Abstract
Background
Because pediatric trauma-related mortality continue to decline, metrics assessing morbidity are needed to evaluate the impact of treatment after injury. Based of its value for assessing children with traumatic brain injuries and other critical illnesses, Functional Status Scale (FSS), a tool that measures function in six domains (communication, feeding, mental, motor, sensory and respiratory), was evaluated as an outcome measure for the overall population of injured children.
Methods
Children with at least one injury (Abbreviated Injury Scale [AIS] severity ≥1) surviving to discharge between December 2011 and April 2013 were identified in a previous study of intensive care unit admissions. Morbidity was defined as additional morbidity in any domain (domain FSS change ≥2) and additional overall morbidity (total FSS change ≥3 or ‘new domain morbidity’) between preinjury status and discharge. Associations between injury profiles and the development of morbidity were analyzed.
Results
We identified 553 injured children, with an average of 2.0 ± 1.9 injuries. New domain and overall morbidity were observed in 17.0% and 11.0% of patients, respectively. New domain morbidity was associated with an increasing number of body regions with an injury with AIS≥ 2 (P<0.001), with severe (AIS ≥ 4) head (P=0.04) and spine (P=0.01) injuries and with at moderately severe (AIS ≥ 2) lower extremity injuries (P=0.01). New domain morbidity was more common among patients with severe spine and lower extremity injuries (55.6% and 48.7%, respectively), with greatest impact in the motor domain (55.6% and 43.6%, respectively). New domain morbidity was associated with increasing ISS, number of moderately severe injuries and number of body regions with more than a moderately severe injury (P<0.001 for all).
Conclusions
Higher morbidity measured by the FSS is associated with increasing injury severity. These findings support the use of the FSS as a metric for assessing outcome after pediatric injury.
Keywords: Functional Status Scale, pediatric trauma, domain morbidity, critically ill children, pediatric critical care
BACKGROUND
Injuries are the third leading cause of disability-adjusted life years (DALY) among children and adolescents.1 Although the health burden of injury-related disability is significant, most pediatric trauma outcome studies have focused on mortality as the primary outcome measure.2 Mortality, however, is now uncommon (<2%) among children hospitalized after injury.3 Because the level of impairment after recovery may now best assess the long-term impact of pediatric injuries, several instruments have been used to assess outcomes other than mortality (PEDI, PedsQL, CHQ-PF28, OSCHI, Mgos, FIM and GOS-E Peds).4–7 These instruments have not had general applicability or gained widespread use for several reasons including (1) a focus on patients with specific injury types or in specific age groups (lack of extension among all injured children); (2) the use of time-consuming instead of brief outcome instruments (training and time required for administration); (3) evaluation at single sites (uncertain generalizability); (4) performance as part of a research protocol rather than in a “real world” setting (need for resources not available at many institutions); and (5) the lack of an organization championing its use (need for change motivation).8–9 Given the importance and frequency of acquired disability and infrequency of mortality, a need remains to develop generalizable methods for assessing functional outcome in multiple dimensions that can be performed as standard practice at any institution that treats injured children. In the absence of these methods, the ability to identify and address systemic factors that influence relevant outcomes after pediatric injury will remain limited.
The Functional Status Scale (FSS) was developed and validated as an age-independent, granular measure of functional status suitable for large-scale studies.10 FSS is practical for assessing hospitalized children because values can be obtained in less than five minutes from the medical record or from the patient’s health providers. The score is based on the concepts of activities of daily living and adaptive behavior and has been validated against the Adaptive Behavior Assessment Scale (ABAS)-II, a comprehensive norm-referenced assessment of adaptive skills.11 FSS assesses functioning in the domains of mental status, sensory function, communication, motor function, feeding and respiratory status. Status in each domain is classified as ‘normal’ to ‘very severe dysfunction,’ with total scores ranging from 6 (best) to 30 (worst). FSS has been found to be precise and reliable as a predictor of morbidity based on physiological profiles, with a three-point change in FSS representing significant “new morbidity.”12 Although FSS has been assessed as a metric for measuring functional status after pediatric traumatic brain injury,13 its value for assessing outcomes in children sustaining injuries in other body regions is not known.
We hypothesized that FSS has applicability as a tool for assessing acquired morbidity in children with injuries affecting different body regions. To test this hypothesis, we evaluated the association between severity of injury measured by the Abbreviated Injury Scale (AIS) and new morbidity measured using FSS. Establishing this association will provide support for using FSS as a measure of morbidity in comparison studies of pediatric trauma management and as a metric for benchmarking centers treating injured children.
