Abstract
Background
The rate of mastectomy is much higher in Newfoundland and Labrador than in any other province in Canada, even for women diagnosed at an early stage. In this paper, we present qualitative data from women who have made a decision for surgical treatment and from breast surgeons in an effort to better explicate factors influencing breast cancer (bca) surgical decision-making.
Methods
The study’s descriptive, qualitative design involved holding interviews with breast surgeons and holding focus groups and interviews with women who were offered the choice of breast-conserving surgery (bcs) or mastectomy (mt).
Results
Participants included 35 women and 13 surgeons. High interest in mt and increasing requests for prophylactic contralateral mt were evident. A host of factors—clinical, demographic, psychosocial, education-related, and cultural—influenced the decisions. A key factor for women was fear of recurrence and a need to “just get rid of it,” but the experiences of others also influenced the decisions. Life stage and family considerations also factored prominently into women’s decisions.
Conclusions
Women with early-stage bca more often chose mt and often demanded prophylactic removal of the healthy breast. Findings highlight the importance of ensuring that women at average risk are appropriately counselled about the low likelihood of a subsequent contralateral bca and the lack of survival benefit associated with prophylactic contralateral mt. Findings also revealed other areas of presurgical discussion that might help women think through their personal circumstances and values so as to encourage informed surgical decisions.
Keywords: Breast cancer, mastectomy, lumpectomy, surgery, decision-making
BACKGROUND
Breast cancer (bca) remains the cancer most commonly diagnosed in Canadian women1. However, improvements in research and treatment suggest a favourable prognosis for many women diagnosed with early-stage bca (stage i or ii)1,2. Guidelines suggest that, as primary surgical treatment (if not contraindicated), these women be offered a choice of mastectomy (mt) or breast-conserving surgery (bcs) with radiotherapy3,4. Survival rates for those two options are equivalent5,6. Given that bcs has a comparable survival benefit and is less invasive in nature, it might be assumed that women with early-stage bca would be more likely to choose bcs. However, wide variation in the surgical management of bca is observed worldwide7–10, highlighting the need for further research into the factors that influence surgical treatment decisions.
Interprovincial variation in surgical choices for bca is reported in Canada2. The mt rate ranged from 26% in Quebec to 69% in Newfoundland and Labrador, with an average crude rate of 39%. Most cases of bca in Canada are diagnosed at an early stage, but in Newfoundland and Labrador (compared with other provinces), a higher percentage are diagnosed at an advanced stage (stage iii or iv)1. The higher mt rate in Newfoundland and Labrador might be explained by the larger number of advanced cases. However, recent quantitative work by our team11 revealed that, although tumour stage is a significant predictor of surgical choice, mt was the favoured choice across all age groups, tumour stages, and regions of the province, suggesting that additional factors underlie these surgical decisions.
A host of factors affect a woman’s choice of mt or bcs. Recent reviews12,13 revealed distance from a radiation facility1,2,14, fear of cancer recurrence and perceived survival outcome15–17, concerns about radiation18, concerns about body image and sexuality19,20, demographic factors such as age and education12,13, and surgeon recommendation to be key factors in surgical treatment choices21,22. Fewer publications about the perspectives of breast surgeons are available, but those that are describe not only increasing rates of mt in their practices, but also increasing requests for contralateral prophylactic mt (cpm)23,24. Surgeons described offering choice only when the clinical benefits were equal; they generally did not make a recommendation for either mt or bcs, instead they presented all the relevant risk and benefit information to women making the decision23,24.
The rate of mt in women with early-stage bca is higher in Newfoundland and Labrador than in any other province2. A better understanding of that pattern is required to ensure appropriate surgical care and to promote informed discussions between women and providers. In the present paper, to better explicate factors influencing bca surgical decision-making, we present qualitative data from surgeons and women who have made such surgical decisions.
METHODS
Sampling and Recruitment
This study was approved by the provincial Health Research Ethics Board (no. 16.023).
Recruitment and data collection occurred simultaneously between May 2016 and May 2017 in the 4 regional health authorities (rhas) of Newfoundland and Labrador. Eastern Health is the largest rha and includes the capital city of St. John’s. The other 3 rhas have smaller populations, with Central being the second most populous, followed by Western Health and Labrador–Grenfell Health. The provincial radiation treatment facility is located at the tertiary health centre and main cancer care site in St. John’s. Thus, any woman living elsewhere in Newfoundland and Labrador and choosing bcs must travel for radiotherapy.
We purposively sampled women and surgeons from the 4 rhas. Purposive sampling is a standard qualitative technique that aims to sample a diverse selection of participants who have lived experience with the issue25. Surgeons and surgical residents for potential participation were identified by the medical oncologist on the study team (EP) through the Canadian Medical Directory and the surgical residency program of the Faculty of Medicine at Memorial University. Surgeons were purposively sampled to ensure variation in rha, rural or urban place of practice, and sex. Surgeons and residents received an e-mail invitation from the medical oncologist.
Multiple methods were used to recruit women who had made surgical decisions. All participating surgeons were invited to inform eligible patients about the study; however, no women were recruited in that way. Multiple study advertisements were disseminated in the 4 rhas. Communications departments of health care centres within the rhas advertised the study through typical social media channels (e-mail messages, e-mail list messages, online newsletters); through provincial events attended by team members who could then advertise the study and answer questions (for example, the Run for the Cure fundraising event); through the annual bca retreat, which placed a 1-page study description in participant information packs; through support groups, who were contacted and sent study invitations (in one instance, a team member attended and explained the study); through a radio interview with the corresponding author held in the Central rha; and through study posters circulated in hard copy to multiple sites and posted to multiple Facebook pages. In all instances, women who were offered a choice of mt or bcs were invited to contact the research team to take part.
Data Collection
Surgeons were invited to take part in a face-to-face or telephone interview, but were also given the choice to provide their answers in a Word document after they had received the interview guide by e-mail. Women were invited to a focus group discussion with other women who had made a bca surgical decision. In an effort to accommodate as many participants as possible, women were also given the option to attend an individual interview or to provide their answers by e-mail. Guides for the interviews and focus groups were created by the study team after a literature review; the guides were also underpinned by the experience of study team members (including a patient partner). The guides are available upon request.
