Abstract
Objective:
To determine the association of posttraumatic stress disorder (PTSD) symptoms following Hurricane Katrina with incident cardiovascular disease (CVD) events in older, hypertensive, community-dwelling adults, overall and stratified by age, sex and race.
Design:
Prospective cohort study.
Setting:
Southeastern Louisiana 12 to 24 months following Hurricane Katrina through February 2011.
Participants:
Community-dwelling older adults (n=2073) enrolled in the Cohort Study of Medication Adherence among Older Adults (CoSMO) with no known history of CVD events.
Measurements:
Posttraumatic stress disorder (PTSD) symptoms were assessed via telephone interview 12 to 24 months following Hurricane Katrina using the PTSD CheckList – Specific Version (PCL-S). The presence of PTSD symptoms was defined by scores ≥ 37. Incident CVD events (stroke, myocardial infarction, hospitalization for congestive heart failure, or CVD death) were identified and adjudicated over a median 3.8 year follow-up period.
Results:
Overall, 8.6% of participants screened positive for PTSD symptoms and 11.6% had an incident CVD event during follow-up. PTSD symptoms were associated with an adjusted hazard ratio (aHR) for CVD events of 1.7 (95% confidence interval [CI] 1.1, 2.6). The association was present among blacks (aHR 3.3, 95% CI 1.7, 6.3) but not whites (aHR 0.9, 95% CI 0.4, 1.9); the interaction of PTSD symptoms and race on CVD events was statistically significant.
Conclusions:
PTSD symptoms following Hurricane Katrina were associated with a higher risk of incident CVD in older adults with hypertension, with stronger association in blacks compared to whites.
Keywords: PTSD symptoms, cardiovascular events, race, sex, Hurricane Katrina, older adults
INTRODUCTION
Hurricane Katrina made landfall in southeastern Louisiana on August 29, 2005, resulting in over 1800 deaths across a disaster area of over 90,000 square miles including the New Orleans metropolitan area (1). Over one million residents were displaced, thousands of homes were destroyed, and entire neighborhoods were lost in the storm, making it one of the most expensive disasters in U.S. history (2). Louisiana’s healthcare safety net and broader public health system were similarly devastated (3). The prevalence of post-traumatic stress disorder (PTSD) in affected areas dramatically increased following the storm (4), and serial cross-sectional analyses have revealed a statistically significant increase in acute myocardial infarction admissions at a major New Orleans hospital in the subsequent six years (5). Longitudinal research on survivors of Hurricane Katrina has proven challenging due to the chaotic nature of the evacuation (6) and the broad dispersion of survivors following the storm (7).
PTSD is a common, debilitating anxiety disorder following exposure to a traumatic event that has been associated with poor health outcomes, particularly with respect to the cardiovascular system (8). Longitudinal studies among mostly white, male veterans with combat-related PTSD have consistently found that PTSD increases the risk of cardiovascular disease (CVD) and related events (9). However, given that risk factors for developing PTSD symptoms after exposure to trauma differ between military and civilian samples (10) and the mental health consequences of trauma vary for different people and depending on its source (11), these findings may not be generalizable to civilians with exposure to other sources of trauma.
Less is known about the association between PTSD symptoms and incident CVD among civilians exposed to natural disasters, and only a few studies have explored this association in samples from non-white (12) and female populations (13), though the risk of PTSD and CVD differ substantially by race and sex (8). Individuals exposed to natural disasters have an increased risk for cardiovascular events compared to those exposed to other sources of trauma (14,15). Hurricane Katrina survivors with PTSD, in particular, have shown evidence of abnormal heart rate variability responsiveness to trauma reminders associated with increased cardiovascular disease risk (16), though recent research found no significant association between PTSD and cardiovascular disease mortality and hospitalization among Katrina survivors with end stage renal disease (17). Data are limited on the association of PTSD symptoms following a natural disaster and incident CVD in older community dwelling women and men. Therefore, we tested whether PTSD symptoms due to Hurricane Katrina in the 12 to 24 months following the storm were associated with incident composite CVD events in a prospective cohort of older adults with established hypertension; we explored differences by age, sex and race.
METHODS
Study Sample and Design
The sample included in the present study was from the Cohort Study of Medication Adherence in Older Adults (CoSMO), a prospective cohort study of factors associated with antihypertensive medication adherence and CVD outcomes in elderly adults with established hypertension in southeastern Louisiana. The eligibility criteria, baseline characteristics, design, and response rates have previously been published (18). Briefly, adults with essential hypertension aged 65 years and older were selected randomly from a managed care organization (MCO). Other key inclusion criteria were having a pharmacy fill for antihypertensive medication in the previous year, being community dwelling, being able to understand and speak English, and not having cognitive impairment. A total of 2,194 participants completed the baseline survey 12 to 24 months after Hurricane Katrina, and were followed through February 2011 for CVD event incidence and mortality. The current analyses were restricted to participants who had pharmacy refill data and no hospitalizations (based on MCO utilization data) for stroke, myocardial infarction (MI), or congestive heart failure (CHF) in the year prior to the administration of the baseline survey. CoSMO was approved by the privacy board of the managed care organization and Ochsner Health System’s Institutional Review Board.
Data Collection Overview
Data were obtained through telephone surveys administered by trained interviewers, administrative databases of the MCO, vital records, and medical records based on a published conceptual model (18, 19).
Primary Independent Variable
The primary independent variable was PTSD symptoms. PTSD symptoms were assessed using the PTSD Checklist – Specific Version (PCL-S) screening tool (20) (the PCL 17 items can be accessed at https://www.ptsd.va.gov/professional/assessment/documents/APCLS.pdf; accessed 9-7-2018). For this study, the PCL-S assessed PTSD symptoms related to their exposure to Hurricane Katrina and its aftermath such as: “Please indicate how much you have been bothered by repeated, disturbing dreams of Hurricane Katrina and the aftermath of the storm in the last month?” Response options included not at all, a little bit, moderately, quite a bit, or extremely. The questionnaire consists of 17 items grouped into three sub-scales: intrusion/re-experiencing symptoms (5 items), avoidance symptoms (7 items), and hyperarousal symptoms (5 items). Each item is scored on a Likert-response scale ranging from 1 to 5, and the total score is the summation of all 17 scored items (possible range 17-85). The PCL has been previously administered by telephone (21) and has high sensitivity for detecting PTSD compared to structured interviews (22). A higher score indicates a higher likelihood of PTSD and severity of PTSD symptoms. The optimal PCL cut-point varies according to clinical setting and sample demographics, and a cut-point of 37 has been identified as optimal for identifying PTSD symptoms in older, community-dwelling adults (23). As such, a PCL score ≥ 37 was used to identify the presence of PTSD symptoms in the current study.
