Abstract
Objective
To test the null hypothesis that there is no difference in patient cost savings between the telemedicine and traditional face‐to‐face approach. The second objective was to assess the financial impact on the peripheral healthcare system, as compared with staffing a conventional clinic with “on‐site” otolaryngologist.
Methods
Twenty‐one patients were enrolled. To assess “patient‐benefit” cost savings, a model was formulated that would utilize a certified nurse practitioner (CNP) to conduct a general otolaryngology clinic at the peripheral site, as compared with having to travel to the tertiary referral center. A “peripheral site‐benefit” cost analysis was performed to assess costs of initiating and operating a telemedicine clinic at the peripheral site, compared with having an on‐site otolaryngologist.
Results
The total patient‐benefit cost savings would be $182.09 per patient per encounter and $333.22 per patient annually. The fixed cost to the peripheral site to initiate the telemedicine system was $9,895. Two hundred sixty telemedicine encounters would be needed to offset the initial cost, and 537 encounters would be needed to surpass revenue of the conventional clinic.
Conclusion
A real‐time telemedicine otolaryngology clinic provides significant cost savings for both patients and the peripheral healthcare system. This pilot study supports telemedicine as a cost‐effective approach to providing general otolaryngology care to rural patients.
Level of Evidence
4
Keywords: Telemedicine, TeleENT, cost savings, cost‐benefit, cost analysis
INTRODUCTION
The need to improve otolaryngology access in rural settings is pressing. Most otolaryngologists (61.8%) are located in large metropolitan cities.1 However, these cities are home to only 55.3% of the total US population, indicating that otolaryngologists are over‐represented in urban areas and under‐represented in rural areas.1 Otolaryngologists are also more likely to be present in areas with a higher mean socioeconomic status.2 Patients in rural regions face two financial barriers to adequate care: high travel costs related to travelling long distances to obtain otolaryngology services, and time missed from work, often consisting of an entire workday for patients referred to our tertiary care center.
Peripheral medical centers are faced with significant challenges to provide more accessible otolaryngology services to patients in rural settings. Some centers attempt to hire their own full‐time otolaryngologist locally, which can be expensive for the peripheral site in rural areas. A second approach is to set up a conventional “on‐site” otolaryngology clinic that is run by a consulting otolaryngologist who travels to and from a private practice or tertiary referral center. This approach has limitations: the peripheral medical center must pay a premium to incentivize the otolaryngologist to travel to their site.
An alternative solution for rural healthcare centers is the use of real‐time telemedicine. Telemedicine is defined as the use of telecommunication technology to provide remote access to patient care.3 Telemedicine models are characterized in two forms: store‐and‐forward (asynchronous) versus real‐time (synchronous). Store‐and‐forward telemedicine requires health care providers to collect relevant data (eg, lab results, photo documentation, and radiology studies) and forward it to the consulting physician, who later reviews the data. In contrast, real‐time telemedicine is live and interactive, and most closely mimics a real‐life encounter between doctor and patient.
Telemedicine has been well‐established in certain fields that may be more amenable to the format, including radiology, ophthalmology, cardiology, dermatology, and psychiatry, but telemedicine applications have been adopted slowly in otolaryngology.3 Although the cornerstone of diagnostics remains history‐taking and detailed physical exam, otolaryngology also relies on objective sources including tympanograms, audiograms, lab results, diagnostic imaging, and endoscopy making it particularly suitable for telemedicine.3 Since most endoscopic and otoscopic images can be digitized, the clinical evaluation of the otolaryngology patient in the telemedicine clinic setting is highly feasible.4
Few studies have evaluated the financial ramifications of using a real‐time telemedicine format to evaluate patients in otolaryngology. However, previous reports estimate that otolaryngology telemedicine programs have saved $48 to $401 per patient per consultation.5, 6, 7, 8 These overall cost savings have taken into consideration the benefits to the patient from decreased travel and lost work time, but also the benefits to the peripheral healthcare system after accounting for costs required to initiate the telemedicine system, which includes equipment purchase, maintenance, and operating expenses. However, variability exists in cost savings between telemedicine systems, which may be attributable to differences in location, type of telemedicine format (real‐time vs. store‐and‐forward), services provided, equipment used, and assigned values for cost predictions. Thus, further data is needed to specifically evaluate the cost savings of a real‐time otolaryngology telemedicine clinic for a given region, both for patients and for the peripheral healthcare system.