All discussions were semi-structured, using prompts and open-ended questions to facilitate discussion. Focus groups are ideal for exploring the personal meaning of health and illness, and are useful when people have shared experiences26. Focus groups were moderated by two team members (ED, HE) experienced in qualitative data collection. Interviews were conducted by one team member (CS) experienced in qualitative interviewing. Interviews lasted about 40 minutes; focus group discussions lasted about 60 minutes. In all discussions, questions were not confined to a specific order, and participants were encouraged to discuss other issues important to them. Despite some different wording that emerged naturally during interviews and focus groups, all discussions encompassed the same content. A core set of topics was covered, including influences on surgical decisions, the decision-making atmosphere, information provided during surgical consultations, and information needs. Here, we focus on the factors that influenced surgical treatment decisions.
Data Analysis
All discussions were tape-recorded and transcribed verbatim. A small proportion of the participants used e-mail, and their transcripts were included verbatim in the analysis. Qualitative description27 was used to summarize the data pertaining to surgical decisions. Qualitative description is a form of naturalistic inquiry with no specific assumptions about the data. Instead, data are presented in the language of participants; no attempt is made to present the data in theoretical ways. The end result is a comprehensive summary of the event in question27.
Transcripts were read and reread several times by one investigator (HE). Interview data were then isolated and organized by discussion topic (for example, initial diagnosis, choice of bca surgery, information provided, and so on). Those sections were read and reread to identify and index emerging categories and themes, which were annotated on the transcripts. No qualitative software was used in the analysis. Inductive subcoding of the data relevant to the surgical decision was completed using the constant comparison method28,29. In that process, data were compared between and within transcripts to establish analytical categories and themes27–29. The method required constant shifting between (and within) transcripts to continuously compare the perceptions and experiences of participants. Three other team members (ED, RR, JC) independently read all transcripts and highlighted emerging themes. Discussions between those investigators throughout the analysis verified emerging categories and themes until no new themes could be added. When the investigators had agreed on the thematic analysis, findings were presented to and discussed with the research team. No new categories or themes were suggested after the team discussion, and data saturation was deemed complete.
RESULTS
The study attracted participation by 35 women, 12 surgeons, and 1 surgical resident. The resident’s responses were very similar to those of the surgeons and are therefore reported with the surgeon group. Focus groups were held with women around the province: 3 in St. John’s, 2 in Corner Brook, 1 in Gander, and 1 in Happy Valley–Goose Bay (Labrador). Table I provides details about data collection.
TABLE I.
Data collection methods used
| Variable | Surgeons (n) | Women (n) |
|---|---|---|
| Health authoritya | ||
| Eastern | 8 | 18 |
| Central | 2 | 4 |
| Western | 1 | 7 |
| Labrador–Grenfell | 1 | 6 |
|
| ||
| Data collection method | ||
| Written response (e-mail) | 3 | 3 |
| Telephone interview | 10 | 3 |
| Focus group discussion | 0 | 29 |
Surgeon numbers do not add to 13 because 1 surgeon did not provide demographic information.
Participants
Table II displays demographic information for the participating surgeons and women.
TABLE II.
Demographic information for 13 surgeon participants and 35 patient participants
| Variable | Value |
|---|---|
| Surgeonsa | |
|
| |
| Women (n) | 5 |
|
| |
| Age (years) | |
| Mean | 46 |
| Range | 30–56 |
|
| |
| Time in practice (years) | |
| Mean | 10 |
| Range | 1–26 |
|
| |
| Practice in rural setting (%) | 15 |
|
| |
| Annual surgeries (%) | |
| Mastectomy (MT) | 63 |
| Breast-conserving surgery (BCS) | 37 |
| MT range | 40–100 |
|
| |
| Practice setting (%) | |
| Academic centre | 39 |
| Community | 31 |
| Urban hospital | 15 |
| Rural hospital | 7 |
| Patients | |
|
| |
| Women (n) | 35 |
|
| |
| Age (years) | |
| Mean | 54 |
| Range | 38–76 |
|
| |
| Breast cancer surgical history (n) | |
| BCS first and only | 1 |
| BCS first, then second BCS at later date | 3 |
| BCS first, then MT at later date | 5 |
| MT first and only | 20 |
| MT first, then prophylactic MT at later date | 6 |
|
| |
| Rural residence (%) | 23 |
|
| |
| Time since last surgery (years) | |
| Mean | ~5 |
| Range | 2–16 |
|
| |
| Self-rated health status at time of interview (%) | |
| Excellent | 3 |
| Very good | 40 |
| Good | 48 |
| Fair | 9 |
Demographic data are provided for the 12 surgeons who provided responses, and thus totals might not reach 100%.
Of the women, 74% underwent either mt as their first and only surgery or mt followed by prophylactic removal of the other breast at a later date. In keeping with the high rate of mt reported in the literature and in accounts from surgeons, a small proportion of the women underwent bcs. Women were 54 years of age on average, and about 5 years had passed since their last bca surgery. Three quarters lived in an urban setting. Most were married with children (approximately 83%), rated themselves in a middle (66%) or high (26%) income bracket, and were highly educated (approximately 60% had an undergraduate or graduate degree).
Surgeons had been in practice for an average of 10 years, and mt constituted the greatest proportion of the bca surgeries that they performed (63%). Some surgeons indicated that they performed no bcs at all. Most practiced in an urban and academic setting, although about one third practiced in a community setting.