Outcome
The primary outcome was a composite CVD endpoint including CVD death and nonfatal hospitalization for stroke, myocardial infarction (MI), or congestive heart failure (CHF) and has been previously described (24). Briefly, deaths were identified using the Social Security Death Index and cross-referencing with administrative databases and obituaries. Death certificates were obtained from local health departments and the cause of death was categorized as CVD or non-CVD-related. Medical record review was used to corroborate causes of death when possible. Hospitalization information was obtained via review of administrative databases, medical records, and physician adjudication. The following International Classification of Diseases, Ninth Revision (ICD9) codes were used over the follow-up period to search administrative databases and medical records for stroke: 430.xx, 431.xx, 432.xx, 433.xx, 434.xx; MI: 410.xx (except 410.x2); and CHF: 402.xl, 428.xx. Each CVD event was recorded on a standardized form by a trained research nurse (25). All outcomes were adjudicated as previously described (24). Participants were followed until their first CVD event or until the end of the follow up period on February 28, 2011.
Socio-demographic, Healthcare, Psychosocial, Lifestyle, Clinical (18), and Hurricane-related Variables
Socio-demographic, healthcare, psychosocial, clinical, and hurricane-related factors were collected from participants’ surveys, medical records, and administrative and claims databases of the managed care organization.
Socio-demographic variables assessed during the baseline telephone interview included age (75 years and over versus 65 years to under 75 years), sex (male versus female), race (black versus white), marital status, and education.
Healthcare variables assessed during the baseline telephone interview included satisfaction with healthcare overall, with healthcare communication, and with healthcare access (26); number of visits to a primary care provider in the previous year; and reduced antihypertensive medications due to cost.
Psychosocial variables assessed during the baseline telephone interview included depressive symptoms, stress, social support, and coping. Depressive symptoms were assessed with the 20-item Center for Epidemiologic Studies Depression Scale (27). Stress was assessed using the Perceived Stress Scale (PSS) (28). Social support was assessed using the Medical Outcomes Study (MOS) social support survey (29). Coping was assessed with seven items from the 12-item John Henry Active Coping scale (30).
Lifestyle variables collected during the baseline telephone interview included self-reported height, weight, current or former smoking status, number of alcoholic drinks consumed per week, and use of lifestyle modifications for blood pressure control (exercise, salt reduction, fruit and vegetable consumption) (18). Body mass index was calculated using self-reported data and the formula weight (kg)/height (m)2.
Clinical variables included antihypertensive medication adherence, blood pressure, comorbidities, and number of antihypertensive medication classes filled. Antihypertensive medication adherence was measured using pharmacy refill data from administrative claims to calculate the prescription-based proportion of days covered (PDC) (31). Blood pressure readings were obtained from medical records. Uncontrolled blood pressure was defined as average systolic blood pressure ≥140 mmHg or average diastolic blood pressure ≥90 mmHg over the two most recent readings relevant to the survey. Claims data were used to determine the Charlson Comorbidity Index (CCI) and number of classes of antihypertensive medication prescriptions filled by each participant.
Hurricane-related factors were assessed during the baseline telephone interview. The ZIP code reported by each participant for his/her residence before Hurricane Katrina was used to categorize participants as residing in high or low affected areas. High-affected areas included parishes (counties) in the greater New Orleans area (i.e., Orleans parish and four adjacent parishes); the remaining parishes were categorized as low-affected. The extent of home damage was assessed using a single item and dichotomized as extensive (>25%) versus less extensive (≥ 25%). Additionally, participants reported whether a friend or family member died within one month of Hurricane Katrina, whether they evacuated prior to the hurricane, and whether they were currently residing in the same home as before the hurricane.
Statistical Analysis
Participant characteristics were calculated overall and by PTSD symptom status using the cut-point of ≥ 37 or < 37 on the PCL. The statistical significance of differences in participant characteristics by PTSD symptom status were assessed using Pearson’s chi-square tests of independence. The statistical significance of differences in mean PCL scores among white and black participants were assessed with Welch’s two-sample t-test. Cumulative incidence of CVD events by PTSD symptom status was calculated via the Kaplan-Meier method. Hazard ratios (HR) and 95% confidence intervals (CI) for CVD events associated with PTSD symptom status were estimated using progressively adjusted Cox proportional hazard models. The proportional hazards assumption was assessed by calculating both scaled and unscaled Schoenfeld residuals (all covariates and the global test were non-significant) as well as inspecting complementary plots. The initial model adjusted for age, sex, race, marital status, and education. Subsequent models adjusted for blood pressure control, Charlson Comorbidity Index, number of antihypertensive medication classes, overall dissatisfaction with healthcare, reduced antihypertensive medications due to cost, number of visits to a primary care physician in the past year, pharmacy refill medication adherence (PDC), depressive symptoms, coping, smoking status, alcohol intake, body mass index, healthy lifestyle behaviors for blood pressure control, living in an area that was highly affected by Hurricane Katrina, extensive home damage, experienced the death of a family member or friend after the hurricane, evacuation prior to the hurricane, and did not return to the same home after the hurricane. All variables that were statistically significantly associated with CVD events in bivariate analyses were included in the Cox proportional hazards model with the exceptions of satisfaction with healthcare access and satisfaction with healthcare communication, which were excluded based on co-linearity with overall satisfaction with healthcare. Smoking status, alcohol intake, body mass index, and healthy lifestyle behaviors were not statistically significantly associated with CVD events in bivariate models but were included to maintain consistency with a previous analysis examining risk factors for cardiovascular events in the CoSMO cohort (24). Age-, race- and sex-stratified subgroup analyses were performed and effect modification was tested by including a PTSD-by-race, PTSD-by-sex, or PTSD-by-age interaction term in the fully adjusted model that included the overall sample. In sensitivity analysis, overall and age-, sex-, and race-stratified HR for composite CVD associated with PTSD were modeled using an alternate cut point (PCL ≥ 44). This cut-point is a commonly used cut point in the general population (7,31). Given the relatively low frequency of occurrence of missing data, a complete case analysis was performed. All analyses were performed using R 3.3.2 (R Core Team).
