Abstract
Objectives
Exercise‐induced laryngeal obstruction (EILO) is a condition causing breathing difficulties and stridor during exercise. The condition has in severe cases been treated surgically with supraglottoplasty. The purpose of this systematic review is to assess the evidence and recommendations for surgical intervention in treating patients with EILO.
Methods
A systematic search was performed in PubMed and Embase to identify relevant studies describing surgical treatment of patients diagnosed with severe EILO. According to eligibility criteria, data were independently extracted by two reviewers. To assess the risk of bias of each included study, the Newcastle‐Ottawa scale (NOS) was used.
Results
The screening process identified 11 observational studies with a total of 75 patients. Findings indicated that many beneficial outcomes are to be found in surgical treatment for EILO. These indications were found both on visual verification of improvement of the laryngeal obstruction during exercise and patient self‐reported symptom severity. The average NOS score (4.3) indicated low level of evidence in the included studies.
Conclusion
Studies reporting effects of surgical treatment of EILO have shown promising results in patients with laryngeal obstruction. However, the heterogeneity of study methodologies and the level of evidence precludes definitive recommendations for or against supraglottoplasty at this time; prospective and methodologically robust studies are now needed.
Level of Evidence
4
Keywords: Larynx, outcomes, EILO, exercise‐induced laryngeal obstruction, supraglottoplasty
INTRODUCTION
Exercise‐induced laryngeal obstruction (EILO) is a condition where anatomical structures in the larynx cause reduced airflow and stridor during high intensity exercise.1, 2 Until recently there has been no consensus regarding nomenclature, diagnostic methods or classification for this condition, and agreement upon a method of treatment is yet to be established.3 Symptoms of EILO are non‐specific and often misdiagnosed as exercise‐induced asthma (EIA),4 thus making identification challenging. EILO is diagnosed by direct visualization of the larynx during peak exercise, as resolving of the obstruction happens within seconds after exercise has ended. This is done by The Continuous Laryngoscopy Exercise (CLE) test, which can be used to assess type and severity of EILO.5 EILO is often diagnosed amongst young and physically active females, and difficulties in inspiration during exercise may cause an unwanted decrease in their fitness activity.6, 7 A study from 2011 estimated that the prevalence in the young population aged 14 to 24 years is 7.5%, making EILO a relatively common condition.8
The therapeutic strategy for treating patients with severe EILO has been diverse and with no established consensus on appropriate treatment.3 There have been some positive reports on medical treatments including psycho‐ and speech therapy,4 but most treatment options are based on weak evidence. An alternative is surgical intervention targeting the supraglottic structures of the larynx in effort to reduce the laryngeal obstruction and the symptoms of breathing difficulties during exertion.9
Several studies have reported positive outcomes from treating EILO surgically, however it has not yet been sufficiently clarified whether surgical intervention in treating EILO is the optimal treatment for this condition. Although advocated in numerous publications, no systematic review has yet performed a structured assessment of bias and level of evidence concerning surgical treatment for EILO. To investigate whether patients suffering from inappropriate supraglottic closure benefit from surgical procedures targeting the supraglottic structures, we reviewed all study types that assessed the outcomes and efficacy of this type of surgical intervention in patients of all ages.
METHOD
This systematic review adheres to the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) guidelines.10 Prior to data extraction and data analysis the protocol for this systematic review was registered at PROSPERO with registration number: CRD42018083887 (https://www.crd.york.ac.uk/prospero/).
Eligibility Criteria
We defined eligibility of studies according to PICOS (participants, interventions, comparators, outcomes, and study types). Participants, of any age, with visually verified inappropriate supraglottic closure on exertion only (ie, by laryngoscopy or other imaging modalities) were included, regardless of the presence of glottic closure (vocal cord dysfunction). Subjects treated surgically in the larynx prior to the examination, and subjects with a medical history of malignancy or any clinical suspicion of malignancy near the larynx, were excluded. Any surgical procedure (eg, cold steel, microdebrider or laser supraglottoplasty) targeting the supraglottic structures (arytenoid mucosa, aryepiglottic folds, or epiglottis) of the larynx was considered eligible for inclusion. For studies with a control group, both between‐group effects and within‐group effects were included in analysis. For studies without a control group, the subjects’ preoperative state was compared to the postoperative state. In order to be included, the severity/degree of the condition had to be measured using the same method pre‐ and postoperatively (ie, CLE test scores, VAS‐score or any other form of outcome measures).
