Abstract
Polar, differentiated epithelial cell culture models (especially at confluence) are difficult to transfect compared with the higher transfection efficiencies that one obtains with relatively less differentiated, nonpolar cell culture models. Here, we sought to develop a strategy to enhance the efficiency of transfecting polar, differentiated epithelial cells. We found that chemically abrading the differentiated CACO-2 human intestinal epithelial cell layer by a trypsin and EDTA pretreatment (before the use of detergent-like transfection reagents) dramatically improved transfection efficiency in this polar, differentiated model. Although this treatment did improve the transfection efficiency, it also induced leakiness in the epithelial barrier by both opening tight junctional complexes and by creating holes in the cell layer because of low-level cell death and detachment. Thus, this approach to enhance the transfection efficiency of polar, differentiated cells will be useful for assessment of the effect of the transfected/expressed protein on (re)formation of an epithelial barrier rather than on a functional barrier itself.
Keywords: CACO-2, epithelial barrier function, polarity, differentiation, apical
INTRODUCTION
Nonviral, transient transfection of plasmid DNA into differentiated, polar epithelia using the calcium phosphate precipitate method or using detergent-like, micellar-forming compounds does not proceed with great efficiency compared with similar transfection methods on nonpolar, relatively undifferentiated cell cultures. Transfection efficiency of the differentiated human intestinal epithelial cell lines CACO-2 or HT-29/B6 proceeds with dramatically lower efficiency than parallel transfections of cell lines that simply do not highly differentiate (and polarize), such as COS-7 or 293T.1 If one’s research utilizes differentiated epithelial cultures such as CACO-2, HT-29, or MDCK, one could resort to transfecting the substantially less differentiated subconfluent culture, but this may very well abrogate the observation of a differentiated feature that one wishes to study. In the time (days) that would be required to achieve differentiation after the transfection of a subconfluent culture, one may suffer the loss of expression of what one transfected into the cells, as expression often peaks 24 h post-transfection and can then rapidly decline to baseline by 96–120 h post-transfection. Contrast that transience of expression with, for example, the 21 d postconfluence that are required for CACO-2 to achieve maximal differentiation.2
Thus, the transient transfection of differentiated epithelial cell layers has presented significant difficulty, and the development of new strategies to improve on this process is warranted. Given the fact that transfection of a differentiated, polar epithelial cell layer normally occurs by contact of transfection reagents and plasmid DNA with only the apical cell surface, that may not be entirely surprising. For a differentiated cell layer, the apical cell membrane is the “upward”-facing cell surface, which is in immediate contact with the culture medium, as opposed to the “downward”-facing basal-lateral cell membrane, which is typically contacting the surface of the culture dish or flask. It seems quite simple, but it can often be overlooked that in conventional cell culture dishes or flasks only the apical membrane has immediate contact with constituents added to the culture medium, as cell polarity and tight junctional (TJ) seals delimit any contact with the basal-lateral surface.3 In a differentiated cell culture, such as CACO-2, the apical membrane is likely more highly populated by integral membrane proteins than would be the case for a nonpolar, relatively undifferentiated cell culture, like COS. This “richer” membrane protein environment may delimit the interaction of transfection reagent, micellar/liposomal structures (containing the plasmid DNA) with the plasma membrane, thereby decreasing delivery of plasmid DNA into the target cell.
In this paper, we describe a simple procedure that will proteolytically shear apical membrane proteins, facilitating micelle fusion with the apical membrane, while also opening up the epithelial barrier, thereby allowing access of the transfection reagents and DNA to the basal-lateral membrane surface. The net effect would be to increase plasmid DNA delivery to the target cells and thereby increase transfection efficiency.
MATERIALS AND METHODS
Cell culture
The CACO-2 cell culture was obtained from American Type Culture Collection (ATCC; Manassas, VA, USA) and was used between passages 52 and 70. Upon confluence, cells were passaged on a weekly basis by trypsinization [0.25% trypsin and 2.2 mM EDTA (Cellgro; Corning, Corning, NY, USA)] and were seeded at 7e5 cells per Falcon 75-cm2 culture flask with 25 ml of DMEM supplemented with 2 mM l-glutamine (Cellgro), 1% Nonessential Amino Acids (Cellgro), 1 mM sodium pyruvate (Cellgro), and 10% defined fetal bovine serum (Avantar, University Park, IL, USA). Cultures were incubated at 37°C in a 95% air and 5% CO2 atmosphere.
