Abstract
Background
The optimal management of hypomagnesemia (hMg) induced by epidermal growth factor receptor inhibitors (egfris) for advanced colorectal cancer is unclear. We surveyed gastrointestinal medical oncologists in Canada to determine practice patterns for the management of egfri-induced hMg.
Methods
Based on distribution lists from the Eastern Canadian Colorectal Cancer Consensus Conference and the Western Canadian Gastrointestinal Cancer Consensus Conference, medical oncologists were invited to participate in an online questionnaire between November 2013 and February 2014.
Results
From the 104 eligible physicians, 40 responses were obtained (38.5%). Panitumumab was more commonly prescribed than cetuximab by 70% of respondents, with 25% prescribing cetuximab and panitumumab equally. Most respondents obtain a serum magnesium level before initiating a patient on an egfri (92.5%) and before every treatment (90%). Most use a reactive strategy for magnesium supplementation (90%) and, when using supplementation, favour intravenous (iv) alone (40%) or iv and oral (45%) dosing. Magnesium sulfate was used for iv replacement, and the most common oral strategies were magnesium oxide (36.4%) and magnesium rougier (18.2%). Under the reactive strategy, intervention occurred at hMg grade 1 (70.3%) or grade 2 (27%). Of the survey respondents, 45% felt that 1–5 of their patients have ever developed symptoms attributable to hMg, and 35% have had to interrupt egfri therapy because of this toxicity, most commonly at grade 3 (30%) or grade 4 (45%) hMg. The most important question about egfri-induced hMg was its relevance to clinical outcomes (45%) and its symptoms (37.5%).
Conclusions
In Canada, various strategies are used in the management of egfri-induced hMg, including prophylactic and reactive approaches that incorporate iv, oral, or a combination of iv and oral supplementation. Clinicians are concerned about the effect of hMg on clinical outcomes and about the symptoms that patients experience as a result of this toxicity.
Keywords: Epidermal growth factor receptor inhibitors, hypomagnesemia, management, surveys
INTRODUCTION
Monoclonal antibodies targeting the epidermal growth factor receptor (egfr) have been evaluated in clinical trials for advanced colorectal cancer and, as monotherapy and in combination with chemotherapy, have been associated with significant improvements in progression-free survival and overall survival1–5. Two egfr inhibitors (egfris), cetuximab and panitumumab, are Health Canada–approved for use in advanced colorectal cancer. Common side effects of those drugs include acneiform rash, hypersensitivity reactions, diarrhea, and hypomagnesemia (hMg). Although hMg was not initially recognized as a side effect of egfris, more recent studies have defined its incidence and severity6.
Magnesium is the second most common intracellular cation (after potassium) in humans and is located mainly intracellularly in bone, muscle, and soft tissue7. It is a cofactor in many enzymatic reactions including atp generation, which is important for glucose metabolism; synthesis of fat, proteins, and nucleic acids; muscle contraction and relaxation; and normal neurologic function8. Most ingested magnesium is eliminated in the feces; the remainder (approximately 30%) is filtered by the kidney, with the largest proportion being reabsorbed and stored in bone, muscle, and soft tissue7. Notably, to maintain magnesium homeostasis, renal excretion and intestinal absorption of magnesium vary depending on plasma level7. Recognized symptoms of hMg include tetany, weakness (including respiratory muscles), mental status changes, and cardiac arrhythmias9.
Mechanistically, Groenestege et al.10 elucidated the cause of egfri-induced hMg. In a genetic analysis of two sisters with isolated recessive renal hMg, mutations in the EGF gene were discovered. Through egfr, EGF stimulates a magnesium channel called trpm6 (the transient receptor potential cation channel, subfamily, member 6) which is located in the distal convoluted tubule. In the tubule, egfris cause decreased stimulation of the trpm6 magnesium channel, the result being magnesium wasting in the urine in the setting of low serum magnesium levels. The trpm6 channels are also present in the gut and are thought to be involved in active magnesium transport, and egfris might therefore inhibit magnesium absorption in the gut as well11.
Clinically, hMg attributable to monoclonal antibodies against egfr is well described. Tejpar et al.12 studied serum magnesium in patients (n = 98) receiving egfris in phase i–iii clinical trials and found that 97% experienced decreased levels over time. More recently, the aspecct trial showed that the rate of grade 3 or 4 hMg was higher with the use of panitumumab than of cetuximab (7% and 3% respectively)13. In addition, all-grade hMg also appeared to be more frequent with panitumumab than with cetuximab (27% vs. 17.7%).
