Abstract
Introduction
Given the high occurrence and morbidity of non-melanoma skin cancer (nmsc), its economic burden on the Canadian health care system is a cause for concern. Despite that relevance, few studies have used patient-level data to calculate the cost of nmsc. The objective of the present study was to use physician billing data to describe the health care costs and service utilization associated with nmsc in Saskatchewan.
Methods
The Saskatchewan Cancer Agency’s cancer registry was used to identify patients diagnosed with nmsc between 2004 and 2008. Treatment services and costs were based on physician billing claims, which detail physician services performed in an outpatient setting. Total and annual outpatient costs for nmsc and mean outpatient cost per person were calculated by skin cell type, lesion site, and geographic location. Service utilization and costs by physician specialty were also explored.
Results
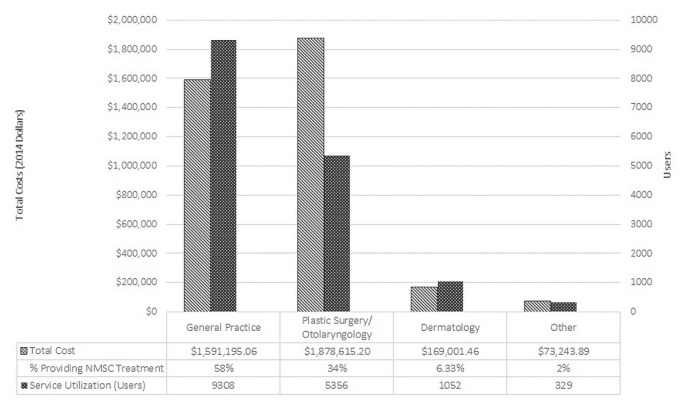
Total outpatient costs grew 12.08% annually, to $845,954.98 in 2008 from $527,458.76 in 2004. The mean outpatient cost per person was estimated at $397.86. Differences in the cost-per-person estimates were observed when results were stratified by skin cell type ($403.41 for basal cell carcinoma vs. $377.85 for squamous cell carcinoma), lesion site ($425.27 for the face vs. $317.80 for an upper limb), and geographic location ($415.07 urban vs. $363.48 rural). Investigation of service utilization found that 92.14% of treatment was delivered by general practice and plastic surgery/otolaryngology physicians; dermatology delivered only 6.33% of services.
Conclusions
Our results underestimate the direct costs of nmsc because inpatient services and non-physician costs were not included in the calculations. The present research represents a first step in understanding the cost burden of nmsc in Saskatchewan.
Keywords: Non-melanoma skin cancer, nmsc, costs, economic burden, physician billing claims, outpatient costs, direct costs, administrative data
INTRODUCTION
Non-melanoma skin cancer (nmsc) is the most commonly diagnosed malignancy in white populations in Europe, Australia, and North America. The incidence of nmsc is increasing annually worldwide1–3. In 2013, nmsc accounted for 40% (81,000) of all cancer cases in Canada4. Although mortality in nmsc is low, the escalating incidence of the disease results in significant morbidity, which is a cause for concern from both a clinical and an economic perspective. Identifying the cost drivers of skin cancer management and describing health resource utilization is challenging, mainly because reporting of nmsc cases in provincial and territorial cancer registries is lacking5,6. The Saskatchewan Cancer Agency’s cancer registry (scr) is one of the few cancer registries in Canada to capture nmsc cases7,8.
Diagnosis and treatment of nmsc occurs primarily in the outpatient setting9. The diagnosis is made by examination and biopsy, and the preferred treatment modality consists of surgical removal of the lesion9—services that are all captured in physician billing claims data. Nonsurgical treatments are not captured in billing data, but surgical treatment is the modality most commonly used in nmsc because of its high cure rate9–11.
Here, we use scr and physician billing data to present outpatient nmsc health care costs and utilization in Saskatchewan during 2004–2008.
METHODS
Patients with nmsc were obtained from the scr, which contains cancer diagnoses and demographic information. Cost and utilization data were obtained from the Saskatchewan Ministry of Health’s physician billing records. Physician billing data contains information about service dates, diagnosis codes, physician specialty, and amount reimbursed for physician services in an outpatient setting, including same-day surgery. Billing codes used to identify nmsc services were determined based on their relevancy to diagnosis and treatment.
