Abstract
Objectives
To evaluate the usefulness of the mandibular cortical index (MCI) obtained by digital panoramic radiography (DPR) and by panoramic reconstruction (PR) of cone-beam CT (CBCT) with three different slice thicknesses for the screening of low bone mineral density (BMD) in post-menopausal women.
Methods
Two trained oral and maxillofacial radiologists assessed the MCI based on the morphology of the mandibular bone cortex (classified as C1, C2 or C3). The DPR and PR of CBCT with slice thicknesses of 5, 15 or 25 mm were compared to the BMD obtained by dual-energy X-ray absorptiometry (DXA) in post-menopausal women. Measures related to accuracy were calculated with MedCalc software. The confidence interval was set at 95%.
Results
54 women (mean age 58.70 ± 7.35 years) participated in the study. The sensitivity and specificity values obtained for DPR were 52.6% and 56.2%, respectively, and values for PR of CBCT with 5, 15, and 25 mm slice thicknesses were 63.1% and 43.7%, 50.0% and 50.0%, and 52.6% and 62.5%, respectively. For the tools evaluated, the positive likelihood ratio ranged from 1.00 to 1.40 and negative likelihood ratio from 0.76 to 1.00. The positive predictive value (PPV) ranged from 70.4 to 76.9% and the negative predictive value (NPV) from 29.6 to 35.7%. Among the examinations, the highest value for area under the curve (AUC) was obtained for CBCT with 25 mm slice thickness (57.6%).
Conclusions
The MCI calculated by DPR and CBCT differed with regard to accuracy. Within the limitations of this study, the PR of CBCT with 25 mm slice thicknesses seems to be the most accurate among the examinations evaluated. Should the dentist be attentive, DPR and CBCT may be useful tools for the screening of low BMD in post-menopausal women, facilitating their timely referral for further assessment.
Keywords: cone-beam CT, dual-energy radiographic absorptiometry, jaw, osteoporosis, panoramic radiography, post-menopausal
Introduction
Osteoporosis is a chronic, multifactorial condition characterized by low bone mineral density (BMD) caused by deterioration of the bone tissue structure. It is often progressive and asymptomatic, and its diagnosis is challenging.1,2 Osteoporosis mostly affects older people, and is usually detected at an advanced stage when the patient may present bone fractures. Fractures are clinically relevant implications of the disease due to their association with morbidity and mortality.3,4 The risk for osteoporosis is also higher among post-menopausal females, as age and estrogen deficiency are both recognized as factors associated with a reduction in bone mass.1,5
Dual-energy X-ray absorptiometry (DXA) is the gold standard method for measuring bone mass.6–8 This examination uses the BMD deviation values of healthy young adults (T-score) as a reference, and patients are classified according to the criteria defined by the World Health Organization.9 Values for BMD are measured in the proximal femur, lumbar spine, and hip. Although reliable, the high cost of DXA represents a disadvantage of this method.2,10
Panoramic radiography has been indicated as a predictive tool for osteoporosis in several studies.4,11–14 A change in the cortical morphology of maxillofacial bones makes it possible to screen patients by this method. This type of examination is often used in clinical practice, and is widely accessible due to its low cost. More recently developed tools, such as digital panoramic radiography (DPR) and cone-beam CT (CBCT), may also be used. The former has improved image quality; however, distortions, overlaps, and extensions still limit the analysis of anatomical features. In contrast, the latter is more detailed as it provides a three-dimensional perspective, and is widely used to evaluate patients’ bone structure in dentistry and associated subspecialties.2,5,8,12,15
Qualitative and quantitative indices have been created to standardize the assessment of BMD in dental imaging.2,6–8,11,16,17 The most frequently used qualitative index is the mandibular cortical index (MCI), also known as the Klemetti index. The MCI evaluates the morphology of the mandibular cortical bone based on the presence of lacuna or porosities.18 It has been recognized that DPR and CBCT provide accurate images with improved resolution, which can be reliably used to measure the thickness of anatomical structures.2,5,16 However, it is still unclear whether the MCI classification obtained by DPR and panoramic reconstruction (PR) of CBCT is a reliable and helpful measure for predicting low BMD. Therefore, it is important to assess the usefulness of both dental examinations compared with DXA, which is the gold standard for the detection of low BMD.