Information Search and Data Collection
Studies were identified searching both MEDLINE via PubMed and Embase. No search criteria on study design were applied. We used free‐text terms related to inappropriate supraglottic closure and terms associated to the surgical type of intervention (Appendix 1). MeSH terms were not used due to the latency of 2 to 3 months for indexing; instead, the free‐text terms were designed to be broad and inclusive to include the most recent studies. Reference lists of included studies and relevant reviews were examined subsequently to identify other potential studies, that had not been included in the search. References from all sources were collected and extracted into an online review management tool (Covidence, https://www.covidence.org/). Subsequent to extraction, all duplicates were removed. Titles and abstracts were screened independently by two authors (KS and EW). Studies, which were considered potentially eligible by any of the reviewers, were read in full text, also independently by the two authors. Disagreement was resolved by consensus.
Data Items and Risk of Bias Assessment
Information extracted from each included study was: 1) number of participants and characteristics of the involved patients (including age and severity of laryngeal closure); 2) type of intervention (eg, laser laryngoscopy or cold steel); and 3) surgical outcome as quantified by any type of measurement done pre‐ and postoperatively, including:
change in the degree of laryngeal obstruction as measured by any measure (eg, Maat score, anterior angle, A‐P diameter of the glottic opening);
change in (ergo‐)spirometry indices such as Peak Inspiratory Flow (PIF) and Forced Inspiratory Flow at 50% (FIF50);
change in patient reported symptom scores (ie, Borg, Visual Analogue Scale (VAS) or other); or
change in exercise capacity.
To ascertain the risk of bias of each included study, we used the Newcastle‐Ottawa scale (NOS).11 This tool is recommended by the Cochrane Collaboration for assessing the quality of non‐randomized studies12 and was an obvious choice as it has recently been stated that no randomized control trials (RCTs) concerning EILO exist.3 The scale was used to assign stars to each individual study regarding each of the following parameters: 1) selection (0–4 stars), 2) comparability (0–2 stars), and 3) outcome (0–3 stars). An adequate length of time for postoperative follow‐up was considered to be ≥1 month. Studies with NOS ≥6, which included appropriate statistical analysis were deemed of high methodological quality.
Data Synthesis
In order to synthesize the findings from each included study, we created a narrative synthesis structured around the type of intervention and the type of outcome. Summaries of intervention effects were made for each individual study. Prior to data extraction we anticipated a limited scope for meta‐analysis due to dissimilarities in type of intervention and outcome measurements.
RESULTS
A total of 11 studies were identified for inclusion in the review (see Fig. 1). The search resulted in a total of 215 records. When duplicates were removed, 161 records remained. Title and abstract screening excluded 135 records, which did not meet the inclusion criteria. In full text screening additionally 12 studies were excluded (Fig. 1). After reviewing study references, no additional studies were identified for inclusion.
Figure 1.
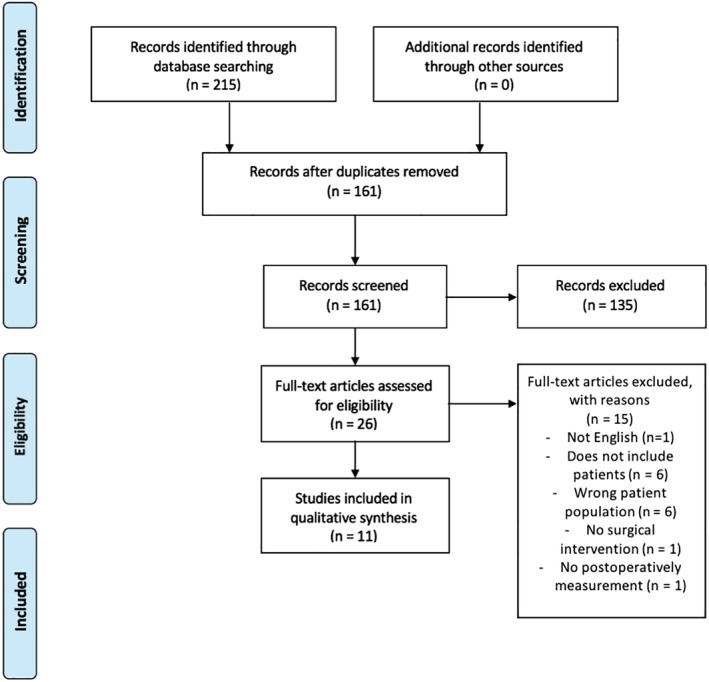
Study inclusion and exclusion.