RESULTS
Baseline Characteristics
Of the 2,194 participants in the CoSMO cohort, 57 were excluded due to hospitalization related to a CVD event in the year prior to the baseline survey. There were 62 participants excluded due to missing pharmacy refill data (24). An additional two participants were excluded from the current analysis due to missing PCL data. Those excluded from the analysis were more likely than those included in the analysis to be male, to have low hypertension knowledge, to have a comorbidity score ≥2, to take three or more classes of antihypertensive medications, to have visited their healthcare provider six or more times in the last year, and to ever have smoked; they were less likely to have evacuated prior to Hurricane Katrina. At baseline, the mean age of the 2,073 participants included in the analyses was 75 years (standard deviation, 5.6), 59.8% were women, 30.3% were black, and 57.0% were married (Table 1). Over a median follow-up of 3.8 years, 240 (11.6%) participants had a total of 335 CVD events including 73 (21.8% of all events) CVD deaths, 48 (14.3%) strokes, 85 (25.4%) MIs, and 129 (38.5%) CHF hospitalizations.
Table 1:
Baseline Characteristics of Participants according to PCL Score
| Overall (n=2073) |
PCL < 37 (n=1895) |
PCL ≥ 37 (n=178) |
p-value † | |
|---|---|---|---|---|
| Socio-Demographics | ||||
| Age ≥ 75 | 1010 (48.7) | 932 (49.2) | 78 (43.8) | 0.17 |
| Female | 1239 (59.8) | 1109 (58.5) | 130 (73.0) | <0.001 |
| Black | 629 (30.3) | 539 (28.4) | 90 (50.6) | <0.001 |
| Married | 1181 (57.0) | 1088 (57.4) | 93 (52.2) | 0.18 |
| High school education or greatera | 1651 (79.7) | 1522 (80.4) | 129 (72.5) | 0.01 |
| Healthcare Variables | ||||
| Uncontrolled blood pressureb | 661 (34.0) | 604 (33.9) | 57 (35.4) | 0.70 |
| Low hypertension knowledge | 656 (31.6) | 580 (30.6) | 76 (42.7) | 0.001 |
| Hypertension duration ≥10 yearsc | 1299 (62.9) | 1190 (63.0) | 109 (61.6) | 0.70 |
| Charlson Comorbidity Index ≥ 2 | 1002 (48.3) | 915 (48.3) | 87 (48.9) | 0.88 |
| Body Mass Index ≥ 25 kg/m2 d | 1591 (76.8) | 1437 (75.9) | 154 (86.5) | 0.001 |
| ≥ 3 classes of antihypertensive medications | 900 (43.4) | 826 (43.6) | 74 (41.6) | 0.60 |
| Low pharmacy refill medication adherence (PDC) | 604 (29.1) | 533 (28.1) | 71 (39.9) | 0.001 |
| Not satisfied with overall healthcared | 96 (4.6) | 75 (4.0) | 21 (11.9) | <0.001 |
| Not satisfied with healthcare communicatione | 218 (10.5) | 185 (9.8) | 33 (18.5) | <0.001 |
| Not satisfied with healthcare access | 93 (4.5) | 72 (3.8) | 21 (11.8) | <0.001 |
| Reduced antihypertensive medications due to costa | 75 (3.6) | 62 (3.3) | 13 (7.3) | 0.006 |
| ≥ 6 visits to primary care physician in past yearf | 456 (22.1) | 405 (21.4) | 51 (28.7) | 0.03 |
| Home blood pressure monitoring | 1034 (49.9) | 954 (50.3) | 80 (44.9) | 0.17 |
| Psychosocial Variables | ||||
| Depressive symptoms | 267 (12.9) | 180 (9.5) | 87 (48.9) | <0.001 |
| High stress | 698 (33.7) | 566 (29.9) | 132 (74.2) | <0.001 |
| Low social support | 701 (33.8) | 617 (32.6) | 84 (47.2) | <0.001 |
| Low copinga | 981 (47.3) | 879 (46.4) | 102 (57.3) | 0.005 |
| Lifestyle Variables | ||||
| Current or former smokerg | 1034 (50.3) | 958 (50.9) | 76 (43.4) | 0.06 |
| ≥ 2 drinks a weekh | 440 (21.3) | 407 (21.6) | 33 (18.6) | 0.35 |
| ≥ 2 lifestyle modifications | 1696 (81.8) | 1539 (81.2) | 157 (88.2) | 0.02 |
| Hurricane Katrina Variables | ||||
| Lived in highly affected areal | 1458 (70.6) | 1309 (69.4) | 149 (84.2) | <0.001 |
| Damage to >25% of residencem | 746 (36.4) | 621 (33.1) | 125 (72.3) | <0.001 |
| Friend or family member died within one monthn | 379 (18.5) | 318 (17.0) | 61 (34.9) | <0.001 |
| Evacuated prior to hurricaneo | 1489 (72.5) | 1340 (71.4) | 149 (83.7) | <0.001 |
| Did not return to same home | 392 (18.9) | 326 (17.2) | 66 (37.1) | <0.001 |
PCL – PTSD CheckList - Specific
PTSD – Posttraumatic Stress Disorder; PDC – proportion of days covered;
p-values from Pearson’s χ2 tests of independence, df=1 for all
n=1 missing;
n=131 missing;
n=8 missing;
n=2 missing;
n=4 missing;
n=6 missing;
n=16 missing;
n=7 missing;
n=9 missing;
n=24 missing;
n=23 missing;
n=19 missing
The point prevalence of PTSD symptoms (PCL ≥ 37) 12 to 24 months following Hurricane Katrina was 8.6%. Participants with PTSD symptoms were more likely to be female, be black, have less than a high school education, have low hypertension knowledge, have low pharmacy fill medication adherence, have a body mass index (BMI) ≥ 25 kg/m2, report low satisfaction with their overall healthcare, communication with their healthcare provider, and access to care, have reduced antihypertensive medication use due to cost, have visited their primary care provider six or more times in the year prior to baseline, have depressive symptoms, have high stress, have low social support, have low coping skills, and use two or more lifestyle modifications to reduce blood pressure. Those with PTSD symptoms were also more likely to have lived in an area highly affected by Hurricane Katrina, to have extensive damage to >25% of their respective homes, to have a friend or family member who died within one month of the hurricane, to have evacuated prior to the hurricane, and not to have returned to the same home they were living in prior to the hurricane (Table 1). Black participants had a statistically significantly higher mean PCL score than white participants: 26.7 ± 10.3 versus 22.7 ± 7.5 (t = −8.92, df = 936.7, p<0.001). Black versus white participants were less likely to report living in a high affected area prior to the storm (66.4% versus 72.5%, Pearson’s χ = 7.8, df = 1, p = 0.005) and evacuating prior to the hurricane (68.6% versus 74.2%, Pearson’s χ = 6.7 df = 1, p = 0.010); but more likely to report having extensive damage to home (55.9% versus 28.0%, Pearson’s χ2 = 145.1, df = 1, p<0.001), having a family member or friend who died within one month of the hurricane (26.5% versus 15.1%, Pearson’s χ2 = 37.5, df = 1, p <0.001), and not having returned to the same home they were living in prior to the hurricane (25.0% versus 16.3%, Pearson’s χ2 = 21.6, df = 1, p<.001).