In order to assess the relevance of oral and maxillofacial imaging in the appraisal of patients with low BMD, the aim of this study was to evaluate the usefulness of the MCI obtained by DPR and by PR of CBCT with three different slice thicknesses (5, 15 or 25 mm) as ancillary tools to detect low BMD in post-menopausal females. We hypothesized that PR of CBCT would be more accurate than DPR when analyzing the morphology of mandibular cortical bone.
Methods and Materials
Patient selection
The participants were post-menopausal females between the ages of 49 and 80 years, who were referred for treatment at the Department of Oral Surgery and Pathology of the School of Dentistry, Universidade Federal Minas Gerais (UFMG; Belo Horizonte, Minas Gerais, Brazil). DPR and CBCT examinations, performed with an indication for dental implants between 2014 and 2016, were randomly selected for inclusion in the study. The analyses for the present study were conducted in 2017. Individuals were excluded if they met any of the following criteria: (1) metabolic bone disease (hyperparathyroidism, hypoparathyroidism, Paget’s disease, osteomalacia or osteogenesis imperfect), (2) diabetes, (3) malignant neoplasm with bone metastasis, (4) kidney disease, (5) ovariectomy, or (6) use of medications that might affect bone metabolism. Individuals undergoing hormone replacement therapy, those submitted to calcium and vitamin D supplementation for at least 6 months, or individuals with missing data were also excluded.
This study was approved by the Institutional Ethics Committee of the UFMG (protocol n°. 903530). Following a clear explanation of the study objectives, all individuals who chose to participate signed a statement of informed consent.
Imaging acquisition
The time elapsed between the DXA and the DPR and CBCT was no longer than 2 weeks.
The DPR images were taken using the KODAK 9000C 3D® system (Kodak Dental Systems, Carestream Dental LLC, Atlanta, GA), with a tube voltage of 70 kVp, tube current of 10 mA, and a scan time of 20 s. A trained operator conducted the examinations. All DPR images were saved in JPG format with 264-dpi resolution. The DPR images were evaluated using Adobe Photoshop 7.0 (Adobe Systems, San Jose, CA) with a standardized image increase of 66.6%.
The PR of CBCT images were obtained using the same equipment with a voxel size of 200 µm, field of view of 50 mm diameter ×37 mm height, tube voltage of 72 kVp, tube current of 10 mA, and scan time of 32.40 s. The Digital Imaging and Communications in Medicine files were processed using the panoramic cutting curve function in Imaging Studio 3.2® (Anne Solutions, São Paulo, SP, Brazil). The panoramic cutting curve was drawn on the axial image in which the two mental foramens were most visible.2 The PR of CBCT templates were observed in full-screen using Implant Viewer software (Anne Solutions, São Paulo, SP, Brazil) for three different slice thicknesses, 5, 15, and 25 mm.
The analyses of all images were carried out on a single 15’ LG monitor (LG Electronics, Taubaté, SP, Brazil) at night in a room with dimmed light. The evaluation was static, i.e. contrast and brightness were enhanced and standardized before the evaluation of all examinations, with no alteration in these parameters during the entire assessment.
The DXA was obtained with the Hologic Discovery DXA System® (Hologic Inc., Bedford, MA) by the same operator. The BMD was evaluated at the femoral neck and lumbar spine (L1–L4). The WHO9 criteria consider the following scores: normal BMD (T-score ≥ −1), osteopenia (−1 > T -score>−2.5), and osteoporosis (T-score ≤−2.5). In this study, two groups were categorized according to DXA: normal BMD (T-score ≥ −1) and low BMD (−1 > T -score>−2.5 and T-score ≤−2.5).
MCI classification
According to Klemetti et al,18 the MCI has three categories: C1, C2, and C3. Patients classified as C1 presented a homogeneous mandibular cortical bone, with no erosion; patients classified as C2 showed at least one mandibular cortex with erosions in the more superficial portion; whereas patients in category C3 had numerous erosions that compromised more than two-thirds of the height of the mandibular cortex, as shown in Figure 1 (DPR) and Figure 2 (PR of CBCT). The mandibular cortical bone region was evaluated bilaterally from the mental foramen to the third molar region. Each side of the mandible was assessed, and in cases with divergence in classification between the right and left side, the one with greater alteration was used for the classification.
