Abstract
Aim
To outline the pathways a cohort of first attendees to our headache clinics had taken over the years in search of explanations and treatment for their headaches. To establish a greater awareness of the shortcomings and failures in their medical journey in the hope that better headache management will emerge in primary care.
Background
At first attendance in primary care most headache sufferers will not receive a firm diagnosis. Treatments provided are often ineffective and so many patients embark on a somewhat random self-made journey searching for a remedy. If they reach a Headache Clinic the most common diagnoses are ‘chronic migraine’ and ‘medication overuse headache’. They are either no better or worse than when their headaches first started despite their efforts.
Method
We undertook a prospective questionnaire-based study of over 200 patients on first attendance at each of our headache clinics, three based in District General Hospitals and one in a tertiary referral centre. We documented the patients’ headache characteristics, the ‘burden’ of their headaches, functional handicap and the financial costs incurred seeking help before referral. We also documented what our patients understood about their headache disorder and the treatments previously tried.
Findings
Most patients had not been given a formal diagnosis in primary care and many remained unconvinced of the benign nature of their headache problem and wanted further investigations. A few had sought help from headache charities. Many had unrealistic attitudes to their problem and medication overuse was rife. A few patients had been offered triptans in primary care. Key deficiencies in the primary care management of these patients included failure to provide a formal headache diagnosis, inadequate understanding of the nature and mechanism of headaches and failure to follow a resilient management strategy. We provide a more effective management pathway in primary care.
Key words: chronic migraine, headache clinic, headache management, headache pathway, medication overuse headache
Introduction
Headache is the commonest of all symptoms and probably a universal experience at some time of life. Primary headache syndromes, notably ‘migraine’ and ‘tension type headache’ as defined by the International Headache Classification [Headache Classification Committee of the International Headache Society (IHS), 2013a; 2013b] affect more than 80% of the adult population in the United Kingdom; 70% of people will experience a significant headache within a three-month period with 20% reporting missed or reduced ability work days as a result (Steiner et al., 2003).
It is not therefore surprising that headache is a frequent presenting symptom in primary care. About 3% of the general population consults primary care for headache each year making it the most common neurological presentation (Latinovic et al., 2006). ‘Chronic headache’ [chronic daily headache (CDH)], defined under the IHC as attacks of headache occurring on more than half the days in a month over a period of more than three months affects 2–4% of the UK population (Stovner et al., 2007). CDH is very often ‘chronic migraine’, which nearly always develops from episodic migraine (Bigal et al., 2008) and nearly half of such cases also have potentially avoidable medication overuse headache (MOH) (Castillo et al., 1999).
In worldwide terms headache is the third most common cause of disability (Steiner et al., 2015). Headache also has a significant social and economic impact. According to the World Health Organisation, migraine is the fifth most common cause of ‘years lived with disability’ (WHO, 2012), ahead of diabetes and osteoarthritis (Vos et al., 2013), and the annual cost of headache disorders in the United Kingdom is estimated to be £5–7 billion (Steiner, 2010).
If correctly diagnosed, nearly all headache patients can be managed in primary care, where common headache co-morbidities and the complex psychosocial factors that are often important in the provocation and perpetuation of headache can be addressed most effectively (The Association of British Neurologists,1993; Belam et al., 2005; Ridsdale and Kernick, 2010). However, most adult migraineurs have never consulted their general practitioner despite high levels of disability (Thomas et al., 2004) and only 2% of those seen in primary care are referred to a neurologist (Latinovic et al., 2006). Of those who do present to their GP, 70% will receive no formal diagnosis and it has been suggested that GPs’ difficulties in diagnosing primary headache contribute to its morbidity and unmet need (Kernick et al., 2008). In Kernick’s study only 5% received a diagnosis in the first year after consultation and in 73% the diagnosis was ‘migraine’ (Kernick et al., 2008).
For many headache patients, pharmacists and opticians are alternative sources of advice and treatment and many patients self-manage (Peters et al., 2003). Others attend Accident and Emergency departments where migraine is the most common of all neurological presentations (Gahir and Larner, 2006).
Very little is known of the journeys patients take before reaching one of the relatively few headache neurologists or specialist headache clinics in the United Kingdom. The authors all work in secondary or tertiary care and specialise in headache. When comparing our practices, we realised we were seeing similar ‘problem’ headache patients – mostly middle age women with long standing chronic migraine, usually previously undiagnosed and often complicated by MOH. Many were also taking migraine prophylactic medications that were clearly ineffective and had also seen a variety of healthcare practitioners with various qualifications in the search for a solution to their headache problem.
