Abstract
Objective:
This study aimed to investigate the incidence of bifid mandibular canals (BMCs) using high-resolution MRI with a three-dimensional volumetric interpolated breath-hold examination sequence (3D-VIBE) through the neurovascular bundle (NVB).
Methods:
In this retrospective study, we extracted 154 datasets from our archive of patients who underwent MRI examination with a 3D-VIBE sequence for mandible lesions from January 2015 to April 2016. The right and the left mandibles were treated independently with 59 cases excluded due to NVB morphology or artifacts, yielding 249 hemi-mandible cases classified among three subtypes: Type 0 with no BMC, Type one with one NVB and two NVBs on route to it, and Type two with two NVBs. We also investigated the incidence of nutrient canals (NCs) using MRI. Finally, we determined whether each BMC case could also be identified via panoramic radiography (PR) or CT.
Results:
Of the 249 cases examined, 6.4% were found to have BMC (Types 1 and 2). Subtypes were classified as follows: 233 as Type 0 (93.6%), 11 as Type 1 (4.4%), and 5 as Type 2 (2.0%). The NC was identified on MRI in a majority of cases. No BMCs were identified using PR or CT except for one, which was identified by CT.
Conclusion:
The incidence rate of BMC per MRI was 6.4% in this study. NCs, including the retromolar canal, had an incidence rate of 58.4-97.6%. Further, BMCs were not verified by PR or CT, indicating that MRI should be used to assess BMCs
Keywords: incidence, magnetic resonance imaging, mandible, panoramic, radiography, tomography, X-ray computed
Introduction
The bifid mandibular canal (BMC) is a normal anatomic variation of the mandible that is rarely detected by dental clinicians. It is important for clinicians to be aware of its existence because amputation of the BMC might cause unexpected bleeding and neurosensory disturbances. It occurs at a rate of 0.08 to 8.3% per panoramic radiography (PR) studies1–4 or 10 to 65% per cone-beam CT for dental use (CBCT).3–7 Based on these studies, CBCT appears to reveal BMCs more frequently than does PR. This may be because CBCT delivers three-dimensional thin-slice sections that enable identification of the BMC while PR provides only two-dimensional and one plane tomographic images that allow for less detection of the BMC. Furthermore, PR-based imaging may result in confusing the mylohyoid groove or mylohyoid nerve with the BMC.3,4,7 The canal can be found on CT or CBCT image by identification of the cortical bone structures itself or by the absence of cancellous bone structures in a corresponding location on the mandible; however, this might limit the detection of the BMC, which can appear similar to the mandibular canal (MC) on CT or CBCT.8,9 Recently, it was reported that the neurovascular bundle (NVB) within the MC may be clearly visualized by MRI10 even in cases where CT imaging did not allow for its identification.11 To the best of our knowledge, no studies have investigated the identification of BMC using MRI, although some studies have reported on the visibility of the MC by 3T MRI, including three-dimensional volumetric interpolated breath-hold examination sequence (3D-VIBE). However, the number of cases in these studies was insufficient to evaluate the visibility of BMC. Hence, the present study sought to investigate the BMC incidence rate as identified by high resolution MRI with a 3D-VIBE through the neurovascular bundle (NVB). This sequence allows acquisition of images with small, isotropic voxels that enable 3D visualization of the NVB and has been employed in several studies.10–13
Methods and Materials
Patients
To investigate the incidence of BMC in MR images, we extracted 154 datasets from the Tokyo Medical and Dental University imaging archive for patients who underwent MRI with 3D-VIBE for mandible lesions between January 2015 and April 2016.11 The ages of these patients (81 males and 73 females) ranged from 11 to 90 years (mean: 58 years). The right and the left mandibles were treated independently and 59 of the total 308 cases were excluded due to the NVB passing through a lesion or the NVB being poorly imaged due to metallic or motion artifacts. A final 249 hemi-mandibles were enrolled in the present study.
This study was approved by the institutional review board of Tokyo Medical and Dental University (No. D2015-530-01) and the need to obtain informed patient consent was waived due to its retrospective design.