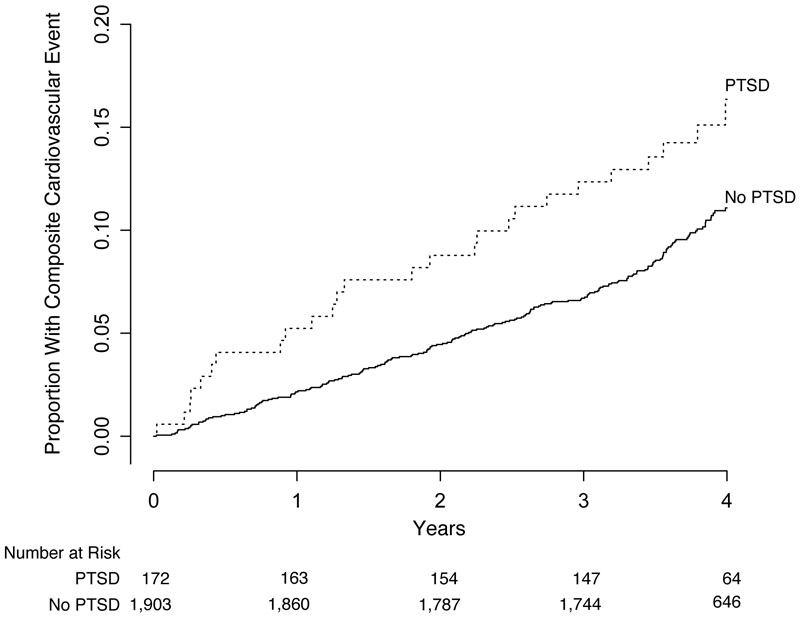
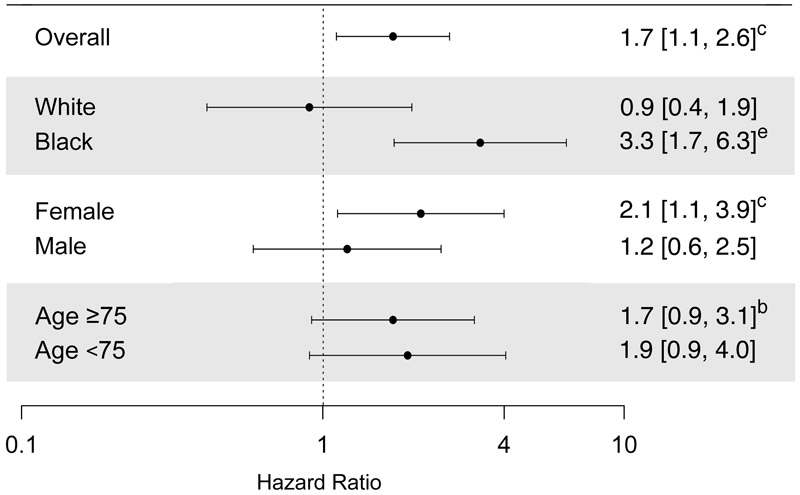
The proportion of the sample experiencing a CVD event during follow-up was 18.0% and 11.0% among those with and without PTSD symptoms, respectively (Figure 1). Compared to those without PTSD symptoms, the adjusted HR (aHR) for the CVD outcome associated with PTSD symptoms was 1.7 (95% CI 1.1, 2.6, Wald χ2 = 4.8, df = 1, p = 0.03) (Figure 2, Table 2, full model results presented in Table S1). The association between PTSD symptoms and the CVD outcome showed a statistically significant interaction by race (Wald χ2 = 11.2, df = 1, p = 0.001), but not sex (Wald χ2 = 1.4, df = 1, p = 0.24) or age (Wald χ2 = 0.4, df = l,p = 0.51) (Figure 2, Table 2, full model results presented in Table S2). Among blacks, the aHR for the CVD outcome associated with PTSD symptoms was 3.3 (95% CI 1.7, 6.3, Wald χ2 = 12.3, df = 1, p<.001). Among whites, the aHR was 0.9 (95% CI 0.4, 1.9, Wald χ2 = 0. 1, df = 1, p = 0.78).
Figure 1: Cumulative Incidence of Cardiovascular Disease by PTSD Symptoms at Baseline (Primary Analysis).
Log-Rank test p-value = 0.006
Analysis performed with a PTSD cut-point of ≥ 37 on PCL.