METHODS
Study Design
A centralized IRB approved this study for all participating sites. We analyzed the functional outcomes of injured children admitted between December 2011 – April 2013 as part of a multicenter prospective study of 10,078 critically ill patients in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN). In this study, patients up to 18 years old admitted to the intensive care unit were randomly selected and stratified by hospital. Patients with vital signs incompatible with life for the first two hours after intensive care unit admission were excluded. Only the first intensive care unit admission during a hospitalization was included.12 We first identified 628 injured children in this cohort who survived to discharge using a disease category of ‘trauma’ during enrollment (22 [3.4%] injured children died during hospitalization). Among these patients, we excluded six with unavailable ICD-9 codes, two with a primary ICD-9 diagnosis code indicating late effects or complications of injury (905.0–909.9 or 958.0–958.9) and 19 with a diagnosis of a burn injury, identified by a diagnosis assigned at enrollment, primary ICD-9 diagnosis code or E-code indicating this injury type. For the remaining 601 children, we identified the AIS severity codes (a scale representing severity of injury: 1-minor, 2-moderate, 3-serious, 4-severe, 5-critical, 6-maximum) of each injury’s ICD-9 code and calculated each patient’s Injury Severity Score (ISS) using the ICDPIC (International Classification of Diseases Program for Injury Categorization) macro implemented in Stata®.14 Body regions associated with each injury were classified using the AIS coding system of nine regions. We excluded from the analysis 47 children whose maximum AIS severity in all body regions was 0 and one child with an injury that had an AIS severity of ‘maximum.’ Our analysis included 553 children who had at least one injury ICD-9 code (800.0–959.9) with an associated AIS severity from ‘minor’ (AIS severity=1) to ‘critical’ (AIS severity=5).
Data Analysis
The primary outcome for this study was a change of ≥2 in any FSS domain between pre-injury and hospital discharge status (‘new domain morbidity’). Secondary outcomes assessed included a change in total FSS of ≥3 (‘new morbidity’)15 between the pre-injury and discharge status. We represented overall injury severity in three ways: ISS, the number of injuries per patient with an AIS severity ≥2 (at least moderately severe injury) and the number of body regions affected by at least one injury AIS severity ≥2.16 We selected a threshold severity value of ‘2’ because injuries with a severity value of ‘1’ are minor injuries (e.g., superficial laceration) with a low likelihood of impact on outcome. In the development of a multivariable model, we considered the following covariates: age (categorized as <14 days, 14 days to <1 month, 1 month to <1 year, 1–17 years), gender, the highest severity value across all body regions and the number of body regions (including the ‘unspecified’ category) with at least one injury with AIS severity≥2 with the presence of at least one injury with AIS severity≥2 and the presence of at least one injury with AIS severity >4 in each body region considered separately. A forward selection approach was used, with the most significant of any potential variable improving predictive ability (P<0.05 by score test) entered at each step. Final model goodness of fit was assessed by the Hosmer-Lemeshow test and predictive ability assessed by the c-statistic which quantifies area under the ROC curve. All statistical analyses were conducted using SAS Version 9.4.
RESULTS
Most of the 553 injured children were male (n=331, 59.9%), with a median age of 5.7 years (Table 1). Most patients had either one or two injuries with AIS severity ≥2. Consistent with being treated in an intensive care unit (ICU), most patients (68.7%) were at least moderately injured as measured by ISS (>9). Patients had a median length of stay in the ICU of 1.5 days and in the hospital of 3 days (Table 1). Almost half of the 1,122 injuries with AIS severity ≥2 were head injuries (n=485, 43.2%) followed by injuries to the upper or lower extremity (n=211, 18.8%) and injuries to the abdomen (n=141, 12.6%) (Tables 1 and 2).
Table 1.
Summary Statistics
| Variable | |
|---|---|
| Age (years, median, IQR) | 5.7 (1.3 – 11.8) |
| Male (No., %) | 331 (59.9) |
| ISS score (No., %) | |
| 1–8 | 173 (31.3) |
| 9–15 | 189 (34.2) |
| 16–24 | 150 (27.1) |
| >24 | 41 (7.4) |
| No. of injuries/patient with severity≥2 (median, IQR) | 1 (1–2) |
| Injuries with AIS severity ≥2 | |
| Total | 1,122 |
| Head (No., %) | 485 (43.2) |
| Face (No., %) | 70 (6.2) |
| Neck (No., %) | 7 (0.6) |
| Thorax (No., %) | 121 (10.8) |
| Abdomen (No., %) | 141 (12.6) |
| Spine (No., %) | 81 (7.2) |
| Upper extremity (No., %) | 86 (7.7) |
| Lower extremity (No., %) | 125 (11.1) |
| Other/unspecified (No., %) | 6 (0.5) |
| Baseline FSS (median, IQR) | 6 (6–6) |
| Discharge FSS (median, IQR) | 6 (6–7) |
| Discharge FSS category (No., %) | |
| 6–7 (good) | 434 (78.5) |
| 8–9 (mildly abnormal) | 66 (11.9) |
| 10–15 (moderately abnormal) | 40 (7.2) |
| 16–21 (severely abnormal) | 9 (1.6) |
| >21 (very severely abnormal) | 4 (0.7) |
| New domain-related morbidity (≥2 in any domain) | 94 (17.0) |
| New morbidity (≥3 change from baseline) (No., %) | 61 (11.0) |
| Change in FSS from baseline (median, IQR) | 0 (0–1) |
| Intensive care unit length of stay (days, median and IQR) | 1.5 (0.8–2.9) |
| Hospital length of stay (days, median and IQR) | 3.0 (1.6–7.7) |
SD-standard deviation; No.-number; ISS-Injury Severity Scale; AIS-Abbreviated Injury Scale; IQR-interquartile range
Table 2.