Viral transfection
Cells were seeded into sterile Millicell polycarbonate filter (PCF) permeable supports (30 mm diameter with 0.4-µm pore size) (MilliporeSigma, Burlington, MA, USA) on d 0 at a seeding density that ranged between 5 × 105 and 8 × 105 cells per insert, depending on the experiment. Four PCF inserts were seeded in a 100-mm Petri dish. On d 1, all cell layers were refed (2 ml apical/15 ml basal-lateral) with control medium containing 50 U/ml penicillin and 50 µg/ml streptomycin. On d 3, PCFs were transfected with Ebola VP40 (40 kDa Viral Protein) plasmid (R.N.H.) at a concentration varying from 0.5 to 2.0 µg/200 µl per PCF insert. Plasmid was made up in Lipofectamine or Lipofectamine 3000 (Thermo Fisher Scientific, Waltham, MA, USA) following the protocol that was supplied with the reagent, with the one exception that the plasmid mixture was left to incubate for 30–45 min. First, cell layers were rinsed twice with Opti Minimal Essential Medium (OptiMEM) Reduced Serum Medium (Thermo Fisher Scientific). Then, trypsin pretreatment was completed: 2 rinses with 0.25% trypsin and 2.2 mM EDTA followed by 2 rinses (3 ml apical/15 ml basal-lateral) with DMEM followed by a rinse [3 ml apical/15 ml basal-lateral (2X PCF inserts)] with OptiMEM. Immediately after came the addition of plasmid: 1 ml of OptiMEM in each ring and then 200 µl of plasmid added dropwise into the rings. Each PCF insert was carefully lifted and swirled to mix. Cultures were incubated for 4 h at 37°C. After 4 h, the plasmid was aspirated off, followed by 1 rinse (PCF inserts only), and refed in OptiMEM overnight. On d 4, all cell cultures were refed in control medium.
Transepithelial permeability measurements
Cells were seeded the same way as for transfection, but on d 5 or 6, they were used for transepithelial measurements. The cell layers were refed with fresh control medium and allowed to incubate at 37°C for 1.5 h prior to electrophysiological readings. Transepithelial potential difference was measured at 37°C using 1 M NaCl salt bridges in series with calomel electrodes. Transepithelial electrical resistance (Rt) was measured using 1-s, 40-µA direct current pulses and calculated using Ohm’s law. As soon as electrical measurements were completed, the basal-lateral medium was aspirated and replaced with 15 ml of medium containing 0.1 mM, 0.10 µCi/ml 14C-D-mannitol (PerkinElmer, Waltham, MA, USA) and incubated at 37°C. Triplicate basal-lateral medium samples (50 µl) were taken for liquid scintillation counting for specific activity determination. Duplicate samples (250 µl) were taken from the apical side at 90 min for liquid scintillation counting to determine flux rates (Jm). The Jm (counts/min (cpm)/min/cm2) was calculated for the 14C-D-mannitol diffusing across the cell layer.
