randomized-controlled trials of the use of mobile technology in adolescents and these trials have measured very short-term outcomes (less than 3 months). Berndt et al. evaluated a mobile diabetes management system with connectivity to health care providers (n=68).(11) After 4 weeks, patients using the system had lower mean HbA1c compared with baseline, but there was not a difference between intervention and control group outcomes. Markowitz et al. used text messaging to send tailored reminders and motivational messages to patients (n=90) and found no difference in change in HbA1c after 4 weeks between intervention and control patients.(12) A previous study using HIT-enhanced SMBG in adolescents has also shown no superiority to using a traditional glucose meter for HbA1c or mean daily SMBG measures.(13)
In the case of assignment to the HIT-enhanced SMBG intervention in our study, some caregivers verbally expressed feelings of relief that someone else would be looking at the SMBG values and texting the child, without action on their part. This might have influenced the outcomes of patients assigned to the HIT-enhanced SMBG intervention alone. Additionally, verbal feedback from adolescents included that they did not like frequently charging the blood glucose meter, and this played a role in declining frequency of SMBG when using the HIT-enhanced SMBG system.
Family conflict around diabetes self-care and SMBG commonly occurs when adolescents fail to meet parental expectations or vice versa. Hilliard et al. reported that higher adolescent-reported family conflict is negatively associated with both mean daily SBMG and HbA1c among adolescents.(3) We hypothesized that a clinic-based intervention to identify short-term goals for both the patient and the parent, and putting these into a written plan would allow for a two-way street for prioritizing patient- and family-centered objectives. Self-Determination Theory predicts autonomous reasons for engaging in a behavior lead to more outcomes that are positive.(14) Thus, each adolescent-parent pair developed autonomous and family-centered goals. This process has the potential to help parents and adolescents better deal with the two conflicting sets of tasks referred to in the miscarried helping model: (1) parents taking responsibility for management and adolescent feeling “controlled”, and (2) parents helping their child take developmentally appropriate steps in managing their own health.(15, 16) We found that this intervention alone did not lead to significant improvement in HbA1c at 3 or 6 months. We suspect that ongoing family goal-setting would be beneficial, and family-based counseling is necessary to impact diabetes control in adolescent youth when family conflict is significant.
Strengths of this study include the randomized-controlled prospective design and the 3-month run-in period. We included a run-in to try to negate the positive effect that participation in a clinical trial can have on HbA1c, regardless of the intervention. The comparative-effectiveness nature of the trial, performed in a real-world clinic based setting is a strength. Weaknesses of the study include being underpowered for some of the analyses comparing group differences. The sample size estimation for the study was based on change in HbA1c at 6 months with patients serving as their own controls. We were not able to tailor automatic text-messages to youth using the Telcare System and so a person (CDE, CNP) was required to individualize recommendations based on SMBG readings. Moreover, feedback on SMBG was not given immediately by health care providers due to lack of personnel and resources. The family-centered goal setting intervention likely would have benefitted from a clinical psychologist in the clinic setting to provide family-centered therapy when needed, but resources were inadequate to provide this option.
In conclusion, our data support that utilizing the family-centered goal setting strategy when implementing HIT-enhanced diabetes technology deserves further study. It may be particularly useful in patients with higher levels of HbA1c. Family-centered goal setting and family counseling could be useful when adolescents are adopting new technology to get optimal clinical results.
Acknowledgements
This research was funded by Agency for Healthcare Research and Quality, Grant 5R24HS022434-05.
Study data were collected and managed using REDCap electronic data capture tools hosted at the Indiana Clinical and Translational Sciences Institute (Indiana CTSI) funded, in part by Grant Numbers UL1TR001108, KL2TR001106, or TL1TR001107 from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award and at the Indiana University Pervasive Technology Institute (https://pti.iu.edu/) which supports REDCap with IT infrastructure and consulting resources. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.
We thank the Pediatric Research Network (PresNet) at Indiana University (Cathy Luthman, Elaine Cuevas, Jen Stanton-Tully, Vicki Cater, Ann Clark and Whitney Fishburn) for assistance with data collection, project management, and data management.