Figure 2: Adjusted Hazard Ratiosa for Incident Cardiovascular Disease Events Associated with PTSD Symptoms (Primary Analysis).
aWald χ2, df=1
bp<0.1, cp<0.05, dp<0.01, ep<0.001
All analyses performed with a PTSD cut-point of ≥ 37 on PCL and adjusted for age, sex, race, marital status, education, blood pressure control, Charlson Comorbidity Index, number of antihypertensive medication classes, satisfaction with healthcare, reduced antihypertensive medications due to cost, number of visits to primary care physician in the past year, medication adherence (pharmacy fill), depressive symptoms, coping, smoking status, alcohol intake, body mass index, healthy lifestyles for blood pressure control (fruit and vegetable intake, exercise, and sodium reduction), living in an area highly affected by Hurricane Katrina, damage to >25% of residence, having a friend or family member who died within one month of hurricane, evacuated prior to hurricane, and did not return to same home after hurricane
Table 2:
Adjusted Hazard Ratios for Incident Cardiovascular Disease associated with Posttraumatic Stress Disorder Symptoms
| n (%) with CVD outcome |
unadjusted HRa (95% CI) |
Model 1 aHRa (95% CI) |
Model 2 aHRa (95% CI) |
Model 3 aHRa (95% CI) |
Model 4 aHRa (95% CI) |
Model 5 aHRa (95% CI) |
|
|---|---|---|---|---|---|---|---|
| Overall | 240(11.6) | ||||||
| n | 2073 | 2072 | 1934 | 1933 | 1910 | 1845 | |
| All Participants | |||||||
| PCL ≥ 37 | 32 (18.0) | 1.7 (1.2, 2.5)** | 1.9 (1.3, 2.8)*** | 1.6 (1.1, 2.4)* | 1.6 (1.0, 2.5)* | 1.6 (1.0, 2.5)* | 1.7(1.1, 2.6)* |
| PCL < 37 | 208 (11.0) | reference | reference | reference | reference | reference | reference |
| Race Stratification | |||||||
| Whites | |||||||
| PCL ≥37 | 12 (13.6) | 1.1 (0.6, 1.9) | 1.2 (0.6, 2.1) | 0.9 (0.5, 1.7) | 0.9 (0.4, 1.8) | 0.9 (0.4, 1.8) | 0.9 (0.4, 1.9) |
| PCL < 37 | 169 (12.5) | reference | reference | reference | reference | reference | reference |
| Blacks | |||||||
| PCL ≥37 | 20 (22.2) | 3.4 (2.0, 5.8)*** | 3.4 (2.0, 5.8)*** | 3.4 (1.9, 6.1)*** | 3.4 (1.8, 6.3)*** | 3.5 (1.9, 6.7)*** | 3.3 (1.7, 6.3)*** |
| PCL < 37 | 39 (7.2) | reference | reference | reference | reference | reference | reference |
| Sex Stratification | |||||||
| Women | |||||||
| PCL ≥ 37 | 20 (15.4) | 1.8 (1.1, 3.0)* | 1.9 (1.2, 3.1)** | 1.8 (1.0, 3.0)* | 1.7 (1.0, 3.1)Λ | 1.70(0.9,3.1)Λ | 2.1 (1.1, 3.9)* |
| PCL < 37 | 98 (8.9) | reference | reference | reference | reference | reference | reference |
| Men | |||||||
| PCL ≥ 37 | 12 (25.0) | 1.8 (1.0, 3.2)Λ | 1.9 (1.0, 3.4)* | 1.4 (0.7, 2.7) | 1.4 (0.7, 2.9) | 1.4 (0.7, 2.8) | 1.2 (0.6, 2.5) |
| PCL < 37 | 110 (14.0) | reference | reference | reference | reference | reference | reference |
| Age Stratification | |||||||
| Age ≥75 years | |||||||
| PCL ≥37 | 17 (21.8) | 1.6 (1.0, 2.7)Λ | 1.8 (1.1, 2.9)* | 1.7 (1.0, 2.9)Λ | 1.6 (0.9, 2.9) | 1.6 (0.9, 2.9) | 1.7 (0.9, 3.1)Λ |
| PCL < 37 | 132 (14.2) | reference | reference | reference | reference | reference | reference |
| Age < 75 years | |||||||
| PCL ≥ 37 | 15 (15.0) | 1.9 (1.1, 3.4)* | 2.2 (1.2, 3.8)** | 1.6 (0.9, 3.0) | 1.9 (0.9, 3.7)Λ | 1.8 (0.9, 3.5) | 1.9 (0.9, 4.0) |
| PCL < 37 | 76 (7.9) | reference | reference | reference | reference | reference | reference |
p<0.10,
p<0.05,
p<0.01,
p<0.001
Waid χ2, df=1 for all
Model 1 adjusted for age, sex, race, marital status, and education
Model 2 adjusted for Model 1 variables plus uncontrolled blood pressure, Charlson Comorbidity Index, number of antihypertensive medication classes, satisfaction with healthcare, reduced antihypertensive medications due to cost, number of visits to primary care physician in the past year, and medication adherence (pharmacy fill) Model 3 adjusted for Model 2 variables plus depressive symptoms and coping
Model 4 adjusted for Model 3 variables plus smoking status, alcohol intake, body mass index, and healthy lifestyles for blood pressure control (fruit and vegetable intake, exercise, and sodium reduction)
Model 5 adjusted for Model 4 variables plus living in an area highly affected by Hurricane Katrina, damage to >25% of residence, having a friend or family member who died within one month of hurricane, evacuated prior to hurricane, and did not return to same home after hurricane
CVD – Cardiovascular disease; PTSD – Posttraumatic Stress Disorder; HR – Hazard Ratio; CI – confidence interval; PCL – PTSD Checklist – Specific
Sensitivity Analysis
The point prevalence of PTSD symptoms 12 to 24 months following Hurricane Katrina using the alternate cut-point on the PCL was 4.4%. Compared to those without PTSD symptoms, the aHR for the incident CVD outcome associated with PTSD symptoms was 3.4 (95% CI 2.0, 5.7, Wald χ2 = 21.7 df = 1, p<.001) (Figure S1, Table S3). The aHR was 4.8 (95% CI 2.2, 10.7, Wald χ2 = 15.0, df = 1, p<.001) among blacks and 2.3 (95% CI 1.0, 5.3, Wald χ2 = 4.0, df = 1, p = 0.046) among whites. There were no statistically significant interactions by race (Wald χ2 = 3.1,df = 1,p = 0.08), sex (Wald χ2 = 0.0, df = 1, p = 0.99) or age (Wald χ2 = 0.7, df = 1, p = 0.41).