The objective of this study was to perform a cost analysis of a real‐time general otolaryngology telemedicine clinic. We evaluated the telemedicine model with respect to the financial impact on patients (the “patient‐benefit” cost analysis) who would otherwise be required to travel to a tertiary center for otolaryngology services, and the financial impact on the peripheral medical site (the “peripheral site‐benefit” cost analysis), as compared with a local conventional otolaryngology clinic with a part‐time otolaryngologist on‐site.
MATERIALS AND METHODS
Telemedicine Setup
After approval by the Ohio State University Institutional Review Board, a real‐time telemedicine pilot clinic was conducted in an established part‐time on‐site otolaryngology clinic between Fayette County Memorial Hospital (FCMH) in Washington Court House, Ohio, and the Department of Otolaryngology–Head and Neck Surgery at the Ohio State University Wexner Medical Center (OSUWMC) in Columbus, Ohio, located 41 miles apart. Patients had been scheduled for a visit with an on‐site otolaryngologist from OSUWMC who travelled and conducted an otolaryngology clinic at FCMH. Patients were called in advance by the department's coordinator and verbal consent was obtained over the phone. At the beginning of that clinic visit, patients were provided with more information on the pilot study, and written informed consent was obtained. This study was conducted over 2 days of otolaryngology clinics at FCMH (Fig. 1). A nurse oriented patients to the telemedicine system. A remote, consulting otolaryngologist at OSUWMC observed the exam in real‐time, via telemedicine equipment. Diagnostic accuracy, patient and physician satisfaction, as well as time measurements were obtained, and these data were presented in a separate manuscript.9 The visit details were charted by the on‐site physician using Allscripts (Allscripts Healthcare Solutions, Inc., Chicago, IL), the electronic medical record used by FCMH. After validation of the telemedicine clinic using an on‐site otolaryngologist to verify diagnostic accuracy and concordance, a nurse practitioner will be utilized as the primary healthcare provider at the peripheral site for future implementation. This manuscript assesses the cost savings associated with our proposed model, which includes the on‐site nurse practitioner and an otolaryngologist consulting remotely.
Figure 1.
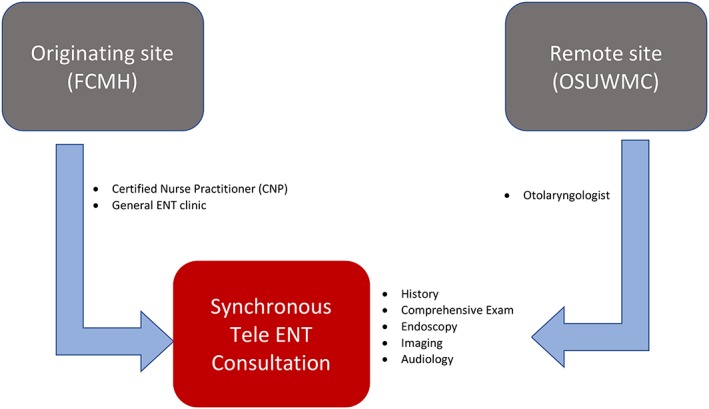
A synchronous telemedicine clinic between FCMH and OSUWMC
Patients are seen in clinic at FCMH by a CNP, who collects data and shares it in real‐time with the remote otolaryngologist at OSUWMC.
CNP = certified nurse practitioner; ENT = ear nose throat; FCMH = Fayette County Memorial Hospital; OSUWMC = Ohio State University Wexner Medical Center.