MRI examination
MR images were obtained using a Magnetom Spectra 3T MRI scanner (Siemens Healthcare, Forchheim, Germany) with 16-channel head and neck array coil. 3D-VIBE sequence scanning was performed as part of the patients’ routine clinical care, with parameter settings as follows: repetition time/echo time of 113.7/3.9 msec., a flip angle of 20 degrees, a field of view of 150 × 150 mm, a matrix size of 192 × 192, a slab thickness of 96 mm and 120 slices providing a spatial resolution of 0.78 × 0.78 × 0.78, and a scan time of 3.35 mins. All examinations were performed after intravenous administration of gadodiamide hydrate (1.0 mmol kg–1).
Evaluation of the images
The incidence of BMC on the 3D-VIBE images was determined independently by two radiologists on a Syngo.via workstation (VB20A; Siemens, Munich, Germany) with a 24.1-inch light-emitting diode monitor (EIZO; Ishikawa, Japan) in a dim room. The radiologists observed the images by freely adjusting sectional planes and window settings on the workstation as needed. BMCs were determined based on the appearance of a double canal with two NVBs running parallel on a sagittal image. The objects were observed and classified as one of three types: Type 0 as a single NVB (an ordinary MC), Type one as a BMC which originated from one NVB at the mandibular foramen and split into two NVBs along its course, and Type two as a BMC originating from two divided NVBs at the mandibular foramen and running in parallel. Representative MR images are in Figure 1. Thereafter, we investigated the incidence of the nutrient canal (NC), defined as the branch arising from the main canal visible on the sagittal image. Once identified, the course of each NC was followed and the NC count was recorded at each destination site, which was divided into the teeth and the interproximal area from the canines to the retromolar areas.
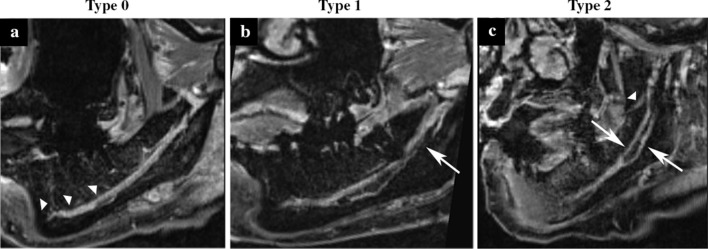
Figure 1.
Three classifications for bifid mandibular canals. Sagittal images were obtained using MRI with three-dimensional volumetric interpolated breath-hold examination sequence. (a) The left mandible of a 48-year-old female. The image depicts a single mandibular canal, which was classified as Type 0. Several nutrient canals are also observed in this section (arrowheads). (b) The left mandible of a 54-year-old female (case number eight in Table 3). Two neuro-vascular bundles (NVB) are divided by the course of one NVB. This was classified as Type 1. The inferior NVB was interrupted around the molar apex (indicated by an arrow) because it meandered out of the section. (c) The left mandible of an 87-year-old female (case number 13 in Table 3). Two NVBs (arrows) are entering the mandible and running in parallel. This was classified as Type 2. In this case, the two NVBs merged. The retromolar canal is also seen in this section (arrowhead).
We also cross-checked whether each BMC that was identified by MRI could also be found either on PR- or CT-archived images. The PR was obtained by Veraviewepocs® (Morita corp., Kyoto, Japan), operated with a tube voltage of 76–80 kV, a tube current of 6–10 mA, and an examination time of 7.7 sec. The latent image was captured with a 10 × 12 inch imaging plate and visualized with a Fuji Computed Radiography system (both FUJIFILM Medical Co., Ltd, Tokyo, Japan). The CT was performed with a Somatom Sensation 64 scanner (Siemens, Munich, Germany), operated with a tube voltage of 120 kV, an effective tube current of 140 mA or a quality effective current of 190 mA, a collimation of 64 × 0.6 mm, and a pitch of 0.6. For patients younger than 12 years of age, reduced-quality effective tube currents of 45–70 reference mA were applied. Sectional images were used and reconstructed with a bone kernel with a 0.6 mm slice thickness and 0.3 mm slice increment. When BMC were not identified by CT, we utilized a fusion volumetric image of MRI and CT, which was created on Syngo.via workstation as described previously.11 A “red” lookup table for MRI was selected on the fusion image, which turned high signal intensities to a bright red color.