Western immunoblot analysis of VP40 expression and tight junctional proteins
Cells were harvested from Millicell PCF rings by the following method: the cells were washed 5 times in cold PBS; 600 μl of lysis buffer with protease and phosphatase inhibitors was added to each PCF; the cell layer was scraped off of the PCF; and the cell suspension was collected, flash-frozen, and stored at −80°C. Whole-cell lysates were prepared by sonication and ultracentrifugation. Samples of these lysates were analyzed by Western blot analysis using a 4−20% gradient Tris-glycine gel (Thermo Fisher Scientific) at 125 V for 1 h and 25 min. Precision Plus Kaleidoscope Protein Standards (Bio-Rad, Hercules, CA, USA) were also included on each gel. Proteins were transferred from the gel to a nitrocellulose membrane at 30 V for 1.5 h. The membranes were then washed 3 times with PBS with Tween 20 (PBS-T; 0.3% Tween 20) for 10 min each and blocked with 5% milk in PBS-T for 1 h at room temperature. For experiments on cells transfected with the Ebola virus VP40 gene, membranes were incubated with a mouse monoclonal anti–VP40 antibody (a gift of R.N.H.) at 2 μl/12 ml in 5% milk/PBS-T overnight at 4°C. The membranes were again washed 3 times (10 min each time) with PBS-T and then incubated with the secondary antibody [goat anti-rabbit-IgG antibody labeled with horseradish peroxidase (Southern Biotech, Birmingham, AL, USA)] for 1 h at room temperature. The membranes were washed 4 times (10 min each time) with PBS-T and then treated for 1 min with Western Lightning Plus-ECL chemiluminescence reagents (PerkinElmer). The membranes were then exposed and quantified on the Bio-Rad ChemiDoc Imaging System. For studies examining the TJ protein claudin-1, immunoblots were probed with a mouse IgG mAb against the C-terminal region (37-4900; Thermo Fisher Scientific, Waltham, MA, USA). For studies examining occludin, a rabbit IgG pAb against the C-terminal region (71-1500; Thermo Fisher Scientific) was used. Rabbit-anti-mouse and goat-anti-rabbit secondary antibodies were used (Southern Biotech, Birmingham, AL, USA).
RESULTS
Improvement of transfection efficiency by trypsin and EDTA pretreatment
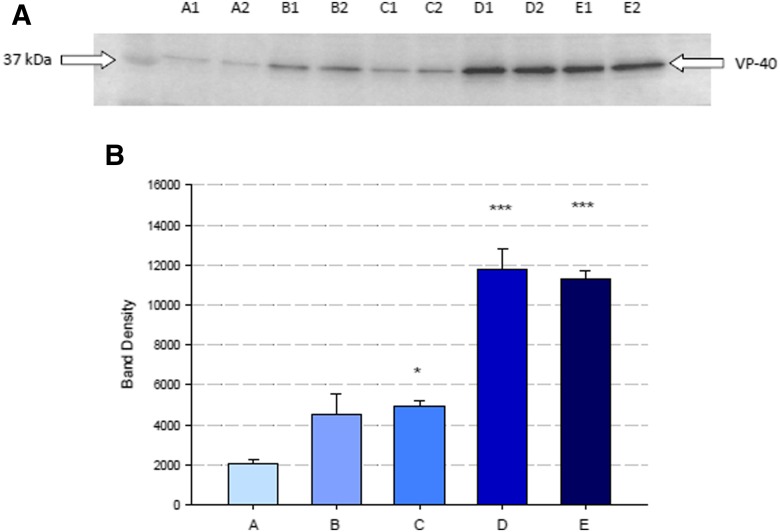
As shown in Fig. 1A, the choice of transfection reagents can significantly improve plasmid delivery and subsequent protein expression. In the case of confluent CACO-2 cell layers, the use of Lipofectamine 3000 transfection reagent (lanes B1/B2 and C1/C2 in Fig. 1A) significantly improved the expression levels of the Ebola virus VP40 protein in confluent CACO-2 cell layers compared with that observed in cells treated with the older-generation Lipofectamine reagent (lanes A1/A2). This is shown here for 2 independent CACO-2 cell layers per condition. The (pre)exposure of the CACO-2 cell layers (in Millicell PCFs) to trypsin and EDTA on the apical surface of the cell layer as described in Materials and Methods, which was followed by treatment with the Lipofectamine 3000 transfection reagents, significantly increased VP40 expression per unit of total protein (lanes B1/B2 and C1/C2 vs. D1/D2 and E1/E2). Figure 1B provides the densitometric quantitation of VP40 expression for these different transfection procedures for a total of 4 independent CACO-2 cell layers per procedure and shows the high degree of statistical difference that was obtained with the trypsin and EDTA pretreatment.
FIGURE 1.