DISCUSSION
In this study of older, community-dwelling adults with established hypertension, participants with PTSD symptoms had a 70% higher risk of incident CVD event than their counterparts without PTSD symptoms after controlling for sociodemographic, healthcare, psychosocial, lifestyle, clinical, and Hurricane Katrina-related variables. The results were consistent in the sensitivity analysis using a higher cut-point to define PTSD symptoms. The interaction of PTSD symptoms and race was statistically significant in the primary analysis: blacks with PTSD symptoms were 3.3 times more likely to have an incident CVD event than blacks without PTSD symptoms while the association of PTSD symptoms with incident CVD event among whites was not significant (however, it was significant in the sensitivity analysis). The results were consistent in men and women and in the younger-old and older-old age groups.
These findings are consistent with previous research suggesting PTSD is an independent risk factor for cardiovascular disease among older adults (9,32,33) and extend the findings to community-dwellers with established hypertension following a natural disaster. Studies have shown that both the prevalence of PTSD (34) and incidence of cardiovascular events (14,15) increase following natural disasters. This pattern held true for areas affected by Hurricane Katrina: serial cross sectional analyses at one New Orleans hospital showed a persistent, threefold increase in acute myocardial infarction admissions (5). PTSD prevalence increased significantly in the years following the storm (35). The current findings suggest PTSD symptoms up to 24 months following Hurricane Katrina may partially explain the increased incidence of CVD and related events following this natural disaster.
Trends in PTSD symptoms following Hurricane Katrina differed from those in other natural disasters. Normally, PTSD incidence peaks immediately after disasters, declines rapidly in the first year, and stabilizes by the end of the second (34). Following Hurricane Katrina, however, PTSD prevalence continued to increase significantly for two years (4). This distinct pattern has been attributed to less severe but chronic stressors indirectly linked to the hurricane – financial and interpersonal loss, destruction of social and community resources – that “erode the resistance resources that would otherwise promote recovery” (35). The assessment of PTSD in the current study occurred between 12 to 24 months following the hurricane. The point prevalence of PTSD symptoms (PCL ≥ 37) 12 to 24 months following Hurricane Katrina in our study cohort of older adults was 8.6%, less than estimates between 14.9%-20.9% for adults of any age living in areas affected by Hurricane Katrina five months to 1.6 years following the storm, but consistent with findings that older adults were less likely to develop PTSD than younger individuals (35). Older adults have been shown to exhibit fewer PTSD symptoms than younger adults following other natural disasters and traumatic experiences as well (35,36,37).
The current finding that the observed association between PTSD symptoms and incident CVD events was stronger among blacks is consistent with a cross-sectional study of chronically depressed elderly combat veterans (12). Cooper and colleagues found that comorbid PTSD was associated with a significantly higher odds of coronary artery disease diagnosis among blacks, significantly lower odds among whites and Hispanics, and no significant difference among Asians (12). Using longitudinal data and after controlling for depressive symptoms, we also found that PTSD symptoms were more strongly associated with subsequent CVD events among older blacks compared to older whites.
A number of factors may contribute to the observed effect modification by race. Controlling for uncontrolled blood pressure and low medication adherence attenuated, but did not eliminate, the strength of the PTSD-CVD association in the present study in the primary analysis. There was no attenuation in the stratified analysis when the same variables were entered into the model. Prior research indicates that blacks may be more susceptible to the chronic cardiovascular effects of PTSD because they are less likely to receive indicated treatment for the disorder (12, 38). Minorities are also less likely than whites to seek and receive indicated mental health care in the U.S., including for PTSD (39). Compared to whites, blacks may have less access to community mental health services and receive lower quality care (40). While the present study lacks income data, all participants were insured and received care through a single managed care organization in southeastern Louisiana, and a number of variables related to quality of and access to healthcare were controlled for in the analysis. As such, it is unlikely that the observed difference is due to confounding by economic status or access to primary care. Data on mental health care utilization were not captured in CoSMO, therefore it is unknown whether blacks in our cohort were less likely to seek or receive mental health care for PTSD symptoms than whites and whether treatment was associated with lower CVD risk.
Although not captured as part of the current study, racial differences in lifetime trauma load may also contribute to the stronger PTSD-CVD association among black versus white participants. Blacks are more likely to experience traumatic events during childhood (39), which increases risk of developing anxiety disorders and associated health issues later in life (41). Chronic stress burden due to racial discrimination has also been associated with PTSD (42,43) and cardiovascular health (44–46). Further work is needed to explore lifetime trauma load as this was beyond the scope of the current study. While, compared to whites, blacks in the Gulf South were significantly less likely to evacuate before the storm, be able to return home if they did evacuate, report reliable emotional support from friends and family, and maintain their employment (47), inclusion of Hurricane Katrina-related variables (extensive home damage, living in a highly affected area, experiencing a death of a family member or friend within one month after the hurricane, evacuation prior to the hurricane, and not currently living in the same residence as before the hurricane) did not substantively change the association between PTSD symptoms and CVD risk in the overall or race-stratified analyses among this sample. Further research is needed to better delineate the factors contributing to the observed racial difference in the association between PTSD symptoms and incident CVD events, the mechanism linking PTSD to incident CVD, and whether screening for PTSD coupled with successful treatment can reduce overall cardiovascular risk.
Study Limitations and Strengths:
The findings should be considered in the context of study limitations. First, the findings are based on a sample of insured hypertensive adults, age 65 and older, residing in southeastern Louisiana and may not be generalizable to other populations or areas of the United States. Thirty-nine percent of the individuals >65 years of age randomly selected from the administrative databases of the MCO and identified as eligible enrolled in the COSMO study; those not enrolled either refused to participate or had invalid contact information, likely resulting from displacement following Hurricane Katrina. Those who refused to participate as well as those who were unable to be reached were more likely to be male, white, and older compared with those who participated in the study (18); therefore, there is a possibility of selection bias. In addition, given the inclusion criteria, the results may not reflect all elderly (e.g., the frail elderly, cognitively impaired and those with previous CVD events). While we had high recapture rate for follow up surveys of 93.6% (48), it is possible that loss to follow up may impact the results. Second, although the PCL is validated and widely used, it is a self-reported screening tool that does not directly diagnose PTSD, is susceptible to social desirability and recall biases, and was assessed only once during the CoSMO study. While the PCL asked about symptoms related to Hurricane Katrina, it is possible that PTSD symptoms related to other sources of trauma are reflected in participants’ responses. Third, the use of ICD-9 codes to identify CVD events is subject to misclassification bias; to minimize this risk, CVD events were confirmed against medical records and physician-adjudicated. Given that all participants were members of the same MCO, it is unlikely that the rate of unaccounted for CVD events prior to baseline differed between those with and without Hurricane Katrina-related PTSD symptoms, however we cannot rule out this possibility. Although all variables were selected based on a published conceptual model, there were a number of variables screened for inclusion in the final models with a possibility of a Type 1 error; therefore, the p values along with the confidence intervals are included in the tables. While adjusting for Hurricane Katrina-related variables did not substantively change the associations between PTSD symptoms and CVD risk in the overall and race-stratified analyses, it is possible that there is residual confounding, based on unknown variables, geographic burden or vulnerability to the effects of Hurricane Katrina. Lastly, while our analysis showed significant effect modification by race, the sample sizes for subgroup analyses were relatively small. Larger longitudinal studies designed specifically to explore age, race and sex differences are needed.