Factors Influencing Surgical Treatment Decisions
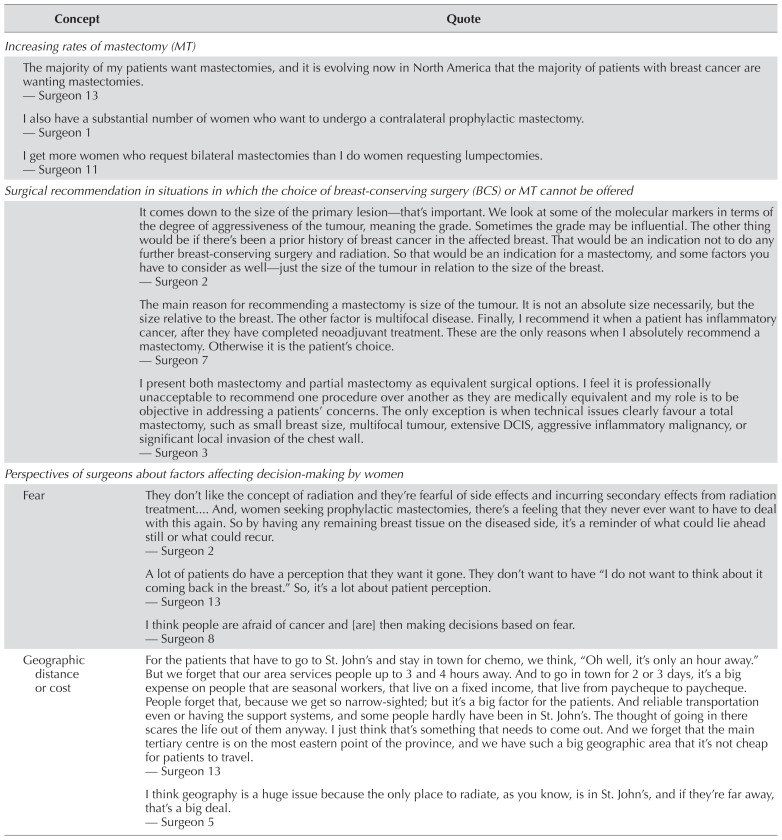
A host of clinical, demographic, cultural, and psychosocial factors were noted to influence women’s decisions about mt or bcs. The accounts of the women and the surgeons showed a high rate of concordance, with only slight differences. Tables III and IV outline key concepts in the data, with supporting quotes.
TABLE III.
Key concepts raised by surgeons, with supporting quotes
| Concept | Quote |
|---|---|
| Increasing rates of mastectomy (MT) | |
|
| |
| The majority of my patients want mastectomies, and it is evolving now in North America that the majority of patients with breast cancer are wanting mastectomies. — Surgeon 13 | |
| I also have a substantial number of women who want to undergo a contralateral prophylactic mastectomy. — Surgeon 1 | |
| I get more women who request bilateral mastectomies than I do women requesting lumpectomies. — Surgeon 11 | |
|
| |
| Surgical recommendation in situations in which the choice of breast-conserving surgery (BCS) or MT cannot be offered | |
|
| |
| It comes down to the size of the primary lesion—that’s important. We look at some of the molecular markers in terms of the degree of aggressiveness of the tumour, meaning the grade. Sometimes the grade may be influential. The other thing would be if there’s been a prior history of breast cancer in the affected breast. That would be an indication not to do any further breast-conserving surgery and radiation. So that would be an indication for a mastectomy, and some factors you have to consider as well—just the size of the tumour in relation to the size of the breast. — Surgeon 2 |
|
| The main reason for recommending a mastectomy is size of the tumour. It is not an absolute size necessarily, but the size relative to the breast. The other factor is multifocal disease. Finally, I recommend it when a patient has inflammatory cancer, after they have completed neoadjuvant treatment. These are the only reasons when I absolutely recommend a mastectomy. Otherwise it is the patient’s choice. — Surgeon 7 |
|
| I present both mastectomy and partial mastectomy as equivalent surgical options. I feel it is professionally unacceptable to recommend one procedure over another as they are medically equivalent and my role is to be objective in addressing a patients’ concerns. The only exception is when technical issues clearly favour a total mastectomy, such as small breast size, multifocal tumour, extensive DCIS, aggressive inflammatory malignancy, or significant local invasion of the chest wall. — Surgeon 3 |
|
|
| |
| Perspectives of surgeons about factors affecting decision-making by women | |
|
| |
| Fear | They don’t like the concept of radiation and they’re fearful of side effects and incurring secondary effects from radiation treatment And, women seeking prophylactic mastectomies, there’s a feeling that they never ever want to have to deal with this again. So by having any remaining breast tissue on the diseased side, it’s a reminder of what could lie ahead still or what could recur. — Surgeon 2 |
| A lot of patients do have a perception that they want it gone. They don’t want to have “I do not want to think about it coming back in the breast.” So, it’s a lot about patient perception. — Surgeon 13 |
|
| I think people are afraid of cancer and [are] then making decisions based on fear. — Surgeon 8 |
|
|
| |
| Geographic distance or cost | For the patients that have to go to St. John’s and stay in town for chemo, we think, “Oh well, it’s only an hour away.” But we forget that our area services people up to 3 and 4 hours away. And to go in town for 2 or 3 days, it’s a big expense on people that are seasonal workers, that live on a fixed income, that live from paycheque to paycheque. People forget that, because we get so narrow-sighted; but it’s a big factor for the patients. And reliable transportation even or having the support systems, and some people hardly have been in St. John’s. The thought of going in there scares the life out of them anyway. I just think that’s something that needs to come out. And we forget that the main tertiary centre is on the most eastern point of the province, and we have such a big geographic area that it’s not cheap for patients to travel. — Surgeon 13 |
| I think geography is a huge issue because the only place to radiate, as you know, is in St. John’s, and if they’re far away, that’s a big deal. — Surgeon 5 |
|
|
| |
| Influence of the stories of others | One of the biggest factors I find is what the neighbour or the friend or one of the older family members had is a big thing. They’ll come and tell me “my friend had this, and that’s what I want” or “my Mom had this.” So previous experience from a family member or a friend is one of the biggest influences. — Surgeon 4 |
| I find a lot of people here anyway use a lot of anecdotal references: So they had a neighbour who had this done and then the cancer came back or various other things. And that tends to sway people’s decision. — Surgeon 8 |
|
| A lot of women know other women who have had breast cancer surgery, and so a lot of them take their information from those women as the most reliable source. I think that influences a lot of people’s decisions, when these other women had their surgery, like, 40 years ago. Things have changed, standards have changed, but a lot of people rely on that—here, at least. — Surgeon 1 |
|
|
| |
| Age or life stage | Yeah, well, obviously age makes a difference, whether ... they’re married or not married, or whether their spouse is alive. All of these things make a difference because, again, they want to maintain their femininity, and they want a less disfiguring operation. If they’re still married, they got young kids, so age is a big factor in it. — Surgeon 12 |
| I think there’s an age component. Elderly women around the bay, especially whose husbands are gone—they don’t care. I don’t think it matters a row of beans to them because it’s not a part of them that matters to them so much anymore. — Surgeon 5 |
|
|
| |
| Lack of understanding or education | The decision-making on the patient’s side depends on education. That’s what it comes down to. So our job is to present all the options and talk about the tumour itself and all its characteristics and everything But I know that education plays a role in decision-making. My impression so far has been that less educated segments of the population tend to choose more radical options. — Surgeon 9 |