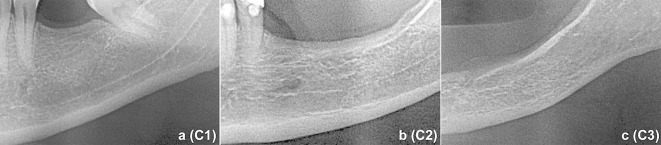
Figure 1.
MCI on the DPR. (a) Left mandibular segment of a patient classified as C1, showing no changes in cortical mandibular morphology; (b) a patient classified as C2, presenting few porosities in the most superficial layer of the mandibular cortical bone; and (c) a patient classified as C3, with larger and more numerous porosities. DPR, digital panoramic radiography; MCI, mandibular cortical index.
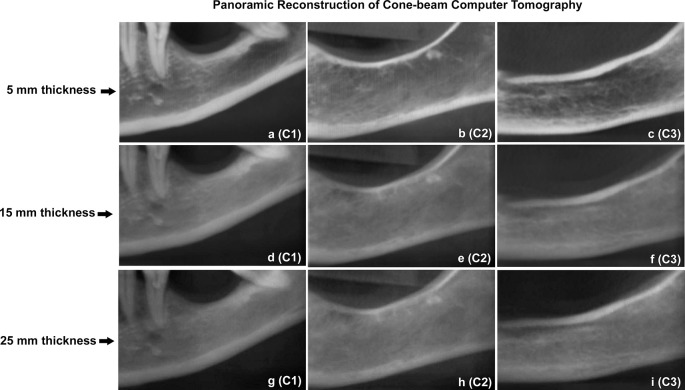
Figure 2.
MCI observed on the panoramic reconstruction of the CBCT image with 5 mm (a-c), 15 mm (d-f), and 25 mm (g-i) thicknesses. The columns correspond to the MCI classification: C1 (column 1), C2 (column 2), and C3 (column 3). CBCT, cone-beam CT; MCI, mandibular cortical index.
Two oral and maxillofacial radiologists with more than 5 years of experience separately evaluated the dental examinations. A training set was performed with 30 images, 15 DPR and 15 PR of CBCTs with five of each of the three slice thicknesses, to test the inter- and intra-examiner agreement. The 30 images were re-evaluated 15 days later to calculate the intra-examiner agreement. The kappa values were above 0.81 for both inter- and intra-examiner agreement. The images used for training were not included in the main study.
In the main study, all images obtained from DPR and CBCT were evaluated by the same two previously trained assessors. The assessors were unaware of any participant or examination information. Each assessor carried out the analyses separately. For the final MCI classification for each examination, if both assessors agreed with the diagnosis, that diagnosis persisted. In cases of disagreement, the image was re-evaluated by both assessors and a final consensus was made.
Statistical analysis
The Statistical Package for the Social Sciences 17.0 (SPSS for Windows; SPSS Inc., Chicago, IL) was used for descriptive analysis and to evaluate the intra- and inter-examiner agreement during training of the assessors. Kappa values > 0.61 were considered to represent substantial agreement.19
To analyze the usefulness of the evaluated methods for the detection of low BMD, participants were categorized into two groups according to MCI: “non-eroded” group, consisting of examinations classified as C1; and “eroded” group, with examinations classified as C2 or C3. Participants were also stratified into two groups according to DXA values: normal BMD group (T-score ≥ −1), and low BMD group [−1 > T -score>−2.5 (osteopenia) or T-score ≤−2.5 (osteoporosis)]. The sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC) were calculated using MedCalc software (MedCalc software bvba, Ostend, Flanders, Belgium). The confidence interval was set at 95%. The results are presented in dichotomous 2 × 2 tables and as AUC (receiver operator characteristic curve).
Results
A total of 58 post-menopausal females underwent the imaging tests. Four were excluded due to missing data, thus, 54 individuals participated in the study. The mean age of participants was 58.70 ± 7.35 years of age. The distribution of post-menopausal females according to the T-scores obtained from DXA values is shown in Table 1.