Number of Injuries by Injury Severity for All Body Regions
| AIS Severity | |||||
|---|---|---|---|---|---|
| Body Region | 1 | 2 | 3 | 4 | 5 |
| Head | 19 | 160 | 202 | 121 | 2 |
| Face | 62 | 67 | 3 | 0 | 0 |
| Neck | 0 | 2 | 5 | 0 | 0 |
| Thorax | 10 | 22 | 91 | 8 | 0 |
| Abdomen | 21 | 90 | 34 | 15 | 2 |
| Spine | 12 | 59 | 10 | 8 | 4 |
| Upper extremity | 8 | 75 | 11 | 0 | 0 |
| Lower extremity | 11 | 74 | 50 | 1 | 0 |
| Unspecified | 267 | 6 | 0 | 0 | 0 |
AIS-Abbreviated Injury Scale
The functional status of most patients (n=536, 96.9%) was normal (FSS 6–7) before being injured. Seventeen patients had baseline impairment measured by FSS, 11 having mild impairment (FSS 8 or 9) and six having moderate impairment (FSS 10–15). Three patients with baseline mild impairment had new domain morbidity at discharge. The level of baseline impairment was not associated with the occurrence of either domain or overall new morbidity (P>0.05). Similar to findings observed in the entire cohort of ICU patients, baseline FSS in the cohort of injured patients was highly correlated with baseline values of the pediatric overall performance category (POPC) and pediatric cerebral performance category (PCPC) scales (P<0.001, Tables 3 and 4). Although most patients (n=434, 78.5%) returned to or remained with ‘good’ functional status at discharge (FSS 6 or 7), we observed higher functional impairment at discharge compared to pre-injury baseline status using domain and overall new morbidity (Table 1). Overall domain and overall new morbidity occurred in 17% and 11% of patients, respectively. We observed an inverse relationship between discharge functional status and injury severity, with new domain morbidity best discriminating change in functional status (Figure 1).
Table 3.
Baseline Functional Status Assessment According to Baseline POPC. Differences between FSS scores in each POPC interval were observed, with an FSS increase with each worsening POPC category (P<0.001 for Spearman correlation between FSS and POPC).
| Baseline POPC | # of patients | Mean (SD) | Range (width)-25th to 75th percentiles | Range (width)-10th to 90th percentiles | Range (width)-5th to 95th percentiles |
|---|---|---|---|---|---|
| 1-Good | 507 | 6.0 (0.1) | 6–6 (0) | 6–6 (0) | 6–6 (0) |
| 2-Mild disability | 38 | 6.9 (1.6) | 6–7 (1) | 6–9 (3) | 6–10 (4) |
| 3-Moderate disability | 5 | 8.8 (0.8) | 8–9 (1) | 8–10 (2) | 8–10 (2) |
| 4-Severe disability | 3 | 13.7 (1.2) | 13–15 (2) | 13–15 (2) | 13–15 (2) |
Table 4.
Baseline Functional Status Assessment According to Baseline PCPC. Differences between FSS scores in each PCPC interval were observed, with an FSS increase with each worsening PCPC category (P<0.001 for Spearman correlation between FSS and PCPC).
| Baseline PCPC | # of patients | Mean (SD) | Range (width)-25th to 75th percentiles | Range (width)-10th to 90th percentiles | Range (width)-5th to 95th percentiles |
|---|---|---|---|---|---|
| 1-Good | 530 | 6.0 (0.2) | 6–6 (0) | 6–6 (0) | 6–6 (0) |
| 2-Mild disability | 16 | 7.9 (2.1) | 6.5–9 (2.5) | 6–10 (4) | 6–14 (8) |
| 3-Moderate disability | 5 | 9.8 (2.9) | 8–9 (1) | 8–15 (7) | 8–15 (7) |
| 4-Severe disability | 2 | 13.0 (0) | 13–13 (0) | 13–13 (0) | 13–13 (0) |
Figure 1.