Eleven studies were thus included comprising a total of 75 patients: six case reports (n = 9 patients)13, 14, 15, 16, 17, 22 and five cohort studies (n = 66 patients).9, 18, 19, 20, 21 Median age was 15.8 years (10 to 62 years of age), the majority of patients being female (75%, n = 56). One study including two patients did not specify the sex of the patients.19 Overall, the patients were physically fit and had a high activity level prior to surgery.
Surgical Technique
Eight studies reported operating on the patients using CO2 laser. Of these, six studies did supraglottoplasty9, 14, 16, 18, 20, 21 and two studies did epiglottoplasty.13, 17 The remaining studies did not specify which surgical technique was used. Of these, one study15 performed staged supraglottoplasty and the two remaining studies did not specify what type of supraglottoplasty was performed.17, 19 Most studies performed pre‐ and postoperative assessment by visualization of the larynx during exercise;9, 13, 14, 16, 17, 18, 20 however, three studies9, 18, 20 in addition reported change in symptoms measured by a VAS score, which was used exclusively in one study.21 One study (n = 1)15 compared pre‐ and postoperative spirometry and one study (n = 2)19 did not perform follow‐up measurements as the patients reported complete resolution of their respiratory symptoms.
Postoperative Visualization of the Larynx During Exercise
Of the included studies, eight studies (64%, n = 48 patients) performed a postoperative assessment with visualization of the larynx at follow‐up.9, 13, 14, 16, 17, 18, 20, 22 Of these, two studies9, 20 (n = 30) compared the pre‐ and postoperative results using the CLE‐score,23 (see Table 1).
Table 1.
Pre‐ and Postoperative CLE Scores.
| At diagnosis | At follow‐up | Mean change (95 % CI) | P‐value | |
|---|---|---|---|---|
| Maat et al.20 (n = 19) | 4.3 (1.2)* | 2.1 (0.7)† | 2.2 (1.6 to 2.8) | <.001 |
| Mehlum et al.9 (n = 11) | 3.9 (1.0)* | 2.8 (1.1)† | 1.1 (0.3 to 2.0) | <.05 |
| Weighted (n = 30) | 4.1 | 2.4 | 1.8 (1.3 to 2.3) |
CLE‐score before surgery presented as mean (standard deviation)
CLE‐score after surgery presented as mean (standard deviation)
CI = confidence interval; CLE = Continuous Laryngoscopy Exercise.
The remaining six studies, including 18 patients, evaluated the patients postoperatively by subjectively assessing the presence or absence of laryngeal obstruction during exercise.13, 14, 16, 17, 18 The larynx of 17 patients showed that there were no longer any supraglottic tissue obstruction. One study17 reported a patient where laryngeal findings indicated improvement, but stated that some fluttering movements still remained after surgery.
Bias assessment in relation to surgical outcomes
A summary of the NOS scores we assigned to the studies is shown in Table 2. The median NOS value was 4.3. None of the studies showed representativeness of exposed cohort, because all patients in the included studies were individually chosen to undergo surgery. Ascertainment of exposure was based upon visual verification in all studies and thus considered appropriate. Only two studies20, 21 presented a control group for comparison, while the remaining studies did not investigate a non‐exposed group. Most studies showed sufficient follow‐up period, with a duration of >1 month,9, 19, 20, 21 except three15, 17, 18 that did not report the follow‐up duration. All studies had adequate follow‐up rate, but one where 47 % was lost to follow‐up in the control group.21
Table 2.