The effect of trypsin/EDTA Pretreatment on Ebola VP40 expression in a CACO-2 cell layer. A) Western immunoblot showing the levels of VP40 expression in CACO-2 cell layers transfected with various reagents/conditions as described in Materials and Methods. The conditions utilized were A) Lipofectamine, B) Lipofectamine 3000 (low formulation), C) Lipofectamine 3000 (high formulation), D) trypsin/EDTA pretreatment + Lipofectamine 3000 (low), and E) trypsin/EDTA pretreatment + Lipofectamine 3000 (high). B) VP40 band densitometric quantitation representing the means of 4 separate cell layers ± se. One-way ANOVA test. *P < 0.05, ***P < 0.001 vs. Lipofectamine-transfected cell layer.
Implications of improved efficiency for barrier function studies
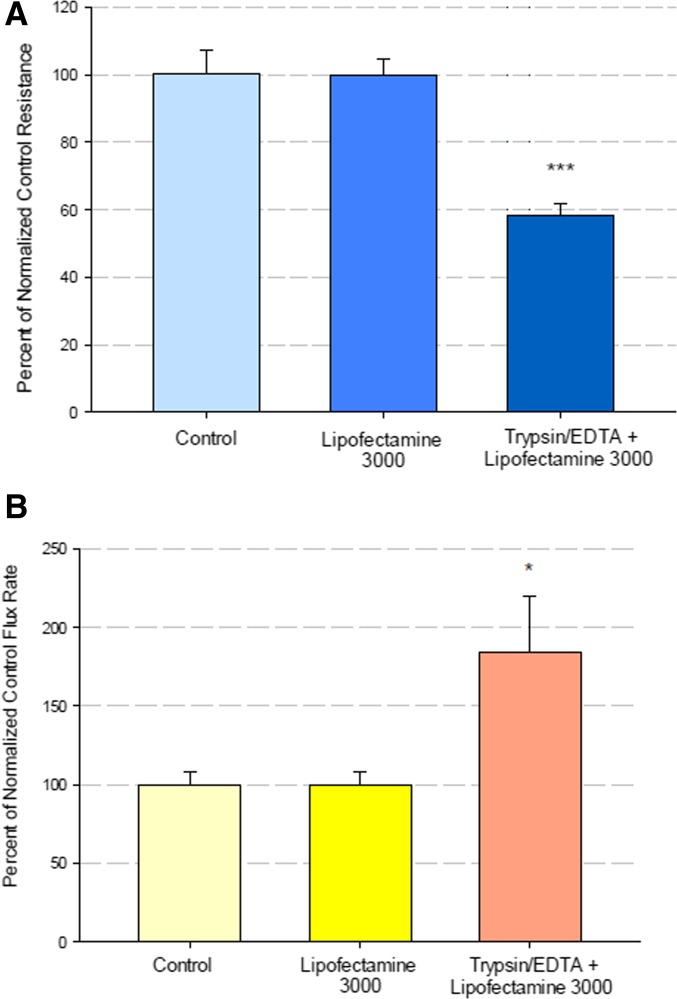
The addition of the trypsin and EDTA pretreatment along with the exposure to the transfection chemicals, however, leads to significant epithelial barrier disruption. Exposure of CACO-2 cell layers to Lipofectamine 3000 alone did not significantly affect epithelial barrier function, but inclusion of a trypsin and EDTA pretreatment step did impair barrier function significantly, with Rt decreased by over 40% (Fig. 2A) and transepithelial mannitol leak increased by over 80% (Fig. 2B).
FIGURE 2.
Effect of trypsin/EDTA pretreatment on CACO-2 barrier function following transfection. Cell layers were treated as described in Materials and Methods in mock transfections without the use of plasmid DNA. Cell Layers were treated with control medium, medium containing Lipofectamine, or Lipofectamine after a trypsin/EDTA pretreatment. Rt (A) and 14C-mannitol flux rate (B) were measured immediately after a 3-h transfection period. Data shown represent the percent of control resistance and mannitol flux rate, expressed as the means ± se of 6 cell layers per condition. One-way ANOVA test. *P < 0.05, ***P < 0.001.