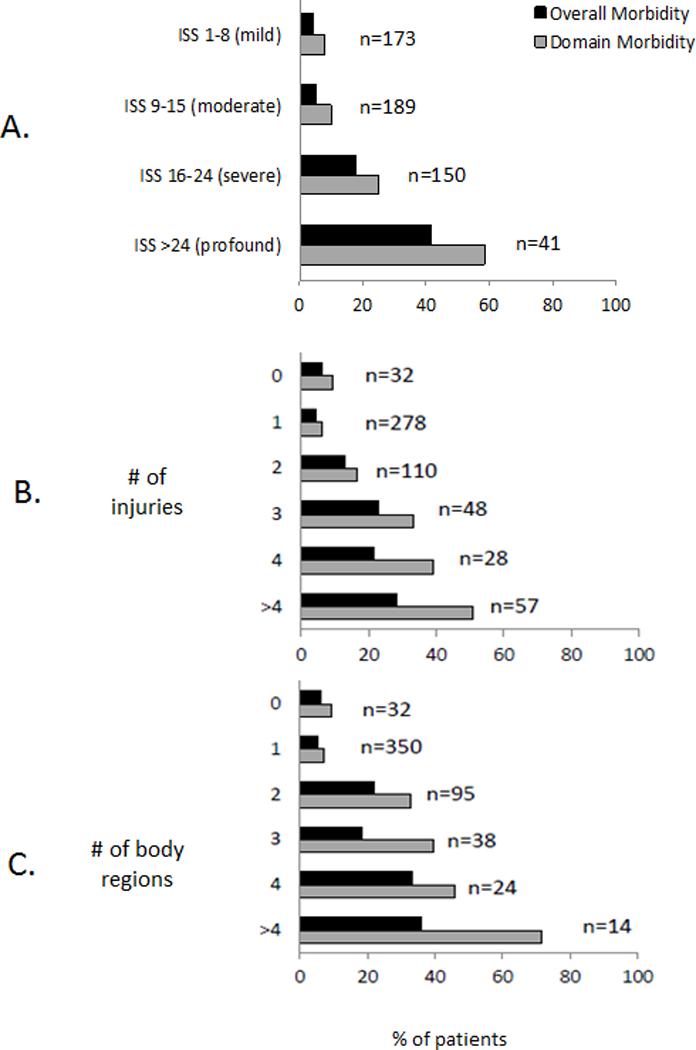
Association of New Overall and Domain Morbidity with Injury Severity A change in functional status, measured as either a change in domain morbidity (change ≥2 in any Functional Status Scale [FSS] domain) or overall new morbidity (change in FSS ≥3), is related to injury severity. Injury severity measured as: A. Injury Severity Score (ISS); B. number of injuries with Abbreviated Injury Scale (AIS) severity ≥2; and C. number of body regions with an injury with AIS severity ≥2. P<0.001 for all associations of categorized factors with rates and outcomes per Cochran-Armitage trend test.
In a multivariable logistic regression analysis, new domain morbidity was associated with both an increasing number of body regions with at least one injury with AIS severity ≥2 and injuries to specific body regions (Table 5). As an example of the former, patients with two injured areas were about five times more likely to acquire new domain-related morbidity than those with at most one injured area, while those with more than four injuries with AIS severity ≥2 were 17 times more likely (P<0.001 for significance of both comparisons via Wald test of model coefficients). The presence of a severe (AIS severity ≥4) injury in the head or spine region (P=0.04 and P=0.01, respectively) and the presence of a lower extremity injury with AIS severity ≥2 (P=0.01) were also independently associated with the occurrence of new domain-related morbidity (Table 5). In an evaluation of the domain-specific effects of covariates in this multivariate model, we observed that an increase in the number of body regions with at least one injury with AIS severity ≥2 was associated with a higher percentage of patients with impairment, with these morbidities being most common in the motor and feeding domains (Table 6). Patients with a severe spine injury (AIS severity ≥4) or a lower extremity injury with AIS severity ≥2 had a higher percentage of new morbidity in the motor domain and the largest change in FSS from baseline than those without injuries in these categories (Tables 6 and 7). Patients with at least a severe head injury had the greatest percentage difference in new domain morbidity and change in overall FSS in the motor domain, with the second largest difference observed in the feeding domain (Tables 6 and 7). The model relating the number of body regions with at least one injury with AIS severity ≥2 and injuries to specific body regions performed well with an area under the curve of 0.80 and a goodness of fit of P=0.79. The 32 patients with only a minor injury (AIS severity=1) had similar morbidity rates to those with only one body-region with an injury with AIS severity ≥2.
Table 5.
Multivariable Logistic Model Predicting Development of New Domain-related Morbidity
| Predictor | Odds Ratio (95% CI) | P-value |
|---|---|---|
| No. of Body Regions with severity ≥2 | <0.001 | |
| 0 or 1 | reference | |
| 2 | 5.29 (2.83, 9.89) | |
| 3 | 6.20 (2.63, 14.59) | |
| 4 | 6.83 (2.53, 18.47) | |
| >4 | 16.78 (4.28, 65.71) | |
| Head injury AIS severity ≥4 | 1.88 (1.03, 3.43) | 0.04 |
| Spine injury AIS severity ≥4 | 6.83 (1.46, 32.04) | 0.01 |
| Lower extremity injury AIS severity ≥2 | 2.29 (1.18, 4.46) | 0.01 |
No.-number; AIS-Abbreviated Injury Scale; c-statistic=80.1%; P=0.79 for Hosmer-Lemeshow test of fit.
Table 6.