The peripheral instruments used to create a tele‐ENT office suite during the encounter included a camera control unit (C‐HUB), digital otoscope (used to obtain otoscopic, nasal, and oral exams), and when indicated, a flexible laryngoscope with distal chip technology (KARL STORZ Endoscopy‐America, Inc., El Segundo, CA). The on‐site physician utilized a workstation on wheels (WOW) with pan‐tilt‐zoom webcam, hardwired for optimal internet connectivity, with connected peripheral devices. The consulting physician utilized a laptop with fixed lens webcam, hardwired for optimal internet connectivity. Quintree (Quintree Medical LLC, Detroit, MI) software was used to connect the two otolaryngologists, allowing for transfer of real‐time, two‐way audio and video with minimal latency. Quintree operated on a stable internet connection at FCMH with an upload and download speed of 4.0 MBit/s. FCMH was connected by a 200 Mbps fiber optic Ethernet circuit. FCMH used the hospital's internet connection as the backup circuit to build a Virtual Private Network (VPN) connection in the event of a problem with the primary circuit. Quintree adheres to HIPAA recommendations with regards to security best practices and Protected Health Information (PHI) controls. Quintree provides data encryption at rest as well as encrypting all traffic. All access is user authenticated and logged in an audit trail. All equipment and software complied with appropriate privacy and HIPAA requirements according to state and federal Regulations. The pilot study also abided by the American Telemedicine Association (ATA) Core Operational Guidelines for Telehealth Services regarding technology requirements.10
Patient‐Benefit Cost Analysis
Patient demographic and clinical data were collected. A patient‐benefit cost analysis was performed to evaluate the cost savings to patients, compared with referral to a tertiary medical center, and to the peripheral institution, compared with hosting an on‐site otolaryngology clinic. Patient travel cost was calculated using the approach by Urquhart, Antoniotti, and Berg, based on number of visits, distance, cost of fuel, insurance, and maintenance, and work time lost while traveling.6 The AAA Driving Cost Study set the cost of fuel, insurance, and maintenance at $0.60 per mile.6, 11 Work time lost was calculated based on the average hourly wage in Washington Courthouse obtained from the median household income, multiplied by 8 hours; patients typically take off an entire day of work to visit our tertiary otolaryngology clinic.12 Mean round‐trip distance from OSUWMC to the patients’ zip codes was recorded. This distance was compared with the mean round‐trip distance from FCMH to the patients’ zip codes. Pilot participants were only seen once for the telemedicine appointment for this study, so number of follow‐up visits was not assessed. Instead, mean number of visits was obtained from a separate, referred cohort (n = 145) from FCMH to OSUWMC over a 1‐year period. Mean number of visits was assessed based on the number of office visits and ancillary visits (imaging, audiology, or diagnostic testing). In this cohort, 48 of 145 (30%) of patients required a tertiary care referral for in‐office follow up, eliminating cost savings on follow‐up visits, and therefore total number of mean office visits were adjusted accordingly.
Peripheral Site‐Benefit Cost Analysis
For the peripheral site‐benefit cost analysis, as compared with hosting an on‐site clinic, we assessed a proposed model using one‐time fixed costs, running costs per encounter, and revenue from collections. Telemedicine fixed costs included the cost of equipment. The running costs per encounter assumed 20 encounters per day, the average number of patients typically seen in the otolaryngology clinic at FCMH over the previous calendar year. Running costs included Quintree software, a nurse practitioner as on‐site clinician and tele‐presenter (who would perform and bill for the visit and procedures), and a consulting physician at OSUWMC. The estimated cost of the nurse practitioner per encounter was based on current annual salary at OSUWMC, divided by 50 work weeks per year, 5 days of clinic per week, and 20 encounters per clinic. The estimated cost of the consulting physician per encounter was based in a similar fashion on 0.5 full‐time equivalent (FTE) at 75th percentile of AAMC Assistant Professor salary, using a 20‐patient clinic template.13 This value ($55.50) was used as a negotiable consulting rate per encounter between the peripheral site and the tertiary medical center otolaryngologist consulting for the telemedicine clinic.
