Abstract
Obesity is a risk factor for asthma. However, it is unclear if increased obesity prevalence contributed to rising childhood asthma prevalence. Using nationally representative 1988–2014 National Health and Nutrition Examination Survey data for 40,644 children aged 2–19 years, we analyzed asthma trends by weight status (BMI age-specific percentiles determined using measured weight and height). We sought to assess if population-level changes in weight status impacted asthma prevalence over time with logistic regression and population attributable fraction (PAF). Although obesity was a risk factor for asthma throughout the period, asthma prevalence increased only among children with normal weight; there was no interaction between weight status and time. The PAF for overweight/obesity rose from 8.5% to 1988–1994 to 11.9% in 2011–2014, but this increase in the portion of asthma prevalence attributable to overweight/obesity was not significant (P=0.44). Together, these data do not support a contribution of obesity trends to asthma prevalence trends.
Keywords: asthma, weight status, obesity, trends, epidemiology
Although obesity is increasingly recognized as an asthma risk factor, childhood asthma prevalence trends by weight status have not been described.1 Prospective studies have shown incident asthma is associated with obesity. Hypotheses for this observation include the proinflammatory state of obesity, sex hormone influence, and a common genetic mechanism for obesity and asthma.1, 3 Prevalence of both childhood asthma and obesity increased in the 1990’s and 2000s,4, 5 and it is not clear if increasing obesity contributed to asthma prevalence trends. We sought to assess if increasing obesity prevalence is associated with increasing asthma prevalence.
We analyzed nationally representative National Health and Nutrition Examination Survey (NHANES) 1988–2014 data for children aged 2–19 years. Younger children were excluded given the difficulty of asthma diagnosis among very young children6 and the different method of determining weight status in this age group. NHANES, a survey of the US civilian non-institutionalized population administered by the National Center for Health Statistics, uses a complex probability design. NHANES III was released as one data set for 1988–1994; data from continuous NHANES from 1999 forward were released in 2-year cycles. Written parental consent was obtained for participants aged <18 years. Conditional examination response rates ranged between 76%−87%.7
Asthma prevalence was defined as an affirmative response to: “Has a doctor or other health professional ever told you that you have/your child has asthma?” and “Do you/does your child still have asthma?” Body mass index (BMI) was calculated as measured weight in kilograms divided by measured height in meters squared.8 Weight status was defined as underweight (BMI age-specific percentile <5th), normal weight (5th-<85th), overweight (85th-<95th) and obese (≥95th).9 Asthma prevalence estimates for the underweight group were not reliable and not shown. Pregnant females and records missing asthma or weight status were excluded (n=1405, 3%); the final sample size was 40,644 (see Table S1 for sample size and population characteristics).
Logistic regression models (excluding underweight children, n=1439) were used to assess the association between asthma and weight status, controlling for age, sex, race/Hispanic origin, and survey cycle. To assess whether the relationship between asthma and weight status varied over time, we entered an interaction term (weight status*survey cycle) into the model. National estimates, trends with orthogonal polynomial contrasts, and logistic regression models were estimated with SAS version 9.3 (SAS Institute, Inc., Cary, NC) using examination weights. Variance estimates were calculated with SUDAAN version 11.0 (RTI, Research Triangle Park, NC) to account for the complex survey design. Significance was set at α<0.05. Population attributable fractions (PAF) of overweight/obesity were assessed for 1988–1994 and for each 4-year period from 1999–2014 using STATA version 3.1 SE. The PAF estimates the proportion of asthma prevalence that can be attributed to overweight/obesity by comparing the observed prevalence to a hypothetical counterfactual in which all children with overweight/obesity had the same odds of asthma as children with normal weight, adjusted for the same covariates used in the logistic regression model. These analyses used Stata ‘svy’ commands to account for the complex sample design.