Rates of Domain-Related New Morbidities (In Any Domain and Domain-Specific) Based on Factors in Multivariable Model
| Variable | No. of Patients | Any Domain (no., %) | Specific Domain (no., %) | |||||
|---|---|---|---|---|---|---|---|---|
| Communication | Feeding | Mental | Motor | Sensory | Respiratory | |||
| No. of body regions with AIS≥2 | ||||||||
| 0 | 32 | 3 (9.4) | 0 (0) | 1 (3.1) | 0 (0) | 2 (6.3) | 0 (0) | 1 (3.1) |
| 1 | 350 | 24 (6.9) | 4 (1.1) | 14 (4) | 6 (1.7) | 16 (4.6) | 5 (1.4) | 2 (0.6) |
| 2 | 95 | 31 (32.6) | 9 (9.5) | 14 (14.7) | 7 (7.4) | 24 (25.3) | 5 (5.3) | 3 (3.2) |
| 3 | 38 | 15 (39.5) | 2 (5.3) | 5 (13.2) | 2 (5.3) | 13 (34.2) | 1 (2.6) | 1 (2.6) |
| 4 | 24 | 11 (45.8) | 0 (0) | 5 (20.8) | 0 (0) | 9 (37.5) | 0 (0) | 1 (4.2) |
| >4 | 14 | 10 (71.4) | 1 (7.1) | 4 (28.6) | 1 (7.1) | 9 (64.3) | 0 (0) | 1 (7.1) |
| Head injury AIS≥4 | ||||||||
| Absent | 439 | 71 (16.2) | 11 (2.5) | 30 (6.8) | 12 (2.7) | 55 (12.5) | 8 (1.8) | 6 (1.4) |
| Present | 114 | 23 (20.2) | 5 (4.4) | 13 (11.4) | 4 (3.5) | 18 (15.8) | 3 (2.6) | 3 (2.6) |
| Spine injury. AIS≥4 | ||||||||
| Absent | 544 | 89 (16.4) | 15 (2.8) | 42 (7.7) | 15 (2.8) | 68 (12.5) | 9 (1.7) | 9 (1.7) |
| Present | 9 | 5 (55.6) | 1 (11.1) | 1 (11.1) | 1 (11.1) | 5 (55.6) | 2 (22.2) | 0 (0) |
| Lower extremity injury AIS≥2 | ||||||||
| Absent | 475 | 56 (11.8) | 11 (2.3) | 30 (6.3) | 12 (2.5) | 39 (8.2) | 9 (1.9) | 6 (1.3) |
| Present | 78 | 38 (48.7) | 30 (6.4) | 79 (16.7) | 24 (5.1) | 207 (43.6) | 12 (2.6) | 19 (3.9) |
AIS-Abbreviated Injury Scale; shading represents relative percentage ranging from 0 (white) to 100 (black). For association of morbidities with number of body regions by Cochran-Armitage trend test: P<0.001 for any domain, feeding, and motor; P=0.02 for communication, P=0.03 for respiratory. For association with head injury, no comparisons are significant at the 0.05 level. For association with spine injury by Fisher’s exact test, P=0.009 for any domain, P=0.003 for motor, P=0.01 for sensory. For association with lower extremity injury by Chi-squared test, P<0.001 for any domain and motor, P=0.002 for feeding.
Table 7.
Change in Overall Functional Status Scale (FSS) Based on Factors in Multivariable Model
| Variable | No. of Patients | Change in FSS from Baseline (SD) | Change in FSS from Baseline by Domain (SD) | |||||
|---|---|---|---|---|---|---|---|---|
| Communication | Feeding | Mental | Motor | Sensory | Respiratory | |||
| No. of body regions with AIS≥2 | ||||||||
| 0 | 32 | 0.4 (1.2) | 0.1 (0.2) | 0.1 (0.4) | 0.1 (0.2) | 0.1 (0.5) | 0.0 (0.0) | 0.1 (0.4) |
| 1 | 350 | 0.5 (1.8) | 0.1 (0.3) | 0.1 (0.4) | 0.1 (0.4) | 0.2 (0.6) | 0.1 (0.4) | 0.0 (0.3) |
| 2 | 95 | 2.1 (3.7) | 0.4 (0.9) | 0.3 (0.8) | 0.3 (0.5) | 0.9 (1.1) | 0.2 (0.7) | 0.1 (0.4) |
| 3 | 38 | 2.0 (3.6) | 0.3 (0.8) | 0.3 (0.7) | 0.2 (0.7) | 1.1 (1.1) | 0.1 (0.7) | 0.1 (0.3) |
| 4 | 24 | 1.9 (2.2) | 0.1 (0.3) | 0.5 (0.9) | 0.1 (0.3) | 1.1 (1.2) | 0.1 (0.3) | 0.1 (0.4) |
| >4 | 14 | 3.6 (3.7) | 0.4 (0.6) | 0.9 0.5) | 0.4 (0.6) | 1.6 (0.9) | 0.1 (0.4) | 0.3 (1.1) |
| Head injury AIS≥4 | ||||||||
| Absent | 439 | 0.9 (2.4) | 0.1 (0.5) | 0.2 (0.6) | 0.1 (0.5) | 0.4 (0.8) | 0.1 (0.5) | 0.0 (0.4) |
| Present | 114 | 1.3 (3.0) | 0.2 (0.5) | 0.3 (0.7) | 0.2 (0.6) | 0.4 (1.0) | 0.1 (0.5) | 0.1 (0.5) |
| Spine injury AIS≥4 | ||||||||
| Absent | 544 | 0.9 (2.5) | 0.1 (0.5) | 0.2 (0.6) | 0.1 (0.5) | 0.4 (0.8) | 0.1 (0.4) | 0.0 (0.4) |
| Present | 9 | 3.7 (5.5) | 0.6 (1.3) | 0.2 (0.7) | 0.4 (1.3) | 1.6 (1.4) | 0.9 (1.5) | 0.0 (0.0) |
| Lower extremity injury AIS≥2 | ||||||||
| Absent | 475 | 0.7 (2.3) | 0.1 (0.5) | 0.1 (0.5) | 0.1 (0.5) | 0.3 (0.8) | 0.1 (0.5) | 0.0 (0.3) |
| Present | 78 | 2.5 (3.4) | 0.3 (0.8) | 0.4 (1.0) | 0.3 (0.7) | 1.3 (0.9) | 0.1 (0.6) | 0.1 (0.6) |
AIS-Abbreviated Injury Scale; SD-standard deviation
DISCUSSION
Injury prevention and treatment advances have led to substantial declines in mortality in children, with a reported decrease in rate from 38 to 12 unintentional deaths/100,000 children (1981 to 2012).17 This decrease has been paralleled by declines in mortality among children treated at trauma centers from 3.4% to 0.9% mortality (1986 to 2015) (data obtained from Pennsylvania Trauma Systems Foundation, Camp Hill, PA), making it increasingly challenging to detect center differences using this metric. Although pediatric trauma mortality is declining, mortality remains the most common outcome measure for assessing quality and comparing treatments among hospitalized injured children.18–19 With an increasing awareness that mortality is declining in value as a quality of care metric, increased focus has been on identifying other measures for assessing quality of life outcomes because most children survive their injury. Children hospitalized after injury have a three-fold higher risk of long-term functional impairment compared to those who are not hospitalized after injury, and more than half will have a residual functional impairment at 12 months.6, 20 Given the impact of injury on short- and long-term functional status, functional status assessment has the potential to serve as a more effective metric for evaluating the outcome of hospitalized children than mortality.