For comparison, costs were computed for a part‐time on‐site OSUWMC otolaryngologist in a “conventional” clinic at FCMH, including having the otolaryngologist travel from OSUWMC to FCMH. This amount was based on a pre‐established contract between institutions. The pre‐established contract for the otolaryngologist took into account travel costs for driving to Washington Courthouse and back, missed time from work, and part‐time salary for providing healthcare services. The running revenue for the peripheral site per encounter was calculated based on actual collections over a 1‐year period (fiscal year 2016) from FCMH, assuming 20 encounters per clinic day, which was $144.70 per encounter; for this study, this value was assumed to be the same for both the telemedicine (nurse practitioner at the peripheral site) and conventional system (otolaryngologist at the peripheral site). The net revenue per encounter from the conventional system was recorded and compared to net revenue per encounter for our telemedicine cohort.
The number of encounters required to offset the initial cost for our telemedicine cohort was then calculated using the following equation:
Additionally, the number of encounters required for the revenue of the telemedicine system to surpass that of the conventional system was calculated using the following equation, where Net revenue is per encounter:
RESULTS
Clinical Characteristics
Twenty‐one patients enrolled. New and return patients were included. Patient characteristics and diagnostic details are found in Table 1. The average age of patients in our cohort was 59.8 years with the majority being females (81%). Most patients presented with otologic complaints (61.9%). All patients underwent a complete head and neck exam. Three patients (14.3%) required flexible laryngoscopy. Only six patients (30%) in the telemedicine cohort had more than a high school education.
Table 1.
Patient Characteristics in Telemedicine Cohort.
| Characteristics N (%) or Mean (SD) | Telemedicine Cohort (n = 21) | |
|---|---|---|
| Age in years | 59.8 (23.5) | |
| Sex | Male | 4 (19%) |
| Female | 17 (81%) | |
| Education level | Some high school | 7 (33.3%) |
| (n = 20) | High school | 7 (33.3%) |
| Some college | 2 (9.5%) | |
| College | 1 (4.8%) | |
| Trade/Technical/Vocational | 3 (14.3%) | |
| Final diagnosis Category | Otologic | 13 (61.9%) |
| Sinonasal | 1 (4.8%) | |
| Pharyngeal/Tonsil | 2 (9.5 %) | |
| Voice | 3 (14.3%) | |
| Neck‐related | 2 (9.5) | |
| Telemedicine Peripheral instruments | Flexible laryngoscopy | 3 (14.3%) |
| Type of visit | New patient | 20 (95.2%) |
| Follow‐up | 1 (4.8%) | |
| Postoperative | 0 (0%) |
SD = standard deviation.
Patient‐Benefit Cost Analysis
The patient‐benefit cost savings per encounter, as compared with having to be referred to our tertiary center, is shown in Table 2. Mean travel distance was calculated at 79.1 ± 14.4 miles for round‐trip. Travel‐cost saved was calculated at $47.46 (79.1 miles × $0.60/mile for fuel, maintenance, and insurance).6, 10 Cost of work time lost per encounter was calculated at $134.62 ($16.83/hour × 8 hours), based on average wage/hour in Washington Court House calculated from median house income. The total cost saved to patients per encounter was $182.09. To assess cost to the patient over the span of a year, average numbers of visits to OSUWMC were obtained from a cohort of referred otolaryngology patients (n = 145) from the same geographic region of Washington Court House, and this data is shown in Table 3. The mean total number of visits over the year was 2.04 per patient. After adjusting for the 30% of patients who had 1 telemedicine visit and subsequent tertiary site visits, mean total number of visits at remote site was 1.83. This value refers to visits which patients save travel money on. In this case this is limited to remote site visits only and does not take into account number of visits at tertiary site.