We had no reason to believe that patients seen in other UK headache clinics would differ significantly from ours. We therefore decided to survey the patients referred to our practices using a questionnaire that we devised to see if our impressions were confirmed and if so, whether a more productive approach could be recommended. In particular, we examined the patients’ headache characteristics and the ‘burden’ of headache in terms of chronicity, functional handicap and financial costs incurred seeking a remedy before referral. We also documented what our patients understood about their headache disorder and the treatments they had tried previously.
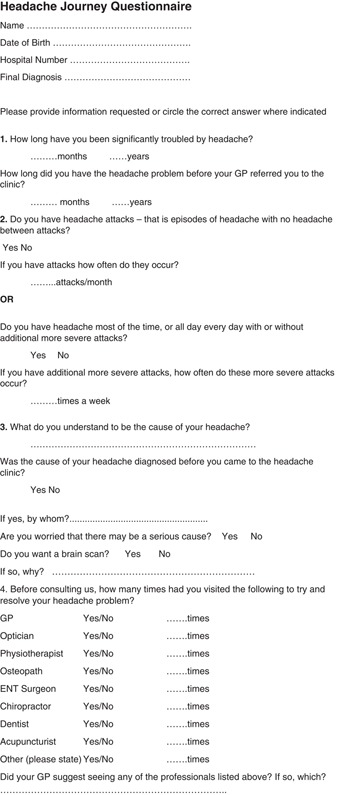
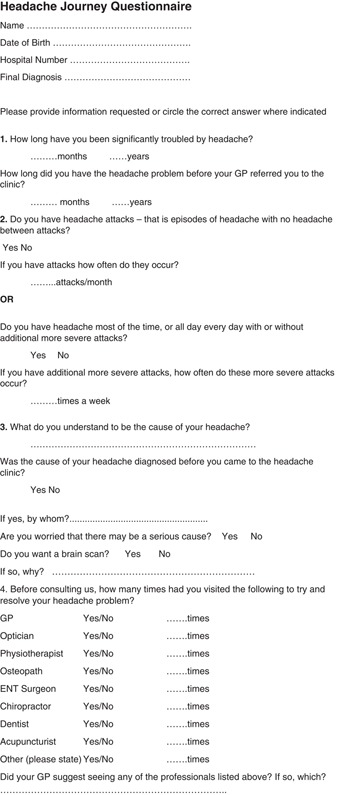
Methods
We conducted a six-month survey of consecutive new patients referred to specialist headache clinics at three district general hospitals (Northampton, York, and Ashford, Middlesex) and one tertiary referral centre [National Hospital for Neurology and Neurosurgery (NHNN), Queen Square, London]. Patients were invited to complete a ‘Headache Pathway’ questionnaire (see Appendix). In addition to demographic data, we documented: how long patients had suffered a headache problem before consulting a GP; the number of GP attendances before referral for expert opinion, time to referral, and whether they had episodic or chronic headache. We also recorded whether patients had been given a specific headache diagnosis by their GP and whether they wanted a brain scan and if so, why. We also asked which other health professionals they had consulted for headache management, how much money they estimated to have spent addressing their headache problem, and how much time off work or full-time education they had lost because of headaches. We documented the headache treatments they had received before referral and how effective they had been, and whether they knew of any of the UK headache charities.
Results
A total of 209 questionnaires were completed (Northampton 46, York 43, Ashford 80 and NHNN 40). The respondents comprised 199 women and 10 men mean age 44.3±15.6 (range 17–82 years). When respondents did not provide an answer to a question, this was recorded.
Headache characteristics and pre-referral diagnosis
More patients had chronic than episodic headaches by a ratio of about 2:1 except in Northampton, where there were more patients with episodic headache. Of 200 responders, only 72 (36%) had been given a specific headache diagnosis before referral. Some patients underwent brain scanning via our headache clinics as a result of patient demand but no relevant intracranial abnormalities were found. Following assessment, all the patients were considered to fulfil criteria for the defined primary headache disorders, ‘episodic migraine’ or ‘CDH’, now considered to be ‘chronic migraine’ (CM), sometimes complicated by MOH (IHS, 2013a) (Table 1).
Table 1.