Patients were included in the study if they had experienced at least 1 incident of nmsc between 1 January 2004 and 31 December 2008. The included patients were followed starting 3 months before and for up to 1 year after the nmsc diagnosis to capture the full episode of care. To allow for the categorization of costs and service utilization for nmsc by skin cell type [basal cell carcinoma (bcc) and squamous cell carcinoma (scc)], patients diagnosed with both bcc and scc were excluded from the analysis. Patients were identified as having multiple or recurrent episodes if more than 1 case of nmsc was recorded in the scr for that patient.
Total and annual outpatient cost of nmsc treatment and mean outpatient cost per patient are presented by skin cell type, lesion site, and geographic location (urban or rural). Outpatient costs are based solely on the physician reimbursement for services provided (fee-for-service payments). Service utilization by physician specialty was also explored. The age-standardized incidence ratio was calculated separately for cases of nmsc, bcc, and scc based on incident nmsc cases identified in the scr (1991 Canadian standard). Costs were adjusted to 2014 Canadian dollars using the health care component of the Canada Consumer Price index.
RESULTS
Overall
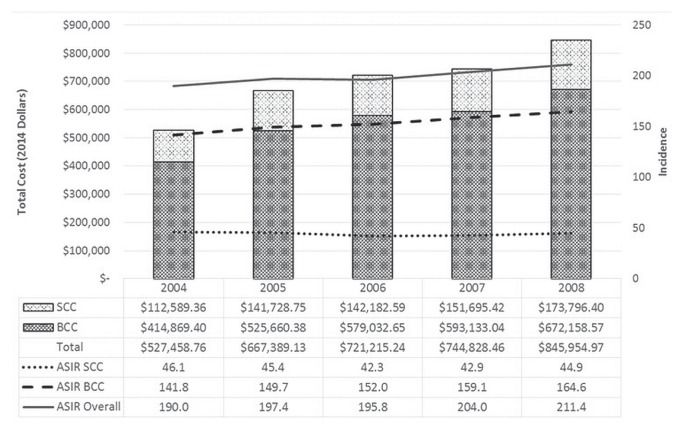
The final cohort consisted of 9330 patients (Table I). At time of diagnosis, mean age in the cohort was 70.87 ± 14.15 years, 65.42% of the patients resided in urban areas, and 54.36% were men. The face was the most common lesion site (64.86%), followed by the trunk (13.73%). Multiple episodes of nmsc occurred in 13.73% of the patients. Total outpatient care costs for those diagnosed between 2004 and 2008 were estimated at $3,712,056.63, with a mean cost per person of $397.86. Depending on the lesion site, the mean cost per person varied from $317.80 (lesions in the upper limbs) to $425.27 (facial lesions). Mean cost per person was $773.33 for patients with multiple episodes of nmsc compared with $312.61 for patients having a single episode. During the observation period, overall costs grew to $845,954.98 in 2008 from $527,458.76 in 2004—a growth rate of 12.08% annually (Figure 1). Comparatively, the age-standardized incidence ratio grew by 3.22% annually. The difference in those growth rates could indicate that incidence was not the sole driver of the cost growth in nmsc during the period of interest.
TABLE I.