Table 2.
Cost Savings for Patients in the Telemedicine Pilot Study.
| Cost‐saving variables Mean (SD) | Value per patient |
|---|---|
| Round‐trip distance from OSUWMC in miles | 96.7 (19.5) |
| Round‐trip distance from FCMH in miles | 17.7 (16.1) |
| Saved distance per encounter | 79.1 (14.4)* |
| Cost of fuel, insurance, and maintenance | $0.60/mile |
| Cost of work time lost | $16.83/hour |
| Total travel savings per patient per encounter | $182.09 |
FCMH = Fayette County Memorial Hospital; OSUWMC = Ohio State University Wexner Medical Center; SD = standard deviation.
Round‐trip distance from OSUWMC to patient zip codes in miles – round‐trip distance from FCMH to patient zip codes in miles = saved distance per encounter. Travel cost was calculated as distance traveled per encounter (round‐trip distance saved) × cost of fuel, insurance, and maintenance + cost of work time lost per hour while traveling × 8 hours.
Table 3.
Travel‐Associated Variables of Referred Patients From Washington Court House.
| Travel‐associated variables Mean per patient per year | Referred Cohort (n = 145) |
|---|---|
| Office visits | 1.63–48 |
| Ancillary visits | 0.41 |
| Total mean visits | 2.04 |
| Adjusted total mean visits | 1.83 |
| Total travel savings per patient per year | $333.22 |
Total travel savings per patient per year was calculated based on total travel savings per patient per encounter from Table 2 × total mean number of visits per year. Ancillary visits include imaging, audiology, diagnostic testing, and referrals. Adjusted total mean visits assumed 33% patients only had one telemedicine visit and required follow‐up in‐office visits.
The costs of diagnostic/imaging services, additional referrals, preoperative medical clearance, and surgery‐related visits were excluded because they were assumed to be similar between both the on‐site and consulting institution. After considering the average number of visits per year, travel cost savings to the patient was calculated as $333.22 annually per patient.
Peripheral Site‐Benefit Cost Analysis
Next, we evaluated the peripheral site‐benefit cost savings for the telemedicine approach, as compared with a conventional on‐site part‐time otolaryngology clinic. The total costs and revenue that would be generated for the peripheral institution are shown in Table 4. One‐time costs for the telemedicine approach were estimated at $9,895 and included peripheral equipment, camera, cart, and laptop. Running costs were estimated at $106.50 per encounter. Revenue was calculated at $144.70 based on actual collections over a 1‐year period (fiscal year 2016) at FCMH. This resulted in net revenue of $38.15 per encounter for the telemedicine approach. To offset the initial cost of $9,895 for our telemedicine cohort, 260 encounters would be needed (Fig. 2). With a proposed clinic template of 20 encounters per day, 13 days of telemedicine clinic would be needed to recover initiating costs. In contrast, running costs in the conventional system with part‐time on‐site otolaryngologist were $125 per encounter. This included the preestablished cost of the OSWUMC otolaryngologist traveling to FCMH and conducting a clinic. Revenue per encounter at the peripheral site was held the same at $144.70. Thus, the net revenue for the conventional approach was $19.70 per encounter. For the revenue of the telemedicine system to surpass the revenue generated from the conventional on‐site system with traveling part‐time otolaryngologist, 537 encounters would be required. With the proposed clinic template, 27 full‐day telemedicine clinics would be needed to surpass the revenue of the conventional system in 1 year.
Table 4.