Overview of Included Studies.
| Source | Study Design | Country of Study | No. of Patients (f/m) | Age at Diagnosis (SD) | Control Group | Follow‐up Time (mos) | NOS |
|---|---|---|---|---|---|---|---|
| Smith et al. (1995)13 | Case series | USA | 1 (1/0) | 10 | No | 4 | 4 |
| Bjornsdottir et al. (2000)14 | Case series | Iceland | 2 (2/0) | 14–16 | No | 12 | 4 |
| Maat et al. (2007)18 | Cohort | Norway | 10 (9/1) | 14–18 | No | 3 | 3 |
| Richter et al. (2008)19 | Cohort | USA | 2 (NS) | 14–16 | No | 7 | 4 |
| McNally et al. (2010)15 | Case series | Ireland | 1 (0/1) | 9 | No | ‐ | 3 |
| Maat et al. (2011)20 | Cohort | Norway | 23 (14/9) | 15.1 (3.8) | Yes | 42 | 7 |
| Dion et al. (2012)16 | Case series | USA | 1 (1/0) | 29 | No | 16 | 4 |
| Hilland et al. (2013)22 | Case series | Norway | 3 (0/3) | ‐ | No | 3–6 | 4 |
| Orbelo et al. (2014)17 | Case series | USA | 1 (1/0) | ‐ | No | ‐ | 3 |
| Norlander et al. (2015)21 | Cohort | Sweden | 14 (14/0) | 16.3 (15.3–16.8) | Yes | 11.5 | 6 |
| Mehlum et al. (2015)9 | Cohort | Denmark | 17 (14/3) | 17 (13–62) | No | >3 | 5 |
f = female; m = male; NOS = Newcastle‐Ottawa Scale; NS = not specified; SD = standard deviation.
VAS‐Score
Four studies,9, 18, 20, 21 including 62 patients (63%), evaluated the results of supraglottoplasty using a VAS score. In three studies the patients were asked to use the VAS scales to grade their severity of symptoms. In the remaining study, the subjects were asked to grade their severity of respiratory complaints during exercise. All studies reported significant overall changes in VAS score (see Table 3). Maat et al. reported one patient that felt no improvement after surgery and one patient that felt a subjective worsening from a preoperative VAS score on 65 and a postoperative VAS score of 73.18 No other studies described worsening in VAS score assessed by the patients. Mehlum et al. described two subjects that reported no change in VAS score.9
Table 3.
Pre‐ and Postoperative Respiratory Symptom Severity.
| At Diagnosis | At Follow‐Up | Mean Change (95% CI) | VAS Assessment | |
|---|---|---|---|---|
| Maat et al.18 (n = 10) | 75.7 (12.8)‡ | 27.7 (28.9)‡ | 48.0 (28.4–67.6) | Severity of respiratory complaint during exercise |
| Maat et al.20 (n = 23) | 87.0 (26.0)‡ | 38.0 (27.0)‡ | 62.0 (46.7–77.3) | Symptom severity |
| Mehlum et al.9 (n = 15) | 82.7 (12.9)‡ | 32.7 (30.0)‡ | 49.9 (33.4–66.5) | Symptom severity |
| Weighted average (n = 33) | 83.3 * | 28.0 * | 55.3 (53.3–57.3) | |
| Norlander et al.21 (n = 14) | 8.2† | 3.8† | 4.5‡ | Symptom severity |
VAS‐score (0–100) presented as mean (standard deviation)
VAS‐score (0–10) presented as median
Δ‐VAS; e VAS‐score (0–100) presented as median
CI = confidence interval; VAS = visual‐analogue score.
Physical Activity
Five studies,13, 14, 16, 20, 21 including 41 patients (55%), reported changes in physical activity at follow‐up. Two studies measured the aerobic endurance after surgery. Of these one reported marked improvement.13 The other study stated, that prior to surgery the exercise challenge had to be stopped due to dyspnea. After surgery the exercise challenge was stopped because of leg‐fatigue, and not breathing difficulties.14 Dion et al.,16 including one patient, reported that the patient had previously been limited by her condition and that the patient resumed normal exercise routine after surgery. Two studies had patients answering a follow‐up questionnaire where only 39%20 and 28.6%21 stated that they were more active after surgery. Maat et al.20 stated that the activity level declined in both the conservatively treated and surgically treated patient groups.