Baseline characteristics and outpatient care–based cost estimates for patients diagnosed with non-melanoma skin cancer (NMSC) in Saskatchewan from 1 January 2004 to 31 December 2008
| Variable | Overall | Skin-cell type | Residence | ||
|---|---|---|---|---|---|
|
|
|
||||
| Basal | Squamous | Urban | Rural | ||
| Patients [n (%)] | |||||
| Overall | 9330 | 7306 | 2024 | 6104 | 3160 |
| With multiple incidents | 1281 (13.73) | ||||
|
| |||||
| Setting [n (%)] | |||||
| Urban | 6104 (65.42) | 4908 (67.18) | 1196 (59.10) | 6104 (100) | 0 (0) |
| Rural | 3160 (33.86) | 2344 (32.08) | 816 (40.31) | 0 (0) | 3160 (100) |
|
| |||||
| Sex | |||||
| Women | 4258 (45.64) | 3416 (46.76) | 842 (41.60) | 2854 (46.76) | 1372 (43.42) |
| Men | 5072 (54.36) | 3890 (53.24) | 1182 (58.40) | 3250 (53.24) | 1788 (56.58) |
|
| |||||
| Mean age | 70.87±14.15 | 69.55±14.34 | 75.64±12.31 | 70.38±14.36 | 71.95±13.58 |
|
| |||||
| Site of skin lesion [n (%)] | |||||
| Face | 6051 (64.86) | 4878 (66.77) | 1173 (57.95) | 3838 (62.88) | 2166 (68.54) |
| Trunk | 1281 (13.73) | 907 (12.41) | 126 (6.23) | 738 (12.09) | 288 (9.11) |
| Upper limb | 958 (10.27) | 536 (7.34) | 422 (20.85) | 657 (10.76) | 297 (9.40) |
| Scalp and neck | 951 (10.19) | 764 (10.46) | 187 (9.24) | 626 (10.26) | 318 (10.06) |
| Lower limb | 303 (3.25) | 195 (2.67) | 108 (5.34) | 225 (3.69) | 77 (2.44) |
| Other | 34 (0.36) | 26 (0.36) | 8 (0.40) | 20 (0.33) | 14 (0.44) |
|
| |||||
| Year of service ($) | |||||
| 2003 | 5,074.34 | 5,074.34 | 823.33 | 4,330.81 | 0.00 |
| 2004 | 527,458.76 | 414,869.40 | 112,589.36 | 349,167.59 | 172,855.16 |
| 2005 | 667,389.13 | 525,660.38 | 141,728.75 | 461,067.10 | 204,457.28 |
| 2006 | 721,215.24 | 579,032.65 | 142,182.59 | 491,417.37 | 226,396.95 |
| 2007 | 744,828.46 | 593,133.04 | 151,695.42 | 496,455.82 | 240,788.25 |
| 2008 | 845,954.98 | 672,158.57 | 173,796.40 | 593,340.78 | 244,359.45 |
| 2009 | 200,134.72 | 157,352.00 | 41,959.38 | 137,826.45 | 59,742.24 |
|
| |||||
| Outpatient care costs ($) | |||||
| Total | 3,712,055.63 | 2,947,280.38 | 764,775.23 | 2,533,605.92 | 1,148,599.33 |
| General practice and surgery | 1,572,165.11 | 1,193,822.58 | 378,342.53 | 987,805.66 | 592,956.73 |
| Dermatology | 168,139.51 | 149,516.58 | 18,622.93 | 121,227.25 | 47,104.76 |
| Plastic surgery or otolaryngology | 1,857,534.35 | 1,541,250.14 | 316,284.21 | 1,376,606.05 | 484,166.26 |
| Other | 114,216.66 | 62,691.09 | 51,525.57 | 47,966.95 | 24,371.59 |
| Mean per person | 397.86 | 403.41 | 377.85 | 415.07 | 363.48 |
| Single NSMC | 312.61 | — | — | — | — |
| Multiple NSMCs | 773.33 | — | — | — | — |
| Face | 425.27 | — | — | — | — |
| Trunk | 332.48 | — | — | — | — |
| Upper limb | 317.80 | — | — | — | — |
| Scalp and neck | 386.24 | — | — | — | — |
| Lower limb | 367.08 | — | — | — | — |
| Other | 362.43 | — | — | — | — |
FIGURE 1.
Total and individual annual treatment expenditures and age-standardized incidence ratios (ASIRs) for outpatient care of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) in Saskatchewan, 2004–2008.
Skin Cell Type
Stratified by skin cell type, bcc and scc constituted 78.30% and 21.70% respectively of the nmsc cases. Similar proportions were observed when comparing the composition of total costs over the time period: bcc and scc represented 79.40% ($2,947,280.38) and 20.60% ($764,775.23) respectively of total outpatient costs (Figure 1). The mean cost per person was $403.41 for patients with bcc and $377.85 for those with scc. Outpatient costs for bcc (Figure 1) increased at a rate of 12.40% annually (to $672,158.57 from $414,869.40), and scc increased by 10.87% annually (to $173,796.40 from $112,589.36). The differences in mean cost per person might be explained by the combined effect of patient volume and the proportion of patients with facial lesions being higher in the bcc group than in the scc group (66.77% vs. 57.95%).