Table 1.
Distribution of dual-energy X-ray absorptiometry (DXA) in post-menopausal females (N = 54)
| Group | DXA | N |
| Normal BMD | T-score ≥ −1 | 16 |
| Low BMD | −1 > T -score>−2.5 and T-score ≤−2.5 | 38 |
BMD, bone mineral density; DXA, dual-energy X-ray absorptiometry according to World Health Organization criteria, 20049;
The results of the comparison of MCI groups determined by DXA with those determined by DPR and PR of CTCB with three slice thicknesses are displayed in Table 2. The sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, PPV, NPV, and AUC measures of all examinations are shown in Table 3. The sensitivity of the PR of CBCT with 5 mm thick slices was 63.1%, which was higher than the other imaging tests. The highest specificity was observed for the PR of CBCT with 25 mm thick slices (62.5%). The PR of CBCT with 25 mm thick slices also presented the highest positive likelihood ratio (1.40), the lowest negative likelihood ratio (0.76), the highest PPV (76.9%), and the highest AUC among examinations analyzed (Figure 3).
Table 2.
Classification of the mandibular cortical index in comparison to dual-energy X-ray absorptiometry test for diagnostic prediction in digital panoramic radiography and in the three thicknesses of the panoramic reconstruction of the CT cone beam (N = 54)
| Test examinations | Gold s tandard DXA | |||
| Groups | Low BMD | Normal BMD | Total | |
| Digital panoramic radiography | Eroded (C2 or C3) | 20 | 7 | 27 |
| No eroded (C1) | 18 | 9 | 27 | |
| Total | 38 | 16 | 54 | |
| Panoramic reconstruction of the CBCT 5 mm | Eroded (C2 or C3) | 24 | 9 | 33 |
| No eroded (C1) | 14 | 7 | 21 | |
| Total | 38 | 16 | 54 | |
| Panoramic reconstruction of the CBCT 15 mm | Eroded (C2 or C3) | 19 | 8 | 27 |
| No eroded (C1) | 19 | 8 | 27 | |
| Total | 38 | 16 | 54 | |
| Panoramic reconstruction of the CBCT 25 mm | Eroded (C2 or C3) | 20 | 6 | 26 |
| No eroded (C1) | 18 | 10 | 28 | |
| Total | 38 | 16 | 54 | |
BMD, bone mineral density; CBCT, cone-beam CT; DXA, dual energy radiographic absorptiometry;
Table 3.
Diagnostic accuracy found for each type of examination evaluated
| Accuracy diagnostic | Test examination | |||||||
| Digital panoramic radiography | Panoramic reconstruction of the CBCT | |||||||
| 5 mm | 15 mm | 25 mm | ||||||
| Value | 95 CI | Value | 95 CI | Value | 95 CI | Value | 95 CI | |
| Sensitivity | 52.6% | 35.8–69.0% | 63.1% | 46.0–78.2% | 50.0% | 33.4–66.6% | 52.6% | 35.8–69.0% |
| Specificity | 56.2% | 29.9–80.2% | 43.7% | 19.8–70.1% | 50.0% | 24.7–75.3% | 62.5% | 35.4–84.8% |
| Positive likelihood ratio | 1.20 | 0.60–2.30 | 1.12 | 0.70–1.80 | 1.00 | 0.60–1.80 | 1.40 | 0.70–2.80 |
| Negative likelihood ratio | 0.84 | 0.50–1.50 | 0.84 | 0.40–1.70 | 1.00 | 0.60–1.80 | 0.76 | 0.50–1.30 |
| PPV | 74.1% | 60.3–84.3% | 72.7% | 61.9–81.4% | 70.4% | 57.0–81.0% | 76.9% | 62.3–87.0% |
| NPV | 33.3% | 22.4–46.3% | 33.3% | 20.0–50.0% | 29.6% | 19.0–43.0% | 35.7% | 25.1–48.0% |
| AUC | 54.4% | 40.3–68.1% | 53.5% | 39.4–67.1% | 50.0% | 36.1–63.9% | 57.6% | 43.4–70.9% |
; AUC, area under the curve; CBCT, cone-beam CT; CI, confidence interval; NPV, negative predictive value; PPV, positive predictive value;
Figure 3.