Spirometry
Postoperative results were assessed by closed loop spirometry in two studies,14, 15 including three patients (4%). Both studies reported flattening of the inspiratory loop in the patients prior to surgery. Björnsdóttir et al.14 described normal flow‐volume curve patterns at follow‐up after surgery. McNally et al.15 stated that the post‐surgery spirometry showed an improved, but not completely normalized inspiratory flow.
Asthma
Twelve patients (16%) had a diagnosis of asthma prior to investigation for EILO. Three patients (4%) were wrongfully diagnosed with EIA13, 19 and two patients (2.7%) were diagnosed with exercise‐induced bronchospasm (EIB).14 Maat et al. did not report the number of patients diagnosed with asthma, but stated that asthma was either ruled out or appropriately treated prior to CLE‐testing.20 Five studies13, 14, 15, 16, 19 reported a total of seven patients (9% of all included patients, 58% of patients with documented asthma) whose symptoms did not resolve despite receiving asthma medication.
DISCUSSION
Supraglottoplasty has empirically proven beneficial for a number of patients with EILO, improving their self‐reported symptom severity and exercise endurance. Although the reviewed studies suggest that laryngeal surgery may be an effective treatment option for patients with EILO, the number of published studies is small and the lack of RCTs highlight the overall absence of high‐quality evidence. Only two cohort studies included a control group for comparison, one comparing VAS‐score and the other comparing both VAS‐ and CLE‐test scores. In the included studies, surgery was performed in the most severe cases whilst the less severe received conservative treatment, potentially biasing the reported treatment effects.
Assessed on the CLE‐tests there has only been reported one patient, where fluttering movements remained at follow‐up testing. While the majority of patients improved from surgical treatment, some did not. Mehlum and colleagues9 reported three patients (27%), with no observed change in CLE sum score. Some centers employ a cautious surgical approach, removing a minimum of laryngeal tissue and subsequently re‐operate if necessary; such an approach could mask the actual success rate if re‐operations are not reported. For assessing the severity of laryngeal obstruction, several centers have now adopted and/or adapted the approach originally described by Maat et al., detailing a set of criteria based on anatomical appearance and movement of the laryngeal structures.23 This scoring system was designed as a descriptive clinical tool to be used as a part of a complete assessment. Inadequate internal and external consistency of a subjective grade scoring approach might not be appropriate if used exclusively to quantify laryngeal obstruction, particularly in a longitudinal assessment.24
Another concern is the scarcity of data on complications to supraglottoplasty for EILO, concerning the small number of surgically treated cases described worldwide in scientific literature (ie, less than 100). Hilland et al.25 recently reported (in conference proceedings) complications for two patients treated for severe EILO. One patient was diagnosed with postoperative unilateral recurrent laryngeal nerve palsy, the other patient was postoperatively diagnosed with extensive scarring requiring a re‐operation. Complications were found in 2 of 66 (3%) patients, indicating that postoperative complications may be more common than currently published studies indicate. Publication bias may also apply to the lack of reports on complications as unsuccessful surgical results are less likely to be published in scientific literature.26
Measured by the VAS‐score, out of a total of 62 patients, three patients (5%) reported no change in symptom severity and only one patient reported subjective worsening. Evaluating interventions using a subjective VAS scale may introduce potential biases in term of expectations; high expectations from surgical interventions are common27 and the relief that something is done to treat a condition may influence the patient‐reported outcomes.
Several other potential aspects of bias were reflected by the low median NOS score (4.3: only two studies performed an independent blinded outcome assessment suggesting detection bias in the remaining studies9, 20). A high risk of selection bias was implied in all studies, as all patients were individually chosen for surgery based on their symptom severity and the level of obstruction visualized during exercise. In the studies that included a control group for comparison, participants were not assigned randomly to the surgically treated and control groups; the assignment was made based on the severity of EILO and patients’ willingness to undergo surgery, thus introducing possible selection bias.