| I think there’s this notion that if the entire breast is removed, the cancer is not going to come back, and I guess part of that comes from a lack of understanding that breast cancer is more of a systemic disease And the same goes for these prophylactic mastectomies of the other side. Well, I’m not going to get it in that breast now that it’s gone. — Surgeon 1 |
|
| They don’t understand that getting a mastectomy versus a lumpectomy and radiation will give you the same outcome. — Surgeon 8 |
|
| They have a poor understanding of research, and long-term outcomes, and stuff like that. And when they hear “cancer,” they just want it off So I think that, even though a lot of us are still pushing breast conservation surgery, I think ... the general consensus out there is “No, I want to have my breast off,” even though you tell them the 5-year survival is the same. — Surgeon 12 |
|
|
| |
| Cultural influences | I think there is a cultural bias in Newfoundland women towards mastectomy led largely by a belief that somehow this is a better operation, which is not true. But people think that. — Surgeon 5 |
| The other thing is there may just be a bit of a cultural difference between [the] expectations and approach to surgery here versus somebody from Toronto, and I think that would be interesting to explore. I don’t have anything to back this up, but I suspect [it] based on the numbers I see in clinic. And so I think maybe cosmesis is not as important of an issue here as it would be somewhere on the mainland. And so for a lot of women the easiest thing is just to say. “Well, you know I want it all off.” I hear that all the time. — Surgeon 1 |
|
| A very small minority of women express any comments about cosmetics of a full mastectomy and when the issue is raised as a potential benefit of a partial mastectomy, the overwhelming response is that cosmetics are not a concern. In the last 10 years, there has been increased presentation of the option for reconstructive surgery, but most women express no interest initially or at follow-up visits. The majority of women and their spouses state that the cosmetics of a full mastectomy have no effects on their relationship or on their perception of overall health. There are many comments that breast exposure is unnecessary and that clothing options eliminate the cosmetic deficit of a total mastectomy. In summary, the breast appears to have a much lower value as a cosmetic asset in my patient population and knowledge that the entire organ has been removed is of far greater value. — Surgeon 3 |
|
TABLE IV.
Key concepts raised by women, with supporting quotes
| Concept | Quote |
|---|---|
| Pushing for mastectomy | |
|
| |
| He didn’t want me to get the second one removed, but I wanted it. It was done a year later. He wanted me to think about it. — Focus group, Labrador | |
| When I did meet with the surgeon, she wanted me to have a lumpectomy definitely. But I said no, I want the breast removed, and I said I want both removed at that time. And I think that was just something in my head: If I end up having cancer at any point in time both the breasts would be removed. And she says, no, you need to go back and think about this. So I just went back out, and I had a 2-week period, I guess, before the surgery. But I would call her office every other day and say I want both my breasts removed. — Focus group 1, Corner Brook | |
| I walked in, and I said this is what I want done. She had said to me, you know, go home and think over what you want done. I said I know what I want done, and this is what I want. — Focus group 1, Corner Brook | |
| I wanted two gone, and she wouldn’t do it. At that point in time, she wanted me to recover from the first surgery and have the chemo and the radiation. I wanted both of them gone right away, but she wouldn’t take the two of them at the time. She said she wanted me to recover, and if I still felt the same way in 2 years’ time she would. And she did. — Focus group 2, St. John’s | |
|
| |
| Factors influencing surgical decisions | |
|
| |
| Clinical factors or genetics | When the biopsy came back, I had a triple-negative breast cancer, which is fairly rare, and there’s a high reoccurrence in the first couple of years. I had small, dense breasts, and pretty much the breast—all the breast—had to be removed because of the size of the tumour and, you know, it had just grown so quickly. — Focus group 2, St. John’s |
| The way the doctors described it to me was that only 10% of breast cancers are genetic, and 30% of that 10% is this BRCA1 and BRCA2. There will be a BRCA3, 4, 5, 6, 7, 8 ... they just haven’t done research yet. So that’s why Newfoundland there are a lot of people with a lot of different cancers that they really feel is a genetic breast cancer, but they cannot say this is what you have, you know [My daughter has] been tested, and she’s positive, and that’s awful. It’s worse than me. — Focus group 2, St. John’s |
|
| I’m high-risk, and I’ve been through the genetics, and they came back with the recommendation that I alternate MRI with mammogram every 6 months, and to start with my daughter at 25 and all my nieces. I’m negative for 9 genes they tested me for, but it’s the strong family history. — Focus group, Gander |
|
|
| |
| Fear or anxiety | The surgeon did tell me my choices. He told me that I could either do lumpectomy which would be definitely followed by radiation or a mastectomy, and I chose the mastectomy because I just wanted it to be gone—that was what I felt. And I read about with the lumpectomy the chance of having to go back and get more surgery if the margins weren’t clear, and I felt like I just wanted to get one surgery and be finished And the idea of radiation scared me, because the things I’d heard about it and being afraid that it could cause other cancers. — Focus group, Labrador |
| I think the thing that resonated with me the most was she said if you have the mastectomy it means no radiation; it also means that we don’t have to ever have to go back a second time because with the lumpectomy, if there weren’t clear margins it means you have to go back for more surgery Having the breast removed, that was just kind of like, you know, let’s just do it. It was the thought of having to have chemo, having to have my body radiated, and what that was going to do to. — Focus group 2, Corner Brook |