These observations were repeated separately two times and with 3-week intervals. Any disagreement between the two radiologists was resolved by discussion and a consensus was reached.
Statistical analyses
Intra- and inter observer reliability was evaluated via intraclass correlation coefficients (ICCs). IBM SPSS Statistics software version 20.0 (IBM Corp., Armonk, NC) was used.
Results
We first assessed whether the BMC could be identified in the MRI images of 249 hemi-mandibles and classified those identified into three types. Intra observer reliabilities for the two radiologists were 0.883 and 0.927, and inter observer reliability was 0.869, values which indicated almost perfect agreement,14 indicating their reliability and reproducibility. These results are shown in Table 1. Type 0 was used to designate ordinary canals, while BMCs were classified as either to Type one or 2. The incidence of BMC by MRI was the summation of Types 1 and 2, found here to be 6.4%.
Table 1.
The bifid mandibular canal (BMC) classification based on MRI
| BMC classification | Type 0 | Type 1 | Type 2 | Total |
| Number (%) | 233 (93.6) | 11 (4.4) | 5 (2.0) | 249 (100) |
The incidence rate of NCs on MRI are summarized in Table 2. NCs were found in 58.4 to 97.6% of cases and their identification was dependent on the area between the canine teeth and the retromolar area. Intra observer reliabilities were 0.758 and 0.809 and inter observer reliability was 0.831 for this measure, all indicating good levels of agreement.14
Table 2.
Nutrient canal identification rates per MRI
| Area | 3 | 3/4 | 4 | 4/5 | 5 | 5/6 | 6 | 6/7 | 7 | Retromolar |
| Number | 219 | 204 | 236 | 212 | 244 | 191 | 237 | 146 | 227 | 208 |
| % of the total cases | 88.0 | 81.9 | 94.8 | 85.1 | 98.0 | 76.7 | 95.2 | 58.6 | 91.2 | 83.5 |
The 3, 4, 5, 6, and seven indicate the canine, first premolar, second premolar, first molar, and second molar, respectively.
The 3/4 indicates the area between the canine and the firsit premolar area. 4/5, 5/6, and 6/7 are similar to 3/4.
We finally assessed whether the BMC cases identified by MRI could be identified either by PR or CT (Table 3). There were 16 BMC cases identified by MRI and while PR did not identify BMC in any of these, CT did in only one of the 13 cases assessed (three cases from the full cohort did not have CT data). Representative cases are presented in Figures 2 and 3.
Table 3.
The bifid mandibular canal (BMC) cases identified on MRI
| Case No. | BMC type | Sex | Age (years) | Side | Pranoramic radiography | CT |
| 1 | 1 | Male | 37 | Right | Type 0 | Type 0 |
| 2 | 1 | Male | 50 | Left | Type 0 | Type 0 |
| 3 | 1 | Male | 29 | Left | Type 0 | Type 0 |
| 4 | 1 | Female | 85 | Left | Type 0 | Type 0 |
| 5 | 1 | Female | 35 | Left | Type 0 | Type 0 |
| 6 | 1 | Female | 57 | Left | Type 0 | NA |
| 7 | 1 | Female | 38 | Right | Type 0 | Type 0 |
| 8 | 1 | Female | 54 | Left | Type 0 | NA |
| 9 | 1 | Female | 36 | Right | Type 0 | Type 0 |
| 10 | 1 | Male | 73 | Left | Type 0 | Type 0 |
| 11 | 1 | Female | 19 | Left | Type 0 | NA |
| 12 | 2 | Male | 40 | Right | Type 0 | Type 2 |
| 13 | 2 | Male | 58 | Right | Type 0 | Type 0 |
| 14 | 2 | Female | 87 | Left | MC was not identified | Type 0 |
| 15 | 2 | Female | 59 | Left | Type 0 | Type 0 |
| 16 | 2 | Female | 12 | Right | MC was not identified | Type 0 |
NA, indicates not available;
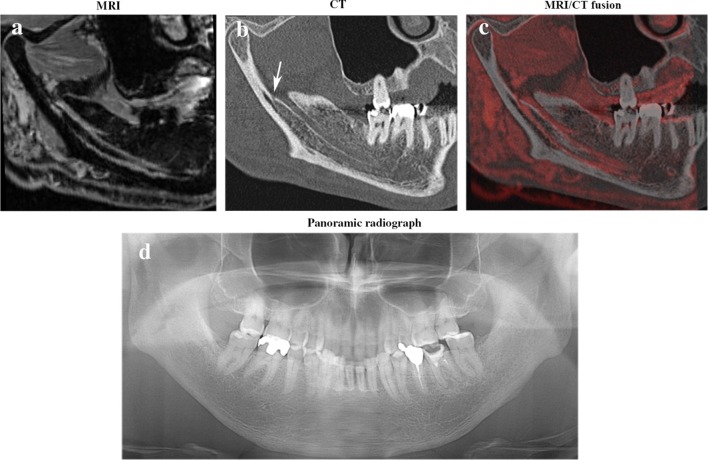
Figure 2.