Indications for supraglottoplasty are highly unclear; although most centers consider only those with severe supraglottic obstruction eligible for surgery, some centers do perform the procedure in individuals with moderate EILO. The presence of concurrent glottic closure is considered a relative contraindication but no solid evidence exists to support or oppose this practice.28 The pathophysiology is poorly understood; potential mechanisms include anatomical‐physiological constitution, laryngeal reflex sensitization, mucosal inflammation, laryngeal hyperreactivity, psychosomatic disorders, and neuromuscular disease.3 Accordingly, surgical outcomes may be influenced by the poor understanding of the underlying condition.
The number of centers performing CLE is rapidly increasing across Europe and the United States and it is likely that the number of patients considered eligible for surgery will rise correspondingly over the next decade. Further, there is no evidence to suggest one treatment option (eg, speech and language therapy, respiratory physiotherapy, or laryngeal surgery) over another; emphasizing the need for a reliable and accurate assessment to be employed in the evaluation of patients’ eligibility for an intervention as well as in the appraisal of the efficacy of interventions. Given the unclear etiology and pathophysiology of EILO and the absence of high‐quality data in scientific literature, we propose that such an assessment ideally include:
Objective characterization of EILO from continuous laryngoscopic video during exercise, or as a minimum a robustly blinded rating/score from multiple raters including an evaluation of the reliability of such assessment;
Patient‐reported outcomes based on respiratory symptoms and quality of life;
A reproducible and sensitive assessment of exercise tolerance; and
Systematic follow‐up, ie, employing comparable examinations pre‐ and post‐intervention.
The recent joint European Respiratory Society/European Laryngological Society Task Force report on inducible laryngeal obstruction highlights that objective assessment and quantification of EILO remains a top priority to progress research and clinical assessment.3 Such a tool is currently in development29 by our group but is yet to be validated clinically and currently, the method described by Maat and colleagues23 remains the preferred EILO grading method. Studies examining subjective or observer‐dependent outcomes could to some extent mitigate potential bias by employing a robust blinding scheme, preferably including multiple raters, to ensure that raters are unaware of clinical and pre‐ and postoperative status. Inter‐observer agreement and internal consistency should be reported and discussed.
Dyspnea is a complex symptom. The use of VAS scores to quantify dyspnea intensity is practical in an exercise testing setting but might not constitute a complete and adequate assessment of the patient's respiratory complaints and is highly dependent on the questions asked. We suggest using validated and detailed dyspnea questionnaires such as Dyspnea‐1230 or Multidimensional Dyspnea Profile31 to assess intervention efficacy, allowing for a better characterization on intervention effects on the individual dimensions of dyspnea.
Presently, CLE is routinely performed with incremental exercise testing. While this approach is likely to be the most sensitive to detect EILO,32 constant work rate testing at high intensity (ie, 80–90% of maximum) might be a more representative and sensitive test to quantify the effect of intervention on exercise tolerance, as seen in other respiratory conditions.33
Strengths and Limitations
The prospective protocol registration with PROSPERO prior to the study search and adherence to the PRISMA‐P and PRISMA guidelines underlines the methodological care undertaken in this systematic review. This acknowledged, the studies eligible for inclusion were only observational studies with incomparable study designs and outcomes that were not qualified for meta‐analysis. In scientific literature, EILO has been described with imprecise nomenclature, making identification of suitable studies difficult. However, this was considered prior to the literature search and consequently studies using different terminology describing the condition were included in the review. The included studies comprised a very limited number of patients and only two studies included a control group for comparison making the studies representation questionable.
CONCLUSION
In conclusion, studies reporting effects of surgical treatment of EILO have shown promising results in patients with severe laryngeal obstruction, but the evidence base is lacking due to the limited number of cases reported and the quality of the eligible studies. No recommendations for or against supraglottoplasty can thus be made at this time. Larger and methodologically robust prospective studies, preferably RCTs, are needed to verify the apparent benefits of the procedure and clarify the risk of complications.