Characteristics of patients’ headaches and pre-referral diagnosis
| Northampton | York | Ashford | NHNN | |
|---|---|---|---|---|
| No. of patients with episodic or chronic daily headache | 16 Episodic | No data | 15 Episodic | 9 Episodic |
| 14 Chronic | 29 Chronic | 30 Chronic | ||
| 16 No response | 30 No response | 1 No response | ||
| No. of patients with a pre-referral headache diagnosis | 15 Diagnosed | 20 Diagnosed | 22 Diagnosed | 15 Diagnosed |
| 26 No diagnosis | 21 No diagnosis | 57 No diagnosis | 24 No diagnosis | |
| 5 No response | 2 No response | 1 No response | 1 No response |
NHNN=National Hospital for Neurology and Neurosurgery.
Headache burden
Headache history and visits to GPs
Patients seen in the DGH clinics reported having headaches for between 6 and 10 years on average before referral. The mean duration was still longer (13.5 years) at the tertiary referral centre (NHNN). All patients reported consulting their GP on numerous previous occasions for headache management before referral. The lowest average number of visits was in York (8.5) and the highest at NHNN (14.8) (Tables 2 and 3).
Table 2.
Headache years and number of GP visits before referral
| Northampton | York | Ashford | NHNN | |
|---|---|---|---|---|
| Duration of headache problem before referral (years) | n=44 (2) | n=43 (0) | n=75 (5) | n=40 (0) |
| 8.6±8.8 | 10.3±14.1 | 6.4±9.6 | 15.4±13.5 | |
| Mean number of visits to GP before referral | n=41 (5) | n=39 (3) | n=59 (22) | n=35 (7) |
| 11.3±11.2 | 8.53±8.7 | 9.3±15.3 | 14.8±9.4 | |
| Mode=10 | Mode=8.7 | Mode=3 | Mode=10 |
The number of patients who did not provide data is shown in brackets.
NHNN=National Hospital for Neurology and Neurosurgery.
Table 3.
Time lost from work or full-time education because of headache and private treatment costs
| Northampton | York | Ashford | NHNN | |
|---|---|---|---|---|
| In paid employment/full time education | n=44 (2) | n=39 (4) | n=73 (7) | n=40 (0) |
| 33 | 24 | 52 | 15 | |
| Days lost in last 12 months? | Mean=13.8±17.7 | Mean=6.8±8.8 | Mean=21.9±57.3 | Mean=43.7±98 |
| Estimated self-financed treatment costs | 34 (12) | 19 (23) | 56 (24) | 31 (9) |
| £354±382 | £612±1174 | £421±2777 | £1935±827 |
Figures in brackets indicate numbers of non-responders.
Time lost from work and full-time education
A total of 124/196 respondents (63%) were in work or full-time education. Table 3 shows the headache ‘burden’ in terms of time lost from work or education because of headache in the 12 months before survey. This ranged from an average of about 14 days in Northampton to 44 at NHNN.
Private treatment costs
In addition to seeking help through the NHS, many patients had paid for private treatment. Most had spent hundreds of pounds over the years (Table 3). The most common privately funded treatments were changes in glasses prescriptions and ‘alternative therapies’ (see below).
Patients’ understanding of their headache problem
Most patients (64%) had not been given a headache diagnosis by their GP. At NHNN, 40% knew that their diagnosis was ‘chronic migraine’. Of the 66 DGH clinic patients who provided responses, 72% wanted a brain scan. This proportion was much less at the tertiary centre (only 2 of 31 respondents) presumably because many had been scanned previously in primary or secondary care. The reasons given for wanting a brain scan varied. Some said ‘to find the cause of my headaches’, or ‘to get to the bottom of the problem’; some ‘because I’m worried’ or ‘for reassurance’. Some did not know why they wanted a scan and some patients who had been scanned previously wanted another scan (Table 4).
Table 4.
Pre-referral diagnosis and requests for brain scan
| Northampton n=46 (5) | York n=43 (2) | Ashford n=80 (1) | NHNN n=40 (1) | ||
|---|---|---|---|---|---|
| Diagnosis given before referral? | Yes | 15 | 20 | 22 | 15 |
| No | 26 | 21 | 57 | 24 | |
| Brain scan wanted? | Yes | 16 | No data | 31 | 2 |
| No | 10 | 9 | 29 |
Figures in brackets indicate number of non-responders.
Previous sources of medical help
In addition to consulting GPs on numerous occasions before referral, the majority of patients at all centres had also attended a wide range of other professionals, and some several. 62% had consulted an optician (Table 5).