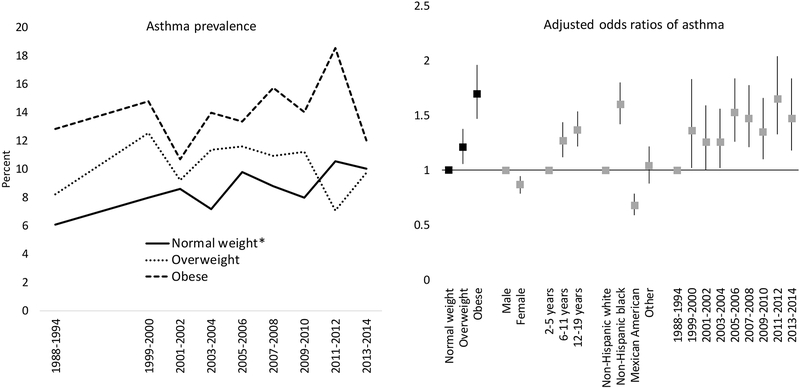
Among children aged 2–19 years, asthma prevalence increased from 7.1% (SE 0.5) in 1988–1994 to 10.3% (SE 0.7) in 2013–2014, and prevalence of obesity increased from 10.0% (SE 0.6) to 17.2% (SE 1.1) (Table S1). Asthma prevalence increased significantly only among children with normal weight from 6.1% (SE 0.5) to 10.1% (SE 0.7) (Figure 1). No significant asthma prevalence trends were observed among overweight or obese categories. However, asthma prevalence among children with obesity was significantly higher than those with normal weight in 1988–1994, 1999–2000, 2003–2004, 2007–2012, and higher than for overweight children in 2011–2012. When weight status was assessed by asthma status, the prevalence of normal weight declined while obesity increased among children without asthma, but there were no trends in weight status among children with asthma (Figure S1).
Figure 1.
(Left) Asthma prevalence by weight status (underweight category not shown because of unreliable point estimates) and (right) adjusted odds ratios and 95% confidence interval for asthma by weight status, sex, age group, race/ethnicity and National Health and Nutrition Examination Survey cycle (the interaction term (weight status*survey cycle) was not statistically significant; underweight category was excluded because of low sample size) – children 2–19 years of age, USA.
* Significant linear trend
Note: CI=confidence interval; Underweight category not shown due to unreliable point estimates.
Logistic regression showed that the odds of having asthma increased with overweight (AOR 1.2, 95% CI 1.1, 1.4) and obesity (AOR 1.7, 95% CI 1.5, 2.0). Adjusted odds for other covariates were similar to those observed in other national data (Figure 1).5 The interaction term between weight status and survey cycle was not statistically significant. Finally, while the PAF for overweight/obesity was 8.5% (95% CI: 5.6, 11.1) in 1988–1994 and 11.9% (95% CI: 8.3, 15.3) in 2011–2014, the difference was not statistically significant (P=0.44).
Limitations include a cross-sectional design and inability to assess causation. Additionally, asthma status is determined based on self-report and was not confirmed using medical records; however, self-report was anchored on receiving an diagnosis from a medical professional, the same methodology used in national asthma surveillance.5 BMI does not directly measure adiposity; however, other studies have found that BMI had a similar or stronger association with asthma status than central adiposity measures, including waist circumference.10, 11 Asthma prevalence estimates by weight status fluctuated between NHANES survey cycles. However, when 4-year cycles were analyzed to increase sample size for each time point observation (1999–2002, 2003–2006, 2007–2010, 2011–2014), results were similar: asthma prevalence trends among the overweight and obese categories were not statistically significant (data not shown). Finally, there is likely to be additional complexity in the association between obesity and asthma within age and sex subgroups, and additional mediators such as physical activity that are not considered in this analysis.
In summary, results suggest that asthma prevalence in 2011–2014 would have been reduced by less than 12% if all children had normal weight. This portion of asthma prevalence attributable to overweight/obesity was not significantly different than that found in 1988–1994 (8.5%). Asthma prevalence increased only among children with normal weight and an interaction term between weight status and survey period was not significant. Among children with asthma, there was no trend in obesity prevalence. However, obesity was a consistent asthma risk factor: asthma prevalence was consistently higher among children with obesity, and in adjusted analyses, obesity was among the strongest risk factors for asthma. Epidemiologic studies such as this one can delineate associations on a population level which are important to better understand the joint public health impact of asthma and obesity, but cannot adequately disentangle the complex interplay between asthma risk factors. This study does, however, inform hypothesis generation for additional research on the potential role of obesity in the development of asthma, adding to the evidence of potential benefits of addressing childhood obesity.