A Type two bifid mandibular canal (BMC) case that was identified using both MRI (a) and CT (b) in a 40-year-old male (case number 12 in Table 3). It is somewhat difficult to indicate the inferior of bifid mandibular canal on CT because of its thin cortical wall, although its bifurcation (arrow) is clearly visible. However, a MRI/CT fusion image (c) reveals the BMC and its surrounding structures. A panoramic radiograph (d) did not reveal the BMC. Note that there is only a single mandibular foramen despite two neuro-vascular bundles. (a), (b), and (c) were taken in the same sectional plane.
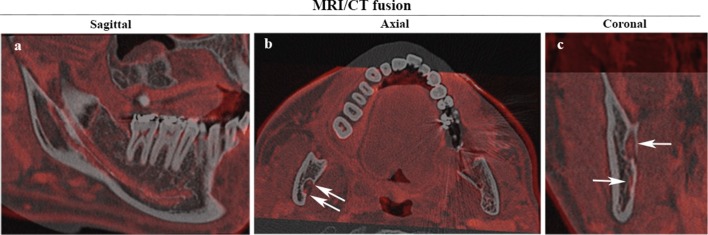
Figure 3.
A Type two bifid mandibular canal case. An MRI/CT fusion image reveals the right mandible of a 58-year-old male (case number 13 in Table 3), which clearly indicates a Type two morphology in the sagittal plane (a). However, a single mandibular foramen is indicated by axial (b) and coronal (c) images. Arrows indicate neuro-vascular bundles.
Discussion
In this study, we aimed to investigate BMC incidence using MRI and successfully classified 249 hemi-mandibles into three types on the basis of the presence of BMC and the number of NVBs. Although there have been many studies on BMC, these have primarily used PR or CT imaging modalities. Additionally, in comparing PR and CT, PR-based findings do not necessarily align with those derived from CT and the accuracy of PR seems to be poor.4,6–8,15 Hence, CT is recommended for the examination of BMC. However, MC identification using CT image relies on bone texture findings, a potential methodological weak point.8,9 High resolution MR images can reveal the NVB within the MC, as recent advances in MRI technologies have decreased voxel sizes to 0.78 mm (length × width × height cube).10,11 Hence, a potential strength MRI is its superior resolving power, which improves the ability of this modality to identify BMCs and their branches at a high rate, as shown in the present study.