Cost of Setting Up and Using Telemedicine for Healthcare System.
| Expenditure | Conventional System | Telemedicine Cohort |
|---|---|---|
| One‐time fixed costs | ||
| Peripheral equipment | $0 | $7645 |
| Laptop | $0 | $1500 |
| Camera | $0 | $250 |
| Cart | $0 | $500 |
| Total fixed costs | $0 | $9895 |
| Running costs per encounter | ||
| Quintree Software | $0 | $18.75 |
| Nurse practitioner | $0 | $32.30 |
| Otolaryngologist | $125 | $55.50 |
| Running revenue per encounter | ||
| Mean patient reimbursements | $144.70 | $144.70 |
| Mean net revenue/ encounter | $19.70 | $38.15 |
Peripheral equipment included laryngoscope, otoscope, and c‐hub. Running costs per encounter were estimated based on daily costs assuming 20 encounters per day. Cost for otolaryngologist for telemedicine cohort is based on 0.5 full‐time equivalent at 75th percentile of AAMC Assistant Professor salary. Cost of otolaryngologist for conventional system is based on a fee for the otolaryngologist coming from OSUWMC to see patients in‐person at FCMH. Mean patient reimbursements is based on actual collections over a 1‐year period at FCMH. Mean net revenue per encounter is based on subtracting running revenue per encounter from running costs per encounter.
AAMC = American Association of Medical Colleges; FCMH = Fayette County Memorial Hospital; OSUWMC = Ohio State University Wexner Medical Center.
Figure 2.
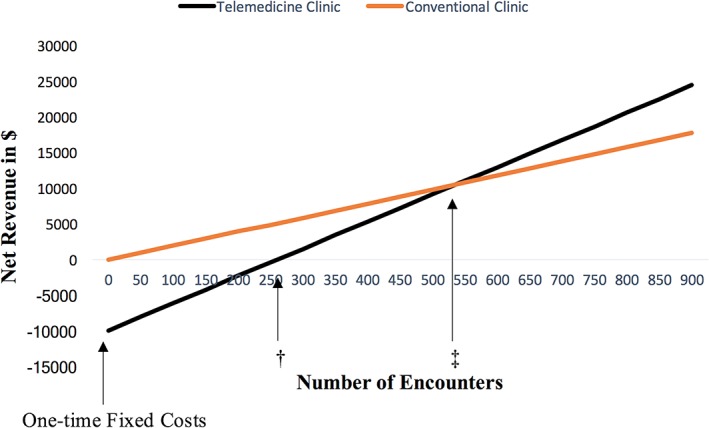
Cost comparison between telemedicine and conventional clinic revenue
Line graph showing number of encounters required for telemedicine clinic to offset initial costs and number of encounters required for net revenue from telemedicine clinic to surpass net revenue from conventional clinic.
† 260 encounters are required for telemedicine clinic to reach breaking‐even point (net revenue = $0)
‡ 537 encounters are required for telemedicine revenue to surpass revenue from conventional system
DISCUSSION
Telemedicine applications in otolaryngology have been gaining popularity with the expansion of technology. Recently, a real‐time pediatric otolaryngology telemedicine program was implemented in Queensland, Australia, and a store‐and‐forward otology telemedicine program has been utilized in Anchorage, Alaska.5, 14 Both centers have geographic and population distribution barriers to access of subspecialty healthcare. These successful telemedicine programs focus on certain populations (pediatric) or certain diagnoses (otologic). To our knowledge, our study presents the first comprehensive, real‐time, adult general otolaryngology telemedicine clinic.
We proposed the application of telemedicine in otolaryngology as a solution for decreasing costs to the patient as well as to the peripheral institution. The cost savings per patient was $182.09 per encounter and $333.22 annually, when compared with referral to a tertiary center. This cost savings to the patients likely has a more significant financial impact than initially apparent. In our cohort, only 30% (6/20) had more than a high school education, reflecting the relatively low socioeconomic status of our cohort. Additionally, in the city of Washington Court House, median household income is $35,905, with 21.8% of people being below the poverty line, as defined by the US Census Bureau.12
The total cost to the peripheral site of initiating the telemedicine system was $9,895. At a net revenue of $38.15 per encounter, 260 encounters would be needed to offset this initial cost for the peripheral site, and 537 encounters (only 27 days of telemedicine clinic) would be needed to surpass revenue of a conventional on‐site clinic with part‐time otolaryngologist. These findings affirm the value of development of an otolaryngology telemedicine program to deliver high‐quality care to outlying rural areas, while maintaining an economic benefit to patients and healthcare systems.