Table 5.
Other practitioners consulted
| Northampton | York | Ashford | NHNN | |
|---|---|---|---|---|
| Optician | 29 of 46 (63%) | 31 of 43 (72%) | 54 of 89 (60%) | 29 of 41 (71%) |
| Physiotherapist | 5 | 3 | 4 | 5 |
| Osteopath | 3 | 4 | 3 | 10 |
| ENT clinic | 1 | 1 | 6 | 8 |
| Chiropractor | 3 | 1 | 6 | 12 |
| Dentist | 7 | 2 | 19 | 14 |
| Acupuncturist | 8 | 0 | 10 | 15 |
Across the four centres less than 15% of patients were aware of the major UK Headache charities (The Migraine Trust and Migraine Action) which can be consulted for management advice and support. In Northampton, only five patients knew of a headache charity (35 did not; six no answer); in York five were aware (30 were not; seven no answer), and at Ashford just four patients knew of these charities (70 were not; six no answer). However, at NHNN, 19 patients were aware of the headache charities (17 were not; four no answer).
Previous drug treatment and treatment responses
Patients in all centres had tried a wide variety of analgesics to treat their headaches. The most commonly used was paracetamol, followed by ibuprofen and aspirin. Disconcertingly, nearly all patients had used Co-codamol and other opiate containing drugs frequently, regularly and often at high doses at some time. Although triptan use was quite common the reported treatment response was not impressive. The most frequently used prophylactic drugs were amitriptyline and propranolol followed by sodium valproate, topiramate and pizotifen. The number of patients who became pain free after taking their acute treatment and the number who had previously tried prophylactic drug treatment is summarised in Table 6.
Table 6.
Use and response to acute treatment, including triptans, and previous use of migraine prophylactic drugs
| Northampton (46) | York (44) | Ashford (82) | NHNN (42) | |
|---|---|---|---|---|
| Triptans | 22 Tried | 9 Tried | 22 Tried | 23 Tried |
| 13 Not tried | 12 Not tried | 41 Not tried | 0 Not tried | |
| 11 No answer | 23 No answer | 19 No answer | 19 No answer | |
| Pain free (more times than not) after using current acute treatment | 10 Pain free | 13 Pain free | 11 Pain free | 4 Pain free |
| 35 Not | 27 Not | 69 Not | 35 Not | |
| 1 No answer | 3 No answer | 2 No answer | 3 No answer | |
| Prophylactic treatment | 30 Tried | 9 Tried | 22 Tried | 23 Tried |
| 14 Not tried | 12 Not tried | 41 Not tried | 0 Not tried | |
| 2 No answer | 23 No answer | 19 No answer | 19 No answer |
Discussion
Our study suggests that in England, the headache sufferer’s journey in search of explanation and treatment can be a long and frustrating one. Most patients referred to our expert clinics were middle aged women with frequent episodic headaches or CDH. ‘Migraine’ or ‘chronic migraine’, often complicated by medication overuse, was the final diagnosis in almost all. Many of these patients had suffered headaches for a decade or more before referral and as a result had lost significant periods of time from work or full-time education.
Despite numerous previous consultations with their GPs, only a third of the patients had been given a specific headache diagnosis before referral. This must surely have resulted in sub-optimal or incorrect treatment in many cases. In our experience, the first advice given for troublesome headaches in primary care is usually an assessment by an optician, although primary ophthalmic problems such as refractive errors are very rarely a cause of headaches in isolation (IHS, 2013b). Migraine in primary care is also often wrongly attributed to ‘sinusitis’ and treated as such (Al-Hashel, 2013).
Without a correct diagnosis, patients can have little understanding as to the true nature of their headache problem and its mechanisms and this is likely to not only heighten anxieties as to causation but impede effective management.
Although no pathological cause for headache was suspected or found in any patient in our study, many patients were anxious about undetected disease despite the chronicity of their headaches; 72% wanted a brain scan, some even if they had been scanned previously. Many patients thought this would ‘get to the bottom of the problem’ but there is no indication for such investigation in the vast majority of cases according to the many publications on ‘when to scan headache’ (Ahmed, 2012). Scanning headache patients in primary care may reduce referrals to secondary care but rarely provides a diagnosis and is unlikely to help the longer-term management in primary care. Indeed, it may add to their anxieties (Howard et al., 2005). Packard concluded that in general, physicians overestimate patients’ wish for ‘headache treatment’ and underestimate their need to understand the basis of their headaches. More emphasis on diagnosis and explanation is clearly needed (Packard, 1979).