Currently, the optimal form of magnesium replacement and the level at which to intervene remain uncertain. Published guidelines are opinion-based because no prospective studies have adequately evaluated those questions9,14,15 .As a result, we surveyed gastrointestinal medical oncologists in Canada to determine practice patterns for the management of egfri-induced hMg.
METHODS
Questionnaire
A questionnaire was developed to assess the mechanistic understanding of hMg, practices for monitoring magnesium levels, methods of magnesium replacement, observed adverse events of hMg, and the perceived clinical importance of hMg on the part of medical oncologists (Table I). The questionnaire was created using SurveyMonkey (http://www.surveymonkey.com).
TABLE I.
Questions included in the online survey
| 1. Which of the two agents (panitumumab and cetuximab) have you most commonly prescribed in the treatment of advanced colorectal cancer? |
| 2. Approximately how many patients have you treated with either epidermal growth factor (EGFR) inhibitor in the past year? |
| 3. What is your understanding of the mechanism of EGFR inhibitor–mediated hypomagnesemia? |
| 4. Do you routinely obtain a baseline serum magnesium level prior to initiating therapy? |
| 5. How frequently do you check serum magnesium levels during therapy? |
| 6. What is your general approach to managing serum magnesium levels during therapy? |
| 7. If you replace reactively, what form of magnesium do you use? |
| 8. If you answered intravenous, oral, or both in question 7, please specify formulations and doses. |
| 9. If a reactive strategy is used, at what level of hypomagnesemia do you initiate replacement? |
| 10. If you supplement prophylactically, what form of magnesium do you use? |
| 11. If you answered intravenous, oral, or both in question 10, please specify formulations and doses. |
| 12. Do you routinely obtain an electrocardiogram for the purpose of measuring a baseline QTc interval prior to initiating therapy? |
| 13. Have any of your patients treated with an EGFR inhibitor experienced a serious arrhythmia in the setting of hypomagnesemia? |
| 14. In your patients who have been treated with EGFR inhibitors, how many do you feel have developed symptoms due to hypomagnesemia? |
| 15. Have you ever had to interrupt EGFR inhibitor therapy because of hypomagnesemia? |
| 16. At what level of hypomagnesemia do you interrupt EGFR inhibitor therapy? |
| 17. Based on your observations, are you concerned about a possible association of EGFR inhibitor–induced hypomagnesemia and outcomes (that is, better or worse survival)? |
| 18. At present, how satisfied are you with your current magnesium supplementation strategy? |
| 19. In your opinion, what is the most important question regarding EGFR inhibitor–induced hypomagnesemia that should be considered? |
| 20. Do you think a Canadian consensus guideline for the management of EGFR inhibitor–induced hypomagnesemia would be useful? |
After Research Ethics Board approval was obtained, the questionnaire was disseminated online by e-mail to medical oncologists nationwide using distribution lists from the Eastern Canadian Colorectal Cancer Consensus Conference and the Western Canadian Gastrointestinal Cancer Consensus Conference. Redeemable Starbucks coupons were given as incentive to participate. Data were collected from November 2013 to February 2014.
Analysis
Data were analyzed in a descriptive fashion. The proportion of respondents choosing each answer was calculated.
RESULTS
Participants
From 104 eligible participants identified, 40 responses obtained (38.5%). Of those respondents, 70% indicated that they prescribed panitumumab more commonly than cetuximab for advanced colorectal cancer, with 25% prescribing cetuximab and panitumumab equally, and only 5% favouring cetuximab. In the past year, 35% indicated that they had treated 1–5 patients with egfris; 37.5%, 6–10 patients; 25%, 11–20 patients; and 2.5%, more than 20 patients.
Mechanistic Understanding
Most respondents (70%) indicated that the mechanism of toxicity was inhibition of a magnesium channel in the kidney alone. Only 25% recognized that inhibition occurs at both the kidney and the intestine.
Monitoring
Almost all respondents (92.5%) indicated that they routinely obtain a baseline serum magnesium level before initiation of an egfri and before every egfri treatment (90%). Only 1 respondent (2.5%) reported routinely obtaining an electrocardiogram to assess the baseline QTc interval before initiating egfri therapy.