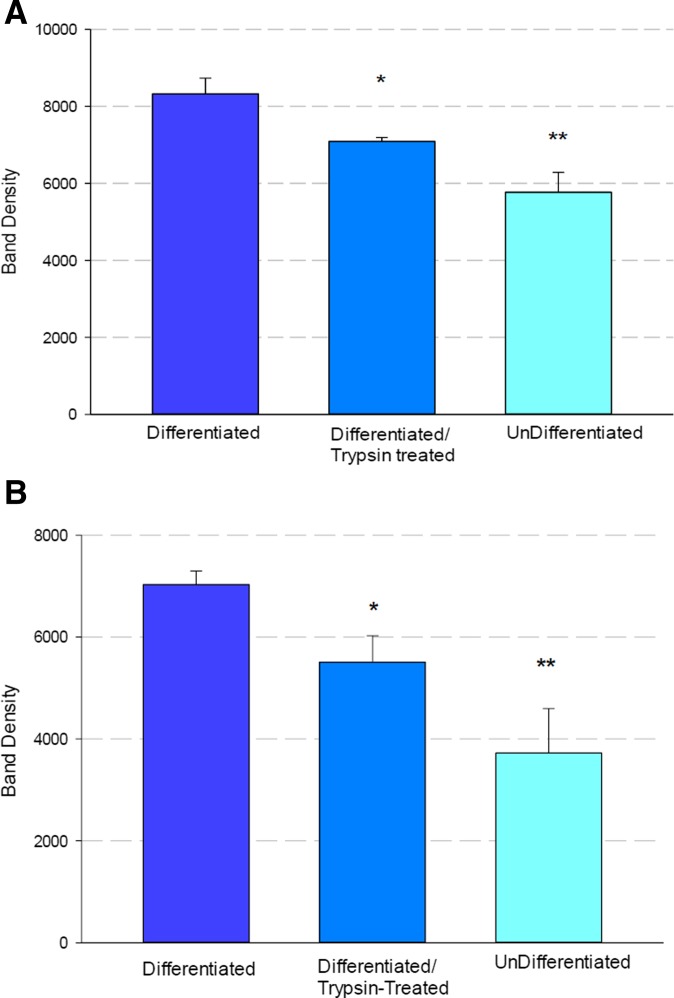
This functional compromise of epithelial barrier function by the trypsin and EDTA treatment is reflected in the combined action of these agents on proteins of the TJ complex. As shown in Fig. 3, subconfluent CACO-2 cultures contain significantly less of the TJ proteins claudin-1 (Fig. 3A) and occludin (Fig. 3B) than confluent, differentiating cell layers. Confluent CACO-2 cell layers that were treated with trypsin and EDTA, as previously described in Materials and Methods, have an intermediate number of these TJ proteins, which are significantly below the level of untreated confluent cell layers. These results further demonstrate that the transfection procedure in use here does compromise the barrier function of the CACO-2 epithelium.
FIGURE 3.
Effect of trypsin/EDTA pretreatment on the CACO-2 TJ proteins. A) Claudin-1; B) Occludin. Confluent and subconfluent CACO-2 cultures in 75-cm2 culture flasks were rinsed twice with trypsin/EDTA then incubated with 2 ml of trypsin/EDTA at 37°C until cells first began to show initial morphologic signs of detaching from each other and the culture flask (∼3–5 min). Trypsin/EDTA was aspirated off, and cultures were rinsed 2 times with culture medium and then refed with culture medium for 18–24 h at 37°C. Cell layers were then removed mechanically by scraping followed by preparing whole-cell lysates as described in Materials and Methods, followed by PAGE and Western immunoblot. Data shown represent the means ± se of 4 cell cultures. Two-tailed Student’s t test. *P < 0.05, **P < 0.01.