Although migraine was by far the most common diagnosis in our cohort, less than half the DGH patients had been offered triptans. In addition, only a minority enjoyed a satisfactory response to their acute treatment. Many actually had undiagnosed chronic migraine and prophylactic therapy should have been a key intervention in management. Although prophylactic drugs had been prescribed in a minority the treatment regimes had been largely ineffective. Many patients had therefore become over-reliant on analgesics. It is well recognised that analgesic overuse is a significant factor in headache chronicity and a frequent complication among problem headache clinic patients (Dowson, 2003; Meskunas et al., 2006). Opiates and compound analgesics are especially culpable and it was sobering to find that most patients in our study had used Co-codamol and other opiate based drugs frequently and on a regular basis despite widely published advice on the dangers of these drugs as a treatment for headache. BASH states that opiates and opioids (including diamorphine, morphine, pethidine, dextropropoxyphene, buprenorphine, tramadol, codeine and dihydrocodeine) ‘should be avoided’ in acute migraine treatment (BASH, 2010).
It is not surprising therefore that our patients looked to alternative resources for help. In addition to opticians, many had also sought the advice of physical therapists (physiotherapists, osteopaths and chiropractors) and had received treatment based on the concept of ‘neck therapies’ although there is little evidence for their effectiveness in the headache population (Biondi, 2005). Although we did not enquire how our patients had made their choices of alternative practitioners, patients had spent considerable amounts of money without benefit.
The majority of our patients had not consulted any of the UK headache charities for advice. These organisations provide excellent evidence-based information not only for conditions like migraine but also with regard to the availability of headache services throughout the United Kingdom.
In summary, our study showed high levels of unmet need and significant economic impact from primary headaches. Most headaches are benign but frequent attacks can be intrusive and disabling. Episodic and chronic migraine are by far the most common headache semiologies but a formal diagnosis at the outset supported by authoritative evidence is an essential part of management. There are many readily available evidence-based guidelines for headache management (British Association for the Study of Headache, 2010; Scottish Intercollegiate Guidelines Network. Diagnosis and management of headache in adults, 2008; National Institute for Health and Care Excellence, 2012), and chronic migraine (Weatherall, 2015). In our opinion, more frequent use of triptans instead of analgesics for episodic headaches and the early introduction of prophylactics with regular review and supervision during dose escalation at an early stage might reduce the tendency to develop chronic migraine and MOH. In addition, there is evidence that improved education for general practitioners supported by general practitioners with a special interest in headache (GPwSI) has the potential to significantly reduce the burden of headache in the United Kingdom. GPwSIs reduce costs as they order less head scans than non-specialist neurologists (Elliot and Kernick, 2011). A healthcare system incorporating GPwSI has been described (Steiner et al., 2011). Improvements in the management of headache in primary care in the United Kingdom are needed now to not only treat the type of patients we see most often in our headache clinics but to try and prevent the common complications that so often develop when the nature of headache is misunderstood and mismanaged.
Conflicts of Interest
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethical Standards
Ethical approval for this survey was granted by the Chairman of the Oxford Regional Ethics Committee.
Acknowledgments:
None.
Appendix
Currently retired.
References
- Ahmed F (2012) Headache disorders: differentiating and managing the common subtypes. British Journal of Pain 6, 124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Hashel JY, Ahmed SF, Algroughani R and Goadsby PJ (2013) Migraine misdiagnosis as sinusitis, a delay that can last for many years. Journal of Headache and Pain 14, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Association of British Neurologists (1993) Guidelines for the care of patients with common neurological disorders in the United Kingdom. London: ABN. [Google Scholar]
- BASH (2010) Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache, medication-overuse headache, third edition (1st revision). Retrieved February 2018 www.bash.org.uk.