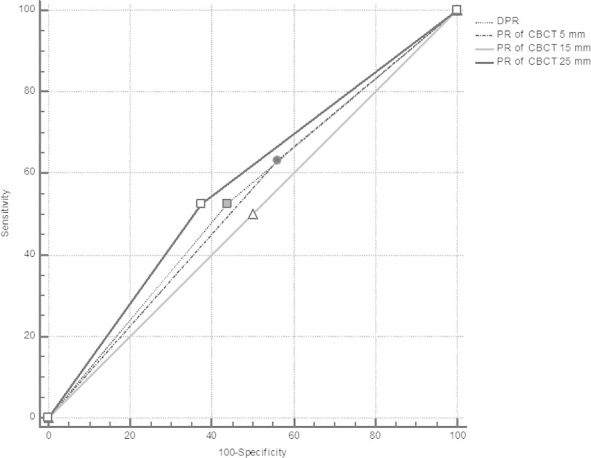
Receiver operator characteristic curves of the examination techniques analyzed and DXA. The largest AUC is represented by a dotted line, corresponding to PR of the CBCT with 25 mm slice thickness. AUC, area under the curve; CBCT, cone-beam CT; DXA, dual-energy X-ray absorptiometry; PR, panoramic reconstruction.
Discussion
Similar to previous investigations,2,4,8,11,12,16,20 this study evaluated oral and maxillofacial imaging examinations used routinely in dental practice. While the analogic PR has been already evaluated,11,18,21 the DPR and the PR of CBCT have been little explored.4,7 Likewise Klemetti et al18 this study compared two groups of females according to DXA: females with normal BMD and females with low BMD. The result of sensitivity was lower than that observed by Klemetti et al18 (71%), Taguchi et al,22 (72.6%) and Gaur et al23 (100%) for analogical PR, and Valerio et al7 (82%) for DPR. In contrast, for specificity, our result was higher than that obtained by Klemetti et al18 (40%), but lower than the results of Taguchi et al22 (65.6%) and Gaur et al23 (88%). Due to the higher sharpness of the digital image, it was expected that the DPR examination would be more accurate than analogical images. However, the value for AUC observed in our study was lower than those reported in studies assessing analogical (60%)17 and digital (62 and 71%)4,7 images.
A systematic review of studies on the detection of osteoporosis by analogical PR and DPR found significant variability among the results of the included articles. The values for sensitivity ranged from 48.7 to 100%, and specificity from 31 to 88.8%.14 Although our results support data presented elsewhere, the values of sensitivity and specificity presented here were lower than expected. Possible factors that may have contributed to this outcome include the subjective characteristic of the MCI index, anatomical variability, and sample size. It is important to perform intra- and inter-evaluator comparisons to increase the method's reliability. Experience or training of the assessors as oral radiologists appears to be associated with higher values of sensitivity and specificity.21 In this study, radiologists with more than 5 years of experience conducted the evaluation. Another factor may be the limited sample size and the presence of individuals with low anatomical variability, who showed no alteration in mandibular cortex, although they were classified as low BMD with DXA. As regards sample size, the sample of the present study makes generalization of the results unfeasible.
Positive and negative likelihood ratios represent how much more likely individuals affected by the disease are to have a positive or a negative test outcome than their peers without the disease. The former is usually a value higher than 1, and the latter is mostly a value between 0 and 1. The further the value is from a score of 1, the higher the indication to rule in or rule out the disease.24 Therefore, for the DPR, an individual with low BMD is 1.20-times more likely to have a positive test result than his/her peers with normal BMD, and is 0.84-times as likely to present a negative test result.