This approach also provides value for the consulting otolaryngologist. Compared to the conventional clinic, our telemedicine model significantly decreases travel costs and time required to travel for the consulting otolaryngologist. By keeping the physician onsite, this allows the consulting otolaryngologist time to utilize between telemedicine consults for academic or administrative purposes, which may increase work efficiency. Although this comes at a decreased reimbursement rate for the consulting otolaryngologist, the value of convenience, decreased travel time, and increased efficiency is significant.
Few other studies have assessed cost savings of a telemedicine system in otolaryngology. A study conducted in rural Nome, Alaska, found that cost savings associated with airfare reached $340 per encounter in 2007 after implementation of a store‐and‐forward telemedicine service.8 A more recent study aimed to demonstrate the cost benefit of using real‐time telemedicine for the postoperative visit in patients undergoing parathyroidectomy.6 This study found that each patient saved $357 in travel costs per encounter by using the telemedicine system. Although our study indicated that each patient saved a smaller amount ($182.09) in travel costs per encounter, due to a mean saved distance of 79.9 ± 14.4 miles, our results still highlight a significant cost savings for patients.
A primary limitation of this study was the size of the cohort. We had 21 patients enroll in our pilot study to assess financial feasibility program. As we continue to expand the program and increase the number of patients, we will have a more accurate representation of cost savings for both the patients and the peripheral healthcare system. Additionally, in this pilot study, we look at a snapshot of our program after one remote office visit. As we expand the program, we will be able to look at prospective long‐term data on patient and tertiary care system cost savings. A second limitation is the assumption that nurse practitioners would be able to bill at the same rate billed by the otolaryngologist including procedural charges. Depending on contractual agreements this may range from 75% to 100% of the otolaryngologist's rate of billing. Determining the actual reimbursement rate for a nurse practitioner at our peripheral site will require a prospective study to track reimbursement from insurance claims. Commercial and government payers in our area do not currently cover the cost of procedures done remotely, therefore all charges related to the office visit and procedures would be generated by the nurse practitioner. The consulting otolaryngologist plays an essential role in this proposed model by providing real‐time assessment for patients with complex issues and those who require presurgical planning. The consulting otolaryngologist would be available for elective surgeries, scheduled separately from clinic, which prevents further travel by patients and promotes continued financial benefit to the institution by retaining both clinic and surgical charges. A third consideration is that our analysis only reflects cost associated with conducting clinic; downstream revenue from surgeries, diagnostic/imaging services, other referrals, preoperative clearance visits, and surgery‐related revenue were excluded from analyses. Under the assumption that care (including ancillary services) is more cost efficient at the patient's home institution versus a tertiary referral center, and with the exclusion of revenue‐generating surgeries, the total cost savings to the peripheral site reported for our cohort might be underestimated. Nonetheless, results of this study suggest that even clinic‐based care was more cost effective for the peripheral site when using a telemedicine approach. These results have significant implications for the feasibility of a telemedicine clinic from a financial standpoint and on its ability to expand care to underserved populations. Further studies will require a comprehensive analysis of financial benefit to the patient, the peripheral site, and the tertiary institution in order to understand the impact of telemedicine on the entire healthcare system.
Ultimately, telemedicine has several implications in addition to cost efficiency. Primarily it expands and improves care in rural and lower socioeconomic areas where access to care is limited.9 Although difficult to quantify, convenience for patients is a very important aspect to support the use of telemedicine. Travel to and from unfamiliar and distant cities might be an inconvenience to many patients. Finally, telemedicine causes a significant reduction in wait times, which occurs because patients receive equivalent care via telemedicine as they would in an in‐person visit with a specialist (otolaryngologist).7 This can lead to improved time to diagnosis, treatment, and improved patient outcomes.