|
| But, then, when you get a mastectomy, you don’t have that breast tissue surrounding your area which can lead to other issues. It can reoccur quicker if you never had a mastectomy. — Face-to-face interview, St. John’s |
|
| I said get me in as soon as he can. I said I don’t care who it is. I said I know that I just want to get this out of me as soon as possible. — Focus group 1, St. John’s |
|
| Since I’ve had the two of them off, I feel like, oh my god, I can conquer the world. And it’s just amazing how just, like, once I had the two of them off, I’m a different person now than what I was when I had these things on. — Focus group 1, St. John’s |
|
|
| |
| Family (sometimes related to geography and access to radiation) | All I was thinking about was I got to live long enough to get my kids raised. — Focus group 2, Corner Brook |
| With the radiation with two small kids and just the thought of having to go through like that length of time, I definitely didn’t want to do that. So that’s I guess my reasoning for opting for the mastectomy. — Focus group, Labrador |
|
| The most important factor in my decision was my daughter, she is only [age], and I want to be here to see my grandkids. If removing my boobs will help make that happen, then, “Bye bye.” As long as I’m here, I’m not worried about having breasts on my chest. They didn’t define who I was, and I don’t need them to live. — E-mail interview, St. John’s |
|
| I am caregiver to my husband, so I had to be at home So radiation was out of the question, both from a money point of view, and there’s no arrangement that you could have someone look after him for 6 weeks I’m [in St. John’s]. — Face-to-face interview, Labrador |
|
| I chose not to have the lumpectomy for the simple fact I would have to go into St. John’s for radiation. At the time I had a teenage daughter at home. I said no. — Focus group 1, Corner Brook |
|
| I think for particularly those that are of lower income living in the more remote areas. That does have a tremendous impact on people... Even for me that was, you know, away from my kids for 6 weeks, and we don’t have to incur that cost because even for us that would have been a financial burden. — Focus group 2, Corner Brook |
|
|
| |
| Life stage | I think if I had been 65, had my kids raised, maybe that decision may have been a very—because I would have been in a very different place. — Focus group 2, Corner Brook |
| At that time in my life, children were grown and out on their own and working in their chosen fields. No matter where I had to go, for however long I had to go, I was prepared to do that. You know that’s just where I was at that time in my life; I didn’t have a reason to or a strong reason to keep me back home type of thing, right? — Focus group 1, Corner Brook (still chose mastectomy) |
|
| I was [age]. I didn’t want to be a swimsuit model. I was finished raising my children. I was no more going to nurse. It hasn’t bothered me. I never bothered with the reconstruction. And I think depending—I mean if you’re younger—I don’t know. — Focus group, Gander |
|
|
| |
| Cultural influences | I was engrossed in it all and talking to everyone. What do you mean you don’t know your stage? Don’t know your grade? You don’t know this, you don’t know that. Like you don’t know your other options. But they don’t care, they don’t want to know. They know it’s cancer—that big “C” word—and they just want to do what seems to be right. Just take it off. It is an attitudinal thing in Newfoundland that leads to all these mastectomies. Probably more attitudinal than the surgeon saying let’s do surgery. Is it something about our society? Is it that we got a lot of women who don’t care that their breast is off or that would rather just take that route get it done and over with? I don’t know. Now whether it’s right or wrong for surgeons to do unnecessary surgery just because of the attitude of the women I don’t know. — Focus group, Gander |
| I had read that article about Newfoundland having the highest rate of mastectomy, and they had talked about why. Maybe geography and those kinds of things. I think that does have an impact. Personally, I don’t think that’s the overwhelming reason. I think that Newfoundland, that women generally who grow up in Newfoundland, primarily small rural communities that we’re very strong and resilient women Most of us are very strong in terms of self- confident. We’re not attached to the breast being the sexual image thing, you know, and I think that does have an impact in terms of decisions. — Focus group 2, Corner Brook |
|
|
| |
| Experiences of others | I know a few other people. There’s another women diagnosed about a month after me. She opted for a lumpectomy, and she’s finding it really difficult. I’m like, thanks be to God I had the mastectomy. People say things like that to me, and it’s a relief to me. — Focus group 1, St John’s (mastectomy) |
| I know from talking to women who’ve had breast cancer in the past, they felt that acted too quickly, too soon. They sort of regretted what they did and I said, “Well, I’m going to take a wait-and-see approach.” So, after the surgery, there was nothing in the lymph nodes I’ve heard women say, “I don’t want to know anything. The less I know, the better.” But I wasn’t like that. I couldn’t get enough information. — Focus group 2, St. John’s (breast-conserving surgery) |
|
| I had an aunt, she was diagnosed with breast cancer the exact same age I was. She had her mastectomy, and after I found out I had breast cancer, I told her I had them both off. She said, “I wish I had done the same thing.” — Focus group 1, Corner Brook (double mastectomy) |
|
| And also talking to this friend of mine, and I thought, yeah, mastectomy, maybe I’ll feel more sure than the other. There was this neighborhood woman who had to have radiation and then 10 years later it was back, and she had to have the mastectomy then anyway. — Face-to-face interview, Labrador (mastectomy) |
|
MRI = magnetic resonance imaging.
Surgeons
All surgeons recognized the high rate of mt in the province, and none were surprised. In keeping with the rising rate of cpm12,16, some recalled patients who requested that both breasts be removed despite the lack of a clinical need (Table III).