Management of hMg
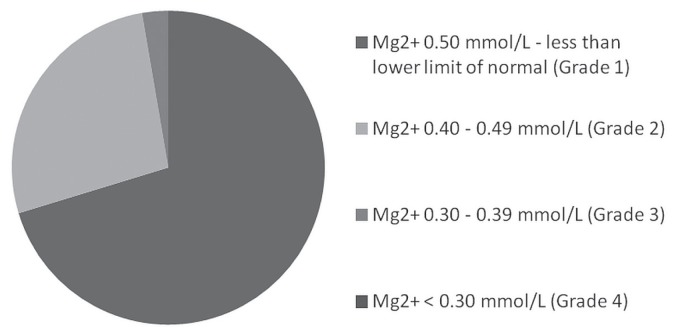
Most respondents indicated using a reactive strategy for magnesium supplementation (90%). Of those using such a strategy, 40% said that they supplemented with an intravenous (iv) replacement alone; 10%, with an oral replacement alone; and 45%, with a combination of iv and oral replacement. The remaining 5% said that they did not supplement at all. Magnesium sulfate was always used in iv replacement. The most common oral replacement strategies were magnesium oxide (36.4%) and magnesium rougier (18.2%). When using a reactive strategy, clinicians most commonly intervened (Figure 1) when hMg reached grade 1 (70.3%) or grade 2 (27%).
FIGURE 1.
Level of hypomagnesemia at which replacement was initiated in patients undergoing treatment with epidermal growth factor inhibitors (EGFRIs).
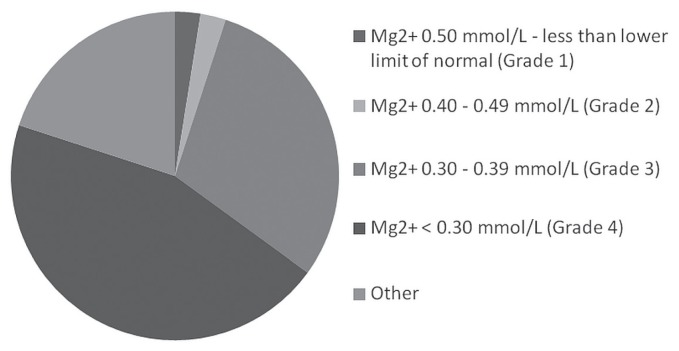
Some respondents (15%) indicated use of a prophylactic replacement strategy. Of those respondents, 45% used iv replacement only, 45% used iv and oral replacement, and 10% used oral replacement only (Figure 2).
FIGURE 2.
Level of hypomagnesemia at which therapy with epidermal growth factor inhibitors (EGFRIs) was interrupted.
Of our survey respondents, 35% indicated having interrupted therapy in response to hMg. Of those who chose to interrupt therapy, the decision to interrupt was usually at grade 3 (30%) or grade 4 (45%) hMg (Figure 2). On a 1–5 Likert scale16 measuring satisfaction with their magnesium supplementation strategy, respondents scored an average of 3.18.
Adverse Events
No respondents reported the development of a serious arrhythmia because of hMg induced by an egfri. Of the survey respondents, 45% reported that they recalled 1–5 patients who had developed symptoms attributable to hMg, and 35% had had to interrupt egfri therapy as a result of symptoms.
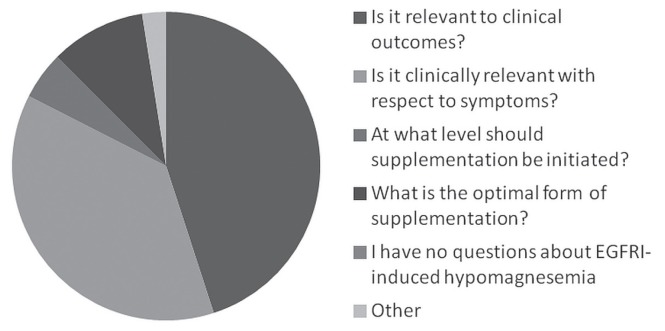
Importance in Clinical Practice
Of the survey respondents, 90% were not concerned about a possible association of egfri-induced hMg and treatment outcomes (positive or negative). The respondents felt that the most important questions to be addressed about egfri-induced hMg (Figure 3) were relevance to clinical outcomes (45%) and symptom profile (37.5%). Respondents were highly interested (90%) in a Canadian consensus guideline addressing this issue.