On the other hand, the PPV of the DPR image demonstrated a high probability (74.1%) of patients with a positive test result to genuinely have the disease. In contrast, the NPV for the same test was low (33.33%). In other words, this means that a low percentage of patients with a negative test result did not actually have the disease. The PPV and NPV depend on the prevalence of the disease. The higher the disease prevalence, the higher the PPV. The NPV, however, is lower. In clinical practice, this means that the usefulness of a test only makes sense if the prevalence of the disease is taken into account. Therefore, the PPV may be high for a given test, regardless of the sensitivity and specificity.25
Recent studies have evaluated the MCI determined by PR of CBCT; however, they did not provide measures of accuracy.2,16 Therefore, the slice thicknesses evaluated in the current study were chosen according to the sharpness and tercile of the CBCT. Among the three slice thicknesses of PR of CBCT, the 5 mm thickness presented the highest sensitivity (63.1%) but the lowest specificity (43.7%), showing a larger number of false negatives compared to the DPR examination and the PR of CBCT with 25 mm thick slices. The greatest slice thickness of CBCT (25 mm) showed values of specificity and PPV very close to those obtained in the DPR examination. This may be explained by the fact that the 25 mm thickness includes a higher number of image slices, similar to those of the DPR. In regard to AUC, the values were better for DPR and for the PR of CBCT with 25 mm slice thickness. Likelihood ratios of the PR of CBCT with 25 mm slice thickness were the most favorable of all examinations evaluated. Similar results were observed for the PPV and NPV of DPR and all three thicknesses of PR of CBCT. It is believed that the thickness of the PR of CBCT influences the MCI classification.
According to MCI classification, the tests varied in terms of accuracy for detecting low BMD in post-menopausal females. This study has some shortcomings that should be recognized. The first regards the sample size. The sample of the present study does not allow us to generalize statements regarding clinical and demographic features to the entire population of post-menopausal females. In addition, in accordance with Alonso et al2 and Gomes et al5 dynamic evaluation of the volume by CBCT may lead to more reliable interpretation of the MCI. On the other hand, this analysis would be more time-consuming to identify areas of erosion in the cortical bone and, consequently, the loss of anatomical references required for classification. It should not be forgotten that the MCI classification was originally created to analyze a static image such as DPR, while in CBCT we analyzed only slices or parts of a whole as a volumetric parameter.
Imprecision in the diagnosis of low BMD when alterations on the mandibular cortical bone are observed by means of dental examinations (DPR or CBCT) might take place. However, screenings are low cost examinations that may help the clinician to perform early diagnoses, and may facilitate timely referrals for treatment, thereby improving disease prognosis.26,27 As a diagnostic test, the examinations evaluated in this study showed poorer performance than DXA (0.50–0.60 score).27 However, as a screening test, they may be useful for the early identification of individuals with non-symptomatic low BMD undergoing dental treatment. As expected, our hypothesis was confirmed, as PR of CBCT images obtained better results than DPR. The PR of CBCT with 25 mm slice thickness also showed a better AUC.
Oral health care practitioners routinely use DPR and PR of CBCT in their daily practice in patients undergoing dental check-ups, as well as in those undergoing more specific dental procedures. Therefore, these examinations can act as ancillary tools allowing oral health care providers to assess craniofacial bones for diagnostic purposes.28 During these examinations, non-dental features may also be noticed. The intention here is not to list dental imaging as the first choice for the diagnosis of BMD, but rather to employ these methods as instruments to alert practitioners of any signs of disease. Our results show that the PR of CBCT with 25 mm slice thickness provided the most accurate measurement of the imaging methods evaluated. Awareness could lead to an important role of dental practitioners in primary care, as they could raise the issue of low BMD and refer females who may be at risk for further assessment.29
Conclusion
The MCI obtained by DPR, and by PR of CBCT with three slice thicknesses, varied with regard to accuracy. Within the limitations of this study, the PR of CBCT with 25 mm slice thickness seems to be the most accurate among the examinations evaluated. Should the dentist be attentive, DPR and PR of CBCT may be useful tools for the identification of low BMD among post-menopausal females, and subsequent referral of those individuals for further assessment.
Footnotes
Acknowledgment: This work was supported by the Brazilian National Council for Scientific and Technological Development (grant n°. CNPq #309322/2015–4). The authors thank the Coordination for the Improvement of Higher Education Personnel (CAPES). RAM is a research fellow at CNPq.
Contributor Information
Camila Nao Kato, Email: cnao20@yahoo.com.br.
Núbia PK Tavares, Email: nubiak.tavares@gmail.com.