Surgeons explained that their surgical recommendation (if one was made) was based strictly on clinical criteria and guidelines: “The standards of care. So basically, I follow our guidelines [Surgeon 13].” Specific clinical factors influenced the recommendation (Table III).
Although they referred solely to evidence-based surgical treatment recommendations, surgeons had clearly observed numerous variables that they perceived to be influencing the decisions taken by their patients (Table III). Those reasons ranged from fear and worry to geography, family influences, age, culture, and lack of education or understanding.
Women
Women recounted numerous influences on their surgical decision (Table IV). Although clinical factors or genetic predisposition were sometimes noted, those factors were mentioned least often. In some cases, women pushed for not only a mt, but a cpm, often against their surgeon’s advice (Table IV).
The factor mentioned most often, by far, was fear. Women described specific fears (for example, of radiation) or simply described generalized bca-associated fear and anxiety that they could not live with (Table IV). As one women remembered it, “Although offered the choice of surgery, I didn’t even consider a lumpectomy; it wasn’t even a consideration for me. I just wanted it gone” [focus group, Labrador]. There was a feeling of relief when breasts were removed (Table IV).
Women described family considerations as well— in particular, having young children or a partner for whom they were a caregiver, as factors in their declining radiation and concomitantly being away from home (Table IV). Related were a woman’s life stage and age at the time of the decision. Those who had finished childrearing indicated that the choice of surgery might have been different had they been younger or still raising children. The experiences of others also seemed to influence decisions, or at least were used as partial justification for bcs or mt (Table IV).
Of the few women who chose lumpectomy, their recollections included a recommendation from their surgeon:
He was very supportive and told me of all the options—types of surgeries, follow-up possibilities (chemo, radiation, meds, etc.)—and recommended lumpectomy and radiation. I was one hundred percent positive that a mastectomy was the only way to go, but after the information obtained, I fully supported that recommendation (lumpectomy/rad), as did my husband.
—St. John’s, e-mail interview
For others, body image concerns seemed to be an important consideration:
I was not ready to look down and see nothing where my breast should be. I made my decision based on my own feelings, which were confirmed by those of my surgeon. Body image and my role as a “woman” were the most important factors in my decision. I didn’t need a whole lot of time and was quite comfortable with it.
—St. John’s, second e-mail interview
DISCUSSION AND CONCLUSIONS
Surgical treatment decisions in bca have been well studied. Nonetheless, the perspectives of surgeons are underexplored, and considerable variation in breast units worldwide suggests that additional research is warranted.
Women described demanding a mt, and often cpm, which was echoed by surgeons. Recent literature describes increasing interest in cpm despite evidence of no significant survival benefit, at least for women with a first diagnosis of unilateral bca23,24,30,31. Although the present study did not focus on cpm, the fact that women spontaneously talked about their experiences with asking surgeons for that surgery is notable. Such findings highlight the importance of ensuring that women at average risk are appropriately counselled about the low likelihood of a subsequent contralateral bca and the lack of survival benefit with cpm. Discussions with those women might cover less invasive treatment options (for example, anti-estrogen therapy) and the risks associated with additional surgery (for example, the potential for additional complications and longer recovery time)23.
Surgeons mentioned clinical factors (tumour characteristics, for instance) and practice guidelines as influencing their surgical recommendation (if a recommendation was made). Otherwise, they presented information about bcs and mt and left the decision to patients, in keeping with practice guidelines in Canada for the treatment of early-stage bca24. In contrast, surgeons in the United States are guided by state legislation that mandates elements of the surgical discussion with patients (for example, reconstruction, presentation of all treatment options)24. Surgeons in our study rarely mentioned reconstruction, and those who did indicated that their patients expressed little interest—a finding that corresponds with the women’s accounts (very few described undergoing or even considering reconstruction).
All participants described a culture in Newfoundland and Labrador that clearly favours mt. Quantitative data generated by our team also bear this out11. Women described the strength and resilience of women in the province; surgeons and women both described a lack of attachment to the breast as a sexual entity and a lack of concern with cosmesis. Only 1 participant who chose bcs spoke about her identity as a women being a key factor in her surgical choice. Body image and sexuality concerns have been reported to influence women’s surgical choices19,20,32, but we did not readily observe such concerns in our data. Although we do not know exactly what it is about the culture in Newfoundland and Labrador that influences the trend of mt, we think it important to note—particularly for surgeons who come to practice in the province. Those findings could provide a kind of anticipatory guidance about what they could face in practice and allow them to prepare alternatives for discussion.
Our findings suggest that the type of information provided to women is critically important; surgeons reported deficiencies in women’s understanding of the equivalence of surgical options for early-stage bca. Women described a need to “just get rid of it” so as to lessen fears or worry and increase their chance of survival, a robust finding in the literature12,13,17,18,32,33 and an attitude that persists despite the equivalency of bcs and mt for prognosis in early-stage bca. Those findings suggest the need for reconsideration of the timing and type of information provided to women about their surgical options. In this paper, we have focused on factors affecting surgical choice; however, a second paper by our team will explore the decision-making context in more detail, including focusing on the information provided and women’s information needs. Here, we note that the push for mt in women eligible for bcs highlights the need to explore what women understand and what is presented during initial surgical consultations. For example, women should understand their personal risks for local, contralateral, and systemic recurrence and how removal of the unaffected breast does not affect those risks equally16.
In line with other research, we observed no consistent effect of age on the surgical decision11–13. But findings in the present study and in other publications suggest a trend of younger women choosing mt. Although surgeons noted that older patients were more likely to be unconcerned about losing a breast, women and surgeons both recognized that life stage—and particularly whether children were grown or not—influenced the decision. The personal circumstances of patients should be part of the discussion at the surgical consultation to encourage women to reflect on personal values and surgical preferences in light of their personal circumstances. Those circumstances can also reflect the influence of geography on the surgical decision. In our quantitative data11, driving time to the province’s only radiation facility was a significant predictor of surgical choice. Women living in rural and remote areas have a greater distance to travel for radiation. In a downloadable Quick Stats file, the Canadian Institute for Health Information provides bca surgical data for the provinces and territories for 2013–2014: https://www.cihi.ca/sites/default/files/document/quickstat_breastcancer_en_1.xlsm. Those data also show a high rate of index mt for Newfoundland and Labrador (63.2%), exceeded only by the territories (70.7%). Saskatchewan and Prince Edward Island had the next highest rates (54.4% and 53.8% respectively). In our quantitative study11, women were 1.15 times more likely to choose mt for every 40-minute increase in driving time. Nonetheless, mt remained the most common choice across all categories of driving time.