FIGURE 3.
Opinions of medical oncologists about the most important question to consider with respect to hypomagnesemia induced by epidermal growth factor inhibitors (EGFRIs).
DISCUSSION
Currently, no guidelines addressing the management of hMg in patients taking egfris have been developed. We therefore conducted a survey to determine how, clinically, medical oncologists handle hMg in the context of egfri treatment.
Current common practice is to obtain baseline serum magnesium before initiating treatment with an egfri and before each cycle of treatment. Our survey demonstrates that the current approach to managing hMg is generally reactive, with most physicians opting to use the iv or a combination of the iv and the oral route for administration. Furthermore, treatment regimens are most commonly interrupted for symptomatic cases of hMg, which tend to be more prevalent at higher grades of hMg.
Given the various physiologic roles of magnesium in the body and the potential consequences arising from its depletion, detecting and rectifying discrepancies is important. However, many questions remain. Firstly, the optimal method of measuring serum magnesium is still a matter of debate. Currently, most oncologists use serum magnesium before initiation of an egfri and before every egfri treatment to infer the total body level; however, those two measures do not necessarily correlate. In fact, only 1% of total body magnesium is found in extracellular fluid and only 0.3% is found in serum. Despite being a poor predictor of total body magnesium, serum magnesium remains the most practical and inexpensive means of assessing acute changes7.
The use of iv magnesium to restore physiologic levels also has issues. Administering magnesium in this manner results in an abrupt, yet transient, increase in plasma concentration. However, uptake of magnesium at the cellular level is slow, and sustained correction is therefore needed for adequate repletion. Theoretically, proper iv repletion would take days (4–5 g over 12–24 hours), which is not feasible in an outpatient setting. Furthermore, in the presence of a sudden increase in serum magnesium, a calcium sensing receptor at the loop of Henle partially inhibits resorption, which could further hinder restoration. Also, repeatedly obtaining peripheral access can be impractical, and in some cases, a central venous line might be required, which is not without risk17,18. High-dose oral supplementation might overcome many of those challenges. In states of low intraluminal magnesium, intestinal absorption is predominantly active and therefore a saturable process. Active transport of magnesium in the gut is thought to be mediated in part by the trpm6 channel, although the mechanistic details are unclear11. The use of egfris leads to less stimulation of that channel. In states of high intraluminal magnesium, passive transport is predominant. That method of absorption would be logical to optimize in the context of egfri use, given that the trpm6 channel is less available. Using high-dose oral supplementation might therefore be a more effective and practical way of providing a sustained increase in available magnesium on an outpatient basis. However, it should be noted that oral magnesium supplementation is known to cause diarrhea19,20. Interestingly, our study showed that iv magnesium repletion is used by most medical oncologists either with or without oral supplementation.
The type of supplement used is another variable that should be optimized. A study looking at 16 healthy volunteers found that absorption of magnesium oxide is lower (4%) relative to other compounds, including magnesium chloride, magnesium l-lactate, and magnesium aspartate21. Another study in 46 healthy volunteers also showed that magnesium oxide is suboptimally absorbed, and that magnesium citrate provides the highest plasma levels both acutely and at 60 days after administration22. Despite the heterogeneity of magnesium absorption studies, a review by Rylander23 concluded, based on current evidence, that magnesium citrate is the most appropriate formulation for supplementation and other therapeutic purposes. In the present study, 100% of the respondents who specified the form of iv supplementation they used, said that they used magnesium sulfate. Of the respondents who specified the form of oral supplementation they used, 7 (50%) used magnesium oxide, 5 (36%) used magnesium glucoheptonate, 1 (7%) used magnesium sulfate, and 1 used magnesium gluconate (7%).
Aside from the method of repletion, another point of contention is determining whether hMg is symptomatic and warrants treatment in cancer patients. Magnesium deficiency produces symptoms that can overlap with the symptoms caused by advancing cancer and chemotherapy. In fact, symptoms of hMg have not been prospectively documented using validated questionnaires. However, severe magnesium deficiency (grade 3 or 4) in patients with cancer has been associated with general symptoms including fatigue, cramping, and somnolence12. Alteration in mentation and tachycardia have also been reported3,12. Because of the inability to attribute a cause to certain symptoms, the point at which hMg should be treated (if at all) is unclear. Although no deaths attributable to hMg have been reported in patients with cancer treated with egfris, cases of egfri dose reduction and treatment discontinuation have been documented24. A recent systematic review showed that there are currently no high-quality studies of hMg treatment in the context of egfri use15. Recently, our group completed a feasibility study assessing an integrated consent model to compare oral supplementation using magnesium oxide with supplementation using magnesium citrate in patients with hMg from egfris and platin agents (NCT02690012 at http://ClinicalTrials.gov/).