- Belam J, Harris G, Kernick D and Goadsby PJ (2005) A qualitative study of migraine involving patient researchers. British Journal of General Practice 55, 87–93. [PMC free article] [PubMed] [Google Scholar]
- Bigal ME, Serrano D, Buse D, Kline F, Lindey K, McWatt J, Mitchell A and Reinholt D (2008) Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache 48, 1157–1168. [DOI] [PubMed] [Google Scholar]
- Biondi DM (2005) Physical treatments for headache: a structured review. Headache 45, 738–746. [DOI] [PubMed] [Google Scholar]
- Castillo J, Munoz P, Guitera V Pascual J (1999) Epidemiology of chronic daily headache in the general population. Headache 39, 190–196. [DOI] [PubMed] [Google Scholar]
- Dowson AJ (2003) Analysis of the patients attending a specialist UK headache clinic over a 3-year period. Headache 43, 4–18. [DOI] [PubMed] [Google Scholar]
- Elliot S Kernick D (2011) Why do GPs with a special interest in headache investigate headache presentations with neuroradiology and what do they find? Journal of Headache and Pain 12, 625–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gahir KK Larner AJ (2006) Primary headache disorder in the emergency department: perspective from a general neurology outpatient clinic. Emergency Medicine Journal 23, 135–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headache Classification Committee of the International Headache Society (IHS) (2013. a) The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33, 629–808. [DOI] [PubMed]
- Headache Classification Committee of the International Headache Society (IHS) (2013. b) The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33, 762. [DOI] [PubMed]
- Howard L, Wessely S, Leese M, Scher A, Stewart WF and Lipton RB (2005) Are investigations anxiolytic or anxiogenic? A randomised controlled trial of neuroimaging to provide reassurance in chronic daily headache. Journal of Neurology, Neurosurgery, and Psychiatry 76, 1558–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernick D, Stapley S Hamilton W (2008) GPs’ classification of headache: is primary headache underdiagnosed? British Journal of General Practice 58, 102–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latinovic R, Gulliford M Ridsdale L (2006) Headache and migraine in primary care: consultation, prescription, and referral rates in a large population. Journal of Neurology, Neurosurgery and Psychiatry 77, 385–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meskunas CA, Tepper SJ, Rapoport AM, Page L, McCrone P, Husain K, Tong J and Dawson A (2006) Medications associated with probable medication overuse headache reported in a tertiary care headache centre over a 15-year period. Headache 46, 766–772. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2012) Diagnosis and management of headache in young people and adults. London: National Institute for Health and Care Excellence. [Google Scholar]
- Packard RC (1979) What does the headache patient want? Headache 19, 370–374. [DOI] [PubMed] [Google Scholar]
- Peters M, Huijer Abu-Saad H, Vydelingum V, Sheftell FD and Bigal ME (2003) Patients’ decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia 23, 833–841. [DOI] [PubMed] [Google Scholar]
- Ridsdale L Kernick D (2010) Improving management in primary care. Report of All-Party Parliamentary Group on Primary Headache disorders. House of Commons, London.
- Scottish Intercollegiate Guidelines Network (SIGN) (2008) Diagnosis and management of headache in adults. A national clinical guideline. Guideline No. 107. Retrieved February 2018 from www.sign.ac.uk.
- Steiner T (2010) The economic cost of migraine and other headache disorders in the UK: A Report of the All-Party Parliamentary Group on Primary Headache Disorders (APPGPHD), House of Commons. In British Association for the Study of Headache. Report on the organisation of headache services, London, pp. 1–3.
- Steiner T, Scher A, Stewart F, Abu-Saad HH, Vydelingum V, Dawson A and Murphy M (2003) The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia 23, 519–527. [DOI] [PubMed] [Google Scholar]
- Steiner TJ, Antonaci F, Jensen R, Kolodner K, Liberman J and Lipton RB (2011) Recommendations for headache service organisation and delivery in Europe. European Headache Federation; Global Campaign against Headache. Journal of Headache and Pain 12, 419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner TJ, Birbeck GL, Jensen RH, Lainez MJ, Lanteri-Minet M and Valade D (2015) Headache disorders are third cause of disability worldwide. Journal of Headache and Pain 16, 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stovner L, Hagen K, Jensen R, Katsarava Z, Stovner LJ and Martelletti P (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27, 193–210. [DOI] [PubMed] [Google Scholar]
- Thomas E, Boardman HF, Ogden H, Katsarava Z, Lipton R, Scher A, Steiner T and Zwart JA (2004) Advice and care for headaches: who seeks it, who gives it? Cephalalgia 24, 740–752. [DOI] [PubMed] [Google Scholar]
- Vos T, Flaxman AD, Naghavi M, Millson DS et al (2013) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weatherall MW (2015) The diagnosis and treatment of chronic migraine. Therapeutic Advances in Chronic Disease 6, 115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2012) WHO Global Health Estimates: DALYs, 2000–2012. Retrieved February 2018 http://www.who.int/healthinfo/global_burden_disease/en/.