The literature is robust in highlighting the influence of proximity to radiation facilities on surgical choice12–15. We had expected to find similar evidence in the present study, such that women from health authorities outside of Eastern Health would be more likely to undergo mt. However, the present findings reveal that distance is particularly problematic depending on life circumstances, such as having school-age children or being a caregiver for a partner. In those situations, women stated that they simply could not be away from home for 6 weeks. Indeed, some reported they did not even consider bcs for that reason. Again, we note that reflection on personal circumstances and a discussion of potential solutions for those women might be an important component of the presurgical discussion so as to ensure that women are not disadvantaged because of where they live. Continued improvements in irradiation techniques (for example, shorter regimens) could mean that surgical trends will favour bcs in the future12. It will therefore be important that women understand the shorter time needed.
Finally, we note the effect of the stories and experiences of others on women’s surgical choices, a factor also described by surgeons and reported in the literature18. It will be important to discuss with women the influence of the stories of others, particularly when those surgical choices were made in a different era, when treatment options were fewer, and prognosis was not as positive. Such experiential knowledge, including empathetic knowledge of the experiences of the cancer journeys of others, influences prophylactic surgical decisions in the context of inherited breast and colon cancer34,35. Our findings suggest that it also plays a role in the surgical decision-making of bca patients. That role is not well described in the literature, and future studies could focus on the influence of experiential knowledge on bca surgical choices.
Study findings should be interpreted in light of our study’s limitations. We did not have access to the clinical records of women participants. We therefore cannot confirm clinical details or factors that might have affected decisions (for example, hormone receptor status, genetic mutation status) or provided a more comprehensive picture of the surgical decision (for example, reconstruction). We note, however, that very few women or surgeons described reconstruction requests.
A key limitation of the study is the small number of women who had chosen bcs. That limitation was unsurprising given the clear preference for mt in our province, but future research might focus exclusively on this group to more clearly elucidate their understanding of surgical choices. We were also able to recruit only a small number of surgeons. Their accounts were very similar, and we noted great congruence between their accounts and the accounts of women. However, larger numbers of participants from areas outside Eastern Health might have highlighted additional influences on surgical decisions.
As in all research, selection bias might be present, in that women with a preference for mt could have been more likely to take part. The data are also subject to recollection and memory biases. Most women had made their surgical decision at least 5 years before being interviewed; although their perspectives are important, they do not reflect the experiences of women who made the decision more recently. Future research could include newly diagnosed women to better reflect decisions at the time of diagnosis.
Despite the foregoing limitations, the data reveal a consistent choice of mt by participants and surgical practices, raising questions about how patients with bca in Newfoundland and Labrador are understanding and exercising their treatment options. We hope that the findings are helpful to women and clinicians alike—in particular, by outlining areas for reflection and discussion during surgical consultations.
ACKNOWLEDGMENTS
We are grateful to the women and surgeons who took part in this study. Funding to HE and ED (co-principal investigators) was provided by a grant from the Enhancing Healthcare in Newfoundland and Labrador competition, administered through the Newfoundland and Labrador Centre for Applied Health Research, St. John’s, NL.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Canadian Partnership Against Cancer (cpac) Breast Cancer Control in Canada: A System Performance Special Focus Report. Toronto, ON: cpac; 2012. [Google Scholar]
- 2.Porter G, Wagar B, Bryant H, et al. Rates of breast cancer surgery in Canada from 2007/08 to 2009/10: retrospective cohort study. CMAJ Open. 2014;2:E102–8. doi: 10.9778/cmajo.20130025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grunfeld E, Sukhbinder DT, Levine M on behalf of the Canadian Breast Screening Initiative, Steering Committee on Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. Clinical practice guidelines for the care and treatment of breast cancer: follow-up after treatment for breast cancer (summary of the 2005 update) CMAJ. 2005;172:1319–20. doi: 10.1503/cmaj.045062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Kingdom, National Institute for Health and Clinical Excellence (nice) Early and Locally Advanced Breast Cancer: Diagnosis and Treatment. Cardiff, UK: National Collaborating Centre for Cancer; 2009. (Clinical guideline 80). [Google Scholar]
- 5.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow up of a randomized study comparing breast conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–32. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 6.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Eng J Med. 2002;347:1233–41. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 7.Ishizaki T, Imanaka Y, Hirose M, Kuwabara K, Ogawa T, Harada Y. A first look at variation in use of breast conserving surgery at five teaching hospitals in Japan. Int J Qual Health Care. 2002;14:411–18. doi: 10.1093/intqhc/14.5.411. [DOI] [PubMed] [Google Scholar]
- 8.Molenaar S, Oort F, Sprangers M, et al. Predictors of patients’ choices for breast-conserving therapy or mastectomy: a prospective study. Br J Cancer. 2004;90:2123–30. doi: 10.1038/sj.bjc.6601835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morrow M, White J, Moughan J, et al. Factors predicting the use of breast-conserving therapy in stage i and stage ii breast carcinoma. J Clin Oncol. 2001;19:2254–62. doi: 10.1200/JCO.2001.19.8.2254. [DOI] [PubMed] [Google Scholar]