Balancing recovery of barrier function against transient nature of transfection
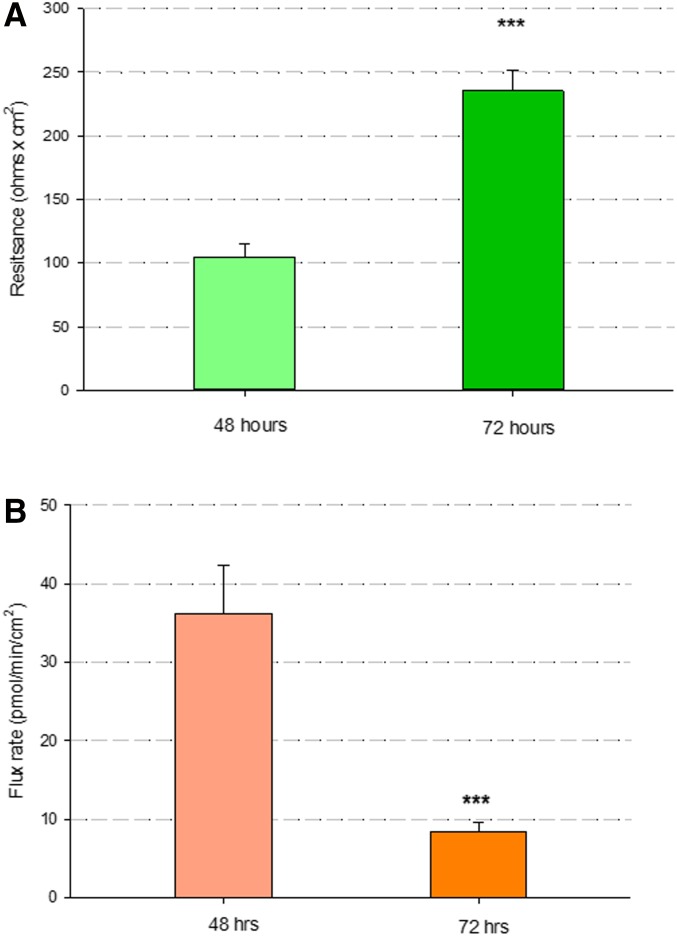
There is, however, relatively rapid recovery of barrier function after a transfection regimen, as shown in Fig. 4. Exposure to trypsin and EDTA followed by Lipofectamine 3000 may bring Rt values down as low as 100 ohms × cm2, even 48 h after exposure. These cell layers were 5–6 d postseeding, a time when Rt values would typically be 400–500 ohms × cm2. Note that Rt values more than double in the following 24 h (72 h post-transfection) (Fig. 4A). Simultaneously, mannitol leak decreases by 80% as cell layers dramatically decrease their permeability to this small carbohydrate (Fig. 4B). This recovery of barrier function is necessary for the performance of any barrier function or TJ study involving the effects of a transfected protein. It is a complicated overall situation, however, because barrier function can be recovering from the effects of transfection methodology just as the expression of one’s transfected protein may be waning (Fig. 5).
FIGURE 4.
Recovery of barrier function after transfection. Transfection of Ebola VP40 was performed on 3-d–postseeding CACO-2 cell layers as described in Materials and Methods. Rt measurements were taken 48 and 72 h after transfection. At each time point, Rt measurements were followed immediately by transepithelial radiotracer flux studies with 0.1 mmol, 0.1 µCi/ml 14C-d-mannitol. Data shown represent the mean resistance (A) and flux rate (B) of 12 CACO-2 cell layers ± se. Student’s t test, 2-tailed. ***P < 0.001.
FIGURE 5.
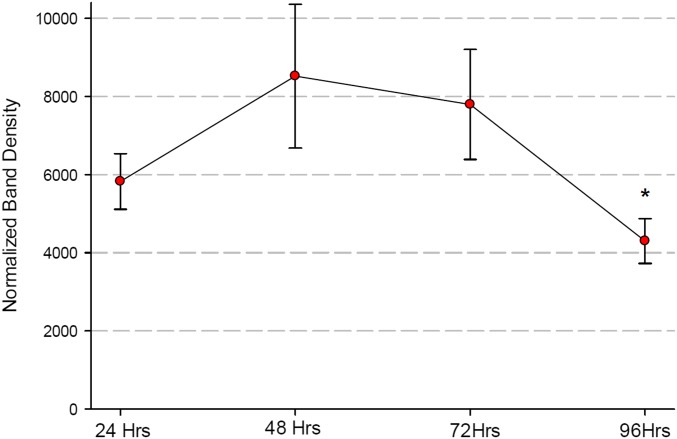
Time course of VP40 expression in CACO-2 cell layers. Cell layers were harvested at indicated times after transfection from Millicell PCF inserts, and whole-cell lysates were prepared as described in Materials and Methods. Results shown represent the densitometry of VP40 bands in Western immunoblots, each data point representing the mean of 4 cell layers per condition ± se. One-way ANOVA. *P < 0.05 vs. 48-h time point.