Contributor Information
Tamara S. Hannon, Indiana University School of Medicine, Department of Pediatrics, 410 W. 10th Street, Suite 2000A, Indianapolis, IN 46202
Lisa G. Yazel-Smith, Indiana University School of Medicine, Section of Pediatric and Adolescent Comparative Effectiveness Research, 410 W. 10th Street, Suite 2000A, Indianapolis, IN 46202.
Amy S. Hatton, Riley Hospital for Children, 705 Riley Hospital Dr. Rm. 3039, Indianapolis, IN 46202.
Jennifer L. Stanton, Indiana University School of Medicine, Indiana Children’s Health Services Research, 410 W. 10th Street, Suite 2000, Indianapolis, IN 46202.
Elizabeth A. S. Moser, Indiana University School of Medicine, Richard M. Fairbanks School of Public Health, Department of Biostatistics, 410 W. 10th Street, Suite 3000, Indianapolis, IN 46202
Xiaochun Li, Indiana University Purdue University Indianapolis, Richard M. Fairbanks School of Public Health, Department of Biostatistics, 410 W. 10th Street, Suite 3000, Indianapolis, IN 46202
Aaron E. Carroll, Indiana University School of Medicine, Department of Pediatrics, Section of Pediatric and Adolescent Comparative Effectiveness Research, 410 W. 10th Street, Suite 2000A, Indianapolis, IN 46202
References
- 1.Pihoker C, et al. (2013) Insulin regimens and clinical outcomes in a type 1 diabetes cohort: the SEARCH for Diabetes in Youth study. Diabetes care 36(1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carroll AE, DiMeglio LA, Stein S, & Marrero DG (2011) Contracting and monitoring relationships for adolescents with type 1 diabetes: a pilot study. Diabetes technology & therapeutics 13(5):543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hilliard ME, Guilfoyle SM, Dolan LM, & Hood KK (2011) Prediction of adolescents’ glycemic control 1 year after diabetes-specific family conflict: the mediating role of blood glucose monitoring adherence. Archives of pediatrics & adolescent medicine 165(7):624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingerski LM, Anderson BJ, Dolan LM, & Hood KK (2010) Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 47(2):191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carroll AE, DiMeglio LA, Stein S, & Marrero DG (2011) Using a cell phone-based glucose monitoring system for adolescent diabetes management. The Diabetes educator 37(1):59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bin-Abbas B, Jabbari M, Al-Fares A, El-Dali A, & Al-Orifi F (2014) Effect of mobile phone short text messages on glycaemic control in children with type 1 diabetes. Journal of telemedicine and telecare 20(3):153–156. [DOI] [PubMed] [Google Scholar]
- 7.Cafazzo JA, Casselman M, Hamming N, Katzman DK, & Palmert MR (2012) Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. Journal of medical Internet research 14(3):e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Froisland DH, Arsand E, & Skarderud F (2012) Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. Journal of medical Internet research 14(4):e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hanauer DA, Wentzell K, Laffel N, & Laffel LM (2009) Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes technology & therapeutics 11(2):99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mulvaney SA, Rothman RL, Wallston KA, Lybarger C, & Dietrich MS (2010) An internet-based program to improve self-management in adolescents with type 1 diabetes. Diabetes care 33(3):602–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berndt RD, et al. (2014) Impact of information technology on the therapy of type-1 diabetes: a case study of children and adolescents in Germany. Journal of personalized medicine 4(2):200–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Markowitz JT, et al. (2014) Text messaging intervention for teens and young adults with diabetes. Journal of diabetes science and technology 8(5):1029–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Bartolo P, et al. (2017) Young patients with type 1 diabetes poorly controlled and poorly compliant with self-monitoring of blood glucose: can technology help? Results of the i-NewTrend randomized clinical trial. Acta diabetologica 54(4):393–402. [DOI] [PubMed] [Google Scholar]
- 14.Ryan RM & Deci EL (2000) Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. The American psychologist 55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 15.Anderson BJ, Auslander WF, Jung KC, Miller JP, & Santiago JV (1990) Assessing family sharing of diabetes responsibilities. Journal of pediatric psychology 15(4):477–492. [DOI] [PubMed] [Google Scholar]
- 16.Anderson BJ, Brackett J, Ho J, & Laffel LM (1999) An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes care 22(5):713–721. [DOI] [PubMed] [Google Scholar]