Sâmila G Barra, Email: samilagbarra@gmail.com.
Tânia MP Amaral, Email: taniapamaral@gmail.com.
Cláudia B Brasileiro, Email: cbbrasileiro@gmail.com.
Lucas G Abreu, Email: lucasgabreu01@gmail.com.
Ricardo A Mesquita, Email: ramesquita@ufmg.br.
REFERENCES
- 1. Baccaro LF, Conde DM, Costa-Paiva L, Pinto-Neto AM. The epidemiology and management of postmenopausal osteoporosis: a viewpoint from Brazil. Clin Interv Aging 2015; 10: 583–91. doi: 10.2147/CIA.S54614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alonso MB, Vasconcelos TV, Lopes LJ, Watanabe PC, Freitas DQ. Validation of cone-beam computed tomography as a predictor of osteoporosis using the Klemetti classification. Braz Oral Res 2016; 30: e73. doi: 10.1590/1807-3107BOR-2016.vol30.0073 [DOI] [PubMed] [Google Scholar]
- 3. Tian L, Yang R, Wei L, Liu J, Yang Y, Shao F, et al. Prevalence of osteoporosis and related lifestyle and metabolic factors of postmenopausal women and elderly men: A cross-sectional study in Gansu province, Northwestern of China. Medicine 2017; 96: e8294. doi: 10.1097/MD.0000000000008294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pallagatti S, Parnami P, Sheikh S, Gupta D. Efficacy of panoramic radiography in the detection of osteoporosis in post-menopausal women when compared to dual energy X-Ray absorptiometry. Open Dent J 2017; 11: 350–9. doi: 10.2174/1874210601711010350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gomes CC, de Rezende Barbosa GL, Bello RP, Bóscolo FN, de Almeida SM. A comparison of the mandibular index on panoramic and cross-sectional images from CBCT exams from osteoporosis risk group. Osteoporos Int 2014; 25: 1885–90. doi: 10.1007/s00198-014-2696-3 [DOI] [PubMed] [Google Scholar]
- 6. Taguchi A. Triage screening for osteoporosis in dental clinics using panoramic radiographs. Oral Dis 2010; 16: 316–27. doi: 10.1111/j.1601-0825.2009.01615.x [DOI] [PubMed] [Google Scholar]
- 7. Valerio CS, Trindade AM, Mazzieiro ET, Amaral TP, Manzi FR. Use of digital panoramic radiography as an auxiliary means of low bone mineral density detection in post-menopausal women. Dentomaxillofac Radiol 2013; 42: 20120059. doi: 10.1259/dmfr.20120059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Güngör E, Yildirim D, Çevik R. Evaluation of osteoporosis in jaw bones using cone beam CT and dual-energy X-ray absorptiometry. J Oral Sci 2016; 58: 185–94. doi: 10.2334/josnusd.15-0609 [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization Scientific Group on the assessment of osteoporosis at primary health care level. summary meeting report 2004(2007) In: World Health Organization. Brussels: World Health Organization; 2004. [Google Scholar]
- 10. Nakamoto T, Taguchi A, Ohtsuka M, Suei Y, Fujita M, Tsuda M, et al. A computer-aided diagnosis system to screen for osteoporosis using dental panoramic radiographs. Dentomaxillofac Radiol 2008; 37: 274–81. doi: 10.1259/dmfr/68621207 [DOI] [PubMed] [Google Scholar]
- 11. Nakamoto T, Taguchi A, Ohtsuka M, Suei Y, Fujita M, Tanimoto K, et al. Dental panoramic radiograph as a tool to detect postmenopausal women with low bone mineral density: untrained general dental practitioners' diagnostic performance. Osteoporos Int 2003; 14: 659–64. doi: 10.1007/s00198-003-1419-y [DOI] [PubMed] [Google Scholar]
- 12. Kim OS, Shin MH, Song IH, Lim IG, Yoon SJ, Kim OJ, et al. Digital panoramic radiographs are useful for diagnosis of osteoporosis in Korean postmenopausal women. Gerodontology 2016; 33: 185–92. doi: 10.1111/ger.12134 [DOI] [PubMed] [Google Scholar]