- 10.Caldon LJM, Walters SJ, Reed JA, Murphy A, Worley A, Reed MWR. Case-mix fails to explain variation in mastectomy rates: management of screen-detected breast cancer in a U.K. region 1997–2003. Br J Cancer. 2005;92:55–9. doi: 10.1038/sj.bjc.6602264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCrate F, Dicks E, Powell E, et al. Breast cancer surgical treatment choices in Newfoundland and Labrador: a retrospective cohort study. Can J Surg. 2018;61:377–84. doi: 10.1503/cjs.015217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mac Bride MB, Neal L, Dilaveri CA, et al. Factors associated with surgical decision making in women with early-stage breast cancer: a literature review. J Womens Health (Larchmt) 2013;22:236–42. doi: 10.1089/jwh.2012.3969. [DOI] [PubMed] [Google Scholar]
- 13.Bellavance EC, Kesmodel SB. Decision-making in the surgical treatment of breast cancer: factors influencing women’s choices for mastectomy and breast conserving surgery. Front Oncol. 2016;6:74. doi: 10.3389/fonc.2016.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boscoe FP, Johnson CJ, Henry KA, et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast. 2011;20:324–8. doi: 10.1016/j.breast.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 15.Shearer R, Rashid M, Hubbard G, Abbott N, Daltrey I, Mullen R. Factors associated with patients in the Scottish Highlands who chose mastectomy when suitable for breast conservation. Gland Surg. 2016;5:385–90. doi: 10.21037/gs.2016.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenberg SM, Sepucha K, Ruddy KJ, et al. Local therapy decision-making and contralateral prophylactic mastectomy in young women with early-stage breast cancer. Ann Surg Oncol. 2015;22:3809–15. doi: 10.1245/s10434-015-4572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swainston K, Campbell C, van Wersch A, Durning P. Treatment decision making in breast cancer: a longitudinal exploration of women’s experience. Br J Health Psychol. 2012;17:155–70. doi: 10.1111/j.2044-8287.2011.02028.x. [DOI] [PubMed] [Google Scholar]
- 18.Caldon LJ, Collins KA, Wilde DJ, et al. Why do hospital mastectomy rates vary? Differences in the decision-making experiences of women with breast cancer. Br J Cancer. 2011;104:1551–7. doi: 10.1038/bjc.2011.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osborn GD, Hodin M, Drew PJ, et al. Patient demographics and treatment for early breast cancer: an observational study. Breast. 2006;15:377–81. doi: 10.1016/j.breast.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 20.Sivell S, Elwyn G, Edwards A, Manstead AS on behalf of the BresDex group. Factors influencing the surgery intentions and choices of women with early breast cancer: the predictive utility of an extended theory of planning behaviour. BMC Med Inform Decis Mak. 2013;13:92. doi: 10.1186/1472-6947-13-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schonberg MA, Birdwell RL, Bychkovsky BL, et al. Older women’s experience with breast cancer treatment decisions. Breast Cancer Res Treat. 2014;145:211–23. doi: 10.1007/s10549-014-2921-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weber K, Soloman D, Meyer B. A qualitative study of breast cancer treatment decisions: evidence for five decision-making styles. Health Commun. 2013;28:408–21. doi: 10.1080/10410236.2012.713775. [DOI] [PubMed] [Google Scholar]
- 23.Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing use of contralateral prophylactic mastectomy despite no improvements in long-term survival for invasive breast cancer. Ann Surg. 2017;265:581–9. doi: 10.1097/SLA.0000000000001698. [DOI] [PubMed] [Google Scholar]
- 24.Covelli AM, Baxter NN, Fitch MI, Wright FC. Increasing mastectomy rates—the effect of environmental factors on the choice for mastectomy: a comparative analysis between Canada and the United States. Ann Surg Oncol. 2014;21:3173–84. doi: 10.1245/s10434-014-3955-4. [DOI] [PubMed] [Google Scholar]
- 25.Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling: merging or clear boundaries? J Adv Nurs. 1997;26:623–30. doi: 10.1046/j.1365-2648.1997.t01-25-00999.x. [DOI] [PubMed] [Google Scholar]
- 26.Wilkinson S. Focus groups in health research: exploring the meanings of health and illness. J Health Psychol. 1998;3:329–48. doi: 10.1177/135910539800300304. [DOI] [PubMed] [Google Scholar]
- 27.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–40. doi: 10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 28.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320:114–16. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, NY: Routledge; 2017. [DOI] [Google Scholar]
- 30.Pesce C, Liederbach E, Wang C, Lapin B, Winchester DJ, Yao K. Contralateral prophylactic mastectomy provides no survival benefit in young women with estrogen receptor–negative breast cancer. Ann Surg Oncol. 2014;21:3231–9. doi: 10.1245/s10434-014-3956-3. [DOI] [PubMed] [Google Scholar]
- 31.Lostumbo L, Carbine N, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev. 2010:CD002748. doi: 10.1002/14651858.CD002748.pub3. [DOI] [PubMed] [Google Scholar]
- 32.Halkett G, Arbon P, Scutter SD, Borg M. The experience of making treatment decisions for women with early stage breast cancer. Eur J Cancer Care (Engl) 2005;14:249–55. doi: 10.1111/j.1365-2354.2005.00565.x. [DOI] [PubMed] [Google Scholar]
- 33.Fisher CS, Martin-Dunlap T, Ruppel MB, Gao F, Atkins J, Margenthaler JA. Fear of recurrence and perceived survival benefit are primary motivators for choosing mastectomy over breast conservation therapy regardless of age. Ann Surg Oncol. 2012;19:3246–50. doi: 10.1245/s10434-012-2525-x. [DOI] [PubMed] [Google Scholar]
- 34.D’Agincourt Canning L. The effect of experiential knowledge on construction of risk perception in hereditary breast/ovarian cancer. J Genet Counsel. 2005;14:55–69. doi: 10.1007/s10897-005-1500-0. [DOI] [PubMed] [Google Scholar]
- 35.Etchegary H, Dicks E, Watkins K, Alani S, Dawson L. Decisions about prophylactic gynecological surgery: a qualitative study of the experience of female Lynch mutation carriers. Hered Cancer Clin Pract. 2015;13:10. doi: 10.1186/s13053-015-0031-4. [DOI] [PMC free article] [PubMed] [Google Scholar]