Another factor that remains unclear is the effect of hMg in the context of carcinogenesis. In healthy cells, magnesium deficiency induces growth arrest by altering the expression of cell-cycle regulatory proteins, dna duplication, and mitosis25. Generally, magnesium levels correlate with the growth rate of cells. However, cancer cells are able to grow independently, and their growth rate does not correlate with the magnesium concentration in vitro26. Interestingly, a magnesium-deficient diet in mice resulted in decreased growth of the primary tumour, but increased metastatic potential27. An antitumour effect of hMg in humans remains to be elucidated, and we have no conclusive evidence that carcinogenesis is affected.
The present study is limited by its sample size and moderately low response rate of 38.5%. It is possible that individual institutions might have blocked e-mail messages arriving from SurveyMonkey, and therefore some individuals might not have received the survey. Respondents were not asked to undertake a formal chart review, and thus the estimations provided are subject to recall bias. The sample population might also not be completely representative of all prescribers of egfris, given that the e-mail addresses came from individuals who were on conference e-mail lists.
CONCLUSIONS
Hypomagnesemia is a common side effect of treatment with egfris. However, evidence about the consequences of this toxicity and its symptom profile is conflicting. Further, no evidence-based guidelines have currently been developed for the management of hMg in the context of cancer treatments using egfris. In the present study, we have summarized the treatment practices of Canadian medical oncologists, but have also highlighted the need for more research to clearly delineate the clinical repercussions of hMg, and how and when intervention should be initiated.
ACKNOWLEDGMENTS
This research was funded by an unrestricted grant from Amgen.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Cunningham D, Humblet Y, Siena S, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351:337–45. doi: 10.1056/NEJMoa033025. [DOI] [PubMed] [Google Scholar]
- 2.Jonker DJ, O’Callaghan CJ, Karapetis CS, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007;357:2040–8. doi: 10.1056/NEJMoa071834. [DOI] [PubMed] [Google Scholar]
- 3.Van Cutsem E, Peeters M, Siena S, et al. Open-label phase iii trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J Clin Oncol. 2007;25:1658–64. doi: 10.1200/JCO.2006.08.1620. [DOI] [PubMed] [Google Scholar]
- 4.Van Cutsem E, Kohne CH, Lang I, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2011;29:2011–19. doi: 10.1200/JCO.2010.33.5091. [DOI] [PubMed] [Google Scholar]
- 5.Douillard JY, Oliner KS, Siena S, et al. Panitumumab–folfox4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369:1023–34. doi: 10.1056/NEJMoa1305275. [DOI] [PubMed] [Google Scholar]
- 6.Streb J, Püsküllüoğlu M, Glanowska I, et al. Assessment of frequency and severity of hypomagnesemia in patients with metastatic colorectal cancer treated with cetuximab, with a review of the literature. Oncol Lett. 2015;10:3749–55. doi: 10.3892/ol.2015.3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jahnen-Dechent W, Ketteler M. Magnesium basics. Clin Kidney J. 2012;5:i3–14. doi: 10.1093/ndtplus/sfr163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ko YH, Hong S, Pedersen PL. Chemical mechanism of atp synthase. Magnesium plays a pivotal role in formation of the transition state where atp is synthesized from adp and inorganic phosphate. J Biol Chem. 1999;274:28853–6. doi: 10.1074/jbc.274.41.28853. [DOI] [PubMed] [Google Scholar]
- 9.Saif MW. Management of hypomagnesemia in cancer patients receiving chemotherapy. J Support Oncol. 2008;6:243–8. [PubMed] [Google Scholar]