The main purpose of this study was to determine the association between injury severity (overall and within different body regions) and change in functional status. Establishing this association will allow identification of cohorts of injured children at highest risk for functional impairment and their need for prospective functional status assessment. Although it is intuitive that functional impairment is related to injury severity and risk of mortality, this finding has not always been observed after pediatric injury. A positive association between higher impairment and ISS was found using the Functional Independence Measure (FIM)/WeeFIM among children, but was not consistently found using the physical summary component of the Child Health Questionnaire (CHQ).21–22 The body region injured has also been associated with the level of short-term functional status, with head and extremity injuries having worse outcomes than abdominal and chest injuries.6, 22 These studies, however, have weaknesses, including small sample size (populations not representing the range of injury types and severity), limited categorization of injury profiles, use of non-generalizable or complex measures applicable to only specific ages (e.g., FIM, CHQ) and performance at single centers (uncertain generalizability).
Although most commonly related to relative mortality risk, AIS severity codes are assigned based on several dimensions in addition to threat to life: impacted energy, extent of organ damage, permanent impairment and required period of injury management.23 For this reason, a useful metric measure of functional status should be expected to detect increasing impairment as AIS severity codes and other measures of injury severity relying on these codes increase. In this study, we observed a direct association between the level of functional impairment and injury severity using several metrics, including ISS, the number of injuries with AIS severity ≥2 and the number of body regions with at least one injury with AIS severity ≥2. This observation is similar to the general pediatric ICU population in which new morbidity is also associated with severity of illness measured by physiological profiles.12 Although ISS is a commonly used measure of overall injury severity, its value as a predictor of long-term functional status has been variable, likely related to calculation of ISS being based on the severity measured in at most three body regions. ISS distinguished functional status at discharge, with the least differentiation of functional status observed in children in lower ISS categories. The number of injury types and number of affected body regions have been proposed as severity metrics that may better predict functional status after injury.16 These metrics have a conceptual advantage over ISS because they allow consideration of the entire profile of injuries sustained and of injuries of lower severity that may have a higher impact on functional status than those with higher severity. Our findings showed that the spread of functional status change was best distributed across patients based on the number of affected body regions, supporting the benefits of using number of affected body regions for measuring injury severity in studies of functional status after injury.
Our findings suggest that domain-related new morbidity may be a more sensitive measure of functional impairment than overall new-morbidity, an observation that will need to be confirmed in follow-up studies. An analysis of the relationship between injury severity and domain-specific changes with increasing number of at least moderately severe injured body regions showed that the most dominant changes in FSS were in the feeding and motor domains. For this reason, new domain-related morbidity may be more sensitive to change than overall new morbidity for injured children, which reflects a composite difference in all domains. We also observed that functional status was normal in almost all children before injury and returned to or remained normal in most children at discharge as measured by FSS. Similar findings were reported in a cohort of injured children admitted to an ICU sustaining traumatic brain injuries.13 Injured children differed from the overall cohort of children treated in an ICU with the latter having more than 25% functional impairment at baseline and more than 35% impairment at hospital discharge.15 These findings suggest that critically injured children are by comparison a ‘healthier’ patient population than other children requiring ICU treatment and that they often return to baseline function at discharge, despite having injuries requiring intensive monitoring.