As is true for any transiently transfected protein, expression of the Ebola VP40 protein in CACO-2 cell layers (after using the trypsin and EDTA treatment step described in Fig. 1) is time dependent (Fig. 5). For example, we observed that expression of the VP40 protein in the CACO-2 cell layers maximizes 48 h post-transfection, but by 96 h it has decreased below the level manifested at 24 h and decreased significantly below the level of expression at 48 h. This time dependence has strong implications regarding any study involving the effect of a transfected protein such as VP40 on epithelial barrier function because barrier function is recovering (changing) as a function of time post-transfection (Fig. 4) while the amount of the putative effector of barrier function (in this case, the VP40 protein) is likewise changing with time (Fig. 5).
DISCUSSION
In this study, we highlight the difficulties of investigations involving the effect of a transiently transfected protein on epithelial barrier function. The study of epithelial barrier function demands a differentiated (confluent) cell layer. However, such a cell population has been shown to be markedly less amenable to transfection than cultures of nonpolar, poorly differentiated cells.1,4
If one’s cellular starting material in a transfection protocol is a confluent, polar cell layer, one is then dealing with a situation in which transfection reagents or plasmids have access to only half of the total cell surface (i.e., the apical or upper-facing cell membrane). This is true when you present reagents or plasmids to cell layers on a solid substratum or when you present reagents or plasmids only to the apical fluid compartment of cell layers on a permeable filter substratum, such as a Millicell or Transwell insert. When transfection reagents or plasmids are presented to cells on a solid substratum, the cell layer barrier will restrict access to the undersurface of the cell layer and the basal-lateral membrane. One could perhaps improve transfection efficiencies by presenting transfection reagents or plasmids to both cell surfaces with cell layers on permeable substrata (e.g., presenting to both fluid compartments of Millicell or Transwell apparatuses), but it is worth considering that only a fraction of the entire cellular basal-lateral surface is sitting atop pore openings in the polycarbonate or polystyrene membrane support. The penetration of micellar complexes through the filters could thus be problematic. In addition, one is faced with gravity pulling down micellar complexes in suspension, away from the overhead basal-lateral cell surface.
As one might use sandpaper to roughen a surface prior to painting, we reasoned that trypsin and EDTA could similarly be used to abrade a cell layer prior to transfection. EDTA’s chelation of Ca++/Mg++ would open TJ barriers, thereby opening access to the basal-lateral cell membranes. Also, trypsin proteolysis of integral membrane proteins may make the heavily protein-populated apical membrane of a differentiated epithelial cell (hydrolases, channels, transporters, etc.) more receptive for fusion with the liposomal, micellar complexes containing the plasmid DNA, resulting in improved intracellular delivery. The data of Fig. 1 showing increased expression of transfected VP40 protein when cells were pretreated with trypsin and EDTA before Lipofectamine exposure indicate that one or both effects are occurring here.
The data shown in Figs. 2 and 3 vs. Fig. 4 indicate that increased transfection efficiency is only half of the overall issue in delivering plasmids to a differentiated epithelial cell layer in the context of a barrier function study. Transient transfections are, of course, “transient,” and the transfected protein is not persisting for long in its expression. In the case of CACO-2 and the Ebola VP40 protein, expression begins declining substantially by 72 h post-transfection. However, the steps being taken to transfect (namely, treatment with protease + chelator + detergent) are injurious to what one wishes to study here (namely, barrier function). Therefore, the price being paid for effective transfection efficiencies is temporary loss of the phenomena under study (namely, TJ complexes and general barrier function). As shown in Fig. 4, barrier function recovers, but it does so in the time frame in which one’s expressed protein of interest can be waning, creating a relatively narrow window in which to perform one’s observations and measurements.