- 13. Muramatsu C, Horiba K, Hayashi T, Fukui T, Hara T, Katsumata A, et al. Quantitative assessment of mandibular cortical erosion on dental panoramic radiographs for screening osteoporosis. Int J Comput Assist Radiol Surg 2016; 11: 2021–32. doi: 10.1007/s11548-016-1438-8 [DOI] [PubMed] [Google Scholar]
- 14. Calciolari E, Donos N, Park JC, Petrie A, Mardas N. Panoramic measures for oral bone mass in detecting osteoporosis: a systematic review and meta-analysis. J Dent Res 2015; 94: 17S–27. doi: 10.1177/0022034514554949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guerra ENS, Almeida FT, Bezerra FV, Figueiredo PTDS, Silva MAG, De Luca Canto G, et al. Capability of CBCT to identify patients with low bone mineral density: a systematic review. Dentomaxillofac Radiol 2017; 46: 20160475. doi: 10.1259/dmfr.20160475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koh KJ, Kim KA. Utility of the computed tomography indices on cone beam computed tomography images in the diagnosis of osteoporosis in women. Imaging Sci Dent 2011; 41: 101–6. doi: 10.5624/isd.2011.41.3.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marandi S, Bagherpour A, Imanimoghaddam M, Hatef M, Haghighi A. Panoramic-based mandibular indices and bone mineral density of femoral neck and lumbar vertebrae in women. J Dent 2010; 7: 98–106. [PMC free article] [PubMed] [Google Scholar]
- 18. Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res 1994; 102: 68–72. [DOI] [PubMed] [Google Scholar]
- 19. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 20. Taguchi A, Ohtsuka M, Nakamoto T, Suei Y, Kudo Y, Tanimoto K, et al. Detection of post-menopausal women with low bone mineral density and elevated biochemical markers of bone turnover by panoramic radiographs. Dentomaxillofac Radiol 2008; 37: 433–7. doi: 10.1259/dmfr/85235532 [DOI] [PubMed] [Google Scholar]
- 21. Taguchi A, Asano A, Ohtsuka M, Nakamoto T, Suei Y, Tsuda M, et al. Observer performance in diagnosing osteoporosis by dental panoramic radiographs: results from the osteoporosis screening project in dentistry (OSPD. Bone 2008; 43: 209–13. doi: 10.1016/j.bone.2008.03.014 [DOI] [PubMed] [Google Scholar]
- 22. Taguchi A, Tsuda M, Ohtsuka M, Kodama I, Sanada M, Nakamoto T, et al. Use of dental panoramic radiographs in identifying younger postmenopausal women with osteoporosis. Osteoporos Int 2006; 17: 387–94. doi: 10.1007/s00198-005-2029-7 [DOI] [PubMed] [Google Scholar]
- 23. Gaur B, Chaudhary A, Wanjari PV, Sunil M, Basavaraj P. Evaluation of panoramic radiographs as a screening tool of osteoporosis in post menopausal women: a cross sectional study. J Clin Diagn Res 2013; 7: 2051–5. doi: 10.7860/JCDR/2013/5853.3403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ 2004; 329: 168–9. doi: 10.1136/bmj.329.7458.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ 1994; 309: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Toscano CM. As campanhas nacionais para detecção das doenças crônicas não-transmissíveis: diabetes e hipertensão arterial. Ci. Saúde Col 2004; 9: 885–95. [Google Scholar]
- 27. Motta VT, Oliveira Filho PF. S, Biomédicos AdeD. Análise de Dados Biomédicos. 1st ed Rio de Janiero: The British Institute of Radiology.; 2009. [Google Scholar]
- 28. Suomalainen A, Pakbaznejad Esmaeili E, Robinson S. Dentomaxillofacial imaging with panoramic views and cone beam CT. Insights Imaging 2015; 6: 1–16. doi: 10.1007/s13244-014-0379-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Verheij JG, Geraets WG, van der Stelt PF, Horner K, Lindh C, Nicopoulou-Karayianni K, et al. Prediction of osteoporosis with dental radiographs and age. Dentomaxillofac Radiol 2009; 38: 431–7. doi: 10.1259/dmfr/55502190 [DOI] [PubMed] [Google Scholar]