Our study has many strengths, including its longitudinal design, ability to capture incident cardiovascular events, relatively high prevalence of PTSD symptoms, and relatively large sample size with diverse sociodemographic and risk factors. We collected comprehensive data from patient surveys, administrative databases, and medical records which allowed us to control for a number of potential confounders including depressive symptoms, medication adherence, and hurricane-related factors. Confounding by access and insurance status, in particular, was reduced by including only community-dwelling, hypertensive, older adults in a managed Medicare sample.
CONCLUSIONS
PTSD symptoms 12 to 24 months following Hurricane Katrina were associated with incident CVD among elderly, community-dwelling adults with hypertension. The association was modified by race, with a stronger association between PTSD symptoms and subsequent CVD among blacks compared to whites. Clinicians and policymakers should be aware of the potential long-term effects of psychological distress in older adults resulting from natural disasters and the increased risk of adverse clinical outcomes associated with PTSD symptoms in such patients.
Supplementary Material
Highlights.
Few studies have examined the longitudinal association between PTSD symptoms and incident CVD in older community-dwelling adults exposed to natural disasters.
Overall, PTSD symptoms following Hurricane Katrina were associated with higher risk of incident cardiovascular disease in this cohort of older adults with hypertension.
The association between PTSD symptoms and incident CVD was significantly stronger among black versus white participants; results were similar among men and women.
Acknowledgements
Conflicts of Interest and Source of Funding:
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number TL1 TR001418 (Lenane – TL1 Trainee). This work was also supported by the National Institute on Aging (Grant Number R01 AG022536, Krousel-Wood – Principal Investigator). The authors have additional sources of support from the National Institutes of Health provided through K12 HD043451 (Krousel-Wood – Principal Investigator, Peacock – Data Analyst), U54 GM104940 (Krousel-Wood – Pilot Project Co-Director), UL1 TR001417 (Krousel-Wood – Site Lead, TL1 Co-Director), and P20 GM109036 (Krousel-Wood – Co-Investigator). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Dr. Paul Muntner has consulted for Amgen for work not related to this manuscript. There are no other conflicts to report for any other author related to this submitted work. All authors have read and approved the submission of the manuscript.
Footnotes
Previous Presentations:
Aspects of this work were presented as a poster, Posttraumatic Stress Disorder Associated with Hurricane Katrina Predicts Cardiovascular Disease Events among Elderly Adults Poster, at the Translational Science 2017 conference in Washington, DC on April 19, 2017.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Knabb RD, Rhome JR, Brown DP. Tropical Cyclone Report, Hurricane Katrina.; 2011. http://www.nhc.noaa.gov/data/tcr/AL122005_Katrina.pdf. [Google Scholar]
- 2.Hallegatte S An Adaptive Regional Input-Output Model and its Application to the Assessment of the Economic Cost of Katrina. Risk Anal. 2008;28(3):779–799. [DOI] [PubMed] [Google Scholar]
- 3.Rudowitz R, Rowland D, Shartzer A. Health care in New Orleans before and after Hurricane Katrina. Health Aff. 2006;25(5):w393–406. [DOI] [PubMed] [Google Scholar]
- 4.Galea S, Brewin CR, Gruber M, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64(12):1427–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peters MN, Moscona JC, Katz MJ, et al. Natural Disasters and Myocardial Infarction: The Six Years After Hurricane Katrina. Mayo Clin Proc. 2014;89(4):472–477. [DOI] [PubMed] [Google Scholar]
- 6.Mills MA, Edmondson D, Park CL. Trauma and stress response among Hurricane Katrina evacuees. Am JPublic Health. 2007;97 Suppl 1:S116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cukor J, Wyka K, Jayasinghe N, et al. Prevalence and predictors of posttraumatic stress symptoms in utility workers deployed to the World Trade Center following the attacks of September 11, 2001. Depress Anxiety. 2011;28(3):210–217. [DOI] [PubMed] [Google Scholar]
- 8.Edmondson D, Kronish IM, Shaffer JA, Falzon L, Burg MM. Posttraumatic stress disorder and risk for coronary heart disease: A meta-analytic review. Am Heart J. 2013;166(5):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beristianos MH, Yaffe K, Cohen B, Byers AL. PTSD and Risk of Incident Cardiovascular Disease in Aging Veterans. Am J Geriatr Psychiatry. 2016;24(3):192–200. [DOI] [PubMed] [Google Scholar]
- 10.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–766. [DOI] [PubMed] [Google Scholar]
- 11.Rubonis A V, Bickman L. Psychological impairment in the wake of disaster: the disaster-psychopathology relationship. Psychol Bull. 1991;109(3):384–399. [DOI] [PubMed] [Google Scholar]
- 12.Cooper DC, Trivedi RB, Nelson KM, et al. Post-traumatic Stress Disorder, Race/Ethnicity, and Coronary Artery Disease Among Older Patients with Depression. J Racial Ethn Heal Disparities. 2014;1(3):163–170. [Google Scholar]
- 13.Kubzansky LD, Koenen KC, Jones C, Eaton WW. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychol. 2009;28(1):125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kario K, McEwen Bruce S, Pickering Thomas G. Disasters and the Heart: a Review of the Effects of Earthquake-Induced Stress on Cardiovascular Disease. Hypertens Res. 2003;26(5):355–367. [DOI] [PubMed] [Google Scholar]