Supplementary Material
Table 1.
Population attributable fraction (PAF) associated with overweight/obesity, NHANES III (1988–1994) and continuous NHANES (1999–2014), adjusted prevalence estimates (%) and PAF (%), 95% confidence interval
| 1988–1994 | 1999–2002 | 2003–2006 | 2007–2010 | 2011–2014 | |
|---|---|---|---|---|---|
| Asthma prevalence based on observed data | 7.1 (6.2–8.2) | 9.3 (8.1–10.6) | 9.9 (9.0–10.8) | 9.9 (9.1–10.9) | 10.9 (9.8–12.1) |
| Counterfactual scenario: all children have normal weight | 6.5 (5.6–7.5) | 8.3 (7.2–9.4) | 8.7 (7.9–9.6) | 8.8 (7.9–9.7) | 9.6 (8.6–10.6) |
| PAF: Overweight/obesity | 8.4 (5.6–11.1) | 10.9 (7.7–14.0) | 11.6 (8.0–15.1) | 11.9 (8.4–15.2) | 11.9 (8.3–15.3) |
Notes: Each set of survey period PAF estimates are based on predicted margins from a logistic regression model of asthma on weight status, age, sex, survey period, and race/Hispanic origin.
Acknowledgements:
LA, LR and TF conceived of the study design. All authors were involved in analysis and interpretation, drafting the manuscript and critical revision of the manuscript.
Abbreviations:
- AOR
adjusted odds ratio
- BMI
body mass index
- NHANES
National Health and Nutrition Examination Survey
- SE
standard error
References
- 1.Beuther DA, Weiss ST, Sutherland ER. Obesity and asthma. American journal of respiratory and critical care medicine. 2006;174(2):112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Black MH, Zhou H, Takayanagi M, Jacobsen SJ, Koebnick C. Increased asthma risk and asthma-related health care complications associated with childhood obesity. American journal of epidemiology. 2013;178(7):1120–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egan KB, Ettinger AS, Bracken MB. Childhood body mass index and subsequent physician-diagnosed asthma: a systematic review and meta-analysis of prospective cohort studies. BMC pediatrics. 2013;13:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akinbami L, Centers for Disease C, Prevention National Center for Health S. The state of childhood asthma, United States, 1980–2005. Advance data. 2006(381):1–24. [PubMed] [Google Scholar]
- 6.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. The New England journal of medicine. 1995;332(3):133–138. [DOI] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics. NHANES Response Rates and CPS Totals. http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. Accessed 05/05/2017 [Google Scholar]
- 8.Divison of Health and Nutrition Examination Survey. National Health and Nutrition Examination Survey: Anthropometry Procedures Manual. https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/manuals/2013_Anthropometry.pdf. Published 2013. Updated January 2013 Accessed 05/22/2017 [Google Scholar]
- 9.National Center fo Health Statistics. CDC Growth Charts. http://www.cdc.gov/growthcharts/cdc_charts.htm. Published 2010 . Updated 9/9/2010. Accessed 05/13/2016, 2016. [Google Scholar]
- 10.Egan KB, Ettinger AS, DeWan AT, Holford TR, Holmen TL, Bracken MB. General, but not abdominal, overweight increases odds of asthma among Norwegian adolescents: the Young-HUNT study. Acta paediatrica. 2014;103(12):1270–1276. [DOI] [PubMed] [Google Scholar]
- 11.Forno E, Acosta-Perez E, Brehm JM, Han YY, Alvarez M, Colon-Semidey A, et al. Obesity and adiposity indicators, asthma, and atopy in Puerto Rican children. The Journal of allergy and clinical immunology. 2014;133(5):1308–1314, [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.