Underlying these issues is one key central issue: using transient transfection methods like these makes it difficult to analyze the effect of an expressed protein on (formed, functional) TJ complexes. It may well be impossible because one’s transfection methods and reagents (not only the transfected plasmid) are changing the TJ complexes and epithelial barriers that one is attempting to measure. [In a separate experiment, we observed that the transfection reagents (Lipofectamine 3000 + trypsin and EDTA pretreatment) impaired barrier function to the same degree when plasmid was transfected or a mock transfection (no plasmid) was performed (unpublished results).] One is, however, able to observe effects of a transfected gene and its expressed protein on the (re)formation of TJ complexes and barrier function. This can be of considerable physiologic and medical interest because, in certain tissue compartments, such as intestinal crypts, this is exactly what is continually transpiring.
One final consideration is that an investigator conducting barrier function studies should not get overly invested intellectually in the allure of focusing only on TJ complexes. It is quite probable that transfection methods like those previously described may not only open TJ complexes but also detach (more than a few) cells from one’s cell layer/barrier. If this occurs with sufficient frequency in the cell layer (i.e., if sufficient barrier area is involved), then the rules of parallel resistors will weigh in, as paracellular leak will not only occur through open TJ complexes but also through multimicron-sized holes in the barrier. Barrier function measurements such as Rt and Jm will not only be influenced by the degree of TJ leakiness but also by the number and size of holes in the barrier. Restoration of barrier function will correspondingly be a function of the changes in TJ complexes that reduce leakiness through these complexes and will also be a function of the reduction in the number or size of barrier holes, a process involving cell migration and cell proliferation.
CONCLUSIONS
In summary, transient transfection using detergent-like reagents with a trypsin and EDTA preliminary step will of necessity perturb the barrier function of a differentiated epithelial cell layer by opening TJ complexes or creating some cell detachment or death. After the transfection, one is left with a barrier that needs to recover. The situation, then, is that one is examining the effect of what one has transfected into the cells, on the (re)formation of a barrier, rather than on the existing barrier per se. It is an important limitation and distinction. To cleanly examine the effect of a transfected and expressed protein on a fully formed and existing barrier, one would need to achieve transfection and expression without any significant perturbation of the barrier and its elements, which will prove elusive using standard transient transfection reagents. Alternatively, one would have to deliver the protein of interest via a different mechanism entirely, such as lentivirus particles, or development of, for example, an inducible, stably transfected cell line.
ACKNOWLEDGMENTS
This research was supported in part by a grant from the National Institutes of Allergy and Infectious Diseases (NIH R21AI139392-01 to R.N.H. and J.M.M.). The authors thank Sandra Alyanakian and Kate Ciavarelli for editorial support in preparing this manuscript. The authors declare no conflicts of interest.
REFERENCES
- 1.Cryan SA, O’Driscoll CM. Mechanistic studies on nonviral gene delivery to the intestine using in vitro differentiated cell culture models and an in vivo rat intestinal loop. Pharm Res 2003;20:569–575. [DOI] [PubMed] [Google Scholar]
- 2.Blais A, Bissonnette P, Berteloot A. Common characteristics for Na+-dependent sugar transport in Caco-2 cells and human fetal colon. J Membr Biol 1987;99:113–125. [DOI] [PubMed] [Google Scholar]
- 3.Gibson MC, Perrimon N. Apicobasal polarization: epithelial form and function. Curr Opin Cell Biol 2003;15:747–752. [DOI] [PubMed] [Google Scholar]
- 4.Brandsch C, Friedl P, Lange K, Richter T, Mothes T. Primary culture and transfection of epithelial cells of human small intestine. Scand J Gastroenterol 1998;33:833–838. [DOI] [PubMed] [Google Scholar]