- 10.Groenestege WM, Thebault S, van der Wijst J, et al. Impaired basolateral sorting of pro-egf causes isolated recessive renal hypomagnesemia. J Clin Invest. 2007;117:2260–7. doi: 10.1172/JCI31680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Wijst J, Bindels RJ, Hoenderop JG. Mg2+ homeostasis: the balancing act of trpm6. Curr Opin Nephrol Hypertens. 2014;23:361–9. doi: 10.1097/01.mnh.0000447023.59346.ab. [DOI] [PubMed] [Google Scholar]
- 12.Tejpar S, Piessevaux H, Claes K, et al. Magnesium wasting associated with epidermal-growth-factor receptor–targeting antibodies in colorectal cancer: a prospective study. Lancet Oncol. 2007;8:387–94. doi: 10.1016/S1470-2045(07)70108-0. [DOI] [PubMed] [Google Scholar]
- 13.Price TJ, Peeters M, Kim TW, et al. Panitumumab versus cetuximab in patients with chemotherapy-refractory wild-type KRAS exon 2 metastatic colorectal cancer (aspecct): a randomised, multicentre, open-label, non-inferiority phase 3 study. Lancet Oncol. 2014;15:569–79. doi: 10.1016/S1470-2045(14)70118-4. [DOI] [PubMed] [Google Scholar]
- 14.Fakih M. Management of anti-egfr–targeting monoclonal antibody–induced hypomagnesemia. Oncology (Williston Park) 2008;22:74–6. [PubMed] [Google Scholar]
- 15.Jiang DM, Dennis K, Steinmetz A, et al. Management of epidermal growth factor receptor inhibitor–induced hypomagnesemia: a systematic review. Clin Colorectal Cancer. 2016;15:e117–23. doi: 10.1016/j.clcc.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 16.Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22:1. [Google Scholar]
- 17.Costa A, Tejpar S, Prenen H, Van Cutsem E. Hypomagnesaemia and targeted anti-epidermal growth factor receptor (egfr) agents. Target Oncol. 2011;6:227–33. doi: 10.1007/s11523-011-0200-y. [DOI] [PubMed] [Google Scholar]
- 18.Schrag D, Chung KY, Flombaum C, Saltz L. Cetuximab therapy and symptomatic hypomagnesemia. J Natl Cancer Inst. 2005;97:1221–4. doi: 10.1093/jnci/dji242. [DOI] [PubMed] [Google Scholar]
- 19.Fine KD, Santa Ana CA, Fordtran JS. Diagnosis of magnesium induced diarrhea. N Engl J Med. 1991;324:1012–17. doi: 10.1056/NEJM199104113241502. [DOI] [PubMed] [Google Scholar]
- 20.Duncan A, Cameron A, Stewart MJ, Russell RI. Diagnosis of the abuse of magnesium and stimulant laxatives. Ann Clin Biochem. 1991;28:568–73. doi: 10.1177/000456329102800605. [DOI] [PubMed] [Google Scholar]
- 21.Firoz M, Graber M. Bioavailability of US commercial magnesium preparations. Magnes Res. 2001;14:257–62. [PubMed] [Google Scholar]
- 22.Walker AF, Marakis G, Christie S, Byng M. Mg citrate found more bioavailable than other Mg preparations in a randomised, double-blind study. Magnes Res. 2003;16:183–91. [PubMed] [Google Scholar]
- 23.Rylander R. Bioavailability of magnesium salts: a review. J Pharm Nutr Sci. 2014;4:57–9. [Google Scholar]
- 24.Kono T, Satomi M, Asama T, et al. Cetuximab-induced hypomagnesaemia aggravates peripheral sensory neurotoxicity caused by oxaliplatin. J Gastrointest Oncol. 2010;1:97–101. doi: 10.3978/j.issn.2078-6891.2010.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anastassopoulou J, Theophanides T. Magnesium–dna interactions and the possible relation of magnesium to carcinogenesis. Irradiation and free radicals. Crit Rev Oncol Hematol. 2002;42:79–91. doi: 10.1016/S1040-8428(02)00006-9. [DOI] [PubMed] [Google Scholar]
- 26.Wolf FI, Maier JA, Nasulewicz A, et al. Magnesium and neoplasia: from carcinogenesis to tumor growth and progression or treatment. Arch Biochem Biophys. 2007;458:24–32. doi: 10.1016/j.abb.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 27.Nasulewicz A, Wietrzyk J, Wolf FI, et al. Magnesium deficiency inhibits primary tumor growth but favors metastasis in mice. Biochim Biophys Acta. 2004;1739:26–32. doi: 10.1016/j.bbadis.2004.08.003. [DOI] [PubMed] [Google Scholar]