Supporting information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Appendix S1: Supporting information
Editor's Note: This Manuscript was accepted for publication on February 5, 2019.
Funding: The study received no funding.
Conflict of Interest: The authors declare no conflicts of interest.
BIBLIOGRAPHY
- 1. Hall A, Thomas M, Sandhu G, Hull JH. Exercise‐induced laryngeal obstruction: a common and overlooked cause of exertional breathlessness. Br J Gen Pract 2016;66(650):e683–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Beaty MM, Wilson JS, Smith RJ. Laryngeal motion during exercise. Laryngoscope 1999;109(1):136–139. [DOI] [PubMed] [Google Scholar]
- 3. Halvorsen T, Walsted ES, Bucca C, et al. Inducible laryngeal obstruction: an official joint European Respiratory Society and European Laryngological Society statement. Eur Respir J 2017;50(3):1602221. [DOI] [PubMed] [Google Scholar]
- 4. Christopher KL, Wood RP, Eckert RC, Blager FB, Raney RA, Souhrada JF. Vocal‐cord dysfunction presenting as asthma. N Engl J Med 1983;308(26):1566–1570. [DOI] [PubMed] [Google Scholar]
- 5. Heimdal JH, Roksund OD, Halvorsen T, Skadberg BT, Olofsson J. Continuous laryngoscopy exercise test: A method for visualizing laryngeal dysfunction during exercise. Laryngoscope 2006;116(1):52–57. [DOI] [PubMed] [Google Scholar]
- 6. Newman KB, Mason UG, Schmaling KB. Clinical features of vocal cord dysfunction. Am J Respir Crit Care Med 1995;152(4):1382–1386. [DOI] [PubMed] [Google Scholar]
- 7. Røksund OD, Maat RC, Heimdal JH, Olofsson J, Skadberg BT, Halvorsen T. Exercise induced dyspnea in the young. Larynx as the bottleneck of the airways. Respir Med 2009;103(12):1911–1918. [DOI] [PubMed] [Google Scholar]
- 8. Christensen PM, Thomsen SF, Rasmussen N, Backer V. Exercise‐induced laryngeal obstructions: prevalence and symptoms in the general public. Eur Arch Otorhinolaryngol 2011;268(9):1313. [DOI] [PubMed] [Google Scholar]
- 9. Mehlum CS, Walsted ES, Godballe C, et al. Supraglottoplasty as treatment of exercise induced laryngeal obstruction (EILO). Eur Arch Otorhinolaryngol 2016;273(4):945–951. [DOI] [PubMed] [Google Scholar]
- 10. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62(10):e1–34. [DOI] [PubMed] [Google Scholar]
- 11. Wells GA, Shea B, O'connell D, et al. The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. Ottawa: Ottawa Hospital Research Institute; 2009.
- 12. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at: http://handbook.cochrane.org.
- 13. Smith RJH, Kramer M, Bauman NM, et al. Exercise‐induced laryngomalacia. Ann Otol Rhinol Laryngol 1995;104(7):537–541. [DOI] [PubMed] [Google Scholar]
- 14. Bjornsdottir US, Gudmundsson K, Hjartarson H, Brondbo K, Magnusson B, Juliusson S. Exercise‐induced laryngochalasia: an imitator of exercise‐induced bronchospasm. Ann Allergy Asthma Immunol 2000;85(5):387–391. [DOI] [PubMed] [Google Scholar]
- 15. McNally P, Greally P. Use of post‐exercise laryngoscopy to evaluate exercise induced dyspnea. Pediatr Pulmonol 2010;45(10):1037–1039. [DOI] [PubMed] [Google Scholar]
- 16. Dion GR, Eller R, Thomas R. Diagnosing aerodynamic supraglottic collapse with rest and exercise flexible laryngoscopy. J Voice 2012;26(6):779–784. [DOI] [PubMed] [Google Scholar]
- 17. Orbelo D, Cofer S. Exertional stridor: Differential diagnosis, investigation, and treatment based on serial exercise tests with flexible transnasal flexible laryngoscopy. Chest 2014;145(3):566A. [Google Scholar]