- 15.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB, Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group the MIDAS (MIDAS 24) S. The effect of Hurricane Sandy on cardiovascular events in New Jersey. J Am Heart Assoc. 2014;3(6):e001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tucker P, Pfefferbaum B, Jeon-Slaughter H, Khan Q, Garton T. Emotional Stress and Heart Rate Variability Measures Associated With Cardiovascular Risk in Relocated Katrina Survivors. Psychosom Med. 2012;74(2):160–168. [DOI] [PubMed] [Google Scholar]
- 17.Edmondson D, Gamboa C, Cohen A, et al. Association of posttraumatic stress disorder and depression with all-cause and cardiovascular disease mortality and hospitalization among hurricane katrina survivors with end-stage renal disease. Am J Public Health. 2013;103(4):e130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93(3):753–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. [DOI] [PubMed] [Google Scholar]
- 20.Weathers F, Litz B, Herman D, Huska J, & Keane T (October 1993). The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- 21.Ruggiero KJ, Rheingold AA, Resnick HS, Kilpatrick DG, Galea S. Comparison of two widely used PTSD-screening instruments: Implications for public mental health planning. J Trauma Stress. 2006; 19(5):699–707. [DOI] [PubMed] [Google Scholar]
- 22.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL). Behav Res Ther. 1996;34(8):669–673. [DOI] [PubMed] [Google Scholar]
- 23.Cook JM, Elhai ID, Areán PA. Psychometric properties of the PTSD Checklist with older primary care patients. J Trauma Stress. 2005;18(4):371–376. [DOI] [PubMed] [Google Scholar]
- 24.Krousel-Wood M, Holt E, Joyce C, et al. Differences in cardiovascular disease risk when antihypertensive medication adherence is assessed by pharmacy fill versus self-report: the Cohort Study of Medication Adherence among Older Adults (CoSMO). JHypertens. 2015;33(2):412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156(9):871–881. [DOI] [PubMed] [Google Scholar]
- 26.Davies AR and Ware JE, GHAA’s consumer satisfaction survey and user’s manual, Group Health Association of America, 1991. [Google Scholar]
- 27.Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behav Res Ther. 1997;35(4):373–380. [DOI] [PubMed] [Google Scholar]
- 28.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 29.Sherbourne CD, Stewart AL. The MOS social support survey. Soc SciMed. 1991;32(6):705–714. [DOI] [PubMed] [Google Scholar]
- 30.Fernander AF, Dura′N REF, Saab PG, Llabre MM, Schneiderman N. Assessing the Reliability and Validity of the John Henry Active Coping Scale in an Urban Sample of African Americans and white Americans. Ethn Health. 2003;8(2):147–161. [DOI] [PubMed] [Google Scholar]
- 31.Choudhry NK, Shrank WH, Levin RL, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15(7):457–464. [PMC free article] [PubMed] [Google Scholar]
- 32.McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD Checklist: A critical review. Clin Psychol Rev. 2010;30(8):976–987. [DOI] [PubMed] [Google Scholar]
- 33.Kubzansky LD, Koenen KC, Spiro A, et al. Prospective Study of Posttraumatic Stress Disorder Symptoms and Coronary Heart Disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64(1):109. [DOI] [PubMed] [Google Scholar]
- 34.Norris FH, Perilla JL, Riad JK, Kaniasty K, Lavizzo EA. Stability and change in stress, resources, and psychological distress following natural disaster: Findings from hurricane Andrew. Anxiety, Stress Coping. 1999;12(4):363–396. [DOI] [PubMed] [Google Scholar]
- 35.Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008;13(4):374–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Acierno R, Ruggiero KJ, Kilpatrick DG, Resnick HS, Galea S. Risk and Protective Factors for Psychopathology Among Older versus Younger Adults After the 2004 Florida Hurricanes. Am J Geriatr Psychiatry. 2006;14(12):1051–1059. [DOI] [PubMed] [Google Scholar]
- 37.Frueh BC, Grubaugh AL, Acierno R, Elhai JD, Cain G, Magruder KM. Age Differences in Posttraumatic Stress Disorder, Psychiatric Disorders, and Healthcare Service Use Among Veterans in Veterans Affairs Primary Care Clinics. Am J Geriatr Psychiatry. 2007;15(8):660–672. [DOI] [PubMed] [Google Scholar]
- 38.Spoont MR, Nelson DB, Murdoch M, et al. Are there racial/ethnic disparities in VA PTSD treatment retention? Depress Anxiety. 2015;32(6):415–425. [DOI] [PubMed] [Google Scholar]
- 39.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41(1):71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alegria M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59(11):1264–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49(12):1023–1039. [DOI] [PubMed] [Google Scholar]
- 42.Butts HF. The Black Mask of Humanity: Racial/Ethnic Discrimination and Post-Traumatic Stress Disorder. J Am Acad Psychiatry Law. 2002;30:336–339. [PubMed] [Google Scholar]
- 43.Chou T, Asnaani A, Hofmann SG. Perception of racial discrimination and psychopathology across three U.S. ethnic minority groups. Cultur Divers Ethnic Minor Psychol. 2012;18(1):74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lepore SJ, Revenson TA, Weinberger SL, et al. Effects of social stressors on cardiovascular reactivity in black and white women. Ann Behav Med. 2006;31(2):120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic Exposure to Everyday Discrimination and Coronary Artery Calcification in African-American Women: The SWAN Heart Study. Psychosom Med. 2006;68(3):362–368. [DOI] [PubMed] [Google Scholar]
- 46.Ayotte BJ, Hausmann LRM, Whittle J, Kressin NR. The relationship between perceived discrimination and coronary artery obstruction. Am Heart J. 2012;163(4):677–683. [DOI] [PubMed] [Google Scholar]
- 47.Elliott JR, Pais J. Race, class, and Hurricane Katrina: Social differences in human responses to disaster. Soc Sci Res. 2006;35(2):295–321. [Google Scholar]
- 48.Krousel-Wood M, Joyce C, Holt E, et al. Predictors of decline in medication adherence: results from the cohort study of medication adherence among older adults. Hypertens. 2011;58(5):804–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.