This study has several limitations. First, this was a secondary data analysis, with injured children being categorized retrospectively using available diagnosis codes and disease category assignments. Although patients were recruited and assessed by experienced research coordinators working within the CPCCRN network, a prospective determination of injury profiles would better define injury categorization. Second, these data were obtained more than five years ago. The use of more contemporaneous data may better represent the current state of trauma care and its outcomes. Third, this study was limited to children treated in an ICU at some point during their hospitalization. It is not known if similar findings extend to those treated outside of a critical care setting or if the timing of their ICU stays influences morbidity. In particular, children with significant orthopedic injuries are often treated outside of an ICU setting.24 Fourth, the long-term implications of hospital discharge functional status in this cohort are not known. Although changes in functional status may be identified at discharge, it is possible that this measured short-term disability may not uniformly be associated with long-term changes.
CONCLUSION
Although most injured children who survive to discharge have a ‘good’ FSS at discharge, a significant number will acquire new domain-related morbidity or overall new morbidity at discharge. New domain-related morbidity in injured children is associated with increasing number of body regions with at least one injury with AIS severity ≥2, an injury to the extremities with AIS severity ≥2 and severe injury (AIS severity ≥4) to the head and spine. The motor domain of the FSS is the most severely affected domain across all injury types, while feeding is the second most common for all categories except spine injury where sensory is, not surprisingly, second most common. Based on these findings, FSS has utility as an outcome measurement tool for the assessment of morbidity in children requiring ICU admission with injuries across a range of body regions. Given that it is granular, simple, relatively rapid to perform and applicable to all ages, FSS has the potential to be a useful metric for large-scale assessment of functional status after pediatric injury. Future studies are needed to define the long-term impact of pediatric injury in the domains measured by FSS and in other domains relevant to the health status of injured children.
ACKNOWLEDGEMENTS
1. Teresa Liu, MPH, CCRP; University of Utah (project management, Data Coordinating Center)
2. Jean Reardon, MA, BSN, RN; Children’s National Medical Center (institutional project management, data collection)
3. Elyse Tomanio, BSN, RN; Children’s National Medical Center (institutional project management, data collection)
4. Morella Menicucci, MD, CCRP; Children’s National Medical Center (data collection)
5. Fidel Ramos, BA; Children’s National Medical Center (institutional project management, data collection)
6. Aimee Labell, MS, RN; Phoenix Children’s Hospital (institutional project management, data collection)
7. Courtney Bliss, BS, DTR; Phoenix Children’s Hospital (data collection)
8. Jeffrey Terry, MBA; Children’s Hospital Los Angeles (data collection)
9. Margaret Villa, RN; Children’s Hospital Los Angeles and Mattel Children’s Hospital UCLA (institutional project management, data collection)
10. Jeni Kwok, JD; Children’s Hospital Los Angeles and Mattel Children’s Hospital (institutional project management, data collection)
11. Amy Yamakawa, BS; Children’s Hospital Los Angeles and Mattel Children’s Hospital UCLA (data collection)
12. Ann Pawluszka, BSN, RN; Children’s Hospital of Michigan (institutional project management)
13. Symone Coleman, BS, MPH; Children’s Hospital of Michigan (data collection)
14. Melanie Lulic, BS; Children’s Hospital of Michigan (data collection)
15. Mary Ann DiLiberto, BS, RN, CCRC; Children’s Hospital of Philadelphia (institutional project management, data collection)
16. Carolann Twelves, BSN, RN; Children’s Hospital of Philadelphia (data collection)
17. Monica S. Weber, RN, BSN, CCRP; University of Michigan (institutional project management, data collection)
18. Thomas Shanley, MD; Department of Pediatrics, University of Michigan, Ann Arbor, MI
19. Lauren Conlin, BSN, RN, CCRP; University of Michigan (data collection)
20. Alan C. Abraham, BA, CCRC; Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center (institutional project management, data collection)
21. Jennifer Jones, RN; Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center (data collection)
22. Jeri Burr, MS, RN-BC, CCRC; University of Utah (project management, Data Coordinating Center)
23. Nichol Nunn, BS, MBA; University of Utah (project management, Data Coordinating Center)
24. Alecia Peterson, BS, CMC; University of Utah (project management, Data Coordinating Center)
25. Carol Nicholson, MD (former Project Officer, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services, for part of the study period)
Research reported in this article was supported, in part, by the following cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN), National Institutes of Health, Department of Health and Human Services: U10HD050096, U10HD049981, U10HD049983, U10HD050012, U10HD063108, U10HD063106, U10HD063114 and U01HD049934. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflicts of interest to report.
REFERENCES
- 1.Institute for Health Metrics and Evaluation. GBD Compare Website Available at https://vizhub.healthdata.org/gbd-compare. Accessed February 15, 2018.