Physician Specialty
Service utilization was classified using 4 distinct physician specialties (Figure 2)12. General practice physicians delivered most of the treatments (58.50%), followed by plastic surgery/otolaryngology physicians (33.64%). Dermatologists delivered only 6.32% of nmsc treatment services. Treatment costs were highest for the general practice and plastic surgery/otolaryngology physicians, totalling $1,572,165.11 and $1,857,534.35 respectively. Plastic surgery was the costliest specialty in proportion to the service volume provided, most likely because severe or esthetically sensitive lesions requiring intricate repair and longer follow-up (for example, flaps or grafts) are referred to that specialty12.
FIGURE 2.
Total outpatient costs and service utilization by physician specialty (defined as the number of patients with at least 1 consultation per category) for patients diagnosed with non-melanoma skin cancer (NMSC) in Saskatchewan between 1 January 2004 and 31 December 2008.
Rural and Urban
The total outpatient care costs for residents in urban and rural areas were $2,533,605.92 and $1,148,599.33 respectively (Table I). The mean cost for treatment was higher in urban areas, at $415.07 per person compared with $363.48 per person in rural areas. The difference in per-person cost might be explained by specialist service availability, given that rural areas tend not to have easy access to specialized services (for example, plastic surgery/otolaryngology).
DISCUSSION
A few publications describe the cost burden of nmsc based on patient-level data. A study in New Brunswick found that the mean direct cost of nmsc treatment was $645 (2014 dollars), much higher than our findings in Saskatchewan13. In a review by Mudigonda et al.14, mean Medicare payments oscillated between $604 and $877 during 1999–2000. There are, however, some methodology differences that might account for the discrepancies. The New Brunswick study included all direct costs, such as acute-care costs (in-office procedures), hospital-based day surgery, and in-patient hospital costs13. For the present study, we restricted the calculations to outpatient expenses, which represent 84% of direct nmsc costs8. Differences in treatment patterns are also likely to influence the cost. In the United States and some Canadian provinces, Mohs surgery—an expensive surgical alternative used for the excision of malignant skin lesions—is offered14,15. Mohs surgery was not offered in Saskatchewan during the study period, and traditional methods of surgical excision were performed at less than half the cost. In cases in which Mohs surgery was deemed necessary by the treating physician, patients were sent out of province for treatment; their costs would not be captured in our data.
The direct costs of nmsc treatment differ according to cell type, which could have influenced the observed difference in mean costs by cell type. The Canadian Partnership Against Cancer estimated that in patients with bcc, 93% of direct costs correspond to primary care–based services (including specialties such as dermatology) and only 7% correspond to inpatient services. In patients with scc, the distribution of those direct costs is estimated to be 64% and 37% respectively8. That difference could contribute to the cost disparity observed between the cell types, because we restricted our cost calculations to outpatient treatments only.
Usage patterns for specialist services in nmsc in Saskatchewan differ considerably from those reported elsewhere. We found that general practice and plastic surgery/ otolaryngology physicians provide most of the health care services; dermatologists had minimal participation in the treatment of nmsc. That trend remained evident even after patients were categorized by geographic area. In a U.S. study that analyzed nmsc treatment costs for 1999–2000, dermatologists provided half the treatment services, with surgery and primary care combined being responsible for roughly 15% of nmsc treatment14. In a study by Chirikov et al.12, approximately 75% of treatment services were provided by dermatologists, and only 12% of treatment services were provided by general practice physicians during 2005–2007. A study in New Brunswick reported similar results for services provided between 2002 and 201013. It is possible that the limited availability of dermatologists in Saskatchewan inf luenced specialist participation in nmsc treatment. Moreover, those differences in treatment patterns might explain the cost differences between the present study and other reports in the literature, given that services provided by general practice physicians are typically relatively less expensive than services provided by specialists.
CONCLUSIONS
In Saskatchewan between 2004 and 2008, we observed an increase in nmsc treatment costs. More than 90% of treatment services were provided by general practice and plastic surgery physicians; dermatologists had minimal participation. Although our study investigated nmsc costs associated with physician services, it is important to acknowledge that nonsurgical treatments related to nmsc (such as radiotherapy and pharmacotherapy) and inpatient services were not captured in our data. To better understand how modalities of treatment, specialist treatment patterns, service utilization, and costs have evolved over time, further work with more current data is required to estimate the true direct cost of nmsc. Understanding the cost of nmsc could inform decision-makers about the cost burden of nmsc and the potential for investments in skin cancer prevention in Saskatchewan.