In our assessment of 249 hemi-mandibles, we yielded a BMC rate of 6.8%. As multiple BMC classifications exist and vary across the literature, especially with regard to inclusion of the retromolar canal, comparing our results to those of previous reports is somewhat challenging. We contend here that the retromolar canal is an important structure because its disturbance can cause unexpected bleeding and/or nerve palsies after procedures such as tooth extractions or orthodontic osteotomies. Additionally, the MC and its many branches have a critical role in providing blood flow and sensory innervation to the alveolar bone and teeth. In the present study, we identified the NC in the retromolar area in 83.2% of the cases assessed, a rate that supersedes all others we found in the existing clinical literature1,3–7 and is similar to that identified in a postmortem study.16 In addition, we identified NCs in other areas at a rate as high as that in the retromolar area (Table 2), although this rate was relatively low (58.4%) in 6/7 cases. We consider that the low value in the 6/7 cases may be attributed to the narrow intertooth area. Therefore, we contest that the retromolar canal is not irregular, but rather always exists in the mandible and should be treated as an NC. Given this, we extracted rates from past studies and determined that the incidences of the BMC (without counting the retromolar canal) reported previously were 0.78% (28/3612),1 1.2% (60/50000),3 0.35% (7/2012),4 and 0.7% (2/301).5 The rate that we report here (6.4%) is considerably higher than these, which would be expected as NVB identification by MRI would be superior to canal identification by PR or CT. However, past studies have reported bilateral BMCs, but we did not encounter any such cases here. This may be due to our limited sample size or to the exclusion criterion used in the present study that the NVB must not pass through a lesion site.
We further defined Type 2 BMCs as having two mandibular foramens in the present study. However, MRI/CT fusion images revealed that all five Type two cases assessed here had only a single mandibular foramen and two separate NVBs, which entered into the mandible from the foramen as shown in Figures 2 and 3. Choi et al reported that the incidence of two mandibular foramens was 1.35%.17 Given this, the probability of our encountering such a case would be one in every 74 cases. Despite our sample size being sufficient to reveal several of these cases, we did not observe them. We attribute this to our relatively small sample size and the fact that we were unable to clarify the number of mandible foramens using MR imaging alone-CT imaging is required to confirm these.
In the present study, we identified 16 BMC cases, although most could not be identified by CT alone (Table 3). Although the incidence rate was as low as 6.4%, these data suggest that dental clinicians should remain vigilant and conduct MR imaging prior to performing surgeries such as osteotomies. Advances in imaging technology have enabled both clinicians and researchers to obtain more information about small, detailed structures in the oral and maxillofacial regions. However, the clinical significance of these advances has not been studied sufficiently and it is thus critical that future studies seek to evaluate how the information obtained from these images should be put to use in practical settings. To reveal the potential clinical significance, more BMC cases with lesions should be evaluated in future studies with regard to the surgical and pathological findings and prognosis. The use of MRI for identifying BMCs may be limited by the restricted availability of MRI in clinical settings. Further, MRI has the potential to provide more precise images in future, but the images in the current study seemed to be of sufficient quality for detecting BMCs.
Conclusion
In the present study, the incidence rate of BMC by MRI was investigated and found to be 6.4%. NCs were also studied and their incidence was found to be between 58.4 and 97.6%, depending on the distribution of the individual’s teeth and/or their interproximal area. Most BMCs were not verified by further PR or CT imaging, indicating that MRI should be used to accurately image the BMC. We believe that the results of our study will be useful in the field of dentomaxillofacial surgery.
Footnotes
Acknowledgment: This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Number 16K11498. We would like to thank Editage (www.editage.jp) for English language editing.
The authors Peerapong Wamasing and Chutamas Deepho contributed equally to the work.