- 2.Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. A systematic review of quality indicators for evaluating pediatric trauma care. Crit Care Med 2010; 38(4):1187–96. [DOI] [PubMed] [Google Scholar]
- 3.Burd RS, Madigan D. The impact of injury coding schemes on predicting hospital mortality after pediatric injury. Acad Emerg Med 2009; 16(7):639–45. [DOI] [PubMed] [Google Scholar]
- 4.Dumas HM, Haley SM, Carey TM, Ni PS. The relationship between functional mobility and the intensity of physical therapy intervention in children with traumatic brain injury. Pediatr Phys Ther 2004; 16(3):157–64. [DOI] [PubMed] [Google Scholar]
- 5.Beers SR, Wisniewski SR, Garcia-Filion P, Tian Y, Hahner T, Berger RP, Bell MJ, Adelson PD. Validity of a pediatric version of the Glasgow Outcome Scale-Extended. J Neurotrauma 2012;29(6):1126–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabbe BJ, Simpson PM, Sutherland AM, Palmer CS, Williamson OD, Butt W, Bevan C, Cameron PA. Functional and health-related quality of life outcomes after pediatric trauma. J Trauma 2011; 70(6):1532–8. [DOI] [PubMed] [Google Scholar]
- 7.Shaklai S, Peretz R, Spasser R, Simantov M, Groswasser Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain Inj 2014; 28(7):915–21. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy ML. Measuring children’s health-related quality of life after trauma. J Trauma 2007; 63(6 Suppl):S122–9. [DOI] [PubMed] [Google Scholar]
- 9.Rios-Diaz AJ, Lam J, Zogg CK. The need for post discharge, patient-centered data in trauma. JAMA Surg 2016;151(12):1101–2. [DOI] [PubMed] [Google Scholar]
- 10.Pollack MM, Holubkov R, Funai T, Clark A, Moler F, Shanley T, Meert K, Newth CJ, Carcillo J, Berger JT, et al. Relationship between the functional status scale and the pediatric overall performance category and pediatric cerebral performance category scales. JAMA Pediatr 2014; 168(7):671–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollack MM, Holubkov R, Glass P, Dean JM, Meert KL, Zimmerman J, Anand KJ, Carcillo J, Newth CJ, Harrison R, et al. Functional Status Scale: new pediatric outcome measure. Pediatrics 2009; 124(1):e18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pollack MM, Holubkov R, Funai T, Berger JT, Clark AE, Meert K, Berg RA, Carcillo J, Wessel DL, Moler F, et al. Simultaneous Prediction of New Morbidity, Mortality, and Survival Without New Morbidity From Pediatric Intensive Care: A New Paradigm for Outcomes Assessment. Crit Care Med 2015; 43(8):1699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bennett TD, Dixon RR, Kartchner C, DeWitt PE, Sierra Y, Ladell D, Kempe A, Runyan DK, Dean JM, Keenan HT Functional Status Scale in children with traumatic brain Injury: A prospective cohort study. Pediatr Crit Care Med 2016; 17(12):1147–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Inj Prev 2015; 21(5):325–30. [DOI] [PubMed] [Google Scholar]
- 15.Pollack MM, Holubkov R, Funai T, Clark A, Berger JT, Meert K, Newth CJ, Shanley T, Moler F, Carcillo J, et al. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med 2014; 15(9):821–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gabbe BJ, Simpson PM, Lyons RA, Ameratunga S, Harrison JE, Derrett S, Polinder S, Davie G, Rivara FP Association between the number of injuries sustained and 12-month disability outcomes: evidence from the injury-VIBES study. PLoS One 2014; 9(12):e113467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Prevention and Control, Health, United States, Injury, 2014. Available at: http://www.cdc.gov/nchs/data/hus/2015/075.pdf. Accessed on December 12, 2016.
- 18.Cooper CG, Santana MJ, Stelfox HT. A comparison of quality improvement practices at adult and pediatric trauma centers. Pediatr Crit Care Med 2013; 14(8):e365–71. [DOI] [PubMed] [Google Scholar]
- 19.McCarthy A, Curtis K, Holland AJ. Paediatric trauma systems and their impact on the health outcomes of severely injured children: An integrative review. Injury 2016; 47(3):574–85. [DOI] [PubMed] [Google Scholar]
- 20.Polinder S, Meerding WJ, Toet H, Mulder S, Essink-Bot ML, van Beeck EF. Prevalence and prognostic factors of disability after childhood injury. Pediatrics 2005; 116(6):e810–7. [DOI] [PubMed] [Google Scholar]
- 21.Winthrop AL, Brasel KJ, Stahovic L, Paulson J, Schneeberger B, Kuhn EM. Quality of life and functional outcome after pediatric trauma. J Trauma 2005; 58(3):468–73; discussion 73–4. [DOI] [PubMed] [Google Scholar]
- 22.Schweer LH, Cook BS, Bivens K, Van Kuiken D, Garcia VF, Falcone RA Jr. Family perception: quality of life following a child’s traumatic injury. J Trauma Nurs 2006; 13(1):6–14. [DOI] [PubMed] [Google Scholar]
- 23.Rau CS, Wu SC, Kuo PJ, Chen YC, Chien PC, Hsieh HY, Hsieh CH. Same Abbreviated Injury Scale values may be associated with different risks to mortality in trauma patients: A cross-sectional retrospective study based on the trauma registry system in a level I trauma center. Int J Environ Res Public Health 2017;14:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tomaszewski R, Gap A. Results of the treatment of the open femoral shaft fractures in children. J Orthop 2014;11(2):78–81. [DOI] [PMC free article] [PubMed] [Google Scholar]