ACKNOWLEDGMENTS
The Ontario Institute for Cancer Research (oicr) is funded by the Government of Ontario through the Ministry of Economic Development, Job Creation and Trade. The Canadian Centre for Applied Research in Cancer Control (arcc) receives core funding from the Canadian Cancer Society (grant no. 2015-703549). Both oicr and arcc are proud to support the publication of this costing series.
Special thanks go to Dr. Roberta MacKay for her review and expertise and to the Saskatchewan Health Quality Council for providing access to Saskatchewan Ministry of Health data. The work conducted by each of the authors, at the time of the research, occurred under the affiliation of the Saskatchewan Cancer Agency. ACC and SS developed the analysis plan, and obtained and analyzed the data. DAT and ACC contributed substantially to manuscript development. RA, Dr. Jon Tonita, and SunSmart Saskatchewan conceived the study idea.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Madan V, Lear JT, Szeimies RM. Non-melanoma skin cancer. Lancet. 2010;375:673–85. doi: 10.1016/S0140-6736(09)61196-X. [DOI] [PubMed] [Google Scholar]
- 2.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166:1069–80. doi: 10.1111/j.1365-2133.2012.10830.x. [DOI] [PubMed] [Google Scholar]
- 3.Barton V, Armeson K, Hampras S, et al. Nonmelanoma skin cancer and risk of all-cause and cancer-related mortality: a systematic review. Arch Dermatol Res. 2017;309:243–51. doi: 10.1007/s00403-017-1724-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2014. Toronto, ON: Canadian Cancer Society; 2014. [Google Scholar]
- 5.Diepgen TL, Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002;146(suppl 61):1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 6.Geller AC, Swetter SM. Reporting and registering nonmelanoma skin cancers: a compelling public health need. Br J Dermatol. 2012;166:913–15. doi: 10.1111/j.1365-2133.2012.10911.x. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2015. Toronto, ON: Canadian Cancer Society; 2015. [Google Scholar]
- 8.Canadian Partnership Against Cancer (cpac) The Economic Burden of Skin Cancer in Canada: Current and Projected. Toronto, ON: cpac; 2010. [Google Scholar]
- 9.Fahradyan A, Howell AC, Wolfswinkel EM, Tsuha M, Sheth P, Wong AK. Updates on the management of non-melanoma skin cancer (nmsc) Healthcare (Basel) 2017;5:E82. doi: 10.3390/healthcare5040082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Motley R, Kersey P, Lawrence C. Multiprofessional guidelines for the management of the patient with primary cutaneous squamous cell carcinoma. Br J Dermatol. 2002;146:18–25. doi: 10.1046/j.0007-0963.2001.04615.x. [DOI] [PubMed] [Google Scholar]
- 11.Telfer NR, Colver GB, Morton CA on behalf of the British Association of Dermatologists. Guidelines for the management of basal cell carcinoma. Br J Dermatol. 2008;159:35–48. doi: 10.1111/j.1365-2133.2008.08666.x. [DOI] [PubMed] [Google Scholar]
- 12.Chirikov VV, Stuart B, Zuckerman IH, Christy MR. Physician specialty cost differences of treating nonmelanoma skin cancer. Ann Plastic Surg. 2015;74:93–9. doi: 10.1097/SAP.0b013e31828d73f0. [DOI] [PubMed] [Google Scholar]
- 13.Pilgrim W, Hayes R, Hanson DW, Zhang B, Boudreau B, Leonfellner S. Skin cancer (basal cell carcinoma, squamous cell carcinoma, and malignant melanoma): new cases, treatment practice, and health care costs in New Brunswick, Canada, 2002–2010. J Cutaneous Med Surg. 2014;18:320–31. doi: 10.2310/7750.2014.13162. [DOI] [PubMed] [Google Scholar]
- 14.Mudigonda T, Pearce DJ, Yentzer BA, Williford P, Feldman SR. The economic impact of non-melanoma skin cancer: a review. J Natl Compr Canc Netw. 2010;8:888–96. doi: 10.6004/jnccn.2010.0066. [DOI] [PubMed] [Google Scholar]
- 15.Zloty D, Guenther LC, Sapijaszko M, et al. on behalf of the Canadian Non-melanoma Skin Cancer Guidelines Committee. Non-melanoma skin cancer in Canada chapter 4: management of basal cell carcinoma. J Cutan Med Surg. 2015;19:239–48. doi: 10.1177/1203475415586664. [DOI] [PubMed] [Google Scholar]