CONCLUSION
Results of this pilot study suggest that a real‐time telemedicine otolaryngology clinic provides significant cost savings for patients and the peripheral healthcare system. Further studies are required to assess cost savings over a longer period with a greater number of patients to determine the financial implications of telecare in otolaryngology.
ACKNOWLEDGMENTS
We would like to thank Fayette County Memorial Hospital and the clinical staff for their support setting up and executing this telemedicine pilot clinic.
Conflict of Interest: None declared for all authors.
Presentation: Oral presentation at The Triological Society Combined Otolaryngology Spring Meeting April 26–30, 2017 in San Diego, California, U.S.A.
BIBLIOGRAPHY
- 1. Vickery TW, Weterings R, Cabrera‐Muffly C. Geographic distribution of otolaryngologists in the United States. Ear Nose Throat J 2016;95:218–223. [PubMed] [Google Scholar]
- 2. Lango MN, Handorf E, Arjmand E. The geographic distribution of the otolaryngology workforce in the United States. Laryngoscope 2017;127:95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Garritano FG, Goldenberg D. Successful telemedicine programs in otolaryngology. Otolaryngol Clin North Am 2011;44:1259–1274. [DOI] [PubMed] [Google Scholar]
- 4. Sclafani AP, Heneghan C, Ginsburg J, Sabini P, Stern J, Dolitsky JN. Teleconsultation in otolaryngology: live versus store and forward consultations. Otolaryngol Head Neck Surg 1999;120:62–72. [DOI] [PubMed] [Google Scholar]
- 5. Xu CQ, Smith AC, Scuffham PA, Wootton R. A cost minimisation analysis of a telepaediatric otolaryngology service. BMC Health Serv Res 2008;8:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Urquhart AC, Antoniotti NM, Berg RL. Telemedicine—an efficient and cost‐effective approach in parathyroid surgery. Laryngoscope 2011;121:1422–1425. [DOI] [PubMed] [Google Scholar]
- 7. Hofstetter PJ, Kokesh J, Ferguson AS, Hood LJ. The impact of telehealth on wait time for ENT specialty care. Telemed J E Health 2010;16:551–556. [DOI] [PubMed] [Google Scholar]
- 8. Kokesh J, Ferguson AS, Patricoski C, LeMaster B. Traveling an audiologist to provide otolaryngology care using store‐and‐forward telemedicine. Telemed J E Health 2009;15:758–763. [DOI] [PubMed] [Google Scholar]
- 9. Seim N, Philips R, Matrka L, et al. Development of a synchronous otolaryngology telemedicine clinic: prospectice study to assess fidelity and diagnostic concordance. Laryngoscope 2018;128:1068–1074. [DOI] [PubMed] [Google Scholar]
- 10.Core Operational Guidelines for Telehealth Services Involving Provider‐Patient Interaction. American Telemedicine Association. Available at: http://www.uwyo.edu/wind/_files/docs/wytn-doc/toolkit-docs/ata_core_provider.pdf. Accessed April 17, 2017.
- 11. Copeland L. Car ownership gets cheaper, says AAA. USA Today. Available at: http://www.usatoday.com/story/news/nation/2014/05/09/aaa-says-cheaper-to-own-a-car/8861533/. Accessed April 17, 2017
- 12. Washington Court House city Ohio QuickFacts . United States Census Bureau. https://www.census.gov/quickfacts/table/INC110212/3981718/. Accessed April 17, 2017.
- 13. Faculty Salary Survey Reports . AAMC. https://services.aamc.org/fssreports/. Accessed April 17, 2017.
- 14. Kokesh J, Ferguson AS, Patricoski C, et al. Digital images for postsurgical follow‐up of tympanostomy tubes in remote Alaska. Otolaryngol Head Neck Surg 2008;139:87–93. [DOI] [PubMed] [Google Scholar]