REFERENCES
- 1. Nortjé CJ , Farman AG , Grotepass FW . Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients . Br J Oral Surg 1977. ; 15 : 55 – 63 . doi: 10.1016/0007-117X(77)90008-7 [DOI] [PubMed] [Google Scholar]
- 2. Durst JH , Snow JE . Multiple mandibular canals: oddities or fairly common anomalies? Oral Surg Oral Med Oral Pathol 1980. ; 49 : 272 – 3 . doi: 10.1016/0030-4220(80)90060-2 [DOI] [PubMed] [Google Scholar]
- 3. Kalantar Motamedi MH , Navi F , Sarabi N . Bifid mandibular canals: prevalence and implications . J Oral Maxillofac Surg 2015. ; 73 : 387 – 90 . doi: 10.1016/j.joms.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 4. Sanchis JM , Peñarrocha M , Soler F . Bifid mandibular canal . J Oral Maxillofac Surg 2003. ; 61 : 422 – 4 . doi: 10.1053/joms.2003.50004 [DOI] [PubMed] [Google Scholar]
- 5. Kuribayashi A , Watanabe H , Imaizumi A , Tantanapornkul W , Katakami K , Kurabayashi T . Bifid mandibular canals: cone beam computed tomography evaluation . Dentomaxillofac Radiol 2010. ; 39 : 235 – 9 . doi: 10.1259/dmfr/66254780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Naitoh M , Hiraiwa Y , Aimiya H , Ariji E . Observation of bifid mandibular canal using cone-beam computerized tomography . Int J Oral Maxillofac Implants 2009. ; 24 : 155 – 9 . [PubMed] [Google Scholar]
- 7. Muinelo-Lorenzo J , Suárez-Quintanilla JA , Fernández-Alonso A , Marsillas-Rascado S , Suárez-Cunqueiro MM . Descriptive study of the bifid mandibular canals and retromolar foramina: cone beam CT vs panoramic radiography . Dentomaxillofac Radiol 2014. ; 43 : 43 . doi: 10.1259/dmfr.20140090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. de Oliveira-Santos C , Souza PH , de Azambuja Berti-Couto S , Stinkens L , Moyaert K , Rubira-Bullen IR , et al. . Assessment of variations of the mandibular canal through cone beam computed tomography . Clin Oral Investig 2012. ; 16 : 387 – 93 . doi: 10.1007/s00784-011-0544-9 [DOI] [PubMed] [Google Scholar]
- 9. Takahashi A , Watanabe H , Kamiyama Y , Honda E , Sumi Y , Kurabayashi T . Localizing the mandibular canal on dental CT reformatted images: usefulness of panoramic views . Surg Radiol Anat 2013. ; 35 : 803 – 9 . doi: 10.1007/s00276-013-1120-6 [DOI] [PubMed] [Google Scholar]
- 10. Weckx A , Agbaje JO , Sun Y , Jacobs R , Politis C . Visualization techniques of the inferior alveolar nerve (IAN): a narrative review . Surg Radiol Anat 2016. ; 38 : 55 – 63 . doi: 10.1007/s00276-015-1510-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Deepho C , Watanabe H , Kotaki S , Sakamoto J , Sumi Y , Kurabayashi T . Utility of fusion volumetric images from computed tomography and magnetic resonance imaging for localizing the mandibular canal . Dentomaxillofac Radiol 2017. ; 46 : 46 . doi: 10.1259/dmfr.20160383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Imamura H , Sato H , Matsuura T , Ishikawa M , Zeze R . A comparative study of computed tomography and magnetic resonance imaging for the detection of mandibular canals and cross-sectional areas in diagnosis prior to dental implant treatment . Clin Implant Dent Relat Res 2004. ; 6 : 75 – 81 . doi: 10.1111/j.1708-8208.2004.tb00029.x [DOI] [PubMed] [Google Scholar]
- 13. Chau A , Anson C . Comparison between the use of magnetic resonance imaging and conebeam computed tomography for mandibular nerve identification . Clin Oral Implants Res 2012. ; 23 : 253 – 6 . doi: 10.1111/j.1600-0501.2011.02188.x [DOI] [PubMed] [Google Scholar]
- 14. Bartko JJ . The intraclass correlation coefficient as a measure of reliability . Psychol Rep 1966. ; 19 : 3 – 11 . doi: 10.2466/pr0.1966.19.1.3 [DOI] [PubMed] [Google Scholar]
- 15. Fukami K , Shiozaki K , Mishima A , Kuribayashi A , Hamada Y , Kobayashi K . Bifid mandibular canal: confirmation of limited cone beam CT findings by gross anatomical and histological investigations . Dentomaxillofac Radiol 2012. ; 41 : 460 – 5 . doi: 10.1259/dmfr/60245722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schejtman R , Devoto FC , Arias NH . The origin and distribution of the elements of the human mandibular retromolar canal . Arch Oral Biol 1967. ; 12 : 1261 – IN9 . doi: 10.1016/0003-9969(67)90127-6 [DOI] [PubMed] [Google Scholar]
- 17. Choi YY , Han SS . Double mandibular foramen leading to the accessory canal on the mandibular ramus . Surg Radiol Anat 2014. ; 36 : 851 – 5 . doi: 10.1007/s00276-014-1310-x [DOI] [PubMed] [Google Scholar]