- 18. Maat RC, Roksund OD, Olofsson J, Halvorsen T, Skadberg BT, Heimdal J‐H. Surgical treatment of exercise‐induced laryngeal dysfunction. Eur Arch Otorhinolaryngol 2007;264(4):401–407. [DOI] [PubMed] [Google Scholar]
- 19. Richter GT, Rutter MJ, deAlarcon A, Orvidas LJ, Thompson DM. Late‐onset laryngomalacia: a variant of disease. Arch Otolaryngol Head Neck Surg 2008;134(1):75–80. [DOI] [PubMed] [Google Scholar]
- 20. Maat RC, Hilland M, Roksund OD, et al. Exercise‐induced laryngeal obstruction: Natural history and effect of surgical treatment. Eur Arch Otorhinolaryngol 2011;268(10):1485–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Norlander K, Johansson H, Jansson C, et al. Surgical treatment is effective in severe cases of exercise‐induced laryngeal obstruction: a follow‐up study. Acta Otolaryngol 2015;135(11):1152–1159. [DOI] [PubMed] [Google Scholar]
- 22. Hilland M, Sandvik L, Halvorsen T, Roksund O. Exercise induced stridor treated with epiglottoplasty. Eur Arch Oto‐Rhino‐Laryngology 2013;270(1):397 10.1007/s00405-012-2208-z. [DOI] [Google Scholar]
- 23. Maat RC, Røksund OD, Halvorsen T, et al. Audiovisual assessment of exercise‐induced laryngeal obstruction: reliability and validity of observations. Eur Arch Otorhinolaryngol 2009;266(12):1929–1936. [DOI] [PubMed] [Google Scholar]
- 24. Walsted ES, Hull JH, Hvedstrup J, Maat RC, Backer V. Validity and reliability of grade scoring in the diagnosis of exercise‐induced laryngeal obstruction. ERJ Open Res 2017. 10.1183/23120541.00070-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hilland M, Engesæter I, Sandnes A, et al. Postoperative Complications After Surgical Treatment For Exercised Induced Laryngeal Obstruction. Medicine & Science in Sports & Exercise. 2017;49(5S):1047 10.1249/01.mss.0000519875.46039.0c. [DOI] [Google Scholar]
- 26. Fanelli D. Do pressures to publish increase scientists’ bias? An empirical support from US states data. PLoS One 2010;5(4):e10271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Williams JB, Popp D, Kobak KA, Detke MJ. P‐640 ‐ The power of expectation bias. Eur Psychiatry 2012;27:1.22153731 [Google Scholar]
- 28. Heimdal JH, Maat R, Nordang L. Surgical intervention for exercise‐induced laryngeal obstruction. Immunol Allergy Clin North Am 2018;38(2):317–324. [DOI] [PubMed] [Google Scholar]
- 29. Lin J, Walsted ES, Backer V, Hull JH, Elson D. Quantification and analysis of laryngeal closure from endoscopic videos. IEEE Trans Biomed Eng 2018. 10.1109/TBME.2018.2867636. [DOI] [PubMed] [Google Scholar]
- 30. Yorke J, Moosavi SH, Shuldham C, Jones PW. Quantification of dyspnoea using descriptors: development and initial testing of the Dyspnoea‐12. Thorax 2010;65(1):21–26. 10.1136/thx.2009.118521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Banzett RB, O'Donnell CR, Guilfoyle TE, et al. Multidimensional Dyspnea Profile: an instrument for clinical and laboratory research. Eur Respir J 2015;45(6):1681–1691. 10.1183/09031936.00038914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Olin JT, Clary MS, Fan EM, et al. Continuous laryngoscopy quantitates laryngeal behaviour in exercise and recovery. Eur Respir J 2016;48(4):1192–1200. http://erj.ersjournals.com/content/early/2016/07/13/13993003.00160-2016.abstract. [DOI] [PubMed] [Google Scholar]
- 33. Hsia D, Casaburi R, Pradhan A, Torres E, Porszasz J. Physiological responses to linear treadmill and cycle ergometer exercise in COPD. Eur Respir J 2009;34(3):605–615. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Appendix S1: Supporting information


